Abstract
Background
Peripheral artery disease (PAD) is a highly prevalent disease that impairs walking ability. Walking tests, such as the 6-minute walk test (6MWT) and 4-meter walk test, are commonly used to assess exercise endurance and ambulatory function over a short distance, respectively. The 6MWT performance is predictive of PAD severity and disease outcomes, but it is not feasible in many clinical settings because it requires a long walkway to serve as the test route and it lengthens clinic visits. As an alternative, the 4-meter walk test is convenient, inexpensive and repeatable, but it is not known if it accurately predicts endurance performance in the long-distance 6MWT.
Objective
To develop a statistical model to predict 6MWT gait speed given 4-meter walk test results and clinical characteristics among patients with PAD.
Methods
6MWT gait speed measures were derived from 183 patients with symptomatic PAD who were evaluated at the University of Oklahoma Health Sciences Center (2004–2012). The testing procedures and research personnel remained constant throughout the duration of the study. Independent variables included demographic and clinical information, and 4-meter walk test gait speed. Five-fold cross validation and manual backward selection were used for model selection. Adjusted-R2 and corrected Akaike information criterion were applied to quantify the predictive performance of the regression models.
Results
A total of 183 people (mean age 65 ± standard deviation 10 years, 54% male) with moderate PAD severity (ankle/brachial index: 0.72±0.24) performed the walking tests. On average, participants covered 335 meters (m) (standard deviation=97 m) distance in the 6MWT. The 4-meter walk gait speed, ankle/brachial index (ABI) and dyspnea were independent predictors of 6MWT speed in the multivariate model(adjusted-R2 = 0.55). The model resulted in 95% prediction interval widths of 30 m for mean and 260 m for individual predicted 6MWT distance measures.
Conclusions
Slower 4-meter walking speed, lower ABI and presence of dyspnea all predict slower 6MWT gait speed, which corresponds to shorter 6MWT distance. Prediction of group means is reasonably precise; however, prediction of individual patient 6MWT performance is imprecise relative to between-group differences that are clinically important.
Keywords: Claudication, exercise, gait speed, walking, 4-meter walk test
INTRODUCTION
Peripheral artery disease (PAD) is a highly prevalent medical condition that affects more than 202 million adults worldwide.1 Approximately 20% of people over 70 years of age and 50% of people over 85 years of age suffer from this disease. With a growing aging population, the prevalence of PAD is likely to increase even further.2
PAD impairs walking/exercise ability, as well as life quality. In clinical settings, the 6-minute walk test (6MWT) is a common and direct way to measure exercise capacity. Shorter 6MWT distance is associated with advanced age, chronic obstructive pulmonary disease (COPD), cardiovascular disease events and neuromuscular disease.3–5 For patients with PAD, the 6MWT distance is a reliable measure, with an intraclass correlation coefficient (ICC) of 0.94.6 Poorer 6MWT performance is associated with worse clinical outcomes, such as impaired vascular reactivity, higher risk of ischemic heart disease events and lower level of physical activity among patients with PAD.6, 7, 9–13 The 6MWT is also used to evaluate the improvement in ambulation among individuals with PAD who participate in exercise-based intervention programs.14, 15 In addition, it has received a Class IIb Recommendation to provide an objective assessment of the functional limitation of claudication and response therapy.8 However, the 6MWT is not feasible in many clinical settings because it requires a long walkway to serve as the test route, and it lengthens clinic visits.
An assessment with a relatively short distance test, the 4-meter walk test, is widely used to measure gait speed.16 Furthermore, gait speed is clinically relevant because it is associated with subsequent morbidity, such as increased risk of disability, hospitalization, and long-term care placement,17, 18 and it is a predictor of all-cause mortality.19 Gait speed is typically the primary outcome measure from this test, while stride length and cadence are additional measures. Slower 4-meter walk test gait speed is associated with worse PAD severity,13, 20–23 and stride length and cadence are also lower in participants with PAD compared with non-PAD controls.23 The 4-meter walk test holds advantages over conventional exercise tests in that it does not require large space, special equipment, nor a long visit time.
Given that the 4-meter walk test is reliable, feasible, and less cumbersome to perform than the 6MWT, the current study aimed to develop a statistical model to predict 6MWT performance using 4-meter walk gait parameters and patient characteristics. Performing a 4-meter walk test to predict 6MWT performance can efficiently give clinicians both a direct measurement of ambulation and an estimate of patients’ walking endurance during more prolonged exercise.
METHODS
Participants
The current study is nested in a larger research program, which investigated the impact of home- and clinic-based exercise programs on PAD.14, 24 Baseline data from the exercise program were utilized in the current project. Participants were recruited from vascular and primary care clinics from the University of Oklahoma Health Sciences Center (OUHSC), and the Oklahoma City Veterans Affairs Medical Center. The Institutional Review Board at the OUHSC approved the design and the procedures of the study. Written informed consent was obtained from each individual prior to initial participation.
Medical Examination
Patients were evaluated at the Exercise Physiology Laboratory at the OUHSC. Patients arrived in the morning having fasted but were permitted to take their usual medications. At the beginning of the visit, participants were evaluated with a medical history and physical examination in which demographic information, height, weight, cardiovascular risk factors, comorbid conditions, claudication history, ABI, blood samples, and a list of current medications were obtained.
Inclusion and Exclusion Criteria
Patients with symptomatic PAD were included in this study if they met the following criteria:25 (a) a history of ambulatory leg pain, (b) ambulatory leg pain confirmed by treadmill exercise, and (c) an ABI ≤ 0.9 at rest or ≤ 0.73 after exercise.26, 27 Patients were excluded for the following conditions: (a) absence of PAD (ABI > 0.90 at rest and ABI > 0.73 after exercise), (b) non-compressible vessels (ABI ≥ 1.40), (c) asymptomatic PAD, (d) use of medications indicated for the treatment of claudication (cilostazol or pentoxifylline) initiated within three months prior to investigation, (e) exercise limited by other diseases or conditions, (f) active cancer, (g) stage 5 chronic kidney disease, (h) abnormal liver function, or (i) failure to complete the 6MWT or the 4-meter walk test. A total 183 patients met the eligibility criteria and were included in the analyses.
Primary Measures
To model the association between the 6MWT and 4-meter walk test, we use the average gait speed in the 6MWT as the dependent variable and gait speed in 4-meter walk test as the primary independent variable. The 6MWT gait speed is linearly associated with the 6MWT distance and it represents the 6MWT performance.
6-Minute Walk Test
The 6MWT was administered based on a published protocol6 by trained exercise technicians. Participants were instructed to cover as much distance as possible and walk up and down a 100-foot hallway for up to 6 minutes. Participants were instructed to walk for the full 6 minutes of the test, but were allowed to take breaks if necessary. Patients were allowed to use an assistive device during both of the walking test if they so desired. The technician stood in the middle of the course and periodically encouraged the participant during the walking test. The total distance walked in the test was recorded, and the 6MWT gait speed was then calculated by
| (1) |
4-Meter Walk Test
The protocol of the 4-meter walk test was implemented as previously published.22, 28 Patients stood 1–2 feet behind the starting line and were told to walk at their usual speed. The timing started when the first foot crossed the start line and ended when one foot crossed the end line that indicated the 4-meter distance. The total time was recorded. In our study, steps were also recorded as the number of foot falls within the 4-meter course. Then three parameters, gait speed, cadence, and stride length were calculated. Stride length was defined by the distance the patient covered per stride (gait cycle), where one stride consists of one left step and one right step. Cadence was defined by the number of strides walked per unit time. The equations below illustrated the calculation of the 4-meter walk gait speed (equation 2) and the association between gait speed, cadence and stride length (equation 3).
| (2) |
| (3) |
To evaluate the reliability of the 4-meter walk test, 24 participants were asked to repeat the test. The test-retest reliability was high for gait speed (ICC = 0.91; 95%CI: 0.80, 0.96), and stride length (ICC = 0.91; 95%CI: 0.80, 0.96), but was moderate for cadence (ICC = 0.66; 95%CI: 0.35, 0.84).
Statistical Analysis
All statistical analyses were conducted with SAS software (SAS System for Windows, version 9.4, SAS Institute Inc., Cary, NC, USA). Simple linear regression was used to perform univariate analysis and identify factors associated with the outcome measure, 6MWT gait speed. Covariates included in the multivariate model were selected from univariate analyses at a 0.1 alpha level. Confounding was addressed by retaining in the model any covariate that resulted in at least a 10% change in the coefficient for the 4-meter walk test upon deletion from the model. The variance inflation factor was used to assess collinearity with a threshold of 10 indicating the presence of collinearity.29 Five-fold cross-validation was used to select the model with the best fit. Manual backward selection was also performed. Two-way interactions between 4-meter gait speed and other covariates were considered. The assumptions of the linear regression model were checked by residual diagnostics. Predictive ability of the model was quantified using an adjusted-R2 and corrected Akaike information criterion (AICc). When the sample size (n) is relatively small compared with the number of parameters (p) in the global model (n/p < 40), AICc is preferable over Akaike information criterion (AIC).30 AICc was manually calculated using the formula below:
| (4) |
where n is the sample size and the p is the number of parameters in the model.30, 31
Two modeling approaches were used in this study. In the first approach, gait speed in the 4-meter walk test was treated as the primary independent variable. In the second approach, cadence, stride length and the interaction term (cadence × stride length), which equals the gait speed, took the place of the 4-meter gait speed in the first modeling approach. The second approach was based on the hypothesis that the variability in cadence and stride length may individually contribute a significant impact on the decline in walking ability among individuals with PAD. To assess the estimation precision, the final model was used to predict gait speed and distance using a range of independent variable values based on the 1st and 3rd quartiles of 4-meter walk gait speed and ABI, as well as the absence/presence of dyspnea for 8 hypothetical observations. The point estimate, 95% confidence limits of the means (CLM) and 95% individual prediction intervals (PI) of 6MWT gait speed and distance were computed. The predicted 6MWT distance was derived by formula (equation 1), which was the product of the 6MWT gait speed (m/sec) and 360 (secs).
RESULTS
Baseline Clinical Characteristics
Table 1 summarizes the demographic and clinical characteristics of the study participants. The average age was 65 years (standard deviation [SD]=10) with a range of 40 to 85 years, and 54% of them were male. Almost half (43%) of the people were obese. Study participants had moderately severe PAD with a mean ABI of 0.72 (SD=0.24). Approximately 95% of people reported that they experienced intermittent claudication(IC) in daily life. The mean 4-meter gait speed and 6MWT gait speed were both close to 1 meter/second. On average, participants covered 335 m (SD=97 m) in the 6MWT.
Table 1.
Summary of demographic and clinical characteristics (N=183).
| Variable | ||
|---|---|---|
| Mean | SD | |
|
|
||
| Age (years) | 65 | 10 |
| Height (cm)* | 169.30 | 9.00 |
| Weight (kg) | 84.40 | 19.30 |
| BMI (kg/m2)* | 29.40 | 6.50 |
| ABI | 0.72 | 0.24 |
| 4-Meter Gait Speed (m/sec) | 1.00 | 0.30 |
| 4-Meter Cadence (strides/sec)** | 0.90 | 0.10 |
| 4-Meter Stride Length (m/stride)** | 1.20 | 0.30 |
| 6MWT Total Distance (m) | 335 | 97 |
| 6MWT Total Gait Speed (m/sec) | 0.90 | 0.30 |
|
| ||
| N | % | |
|
|
||
| Sex (Male) | 100 | 54 |
| Race (Caucasian) | 114 | 62 |
| Ever Smoking* | 165 | 91 |
| Obesity (BMI >30 kg/m2) | 79 | 43 |
| Coronary Artery Disease | 64 | 35 |
| Cerebral Vascular Disease | 31 | 17 |
| Kidney Disease | 42 | 23 |
| Dyslipidemia | 161 | 88 |
| COPD | 47 | 26 |
| Dyspnea | 107 | 58 |
| Diabetes | 62 | 34 |
| Cancer | 26 | 14 |
| Arthritis | 107 | 58 |
| Hypertension | 146 | 80 |
| Congestive Heart Failure | 16 | 9 |
| IC | 173 | 95 |
| Both Legs with IC | 117 | 64 |
number missing n=1
number missing n=2
SD = standard deviation,
ABI = ankle/brachial index,
BMI = body mass index,
6MWT = 6-minute walk test,
COPD = chronic obstructive pulmonary disease,
IC = intermittent claudication.
Univariate Analysis
The univariate analyses were based on non-missing observations for each variable. The results of univariate analyses are provided in Table 2. At the 0.05 alpha level, independent variables that were associated with 6MWT gait speed were 4-meter walk gait speed, cadence and stride length, height, ABI, sex, number of legs with IC, dyspnea, diabetes and chronic kidney disease. Other factors identified at the 0.1 alpha level, for inclusion in the multivariate model, included BMI, obesity, COPD and cancer. As shown in Figure 1, the spline curve demonstrates a linear association between 4-meter walk gait speed and 6MWT gait speed.
Table 2.
Summary of univariate analysis. Estimates are reported as the linear regression coefficient for each variable in predicting the outcome measure 6MWT total gait speed, the 95% confidence interval (CI), and the p-value.
| Variable | Coefficient | 95% CI | P-value |
|---|---|---|---|
| Age (years) | −0.003 | (−0.007,0.0008) | 0.12 |
| Height (cm) | 0.009 | (0.005,0.13) | <0.0001 |
| Weight (kg) | −0.00011 | (−0.0022,0.002) | 0.91 |
| Obesity (BMI≥30 kg/m2 vs. <30 kg/m2) | −0.077 | (−0.012,0.0005) | 0.056 |
| BMI (kg/m2) | −0.0056 | (−0.01,0.0005) | 0.07 |
| ABI | 0.3 | (0.14,0.5) | 0.0003 |
| Sex (Male vs. Female) | 0.14 | (0.07,0.22) | 0.0002 |
| Race (Caucasian vs. Non-Caucasian) | 0.032 | (−0.049,0.11) | 0.44 |
| Smoking (Ever vs. Never) | −0.042 | (−0.18,0.094) | 0.54 |
| Number of Leg(s) with IC | −0.09 | (−0.16, −0.026) | 0.0065 |
| Co-morbid Conditions (Present vs. Absent) | |||
| IC | −0.071 | (−0.24,0.1) | 0.42 |
| Dyslipidemia | 0.068 | (−0.053,0.19) | 0.27 |
| COPD | −0.085 | (−0.17,0.004) | 0.062 |
| Dyspnea | −0.12 | (−0.2, −0.05) | 0.0019 |
| Diabetes | −0.096 | (−0.18, −0.01) | 0.022 |
| Cancer | 0.095 | (−0.02,0.21) | 0.09 |
| Arthritis | −0.049 | (−0.13,0.03) | 0.22 |
| Hypertension | −0.035 | (−0.13,0.06) | 0.48 |
| Congestive Heart Failure | 0.028 | (−0.11,0.17) | 0.69 |
| Coronary Artery Disease | −0.052 | (−0.13,0.03) | 0.21 |
| Cerebral Vascular Disease | −0.051 | (−0.15,0.05) | 0.34 |
| Chronic Kidney Disease | −0.1 | (−0.19, −0.0004) | 0.049 |
| 4-Meter Gait Speed (M/Sec) | 0.67 | (0.58,0.77) | <0.0001 |
| 4-Meter Cadence (Strides/Min) | 1.24 | (0.97,1.52) | <0.0001 |
| 4-Meter Stride Length (M/Stride) | 0.63 | (0.51,0.75) | <0.0001 |
ABI = ankle/brachial index,
BMI = body mass index,
6MWT = 6-minute walk test,
COPD = chronic obstructive pulmonary disease,
IC = intermittent claudication.
Figure 1.
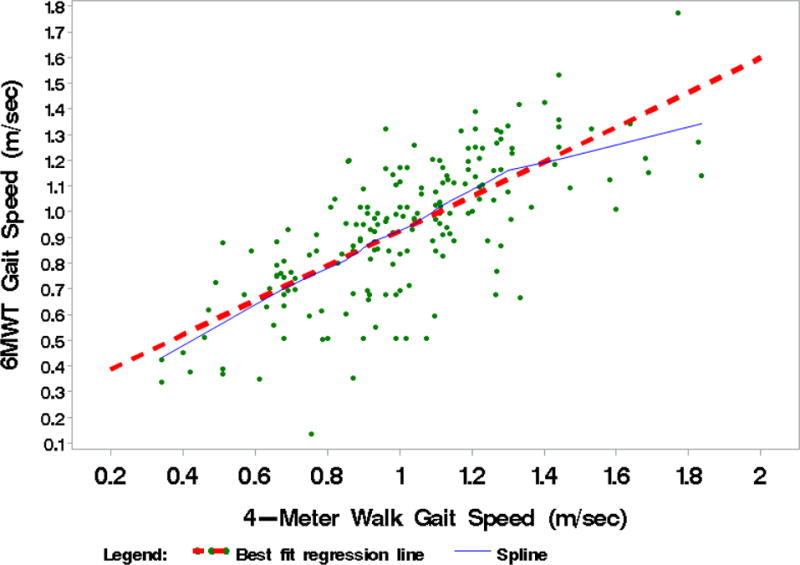
Spline curve demonstrating a linear association between 4-meter walk gait speed and 6-minute walk test (6MWT) gait speed.
Multivariate Analysis
All of the univariate variables with a P ≤ .10 identified in simple linear regression analysis were included in the multivariate analysis. Although both BMI and obesity (BMI>30 kg/m2) were evaluated in the univariate analysis, only BMI was retained in the model as a continuous measure.
Using non-missing observations, the first approach, focused on 4-meter walk gait speed, included 182 people and the second approach, focused on the components of stride length and cadence, included 180 people. In both modeling approaches, no significant interactions between 4-meter measures and other covariates were found. No significant collinearity was found in either of the full models. A parsimonious model without interaction terms was selected in each approach. To make the formal comparison between the models selected from each approach, the common sample with 180 observations was used to refit the model selected from the first approach. The first model had an adjusted-R2 of 0.55 and AICc of −618, and the second model had an adjusted-R2 of 0.55 and AICc of −609. Since the first model (Table 3) was more parsimonious and showed a higher predictive ability, it was then selected as the final model to predict 6MWT gait speed, and it can be expressed as:
| (5) |
Table 3.
Final estimated linear regression model. Estimates are reported as the linear regression coefficient for each term in multivariate model predicting the outcome measure 6MWT total gait speed, the 95% confidence interval (CI), and the p-value.
| Term | Coefficient | 95%CI | P-value | VIF |
|---|---|---|---|---|
| Intercept | 0.18 | (0.05,0.31) | 0.006 | |
| 4-Meter Gait Speed (m/sec) | 0.63 | (0.54,0.73) | <.0001 | 1.04 |
| ABI | 0.2 | (0.08,0.31) | 0.0007 | 1.01 |
| Dyspnea | −0.06 | (−0.11, −0.001) | 0.047 | 1.03 |
6MWT = 6-minute walk test, ABI = ankle/brachial index, VIF = Variance inflation factor
The covariates included in the final model were 4-meter gait speed, ABI and dyspnea. This model explained 55% variance of 6MWT gait speed. Slower 4-meter walking speed, lower ABI and presence of dyspnea predicted slower 6MWT gait speed, which corresponded to shorter 6MWT distance.
Prediction of 6MWT Performance for Hypothetical New Observations
To better assess the precision in predicting 6MWT performance, the final model was applied to a set of new hypothetical observations. We constructed 8 hypothetical new observations, which were derived from the combination of the 1st and the 3rd quartiles of continuous variables (4-meter gait speed and ABI) of the study sample, and absence/presence of dyspnea. Table 4 lists the predicted 6MWT gait speed and distance for each hypothetical observation. The interval width of 95% CLM was approximately 30m and the interval width of 95% PI was approximately 260m for 6MWT distance.
Table 4.
Prediction of 6MWT gait speed and distance for presence and absence of dyspnea and first and third quartiles of ABI and 4-meter gait speed for 8 hypothetical observations.
| Independent variables | Predicted values | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| New Obs | ABI | Dyspnea | 4-Meter GS (m/sec) | Predicted 6MWT GS (m/sec) | 95%CLM of 6MWT GS (m/sec) | 95%PI of 6MWT GS (m/sec) | Predicted 6MWT Distance (m) | 95%CLM of 6MWT Distance (m) | 95%PI of 6MWT Distance (m) |
| 1 | 0.54 | No | 0.84 | 0.82 | (0.77,0.87) | (0.46,1.18) | 296 | (278,314) | (166,426) |
| 2 | 0.88 | No | 0.84 | 0.77 | (0.73,0.81) | (0.41,1.13) | 276 | (262,291) | (147,406) |
| 3 | 0.54 | Yes | 0.84 | 1.04 | (1,1.09) | (0.68,1.4) | 376 | (359,393) | (246,506) |
| 4 | 0.88 | Yes | 0.84 | 0.99 | (0.94,1.04) | (0.63,1.35) | 356 | (340,373) | (227,486) |
| 5 | 0.54 | No | 1.19 | 0.82 | (0.77,0.87) | (0.46,1.18) | 296 | (278,314) | (166,426) |
| 6 | 0.88 | No | 1.19 | 0.77 | (0.73,0.81) | (0.41,1.13) | 276 | (262,291) | (147,406) |
| 7 | 0.54 | Yes | 1.19 | 1.04 | (1,1.09) | (0.68,1.4) | 376 | (359,393) | (246,506) |
| 8 | 0.88 | Yes | 1.19 | 0.99 | (0.94,1.04) | (0.63,1.35) | 356 | (340,373) | (227,486) |
95%CLM = 95% confidence limits of the mean, 95%PI = 95% confidence interval of the individual prediction, GS = gait speed, ABI = ankle/brachial index, 6MWT = 6-minute walk test, Obs = observations.
DISCUSSION
The 6MWT distance is a reliable measure to estimate walking endurance among patients with PAD. This is the first study to propose modeling the 6MWT performance (6MWT gait speed) by the 4-meter walk test parameters and clinical characteristics among patients with PAD. The independent predictors of 6MWT performance were 4-meter gait speed, ABI and dyspnea history.
Independent Predictors of 6MWT Performance
The current model revealed that 4-meter walk gait speed, ABI, and dyspnea were independent predictors of 6MWT performance for patients with PAD. These results support a previous study from our laboratory,6 and extend these findings by quantifying the association between the 6MWT performance and independent variables in a multivariate model. After adjusting for other factors in the model, for every 0.1 m/sec increase in the 4-meter walk gait speed, 6MWT gait speed is expected to increase 0.063 m/sec (95% CI: 0.055, 0.073 m/sec), which corresponds to 22.7 m (95% CI: 19.8, 26.3 m) in 6MWT distance. For every 0.1 unit increase in ABI, 6MWT gait speed is expected to increase 0.02 m/sec (95% CI: 0.008, 0.031 m/sec), which corresponds to 7.2 m (95% CI: 2.9, 11.2 m) in 6MWT distance. Having dyspnea in the final model indicates that respiratory function is another factor determining performance in long-distance walking for the PAD population.
Modeling the individual components, 4-meter cadence and stride length, did not improve the model predictive performance. Although age is considered an important factor associated with 6MWT performance,32 it was not significant in our model. For the PAD population, the association between age and 6MWT performance is not consistent, as age is negatively associated with 6MWT distance in one previous study,10 but not in another.6 This discrepancy might be due to the latter study only enrolling symptomatic patients, whereas the former study primarily enrolled asymptomatic patients.
To the best of our knowledge, no studies have reported a model to predict 6MWT performance among patients with PAD. In previous published models targeting healthy populations, age and anthropometric measurements were commonly reported as independent predictors. However, non-significant associations between anthropometrics and 6MWT performance were found in our multivariate analysis. Previous studies also reported that among patients with PAD, weight and BMI were not associated with 6MWT distance.6, 33 It is possible that among patients with PAD, body composition may be less important for walking performance than in those without PAD, primarily because PAD patients are limited by their poor leg perfusion. Further study on what is the role of anthropometrics on walking capacity of PAD patients may be established to understand this phenomenon. The approach using 4-meter gait speed to predict 6MWT performance was supported by previous publications, which showed physical function measures (balance test, 4-meter walk gait speed and grip strength) were strongly associated with 6MWT distance in healthy elderly people.34, 35 Although log-linear models and quadratic models outperformed multiple linear regression in some previous studies, when using age and anthropometrics as the predictors,36, 37 these techniques were not advantageous in our study due to the obvious linear relationship between 4-meter gait speed and 6MWT gait speed (Figure 1).
Model Precision of Predicting 6MWT Performance
When applying the final model to the new hypothetical observations, the width of 95% CLM of 6MWT distance was approximately 30 m. From a research perspective, prediction of the mean value would be of interest, for example, when identifying factors at a population level that are associated with better endurance among patients with PAD. Compared with the average distance (335 m), the model had acceptable precision in predicting the mean of our sample. However, our prediction interval of hypothetical observations for a randomly chosen patient had a width of approximately 260m. It is important to note that the 95% PI not only considers the uncertainty in estimating the mean but also accounts for the deviation of the dependent variable from the mean.38 To better interpret this broad prediction interval, a previous study found that the mean difference in 6MWT distance in non-PAD controls compared to patients with moderate and severe PAD was 101m and 179 m, respectively, after adjustment for age.39 The 260 m width of the 95% PI in the current study exceeds both of these estimated between-group differences in 6MWT distance. While, the proposed regression model does not have sufficient precision to predict the individual 6MWT performance relative to these reported differences between PAD and non-PAD groups, it is important to note that the regression model did account for 55% of the variation in 6MWT performance. Based on the raw 6MWT measures, a 95% central range width is 380m compared to the tighter interval width of 260m based on the predicted model. Precision of the predicted 6MWT measures is improved using our model, but prediction remains a challenge given the high amount of variation in the raw measures.
Limitations
Several limitations exist in this study. First, the sample size was relatively small compared to the total of twelve independent variables in the global model. Therefore, the sample size is not sufficient to identify potential interactions between 4-meter parameters and other covariates, nor can the model be sufficiently validated. Future study with an independent group of patients is needed to validate the model. The second limitation relates to potential selection bias. It is possible that the patients who volunteered for the study are healthier and more motivated than patients with claudication who did not volunteer. Third, the cross-sectional study design cannot account for the cumulative effects of having PAD and comorbid conditions on the outcome measures. In future studies, using a longitudinal cohort design with prospective follow-up of patients who initially did not have extensive disease may address the concerns regarding selection bias and would also potentially enhance model prediction. In addition, we did not quantify the usage of medicine, such as NSAIDS, which may have potential effect on walking performance. Finally, our results are generalizable to symptomatic patients with PAD, but may not be generalizable to a broader clinical population of patients with PAD who are asymptomatic.
Conclusion
Clinicians can perform a 4-meter walk test to obtain a direct and meaningful measurement of ambulation, and utilize the statistical model to estimate walking endurance during more prolonged exercise in an efficient manner. Slower 4-meter walking speed, lower ABI and presence of dyspnea all predict slower 6MWT gait speed, which corresponds to shorter 6MWT distance. Prediction of group means is reasonably precise; however, prediction of individual patient 6MWT performance is relatively imprecise compared to between-group differences. There is potential room for improvement in the precision of the model prediction of 6MWT gait speed.
Acknowledgments
Supported by grants from the National Institutes of Health (R01-AG-24296, M01-RR-14467, and 1UG54GM104938).
References
- 1.Fowkes FG, Rudan D, Rudan I, Aboyans V, Denenberg JO, McDermott MM, et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet. 2013;382(9901):1329–40. doi: 10.1016/S0140-6736(13)61249-0. [DOI] [PubMed] [Google Scholar]
- 2.Sigvant B, Lundin F, Wahlberg E. The Risk of Disease Progression in Peripheral Arterial Disease is Higher than Expected: A Meta-Analysis of Mortality and Disease Progression in Peripheral Arterial Disease. Eur J Vasc Endovasc Surg. 2016 doi: 10.1016/j.ejvs.2015.10.022. [DOI] [PubMed] [Google Scholar]
- 3.Anderson KL. The effect of chronic obstructive pulmonary disease on quality of life. Res Nurs Health. 1995;18(6):547–56. doi: 10.1002/nur.4770180610. [DOI] [PubMed] [Google Scholar]
- 4.Rostagno C, Olivo G, Comeglio M, Boddi V, Banchelli M, Galanti G, et al. Prognostic value of 6-minute walk corridor test in patients with mild to moderate heart failure: comparison with other methods of functional evaluation. Eur J Heart Fail. 2003;5(3):247–52. doi: 10.1016/s1388-9842(02)00244-1. [DOI] [PubMed] [Google Scholar]
- 5.Hirsch CH, Fried LP, Harris T, Fitzpatrick A, Enright P, Schulz R. Correlates of performance-based measures of muscle function in the elderly: the Cardiovascular Health Study. J Gerontol A Biol Sci Med Sci. 1997;52(4):M192–200. doi: 10.1093/gerona/52a.4.m192. [DOI] [PubMed] [Google Scholar]
- 6.Montgomery PS, Gardner AW. The clinical utility of a six-minute walk test in peripheral arterial occlusive disease patients. J Am Geriatr Soc. 1998;46(6):706–11. doi: 10.1111/j.1532-5415.1998.tb03804.x. [DOI] [PubMed] [Google Scholar]
- 7.McDermott MM, Liu K, Greenland P, Guralnik JM, Criqui MH, Chan C, et al. Functional decline in peripheral arterial disease: associations with the ankle brachial index and leg symptoms. JAMA. 2004;292(4):453–61. doi: 10.1001/jama.292.4.453. [DOI] [PubMed] [Google Scholar]
- 8.Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, et al. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic) Circulation. 2006;113(11):e463–e654. doi: 10.1161/CIRCULATIONAHA.106.174526. [DOI] [PubMed] [Google Scholar]
- 9.McDermott MM, Hoff F, Ferrucci L, Pearce WH, Guralnik JM, Tian L, et al. Lower extremity ischemia, calf skeletal muscle characteristics, and functional impairment in peripheral arterial disease. J Am Geriatr Soc. 2007;55(3):400–6. doi: 10.1111/j.1532-5415.2007.01092.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McDermott MM, Greenland P, Tian L, Kibbe MR, Green D, Zhao L, et al. Association of 6-Minute Walk Performance and Physical Activity With Incident Ischemic Heart Disease Events and Stroke in Peripheral Artery Disease. J Am Heart Assoc. 2015;4(7) doi: 10.1161/JAHA.115.001846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Silva Rde C, Wolosker N, Yugar-Toledo JC, Consolim-Colombo FM. Vascular Reactivity is Impaired and Associated With Walking Ability in Patients With Intermittent Claudication. Angiology. 2015;66(7):680–6. doi: 10.1177/0003319714545486. [DOI] [PubMed] [Google Scholar]
- 12.Nardi Gomes TJ, Martins de Albuquerque I, de Moraes Costa P, Cardoso DM, de Moraes Costa G, da Costa Vieira JL. Association between the ankle-brachial index, intermittent claudication, and physical activity level: what is the influence on the functional capacity of patients with or at high risk of cardiovascular disease? Int J Gen Med. 2015;8:55–62. doi: 10.2147/IJGM.S76446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gardner AW, Parker DE, Montgomery PS, Sosnowska D, Casanegra AI, Ungvari Z, et al. Influence of Diabetes on Ambulation and Inflammation in Men and Women with Symptomatic Peripheral Artery Disease. J Clin Transl Endocrinol. 2015;2(4):137–43. doi: 10.1016/j.jcte.2015.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gardner AW, Parker DE, Montgomery PS, Blevins SM. Step-monitored home exercise improves ambulation, vascular function, and inflammation in symptomatic patients with peripheral artery disease: a randomized controlled trial. J Am Heart Assoc. 2014;3(5):e001107. doi: 10.1161/JAHA.114.001107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McDermott MM, Guralnik JM, Criqui MH, Ferrucci L, Zhao L, Liu K, et al. Home-based walking exercise in peripheral artery disease: 12-month follow-up of the GOALS randomized trial. J Am Heart Assoc. 2014;3(3):e000711. doi: 10.1161/JAHA.113.000711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rydwik E, Bergland A, Forsen L, Frandin K. Investigation into the reliability and validity of the measurement of elderly people’s clinical walking speed: a systematic review. Physiother Theory Pract. 2012;28(3):238–56. doi: 10.3109/09593985.2011.601804. [DOI] [PubMed] [Google Scholar]
- 17.Vermeulen J, Neyens JC, van Rossum E, Spreeuwenberg MD, de Witte LP. Predicting ADL disability in community-dwelling elderly people using physical frailty indicators: a systematic review. BMC Geriatr. 2011;11:33. doi: 10.1186/1471-2318-11-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cawthon PM, Fox KM, Gandra SR, Delmonico MJ, Chiou CF, Anthony MS, et al. Do muscle mass, muscle density, strength, and physical function similarly influence risk of hospitalization in older adults? Journal of the American Geriatrics Society. 2009;57(8):1411–9. doi: 10.1111/j.1532-5415.2009.02366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, et al. Gait speed and survival in older adults. Jama. 2011;305(1):50–8. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McDermott MM, Liu K, Ferrucci L, Tian L, Guralnik J, Kopp P, et al. Vitamin D status, functional decline, and mortality in peripheral artery disease. Vasc Med. 2014;19(1):18–26. doi: 10.1177/1358863X13518364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McDermott MM, Ferrucci L, Guralnik JM, Dyer AR, Liu K, Pearce WH, et al. The ankle-brachial index is associated with the magnitude of impaired walking endurance among men and women with peripheral arterial disease. Vasc Med. 2010;15(4):251–7. doi: 10.1177/1358863X10365181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nickel KJ, Acree LS, Montgomery PS, Gardner AW. Association between lower-extremity function and arterial compliance in older adults. Angiology. 2008;59(2):203–8. doi: 10.1177/0003319707306143. [DOI] [PubMed] [Google Scholar]
- 23.Gardner AW, Forrester L, Smith GV. Altered gait profile in subjects with peripheral arterial disease. Vasc Med. 2001;6(1):31–4. [PubMed] [Google Scholar]
- 24.Gardner AW, Montgomery PS, Scott KJ, Afaq A, Blevins SM. Patterns of ambulatory activity in subjects with and without intermittent claudication. J Vasc Surg. 2007;46(6):1208–14. doi: 10.1016/j.jvs.2007.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gardner AW, Parker DE, Montgomery PS. Sex-specific predictors of improved walking with step-monitored, home-based exercise in peripheral artery disease. Vasc Med. 2015;20(5):424–31. doi: 10.1177/1358863X15596237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) Eur J Vasc Endovasc Surg. 2007;33(Suppl 1):S1–75. doi: 10.1016/j.ejvs.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 27.Gardner AW, Skinner JS, Cantwell BW, Smith LK. Progressive vs single-stage treadmill tests for evaluation of claudication. Med Sci Sports Exerc. 1991;23(4):402–8. [PubMed] [Google Scholar]
- 28.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 29.Chatterjee S, Hadi AS. Regression analysis by example. John Wiley & Sons; 2015. [Google Scholar]
- 30.Burnham KP, Anderson DR. Model selection and multimodel inference: a practical information-theoretic approach. Springer Science & Business Media; 2003. [Google Scholar]
- 31.Institute Inc SAS. SAS/STAT® 9.22 User’s Guide. Cary NC: SAS insitute Inc; 2010. [Google Scholar]
- 32.Enright PL, Sherrill DL. Reference equations for the six-minute walk in healthy adults. Am J Respir Crit Care Med. 1998;158(5 Pt 1):1384–7. doi: 10.1164/ajrccm.158.5.9710086. [DOI] [PubMed] [Google Scholar]
- 33.Sun KS, Lin MS, Chen YJ, Chen YY, Chen SC, Chen W. Is asymptomatic peripheral arterial disease associated with walking endurance in patients with COPD? Int J Chron Obstruct Pulmon Dis. 2015;10:1487–92. doi: 10.2147/COPD.S85430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Caballer VB, Lison JF, Rosado-Calatayud P, Amer-Cuenca JJ, Segura-Orti E. Factors associated with the 6-minute walk test in nursing home residents and community-dwelling older adults. J Phys Ther Sci. 2015;27(11):3571–8. doi: 10.1589/jpts.27.3571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harada ND, Chiu V, Stewart AL. Mobility-related function in older adults: assessment with a 6-minute walk test. Arch Phys Med Rehabil. 1999;80(7):837–41. doi: 10.1016/s0003-9993(99)90236-8. [DOI] [PubMed] [Google Scholar]
- 36.Duncan MJ, Mota J, Carvalho J, Nevill AM. An Evaluation of Prediction Equations for the 6 Minute Walk Test in Healthy European Adults Aged 50-85 Years. PLoS One. 2015;10(9):e0139629. doi: 10.1371/journal.pone.0139629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Soaresa MR, Pereira CA. Six-minute walk test: reference values for healthy adults in Brazil. J Bras Pneumol. 2011;37(5):576–83. doi: 10.1590/s1806-37132011000500003. [DOI] [PubMed] [Google Scholar]
- 38.Altman DG, Gardner MJ. Statistics in Medicine: Calculating confidence intervals for regression and correlation. British medical journal (Clinical research ed) 1988;296(6631):1238. doi: 10.1136/bmj.296.6631.1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McDermott MM, Liu K, Guralnik JM, Mehta S, Criqui MH, Martin GJ, et al. The ankle brachial index independently predicts walking velocity and walking endurance in peripheral arterial disease. J Am Geriatr Soc. 1998;46(11):1355–62. doi: 10.1111/j.1532-5415.1998.tb06001.x. [DOI] [PubMed] [Google Scholar]


