Abstract
The rarely seen eruptive syringoma (ES) is characterized by small, skin-colored, papules. Lesions are benign; however, treatment is often unsuccessful. Recent studies have a suggested role of the autoimmune response, rather than reactive proliferation of acrosyringium in the pathogenesis of ES. There are reports in the literature of an association between syringoma and diabetes mellitus as well as alopecia areata, which support a theory of an autoimmune role; however, there has been no report of coexistence of ES and vitiligo thus far. Presently described is a case of bilateral nipple vitiligo and eruptive syringoma in a 29-year old female.
Keywords: Autoimmunity, syringoma, vitiligo
Syringomas are benign adnexal tumors originating from the eccrine sweat glands. They usually appear as several small, round, smooth-surfaced, yellowish, papules. They are often located on the face and around the eyelids [1]. Eruptive syringoma (ES), occurring more often in puberty and adolescence, presents as multiple papules, often located on the trunk [1, 2]. Although ES may appear to be simple, lesions may be confused with acne vulgaris, sebaceous hyperplasia, eruptive xanthoma, Darier’s disease, Fox-Fordyce disease, verruca plana, lichen planus, mastocytosis, granuloma annulare, lichen nitidus, pseudoxanthoma elasticum, trichoepithelioma or sarcoidosis [1–3].
The case of a 29-year-old female with bilateral vitiligo localized to bilateral breast areolae and coexisting eruptive syringoma is presently described.
CASE REPORT
A 29-year-old female patient presented at the outpatient clinic with complaints of depigmentation on bilateral nipples that appeared during childhood and yellow-brown papules proliferating over time on the trunk and face. She had no complaints other than for cosmetic reasons. The patient reported that approximately 2 years after nipple depigmentation, yellow-brown lesions began to spread from front part of the chest to the lower part of the abdomen and to the face, including the eyelids. There was nothing noteworthy in the past medical history of the patient. Family history revealed that her sister was being followed-up with diagnosis of morphea. Systemic inquiry and physical examination were normal. Dermatological examination revealed some skin-colored lesions around the eyes, and multiple, yellow-brown pigmented papular lesions under the chin, on the neck, the trunk, on both breasts (Figure 1 A–C), and the abdomen measuring 1 to 5 mm in diameter (Figure 2 A–C). Some hypo-pigmented patches were observed on the bilateral areolae and Wood’s lamp examination was consistent with vitiligo. The patient refused biopsy from areola region.
Figure 1.
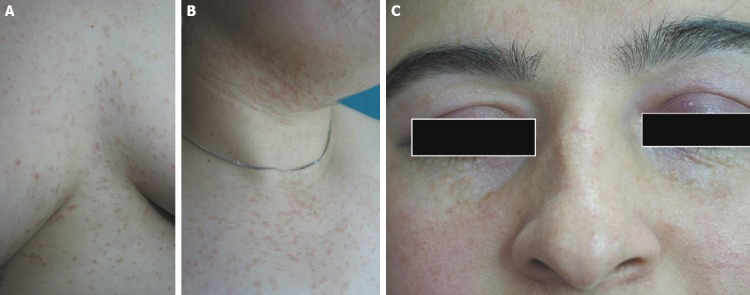
(A, B, C) Multiple syringomas located near the eyes, on the neck, and on the thorax.
Figure 2.
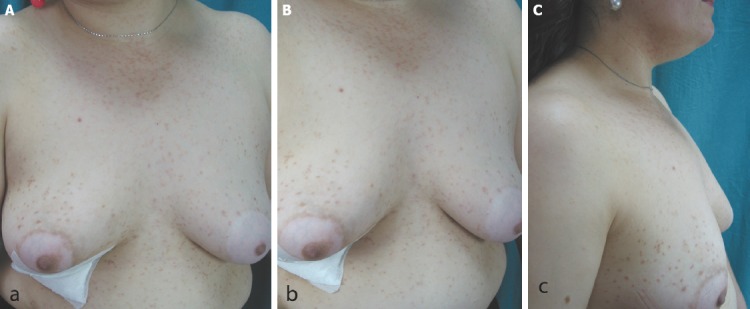
(A, B, C) Coexistence of bilateral nipple areolae vitiligo and eruptive syringoma.
No abnormality was detected in the laboratory test results (complete blood count, biochemical parameters, blood glucose, glycated hemoglobin, and extractable nuclear antigen antibody profiles).
A 4-mm punch biopsy was taken from papular lesions on front of the chest with prediagnosis of eruptive histiocytosis, eruptive xanthoma, eruptive lichen, urticaria pigmentosa and syringoma. Histopathological examination established diagnosis of syringoma by determining dilated cystic cavities lined with epithelial and cuboidal cells (Figure 3 A, B).
Figure 3.
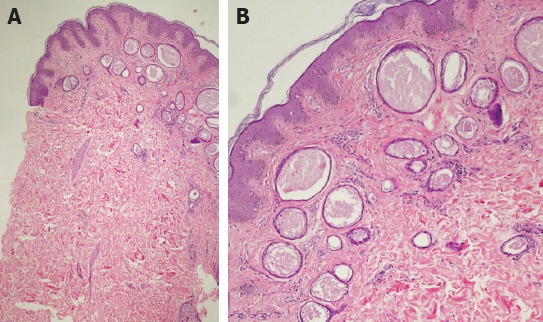
(A, B) Diagnosis of syringoma was established in the histopathological examination by determining dilated cystic cavities lined with epithelial and cuboidal cells (H&E x100, x200).
Based on assessment of clinical and histopathological findings, the patient was diagnosed with ES.
Cryotherapy was performed twice for 5 seconds to all lesions separately to create double freeze-thaw cycle, but there was no satisfactory response. Topical tretinoin and systemic isotretinoin 20 mg for 6 months also resulted in only slight flattening of lesions (Figure 4 A, B).
Figure 4.
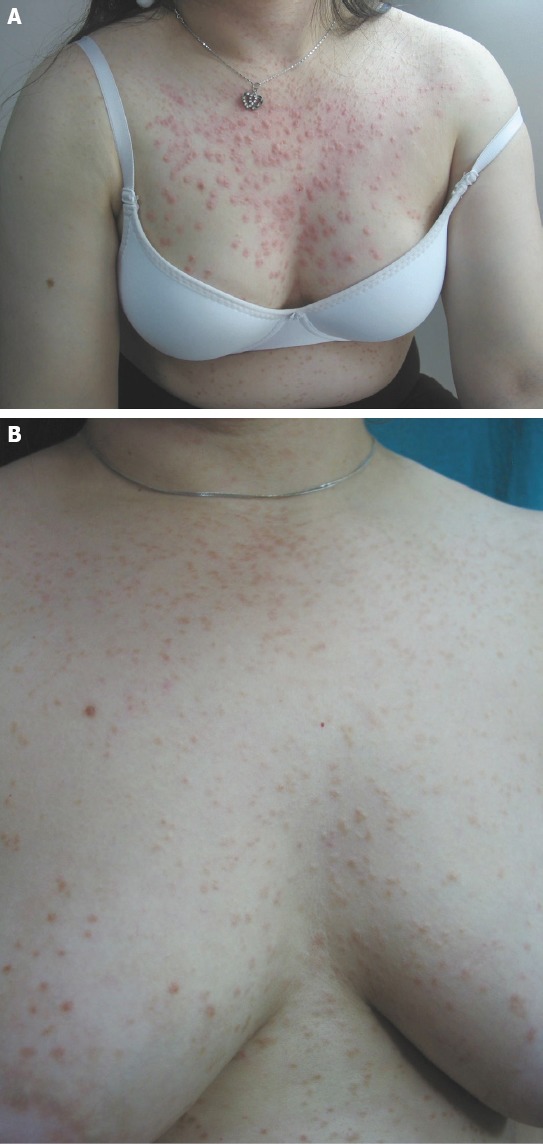
(A) Edema and erythema after cryosurgery. (B) Partial remission after therapy.
DISCUSSION
Syringomas are benign eccrine sweat gland tumors with a frequency in the population of 0.6%. Females are affected by syringomas more often than males. The clinical appearance of syringomas is typically several, asymptomatic, small, round, smooth-surfaced, yellowish papules. They are more commonly located on the face and around the eyelids, less often in the genital area, on the scalp, the neck, the trunk, or the armpits [1–3]. Tumors mostly occur in adolescence and may increase in number with age. Friedman and Butler distinguished 4 clinical variants of syringoma: a localized form, a form associated with Down’s syndrome, a familial form, and a form that encompasses ES [3].
ES, first described by Darier and Jaquet, is rare variant of syringoma and is characterized by multiple papules occurring in puberty and in adolescence, usually located on the trunk [3]. Histopathology of syringoma reveals ductal structures that are usually lined by 2 rows of cuboidal-to-flattened epithelial cells in the upper and middle dermis embedded in sclerotic stroma, and some ducts have elongated tails of epithelial cells that produce the characteristic comma-shaped or tadpole appearance [1, 2]. Histopathology examination of papular lesions on the trunk of our patient was consistent with syringoma.
ES is disease of unknown pathogenesis that may have a sporadic or hereditary etiology. Diseases reported to be associated with ES include trisomy 21, Marfan syndrome, Ehler-Danlos syndrome, sarcoidosis, diabetes mellitus, cicatricial alopecia, and alopecia areata [2–6]. Some authors have reported that in the etiology of the disease, the inflammatory process leads to syringoma by evoking a hyperplasic response in the eccrine glands [2, 7, 8].
Vitiligo is known as pigmentary disorder of the skin and mucous membranes. Autoimmune mechanisms, neural interaction, and cytotoxicity are focuses of etiology. Diseases associated with vitiligo include autoimmune diseases, such as Hashimoto’s thyroiditis, pernicious anemia, alopecia areata, morphea, and diabetes mellitus [9]. It has been suggested that the disease occurs as result of melanocytes targeted by autoantibodies produced by these diseases. Damage to melanocytes may also be induced by autocytotoxic effect occurring in response to viral or other triggering factors [9]. Reports on an association of other autoimmune diseases with ES and vitiligo suggest that, as in our case, coexistence of vitiligo and ES may be result of common immunopathogenesis. In our patient, lesions of vitiligo on the nipples developed first, subsequently followed by syringomas. We believe that the inflammatory response leading to vitiligo also gave rise to syringoma by evoking a hyperplasic response to acrosyringium. In our patient, because evident inflammatory cell infiltration was not observed around the eccrine glands on histological examination, non-cell-dependent immune response mechanisms may have played a role in incidence of these 2 conditions.
To our knowledge, no association of ES and vitiligo has been reported in the literature. Although patients with vitiligo and syringoma were encountered in studies dermatologically assessing patients with Down’s syndrome, an association of the 2 diseases was not mentioned [10].
For the first time, we report case of coexisting vitiligo and ES. It is thought that the inflammatory process caused by a factor or factors that triggered vitiligo may have given rise to ES.
Footnotes
Conflict of Interest: None declared.
Financial Disclosure: The authors declared that this study has received no financial support.
Authorship contributions: Concept – S.Y., N.D., P.G.; Design – S.Y., N.D., P.G.; Supervision – S.Y., N.D., P.G.; Materials – S.Y., N.D., P.G.; Data collection &/or processing – S.Y., N.D., P.G.; Literature search – S.Y., N.D., P.G.; Writing – S.Y., N.D., P.G.; Critical review – S.Y., N.D., P.G.
REFERENCES
- 1.Thomas VD, Swanson NA, Lee KK. Benign epithelial tumors, hamartomas and hyperplasias. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Pallers AS, Lefell DJ, et al., editors. Fitzpatrick's Dermatology in general medicine. 7th ed. New York: McGraw Hill; 2008. pp. 1054–67. [Google Scholar]
- 2.Soler-Carrillo J, Estrach T, Mascaró JM. Eruptive syringoma:27 new cases and review of the literature. J Eur Acad Dermatol Venereol. 2001;15:242–6. doi: 10.1046/j.1468-3083.2001.00235.x. [DOI] [PubMed] [Google Scholar]
- 3.Jamalipour M, Heidarpour M, Rajabi P. Generalized eruptive syringomas. Indian J Dermatol. 2009;54:65–7. doi: 10.4103/0019-5154.48992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Janniger CK, Brodkin RH. Eruptive syringomas. Cutis. 1990;46:247–9. [PubMed] [Google Scholar]
- 5.Urban CD, Cannon JR, Cole RD. Eruptive syringomas in Down's syndrome. Arch Dermatol. 1981;117:374–5. [PubMed] [Google Scholar]
- 6.Barnhill RL, Goldberg B, Stenn KS. Proliferation of eccrine sweat ducts associated with alopecia areata. J Cutan Pathol. 1988;15:36–9. doi: 10.1111/j.1600-0560.1988.tb00513.x. [DOI] [PubMed] [Google Scholar]
- 7.Guitart J, Rosenbaum MM, Requena L. 'Eruptive syringoma': a misnomer for a reactive eccrine gland ductal proliferation? J Cutan Pathol. 2003;30:202–5. doi: 10.1034/j.1600-0560.2003.00023.x. [DOI] [PubMed] [Google Scholar]
- 8.Dyall-Smith DJ, Connors TJ, Scurry J. Generalised eruptive syringoma--a papular dermatosis. Australas J Dermatol. 1990;31:95–8. doi: 10.1111/j.1440-0960.1990.tb00661.x. [DOI] [PubMed] [Google Scholar]
- 9.Sehgal VN, Srivastava G. Vitiligo: auto-immunity and immune responses. Int J Dermatol. 2006;45:583–90. doi: 10.1111/j.1365-4632.2005.02651.x. [DOI] [PubMed] [Google Scholar]
- 10.Daneshpazhooh M, Nazemi TM, Bigdeloo L, Yoosefi M. Mucocutaneous findings in 100 children with Down syndrome. Pediatr Dermatol. 2007;24:317–20. doi: 10.1111/j.1525-1470.2007.00412.x. [DOI] [PubMed] [Google Scholar]


