Abstract
Purpose
High rates of mechanical failure have been reported in type III acetabular defects. Recently porous trabecular metal augments have been introduced with, excellent biomechanical characteristics and biocompatibility, allowing early stability and greater bone ingrowth. The aim of the study was to assess the short term clinical and radiological outcome of the trabecular metal augments.
Materials and Methods
We performed, 22 revision total hip arthroplasties (THA) and 6 primary THA (total 28) using trabecular metal augments to reconstruct acetabular defect between 2011 to 2015. Among 28 patients, 18 were males, 10 females. Mean age of patients was 61.21 years. Paprosky classification for acetabular bone defects was used. Eighteen cases were classified as grade 3 A and 10 cases as grade 3B. Hip center was calculated in each case preoperatively and compared postoperatively to check whether it has been brought down. Clinical outcome assessed using Harris hip score (HHS) and radiological outcomes as osteolysis in acetabular zones and osseointegration, according to Moore's criteria.
Results
HHS improved from 58.00 to 86.20. Centre of rotation of hip joint corrected from 38.90 mm preoperatively to 23.85 mm postoperatively above the interteardrop line. Among 28 patients, 18 patients had three or more signs of osseointegration (Moore's criteria), during final follow up and 10 had one/two signs. No radiolucency, osteolysis, or loosening found during follow up radiographic examination.
Conclusion
Our study showed that trabecular metal augments were highly satisfactory in short term. However, long term study is required for better evaluation.
Keywords: Metal augment, Acetabular, Bone defect, Total hip arthroplasty
INTRODUCTION
The number of total hip arthroplasties (THA) performed each year is increasing and similar trend has also been observed for revision hip procedures1). Reconstructing acetabular defects in revision hip arthroplasty can be challenging. Small, contained defects can be successfully reconstructed with porous-coated hemispheric cups with or without supplementary allografts2). Paprosky type III acetabular bone defects can be reconstructed with various methods depending on size and location of the defect. Different implant designs and sizes are available for THA acetabular revisions3), which include mainly reinforcement devices (roof-reinforcement rings and anti-protrusio cages), custom-made triflanged acetabular components, jumbo cups and tantalum metal systems. Each designs and methods has various success rates as well various complication rates4,5). Trabecular metal can be used in acetabular cup alone or in conjunction with augments, depending upon type of defect of acetabulum. Trabecular materials facilitate rapid bony ingrowth because of high porosity of these products. These porous trabecular titanium comes in various shapes and sizes which offer to fill variable defect types and provide structural support in the acetabulum. Trabecular titanium augments along with uncemented porous coated cups have given the better results in high grades of acetabular bone loss as compared to uncemented hemispherical cup only6,7).
The purpose of this study was to evaluate (1) the role of trabecular metal augments in early outcome of large acetabular defect reconstruction; (2) the functional outcome of these patients; (3) the restoration of the center of rotation of the hip joint after reconstruction; and (4) the osseointegration of the components as assessed on plain radiographs.
MATERIALS AND METHODS
Twenty-eight hips (in 28 patients) in which trabecular metal augments in conjunction with standard acetabular components operated from November 2011 to November 2015 were retrospectively reviewed. All surgeries were performed by single senior orthopaedic surgeon between this time periods. Out of 28 patients, there were 18 male (64.3%) and 10 female (35.7%) patients. The mean age of all patients was 61.21 years (range, 46 to 79 years). There were 18 cases of right hip and 10 cases of left hip involvement. There was no case with bilateral trabecular metal augments. This study was approved by the institutional review board of Korea University Guro Hospital (IRB No. MD 16049).
Out of 28 hips, 22 hips were revision arthroplasty cases and six hips were primary procedures. Major reasons of acetabular defect in primary cases were dysplasia, infection and post traumatic post-surgical arthritis. Among the 22 revision procedures, infection of previously inserted prosthesis was the most common cause (12 hips out of 22 revision hips), followed by aseptic loosening and osteolysis of acetabular bone stock. In this retrospective study, mean follow up was 22 months (range, 12 to 42 months). Radiographic evaluation was performed by a single reviewer (CD). Digitalized images of all radiographs were acquired using a picture archiving and communication system (PACS; Infinite, Seoul, Korea). The acetabular components were considered loose, if they had circumferential radiolucencies, more than 3-mm migration, or more than 5° change in inclination8). Osteolytic lesions more than 5 mm in the largest dimension were also reported. We had complete radiological follow up as well as complete clinical outcome questionnaire follow up of all 28 patients. There was no loss to follow up as well no death of any patients.
1. Preoperative Planning
As part of preoperative evaluation, we did anteroposterior view, cross table lateral view, frog lateral view and Judet's view radiographs of pelvis and computed tomography (CT) scan of the pelvis for better understanding of acetabular defect. We classify the acetabular defect in all patients according to the Paprosky classification7), based on the preoperative anteroposterior radiograph of pelvis, Judet's view of pelvis, and CT scan of pelvis with three-dimmensional reconstruction. The preoperative findings were confirmed intraoperartively in each case. We also confirmed our grading intraoperatively. In our study, 18 cases were classified as grade 3A and 10 cases as grade 3B.
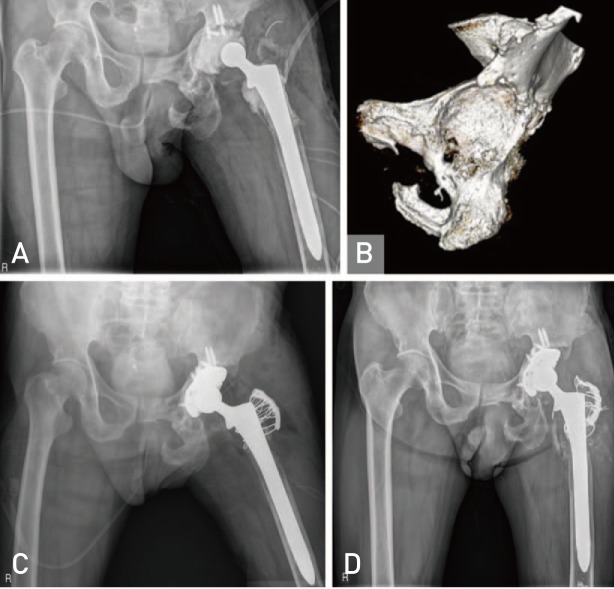
2. Operation Method
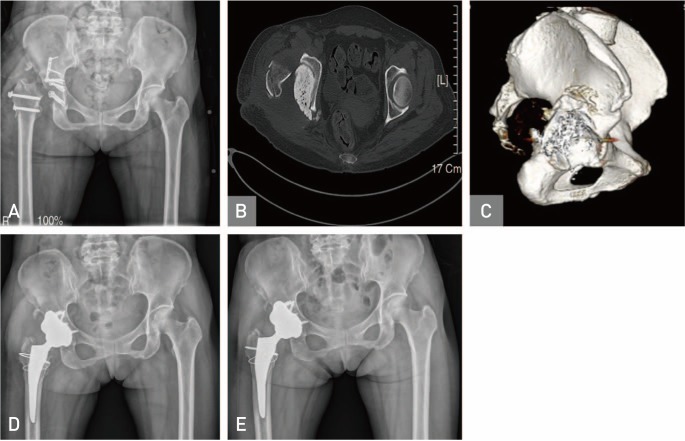
Trabecular metal augments (Zimmer Inc., Warsaw, IN, USA; Fig. 1) are very stable mechanically and restore the center of the hip, which are a more recently available option to address bone loss. The indication for the use of trabecular metal augments was preoperative determination of acetabular defects using digital X-rays and CT scans which lead to the anticipation of the use of the trabecular metal augments (Fig. 2). Also the poor stability of acetabular cup and inability to achieve desired superolateral coverage of acetabular cup intraoperatively was also a guide.
Fig. 1. Trabecular metal augment.
Fig. 2. (A) Anteroposterior radiograph of patient after debridement for infection which occurred after open reduction and internal fixation for Pipkin IV fracture dislocation. (B) Preoperative axial computed tomography (CT) scan shows large posterior bone defect of the acetabulum. (C) Preoperative three-dimensional CT scan shows large posterior bone defect of the acetabulum. (D) Immediate postoperative anteroposterior radiograph. (E) One year postoperative radiograph shows well fixed trabecular metal augment and the acetabular cup along with bony ingrowth after total hip arthroplasty.
We did templating in all cases, preoperatively. With the help of pre-operative templating, it becomes easy to forecast the possible requirement of trabecular metal augments as well as tentative amount of bone loss and hence the size of augments, preoperatively. The need for augments was predicted on the basis of templating as well as poor stability of acetabular component during the surgery. A posterior approach was used in all patients. After the complete exposure of acetabulum, hemispherical reamers were used to prepare the acetabulum. After that, the desired position for final acetabular prosthesis was determined with the trial cup. The location and the amount of remaining supportive host bone was determined with trial cup in situ. With the trial cup in the desired degree of anteversion and abduction, the trial augment was placed against the deficient host bone. Although, we can place augment in any position, we preferred to place the augment in posterior-superior position in most of cases, so that we can bring down the centre of rotation of hip joint. We contoured the acetabulum with a barrel burr to optimize the surface contact area. Then we left the trial cup in situ and the real augment implant was secured to the host bone with one or two screws. The augment was then packed with allobone graft and morsellized allobone graft was filled in the augment windows and around any peripheral residual gaps and defects in the region of augment using impaction punch and mallet. Polymethylmethacrylate cement was then placed directly onto the acetabular cup only in the areas mating with the augments. Then acetabular component was implanted using press-fit technique with a caution to prevent soft tissue interposition between prosthetic component and host bone during final implantation. Then, we placed multiple screws in acetabular cup to give additional support, initially. Then we impacted liner followed by uncemented femoral stem and femoral head. Finally, we reduced the hip joint and wound closure was done layer by layer over hemovac drain.
3. Rehabilitation after Operation
Post operatively, abduction brace was given to all patients for 6 weeks. Patients were allowed high sitting and knee range of movements along with static quadriceps and ankle pumping from the second day of operation. Non weight bearing walking with crunches was allowed for 6 weeks and partial weight bearing walking with support for another 6 weeks. Patients were allowed to start full weight bearing walking after 3 months of surgery or as tolerated under the no evidence of acetabular component migration on follow up radiologic finding. We reviewed patients clinically and radiographically at 6 weeks post operatively and then monthly up to one year and yearly, thereafter. Clinical outcome was evaluated with Harris hip score (HHS) and radiographs were evaluated for change in center of rotation of hip joint, osteolysis of acetabular dome and osseointegration of acetabular component and trabecular metal augments with host bone according to the criteria of Moore et al9). This criteria includes following signs: (1) absence of radiolucent lines; (2) presence of a superolateral buttress; (3) presence of medial stress shielding; (4) presence of radial trabeculae; (5) presence of an inferomedial buttress. Moore et al.9) noted that when three or more of these signs present, positive predictive value for bone ingrowth is very high.
RESULTS
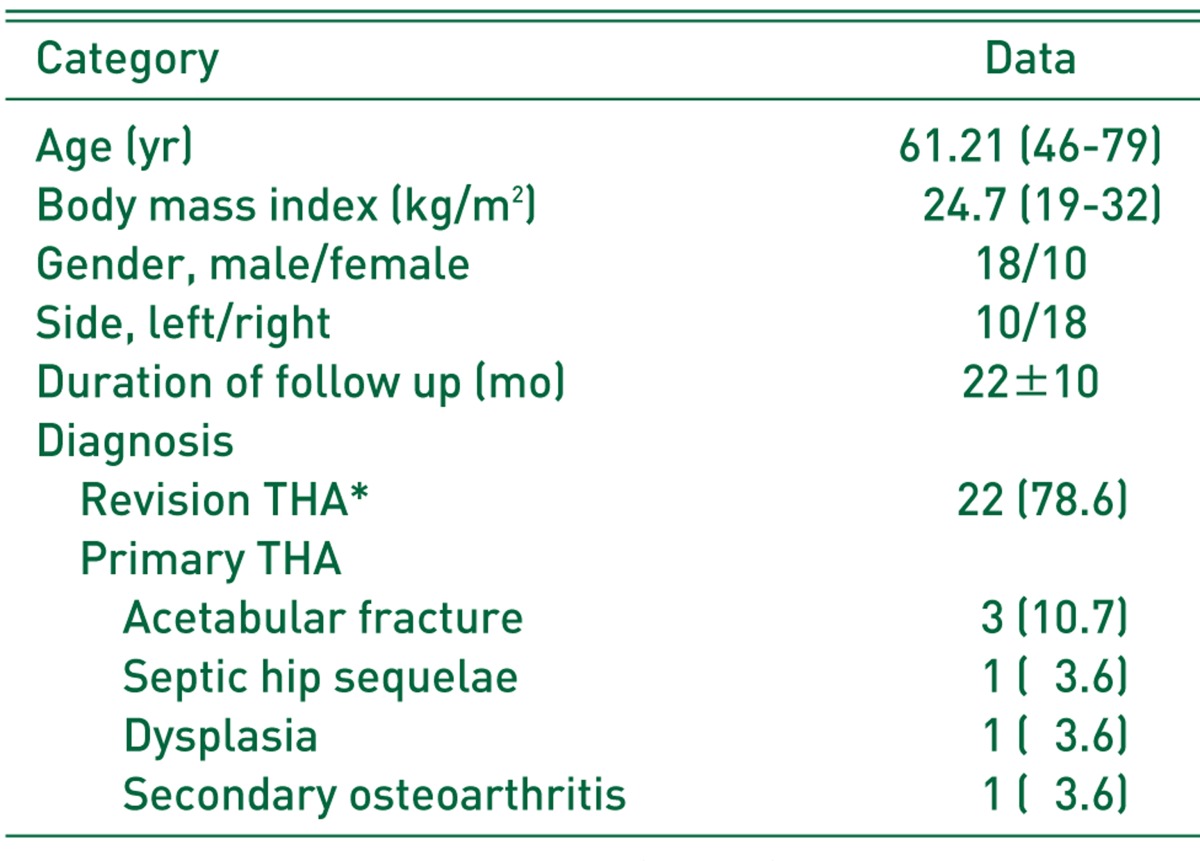
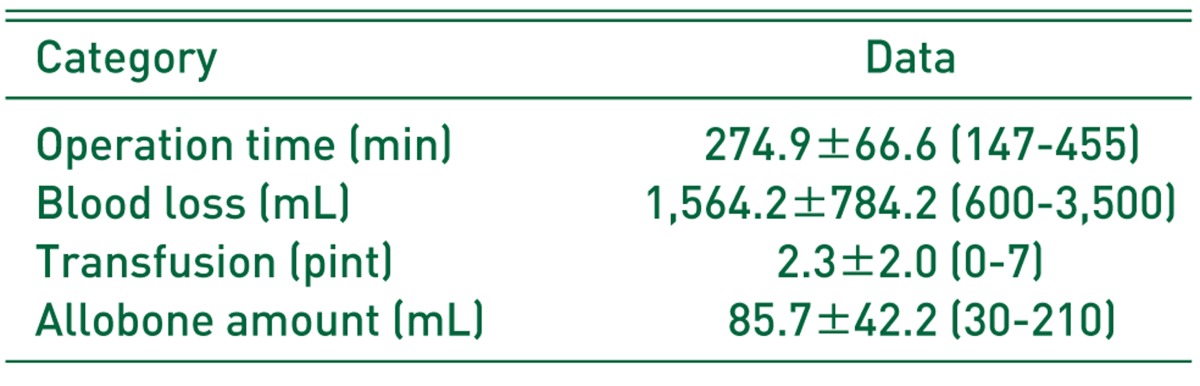
There were the demographics and clinical characteristics of patients (Table 1). Mean operation time was 274.9 minutes (147-455 minutes) and blood loss was 1,564.2 mL (600-3,500 mL). Also, mean transfusion and allograft amount were 2.3 pints (0-7 pints) and 85.7 mL (30-210 mL) (Table 2).
Table 1. Dermographic Data of Patients.
Values are presented as mean (range), number only, mean±standard deviation, or number (%).
THA: total hip arthroplasty.
*Revision, 13; re-revision or more, 9.
Table 2. Intraoperative Data of Patients.
Values are presented as mean±standard deviation (range).
1. Clinical Outcome
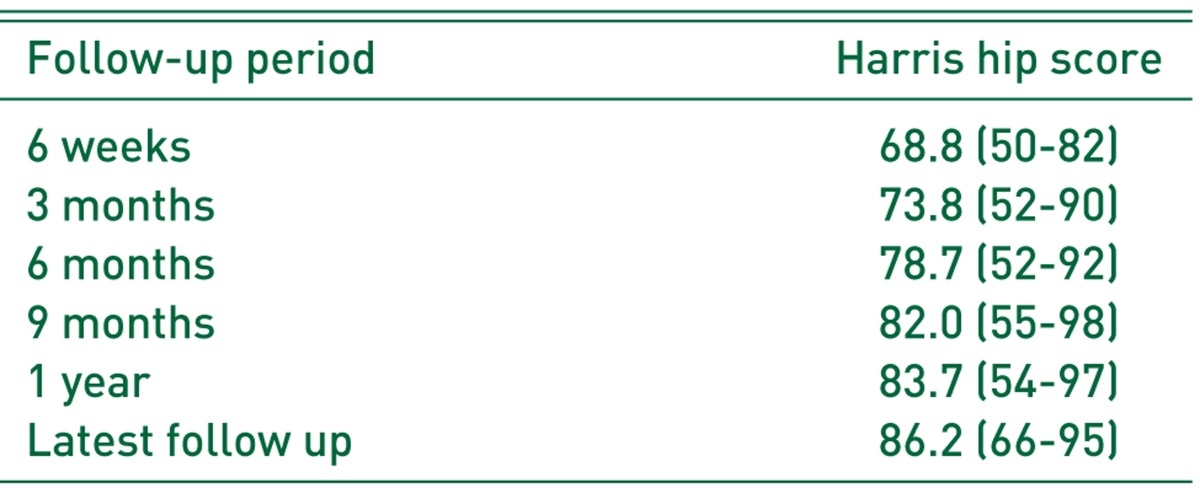
For clinical outcome, we compare pre-operative HHS with the most recent post-operative HHS. The average HHS was improved from 58.00 pre-operatively to 86.20 post-operatively. There were the HHS of follow up periods in Table 3.
Table 3. Clinical Outcome after Operation.
Values are presented as mean (range).
2. Radiographic Outcome
For radiological outcome, we compared initial postoperative radiograph with the final follow up radiograph. Regarding the acetabular cup, the average diameter of acetabular cup used was 55.64 mm (range, 48-62 mm) and an average degree of cup abduction was 44.29° (range, 26.27° -55.02°). The degree of cup abduction remained unchanged at the time of final follow up, as well as the position of acetabular cup with reference to the inter-teardrop line also remained unchanged at the time of final follow up. In our study, there was no case exhibiting osteolysis around acetabulum as well as there was no radiolucent line visible at host bone vs. cup and host bone vs. augment interface in any case at the time of final follow up. Regarding the trabecular metal augment, 50 mm was the most common diameter of augment used and 10 mm was the most common thickness of the augment used. Fifty-millimeters diameter of augment was used in 13 patients and 54-mm diameter of augment was used in 4 patients, followed by 58-mm diameter of augment in 11 patients. Ten-millimeters thickness of augment was used in 18 patients. We used one or two screws per augment and two or three screws per acetabular shell.
In our study, center of rotation of hip joint was located preoperatively, at a mean of 38.90 mm (range, 20.24-66.35 mm) above the interteardrop line. With the help of trabecular metal augments, we were able to bring down the center of rotation of hip joint postoperatively at a mean of 23.85 mm (range, 11.82-37.69 mm) above the interteardrop line. A high hip center was defined as being more than 35 mm above the interteardrop line10), because the inner to outer table thickness of the ilium attained its maximum of 42 mm (±9 mm) at a point 35 mm (±3 mm) above the anatomic teardrop, corresponding to the acetabular dome11). Preoperatively, there were 19 patients either with high hip center or with excisional arthroplasty of femoral head with proximal migration of femur, while post-operatively there was only one patient with high hip center (that was at 37.69 mm above the interteardrop line).
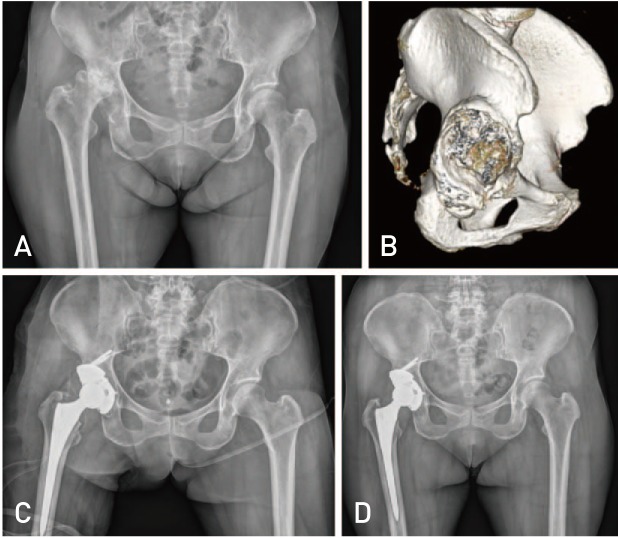
At the time of final follow up, out of 28 patients, radiographs of 5 patients showed four signs and 13 patients showed three signs of osseointegration according to the criteria of Moore et al.9), while 5 patients showed two signs and remaining 5 patients showed one sign of osseointegration according to the criteria of Moore et al9). So together, 18 patients out of 28 patients have three or more signs of osseointegration, which suggest there is very high probability of bone ingrowth into acetabular shell and the augments in these patients (Fig. 3).
Fig. 3. (A) Anteroposterior radiograph after undergoing 1st stage debridement for fourth time recurrent periprosthetic hip joint infection due to underlying chronic pelvic infection. (B) Three-dimensional computed tomography scan shows large bone defect of the acetabulum. (C) Immediate postoperative anteroposterior radiograph. (D) Three years postoperative anteroposterior radiograph shows a well fixed trabecular metal augment and the acetabular cup with bony ingrowth.
3. Complications
There was no further revision required in any patient. There was no evidence of radiolucent line, migration of acetabular component and signs of loosening of the augment and/or acetabular component in any patient. There is no sign of operative site infection in any patient. Only one patient had history of single episode of dislocation of hip joint in 4 weeks after surgery, for which close reduction under the general anesthesia was done and had no recurrent dislocation.
DISCUSSION
There are many options available to reconstruct the acetabular defect, depending upon the type and location of the defect. Uncemented porous coated hemispherical components with screw fixation or extra-large acetabular components have been reported successful for acetabular revisions12,13). However, uncemented hemispherical components alone have higher rates of failure in hips with severe bone loss, including D'Antonio et al.14) class IV defects, Paprosky et al.7) type 3 acetabular defects, and when there is less than 50% contact with living host bone7,15). Uncemented hemispherical components when used in conjunction with impaction bone grafting also showed poor results in large acetabular defects16). In such cases of severe bone loss, additional support is necessary to improve the outcome of revision reconstruction surgery. Acetabular defects can be reconstructed either by bone grafting alone or with cage or trabecular metal augments. Although, all of them have specific indications, there is a gray area where decision making is difficult3). Trabecular metal augment is one of the options for such reconstruction. Trabecular metal for revision surgery and for complex primary cases was introduced at the end of the twentieth century (Fig. 4). Trabecular titanium is an innovative highly porous structure that imitates the morphology of trabecular bone17). The average diameter of the cell pores, used in Ti6Al4V (trabecular titanium alloy) construct is 640 micrometer and the structure has an average porosity of 65%18). Trabecular titanium has exceptional biomechanical characteristics in terms of compression tests and tension tests for adhesion17,18). In-vivo studies showed promising results and remarkably fast and complete osseointegration17). Trabecular metal augments have very favourable biomechanical and biochemical properties for bony ingrowth. High coefficient of friction and its elastic modulus similar to bone makes it more suitable for biologic fixation6,17,18). In addition to this, their theoretical advantages like easy to use, modularity and lack of resorption (which is major problem with impaction bone grafting), make the augments very suitable implant for such reconstruction.
Fig. 4. (A) Anteroposterior radiograph shows secondary osteoarthritis due to underlying hip dysplasia. (B) Three-dimensional computed tomography scan shows large bone defect of the acetabulum. (C) Immediate postoperative anteroposterior radiograph. (D) Three years postoperative anteroposterior radiograph shows a well fixed trabecular metal augment and the acetabular cup with bony ingrowth.
In this study, the average HHS has improved from 58.00 pre-operatively to 86.20 post-operatively, which was good. Other studies using trabecular metal augments, like Van Kleunen et al.19), Del Gaizo et al.20), and Weeden and Schmidt21) reported average post-operative HHS 76.00, 81.50, and 84.00 respectively. This difference in HHS may be due to very low (lesser than our study) preoperative HHS in all these studies. Studies which have used other techniques for acetabular reconstruction (other than augments) like Gustke et al.22) and Patel et al.23) have reported average HHS of 72.00 and 81.00, respectively, after reconstruction with jumbo cups while, Schreurs et al.24) reported an average HHS of 79 after reconstruction with impaction grafting. Trabecular metal augment offers the adventages of a modular cup and augment system that require less stripping of the ilium and mobilization of the abductors, a technically easier and faster procedure. The potential for biologic fixation with the use of a trabecular metal augment way also provide improved postoperative rehabilitation and long-term outcomes25,26). In this study, trabecular metal augments shows good results of reconstruction of massive acetabular defect in achieving stable, pain free and well-functioning hip joint.
We were able to bring down the center of rotation of hip joint at a mean of 38.90 mm above the interteardrop line, preoperatively, to at a mean of 23.85 mm above the interteardrop line, postoperatively. As the augments are hemispherical in the shape, eccentric placement of the augment was solve this purpose. As the most of cases of severe acetabular defect have variable amount of superior rim deficiency, (for example Paprosky type 2B, 3A and 3B), center of rotation of hip joint has lost superior lateral buttress and migrates proximally. In such cases, to restore the anatomy of abductor muscles, trabecular metal augments are helpful in bringing down the center of rotation of hip joint to its normal or near normal position, which is not possible with other reconstruction options like jumbo cups and cages. As per study of Abolghasemian et al.27) and Banerjee et al.28), post-operative center of rotation of hip joint was at a mean of 24.8 mm and 24.1 mm, respectively. This suggests that the anatomy of the abductor muscle can be restored to normal with the augments.
Radiographically, loosening was considered present if the cup migrated superiorly more than 5 mm, medial migration (severe, cup in pelvis), continuous radiolucencies around cup in zones 1 to 3 of DeLee and Charnley29), cement fracture, broken cup or presence of progressive tilt as shown by studies of Röder et al.30) In our study, till the time of final follow up, no case exhibits radiolucent line between host bone and the implant (acetabular cup as well as augment). As per other studies, like Sporer and Paprosky31) and Del Gaizo et al.20), there was no case and one case of aseptic loosening, respectively. This is because of initial stability given by augment and also fastens osseointegration resulting into stable cup. None of our case exhibit osteolysis around acetabulum. Out of 28 patients in our study, there were 18 patients with three or more signs of osseointegration according to the criteria of Moore et al9). This may be due to short term study period and needs to be further follow up. None of our cases needed re-revision surgery.
There are several limitations of this study. First of all, being a retrospective study design, it is never as ideal as randomized controlled trial for comparison of this technique with other technique of reconstruction. Second, sample size of this study is also a limiting factor. As trabecular metal augments have limited indication in revision surgery and very rarely in primary cases, it was very difficult to get large number of cases. Third, mean follow up period of this study is also short in comparison to other studies19,20,22).
CONCLUSION
Results of acetabular reconstruction using trabecular metal augments for massive acetabular defects are very satisfactory but more long term studies are required preferably for better evaluation and comparison with other techniques of reconstruction to draw out any conclusion regarding which technique is better.
Footnotes
CONFLICT OF INTEREST: The authors declare that there is no potential conflict of interest relevant to this article.
References
- 1.Necas L, Katina S, Uhlarova J, Colton CL. Survival analysis of total hip and knee replacement in Slovakia 2003-2011. Acta Chir Orthop Traumatol Cech. 2013;80(Suppl):1–85. [Google Scholar]
- 2.Templeton JE, Callaghan JJ, Goetz DD, Sullivan PM, Johnston RC. Revision of a cemented acetabular component to a cementless acetabular component. A ten to fourteen-year follow-up study. J Bone Joint Surg Am. 2001;83-A:1706–1711. doi: 10.2106/00004623-200111000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Jain S, Grogan RJ, Giannoudis PV. Options for managing severe acetabular bone loss in revision hip arthroplasty. A systematic review. Hip Int. 2014;24:109–122. doi: 10.5301/hipint.5000101. [DOI] [PubMed] [Google Scholar]
- 4.Gill TJ, Sledge JB, Müller ME. The Bürch-Schneider anti-protrusio cage in revision total hip arthroplasty: indications, principles and long-term results. J Bone Joint Surg Br. 1998;80:946–953. doi: 10.1302/0301-620x.80b6.8658. [DOI] [PubMed] [Google Scholar]
- 5.Herrera A, Martínez AA, Cuenca J, Canales V. Management of types III and IV acetabular deficiencies with the longitudinal oblong revision cup. J Arthroplasty. 2006;21:857–864. doi: 10.1016/j.arth.2005.08.026. [DOI] [PubMed] [Google Scholar]
- 6.Bobyn JD, Stackpool GJ, Hacking SA, Tanzer M, Krygier JJ. Characteristics of bone ingrowth and interface mechanics of a new porous tantalum biomaterial. J Bone Joint Surg Br. 1999;81:907–914. doi: 10.1302/0301-620x.81b5.9283. [DOI] [PubMed] [Google Scholar]
- 7.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994;9:33–44. doi: 10.1016/0883-5403(94)90135-x. [DOI] [PubMed] [Google Scholar]
- 8.Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990;(257):107–128. [PubMed] [Google Scholar]
- 9.Moore MS, McAuley JP, Young AM, Engh CA., Sr Radiographic signs of osseointegration in porous-coated acetabular components. Clin Orthop Relat Res. 2006;444:176–183. doi: 10.1097/01.blo.0000201149.14078.50. [DOI] [PubMed] [Google Scholar]
- 10.Whitehouse MR, Masri BA, Duncan CP, Garbuz DS. Continued good results with modular trabecular metal augments for acetabular defects in hip arthroplasty at 7 to 11 years. Clin Orthop Relat Res. 2015;473:521–527. doi: 10.1007/s11999-014-3861-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Antoniades J, Pellegrini VD., Jr Cross-sectional anatomy of the ilium: implications for acetabular component placement in total hip arthroplasty. Clin Orthop Relat Res. 2012;470:3537–3541. doi: 10.1007/s11999-012-2574-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Della Valle CJ, Berger RA, Rosenberg AG, Galante JO. Cementless acetabular reconstruction in revision total hip arthroplasty. Clin Orthop Relat Res. 2004;(420):96–100. doi: 10.1097/00003086-200403000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Whaley AL, Berry DJ, Harmsen WS. Extra-large uncemented hemispherical acetabular components for revision total hip arthroplasty. J Bone Joint Surg Am. 2001;83-A:1352–1357. doi: 10.2106/00004623-200109000-00010. [DOI] [PubMed] [Google Scholar]
- 14.D'Antonio JA, Capello WN, Borden LS, et al. Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop Relat Res. 1989;(243):126–137. [PubMed] [Google Scholar]
- 15.Berry DJ. Revision total hip arthroplasty: uncemented acetabular components. In: Callaghan JJ, Rosenberg AG, Rubash HE, editors. The adult hip. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2007. pp. 1371–1381. [Google Scholar]
- 16.van Haaren EH, Heyligers IC, Alexander FG, Wuisman PI. High rate of failure of impaction grafting in large acetabular defects. J Bone Joint Surg Br. 2007;89:296–300. doi: 10.1302/0301-620X.89B3.18080. [DOI] [PubMed] [Google Scholar]
- 17.Benazzo F, Botta L, Scaffino MF, et al. Trabecular titanium can induce in vitro osteogenic differentiation of human adipose derived stem cells without osteogenic factors. J Biomed Mater Res A. 2014;102:2061–2071. doi: 10.1002/jbm.a.34875. [DOI] [PubMed] [Google Scholar]
- 18.Marin E, Fusi S, Pressacco M, Paussa L, Fedrizzi L. Characterization of cellular solids in Ti6Al4V for orthopaedic implant applications: Trabecular titanium. J Mech Behav Biomed Mater. 2010;3:373–381. doi: 10.1016/j.jmbbm.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 19.Van Kleunen JP, Lee GC, Lementowski PW, Nelson CL, Garino JP. Acetabular revisions using trabecular metal cups and augments. J Arthroplasty. 2009;24(6 Suppl):64–68. doi: 10.1016/j.arth.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 20.Del Gaizo DJ, Kancherla V, Sporer SM, Paprosky WG. Tantalum augments for Paprosky IIIA defects remain stable at midterm followup. Clin Orthop Relat Res. 2012;470:395–401. doi: 10.1007/s11999-011-2170-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weeden SH, Schmidt RH. The use of tantalum porous metal implants for Paprosky 3A and 3B defects. J Arthroplasty. 2007;22(6 Suppl 2):151–155. doi: 10.1016/j.arth.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 22.Gustke KA, Levering MF, Miranda MA. Use of jumbo cups for revision of acetabulae with large bony defects. J Arthroplasty. 2014;29:199–203. doi: 10.1016/j.arth.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 23.Patel JV, Masonis JL, Bourne RB, Rorabeck CH. The fate of cementless jumbo cups in revision hip arthroplasty. J Arthroplasty. 2003;18:129–133. doi: 10.1054/arth.2003.50038. [DOI] [PubMed] [Google Scholar]
- 24.Schreurs BW, Luttjeboer J, Thien TM, et al. Acetabular revision with impacted morselized cancellous bone graft and a cemented cup in patients with rheumatoid arthritis. A concise follow-up, at eight to nineteen years, of a previous report. J Bone Joint Surg Am. 2009;91:646–651. doi: 10.2106/JBJS.G.01701. [DOI] [PubMed] [Google Scholar]
- 25.Nehme A, Lewallen DG, Hanssen AD. Modular porous metal augments for treatment of severe acetabular bone loss during revision hip arthroplasty. Clin Orthop Relat Res. 2004;(429):201–208. doi: 10.1097/01.blo.0000150133.88271.80. [DOI] [PubMed] [Google Scholar]
- 26.Unger AS, Lewis RJ, Gruen T. Evaluation of a porous tantalum uncemented acetabular cup in revision total hip arthroplasty: clinical and radiological results of 60 hips. J Arthroplasty. 2005;20:1002–1009. doi: 10.1016/j.arth.2005.01.023. [DOI] [PubMed] [Google Scholar]
- 27.Abolghasemian M, Tangsataporn S, Sternheim A, Backstein D, Safir O, Gross AE. Combined trabecular metal acetabular shell and augment for acetabular revision with substantial bone loss: a mid-term review. Bone Joint J. 2013;95-B:166–172. doi: 10.1302/0301-620X.95B2.30608. [DOI] [PubMed] [Google Scholar]
- 28.Banerjee S, Issa K, Kapadia BH, Pivec R, Khanuja HS, Mont MA. Systematic review on outcomes of acetabular revisions with highly-porous metals. Int Orthop. 2014;38:689–702. doi: 10.1007/s00264-013-2145-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 30.Röder C, Eggli S, Aebi M, Busato A. The validity of clinical examination in the diagnosis of loosening of components in total hip arthroplasty. J Bone Joint Surg Br. 2003;85:37–44. doi: 10.1302/0301-620x.85b1.13367. [DOI] [PubMed] [Google Scholar]
- 31.Sporer SM, Paprosky WG. The use of a trabecular metal acetabular component and trabecular metal augment for severe acetabular defects. J Arthroplasty. 2006;21(6 Suppl 2):83–86. doi: 10.1016/j.arth.2006.05.008. [DOI] [PubMed] [Google Scholar]