Abstract
Background:
Although scapular malpositioning is commonly associated with rotational deficits and risk of injury, modifiable causes of such malpositioning in overhead athletes are not well described.
Purpose/Hypothesis:
The purpose of this study was to examine the scapulothoracic profile of adolescent baseball players, specifically, pectoralis minor (PM) length. We hypothesized that PM would be shorter in throwing shoulders compared with nonthrowing shoulders.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
Forty-nine healthy adolescent baseball players underwent clinical screening of PM lengths in throwing and nonthrowing shoulders by means of previously described, validated techniques. PM measurements were conducted while players were supine with arms at rest, sitting with arms at rest, and sitting with shoulders in maximal external rotation; measurements were made with a digital caliper and by assessment of table-to-acromion distance. Static scapular position and range of motion measurements were recorded. Demographic information and playing history were documented.
Results:
All players were male, they had a mean ± SD age of 16.2 ± 1.16 years, and they predominantly threw right-handed (83.7%). Sixty-nine percent of players were pitchers, 61.2% had played baseball for 9 or more months per year, and 67.3% had played in excess of 30 games in the previous year. Significant differences were noted during side-to-side comparisons within participants. Absolute PM length was significantly shorter in throwing compared with nonthrowing shoulders when measured with players sitting with arms at rest (by 3.7 ± 11.8 mm) and with their shoulders in maximal external rotation (by 4.8 ± 15.1 mm) (P < .004 for both). The PM index was significantly reduced in throwing compared with nonthrowing shoulders while players were supine with arms at rest (P = .007), sitting with arms at rest (P = .006), and sitting with shoulders in maximal external rotation (P < .001). Mean table-to-acromion distance was increased 7.7 ± 1.26 mm in throwing versus nonthrowing arms (P < .001). The scapular index was significantly reduced in throwing compared with nonthrowing shoulders (P < .005).
Conclusion:
Asymptomatic adolescent baseball players have significant differences in PM length and static scapular measurements in throwing compared with nonthrowing shoulders. The clinical significance requires further investigation, but emphasis on PM stretching routines is encouraged.
Keywords: pectoralis minor length, baseball, range of motion, overuse injuries
Shoulder injuries are common in the overhead athlete, particularly the elite baseball player. Young athletes are now throwing more often and throwing harder, factors that are predictive of injury risk and subsequent surgery.12,21 Fierce competition within youth baseball encourages talented players to participate in additional training sessions, year-round playing, and multiple teams, risking overuse injuries.9
Although a variety of shoulder injuries occur in adolescent baseball players, including apophysitis, labral injury, and rotator cuff injury, predictors of these injuries are not well defined. In contrast, a large body of research has described physiologic adaptations in the glenohumeral joint and associated range of motion deficits in the professional player.5–7,14,18 The throwing arms of major league pitchers often demonstrate a uniform increase in external rotation with a corresponding decrease in internal rotation. When severe, the glenohumeral internal rotational deficit (GIRD) plays an essential role in the pathologic cascade within the shoulder and has been described as one of the primary causes of shoulder injuries.6,31
A strong clinical interest has arisen in the role of the scapula and in reliable tests that are able to detect and quantify impaired shoulder mechanics. The pectoralis minor (PM) muscle originates on ribs 3, 4, and 5 near the costosternal junction, attaches to the coracoid process of the scapula, and is the only scapulothoracic muscle with an anterior thoracic attachment.4,19 Repetitive use of the upper extremity for activities that protract and downwardly rotate the scapula may contribute to adaptive shortening of the PM, which has been associated with shoulder pain in athletes.2,11,24 Adaptive shortening of the PM can subsequently modify the resting position of the scapula, altering scapular mechanics during arm elevation.15,16 Asymmetric PM shortening has been associated with shoulder pain and disability in competitive swimmers, volleyball, and tennis players.8,10,22 A longitudinal study of collegiate volleyball players identified an increased risk of shoulder pain associated with asymmetric pectoral shortening, which was present in 63% of athletes examined.22
Although scapular malpositioning is commonly associated with rotational deficits and risk of injury, modifiable causes of this malpositioning are not well described in overhead athletes. The PM resting length may be a potential contributor to detrimental shoulder kinematics, and clinical assessment of resting length may be valuable for early intervention. The purpose of this study was to examine the scapulothoracic profile of adolescent baseball players and, in particular, PM length. We hypothesized that the PM would be shorter in throwing compared with nonthrowing shoulders.
Methods
Examination Methods
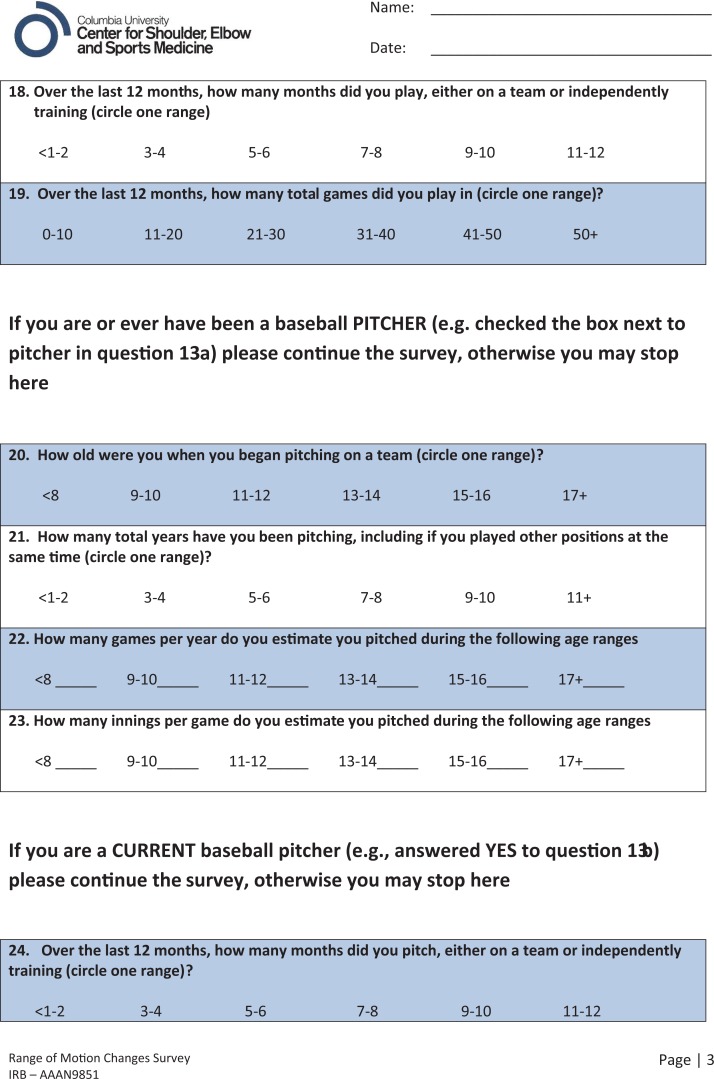
Study participants were recruited from a single baseball training facility between December 2014 and March 2015. All participants were competitive baseball players completing off-season training, and data were collected on-site at the facility. Eligible participants met the following inclusion criteria: age between 14 and 18 years, participation in organized baseball for at least 1 year, no pain in either shoulder, and completion of an online demographic survey. Prior to physical examination, all participants completed a web-based questionnaire to collect demographic information (Qualtrics) (see the Appendix). Demographic information included age, sex, throwing arm, primary position, injury history, surgery history, baseball experience, and number of games played in the past year. Measurements were performed on 56 players. Seven were unwilling to complete the survey, leaving 49 participants for study inclusion. This study was approved through the research compliance and administration system at Columbia University Medical Center.
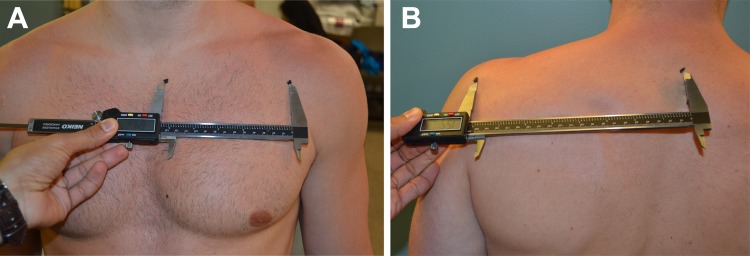
Measurements of PM length were performed in accordance with a technique that was previously validated1 and reproduced in subsequent clinical studies.8,23,26,28 This measurement method has been shown to have excellent intratester reliability, with demonstrated intraclass correlation coefficients (ICCs) of 0.96 and 0.94.1,28 PM length was estimated by the measured distance from the medial-inferior tip of the coracoid process to the inferior portion of the fourth rib, immediately lateral to the sternocostal junction (Figure 1). Measurements were taken with players supine with arms at rest, sitting with arms at rest, and sitting with shoulders in maximal external rotation. All measurements were performed with a digital vernier caliper (Neiko). Lengths were recorded as raw values and then normalized to player height to determine the relative PM length using the pectoralis minor index (PMI).1 The PMI is calculated by dividing the PM length by the patient’s height in centimeters and multiplying by 100.
Figure 1.

Measurement of pectoralis minor muscle length taken with digital vernier caliper.
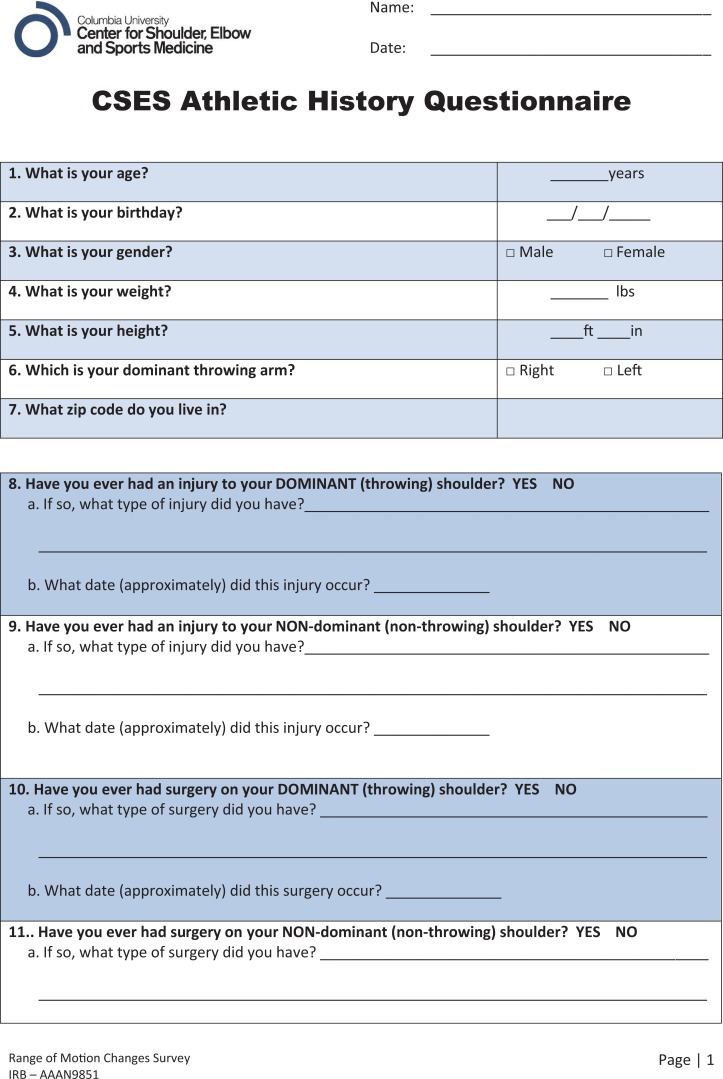
Length of the PM was indirectly measured using the table-to-acromion distance, or “tabletop test.”24 Designed to identify postural shortening of the PM, the tabletop test has been shown to have an excellent ICC.13 The player is supine with the arms at one side and elbows flexed, with the hands resting against the lateral wall of the abdomen. The investigator measures the linear distance in millimeters from the treatment table to the posterolateral acromion using a rigid transparent plastic protractor (Figure 2).
Figure 2.
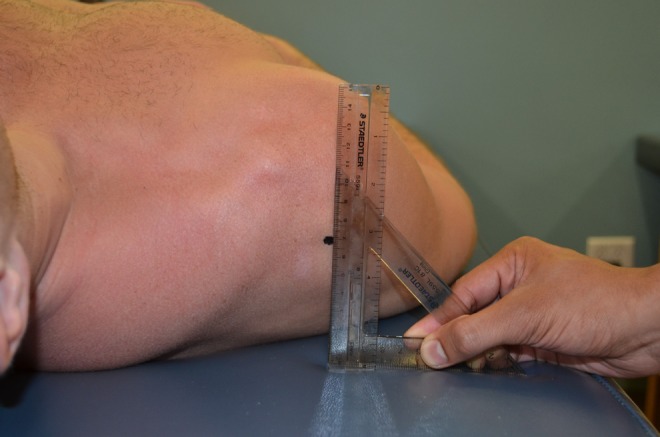
The table-to-acromion distance, or “tabletop test.”
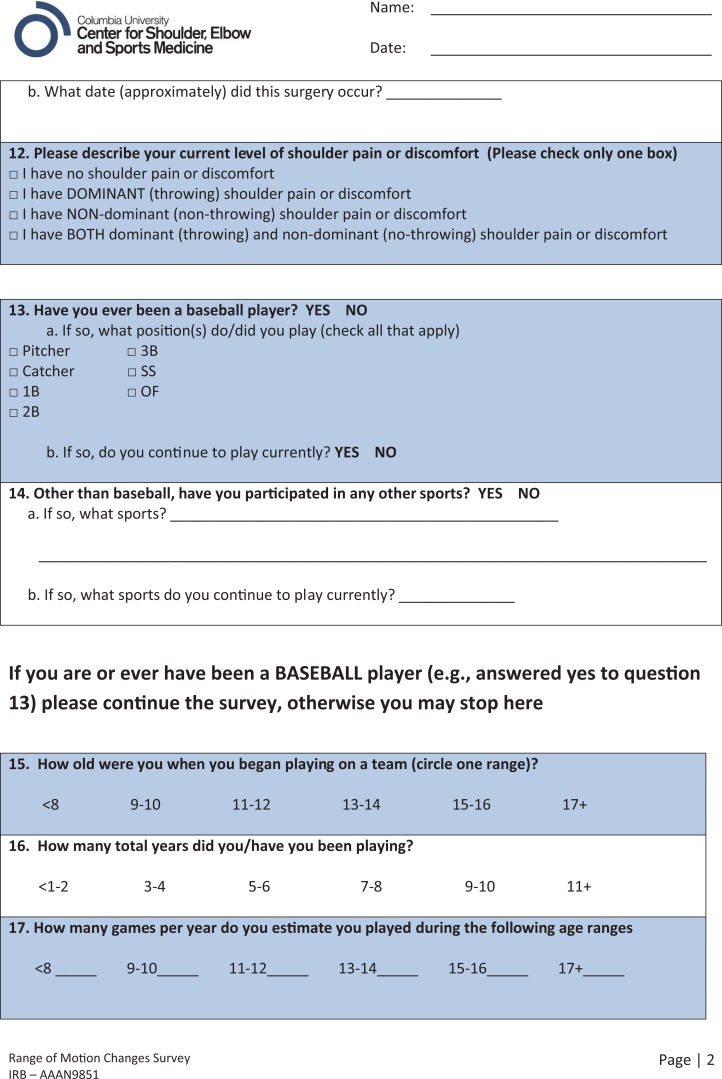
The resting position of the scapula was determined by measuring the distance from the midpoint of the sternal notch (SN) to the medial aspect of the coracoid process (CP) and the horizontal distance from the posterolateral angle of the acromion (PLA) to the thoracic spine (TS) (Figure 3). All measurements were performed using a digital vernier caliper with the player in the upright position. Static scapular measurements, particularly the SN-to-CP distance, have demonstrated high correlation with PM muscle length, reflecting postural impairment.2 The scapular index was calculated using the equation [(SN to CP / PLA to TS) × 100] to capture the transverse-plane orientation of the scapula.2
Figure 3.
Scapular index measurement. (A) Sternal notch to coracoid process distance. (B) Posterolateral angle of scapula to thoracic spine distance.
Bilateral glenohumeral passive range of motion (PROM) measurements were taken on all participants while supine. A standard goniometer combined with a validated mobile application-based digital inclinometer was used.30 The shoulders were abducted 90° in the plane of the body. The scapula was stabilized during measurements, where the investigator (D.K.) supported the humerus to ensure neutral sagittal position and manually stabilized the scapula as described in a prior investigation.29 A second investigator (W.R.) used the digital inclinometer to determine the angle between the ulnar axis and a perpendicular plane to the examination table during rotation and recorded the result.
All PM and scapular measurements were performed on throwing and nonthrowing shoulders by a single observer (J.L.H.). All PROM measurements were performed by 2 examiners (D.K. and W.R.), where the same investigator performed all motion maneuvers and the other recorded the results. All investigators were blinded to arm dominance, and the order of measurements was randomized.
Statistical Analysis
Analysis was conducted using SAS 9.4 (SAS Institute).25 P values less than .05 were considered significant. Descriptive statistics were performed for all variables. PM and scapular measurements were compared between throwing and nonthrowing shoulders by use of paired Student t tests. Post hoc analyses were performed via a Bonferroni procedure when significant differences were detected. A multivariate regression model was built to assess the impact of demographic variables collected in the study survey on each measured variable.
Results
A total of 49 adolescent baseball players were included during the data collection period (Table 1). All players were male, they were predominantly right-handed (83.7%), and the majority listed pitcher as their primary position (69.4%). The mean age was 16.2 years, and more than 60% of players had played in excess of 9 months of baseball in the prior calendar year.
TABLE 1.
Player Demographics (N = 49)
| Variable | n (%)a |
|---|---|
| Age, y | 16.2 ± 1.2 |
| Male sex | 49 (100) |
| Race | |
| White | 24 (49) |
| Hispanic | 4 (8.2) |
| Asian | 2 (4.1) |
| Black | 1 (2) |
| Not reported | 18 (36.7) |
| Hand dominance | |
| Right | 41 (83.7) |
| Left | 8 (16.3) |
| Primary position | |
| Pitcher | 34 (69.4) |
| Position player | 15 (30.6) |
| Time playing baseball | |
| >11 y | 15 (30.6) |
| 9-10 y | 15 (30.6) |
| 7-8 y | 13 (26.5) |
| Other | 6 (12.2) |
| Played >9 months over last year | 39 (61.2) |
| Played >30 games over last year | 33 (67.3) |
aValues expressed as n (%) of participants, except for age, which is expressed as mean ± standard deviation.
Significant differences were found in PM length between throwing and nonthrowing arms (Table 2). Absolute mean ± SD length of the PM muscle was significantly shorter in throwing shoulders when measured while players were sitting with arms at rest (158.8 ± 11.8 mm) and sitting with shoulders in maximal external rotation (194.6 ± 15.6 mm) compared with nonthrowing shoulders measured while players were sitting with arms at rest (162.5 ± 12.8 mm) and sitting with shoulders in maximal external rotation (199.4 ± 15.1 mm) (P = .004 for both). Similarly, the PMI was significantly less in throwing shoulders when players were supine with arms at rest (97.7 ± 7.3 mm; P = .007), sitting with arms at rest (88.2 ± 6.0 mm; P = .006), and sitting with shoulders in maximal external rotation (108.1 ± 7.5 mm; P < .001). The mean table-to-acromion distance was significantly greater in throwing (51.6 ± 12.5 mm) compared with nonthrowing (43.9 ± 12.6 mm) shoulders, representing shorter PM lengths (P < .001).
TABLE 2.
Pectoralis Minor Muscle Measurements
| Throwinga | Nonthrowinga | P | |
|---|---|---|---|
| Pectoralis minor length | |||
| Supine, arms at rest | 175.7 ± 14.7 | 178.3 ± 14.4 | .116 |
| Sitting, arms at rest | 158.8 ± 11.8 | 162.5 ± 12.8 | .004 |
| Sitting, shoulder in maximal ER | 194.6 ± 15.6 | 199.4 ± 15.1 | .004 |
| Pectoralis minor index | |||
| Supine, arms at rest | 97.7 ± 7.3 | 100.3 ± 6.8 | .007 |
| Sitting, arms at rest | 88.2 ± 6.0 | 90.5 ± 6.3 | .006 |
| Sitting, shoulder in maximal ER | 108.1 ± 7.5 | 111.6 ± 6.4 | <.001 |
| Table-to-acromion distance | 51.6 ± 12.5 | 43.9 ± 12.6 | <.001 |
aValues (in millimeters) expressed as mean ± standard deviation. ER, external rotation.
There was a significant difference in the calculated scapular index of throwing (70.1 ± 5.7 mm) versus nonthrowing (71.8 ± 5.9 mm) shoulders (P = .005) (Table 3).
TABLE 3.
Static Scapular Measurements
| Throwinga | Nonthrowinga | P | |
|---|---|---|---|
| Sternal notch to coracoid process | 139.9 ± 10.4 | 139.8 ± 10.4 | .978 |
| Posterolateral corner to thoracic spine | 200.4 ± 16.8 | 195.4 ± 16.2 | <.001 |
| Scapular index | 70.1 ± 5.7 | 71.8 ± 5.9 | .005 |
aValues (in millimeters) expressed as mean ± standard deviation.
Players typically had less internal rotation and significant increases in external rotation in throwing compared with nonthrowing shoulders (Table 4). The mean external rotation in the throwing shoulder was 112.3° ± 10.5°, compared with 105.1° ± 10.2° for the nonthrowing shoulder, a mean difference of 7.1° (P < .001). Only 2 players met the criteria for GIRD,4 with rotational deficits in excess of 20°.
TABLE 4.
Bilateral Shoulder PROMa
| Shoulder PROM | Throwingb | Nonthrowingb | Mean Differenceb,c | P |
|---|---|---|---|---|
| Internal rotation | 58.7 ± 9.2 | 62.3 ± 8.3 | –3.5 ± 9.9 | .01 |
| External rotation | 112.3 ± 10.5 | 105.1 ± 10.2 | 7.1 ± 9.8 | <.001 |
| Total rotation | 171 ± 11.6 | 167.4 ± 11.9 | 3.6 ± 11.3 | .02 |
aPROM, passive range of motion.
bValues (in degrees) expressed as mean ± SD.
cDifference calculated as (throwing shoulder PROM) – (nonthrowing shoulder PROM).
Multivariate analysis performed to assess the relationship between player demographic variables and pectoralis minor and scapular measurements and shoulder range of motion did not identify any significant associations.
Discussion
Although scapular malpositioning is commonly associated with shoulder rotational deficits and injury risk, modifiable causes of this malpositioning are not well defined in overhead athletes. Our study analyzed the scapulothoracic profile of adolescent baseball players and specifically the resting length of the PM muscle as a reliable clinical examination maneuver. We confirmed our hypothesis of significantly shorter PM lengths in throwing compared with nonthrowing shoulders when participants were sitting with arms at rest and sitting with shoulders in maximal external rotation (P = .004 for both). The PMI, normalized to player height, was significantly less in throwing shoulders when players were supine with arms at rest (P = .007), sitting with arms at rest (P = .006), and sitting with shoulders in maximal external rotation (P < .001). The table-to-acromion distance was significantly larger in throwing (51.6 mm) compared with nonthrowing (43.9 mm) shoulders, indicative of asymmetric scapular posturing (P < .001).
The PM tendon originates on ribs 3, 4, and 5 near the costosternal junction and attaches to the inferior border of the coracoid process of the scapula. Anatomic shortening of the PM can lead to an increase in scapular anterior tilting and internal rotation and a decrease in scapular upward rotation, which can reduce the subacromial space and lead to shoulder impingement.4,19 The PM length is potentially shortened due to repetitive use of the muscle, often seen in overhead athletes, resulting in adaptive changes in PM muscle tension.8,27 A decreased resting length of the PM muscle can thus alter shoulder kinematics and be associated with scapular dyskinesis.15,17 In the throwing athlete, players with reduced PM muscle length may have reduced shoulder external rotation, requiring compensatory scapular motion. Adaptive tightness in the PM is characteristic in the development of scapular malpositioning, inferior medial border prominence, coracoid pain, and malposition syndrome.7 Here, impingement-like symptoms result from the anteroinferior angulation of the acromion secondary to scapular protraction in overhead athletes.7 Therefore, the detection of asymmetric PM shortening via a reliable clinical test may be helpful in identifying players at risk and may allow for a preventive stretching routine.3 In addition, overuse has been described as a major cause of player injury in youth baseball, with significant increases in the risk of surgery for those throwing more than 80 pitches per game and pitching more than 8 months per year.12,21 In the present study, 61.2% of players indicated on the demographic survey that they had played in excess of 9 months of baseball in the previous year. Further education regarding the injury risks of overuse and the importance of compliance with suggested throwing guidelines should be emphasized in this study population.
Two main techniques for measuring the PM muscle have been described in the literature. The direct method, which entails using a vernier caliper to measure the resting length of the PM muscle from the coracoid process to the fourth rib space, has been validated in human cadavers by electromagnetic tracking.1 Subsequent studies using tape measures and calipers alike have shown good to excellent reliability when validated by electromagnetic tracking (ICC ranging from 0.82 to 0.97).1,23,28 Alternatively, the tabletop test indirectly measures the PM length via scapular protraction and internal rotation by assessing the distance of the posterolateral acromion to the examination table.24 Previous studies have demonstrated excellent intratester and intertester reliability and have reported ICCs above 0.90 and 0.88, respectively.13,20 However, the ability of this method to accurately measure PM length and the extent to which other potential factors influence the test remain unclear.28
In our study, absolute PM muscle lengths were significantly shorter in throwing arms when players were sitting with arms at rest and sitting with shoulders in full external rotation, with mean differences of 3.7 mm and 4.8 mm, respectively. Although small, these adaptive differences are noteworthy given their occurrence in asymptomatic adolescent players with a mean age of 16.2 years in whom no differences in total PROM arc were identified between throwing and nonthrowing shoulders. It is possible that more pronounced, clinically relevant PM shortening may be seen in mature professional players or those with shoulder pain. For instance, a cross-sectional study of NCAA Division I swimmers demonstrated significant differences in PM length between the dominant arms of athletes with a history of shoulder pain.10 Swimmers with shoulder pain and disability had mean PM shortening differences of 5.3 mm and 6.8 mm with arms at rest and in maximal external rotation, respectively. Similar adaptations have been demonstrated in elite asymptomatic adolescent tennis players, in whom significant differences in PM lengths of 12 mm were identified between dominant and nondominant shoulders.8 Whether absolute PM length should be measured with the player in the supine or upright position remains controversial.8,23,26 Advocates of the upright position argue that the elimination of gravity when the player is supine modifies the typical forces acting on the shoulder complex and that the addition of the weight of the thorax can alter scapular position and PM length.23 Ultimately, typical functional activities of the upper extremity are performed when the athlete is upright. Our study failed to demonstrate a significant difference in PM length when players were supine. The PMI values, which express the PM muscle length as a percentage of the athlete’s height, were significantly less in all measured positions for the throwing shoulders. However, normative values for the PMI are currently unavailable in the literature. As such, the direct measurement of muscle length may be more useful in detecting PM shortening in individual patients and documenting changes after intervention.
The table-to-acromion distance is an indirect measure of PM length. Dominant shoulders demonstrated a significant mean increase of 7.7 mm compared with nondominant shoulders, suggesting forward scapular posture. The mean values of 51.6 mm for dominant shoulders and 43.9 mm for nondominant shoulders are expectantly smaller than the values reported previously in adult populations; values ranged from 59.6 to 65.7 mm and from 59 to 65 mm in 2 other investigations.2,13 Previously, it was suggested that when the PM muscle is of normal length, the table-to-acromion distance should not exceed 25.4 mm (1 inch), where greater values are indicative of muscular imbalance and PM shortening.24 Subsequent studies have challenged the validity of this threshold and have shown it unable to distinguish between short and “normal” PM lengths.13,28
To assess the scapular profile of the athletes, static measurements were taken from palpable anatomic landmarks. In theory, those individuals with shorter PM resting lengths should exhibit increased scapular internal rotation, therefore having a shorter resting SN-to-CP distance with a concurrent increase in TS-to-PLA distance. The SN-to-CP distance has demonstrated a high correlation with measured PM length, and the scapular index has shown a moderate correlation with scapular internal rotation.2 In the current study, the scapular index was significantly reduced in throwing shoulders, suggesting internal rotation of the scapular within the transverse plane. However, the use of the scapular index has not been validated, and the index measurement is not necessarily suggestive of scapular kinematic alternations. In addition, normative values have not been reported for widespread clinical use.
The present study has limitations. The PROM and PM assessments were performed during the off-season, so most players were not throwing in the same capacity as in game situations, and their measurements may represent different values from in-season PROM and PM resting length. The investigation lacked a control group, but previous studies have demonstrated the validity of PM measurements in both symptomatic and asymptomatic athletes.10,13,23 A number of variables examined in the study were explored for the first time in adolescent baseball players, and future studies should compare results with age-matched nonathletic participants. Only a single rater performed the PM measurements, and the generalizability of the results to the population of clinicians has not been established. An analysis using multiple raters should be considered to determine the validity and reliability of these measurements in baseball players. The scapular index and its components (SN-to-CP distance and TS-to-PLA distance) have not been validated or tested for reliability. Finally, the differences in PM muscle length were small, and additional studies are needed to determine the minimal clinically important difference to establish the amount of change in length that is meaningful for the player. It is possible that more pronounced adaptive changes would be seen in mature professional players. Although PM shortening is hypothesized to be a primary adaptive change in the throwing shoulder, it is possible that shortening occurs secondarily from other alterations in scapular mechanics, and the current study is not sufficient to determine direct causation.
Conclusion
Asymptomatic adolescent baseball players have significant differences in PM length and static scapular measurements in throwing compared with nonthrowing shoulders. The clinical significance of this finding requires further investigation, but PM stretching routines are encouraged.
Appendix
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was obtained from the Columbia University Medical Center Institutional Review Board (protocol No. IRB-AAAN9851).
References
- 1. Borstad JD. Measurement of pectoralis minor muscle length: validation and clinical application. J Orthop Sports Phys Ther. 2008;38(4):169–174. [DOI] [PubMed] [Google Scholar]
- 2. Borstad JD. Resting position variables at the shoulder: evidence to support a posture-impairment association. Phys Ther. 2006;86(4):549–557. [PubMed] [Google Scholar]
- 3. Borstad JD, Ludewig PM. Comparison of three stretches for the pectoralis minor muscle. J Shoulder Elbow Surg. 2006;15(3):324–330. [DOI] [PubMed] [Google Scholar]
- 4. Borstad JD, Ludewig PM. The effect of long versus short pectoralis minor resting length on scapular kinematics in healthy individuals. J Orthop Sports Phys Ther. 2005;35(4):227–238. [DOI] [PubMed] [Google Scholar]
- 5. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part I: pathoanatomy and biomechanics. Arthroscopy. 2003;19(4):404–420. [DOI] [PubMed] [Google Scholar]
- 6. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part II: evaluation and treatment of SLAP lesions in throwers. Arthroscopy. 2003;19(5):531–539. [DOI] [PubMed] [Google Scholar]
- 7. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part III: the SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003;19(6):641–661. [DOI] [PubMed] [Google Scholar]
- 8. Cools AM, Johansson FR, Cambier DC, Velde AV, Palmans T, Witvrouw EE. Descriptive profile of scapulothoracic position, strength and flexibility variables in adolescent elite tennis players. Br J Sports Med. 2010;44(9):678–684. [DOI] [PubMed] [Google Scholar]
- 9. Fleisig GS, Andrews JR, Cutter GR, et al. Risk of serious injury for young baseball pitchers: a 10-year prospective study. Am J Sports Med. 2011;39(2):253–257. [DOI] [PubMed] [Google Scholar]
- 10. Harrington S, Meisel C, Tate A. A cross-sectional study examining shoulder pain and disability in division I female swimmers. J Sport Rehabil. 2014;23:65e75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kendall FPME, Provance PG. Muscles: Testing and Function. 4th ed Baltimore, MD: Williams & Wilkins; 1993. [Google Scholar]
- 12. Kerut EK, Kerut DG, Fleisig GS, Andrews JR. Prevention of arm injury in youth baseball pitchers. J La State Med Soc. 2008;160(2):95–98. [PubMed] [Google Scholar]
- 13. Lewis JS, Valentine RE. The pectoralis minor length test: a study of the intra-rater reliability and diagnostic accuracy in subjects with and without shoulder symptoms. BMC Musculoskelet Disord. 2007;8:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Limpisvasti O, ElAttrache NS, Jobe FW. Understanding shoulder and elbow injuries in baseball. J Am Acad Orthop Surg. 2007;15(3):139–147. [DOI] [PubMed] [Google Scholar]
- 15. Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80(3):276–291. [PubMed] [Google Scholar]
- 16. Lukasiewicz AC, McClure P, Michener L, Pratt N, Sennett B. Comparison of 3-dimensional scapular position and orientation between subjects with and without shoulder impingement. J Orthop Sports Phys Ther. 1999;29:574–583. [DOI] [PubMed] [Google Scholar]
- 17. McClure P, Greenberg E, Kareha S. Evaluation and management of scapular dysfunction. Sports Med Arthrosc. 2012;20(1):39–48. [DOI] [PubMed] [Google Scholar]
- 18. McFarland EG, Wasik M. Epidemiology of collegiate baseball injuries. Clin J Sport Med. 1998;8(1):10–19. [DOI] [PubMed] [Google Scholar]
- 19. Muraki T, Aoki M, Izumi T, Fujii M, Hidaka E, Miyamoto S. Lengthening of the pectoralis minor muscle during passive shoulder motions and stretching techniques: a cadaveric biomechanical study. Phys Ther. 2009;89(4):333–341. [DOI] [PubMed] [Google Scholar]
- 20. Nijs J, Roussel N, Vermeulen K, Souvereyns G. Scapular positioning in patients with shoulder pain: a study examining the reliability and clinical importance of 3 clinical tests. Arch Phys Med Rehabil. 2005;86(7):1349e55. [DOI] [PubMed] [Google Scholar]
- 21. Olsen SJ II, Fleisig GS, Dun S, Loftice J, Andrews JR. Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am J Sports Med. 2006;34(6):905–912. [DOI] [PubMed] [Google Scholar]
- 22. Reeser JC, Joy EA, Porucznik CA, Berg RL, Colliver EB, Willick SE. Risk factors for volleyball-related shoulder pain and dysfunction. PM R. 2010;2(1):27e36. [DOI] [PubMed] [Google Scholar]
- 23. Rosa DP, Borstad JD, Pires ED, Camargo PR. Reliability of measuring pectoralis minor muscle resting length in subjects with and without signs of shoulder impingement. Braz J Phys Ther. 2016;20(2):176–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sahrmann S. Diagnosis and Treatment of Movement Impairment Syndromes. London, UK: Mosby; 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. SAS [computer program]. Version 9.4 Cary, NC: SAS Institute; 2013. [Google Scholar]
- 26. Struyf F, Meeus M, Fransen E, et al. Interrater and intrarater reliability of the pectoralis minor muscle length measurement in subjects with and without shoulder impingement symptoms. Man Ther. 2014;19(4):294–298. [DOI] [PubMed] [Google Scholar]
- 27. Tate A, Turner GN, Knab SE, Jorgensen C, Strittmatter A, Michener LA. Risk factors associated with shoulder pain and disability across the lifespan of competitive swimmers. J Athl Train. 2012;47:149e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Weber C, Enzler M, Wieser K, Swanenburg J. Validation of the pectoralis minor length test: a novel approach. Man Ther. 2016;22:50–55. [DOI] [PubMed] [Google Scholar]
- 29. Werner BC, Holzgrefe RE, Griffin JW, et al. Validation of an innovative method of shoulder range-of-motion measurement using a smartphone clinometer application. J Shoulder Elbow Surg. 2014;23(11):e275–e282. [DOI] [PubMed] [Google Scholar]
- 30. Wilk KE, Macrina LC, Arrigo C. Passive range of motion characteristics in the overhead baseball pitcher and their implications for rehabilitation. Clin Orthop Relat Res. 2012;470(6):1586–1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wilk KE, Meister K, Andrews JR. Current concepts in the rehabilitation of the overhead throwing athlete. Am J Sports Med. 2002;30(1):136–151. [DOI] [PubMed] [Google Scholar]