Summary
Background
Japan has entered the era of super-ageing and advanced health transition, which is increasingly putting pressure on the sustainability of its health system. The level and pace of this health transition might vary across regions within Japan and concern is growing about increasing regional variations in disease burden. The Global Burden of Diseases, Injuries, and Risk Factors Study 2015 (GBD 2015) provides a comprehensive, comparable framework. We used data from GBD 2015 with the aim to quantify the burden of disease and injuries, and to attribute risk factors in Japan at a subnational, prefecture-level.
Methods
We used data from GBD 2015 for 315 causes and 79 risk factors of death, disease, and injury incidence and prevalence to measure the burden of diseases and injuries in Japan and in the 47 Japanese prefectures from 1990 to 2015. We extracted data from GBD 2015 to assess mortality, causes of death, years of life lost (YLLs), years lived with disability (YLDs), disability-adjusted life-years (DALYs), life expectancy, and healthy life expectancy (HALE) in Japan and its 47 prefectures. We split extracted data by prefecture and applied GBD methods to generate estimates of burden, and attributable burden due to known risk factors. We examined the prefecture-level relationships of common health system inputs (eg, health expenditure and workforces) to the GBD outputs in 2015 to address underlying determinants of regional health variations.
Findings
Life expectancy at birth in Japan increased by 4·2 years from 79·0 years (95% uncertainty interval [UI] 79·0 to 79·0) to 83·2 years (83·1 to 83·2) between 1990 and 2015. However, the gaps between prefectures with the lowest and highest life expectancies and HALE have widened, from 2·5 to 3·1 years and from 2·3 to 2·7 years, respectively, from 1990 to 2015. Although overall age-standardised death rates decreased by 29·0% (28·7 to 29·3) from 1990 to 2015, the rates of mortality decline in this period substantially varied across the prefectures, ranging from −32·4% (−34·8 to −30·0) to −22·0% (−20·4 to −20·1). During the same time period, the rate of age-standardised DALYs was reduced overall by 19·8% (17·9 to 22·0). The reduction in rates of age-standardised YLDs was very small by 3·5% (2·6 to 4·3). The pace of reduction in mortality and DALYs in many leading causes has largely levelled off since 2005. Known risk factors accounted for 34·5% (32·4 to 36·9) of DALYs; the two leading behavioural risk factors were unhealthy diets and tobacco smoking in 2015. The common health system inputs were not associated with age-standardised death and DALY rates in 2015.
Interpretation
Japan has been successful overall in reducing mortality and disability from most major diseases. However, progress has slowed down and health variations between prefectures is growing. In view of the limited association between the prefecture-level health system inputs and health outcomes, the potential sources of regional variations, including subnational health system performance, urgently need assessment.
Funding
Bill & Melinda Gates Foundation, Japan Ministry of Education, Science, Sports and Culture, Japan Ministry of Health, Labour and Welfare, AXA CR Fixed Income Fund and AXA Research Fund.
Introduction
Japan is one of the fastest ageing countries in the world with a population that has started to shrink since 2008 mainly due to a low fertility rate.1 The number of Japanese people aged 65 years or older has nearly quadrupled in the past 40 years to 27% of the total population in 2016,2 making Japan the country with the highest proportion of elderly people in the world.3 This figure is expected to increase to 35% of the population by 2040, and to 40% by 2060.4 The ageing population has a substantial effect on disease structure, turning Japan into the advanced stage of epidemiological transitions—ie, elderly Japanese people experience more chronic and multimorbidity, which require long-term care and put pressures on health-care expenditure and use of resources.5 However, the pace of epidemiological transitions as well as population decline varies substantially by region,6, 7 and such regional variations could have great influence on the performance of regional health systems and population health outcomes.8 In Japan, regional variations in health outcomes, its causes, performance of regional health systems, and the effects of social determinants of health are becoming increasingly complex with the country's transition to a super-ageing society.5, 9, 10
Research in context.
Evidence before this study
Japan is one of the most successful countries in the world for many health indicators, but the level and pace of progress in health are not unique across the country and concern is growing about increasing health variations in Japan and its prefectures. These trends suggest Japan is experiencing a more complex process of health transition than historically observed; however, to our knowledge, no systematic and comprehensive study has been implemented to explore the variation within the country. Attributable risks have been calculated for some causes (eg, tobacco smoking and alcohol consumption) and for some disorders (eg, cancer) but are not available in a comprehensive framework covering multiple risks and diseases because no single accessible data source describing disease burden by cause exists in Japan.
Added value of this study
To our knowledge, this study is the first to assess GBD results at the prefecture level in Japan, using a range of routine and published data sources. Our comprehensive subnational comparisons within Japan's 47 prefectures provide new insights into health trends and determinants, particularly in light of the rapid population ageing process and growing regional variations in health.
Implications of all available evidence
Despite substantial reductions in the mortality and disability from most preventable diseases and improvement in life expectancy since 1990, many leading causes of death varied markedly at prefecture level in Japan. National and local health policies should therefore address region-specific health interventions in the most at-risk prefectures, aiming at dealing with regional variations in health. Preventive public health measures still have a huge capacity to reduce the continuing burden of preventable diseases via scaling up of investment in research and development of new and better prevention, treatment, and care strategies. Increasing levels of multimorbidity—because of the growing effect of survivorship, together with the super-ageing population—need to be addressed in Japan's recent health system reforms, in which a range of public services spanning health and social care services that respond to the specific needs, contexts, and circumstances of individual patients are offered. Although health in Japan is improving, substantial opportunities exist for a healthier population in Japan via modifiable risk factor approaches throughout life, especially through tackling of unhealthy diet and tobacco smoking.
Although regional health variations associated with communicable diseases have been narrowing over time globally, disease burden due to non-communicable diseases (NCDs) and injury varies markedly across regions.11, 12, 13 Previous subnational studies in the UK,11 Mexico,12 and China13 shed light on the importance of the subnational estimates of disease burden. These enabled policy makers to improve understanding of the health needs of each region and to inform domestic health policy making.11, 12, 13 The issue of regional variations in health is especially relevant in Japan, as the country is confronted by a super-ageing population and increasing health expenditure.8 In this context, what is happening in Japan—the country at the forefront of the world's hyper-ageing societies—has many implications for other countries. However, to our knowledge, no systematic subnational comparative assessment of disease burden and risk factors have been done in the context of Japan.14 Empirical evidence in Japan would be immensely helpful to reveal the features of an ageing society in the advanced stage of epidemiological transition, and understanding how to respond to regional health variations.
Using the latest data from the Global Burden of Diseases, Injuries, and Risk Factors Study 2015 (GBD 2015), we compared mortality, causes of death, years of life lost (YLLs), years lived with disability (YLDs), disability-adjusted life-years (DALYs), life expectancy at birth, and healthy life expectancy at birth (HALE, the average number of years that a newborn can expect to live in full health), as well as attributable risk factors in Japan's 47 prefectures—the country's first-order administrative division. This study comes at a time when both national and local health policy makers are reviewing and assessing priorities for action in light of the rapidly ageing population and growing regional health variation.6, 7 This subnational analysis we report here supports mapping of the disease burden in Japan; and contributes to national and region-specific health policies.
Methods
Overview
GBD 2015 provides updated and improved data and methods from previous GBD versions (2010 and 2013).15, 16, 17, 18 We used data from GBD 2015 for 315 causes and 79 risk factors of death, disease, and injury incidence and prevalence to measure the burden of diseases and injuries in Japan and in the 47 Japanese prefectures from 1990 to 2015. The population demographic of each prefecture can be found elsewhere.4 The methods used in GBD 2015, including the systematic approach to collating cause of death from different countries, the mapping across different revisions and national variants of the International Classification of Diseases and Injuries and Related Health Problems (ICD), redistribution of deaths assigned to so-called garbage codes, and the cause of death modelling approach used for each cause, have been described in detail elsewhere.15, 16, 17, 18 Unless indicated otherwise, we present results in terms of age-standardised rates, as derived from world population standards developed for GBD 2015.15
Our estimates for each measure (eg, deaths, DALYs, life expectancy) depend on the Bayesian approach and, unless noted otherwise, 95% uncertainty intervals (UIs)—also known as credible intervals—are presented along with them. These UIs include uncertainty in our estimates that depend on the sample size of data, adjustments to different sources of all-cause mortality, and cause-of-death model specification and estimation. Uncertainty from all of these sources is propagated into the final quantities of interest by taking 1000 draws from the posterior distribution of each component quantity of interest.15, 16, 17, 18 We were unable to quantify and include uncertainty in garbage code redistribution algorithms—statistical models adopted in GBD 2015 to reassign deaths in garbage codes to more specific causes of death.15 In this study, we focus on specific data and analyses used to quantify mortality, causes of death, YLLs, YLDs, DALYs, life expectancy at birth and HALE at birth.
Mortality, cause of death, life expectancy, and YLLs
We used national population censuses and national and prefecture-level records on all-cause mortality derived from Japan's national vital registration systems. Vital registration data from 1990 to 2013 were included to align with GBD 2015, which spans 25 years from 1990 to 2015. Additional details on the full range of data sources are in the appendix (pp 10–25). Details for GBD 2015 estimation methods for all-cause mortality have been reported previously.15, 19
As described previously,15, 20 an expanded cause-of-death database was constructed for GBD 2015. To generate estimates on cause-specific mortality rate, we analysed prefecture-level vital registration data from 1990 to 2013. We sought to account for vital registration data quality and completeness, which included adjustment of cause-of-death data and standardisation of data to align with cause classifications and hierarchies in the GBD 2015 study.15 We then systematically identified causes of death that could not or should not be classified as underlying causes of death (so-called garbage codes), and applied standard GBD 2015 garbage code redistribution algorithms. To examine the changes in life expectancy at birth in 2015 from 2005, we have applied the life expectancy cause-specific decomposition method developed by Beltran-Sanchez, Preston, and Canudas-Romo.21 We computed YLLs using the standard GBD methods whereby we multiplied each death by the reference life expectancy at each age. The reference life expectancy at birth is 86·59 years, which is based on the lowest observed death rates for each 5-year age group in populations larger than 5 million.15
Disease and injury incidence, prevalence, and YLDs
Data sources used for quantifying non-fatal outcomes in Japan are in the appendix (pp 10–25). We used DisMod-MR 21, an updated Bayesian-regression analytic tool,16 to synthesise consistent estimates of disease incidence, prevalence, remission, excess mortality, and cause-specific mortality rates. Details of the estimation method, including the source code are published in the methods appendix of GBD 2015 publications.16 Following GBD 2015 methods,16 we multiplied prevalence of each sequela by the disability weight for the corresponding health state to calculate YLDs for the particular sequela. The sum of all YLDs for relevant sequelae equated to overall YLDs for each disease. GBD 2015 used the same disability weights as in GBD 2013, details of which including data collection and disability weight construction, have been described previously.22
DALYs, HALE, and attributable risks
Following GBD 2015 methods,17 national and prefecture-level DALYs were computed by summing YLLs and YLDs for each cause, age, and sex in 1990, 2005, and 2015. HALE was calculated for Japan and each prefecture using multiple-decrement life tables and estimated YLDs per person.17 To calculate risk-attributable fractions of disease burden by cause, we modelled the effects of risk exposure levels, documented relative risks associated with risk exposure and specific health outcomes, and computed counterfactual levels of risk exposure on estimates of national and prefecture-level deaths, YLLs, YLDs, and DALYs. Detailed descriptions of the GBD 2015 methods for risk factor assessment and attribution are found elsewhere.18
Health system inputs and health outcomes in 2015
Health systems are important underlying determinants of health and are mainly responsible for health variations.23 Correlations of prefecture-level per capita health expenditure and number of health workforce per population (physicians, registered nurses, and public health nurses)—common inputs for health system and major control levers for the Japanese health policy—to health outcomes in 2015, such as mortality and DALYs were calculated using Pearson's correlation coefficients. We also used a univariate linear regression analysis to assess the association between them. We extracted data for total health expenditure per capita for each prefecture in 2015 and the number of physicians, registered nurses, and public health nurses for each prefecture in 2014 from the database maintained by the Ministry of Health, Labour and Welfare of Japan.24, 25, 26
Role of the funding source
The funder of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the paper. All authors had full access to all the data in the study and had final responsibility to submit for publication.
Results
Between 1990 and 2015, a 4·2-year increase in life expectancy at birth was recorded in Japan, rising from 79·0 years (95% UI 79·0–79·0) to 83·2 years (83·1–83·2; appendix pp 26–31). The life expectancy at birth in 2015 was 79·9 years (79·9–80·0) for men and 86·3 years (86·3–86·4) for women. Okinawa recorded the smallest improvement of 3·2 years, whereas Saga had the largest gains of 4·8 years in the same period. The gap between prefectures with the lowest and highest life expectancies in 1990 was 2·5 years. By 2015, the longevity gap widened to 3·1 years.
Healthy life expectancy (HALE) at birth rose from 70·4 years (95% UI 67·8–72·6) in 1990 to 73·9 years (71·3–76·3) in 2015 (appendix pp 26–31). In 2015, HALE was 71·5 years (69·1–73·7) for men and 76·3 years (73·3–78·9) for women. The approximate 9-year gap between life expectancy at birth and HALE at birth observed in 1990 has been static until 2015 (appendix pp 26–31). The gap between prefectures with the lowest and highest HALE in 1990 was 2·3 years. As with life expectancy, this gap in HALE among prefectures increased by 2015 to 2·7 years.
All-cause age-standardised death rates decreased by 29·0% (95% UI 28·7–29·3) between 1990 and 2015, falling from 584·1 deaths per 100 000 people (583·2–585·1) in 1990 to 414·8 deaths per 100 000 people (413·3–416·4) in 2015 (appendix pp 26–31). Prefecture-level reductions in all-cause age-standardised death rates largely varied from 22·0% (20·1–24·0) in Okinawa to 32·4% (30·0–34·8) in Shiga between 1990 and 2015. During the same time period, the rate of age-standardised DALYs reduced by 19·8% overall (17·9–22·0). The reduction in the rate of age-standardised YLLs was 33·4% (33·0–33·8; appendix pp 32–37), indicating a proportionately larger reduction in premature mortality when compared with overall mortality. By contrast, reduction in rates of age-standardised YLDs was very small between 1990 and 2015 (3·5% [2·6–4·3]).
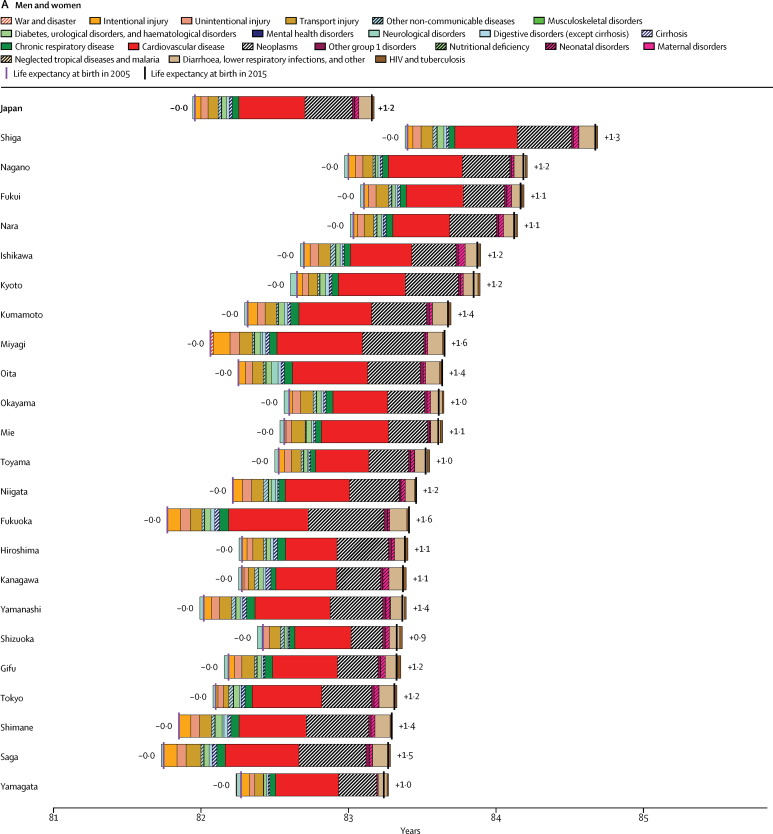
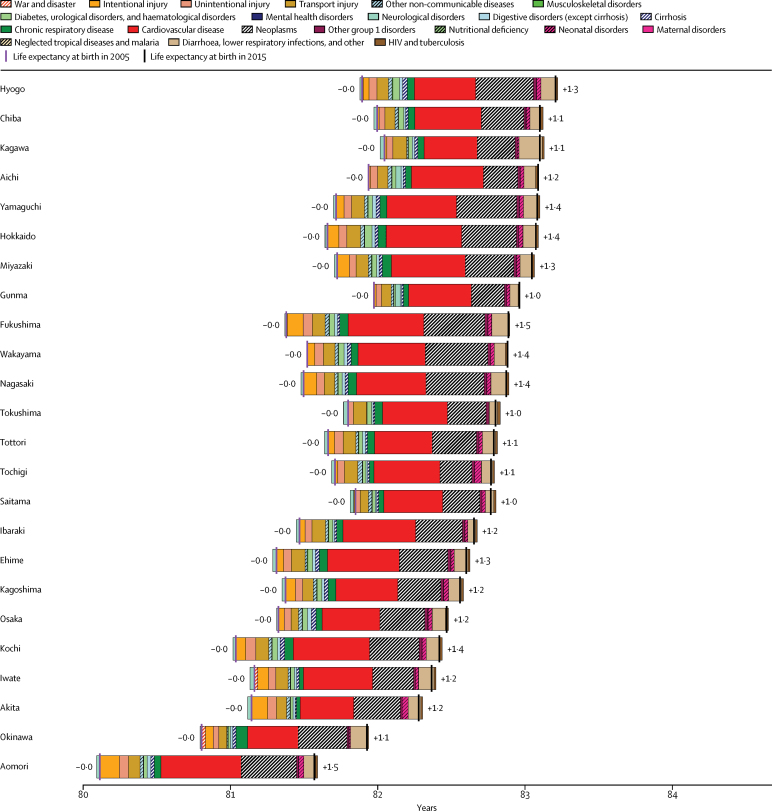
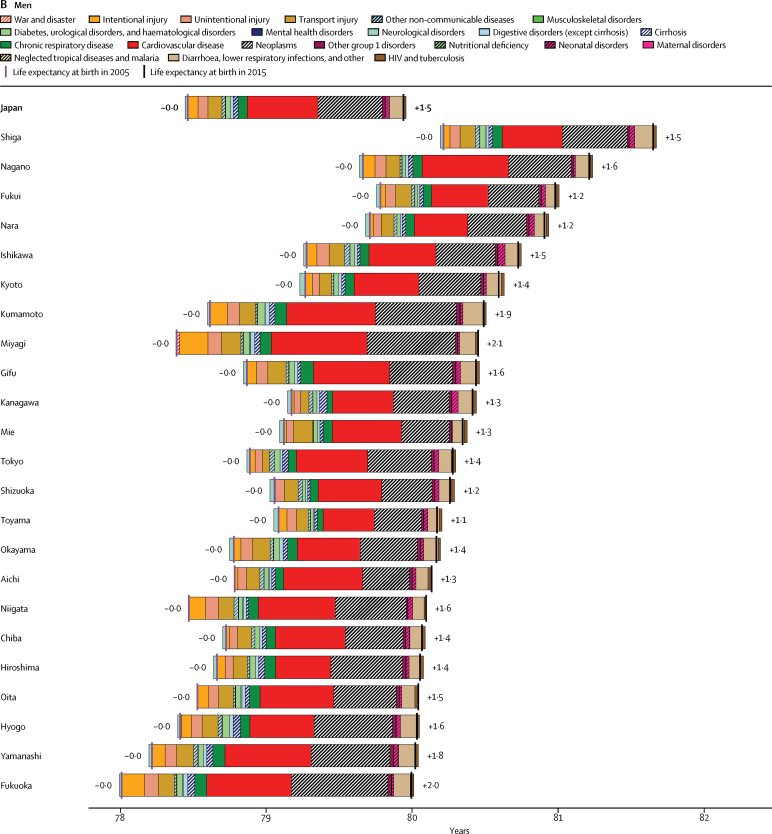
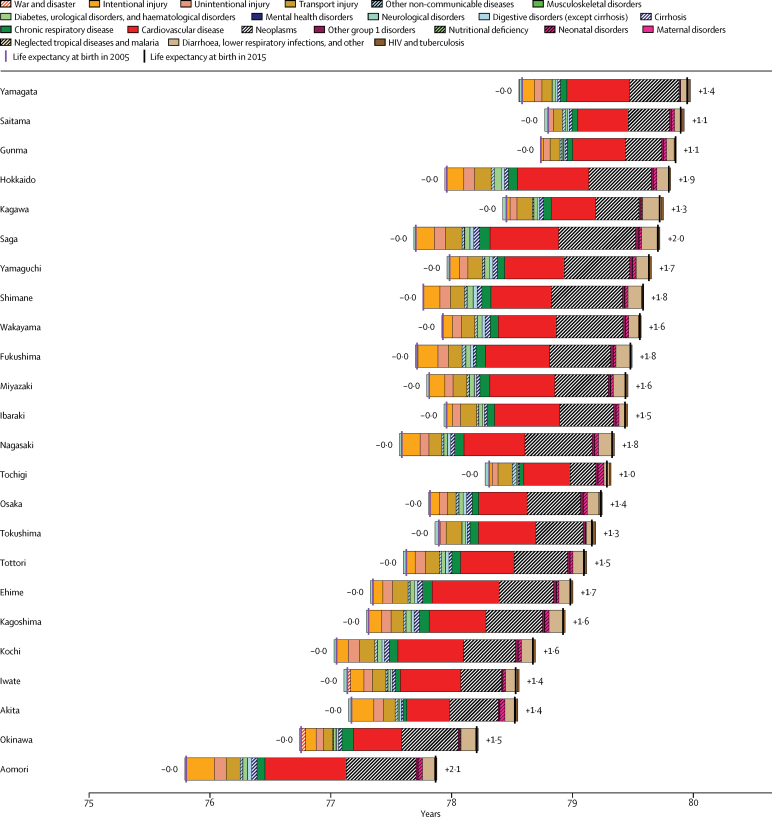
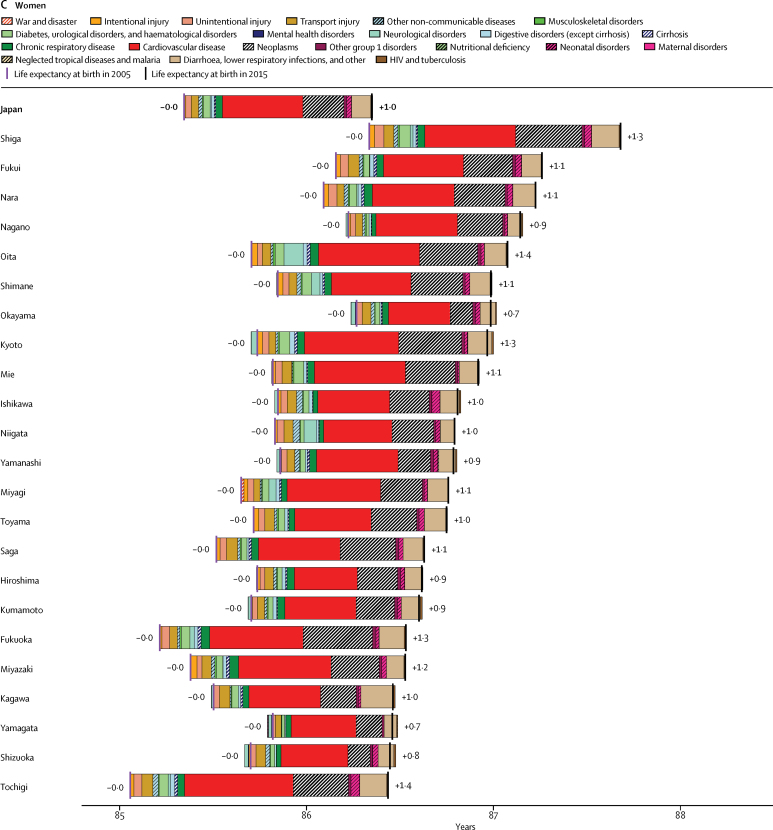
In the 10 years between 2005 and 2015, all 47 prefectures had more than 1 year of life expectancy gains (figure 1), but the gap in the gains between prefectures was distinctive. Across the prefectures, decreased mortality because of cardiovascular diseases (mostly cerebrovascular diseases and ischaemic heart diseases) and neoplasms or cancers was the leading driver of increased life expectancy.
Figure 1.
Life expectancy at birth in Japan and the 47 prefectures in 2015 and its change from 2005 to 2015 decomposed into the contribution of GBD level 2 cause group for (A) both sexes combined, (B) men, and (C) women
Causes to the left of the 2005 life expectancy values reflect causes that contributed to reduced life expectancy between 2005 and 2015. Causes to the right of the 2005 life expectancy values reflect causes that contributed to increased life expectancy between 2005 and 2015. GBD=Global Burden of Diseases, Injuries, and Risk Factors.
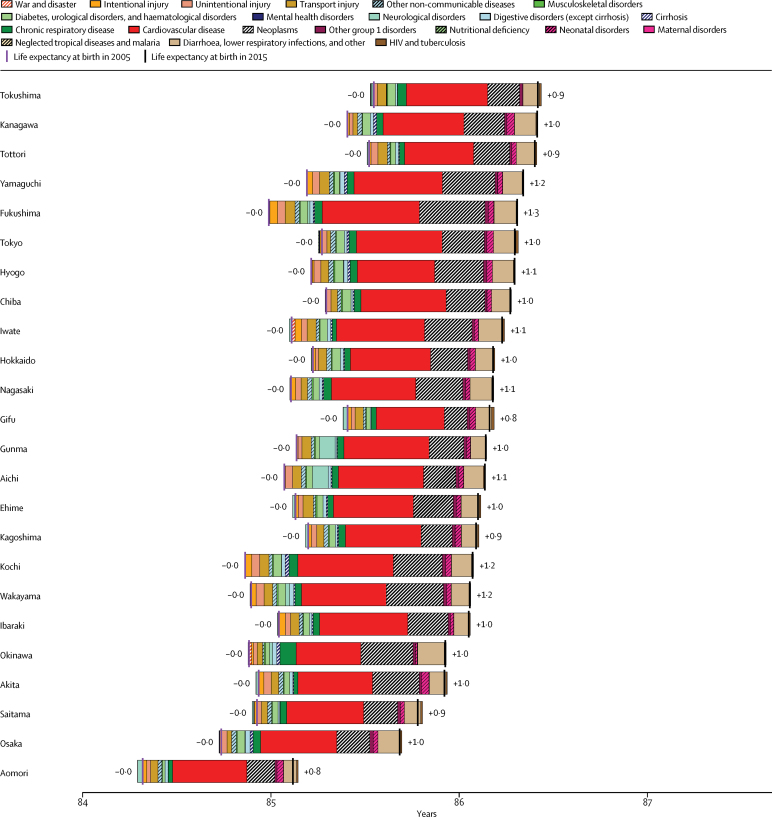
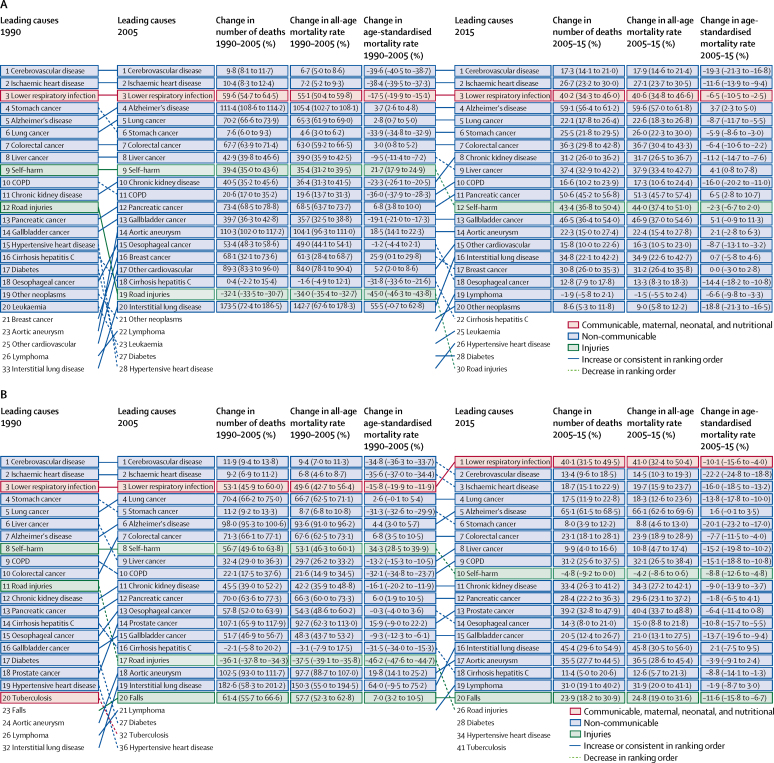
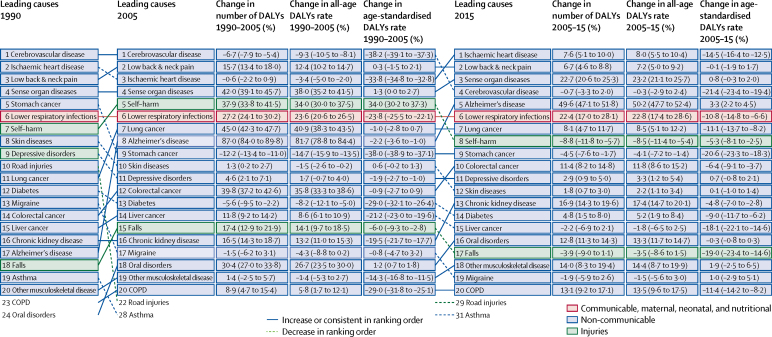
The leading causes of death using broad disease categories (level 3 in the GBD cause hierarchy) are in figure 2. The top three causes of death in 1990 (cerebrovascular diseases, ischaemic heart diseases, and lower respiratory infection) remained at the top in 2015, despite substantial declines in their age-standardised rates (−19·3% [95% UI −21·3 to −16·8], −11·6% [–13·9 to −9·4], and −6·5% [–10·5 to −2·5]; figure 2). In addition, the speed of mortality decline in these three leading causes and many other causes has levelled off since 2005 for both men and women (average annual percentage change in age-standardised death rates between 1990 and 2005 was −2·6% for cerebrovascular diseases, −2·6% ischaemic heart diseases, and −1·2% for lower respiratory infection; after 2005, −1·9%, −1·2%, and −0·7%). Alzheimer's disease and other dementias were the only causes out of the ten leading causes that showed a significant increase in age-standardised death rates since 2005 (3·7% [95% UI 2·3–5·0]). The leading causes of YLLs are shown in the appendix (p 1).
Figure 2.
GBD level 3 causes of death in Japan in 1990, 2005, and 2015 for (A) both sexes combined, (B) men, and (C) women, with all-age and age-standardised death rate change
Ranking is based on the number of deaths from each cause. Percentage change in number of deaths and in all-age and age-standardised death rates are shown with 95% UI in parentheses. Alzheimer's disease=Alzheimer's disease and other dementias. Cirrhosis hepatitis C=cirrhosis of the liver due to hepatitis C. COPD=chronic obstructive pulmonary disease. GBD=Global Burden of Diseases, Injuries, and Risk Factors.
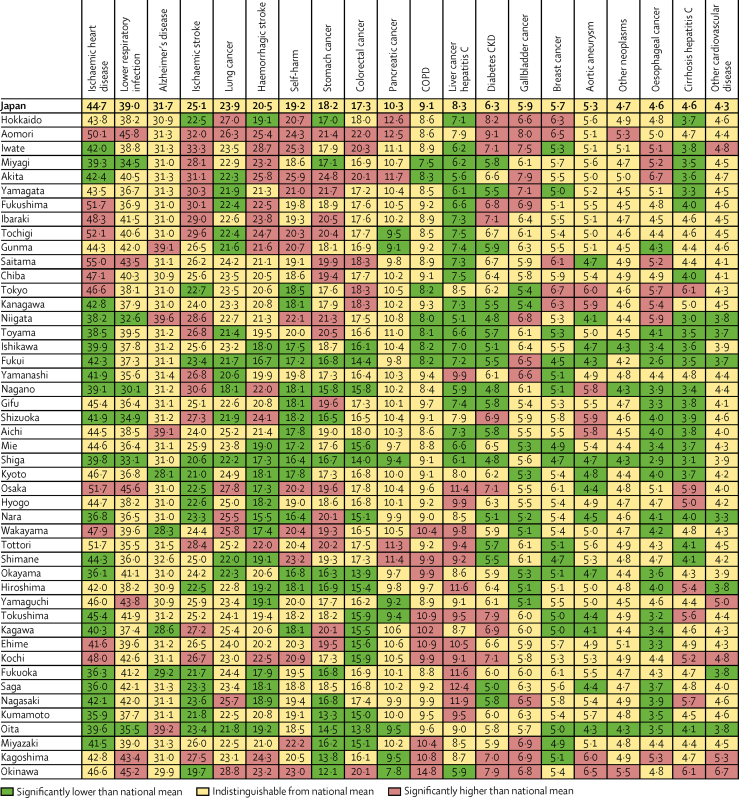
Age-standardised death rates for GBD's most detailed causes between Japan and the 47 prefectures in 2015 are shown in figure 3. A subnational comparison of age-standardised rates for YLLs are shown in figure appendix 2 (p 2). Many of the leading causes of mortality and YLLs showed striking variation by prefecture (figure 3). For example, due to cerebrovascular disease (combined mortality of ischaemic stroke, haemorrhagic stroke, and other types of stroke), Shiga's age-standardised death rates (37·9 per 100 000 people)—the lowest in Japan in 2015—was 1·6 times lower than Iwate's, which was the highest (62·0 per 100 000 people). For ischaemic heart disease, the age-standardised death rate was 1·5 times lower in Kumamoto (lowest; 35·9 per 100 000 people) and Saitama (highest; 55·0 per 100 000 people). Some causes had distinct patterns largely determined by geography (higher rates in the north, and lower in the central and south), and others did not.
Figure 3.
Age-standardised rates (per 100 000) of mortality by GBD level 4 cause group for Japan and the 47 prefectures in 2015 for both sexes combined
Japan and prefectures are ordered from north (Hokkaido) to south (Okinawa). The causes shown are the top 20 age-standardised rates of mortality in Japan. Rates are colour-coded to denote statistically significant differences from Japan's national mean. Significance set at p<0·05. Alzheimer's disease=Alzheimer's disease and other dementias. COPD=chronic obstructive pulmonary disease. Liver cancer hepatitis C=liver cancer due to hepatitis C. Cirrhosis hepatitis C=cirrhosis of the liver due to hepatitis C. GBD=Global Burden of Diseases, Injuries, and Risk Factors.
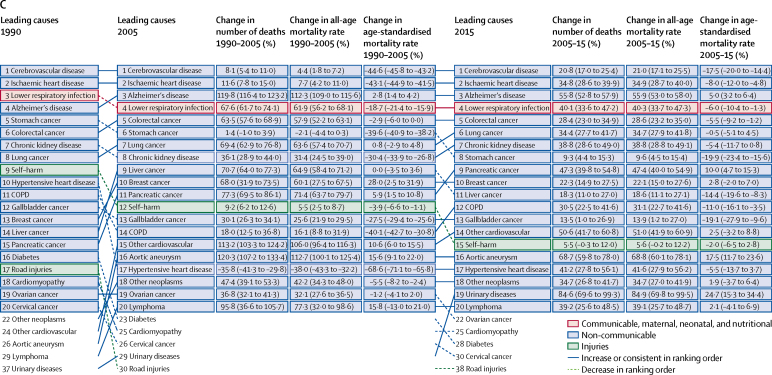
Cerebrovascular disease and ischaemic heart diseases are now at similar levels nationally in Japan (figure 4). As with mortality, the pace of reduction in DALYs in these causes largely levelled off since 2005. The average yearly percentage change in age-standardised DALY rates was −2·6% for both ischaemic heart diseases and cerebrovascular disease from 1990 to 2005, which reduced to −1·5% for ischaemic heart diseases and −2·1% for cerebrovascular disease after 2005. With no significant change in age-standardised DALY rates since 2005, low back and neck pain, sense organ diseases (consisting of hearing loss and vision loss), and depressive disorders were leading causes of DALYs in 2015, although they did not cause substantial death and YLLs but major disabilities. Alzheimer's disease and other dementias are distinctive causes of DALYs, which was only one (of the ten leading causes) that significantly increased age-standardised DALY rates between 2005 and 2015 by 3·3% (95% UI 2·2–4·5).
Figure 4.
GBD level 3 causes of DALYs in Japan in 1990, 2005, and 2015 for both sexes combined, with all-age and age-standardised DALY rate change
Ranking is based on the number of DALYs from each cause. Percentage change in number of DALYs and in all-age and age-standardised DALY rates are shown with 95% UI in parentheses. Alzheimer's disease=Alzheimer's disease and other dementias. COPD=chronic obstructive pulmonary disease. DALYs=disability-adjusted life-years. GBD=Global Burden of Diseases, Injuries, and Risk Factors.
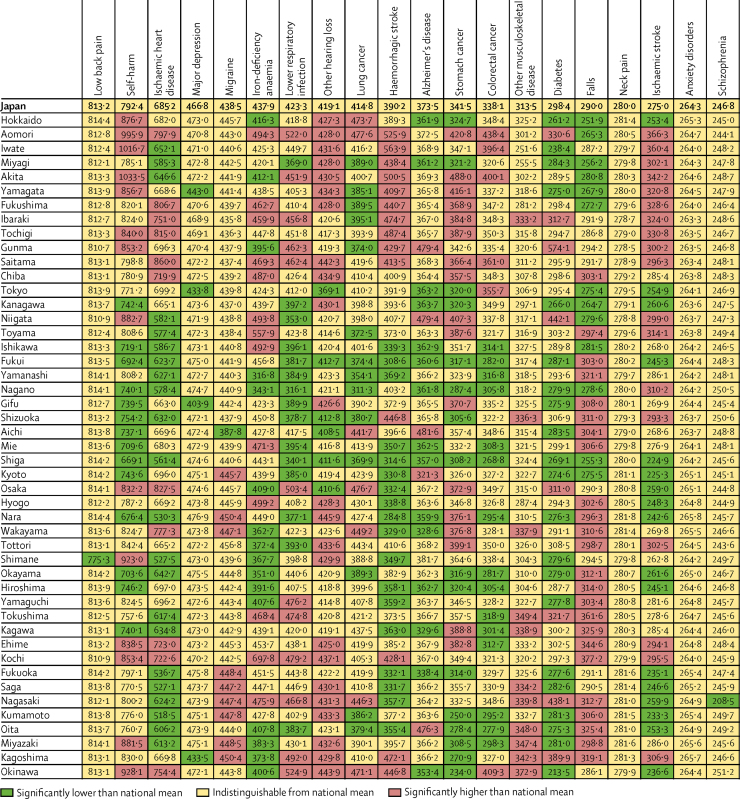
Age-standardised DALY rates by Japan's 47 prefectures for GBD's most detailed causes are in figure 5. Many causes, that were also significant causes of death (eg, ischaemic heart diseases and cerebrovascular disease), showed substantial variation between prefectures, which largely followed patterns determined by geography. As with mortality, the difference between prefectures with the lowest and highest DALY rates in 2015, was 1·7 times for ischaemic heart disease and 1·8 times for cerebrovascular disease (combined DALY rates of ischaemic stroke, and haemorrhagic and other stroke). Many disabling conditions that predominantly lead to DALYs but do not cause substantial death, such as low back and neck pain, major depression, anxiety disorders, and schizophrenia, were homogeneous across the prefectures, revealing no distinct patterns.
Figure 5.
Age-standardised rates (per 100 000) of DALYs by GBD level 4 cause group for Japan and the 47 prefectures in 2015 for both sexes combined
Japan and prefectures are ordered from north (Hokkaido) to south (Okinawa). The causes shown are the top 20 age-standardised DALYs rates in Japan. Rates are colour-coded to denote statistically significant differences from Japan's national mean. Significance set at p<0·05. Alzheimer's disease=Alzheimer's disease and other dementias. DALYs=disability-adjusted life-years. GBD=Global Burden of Diseases, Injuries, and Risk Factors. Other hearing loss=age-related and other hearing loss.
Overall for Japan in 2015, 47·1% (95% UI 44·9–49·3) of total deaths were attributable to identified risk factors: behavioural risk factors accounted for 33·7% (30·9–36·8) of total deaths, metabolic risks for 24·5% (22·6–26·4), and environmental and occupational risks for 6·7% (5·4–8·2; data not shown). Similarly, all identified risk factors jointly explained 34·5% (95% UI 32·4–36·9) of DALYs, with the remaining 65·6% DALYs as yet unexplained by the risk factors analysed. Nationally, behavioural risk factors made a greater contribution to DALYs in 2015 (25·2% of total DALYs [22·9–27·7]) than metabolic risks (16·4% [15·2–17·6]) or environmental and occupational risks (4·4% [3·9–4·1]).
Dietary risks—combined risks of diets high in sodium, and diets low in whole grains, fruits, vegetables, and nuts and seeds—were the leading risk for DALYs both in men (13·8% [95% UI 11·7–16·3]) and women (9·3% [7·8–11·5]) in 2015. Among the dietary risks, high sodium consumption was the dominant risk for DALYs in both men and women (men 4·4% [2·2–7·3]; women 3·0% [1·4–5·2]). Tobacco smoking was the second leading risk factor for men (12·5% [11·0–14·0]). A number of metabolic risks, such as high blood pressure and high fasting plasma glucose, were among the five leading risk factors for DALYs in both men and women. The contributions of these risk factors to DALYs did not vary much across the prefectures in 2015 (appendix pp 3–5). For example, dietary risks accounted for 10·4% (8·7–12·4) of total DALYs in Fukuoka (lowest) and 13·5% (11·3–15·6) in Aomori (highest). High sodium—the dominant downstream risk of dietary risks—explained 3·2% (1·5–5·4) of total DALYs in Okinawa (lowest) and 4·5% (2·2–7·4) in Akita (highest). For mortality, smoking was the leading risk factor for men (18·9% [95% UI 17·4–20·4]), while dietary risks were the major contributors to the total deaths for both men (18·8% [15·7–21·8], second rank) and women (18·0% [15·0–21·4], first rank). The contributions of these risk factors to mortality also did not vary much across the prefectures in 2015 (appendix pp 6–8).
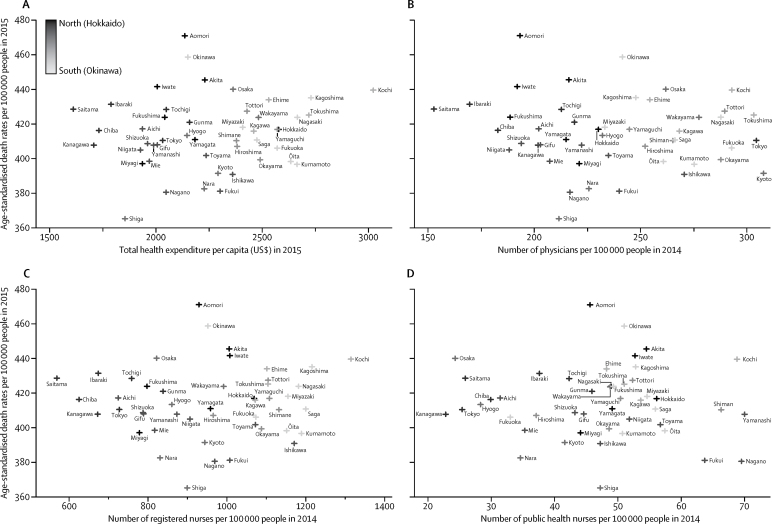
We observed a distinct north–south gradient—with higher values in the south and lower in the north for the health system inputs analysed (appendix p 38). The prefectural mean of per capita health expenditure was US$2246 (SD 311). In 2015, the average number of health workforce per 100 000 people across prefectures in 2014 was 237 (39) physicians, 957 (178) registered nurses, and 47 (12) public health nurses. The associations between the age-standardised death rates in 2015 and prefecture's per capita health expenditure (in 2015), number of physicians, registered nurses, and public health nurses per 100 000 people (in 2014) are shown in figure 6. Their Pearson's correlation coefficients were all very small (0·12, 0·10, 0·02, and −0·05, respectively), indicating very weak correlations, and there were no statistically significant relationship between them with small regression coefficient of 0·01, −0·05, 0·00, and −0·08, respectively. Similar results were obtained for age-standardised DALY rates (appendix p 9).
Figure 6.
Association between age-standardised death rates and (A) total health expenditure per capita, (B) number of physicians, (C) registered nurses, and (D) public health nurses per 100 000 people
A gradation of symbols refers to the dark to light (black to white) from north (Hokkaido) to south (Okinawa). We defined the total health expenditure as the sum of inpatient and outpatient expenditures (not including those on dental care). In presenting results, we used the exchange rate of 112 Japanese yen per US$ as of Feb 3, 2017.
Discussion
Japan has had the highest average life expectancy in the world since 1986.27 Annual mortality statistics show a decline in age-standardised mortality rates in Japan since 1998 to present,28 except for 2011, when an unprecedented earthquake of magnitude 9·0 off the Pacific coast of Japan killed more than 18 000 people.29 Across the prefectures, decreased mortality due to cardiovascular diseases and neoplasms has been the leading driver of increased life expectancy; however, the pace of reduction in age-standardised death rates from many leading causes, in particular from cardiovascular diseases, has slowed down since 2005. Although mortality from many leading causes has declined, mortality from Alzheimer's disease and other dementia has substantially increased in both number of people dying and age-standardised death rates since 2005, indicating that improvements in overall mortality in Japan might have levelled off mainly due to these causes. Similar to mortality, the pace of reduction in DALYs in these leading causes also largely slowed down since 2005. All-cause age-standardised YLLs decreased by 33·4% between 1990 and 2015; however, the reduction in the rate of age-standardised YLDs was only 3·5% (appendix pp 32–37). These findings indicate an increase in the proportion of the population with morbidity, particularly age-related disorders.
One important implication of our results is that, coupled with the slowed-down progress in population health, Japan is experiencing a morbidity expansion due to its health transition. This expansion will require a shift in the health system framework in Japan. Yasuhisa Shiozaki, the Minister of Health, Labour, and Welfare, commissioned the “Health Care 2035 Advisory Panel” in 2015 that brought together young Japanese health policy leaders to develop a long-term strategy for Japan's future health policy for the next 20 years. Their report—Japan Vision: Health Care 203530, 31—proposes integrating health care into social and community system frameworks around the country. The report also proposes that Japan's new health system should continue to value equality and solidarity, while recognising individual patient priorities and values and incorporating global health perspectives. The report further suggests a shift in focus from inputs to outcomes. The system should redirect attention from the quantity of services provided to the quality of care, from cure to health maintenance and wellbeing, from central regulation to professional self-regulation, and from specialisation of services to integrated approaches across medical and social service sectors.30
Gaps in life expectancy and HALE between prefectures have widened from 2·5 to 3·1 years in 1990 and from 2·3 to 2·7 years in 2015 (appendix pp 26–31). Consistent with other analyses,14 a broad tendency of higher mortality was observed in the north. Age-standardised mortality reduction between 1990 and 2015 varied across the prefectures. These results could indicate an unequal health transition in the past 2 decades across Japan, and regional variations in national and local public health policy and strategy should therefore be addressed.
Many disabling conditions that predominantly lead to DALYs but do not cause substantial death, such as low back and neck pain, and depressive disorders, had no distinct patterns across the prefectures. This low regional variation might be an artifact of our limited coverage of subnational data sources for Japan. Nevertheless, many of the leading causes of mortality and YLLs, including cerebrovascular disease, ischaemic heart diseases, and self-harm showed remarkable variations by prefecture (appendix p 2). In view of the prominence of the different variation patterns in causes across regions, cause-specific and region-specific health interventions might need to be addressed in the most at-risk prefectures to deal with regional variations.
Several plausible mechanisms exist as to why some prefectures are achieving better health outcomes than others. First, according to the National Health and Nutrition Survey 2012, a nationwide survey conducted by the Ministry of Health, Labour and Welfare, statistically significant, slight variations by prefectures were observed in major lifestyle-associated behavioural factors (eg, salt intake and smoking) among adults aged 20 years and older.32 These variations are consistent with the patterns by geography we found in our study (higher death or DALY rates in the north, lower in the central and south). Therefore, regional variations in lifestyles might explain the regional health variations. However, importantly, our estimates showed that the contributions of such behavioural risk factors (ie, dietary risks, smoking, alcohol consumption) to DALYs as well as mortality did not vary much across the prefectures (appendix pp 3–8). This implies that regional variations in health might be driven by other unobserved factors, such as health system performance, which varies across the country.5 However, as mentioned previously, the low regional variation in risk factor contributions could be due to our poor data coverage of limited subnational data sources.
Second, a north–south gradient (lower–higher) was suggested in major proxy indicators of health system inputs, such as per capita health expenditures, and health workforce in numbers (appendix p 38), which might differentiate health outcomes across the country. However, prefecture-level associations between these health system inputs and mortality and DALYs were weak and not significant, suggesting other social determinants of health might suitably capture the regional variations in health (ie, socioeconomic and political contexts, including income and education levels23). Health-care spending is strongly linked with health conditions and varies across Japan.8, 33 In future rounds of subnational analysis for the GBD study in Japan, we plan to quantify the effect of personal health-care spending and public health spending as well as other social determinants of health on the outputs from GBD, to identify prefecture-level characteristics potentially associated with improved health outcomes.
As observed elsewhere in the world,34 the overall proportion of disease burden decreased in Japan between 1990 and 2015 largely due to a substantial decline in the incidence of preventable diseases (eg, cerebrovascular diseases, ischaemic heart diseases, lower respiratory infection, and some types of cancer), resulting in increased life expectancy. However, these diseases remained top causes of death and DALYs in 2015, which underlines the need to scale up effective coverage of preventive and public health measures nationally, such as screening and risk factor reduction to tackle the continuing burden of preventable diseases. Simultaneously, the scale-up of preventive measures should raise debates on investment in comparative cost-effectiveness assessment of policies and programmes to aid decision making.
In Japan, in 2015, behavioural risk factors made a greater contribution to both DALYs (25·2%) and mortality (33·7%) than did metabolic risks (DALYs 16·4%; mortality 24·5%) or environmental and occupational risks (DALYs 4·4%; mortality 6·7%). Unhealthy diets (particularly diets high in salt) and tobacco smoking were the two most important behavioural risk factors for many health conditions.
Smoking also increases the probability of many of serious clinical conditions.35, 36, 37 In 2017, Japan is expected to pass its strictest-ever smoking laws that would ban smoking on the premises of public facilities, such as restaurants, pubs, hospitals, and municipal offices. However, opposition is mounting from members of parliament. A group of parliamentarians has suggested that Japan should instead focus on smoke segregation policies that divide smoking and non-smoking areas in public places (ie, designated smoking rooms), which is not in line with the 2010 agreement adopted by WHO and the International Olympic Committee. Japan is responsible for hosting a smoke-free Olympics Games in 2020.38
In view of our findings, addressing of these modifiable risk factors throughout an individual's life (namely risk factor approach) within national and local public health policies and strategies could enable the whole population to age better than in the past and maximise their health and longevity. More importantly, the contributions of these modifiable behavioural risk factors to DALYs and mortality did not vary much across the prefectures (appendix pp 3–8), implying that national systematic action could make a significant difference.
To our knowledge, this study is the first to provide a comprehensive picture of disease burden and patterns in Japan and prefectures—the country with the fastest ageing population in the world. Our subnational estimates of disease burden are the first and crucial step toward a greater understanding of prefecture-specific health priorities aligned to national and local health policy and programme implementations. Our study, therefore, can help not only guide policy agendas and programme implementation, and facilitate intervention prioritisation, nationally and locally, to further improve the population health in Japan but also identify particular regions in the county where more targeted policy attention might be required.
Our analyses are, however, subject to the same limitations described for GBD 2015,15, 16, 17, 18, 39 as well as specific limitations associated with data availability for Japan. First, we had limited data access to up-to-date vital data, especially cause of death. Registration of death that occurred in Japan is a legal requirement. Therefore, we assumed mortality data were complete. However, a time lag between data registration and becoming available in databases exists. Second, sources of subnational data are not available at the prefecture level for the estimates of prevalence and incidence for several diseases as well as their risk factors. Our subnational estimates depend on the GBD Bayesian models, which allow for borrowing strength from other studies while using available covariates as predictors for imputing the missing data. Addressing of the sparse availability of individual-level morbidity data, such as patient records (ie, hospital inpatient and outpatient data) by prefecture will substantially improve future analytic efforts. Finally, as with other GBD studies reported elsewhere, the relative ranking across causes and risk factors are dependent on the level of their aggregation. Online data visualisations provide access to results based on different levels of the GBD 2015 hierarchy of causes and risk factors, including a complete set of age-specific, gender-specific, cause-specific, and prefecture-specific estimates of GBD outputs from 1990 until 2015.
Our study showed that health in Japan has been improving and life expectancy is rising because of the successful reduction in mortality and disability from most preventable diseases, such as cerebrovascular diseases, ischaemic heart diseases, lower respiratory infection, and some cancers that were previously severe and often fatal. However, the progress in population health has slowed down and variation in health is growing between prefectures for many leading causes. National and local health policies should therefore address region-specific health interventions to deal with these variations. The subnational health system inputs were not obviously associated with health outcomes, suggesting they are weakly associated with regional health variations. Therefore, the potential sources of the regional health variations, including subnational health system performance, need assessment.
This online publication has been corrected. The corrected version first appeared at thelancet.com on Sept 21, 2017
Acknowledgments
Acknowledgments
This work was conducted as part of the Global Burden of Diseases, Injuries, and Risk Factors Study 2015 (GBD 2015), which was primarily funded by the Bill & Melinda Gates Foundation. This work was also partly funded by research grants from the Ministry of Education, Science, Sports and Culture of Japan (16H02643), the Ministry of Health, Labour and Welfare, Japan (H26-chikyukibo-ippan-001), AXA CR Fixed Income Fund, and AXA Research Fund. The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The views expressed in this paper are solely those of the authors.
Contributors
All authors contributed to the draft, and have seen and approved the final version of the report.
Declaration of interests
KS reports grants from the Ministry of Health, Labour and Welfare of Japan, grants from the Ministry of Education, Science, Sports and Culture of Japan, grants from the AXA CR Fixed Income Fund, grants from the AXA Research Fund, during the conduct of the study. NJK reports personal fees and nonfinancial support from Vifor Pharmaceuticals, outside the submitted work. NoK reports personal fees from Junpukai Foundation, Softbank, and Infosoft Technologies outside the submitted work. MI reports a financial contribution from the AXA Research Fund as chair-holder of the AXA Department of Health and Human Security, Graduate School of Medicine, The University of Tokyo. All other authors declare no competing interests.
Supplementary Material
References
- 1.Ministry of Health. Labour and Welfare Overview of vital statistics in 2015. 2016. http://www.mhlw.go.jp/toukei/saikin/hw/jinkou/kakutei15/index.html (accessed April 20, 2017).
- 2.Statistics Bureau Population estimates by age (5-Year Age Group) and sex. 2016. http://www.stat.go.jp/english/data/jinsui/tsuki/index.htm (accessed April 20, 2017).
- 3.OECD . OECD Factbook: Economic, Environmental and Social Statistics. 2015–2016. Organisation for Economic, Co-operation Development; Paris: 2016. [Google Scholar]
- 4.Statistics Bureau Chapter 2 Population and Households. 2017. http://www.stat.go.jp/english/data/nenkan/66nenkan/14310-2.htm (accessed April 20, 2017).
- 5.Ikegami N, Yoo BK, Hashimoto H. Japanese universal health coverage: evolution, achievements, and challenges. Lancet. 2011;378:1106–1115. doi: 10.1016/S0140-6736(11)60828-3. [DOI] [PubMed] [Google Scholar]
- 6.Ministry of Health. Labour and Welfare Health Japan 21 (the second term) http://www.mhlw.go.jp/seisakunitsuite/bunya/kenkou_iryou/kenkou/kenkounippon21/en/kenkounippon21/ (accessed April 20, 2017).
- 7.Ministry of Health. Labor and Welfare . Annual Health, Labour and Welfare Report (2016 edition): consider a social model which overcomes the aging of the population [Japanese] Ministry of Health, Labor and Welfare; Tokyo: 2016. [Google Scholar]
- 8.Tsugawa Y, Hasegawa K, Hiraide A, Jha AK. Regional health expenditure and health outcomes after out-of-hospital cardiac arrest in Japan: an observational study. BMJ Open. 2015;5:e008374. doi: 10.1136/bmjopen-2015-008374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fukuda Y, Nakamura K, Takano T. Cause-specific mortality differences across socioeconomic position of municipalities in Japan, 1973–1977 and 1993–1998: increased importance of injury and suicide in inequality for ages under 75. Int J Epidemiol. 2005;34:1009. doi: 10.1093/ije/dyh283. [DOI] [PubMed] [Google Scholar]
- 10.Fukuda Y, Nakamura K, Takano T. Socioeconomic pattern of smoking in Japan: income inequality and gender and age differences. Ann Epidemiol. 2005;15:365–372. doi: 10.1016/j.annepidem.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 11.Newton JN, Briggs ADM, Murray CJL. Changes in health in England, with analysis by English regions and areas of deprivation, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:2257–2274. doi: 10.1016/S0140-6736(15)00195-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gómez-Dantés H, Fullman N, Lamadrid-Figueroa H. Dissonant health transition in the states of Mexico, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2016;388:2386–2402. doi: 10.1016/S0140-6736(16)31773-1. [DOI] [PubMed] [Google Scholar]
- 13.Zhou M, Wang H, Zhu J. Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387:251–272. doi: 10.1016/S0140-6736(15)00551-6. [DOI] [PubMed] [Google Scholar]
- 14.Gilmour S, Liao Y, Bilano V, Shibuya K. Burden of disease in Japan: using national and subnational data to inform local health policy. J Prev Med Public Health. 2014;47:136–143. doi: 10.3961/jpmph.2014.47.3.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.GBD 2015 Mortality and Causes of Death Collaborators Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1459–1464. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.GBD 2015 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–1562. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.GBD 2015 DALYs and HALE Collaborators Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1603–1605. doi: 10.1016/S0140-6736(16)31460-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.GBD 2015 Risk Factors Collaborators Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1659–1667. doi: 10.1016/S0140-6736(16)31679-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Foreman KJ, Lozano R, Lopez AD, Murray CJ. Modeling causes of death: an integrated approach using CODEm. Popul Health Metr. 2012;10:1. doi: 10.1186/1478-7954-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Naghavi M, Makela S, Foreman K, O'Brien J, Pourmalek F, Lozano R. Algorithms for enhancing public health utility of national causes-of-death data. Popul Health Metr. 2010;8:9. doi: 10.1186/1478-7954-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beltran-Sanchez H, Preston SH, Canudas-Romo V. An integrated approach to cause-of-death analysis: cause-deleted life tables and decompositions of life expectancy. Demogr Res. 2008;19:1323–1350. doi: 10.4054/DemRes.2008.19.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salomon JA, Haagsma JA, Davis A. Disability weights for the Global Burden of Disease 2013 study. Lancet Glob Health. 2015;3:e7122–e7123. doi: 10.1016/S2214-109X(15)00069-8. [DOI] [PubMed] [Google Scholar]
- 23.Solar O, Irwin A. A conceptual framework for action on the social determinants of health—social determinants of health discussion paper 2 (policy and practice) World Health Organization; Geneva: 2010. [Google Scholar]
- 24.Ministry of Health. Labour and Welfare Health expenditure database [Japanese] http://www.mhlw.go.jp/bunya/iryouhoken/iryouhoken03/01.html (accessed April 20, 2017).
- 25.Ministry of Health. Labour and Welfare Overview of the survey on physicians, dentists, and pharmacists in 2014 [Japanese] 2015. http://www.mhlw.go.jp/toukei/saikin/hw/ishi/14/index.html (accessed April 20, 2017).
- 26.Ministry of Health. Labour and Welfare Overview of report on public health admministration and services (practicing health professionals) in 2014 [Japanese] 2015. http://www.mhlw.go.jp/toukei/saikin/hw/eisei/14/ (accessed April 20, 2017).
- 27.WHO . World Health Statistics 2015. World Health Organization; Geneva: 2015. [Google Scholar]
- 28.Vital, Health and Social Statistics Office Vital statistics [Japanese] http://www.mhlw.go.jp/toukei/list/811-a.html (accessed April 20, 2017).
- 29.National Police Agency . Damage situation and police countermeasures associated with 2011 Tohoku district—off the Pacific Ocean Earthquake. National Police Agency; Tokyo: 2016. [Google Scholar]
- 30.Miyata H, Ezoe S, Hori M. Japan's vision for health care in 2035. Lancet. 2015;385:2549–2555. doi: 10.1016/S0140-6736(15)61135-7. [DOI] [PubMed] [Google Scholar]
- 31.Reich MR, Shibuya K. The future of Japan's health system—sustaining good health with equity at low cost. N Engl J Med. 2015;373:1793–1797. doi: 10.1056/NEJMp1410676. [DOI] [PubMed] [Google Scholar]
- 32.Ministry of Health. Labour and Welfare Prefecture-specific results of the National Health and Nutrition Survey in 2012 (in Japanese) 2012. http://www.mhlw.go.jp/bunya/kenkou/eiyou/dl/h24-houkoku-07.pdf (accessed April 20, 2017).
- 33.Dieleman JL, Baral R, Birger M. US spending on personal health care and public health, 19962–013. JAMA. 2016;316:2627–2646. doi: 10.1001/jama.2016.16885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bongaarts J. Trends in causes of death in low-mortality countries: implications for mortality projections. Popul Dev Rev. 2014;40:189–212. [Google Scholar]
- 35.Pearson TA, Blair SN, Daniels SR. AHA guidelines for primary prevention of cardiovascular disease and stroke: 2002 update: consensus panel guide to comprehensive risk reduction for adult patients without coronary or other atherosclerotic vascular diseases. american heart association science advisory and coordinating committee. Circulation. 2002;106:388–391. doi: 10.1161/01.cir.0000020190.45892.75. [DOI] [PubMed] [Google Scholar]
- 36.Vineis P, Alavanja M, Buffler P. Tobacco and cancer: recent epidemiological evidence. J Natl Cancer Inst. 2004;96:99–106. doi: 10.1093/jnci/djh014. [DOI] [PubMed] [Google Scholar]
- 37.Centers for Disease C, Prevention Smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 20002–004. MMWR Morb Mortal Wkly Rep. 2008;57:1226–1228. [PubMed] [Google Scholar]
- 38.The Japan Times Japan's tobacco lobby fires up as government pushes ahead with tougher smoking laws. 2017. http://www.japantimes.co.jp/news/2017/03/13/national/social-issues/japans-tobacco-lobby-fires-government-pushes-ahead-tougher-smoking-laws/ (accessed May 1, 2017).
- 39.GBD 2015 Child Mortality Collaborators Global, regional, national, and selected subnational levels of stillbirths, neonatal, infant, and under-5 mortality, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1725–1774. doi: 10.1016/S0140-6736(16)31575-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.