Abstract
Objective:
To determine whether e-mail is a useful mechanism to provide prompt, case-specific data feedback and improve door-to-needle (DTN) time for acute ischemic stroke treated with intravenous tissue plasminogen activator (IV-tPA) in the emergency department (ED) at a high-volume academic stroke center.
Methods:
We instituted a quality improvement project at Columbia University Medical Center where clinical details are shared via e-mail with the entire treatment team after every case of IV-tPA administration in the ED. Door-to-needle and component times were compared between the prefeedback (January 2013 to March 2015) and postfeedback intervention (April 2015 to June 2016) periods.
Results:
A total of 273 cases were included in this analysis, 102 (37%) in the postintervention period. Median door-to-stroke code activation (2 vs 0 minutes, P < .01), door-to-CT Scan (21 vs 18 minutes, P < .01), and DTN (54 vs 49 minutes, P = .17) times were shorter in the postintervention period, although the latter did not reach statistical significance. The proportion of cases with the fastest DTN (≤45 minutes) was higher in the postintervention period (29.2% vs 42.2%, P = .03).
Conclusion:
E-mail is a simple and effective tool to provide rapid feedback and promote interdisciplinary communication to improve acute stroke care in the ED.
Keywords: stroke and cerebrovascular disease, quality, education, thrombolysis
Introduction
Shorter door-to-needle (DTN) time is associated with better outcomes in acute ischemic stroke.1 Prompt data feedback is a Target: Stroke best practice and has been shown to improve DTN times in the absence of other interventions.2,3 Since optimal acute stroke treatment requires efficient multidisciplinary cooperation, we hypothesized that for feedback to be successful, it must rapidly reach all members of the treatment team including rotating resident physicians. We developed and implemented a quality improvement (QI) initiative to evaluate whether e-mail would be an effective medium to improve DTN and component treatment times in the emergency department (ED). Although other methods of feedback have been used in acute stroke, the utility of rapid e-mail feedback designed to widely disseminate data and foster communication between disciplines has not been previously studied.4
Methods
Study Design/Setting
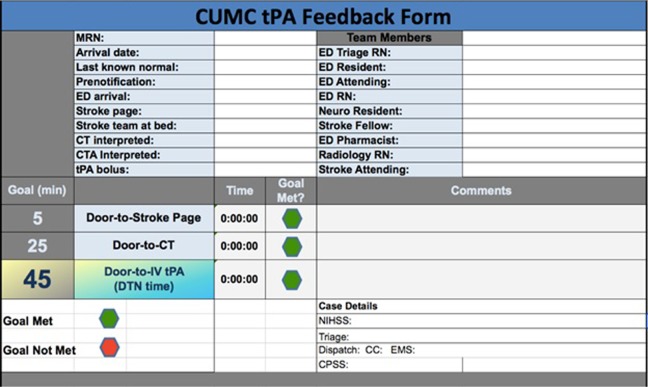
In April 2015, we began a rapid e-mail feedback protocol following every case of intravenous (IV) thrombolysis in the ED at Columbia University Medical Center. Patients with acute stroke who receive IV tissue plasminogen activator (IV-tPA) are identified via the electronic medical record. A stroke fellow reviews each case with the treating neurology resident and prepares the feedback e-mail. Neurology residents are the primary responders to all stroke codes at our institution, and their observations are solicited to augment the fellows’ case-specific data review. Within 48 hours of thrombolysis, the fellow sends the encrypted feedback e-mail. The body of the e-mail contains a brief case narrative detailing the patient’s presenting symptoms, mode of arrival, whether emergency medical services (EMS) provided prenotification, and if so, whether stroke code activation occurred prior to EMS arrival in the ED. Any potential case-specific sources of treatment delay identified by the fellow are also noted. The e-mail concludes with an open-ended request for any team member to use reply all to comment on the noted sources of delay, suggest other causes of delay or relevant case-specific observations, and brainstorm improvements. A standardized form is included at the end of each e-mail which (1) indicates whether institutional goals were met for door-to-stroke code activation (≤5 minutes), door-to-CT Scan (≤25 minutes), and DTN (≤45 minutes) times and (2) identifies the involved team members by name (Figure 1). The e-mail is sent to the individual practitioners involved in the case (neurology resident, stroke fellow and attending, emergency medicine resident and attending, ED nurses, pharmacist, and radiology technician) as well as to the relevant division supervisors (neurology and emergency medicine stroke directors, neurology chief resident, directors of ED nursing, radiology, laboratory services, pharmacy, telecommunications, EMS, and quality assurance).
Figure 1.
Feedback form included in each e-mail. The team members are listed by name. Any comments about delays in each time interval are included as text. A green (goal met) or red (goal not met) hexagon is included for each interval.
Prior to April 2015, stroke cases were reviewed at monthly stroke performance improvement meetings approximately 2 months after patient presentation. This review process continued after the introduction of the e-mail feedback protocol. There were no other QI initiatives concurrent with the e-mail feedback protocol. The institutional review board of (IRB) Columbia University approved this analysis (IRB# AAAQ8818) and granted a waiver of informed consent. The feedback QI initiative was IRB exempt.
Data Analysis
We compared baseline demographics, median DTN, and component times in the postfeedback (April 1, 2015, to June 30, 2016) to the prefeedback (January 1, 2013, to March 31, 2015) period. We also compared median DTN by calendar year. Categorical variables were compared with χ2 and continuous variables with Student t tests. Median times were compared with Mann-Whitney U or Kruskal-Wallis tests. Changes in the slope of the linear trend associated with the feedback intervention were assessed with linear regression. SPSS version 23.0 was used for all analyses, with P < .05 taken as significant.
Results
A total of 273 cases were included in this analysis: 171 (62.6%) in the prefeedback and 102 (37.4%) in the postfeedback period. Baseline group demographics did not differ between periods (Table 1). Median door-to-stroke code activation (2 vs 0 minutes, P < .01), door-to-CT (21 vs 18 minutes, P < .01), and DTN (54 vs 49 minutes, P = .17) were shorter in the postfeedback period, but the difference in DTN was not significant. The proportion of cases with DTN ≤60 minutes was the same between periods (67.8% vs 66.7%, P = .89). Improvement was seen in all institutional time goals in the postfeedback period: door-to-stroke code activation ≤5 minutes (63.7% vs 78.4%, P = .01), door-to-CT ≤25 minutes (63.2% vs 75.5%, P = .04), and DTN ≤45 minutes (29.2% vs 42.2%, P = .03). The proportion of EMS prenotifications with stroke activation prior to ED arrival more than doubled in the postfeedback period (26.9% vs 58.0%, P < .01). Median DTN was significantly lower in 2016 than in the prior 3 years (Figure 2). The median DTN between June and July 2015 did not differ, suggesting the absence of a July effect in the postfeedback period.
Table 1.
Demographic, Time Intervals, and Specific Benchmarks Pre- and Postfeedback Intervention.
| Preintervention | Postintervention | P value | |
|---|---|---|---|
| January 2013 to March 2015 (n = 171) | April 2015 to June 2016 (n = 102) | ||
| Age, mean (SD) | 69 (16.5) | 65 (17.9) | .05 |
| Men (%) | 68 (39.8) | 50 (49.0) | .14 |
| English speaking (%) | 89 (52.0) | 63 (61.8) | .19 |
| National Institutes of Health Stroke Scale, median (IQR) | 7 (4-15) | 6 (3 to 12) | .15 |
| Arrive by EMS (%) | 128 (74.9) | 71 (69.6) | .27 |
| Prenotification (%) | 78 (60.9) | 50 (70.4) | .24 |
| Treatment intervalsa | |||
| Onset-to-door | 68 (45-98) | 65 (43 to 112) | .82 |
| Door-to-stroke code activation | 2 (0-11) | 0 (−1 to 4) | <.01 |
| Door-to-CT Scan | 21 (15-36) | 18 (14 to 25) | <.01 |
| Door-to-needle | 54 (45-70) | 49 (37 to 77) | .17 |
| Specific benchmarks | |||
| Door-to-stroke code activation ≤5 minutes (%) | 109 (63.7) | 80 (78.4) | .01 |
| Door-to-CT Scan ≤25 minutes (%) | 108 (63.2) | 77 (75.5) | .04 |
| DTN ≤ 45 minutes (%) | 50 (29.2) | 43 (42.2) | .03 |
| Stroke code activation prior to ED arrival (%)b | 21 (26.9) | 29 (58.0) | <.01 |
Abbreviations: DTN, door-to-needle; EMS, emergency medical services; ED, emergency department; IQR, interquartile range; SD, standard deviation.
aMedian (IQR).
bOf those with prenotification.
Figure 2.
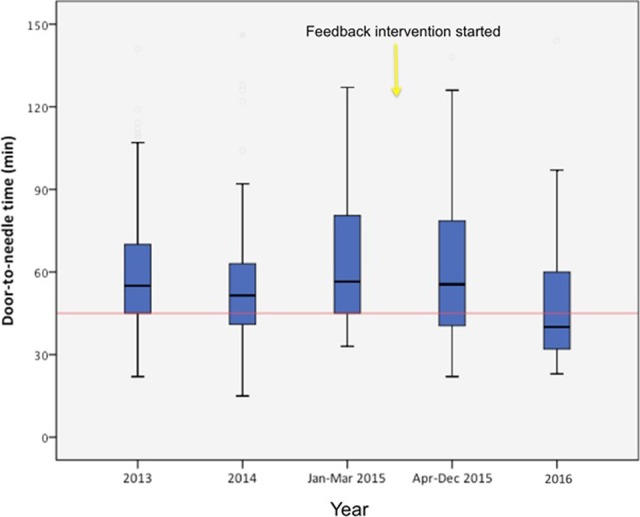
Door-to-needle (DTN) time by year with 2015 separated to demarcate before and after the feedback intervention and includes all cases through June 30, 2016. Red line on y-axis indicates DTN of 45 minutes. P = .03 for difference in medians, Kruskal-Wallis test.
Figure 3 demonstrates the linear trend in DTN in the pre- and postfeedback periods. Visual inspection shows more rapid treatment in the postintervention period. The linear trend for DTN in the prefeedback period was not significant (slope = −0.3 min/mo, 95% confidence interval [CI] −0.8 to 0.2, P = .24). During the postfeedback period, the linear trend for DTN approached, but did not reach, statistical significance (slope = −1.3 min/mo, 95% CI: −2.7 to 0.1, P = .07).
Figure 3.
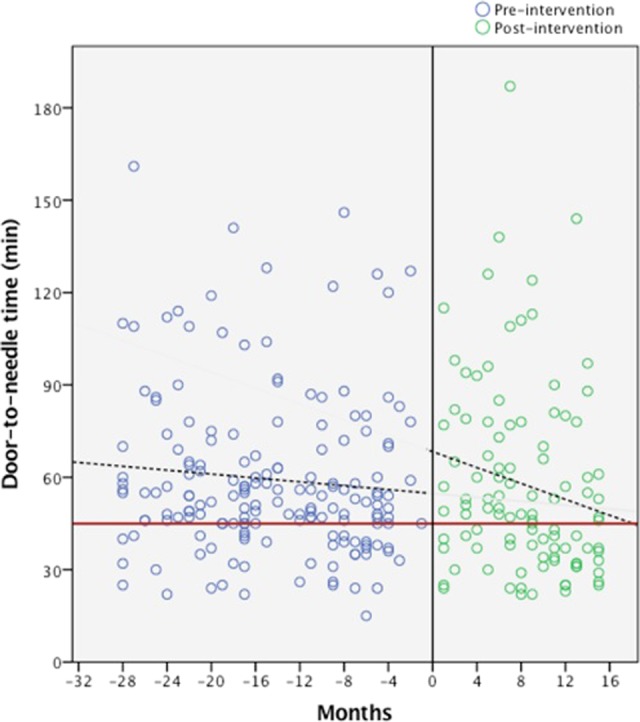
Door-to-needle (DTN) times before and after the e-mail feedback intervention were introduced in April 2015 (month 0). The dashed lines show the linear trend in the pre- and postfeedback periods. The red line on the y-axis indicates DTN of 45 minutes.
Discussion
Following the introduction of a rapid e-mail feedback protocol for all IV-tPA stroke cases treated in the ED at an academic medical center, we witnessed improvements in all DTN benchmarks, specifically in the proportion of cases with door-to-stroke code activation ≤5 minutes, door-to-CT ≤25 minutes, and DTN ≤45 minutes. An analysis by calendar year revealed a significant improvement in median DTN following introduction of our feedback intervention. Our findings suggest that e-mail is a simple and effective tool to provide multidisciplinary feedback and improve DTN and component IV-tPA times.
E-mail may succeed as a feedback medium because it enables rapid data sharing and communication among team members from many disciplines. Acute stroke treatment requires collaboration between many divisions and varying levels of health-care providers, including rotating neurology and emergency medicine trainees. Those involved in caring for a patient with acute stroke who received IV-tPA often have discordant schedules, making rapid face-to-face interactions logistically challenging. This is particularly acute at academic centers, as neurology residents, who play a pivotal role in acute stroke care delivery, rotate through the ED. Although there are well-known strategies to improve DTN, delays in DTN may be institution specific.5,6 Effective feedback requires engagement of all stakeholders and a forum to share sources of delay on a case-by-case basis proximate to the time of care delivery.7 An additional benefit of e-mail may be the ability of the medium to neutralize implicit hierarchy and promote dialogue between health-care providers of varying levels.6 Specifically, e-mail can directly link the individual treatment team and division supervisors, so that ground-level observations and suggestions for improvement can be effectively incorporated into systematic changes.
Indeed, many sources of delay were identified through responses to the feedback e-mails from various team members and strategies to address the delays developed from electronic discussion. Several examples follow: (1) Delays in stroke activation for EMS prenotified cases were identified. Inaccessibility of the prenotification phone and unfamiliarity with the prenotification protocol by ED nursing staff were some of the sources of delay. Solutions included moving the prenotification phone to a central location in the ED and providing additional nursing education. (2) Delays in ordering tPA were identified. Lack of convenient computer access for the neurology stroke resident contributed to this delay. This was solved by installing a computer dedicated to neurology residents in the CT control room. (3) Delays between tPA mixing and administration were identified. Inconsistent availability of IV pumps was one source of delay. This was solved by storing IV pumps in pharmacy and having pharmacists bring the pumps with tPA. (4) Delays in tPA administration for some Spanish-speaking patients were identified. Inconsistent arrival of Spanish interpreters to the stroke codes contributed to this delay. This was solved by adding the Spanish interpreters to the stroke code activation. Thus, a number of changes in our institutional acute stroke care system as a result of the rapid e-mail feedback protocol may have contributed to the reduction in treatment times we observed.
However, it is also possible that rapid feedback and the sharing of treatment time lines engendered a Hawthorne effect, which led to the improvements we witnessed.8 Alternatively, improved relationships between departments or within departments between residents, fellows, and attendings may have been facilitated by the e-mails leading to more efficient real-time collaboration during subsequent IV-tPA cases.
Our findings are consistent with those of prior studies in that initiatives focused exclusively on feedback have led to improved acute stroke treatment timelines.3,4 Other centers have incorporated feedback into broader QI initiatives, and some have shared DTN times via e-mail.9 However, we are not aware of any data demonstrating the effect of e-mail feedback as a stand-alone mechanism to improve the quality of stroke care. Data from other disciplines suggest e-mail may be a useful tool for developing process changes in keeping with our findings.10
Limitations
There are a number of limitations to our study. We do not know whether the results we report will be sustained over time since our findings are after only 15 months of experience with the e-mail feedback protocol. Barriers to rapid thrombolysis at our center may differ from those elsewhere, limiting the generalizability of our results. Frequent e-mails could lead to fatigue, which may limit sustained utility. Additionally, we did not include read receipts with our feedback e-mails, so we do not know how often all intended recipients read the feedback e-mail. Although no other QI initiatives occurred during this period, secular trends may have contributed to improved treatment time lines independent of the e-mail feedback protocol.
Conclusion
Rapid, case-specific feedback via e-mail to the multidisciplinary care team was associated with improved DTN and component times for acute stroke cases treated with IV-tPA in the ED. Further study is warranted to assess the durability of our findings.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Sara K. Rostanski received funding from NIH/NINDS StrokeNet grant 1U10 NS086728.
References
- 1. Lees KR, Bluhmki E, von Kummer R, et al. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet. 2010;375(9727):1695–1703. [DOI] [PubMed] [Google Scholar]
- 2. Fonarow GC, Smith EE, Saver JL, et al. Improving door-to-needle times in acute ischemic stroke: the design and rationale for the American Heart Association/American Stroke Association’s Target: Stroke initiative. Stroke. 2011;42(10):2983–2989. [DOI] [PubMed] [Google Scholar]
- 3. Ghrooda E, Alcock S, Jackson AC. Improvement in thrombolytic therapy administration in acute stroke with feedback. Can J Neurol Sci. 2012;39(6):789–792. [DOI] [PubMed] [Google Scholar]
- 4. Burnett MM, Zimmermann L, Coralic Z, Quon T, Whetstone W, Kim AS. Simple text-messaging intervention is associated with improved door-to-needle times for acute ischemic stroke. Stroke. 2014;45(12):3714–3716. [DOI] [PubMed] [Google Scholar]
- 5. Xian Y, Smith EE, Zhao X, et al. Strategies used by hospitals to improve speed of tissue-type plasminogen activator treatment in acute ischemic stroke. Stroke. 2014;45(5):1387–1395. [DOI] [PubMed] [Google Scholar]
- 6. Prabhakaran S, Khorzad R, Brown A, Nannicelli AP, Khare R, Holl JL. Academic-community hospital comparison of vulnerabilities in door-to-needle process for acute ischemic stroke. Circ Cardiovasc Qual Outcomes. 2015;8(6 suppl 3):S148–S154. [DOI] [PubMed] [Google Scholar]
- 7. Croskerry P. The feedback sanction. Acad Emerg Med. 2000;7(11):1232–1238. [DOI] [PubMed] [Google Scholar]
- 8. Sedgwick P, Greenwood N. Understanding the Hawthorne effect. BMJ. 2015;351:h4672. [DOI] [PubMed] [Google Scholar]
- 9. Ruff IM, Ali SF, Goldstein JN, et al. Improving door-to-needle times: a single center validation of the target stroke hypothesis. Stroke. 2014;45(2):504–508. [DOI] [PubMed] [Google Scholar]
- 10. Harewood GC, Petersen BT, Ott BJ. Prospective assessment of the impact of feedback on colonoscopy performance. Aliment Pharmacol Ther. 2006;24(2):313–318. [DOI] [PubMed] [Google Scholar]