Abstract
Basidiobolomycosis is a rare fungal infection with high prevalence in southwestern province of Saudi Arabia (Tohama region); it mainly causes subcutaneous infections and rarely gastrointestinal disease. Because of its indolent presentation, it is often misdiagnosed as IBD, tuberculosis or Malignancy.
We are reporting a 7 year old Saudi girl with abdominal mass, fever and eosinophilia resembling malignancy on radiological and pathological picture fully recovered with only medical therapy in the form of oral Voriconazole 2012 Elsevier Ltd. All rights reserved.
Keywords: Gastrointestinal, Basidiobolomycosis, Voriconazole
1. Introduction
Basidiobolus ranarum it is a member of the order Entomophthorales, which were previously classified in the class Zygomycetes. Basidiobolus ranarum was first described in 1886 in frogs. This fungus is an environmental saprophyte found in soil and decaying vegetable materials [1]. The disease mainly presents as a chronic non-angioinvasive subcutaneous infection in immunocompetent individuals [2]. Involvement of the gastrointestinal tract is a rare presentation, which in all reported cases has posed diagnostic difficulties [3]. Most of the cases diagnosed by histopathology findings and the first case of gastrointestinal basidiobolomycosis proven by culture was on 1986 in USA [4].
Our case is a Saudi girl from high risk area who presented with tumor-like abdominal mass which turned out to be gastrointestinal basidiobolomycosis treated successfully with Voriconazole without surgical intervention.
2. Case
Our patient is a previously healthy 7 years old girl from Tohama Aseer which is located in the south western region in Saudi Arabia. She presented with 3 months history of abdominal pain and mass felt in her lower abdomen with constipation. It was associated with intermittent fever and significant weight loss. She went to a local hospital in Asser where computed tomography (CT) scan of the abdomen revealed a big pelvic mass with high suspicion of lymphoma. She was referred to our hospital (day 0) (King Fahad Medical City) for further diagnosis and management.
Physical examination revealed cachectic child with severe pain and a large tender palpable mass extending from the hypogastric to the left iliac region of the abdomen measuring about 5*8 cm with no organomegaly or lymphadenopathy. Respiratory and cardiac examination were unremarkable.
Laboratory investigations showed white blood cell count (19.000 × 109/l), hemoglobin 7.4 g/dl, Platelets 822 × 109/l, eosinophilia (3000 × 109/l), and elevated erythrocyte sedimentation rate (ESR) 120 mm/h. Liver function test and alpha fetoprotein were normal.
Enhanced CT scan of abdomen with oral contrast (day1) revealed a large lobulated heterogonous pelvic mass most likely arising from the sigmoid colon causing narrowing, however there is no bowel obstruction. The mass is extended posteriorly to right pelvic side-wall causing compression on the rectum and distal right ureter resulting in right sided hydronephrosis. Magnetic resonance imaging (MRI) was done (day 2) for further characterization and it revealed heterogeneous mass on T2 with heterogeneous post contrast enhancement. The radiological appearance is highly suspicious for malignancy like Rhabdomyosarcoma (Fig. 1, Fig. 2).
Fig. 1.
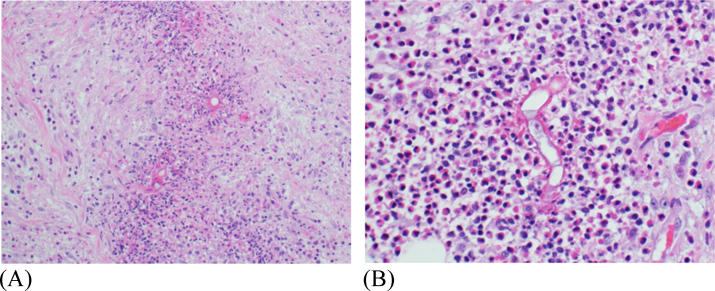
Mesenteric fat and connective tissue with heavy infiltration by lymphocytes, histiocytes, plasma cells and eosinophils. Large and wide septated fungal hyphae are seen in association with nucleated basidiospores. Eosinophilic cell aggregates condense around the fungal hyphae forming Splendore-Hoeppli phenomenon.
Fig. 2.
There is a large pelvic mass extending from the anterior abdominal wall to the right side of the pelvis posteriorly it is surrounding the sigmoid which is seen passing through the mass with no signs of obstruction however the mass is causing significant mass effect on the rectum and right-sided vesicouretric junction causing right side hydrouretronephrosis.
Laparotomy was done and biopsy was taken from the pelvic mass(day 3). The preliminary intra-operative frozen section showed dense infiltration by lymphocytes,histiocytes, plasma cells and eosinophils. This cellular infiltrate was interpreted as round blue cell tumor. porta Cath inserted preparing her for chemotherapy (day 6).
Histopathological examination of the biopsy revealed mesenteric fat and connective tissue with heavy infiltration by lymphocytes, histiocytes, plasma cells and eosinophils. Large and septated fungal hyphae are seen in association with nucleated basidiospores. Eosinophilic cells aggregates condense around the fungal hyphae forming Splendore-Hoeppli phenomenon. The fungal hyphae are positive for PAS special stain (Day7) (Figure 3 and 4).
The patient was treated with IV Voriconazole (7 mg/kg/dose every 12 h) (day 7), she showed quick improvement within few days, fever subsided and pain resolved with good oral intake. She was shifted to oral Voriconazole with the same dose (7 mg/kg/dose every 12 h) after one month of IV therapy. The patient was followed up in monthly bases as outpatient. She showed significant improvement both clinically and radiologically. Voriconazole was stopped after complete disappearance of the intra-abdominal mass. She received total of 9 months of Voriconazole.
3. Discussion
Basidiobolomycosis is an unusual fungal infection caused by Basidiobolus ranarum. It belongs to the order Entomophthorales which were previously classified in the class Zygomycetes. Basidiobolus species is fungus found in soil and decaying vegetables [1], [3]. It is well known to cause subcutaneous involvement and it may leads to subcutaneous nodules, lymphedema and hyperpigmentation mainly in limb, buttocks and back. It is seen frequently in tropical areas [4]. The first case of subcutaneous mycosis caused by Basidiobolus ranarum was reported in 1956 in Indonesia [5].
Gastrointestinal basidiobolomycosis is a very rare and potentially lethal fungal infection which affects mostly the immunocompetent host, to date less than 80 cases have been reported in English literature in both children and adult. Most of the cases reported from Saudi Arabia (Tohama region), United States (Arizona) and Iran [6], [7]. the first case reported as Gastrointestinal basidiobolomycosis was in 1964 in 6 years old Nigerian boy [8]. Basidiobolus ranarum has been found in soil and decaying vegetation and it is still unclear how acquisition of infection occur. The theory of contaminated food, animal feces and soil ingestion is the most likely route of transmission [9].
Based on available data gastrointestinal basidiobolomycosis affects males more than female. The presentation of the disease is vague and indolent. It commonly presents as abdominal pain, prolonged fever, weight loss, high ESR and peripheral eosinophilia. Most of the cases has been misdiagnosed as malignancy, Tuberculosis or Crohn's disease [6], [10]. There are several reasons behind this diagnostic confusion. First, the nonspecific clinical presentation. Shreef et al. [11] did a systematic review about all cases of gastrointestinal basidiobolomycosis in Saudi Arabia and he found that abdominal pain was the most common presentation (94.4%) followed by constipation (83.3%) and abdominal mass (77.8%); only 22.2% of cases presented with fever. Second, it often confused with malignancy or Crohn's disease because of the spread of the abdominal mass to other organs. Third, that endoscopic specimens usually shows nonspecific inflammation because the infection involves the nonmucosal layers of the gastrointestinal tract.
Radiologically, most of the cases reported as abdominal masses in the colon, liver mass or small bowel mass. Serious complication such as intestinal perforation, abscess and hydronephrosis were reported as well [12].
Although, majority of the cases were diagnosed based on the histopathological findings but the definitive diagnosis were proven by culture which is the gold standard. Sabouraud agar is the medium used for isolation of Basidiobolus ranarum and the growth needs 2–3 days in 25–30c. Colonies appear as white to gray with radial folds in the plates [13], [14]. PCR has been used recently to diagnose gastrointestinal basidiobolomycosis and it showed high sensitivity and specificity but still not widely used due to the rarity of the disease [15].
Most of the reported cases treated as combined treatment (surgical and medical). There are few reported cases responded to medical treatment alone without surgical intervention [18,19]. The azoles antifungal group are consider the best choice for basidiobolomycosis while amphotericin showed treatment failure. Itraconazole is the most frequently used antifungal to treat gastrointestinal basidiobolomycosis.recently, Voriconazole and Posaconazole showed to be effective treatment [16], [17].death and recurrence has been reported in some cases [7].
In conclusion, our case and several reported cases showed success of antifungal therapy without surgery. Abdominal mass with eosinophilia should raise the possibility of gastrointestinal basidiobolomycosis especially for patients coming from high risk area such as Tohama region in Saudi Arabia. Early diagnosis and treatment are associated with favorable prognosis and outcome. New generations of antifungal therapy in the form of Voriconazole can be sufficient treatment for basidiobolomycosis unless there is an obstruction of the bowel or serious pressure effects to the intraabdominal organs.
Conflict of interest
The authors declare that they have no competing interests.
Acknowledgements
None
References
- 1.Kwon-chung K.J. Taxonomy of fungi causing mucormycosis and Entomophthoramycosis (zygomycosis) and nomenclature of the disease. Clin. Infect. Dis. 2012;54:S8–S15. doi: 10.1093/cid/cir864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prasad P.V., Paul E.K., George R.V., Ambujam S., Viswanthan P. Subcutaneous phycomycosis in a child. Indian J. Dermatol. Venereol. Leprol. 2002;68:303–304. [PubMed] [Google Scholar]
- 3.Al-Shanafey S., AlRobean F., Bin Hussain I. Surgical management of gastrointestinal basidiobolomycosis in pediatric patients. J. Pediatr. Surg. 2012;47:949–951. doi: 10.1016/j.jpedsurg.2012.01.053. [DOI] [PubMed] [Google Scholar]
- 4.Schmidt J.H., Howard R.J., Chen J.L., Pierson K.K. First culture-proven gastrointestinal entermophthoromycosis in the United States: a case report and review of the literature. Mycopathologia. 1986;95:101–104. doi: 10.1007/BF00437168. [DOI] [PubMed] [Google Scholar]
- 5.Okafor J.I., Testrake D., Mushinsky H.R., Yangco B.G. A Basidiobolus sp. and its association with reptiles and amphibians in southern Florida. Sabouraudia. 1984;22:47–51. doi: 10.1080/00362178485380081. [DOI] [PubMed] [Google Scholar]
- 6.Shaikh N., Hussain K.A., Petraitiene R., Schuetz A.N., Walsh T.J. Entomophthoramycosis: a neglected tropical mycosis. Clin. Microbiol. Infect. 2016;22:688–694. doi: 10.1016/j.cmi.2016.04.005. [DOI] [PubMed] [Google Scholar]
- 7.Joe L.K., ENG N.T., Pohan A., Van Dr Meulen H., Emmonos C.W., Bethesda Basidiobolus ranarum as a cause of subcutaneous mycosis in Indonesia. AMA Arch. Derm. 1956;74(4):378–383. doi: 10.1001/archderm.1956.01550100046008. [DOI] [PubMed] [Google Scholar]
- 8.Al Jarie T., Al Azraki I., Al Mohsen S., Al Jumaah A., Almutawa, Fahim Y. Mohd. Basidiobolomycosis: case series. J. Med. Mycol. 2011;21:1. doi: 10.1016/j.mycmed.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 9.Geramizadeh B., Heidari M., Shekarkhar G. Gastrointestinal basidiobolomycosis, a rare and Under-diagnosed fungal infection in immunocompetent hosts: a review article. Iran. J. Med. Sci. 2015;40(2):90–97. [PMC free article] [PubMed] [Google Scholar]
- 10.Edington G.M. Phycomycosis in Ibadan, Western Nigeria: two postmortem reports. Trans. R. Soc. Trop. Med. Hyg. 1964;58:242–245. doi: 10.1016/0035-9203(64)90036-7. [DOI] [PubMed] [Google Scholar]
- 11.Shreef K., Saleem M., Saeedd M., Eissa M. Gastrointestinal basidiobolomycosis an emerging, and a confusing, disease in children(a multicenter experience) Eur. J. Pediatr. Surg. 2016;5(5):131–134. doi: 10.1055/s-0037-1598104. [DOI] [PubMed] [Google Scholar]
- 12.Al-Asmi M.M., Faqeehi H.Y., Alshahrani D.A., Al-Hussaini A.A. A case of pediatric gastrointestinal Basidiobolomycosis mimicking Crohn's disease. A review of pediatric literature. Saudi Med. J. 2013;34:1068–1072. [PubMed] [Google Scholar]
- 13.El-Shabrawi M.H., Kamal N.M., Kaerger K., VoigtK Diagnosis of gastrointestinal basidiobolomycosis: a mini-review. Mycoses. 2014;57:138–143. doi: 10.1111/myc.12231. [DOI] [PubMed] [Google Scholar]
- 14.Flicek K.T., Vikram H.R., De Petris G.D., Johnson C.D. Abdominal imaging findings in gastrointestinal basidiobolomycosis. Abdom. Imaging. 2015;40(2):246–250. doi: 10.1007/s00261-014-0212-z. (02) [DOI] [PubMed] [Google Scholar]
- 15.Gugnani H.C. A review of zygomycosis due to Basidiobolus ranarum. Eur. J. Epidemiol. 1999;15:923–929. doi: 10.1023/a:1007656818038. [DOI] [PubMed] [Google Scholar]
- 16.Zabolinejad N., Naseri A., Davoudi Y., Joudi M., Aelami M.H. Colonic basidiobolomycosis in a child: report of a culture-proven case. Int. J. Infect. Dis. 2014;22:41–43. doi: 10.1016/j.ijid.2013.11.016. [DOI] [PubMed] [Google Scholar]
- 17.Gómez-Muñoz M.T., Fernández-Barredo S., Martínez-Díaz R.A., Pérez-Gracia M.T., Ponce-Gordo F. Development of a specific polymerase chain reaction assay for the detection of Basidiobolus. Mycologia. 2012;104:585–591. doi: 10.3852/10-271. [DOI] [PubMed] [Google Scholar]
- 18.Albaradi Bandar A., Babiker Amir M.I., Al-Qahtani Hadi S. Successful treatment of gastrointestinal basidiobolomycosis with Voriconazole without surgical intervention. J. Trop. Pediatr. 2014;60(6):476–479. doi: 10.1093/tropej/fmu047. [DOI] [PubMed] [Google Scholar]
- 19.Rose S.R., Lindsley M.D., Hurst S.F., Paddock C.D., Damodaran T., Bennett J. Gastrointestinal basidiobolomycosis treated with posaconazole. Med. Mycol. Case Rep. 2013;2:11–14. doi: 10.1016/j.mmcr.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]