Abstract
Objective:
The objective of the study was to evaluate the etiology of hospital-acquired hyponatremia (HAH) and its effects on morbidity and mortality in the Pediatric Intensive Care Unit (PICU) patients.
Design:
This study design was a prospective observational case–control study.
Setting:
this study was conducted at tertiary care PICU.
Materials and Methods:
All consecutive cases admitted with at least one measured serum sodium (PNa) value were evaluated. Those with normal admission PNa were followed till they develop hyponatremia (PNa < 35 mEq/L) 7 days or PICU discharge whichever was earlier.
Results:
During the study period, 123 (19.6%) cases developed HAH and 126 patients remained isonatremic (control group). The admission PNa 138.8 ± 3.03 mEq/L decreased to 132 ± 2.58 mEq/L (drop of 6.68 ± 3.39 mEq/L, P < 0.001) in HAH cases. The use of antidiuretic hormone (ADH)-stimulating drugs (odds ratio [OR]: 2.83, P = 0.01), postsurgical status (OR: 2.95, P = 0.006), and fluid intake ml/kg (OR: 1.0, P = 0.001) were found to be significant risk factors in HAH group on multivariate analysis. HAH cases had prolonged PICU stay (P = 0.000) and mechanical ventilation (P = 0.01), but no difference in the mortality when compared to controls.
Conclusions:
HAH is associated with increased fluid intake, presence of ADH-stimulating drugs or conditions, and postsurgical status and has an adverse effect on the outcome of PICU patients.
Keywords: Antidiuretic hormone, dysnatremia, hyponatremia intravenous fluid, pediatric intensive care, sodium
INTRODUCTION
Hyponatremia (serum sodium [PNa] <135 mEq/L) is more frequent electrolyte abnormality in hospitalized patients and is associated with increased morbidity and mortality.[1,2] Hyponatremic patients are more likely to require intensive care, mechanical ventilation, and have significantly higher chances of increased length of stay, treatment costs, and mortality (3 times compared to patients with normal PNa).[3,4,5]
Most of the previous studies evaluating incidence of hospital-acquired hyponatremia (HAH) in adult ICUs have shown an incidence of 20%–30% and have also reported poor morbidity and mortality.[6,7,8,9]
Depending on the definition of hyponatremia, the reported incidence of HAH in children varies between 10%–50% in various studies and with significant morbidity and mortality.[10,11,12,13,14,15] Majority of patients included in these studies were those admitted in pediatric wards and emergency units. Studies from Pediatric Intensive Care Unit (PICU) on postoperative patients have focused primarily on the effects of hypotonic fluid on serum sodium.[16,17,18]
To the best of our knowledge, there are no studies done to comprehensively evaluate the incidence, etiology, and impact on the outcome of HAH in critically sick children. Hence, in the present study, we aim to investigate the incidence, etiological characteristics, and effect of HAH on the outcome of PICU patients.
MATERIALS AND METHODS
This prospective, observational, case–control study was conducted over a year in the PICU of a tertiary care teaching hospital. Institutional Research Ethics Board approved the study. Written informed consent was obtained from parents or guardians for all participants, and assent was obtained from children over 7 years of age if appropriate.
Data collection
The sample size was calculated to estimate the number of patients required to calculate the incidence of HAH. With 9.3% incidence of HAH as per the previous study, an error of 2.5%, and confidence interval of 95%, the estimated sample size was 610.[10] All children between the age group of 1 month to 16 years who received intravenous fluid (IVF) with at least one measured PNa value at admission were included in the study. All PNa levels were measured by direct ion selective electrode method. Patients with hyponatremia or hypernatremia at admission were excluded from the study. As per the unit protocol, blood chemistries were monitored 12 hourly. Patients with normal PNa at admission were further followed till they developed hyponatremia (PNa < 135 mEq/L) for a maximum of 7 days or PICU discharge whichever was earlier. Those who developed hypernatremia (PNa > 145 mEq/L) and without follow-up PNa values were excluded from the study [Figure 1].
Figure 1.
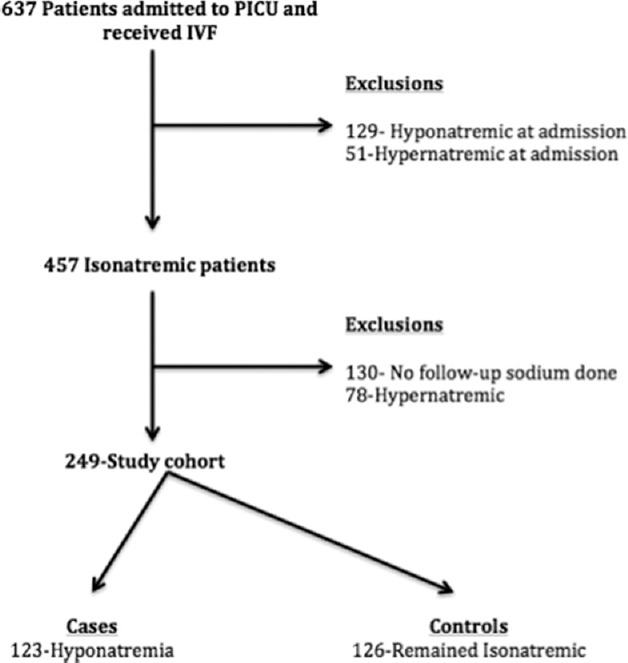
Study flowchart
The following data were recorded for the enrolled cohort: age, gender, weight, diagnosis, renal function tests, liver function tests, and random blood sugar levels. The total intake (oral and type and volume of IVF), output, and net balance were recorded. Other parameters such as the presence of antidiuretic hormone (ADH)-stimulating clinical condition, ADH-stimulating drugs, postsurgical state, and the use of 3% saline were recorded.
As per the unit protocol, half-normal saline (0.45% with 5% dextrose), 0.9% saline with dextrose (DNS), and normal saline were used as the standard maintenance IVF in age groups <2 and >2 years, respectively. The volume of maintenance IVF requirement was according to Holliday-Segar formula.
Other parameters such as the use of inotropes, length of stay in PICU, total ventilator days, and final outcome (survival/death) were also recorded. As per the unit protocol for the management of HAH patients, we also did serum osmolality and urinary osmolality, sodium and creatinine to evaluate the sodium excretion status, and rule out pseudohyponatremia. The levels of serum ADH could not be estimated due to the financial constraints.
Definitions
Hyponatremia and hypernatremia were defined as PNa <135 mEq/L and >145 mEq/L, respectively. HAH was defined as at least one documented value of PNa <135 mEq/L during the hospital stay, at least 12 h after admission in those with normal PNa (135–145 mEq/L) at admission. Acute hyponatremia was defined as the development of hyponatremia within 48 h of admission. Hyponatremia was classified into mild (PNa <131–134 mEq/L), moderate (PNa130–125 mEq/L), and severe hyponatremia (PNa <125 mEq/L).
Statistical analysis
Data were compiled in an Excel spreadsheet, and statistical analysis was done using SPSS version 23, Chicago, IL, USA. The mean, median, and standard deviation were calculated for the baseline characteristics and other continuous parameters. The Chi-square or Fisher's exact test was used to compare groups with respect to categorical data. Student's t-test or ANOVA was used to compare the association between groups with respect to continuous data following normal distribution otherwise Mann–Whitney U-test was used. The factors, which were significant in univariate analysis, were considered for multivariate analysis. Using step-wise logistic regression modeling, we built a final multivariable model evaluating the effect of each variable on the development of hyponatremia. To compare the durations of mechanical ventilation and PICU stay of study cases and controls, Kaplan–Meier curves were plotted. For all the comparisons, the 5% probability level (P < 0.05) was considered statistically significant.
RESULTS
A total of 637 patients were admitted to the PICU during the study period of 1 year and 457 patients were isonatremic at the time of admission. HAH was observed in 123 (19.3%) patients [Figure 1]. The admission PNa was 138.7 ± 2.97 mEq/L in these patients which decreased to 132.0 ± 2.5 mEq/L (difference - 6.6 ± 3.8 mEq/L; P < 0.001). Acute hyponatremia was seen in 64 (52%) patients. Twenty-two (17.9%) patients had moderate-to-severe hyponatremia whereas rest had mild hyponatremia. Of the hyponatremic group patients, 82 (66.7%) received N/2 whereas rest received NS and DNS. The baseline characteristics were comparable between the two groups [Table 1]. Respiratory and central nervous system disorders were the predominant disease categories in both groups [Table 2].
Table 1.
Comparison of characteristics of study cohort and controls
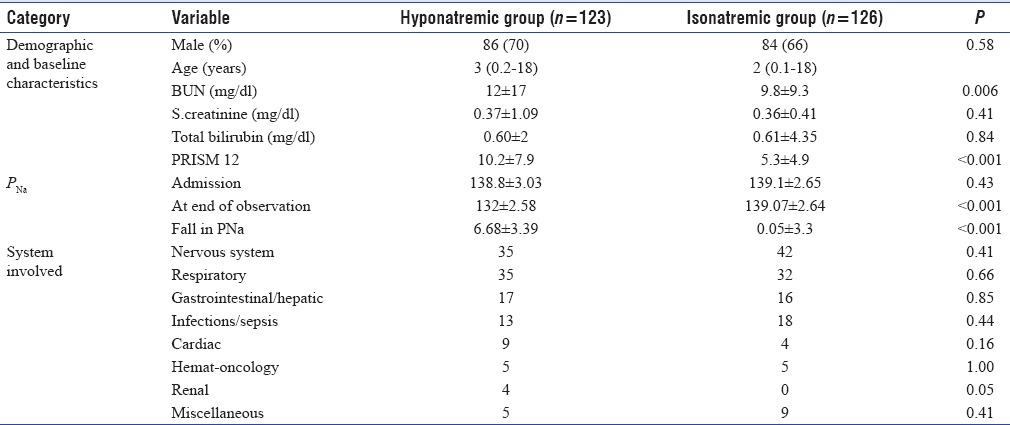
Table 2.
Frequency of ADH stimulating drugs and ADH stimulating conditions in study cohort and control group
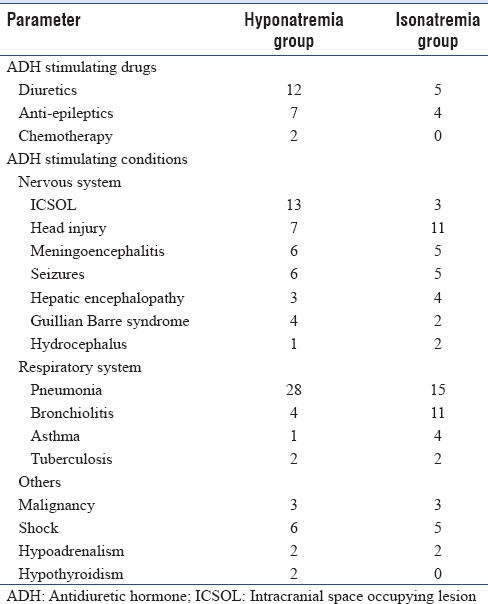
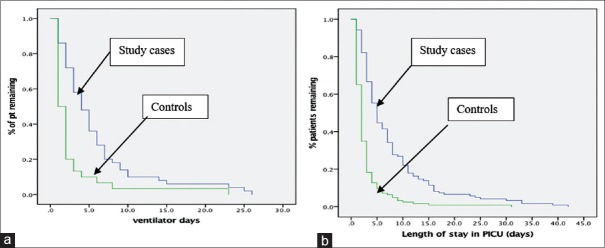
The patients in the HAH group had a higher incidence of ADH-stimulating drugs (P = 0.02), ADH-stimulating clinical conditions (P = 0.03), postsurgical status (P < 0.001), use of inotropes (P = 0.04), fluid intake (ml/kg) (P < 0.001), and output (ml/kg) (P < 0.001) than the isonatremic group on univariate analysis [Table 3]. ADH-stimulating drugs (P = 0.01), postsurgical status (P = 0.008), and input (P = 0.001) were found to be significantly different between the two groups on multivariate analysis [Table 4]. There was no significant difference in the type of IVFs received by the two groups (p-0.50). Hyponatremia developed in 82 (52%) children receiving hypotonic fluids and 41 (46%) of those receiving isotonic fluids. The patients with HAH had a longer length of stay in PICU (P < 0.001) and higher ventilator days (P = 0.01) [Figure 2]. There were three deaths in hyponatremic group and five in isonatremic patients (P = 0.72).
Table 3.
Comparison of etiological characteristics and outcome in study cohort and control cases
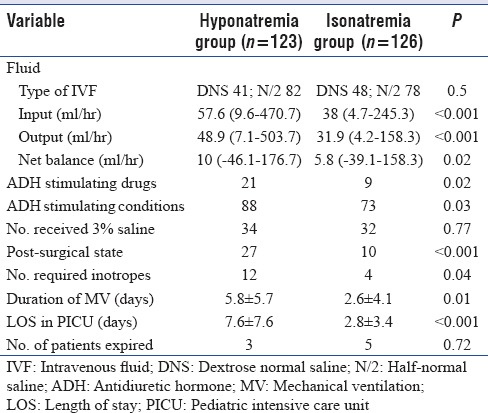
Table 4.
Multivariate analysis
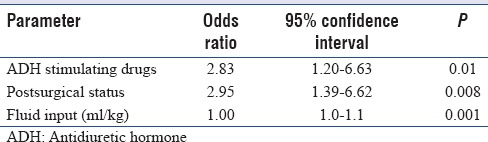
Figure 2.
Kaplan–Meier curve for duration of (a) mechanical ventilation (log rank 14.65, P = 0.01) and (b) length of stay in pediatric intensive care unit (log rank 67.22, P = 0.01) of patients with hyponatremia and isonatremia
DISCUSSION
In the present study, we found that HAH is common in the PICU patients, and postsurgical status, use of ADH-stimulating drugs, and fluid intake were significant risk factors for the development of HAH. The patients with HAH had prolonged PICU stay and longer mechanical ventilation days.
The incidence of HAH in our study was 19.3% in all the children admitted to the PICU. The incidence of HAH varies between 10% and 50% in different studies depending on the definition of hyponatremia and methodology used.[11,12,13,14,15] The incidence of HAH in our study was higher than the one reported by Hoorn et al.[10] This study evaluated patients for 48 h and included cases admitted to emergency units and pediatric wards who might be at a lower risk than patients admitted to the ICU.
The incidence of HAH in PICU patients as reported by Rey et al. and Montañana et al. was 43% and 23%, respectively, which is higher than that found in our study.[17,18] These studies were designed primarily to evaluate the effect of IVF on sodium balance. Furthermore, these studies included patients with hyponatremia at admission which probably predispose them to further hyponatremia. In our study, we included only those patients who were isonatremic at admission.
The incidence of acute hyponatremia (<48 h) in our study was 52% similar to the one seen in the study by Bibi et al. (64%).[11] Majority of the patients in our study had mild hyponatremia, 82% which is similar to those reported in studies of Bibi et al. and Luu et al. (79% and 82%, respectively).[11,15]
Various studies have shown that the use of the ADH-stimulating drugs such as diuretics, opioids, and chemotherapy drugs is known to cause hyponatremia both by virtue of their action and by stimulating ADH release.[19,20] Similarly, clinical conditions such as meningitis, intracranial tumors, head injury, pneumonia, bronchiolitis, asthma, malignancy, hypovolemia, shock, and endocrine abnormalities were associated with hyponatremia in various studies.[20,21,22] However, these conditions and drugs were present even in isonatremic patients also who did not develop hyponatremia. The subgroup analysis done for the same showed that patients in hyponatremic group had multiple risk factors such as higher PRISM score, postsurgical status, higher intake of fluid, and use of inotropes along with these factors which may explain why only these patients developed hyponatremia.
Patients in hyponatremic group had a higher intake of fluids when compared to isonatremic group which is consistent with previous studies which have shown that the presence of free water and ADH secretion are required for the development of hyponatremia.[10] Postoperative patients are predisposed to hyponatremia due to various reasons such as occult hypovolemia and nonosmotic stimuli such as nausea, vomiting, pain, anesthesia, and opioid analgesics.[23] Such patients admitted in PICU were shown to have higher chances of hyponatremia in various studies.[16,24,25,26,27] The need for inotropes indicates a state of circulatory insufficiency which may act as a stimulus for ADH secretion, thereby causing a state of increased water retention and leading to hyponatremia.
With regards to IVFs, the majority of the patients (66%) in hyponatremic group had received half-saline (0.45% NaCl with 5% dextrose), but there was no significant difference in the type of IVF used between the two groups. Even patients who received isotonic fluids had developed hyponatremia. The previous studies have shown that the use of hypotonic fluids is associated with increased risk of HAH when compared to isotonic fluids.[10,11,12,13,14,15,16,17,18] A study by Saba et al. in 2010 showed that sodium values showed a fall even in 19% of patients who received normal saline when compared to 24% in those receiving half-normal saline. They also reported that the use of half-normal saline in appropriate rate and volume has a similar risk of hyponatremia as that of normal saline.[28] Similarly, in a study by Carandang et al. in 2013, hyponatremia was seen even in 23% of children receiving isotonic fluids.[29] 3% NaCl was used in both groups as a part of standard therapy for patients with raised intracranial pressure. The use of 3% NaCl was similar in both the groups.
Children in hyponatremic group had a higher length of PICU stay and ventilator days. Previous studies done in adult ICUs have shown worse mortality and morbidity profile in hyponatremic patients.[7,8,9] Similar observations were reported by Luu et al. in children with bronchiolitis with HAH.[15]
Our study also has few limitations such as the exclusion of sources of water intake such as the amount of fluids received before PICU admission and occult sources of water-like parents giving drinks to children without informing the nurse which may not be included in the intake but affected the electrolyte balance. We could not evaluate the levels of ADH due to financial constraints, which would have helped to ascertain the status of ADH in a better manner. Furthermore, we did not estimate the urinary electrolyte and urinary osmolality profile in isonatremic patients, which could have helped us in comparing the sodium excretion state in both groups.
CONCLUSIONS
Based on our results, we conclude that HAH is common in PICU and is associated with poor morbidity profile. Based on our results, we also suggest the use of isotonic fluids alone may not completely eliminate the risk of developing hyponatremia in the presence of other risk factors. We suggest well-structured randomized control trials to assess the effect of risk factors on the development of HAH.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Anderson RJ, Chung HM, Kluge R, Schrier RW. Hyponatremia: A prospective analysis of its epidemiology and the pathogenetic role of vasopressin. Ann Intern Med. 1985;102:164–8. doi: 10.7326/0003-4819-102-2-164. [DOI] [PubMed] [Google Scholar]
- 2.Gill G, Huda B, Boyd A, Skagen K, Wile D, Watson I, et al. Characteristics and mortality of severe hyponatraemia – A hospital-based study. Clin Endocrinol (Oxf) 2006;65:246–9. doi: 10.1111/j.1365-2265.2006.02583.x. [DOI] [PubMed] [Google Scholar]
- 3.Zilberberg MD, Exuzides A, Spalding J, Foreman A, Jones AG, Colby C, et al. Epidemiology, clinical and economic outcomes of admission hyponatremia among hospitalized patients. Curr Med Res Opin. 2008;24:1601–8. doi: 10.1185/03007990802081675. [DOI] [PubMed] [Google Scholar]
- 4.Arieff AI, Ayus JC, Fraser CL. Hyponatraemia and death or permanent brain damage in healthy children. BMJ. 1992;304:1218–22. doi: 10.1136/bmj.304.6836.1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Waikar SS, Mount DB, Curhan GC. Mortality after hospitalization with mild, moderate, and severe hyponatremia. Am J Med. 2009;122:857–65. doi: 10.1016/j.amjmed.2009.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Palmer BF. Hyponatremia in the Intensive Care Unit. Semin Nephrol. 2009;29:257–70. doi: 10.1016/j.semnephrol.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 7.Arampatzis S, Frauchiger B, Fiedler GM, Leichtle AB, Buhl D, Schwarz C, et al. Characteristics, symptoms, and outcome of severe dysnatremias present on hospital admission. Am J Med. 2012;125:1125e1–e7. doi: 10.1016/j.amjmed.2012.04.041. [DOI] [PubMed] [Google Scholar]
- 8.Funk GC, Lindner G, Druml W, Metnitz B, Schwarz C, Bauer P, et al. Incidence and prognosis of dysnatremias present on ICU admission. Intensive Care Med. 2010;36:304–11. doi: 10.1007/s00134-009-1692-0. [DOI] [PubMed] [Google Scholar]
- 9.DeVita MV, Gardenswartz MH, Konecky A, Zabetakis PM. Incidence and etiology of hyponatremia in an Intensive Care Unit. Clin Nephrol. 1990;34:163–6. [PubMed] [Google Scholar]
- 10.Hoorn EJ, Geary D, Robb M, Halperin ML, Bohn D. Acute hyponatremia related to intravenous fluid administration in hospitalized children: An observational study. Pediatrics. 2004;113:1279–84. doi: 10.1542/peds.113.5.1279. [DOI] [PubMed] [Google Scholar]
- 11.Bibi S, Bibi S, Gilani SY, Shah SR, ul Haq A, Billo AG. Frequency of hospital acquired hyponatremia in a pediatric tertiary care setting. J Ayub Med Coll Abbottabad. 2015;27:560–3. [PubMed] [Google Scholar]
- 12.Armon K, Riordan A, Playfor S, Millman G, Khader A. Paediatric Research Society. Hyponatraemia and hypokalaemia during intravenous fluid administration. Arch Dis Child. 2008;93:285–7. doi: 10.1136/adc.2006.093823. [DOI] [PubMed] [Google Scholar]
- 13.Wattad A, Chiang ML, Hill LL. Hyponatremia in hospitalized children. Clin Pediatr (Phila) 1992;31:153–7. doi: 10.1177/000992289203100305. [DOI] [PubMed] [Google Scholar]
- 14.Kannan L, Lodha R, Vivekanandhan S, Bagga A, Kabra SK, Kabra M. Intravenous fluid regimen and hyponatraemia among children: A randomized controlled trial. Pediatr Nephrol. 2010;25:2303–9. doi: 10.1007/s00467-010-1600-4. [DOI] [PubMed] [Google Scholar]
- 15.Luu R, DeWitt PE, Reiter PD, Dobyns EL, Kaufman J. Hyponatremia in children with bronchiolitis admitted to the pediatric Intensive Care Unit is associated with worse outcomes. J Pediatr. 2013;163:1652–6.e1. doi: 10.1016/j.jpeds.2013.06.041. [DOI] [PubMed] [Google Scholar]
- 16.Eulmesekian PG, Pérez A, Minces PG, Bohn D. Hospital-acquired hyponatremia in postoperative pediatric patients: Prospective observational study. Pediatr Crit Care Med. 2010;11:479–83. doi: 10.1097/PCC.0b013e3181ce7154. [DOI] [PubMed] [Google Scholar]
- 17.Rey C, Los-Arcos M, Hernóndez A, Sónchez A, Díaz JJ, López-Herce J. Hypotonic versus isotonic maintenance fluids in critically ill children: A multicenter prospective randomized study. Acta Paediatr. 2011;100:1138–43. doi: 10.1111/j.1651-2227.2011.02209.x. [DOI] [PubMed] [Google Scholar]
- 18.Montañana PA, Modesto i Alapont V, Ocón AP, López PO, López Prats JL, Toledo Parreño JD. The use of isotonic fluid as maintenance therapy prevents iatrogenic hyponatremia in pediatrics: A randomized, controlled open study. Pediatr Crit Care Med. 2008;9:589–97. doi: 10.1097/PCC.0b013e31818d3192. [DOI] [PubMed] [Google Scholar]
- 19.Spital A. Diuretic-induced hyponatremia. Am J Nephrol. 1999;19:447–52. doi: 10.1159/000013496. [DOI] [PubMed] [Google Scholar]
- 20.Decaux G. The syndrome of inappropriate secretion of antidiuretic hormone (SIADH) Semin Nephrol. 2009;29:239–56. doi: 10.1016/j.semnephrol.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 21.Shann F, Germer S. Hyponatraemia associated with pneumonia or bacterial meningitis. Arch Dis Child. 1985;60:963–6. doi: 10.1136/adc.60.10.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Powell KR, Sugarman LI, Eskenazi AE, Woodin KA, Kays MA, McCormick KL, et al. Normalization of plasma arginine vasopressin concentrations when children with meningitis are given maintenance plus replacement fluid therapy. J Pediatr. 1990;117:515–22. doi: 10.1016/s0022-3476(05)80682-1. [DOI] [PubMed] [Google Scholar]
- 23.Easley D, Tillman E. Hospital-acquired hyponatremia in pediatric patients: A review of the literature. J Pediatr Pharmacol Ther. 2013;18:105–11. doi: 10.5863/1551-6776-18.2.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Choong K, Arora S, Cheng J, Farrokhyar F, Reddy D, Thabane L, et al. Hypotonic versus isotonic maintenance fluids after surgery for children: A randomized controlled trial. Pediatrics. 2011;128:857–66. doi: 10.1542/peds.2011-0415. [DOI] [PubMed] [Google Scholar]
- 25.Au AK, Ray PE, McBryde KD, Newman KD, Weinstein SL, Bell MJ. Incidence of postoperative hyponatremia and complications in critically-ill children treated with hypotonic and normotonic solutions. J Pediatr. 2008;152:33–8. doi: 10.1016/j.jpeds.2007.08.040. [DOI] [PubMed] [Google Scholar]
- 26.Singhi S. Hyponatremia in hospitalized critically ill children: Current concepts. Indian J Pediatr. 2004;71:803–7. doi: 10.1007/BF02730718. [DOI] [PubMed] [Google Scholar]
- 27.Friedman JN. Canadian Paediatric Society, Acute Care Committee. Risk of acute hyponatremia in hospitalized children and youth receiving maintenance intravenous fluids. Paediatr Child Health. 2013;18:102–7. [PMC free article] [PubMed] [Google Scholar]
- 28.Saba TG, Fairbairn J, Houghton F, Laforte D, Foster BJ. A randomized controlled trial of isotonic versus hypotonic maintenance intravenous fluids in hospitalized children. BMC Pediatr. 2011;11:82. doi: 10.1186/1471-2431-11-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carandang F, Anglemyer A, Longhurst CA, Krishnan G, Alexander SR, Kahana M, et al. Association between maintenance fluid tonicity and hospital-acquired hyponatremia. J Pediatr. 2013;163:1646–51. doi: 10.1016/j.jpeds.2013.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]