Abstract
Background
Many adults are discharged to skilled nursing facilities (SNFs) prior to returning home from the hospital. Patient characteristics and factors that can help to prevent post-discharge adverse outcomes are poorly understood.
Objective
To identify whether early post SNF discharge care reduces likelihood of 30 day hospital readmissions.
Design
Secondary data analysis using the Electronic Medical Record, Medicare, Medicaid and the Minimum Data Set.
Participants/Setting
Older (age > 65), community dwelling adults admitted to a safety net hospital in the Midwest for 3 or more nights and discharged home after a SNF stay (n=1,543).
Measurements
The primary outcome was hospital readmission within 30 days of SNF discharge. The primary independent variables were either a home health visit or an outpatient provider visit within a week of SNF discharge.
Results
Out of 8,754 community dwelling, hospitalized older adults, 3,025 (34.6%) were discharged to a SNF, of whom 1,543 (51.0%) returned home. Among the SNF to home group, a home health visit within a week of SNF discharge was associated with reduced hazard of 30-day hospital readmission (adjusted hazard ratio (aHR) 0.61, p<0.001) but outpatient provider visits were not associated with reduced risk of hospital readmission (aHR=0.67, p= 0.821).
Conclusion
For patients discharged from a SNF to home, the finding that a home health visit within a week of discharge is associated with reduced hazard of 30 day hospital readmissions suggests a potential avenue for intervention.
Keywords: care transitions, home care, primary care, hospital readmission, skilled nursing facility
Introduction
Since 1990, there has been a dramatic rise in patients discharged from the hospital to a skilled nursing facility (SNF), from 20 million bed days per year to over 50 million.1,2 This rise in SNF use has been accompanied by a decrease in hospital length of stay (LOS) and an increase in the acuity of patients arriving in SNFs.2,3 Community dwelling older patients enter a familiar cycle when they become acutely ill that includes the following points of care (Figure 1): hospital admission, discharge to SNF, and eventual transition back home. Despite this common trajectory, there is very little evidence regarding the distinct patient characteristics, needs and outcomes of this transition from a SNF to home. 2-4
Figure 1. Hospital to SNF to Home Trajectory.
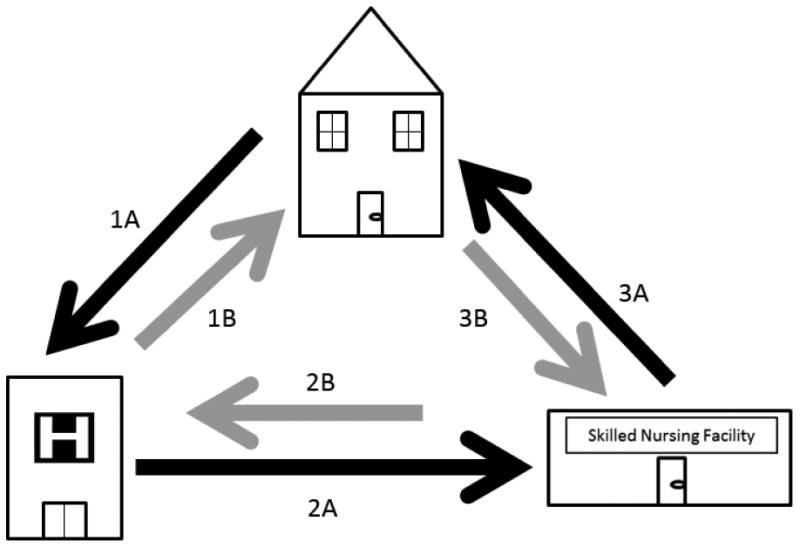
We describe two populations: 1) the Hospital to Home Group which traverses Arrow 1A followed by Arrow 1B and; 2) the SNF to Home Group which traverses Arrows 1A, 2A, and 3A.
There is evidence that after a discharge from hospital to home, patients are at risk of adverse drug events, lost inpatient test results, social isolation, Emergency Department (ED) visits and hospital readmissions.5-7 Patients who are discharged home from SNFs are generally more vulnerable to poor outcomes than patients who are discharged directly home from hospitals, and thus are at higher risk of adverse outcomes.3 However, little is known about the transition from SNF to home or the risk factors for adverse outcomes such as hospital readmission. Care in SNFs has come under amplified scrutiny as evidenced by Medicare rules to levy 30-day readmission penalties on SNFs.8 Data are needed to identify both risk factors for adverse outcomes such as readmission and potential targets for intervention.
In the hospital to home literature, early outpatient follow-up, such as early home health visits and early provider visits, have been identified as potential targets for intervention, yet, the evidence for each intervention is mixed. Increased readmissions for post-hospital patients with primary care follow up has been demonstrated in observational studies however, other studies have demonstrated reduced ED visits and hospital admissions for patients who frequently utilize primary care.9-11 The same conflicting results are seen in studies of home health interventions.12-17 For example, one study found surgical patients discharged home with home healthcare were more likely to have a “nonsevere” readmission but not a “severe”readmission, with severe readmission being defined by whether or not an invasive procedure is performed during the readmission stay.15 Another study of heart failure patients found that neither one week home health nor one week primary care visits were preventative of 30-day readmissions but, in combination, they significantly reduced the likelihood of hospital readmissions.14
Primary care follow up within a week of SNF discharge is the recommended best practice by the American Geriatrics Society, the Society of General Internal Medicine and AMDA-The Society for Post-Acute and Long Term Care.18 Yet there is little empiric evidence for this approach for the SNF to home population, and few of the published interventions aimed at improving the SNF to home transition incorporate tactics that include partnering with outpatient care providers into their program.19-21 We conducted a secondary data analysis to determine whether early outpatient follow-up is associated with hospital readmission. The primary hypothesis of our study is that patients who have early post-discharge care, here meaning an outpatient clinic visit or home health visit within a week of SNF discharge, will be less likely to return to the hospital within 30 days of SNF discharge.
Methods
Study Design
This is a secondary data analysis utilizing the Older Adults Transition Study (OATS) database. The OATS database has been described elsewhere.22,23 This database includes a cohort of 33,386 patients cared for at a safety net hospital in central Indiana. Eskenazi Health (formerly Wishard Memorial Hospital) includes a hospital plus eight community health centers that primarily serve a vulnerable patient population in Indianapolis, IN. Older adults in the cohort were seen at Eskenazi Health during the study period between January 1, 2007 and October 1, 2010. The OATS database combines data from Medicare and Medicaid claims, the Minimum Data Set (MDS), Outcome and Assessment Information Set (OASIS) and Eskenazi's local electronic medical records. This data enabled us to monitor patients' transitions across settings of care over time. The Indiana University Institutional Review Board approved this study.
Patients
We identified Medicare or dual eligible (Medicare and Medicaid) enrollees who experienced an acute hospitalization of greater than or equal to three nights and were then discharged home or to a SNF (Figure 2). Inclusion in the cohort was confirmed by matching the hospital discharge date to the SNF admission date. We excluded patients who died in the SNF, patients who did not enter the SNF directly from the hospital, and long stay patients (> 106 days based on a previous study24). We limited the eligible hospitalization period because of the change in MDS versions from 2.0 to 3.0 on October 1, 2010. OATS data were extracted one year prior and one year after the index hospitalization and SNF stay. All included patients had a SNF discharge date prior to October 1, 2010, the date MDS 3.0 was universally instituted with outcomes data through September 30, 2011.
Figure 2. Primary Cohort Flowchart.
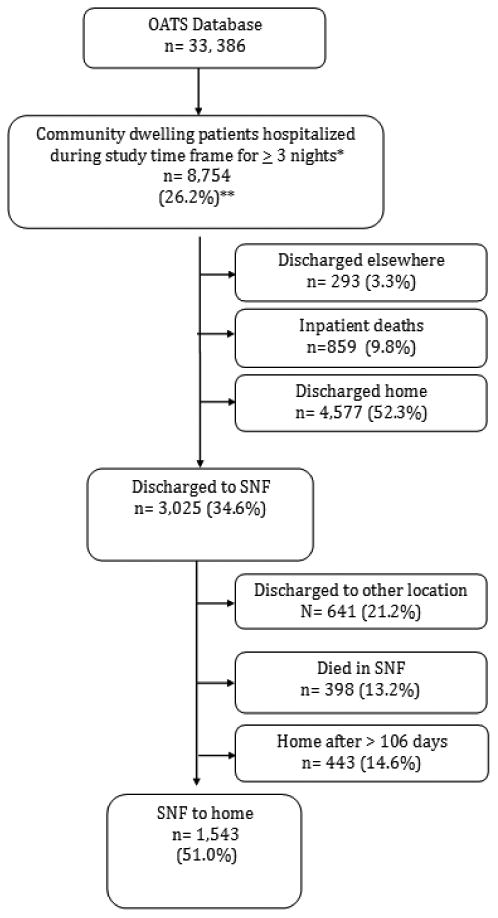
*Hospital admit dates are: 1/1/07-6/16/10. SNF subjects must be discharged from the SNF prior to 10/1/10.
** Percentages reported are the percent taken from the previous population on the figure; thus, 26.2% of the total OATS cohort was hospitalized during our study timeframe.
Data Collection
Data extracted from the OATS database included demographic data, data on the degree of pre-hospitalization health care use, pre-SNF inpatient hospitalization characteristics, and post-discharge healthcare utilization. The MDS enabled collection of detailed data obtained while in the SNF including in-SNF patient characteristics, and common geriatric syndromes and conditions. Electronic medical record and Medicare billing diagnosis codes for common chronic comorbidities were also examined using lists of ICD-9 diagnosis codes from previous studies22,25 Hospital admission diagnosis codes were grouped into the general systems based categories, for example, diagnoses in the 400s were circulatory. We calculated the LACE Index using hospital admission claims data. A LACE score greater than 10 identifies patients who have a high likelihood of 30-day hospital readmission or mortality.26
The MDS and electronic medical record allowed for more detailed data than claims data alone to be collected including in-SNF patient characteristics such as ADLs, and common geriatric syndromes such as sensory impairment, falls, medication and weight. ADL scores were derived from MDS data using a 6 point scale with higher scores indicating worse ADL functioning.27 We used the MDS to quantify the use of potentially unsafe medications (antipsychotics, anxiolytics, and hypnotics). Polypharmacy was defined as seven or more medications based on the least strict count from a panel of experts consensus via Delphi process.28
Our primary outcome variable, hospital readmission, was defined as readmission to an acute care hospital within 30 days of discharge from the SNF. We identified home health visits by using billing data from the OASIS home health dataset, and we identified outpatient provider visits using CMS billing data. The providers may be specialists or generalists, physicians or advanced practitioners. In either case, we used the first date of either home health or an outpatient clinic visit to determine whether they occurred within a week of SNF discharge or later.
Analysis
We assessed the bivariate associations between hospital readmission within 30 days and demographic, geriatric, and other patient characteristics by using chi-square tests for categorical data, and t tests for continuous variables; skewed variables were compared using Wilcoxon tests. To account for the inflation of Type 1 error rate, we adjusted p values by using the False Discovery Rate methods.29 We conducted a survival analysis to evaluate the distributions of time from SNF discharge to hospital readmission. Patients who were not readmitted were censored at the end of the 30 day period after SNF discharge. Similarly, patients who died within the first 30 days were censored at the time of death. Kaplan-Meier estimates of the survival functions for the SNF to home and hospital to home groups were presented to depict the survival functions. We compared the survival functions using the Wilcoxon test. Similarly we examined the distributions of time to outpatient visits. Finally, Cox proportional hazard models were used to model the times from discharge to readmission. Independent variables included the basic demographic and clinical characteristics, pre-hospital, hospital, and SNF events, as well as post hospital health care utilization. The independent variables entered the model by block in the aforementioned sequence. The final model was constructed based on the research team's content expertise, with the aid of values of Akaike's Information Criteria (AIC). All analyses were implemented using SAS v9.4 software (SAS Institute, Cary, NC). P values less than 0.05 were considered statistically significant.
Results
The sample cohort included 8,754 community dwelling patients admitted to the hospital for a minimum of three nights during our study time frame (Figure 2). Of those, 859 died while inpatient. Patients discharged directly home totaled 4,577 (hospital to home cohort) and patients discharged to the SNF, 3,090. The remaining 293 did not qualify for the study because they were discharged elsewhere such as an inpatient rehabilitation unit or a long-term acute care hospital. Of the SNF patients, 1,543 were discharged home within 106 days of hospital admission (SNF to home group).
In the bivariate comparison of patients readmitted to the hospital within 30 days of SNF discharge and those who were not (Table 1), we found that 30 day hospital readmission was associated with ED visits prior to the index hospital admission (p<0.001), dual eligibility (p=0.039), higher comorbidity counts (p<0.001), and the common comorbidities of heart disease, heart failure, and COPD (p values are 0.194, 0.002, and 0.005 respectively). Fewer patients who had had falls within the 30 days prior to admission were readmitted after SNF discharge (p=0.022). Patients admitted to the hospital for circulatory disorders (p=0.009) or pulmonary disorders (p=0.011) were more likely to be readmitted to the hospital within 30 days of SNF discharge. Those with a longer average hospital LOS were also more likely to be readmitted (p=0.039). Readmitted patients had higher LACE scores on average than those who were not (p<0.001).
Table 1. SNF to home patients readmitted to the hospital in 30 days versus not readmitted.
| SNF to home cohort n=1,543 | 30-day readmissions n=225 (14.6%) | No 30-day readmission n=1,318 (85.4%) | P-value (multiple test adjustment using False Discovery Rate) | |
|---|---|---|---|---|
| Demographics | ||||
| Age | 78 (36 – 103) | 77 (61 – 96) | 78 (36 – 103) | .551 |
| Gender (female) | 1069 (69.4) | 147 (65.9) | 922 (70.0) | .413 |
| White | 1014 (67.6) | 159 (71.6) | 855 (66.9) | .321 |
| Black | 486 (32.4) | 63 (28.4) | 423 (33.1) | |
| BMI | 27 (12 – 147) | 26 (13 – 64) | 27 (12 – 147) | 1.000 |
| Dual Eligible | 714 (46.3) | 122 (54.2) | 592 (44.9) | .039 |
| Lives Alone | 671 (43.6) | 96 (42.7) | 575 (43.7) | .837 |
| <High school | 497 (32.6) | 76 (34.4) | 421 (32.3) | .729 |
| ≥High school | 1027 (67.4) | 145 (65.6) | 882 (67.7) | |
| Comorbidities number | 6 (0 – 11) | 7 (0 – 11) | 6 (0 – 11) | <.001 |
| CAD | 1037 (67.2) | 170 (75.6) | 867 (65.8) | .019 |
| CHF | 912 (59.1) | 158 (70.2) | 754 (57.2) | .002 |
| HTN | 1488 (96.4) | 218 (96.9) | 1270 (96.4) | .821 |
| Arthritis | 1221 (79.1) | 189 (84.0) | 1032 (78.3) | .148 |
| Diabetes | 934 (60.5) | 150 (66.7) | 784 (59.5) | .124 |
| COPD | 919 (59.6) | 157 (69.8) | 762 (57.8) | .005 |
| Cancer | 831 (53.9) | 138 (61.3) | 693 (52.6) | .055 |
| Liver disease | 318 (20.6) | 55 (24.4) | 263 (20.0) | .282 |
| Stroke | 438 (28.4) | 79 (35.1) | 359 (27.2) | .055 |
| Renal | 137 (8.9) | 26 (11.6) | 111 (8.4) | .282 |
| Dementia | 727 (47.1) | 113 (50.2) | 614 (46.6) | .481 |
| Pre hospital events | ||||
| Falls in past 30 days | 568 (36.8) | 64 (28.4) | 504 (38.2) | .022 |
| Home Health | 28 (1.8) | 2 (0.9) | 26 (2.0) | .318 |
| ED visits | 375 (24.3) | 80 (35.6) | 295 (22.4) | <.001 |
| Hospital events and diagnoses | ||||
| Hospital Admit dx* | ||||
| Injury | 271 (17.6) | 27 (12.0) | 244 (18.5) | .059 |
| MSK | 168 (10.9) | 15 (6.7) | 153 (11.6) | .088 |
| Blood | 12 (0.8) | 1 (0.4) | 11 (0.8) | .729 |
| Circulatory | 323 (20.9) | 65 (28.9) | 258 (19.6) | .009 |
| Congenital | 2 (0.1) | 0 (0) | 2 (0.2) | .729 |
| Dermatologic | 24 (1.6) | 6 (2.7) | 18 (1.4) | .300 |
| Endocrine | 66 (4.3) | 15 (6.7) | 51 (3.9) | .151 |
| Gastrointestinal | 76 (4.9) | 10 (4.4) | 66 (5.0) | .821 |
| Genitourinary | 123 (8.0) | 11 (4.9) | 112 (8.5) | .169 |
| Infectious | 62 (4.0) | 5 (2.2) | 57 (4.3) | .296 |
| Mental | 30 (1.94) | 4 (1.8) | 26 (2.0) | .889 |
| Neoplasm | 53 (3.4) | 9 (4.0) | 44 (3.3) | .769 |
| Nervous System | 52 (3.4) | 4 (1.8) | 48 (3.6) | .305 |
| Pulmonary | 158 (10.2) | 36 (16.0) | 122 (9.3) | .011 |
| ICU admission | 490 (31.8) | 76 (33.8) | 414 (31.4) | .688 |
| ICU LOS | 4 (1 – 31) | 4 (1 – 31) | 4 (1 – 31) | .658 |
| LACE score | 12 (4 – 19) | 13 (7 – 19) | 12 (4 – 19) | <.001 |
| Hospital LOS | 7 (3 – 82) | 8 (3 – 82) | 7 (3 – 47) | .039 |
| SNF events and diagnoses | ||||
| Incontinence | 512 (33.2) | 63 (28.0) | 449 (34.1) | .185 |
| Sensory impairment (hearing) | 195 (12.6) | 34 (15.1) | 161 (12.2) | .413 |
| Sensory impairment (vision) | 194 (12.6) | 30 (13.3) | 164 (12.4) | .821 |
| ADL score | 3 (0 – 6) | 3 (0 – 6) | 3 (0 – 6) | .769 |
| SNF LOS | 35 (3 – 107) | 35 (10 – 107) | 35 (3 – 107) | .887 |
| SNF emergency department transfer (any) | 280 (18.2) | 60 (26.7) | 220 (16.7) | .003 |
| Post Hospital Utilization | ||||
| Polypharmacy (≥ 7 medications) | 779 (85.3) | 126 (88.1) | 653 (84.8) | .481 |
| Outpatient visit within one week | 355 (23.0) | 45 (20.0) | 310 (23.5) | .435 |
| Home health care within 1 week | 778 (50.4) | 102 (45.3) | 676 (51.3) | .464 |
| 30 day mortality (post discharge to home) | 14 (0.9) | 7 (3.1) | 7 (0.5) | .002 |
Of the hospital admissions diagnosis codes, 123 were excluded from analysis because they were missing or not able to be categorized in the standard systems- based categories.
Values are medians (minimum - maximum) for continuous variables and frequencies (percentages) for categorical variables. For continuous variables, p-values are from Student's t-tests and Wilcoxon rank-sum tests. For categorical variables, p-values are from Chi-Square tests. Age is mean plus standard deviation
Several factors were examined from the MDS data collected during the SNF stay, including incontinence, sensory impairment, and SNF LOS. The only variable that was significantly associated with hospital readmission during the 30 days following SNF discharge was ED transfer during the SNF stay (p=0.003). After SNF discharge, those who died within 30 days were more likely to have been readmitted to the hospital, pre-death.
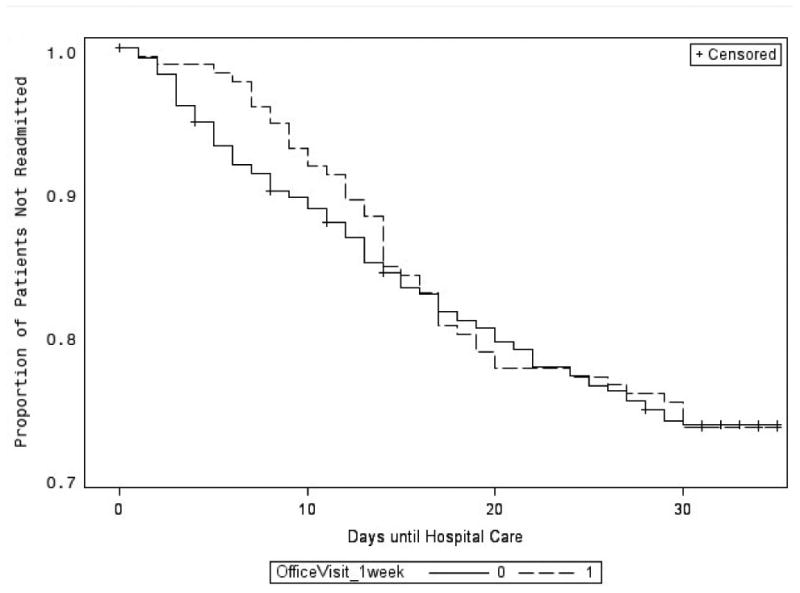
Kaplan-Meier estimates of time to readmission showed those who had a home health visit within a week of SNF discharge were less likely to have early readmission in the first 30 days than those who did not (p<0.001 per Wilcoxon test; Figure 3A). We found no difference in 30-day readmission rate among older adults discharged from a SNF between groups with and without an early ambulatory care visit (Figure 3B). Because the Kaplan-Meier curve appeared as though it may be significant prior to 30 days, we examined one, two and three week intervals for home care visits and outpatient visits. At all of these intervals, the home care visit was significantly associated with reduced likelihood of readmission. The outpatient clinic visits were associated with reduced likelihood of readmission at weeks 2 and 3 (p=0.009 and p=0.028) but not at weeks 1 or 30 days (p=0.172 and p=0.252). Finally, the multivariable Cox proportional hazards model analysis confirmed a lower hazard of 30 day post SNF hospital readmission when a home health visit occurred within a week of discharge from the SNF (p<0.001; Table 2). Outpatient visits with providers within a week of discharge were not associated with reduced hazard of a 30 day hospital readmission.
Figure 3. Product limit estimator graphs.
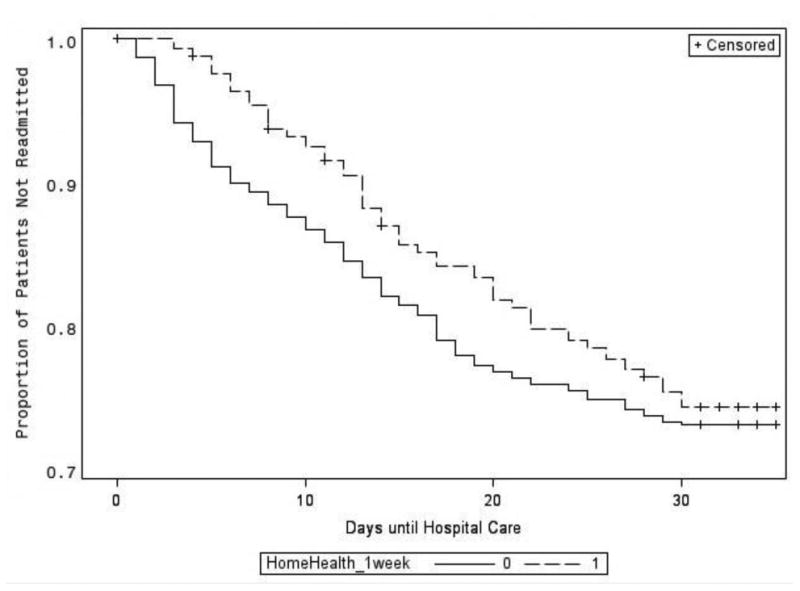
3A.: Hospital readmissions for those who had home health within a week versus those who did not.
Wilcoxon p-value for equality across state: p<0.001
3B.: Hospital readmissions for those who had outpatient visits within a week versus those who did not.
Wilcoxon p-value for equality across state: p=0.252
Table 2. Cox regression model for 30-day hospital readmissions of SNF to home patients.
| Variable | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 |
|---|---|---|---|---|---|
| Demographics | |||||
| Age (continuous) | 1.00;p=0.955 | 1.00;p=0.916 | 1.00;p=0.921 | 1.00;p=0.780 | 0.99;p=0.661 |
| Race (African American v. all others) | 1.16;p=0.348 | 1.21;p=0.240 | 1.37;p=0.067 | 0.81;p=0.072 | 0.82;p=0.211 |
| Gender (dichotomous) | 1.06;p=0.697 | 1.04;p=0.780 | 1.05;p=0.756 | 0.86;p=0.511 | 0.86;p=0.953 |
| Lives alone (yes v. no-dichotomous) | 0.98;p=0.865 | 0.98;p=0.893 | 0.99;p=0.934 | 0.98;p=0.610 | 0.97;p=0.514 |
| Dual-eligible | 0.91;p=0.564 | 0.93;p=0.663 | 0.90;p=0.524 | 1.12;p=0.663 | 1.10;p=0.910 |
| BMI | 1.00;p=0.760 | 1.00;p=0.693 | 1.01;p=0.534 | 1.00;p=0.297 | 1.01;p=0.082 |
| Dementia | 0.87;p=0.407 | 0.90;p=0.538 | 0.90;p=0.563 | 0.83;p=0.601 | 0.82;p=0.155 |
| Comorbidities # | 1.07;p=0.103 | 1.06;p=0.148 | 1.08;p=0.061 | 1.09;p=0.125 | 1.11;p=0.103 |
| Pre hospital events | |||||
| ED visits | 1.10;p=0.522 | 1.21;p=0.225 | 1.48;p=0.404 | 1.44;p=0.923 | |
| Home health | 0.43;p=0.254 | 0.34;p=0.143 | 0.31;p=0.129 | 0.32;p=0.071 | |
| Falls w/in the past 30 days | 1.19;p=0.301 | 1.20;p=0.277 | 0.73;p=0.183 | 0.71;p=0.159 | |
| Hospital events | |||||
| ICU admit (dichotomous y/n) | 0.69;p=0.017 | 0.89;p=0.025 | 0.89;p=0.062 | ||
| Hospital LOS | 0.99;p=0.403 | 1.01;p=0.535 | 1.01;p=0.667 | ||
| SNF events | |||||
| ADL score | 1.09;p=0.548 | 1.12;p=0.678 | |||
| SNF LOS | 1.00;p=0.221 | 1.00;p=0.451 | |||
| SNF ED transfer | 1.74;p=0.100 | 1.64;p=0.126 | |||
| Sensory impairment (hearing) | 1.06;p=0.497 | 1.08;p=0.126 | |||
| Sensory impairment (vision) | 1.13;p=0.193 | 1.16;p=0.096 | |||
| Incontinence | 0.77;p=0.746 | 0.77;p=0.498 | |||
| Post Hospital utilization | |||||
| Home with home health care within 1 week (Yes v. no) | 0.61;p<0.001 | ||||
| Outpatient visit within one week (yes v. no) | 0.67;p=0.821 | ||||
| AIC | 1968.278 | 1971.833 | 1968.538 | 1974.923 | 1959.407 |
Discussion
In this study, we found that home health visits within a week of SNF discharge were associated with reduced 30 day hospital readmissions. Outpatient clinician visits were associated with reduced hospital readmissions at weeks 2 and 3 but not overall 30 day readmissions. Home health visits can involve therapy, lab test monitoring, assistance with medication reconciliation and management, collaboration with family caregivers, in addition to early identification of environmental or social factors which may contribute to readmission.7,30,31 The ability of home health visits to provide insight on the home environment in addition to catching errors in a smooth transition of care may help explain the significance of the home health visit. These findings raise the question of whether an early home health visit may be a potential intervention to reduce hospital readmissions after a transition from SNF to home. A qualitative study or a study using more detailed OASIS billing data may lend insight to this important question. What is not clear from this secondary data analysis is what specific aspects of home health visits are helping patients to remain at home, especially since this group is high risk for hospital admission.32 Future research is needed to explore this important question.
In contrast, clinician visits were not significantly associated with reduced 30 day readmission, though there was an effect at two and three weeks. It is possible that these visits could be both preventative when they clarify transitions issues but also causative when clearly sick patients are sent back to the hospital from a clinic. Home health visits would also likely identify patients needing more acute level care but possibly less so because their assessments can be less intense than a clinic visit or because they refer ill-appearing patients to the clinic for further work-up. Thus, patients would be readmitted after these clinic visits. More fine tuned studies of the role of post-SNF clinic visits and home health visits are warranted.
In bivariate analyses, we found that several demographic factors that have been found to be associated with hospital readmission after discharge home such as age, race and gender were not significantly associated with hospital readmission after SNF discharge in our population of interest.13,30,33 Having Medicaid insurance, which may be a proxy for more disadvantaged socioeconomic status, was associated with readmission in bivariate analysis but was no longer significant in the multivariable model. Currently, the nursing home hospital readmission penalty adjusts for gender because women are thought to be significantly lower risk for readmission.34 Additional sociodemographic variables are being considered as candidates to add to the risk stratification formula for hospital readmission penalties.13 The lack of association between demographic variables and readmission after SNF discharge suggest that this risk adjustment may not be warranted.
In terms of comorbidities and hospital diagnoses it is unsurprising that cardiac and pulmonary disorders are significant both as chronic diseases and as acute exacerbating conditions (Table 1). In readmissions literature, patients with these comorbidities are recognized as high risk for hospital readmission.35-37It is intriguing however that having a fall prior to admission indicates one is less likely to be readmitted. One of the more common reasons for patients to be transferred from nursing homes to EDs is falls in the facility and falls are a common post-hospital discharge adverse event.6,38,39 The incidence of falls increases with age and is high among nursing home residents overall.40 It is possible that because falls represent an acute event that those patients with some physical reserve can recuperate to previous level of function. Those discharged to SNFs who have experienced falls may do so because of the fall and not because of the overall frailty that lands patients with exacerbations of chronic comorbidities such as heart failure and COPD in a SNF. This is borne out in the hospital diagnoses that are associated with readmission. Injury is less likely to be associated with 30-day readmission whereas, admission diagnoses for heart or pulmonary conditions are more likely to be. It is also possible that those who do not revert to pre-fall levels of function may convert to long stay patients.41
Other findings from the bivariate analyses, while not significant in the final regression model were still of interest clinically. For example, there was a high number of ED transfers and hospital admissions during the patients' stays in the SNFs. Several efforts are underway now to reduce avoidable transfers of long term nursing home patients.42,43 Extension of these efforts may also be warranted in the short stay SNF population of patients.
Limitations of the study include that it is retrospective and that the cohort is only comprised of patients seen at our urban, safety net hospital in Indiana. Therefore, our findings may not generalize to other patient populations. The post-acute care environment has evolved somewhat since our data was collected however, the basic question of whether prevention of adverse post SNF discharge outcomes should focus on early provider care or early home health visits remains true today. Although home health care was significantly associated with reduced readmissions, this study does not provide information on the specific aspects of home care that were beneficial. A future study of this would enable home health providers to provide more targeted care to post-SNF patients who are high risk for readmission.
Conclusion
The finding that home health visits within a week of SNF discharge are associated with lower hazard of 30 day hospital readmission suggests that early home health should be further examined as a potential intervention to improve outcomes for this population. More study of what aspects of a home health visit are preventative and why outpatient provider visits may or may not be preventative is warranted to better serve this unique, growing, and vulnerable group of patients.
Acknowledgments
We would like to acknowledge Timothy E. Stump, MA and Roberta J. Ambuehl, BA for their assistance in data management for this manuscript.
This study was supported by National Institute on Aging Grant R01 AG031222.
Footnotes
No authors have conflicts of interest to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Commission MPA. Data Book: Healthcare spending and the Medicare program. [Accessed June 1, 2016];2015 Jun; http://medpac.gov/documents/data-book/june-2015-databook-health-care-spending-and-the-medicare-program.pdf?sfvrsn=0.
- 2.David S, Sheikh F, Mahajan D, Greenough W, Bellantoni M. Whom Do We Serve? Describing the target population for post-acute and long-term care, focusing on nursing facility, settings, in the era of population health. 2016 doi: 10.1016/j.jamda.2016.05.004. http://www.paltc.org/amda-white-papers-and-resolution-position-statements/whom-do-we-serve-describing-target-population. [DOI] [PubMed]
- 3.Burke RE, Juarez-Colunga E, Levy C, Prochazka AV, Coleman EA, Ginde AA. Patient and Hospitalization Characteristics Associated With Increased Postacute Care Facility Discharges From US Hospitals. Medical care. 2015;53(6):492–500. doi: 10.1097/MLR.0000000000000359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bell SP, Vasilevskis EE, Saraf AA, et al. Geriatric Syndromes in Hospitalized Older Adults Discharged to Skilled Nursing Facilities. Journal of the American Geriatrics Society. 2016;64(4):715–722. doi: 10.1111/jgs.14035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walz SE, Smith M, Cox E, Sattin J, Kind AJ. Pending laboratory tests and the hospital discharge summary in patients discharged to sub-acute care. Journal of general internal medicine. 2011;26(4):393–398. doi: 10.1007/s11606-010-1583-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–167. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 7.Greysen SR, Hoi-Cheung D, Garcia V, et al. “Missing pieces”--functional, social, and environmental barriers to recovery for vulnerable older adults transitioning from hospital to home. Journal of the American Geriatrics Society. 2014;62(8):1556–1561. doi: 10.1111/jgs.12928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carnahan JL, Unroe KT, Torke AM. Hospital Readmission Penalties: Coming Soon to a Nursing Home Near You! Journal of the American Geriatrics Society. 2016;64(3):614–618. doi: 10.1111/jgs.14021. [DOI] [PubMed] [Google Scholar]
- 9.Field TS, Ogarek J, Garber L, Reed G, Gurwitz JH. Association of Early Post-Discharge Follow-Up by a Primary Care Physician and 30-Day Rehospitalization Among Older Adults. Journal of general internal medicine. 2014 doi: 10.1007/s11606-014-3106-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li J, Williams MV. Care transitions: it's the how, not just the what. Journal of general internal medicine. 2015;30(5):539–540. doi: 10.1007/s11606-015-3225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nyweide DJ, Bynum JP. Relationship Between Continuity of Ambulatory Care and Risk of Emergency Department Episodes Among Older Adults. Ann Emerg Med. 2016 doi: 10.1016/j.annemergmed.2016.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gay JC, Thurm CW, Hall M, et al. Home Health Nursing Care and Hospital Use for Medically Complex Children. Pediatrics. 2016;138(5) doi: 10.1542/peds.2016-0530. [DOI] [PubMed] [Google Scholar]
- 13.Meddings J, Reichert H, Smith SN, et al. The Impact of Disability and Social Determinants of Health on Condition-Specific Readmissions beyond Medicare Risk Adjustments: A Cohort Study. Journal of general internal medicine. 2017;32(1):71–80. doi: 10.1007/s11606-016-3869-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murtaugh CM, Deb P, Zhu C, et al. Reducing Readmissions among Heart Failure Patients Discharged to Home Health Care: Effectiveness of Early and Intensive Nursing Services and Early Physician Follow-Up. Health services research. 2016 doi: 10.1111/1475-6773.12537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sanford DE, Olsen MA, Bommarito KM, et al. Association of discharge home with home health care and 30-day readmission after pancreatectomy. J Am Coll Surg. 2014;219(5):875–886.e871. doi: 10.1016/j.jamcollsurg.2014.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O'Connor M, Bowles KH, Feldman PH, et al. Frontloading and intensity of skilled home health visits: a state of the science. Home health care services quarterly. 2014;33(3):159–175. doi: 10.1080/01621424.2014.931768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wong FK, Chow SK, Chan TM, Tam SK. Comparison of effects between home visits with telephone calls and telephone calls only for transitional discharge support: a randomised controlled trial. Age Ageing. 2014;43(1):91–97. doi: 10.1093/ageing/aft123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lindquist LA, Miller RK, Saltsman WS, et al. SGIM-AMDA-AGS Consensus Best Practice Recommendations for Transitioning Patients' Healthcare from Skilled Nursing Facilities to the Community. Journal of general internal medicine. 2016 doi: 10.1007/s11606-016-3850-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berkowitz RE, Jones RN, Rieder R, et al. Improving disposition outcomes for patients in a geriatric skilled nursing facility. Journal of the American Geriatrics Society. 2011;59(6):1130–1136. doi: 10.1111/j.1532-5415.2011.03417.x. [DOI] [PubMed] [Google Scholar]
- 20.Delate T, Chester EA, Stubbings TW, Barnes CA. Clinical Outcomes of a Home-Based Medication Reconciliation Program After Discharge from a Skilled Nursing Facility. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy. 2008;28(4):444–452. doi: 10.1592/phco.28.4.444. [DOI] [PubMed] [Google Scholar]
- 21.Berkowitz RE, Fang Z, Helfand BK, Jones RN, Schreiber R, Paasche-Orlow MK. Project ReEngineered Discharge (RED) lowers hospital readmissions of patients discharged from a skilled nursing facility. Journal of the American Medical Directors Association. 2013;14(10):736–740. doi: 10.1016/j.jamda.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 22.Callahan CM, Arling G, Tu W, et al. Transitions in care for older adults with and without dementia. Journal of the American Geriatrics Society. 2012;60(5):813–820. doi: 10.1111/j.1532-5415.2012.03905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.LaMantia MA, Lane KA, Tu W, Carnahan JL, Messina F, Unroe KT. Patterns of Emergency Department Use Among Long-Stay Nursing Home Residents With Differing Levels of Dementia Severity. Journal of the American Medical Directors Association. 2016 doi: 10.1016/j.jamda.2016.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Toles M, Anderson RA, Massing M, et al. Restarting the cycle: incidence and predictors of first acute care use after nursing home discharge. Journal of the American Geriatrics Society. 2014;62(1):79–85. doi: 10.1111/jgs.12602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.LaMantia MA, Stump TE, Messina FC, Miller DK, Callahan CM. Emergency Department Use Among Older Adults With Dementia. Alzheimer disease and associated disorders. 2015 doi: 10.1097/WAD.0000000000000118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van Walraven C, Dhalla IA, Bell C, et al. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. CMAJ. 2010;182(6):551–557. doi: 10.1503/cmaj.091117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. J Gerontol A Biol Sci Med Sci. 1999;54(11):M546–553. doi: 10.1093/gerona/54.11.m546. [DOI] [PubMed] [Google Scholar]
- 28.Fried TR, Niehoff K, Tjia J, Redeker N, Goldstein MK. A Delphi process to address medication appropriateness for older persons with multiple chronic conditions. BMC Geriatr. 2016;16:67. doi: 10.1186/s12877-016-0240-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Benjamini Y, Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. Journal of the Royal Statistical Society Series B (Methodological) 1995;57(1):289–300. [Google Scholar]
- 30.Arbaje AI, Wolff JL, Yu Q, Powe NR, Anderson GF, Boult C. Postdischarge environmental and socioeconomic factors and the likelihood of early hospital readmission among community-dwelling Medicare beneficiaries. Gerontologist. 2008;48(4):495–504. doi: 10.1093/geront/48.4.495. [DOI] [PubMed] [Google Scholar]
- 31.Kind AJ, Jencks S, Brock J, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med. 2014;161(11):765–774. doi: 10.7326/M13-2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Monsen KA, Swanberg HL, Oancea SC, Westra BL. Exploring the value of clinical data standards to predict hospitalization of home care patients. Applied clinical informatics. 2012;3(4):419–436. doi: 10.4338/ACI-2012-05-RA-0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Middleton A, Graham JE, Lin YL, et al. Motor and Cognitive Functional Status Are Associated with 30-day Unplanned Rehospitalization Following Post-Acute Care in Medicare Fee-for-Service Beneficiaries. Journal of general internal medicine. 2016;31(12):1427–1434. doi: 10.1007/s11606-016-3704-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smith L, West S, Coots L, et al. Skilled Nursing Facility Readmission Measure (SNFRM) NQF #2510: All-Cause Risk-Standardized Readmission Measure: Draft Technical Report. RTI International; Mar, 2015. [Google Scholar]
- 35.Ouslander JG, Diaz S, Hain D, Tappen R. Frequency and diagnoses associated with 7- and 30-day readmission of skilled nursing facility patients to a nonteaching community hospital. Journal of the American Medical Directors Association. 2011;12(3):195–203. doi: 10.1016/j.jamda.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 36.Hines AL, Barrett ML, Jiang HJ, Steiner CA. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Healthcare Research and Quality (US); 2014. Conditions With the Largest Number of Adult Hospital Readmissions by Payer, 2011: Statistical Brief #172. [PubMed] [Google Scholar]
- 37.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. The New England journal of medicine. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 38.Ackermann RJ, Kemle KA, Vogel RL, Griffin RC., Jr Emergency department use by nursing home residents. Ann Emerg Med. 1998;31(6):749–757. doi: 10.1016/s0196-0644(98)70235-5. [DOI] [PubMed] [Google Scholar]
- 39.Cigolle CT, Langa KM, Kabeto MU, Tian Z, Blaum CS. Geriatric conditions and disability: the Health and Retirement Study. Ann Intern Med. 2007;147(3):156–164. doi: 10.7326/0003-4819-147-3-200708070-00004. [DOI] [PubMed] [Google Scholar]
- 40.Friedman SM, Mendelson DA, Bingham KW, McCann RM. Hazards of hospitalization: residence prior to admission predicts outcomes. Gerontologist. 2008;48(4):537–541. doi: 10.1093/geront/48.4.537. [DOI] [PubMed] [Google Scholar]
- 41.Seematter-Bagnoud L, Wietlisbach V, Yersin B, Bula CJ. Healthcare utilization of elderly persons hospitalized after a noninjurious fall in a Swiss academic medical center. Journal of the American Geriatrics Society. 2006;54(6):891–897. doi: 10.1111/j.1532-5415.2006.00743.x. [DOI] [PubMed] [Google Scholar]
- 42.Unroe KT, Nazir A, Holtz LR, et al. The Optimizing Patient Transfers, Impacting Medical Quality, andImproving Symptoms:Transforming Institutional Care approach: preliminary data from the implementation of a Centers for Medicare and Medicaid Services nursing facility demonstration project. Journal of the American Geriatrics Society. 2015;63(1):165–169. doi: 10.1111/jgs.13141. [DOI] [PubMed] [Google Scholar]
- 43.Ingber MJ, Feng Z, Khatutsky G, et al. Initiative To Reduce Avoidable Hospitalizations Among Nursing Facility Residents Shows Promising Results. Health affairs (Project Hope) 2017;36(3):441–450. doi: 10.1377/hlthaff.2016.1310. [DOI] [PubMed] [Google Scholar]


