Abstract
Objective:
To explore the utilization of platelet-rich plasma (PRP) for degenerative cartilage processes and evaluate whether there is sufficient evidence to better define its potential effects.
Design:
Systematic literature reviews were conducted in PubMed/MEDLINE and Cochrane electronic databases till May 2015, using the keywords “platelet-rich plasma OR PRP OR autologous conditioned plasma OR ACP AND cartilage OR chondrocyte OR chondrogenesis OR osteoarthritis (OA) OR arthritis.”
Results:
The final result yielded 29 articles. Twenty-six studies examined PRP administration for knee OA and 3 involved PRP administration for hip OA. The results included 9 prospective randomized controlled trials (RCTs) (8 knee and 1 hip), 4 prospective comparative studies, 14 case series, and 2 retrospective comparative studies. Hyaluronic acid (HA) was used as a control in 11 studies (7 RCTs, 2 prospective comparative studies, and 2 retrospective cohort). Overall, all RCTs reported on improved symptoms compared to baseline scores. Only 2 RCTs—one for knee and one for hip—did not report significant superiority of PRP compared to the control group (HA). Nine out of 11 HA controlled studies showed significant better results in the PRP groups. A trend toward better results for PRP injections in patients with early knee OA and young age was observed; however, lack of uniformity was evident in terms of indications, inclusion criteria, and pathology definitions in the different studies.
Conclusion:
Current clinical evidence supports the benefit in PRP treatment for knee and hip OA, proven to temporarily relieve pain and improve function of the involved joint with superior results compared with several alternative treatments. Further research to establish the optimal preparation protocol and characteristics of PRP injections for OA is needed.
Keywords: platelet-rich plasma, PRP, osteoarthritis, cartilage, hyaluronic acid, injections
Introduction
Background
Degenerative osteoarthritis (OA) is the most common form of arthritis and a major public health problem worldwide. It affects nearly 27 million adults in the United States alone.1 Often causing pain, loss of function, and disability, it has a substantial social impact due to the rising mean age of the population, increasing rates of obesity, and a growing emphasis on physical activity in all age groups.2 Attempts to analyze and understand the biology of this disease have not yet led to satisfactory results. OA is regarded as the result of a long chain of events; however, some parts in that chain are still a mystery and uncertainty exists regarding which part of this process should be targeted in order to inhibit and prevent disease progression. Cartilage possesses limited regeneration properties. Joint tissue damage and OA may result from loss of proper tissue homeostasis due to trauma or chronic repetitive overload, but could also be the result of metabolic and biological predispositions.3 Numerous approaches have been proposed as noninvasive treatment options4; however, none has shown any distinct ability to change the natural history of the disease. The fact that current conservative OA therapies are unable to supply consistent satisfying results is attributed mainly to insufficient understanding of the molecular basis of disease development and progression, as well as the lack of dynamic biomarkers that might reflect specific biological or pathological processes. There are currently no disease modifying medical interventions for OA, and treatments are primarily aimed at symptom relief.5 In recent years, research efforts have shifted toward identifying key biochemical pathways that can be targeted therapeutically through biological intervention. One of the major foci of research in the past decade has been platelet-rich plasma (PRP), drawing much attention as an innovative and promising therapeutic modality. PRP therapies are considered a major potential breakthrough in the treatment of many medical conditions and are currently one of the hottest topics in regenerative medicine. Among these, PRP has emerged as a biological therapy for the treatment of cartilage injuries and for intraarticular application to address knee pain. The purpose of this study was to systematically review the scientific evidence for utilization of PRP in pathologic processes of cartilage and as a potential addition to the management strategy algorithm for OA. Using the existing data, our aim was to explore the rationale behind the utilization of PRP in pathologic degenerative cartilage processes and evaluate whether there is sufficient evidence to better define its potential effects.
Rationale behind the Use of PRP for Degenerative Cartilage Disease
PRP is defined as a biological therapeutic modality consisting of preparations containing a supraphysiological concentration of platelet and plasma proteins that accelerate the repair process by direct and indirect mechanisms. The aim of this treatment is to improve the reparability of endogenous cells. It is based on the intraarticular delivery of autologous platelet-rich preparations containing a large pool of growth factors and proteins stored in the alpha-granules of platelets. These growth factors and proteins, which have been implicated in tissue repairing mechanisms and have been found to take part in the regulation of articular cartilage,6 are aimed at stimulating repair and replacement of damaged cartilage. Numerous growth factors in PRP stimulate cartilage matrix synthesis and counteract the effects of catabolic cytokines such as interleukin-1 and tumor necrosis factor-α. Growth factors, as a pool, have been found to possess synergistic effects on cartilage matrix synthesis7,8 and are known to induce further growth factor protein production by neighboring articular chondrocytes.9 Basic science evidence supports the therapeutic potential of PRP. Chondrocytes treated in vitro with releasate from thrombin-clotted leukocyte-PRP (L-PRP)10 resulted in significantly increased cell proliferation, synthesis rate, and accumulation of glycosaminoglycans and collagen type II (COL2) compared with controls.11 In another study, human OA chondrocytes were removed from patients undergoing total hip arthroplasty, and PRP application induced the expression of proteins involved in chondrocytic differentiation compared with platelet poor plasma (PPP) and fetal bovine serum.12 In this study, PRP was shown to be more effective than PPP or fetal bovine serum at increasing cell proliferation and inducing expression of genes associated with normal chondrocyte phenotype, including aggrecan and Sox-9 with sustained but not increased levels of COL2. Other basic science research demonstrated that PRP causes inhibition of the transactivating activity of nuclear factor-κB (NF-κB) and decreased expression of cyclooxygenase-2, which are important inflammatory regulators.13 These findings suggest that PRP has the ability to stimulate local host cartilage and improve repair. Anitua et al. examined the effect of a platelet-derived preparation rich in growth factors (PRGFs) in OA synovial cell biology and revealed the ability of PRGF to stimulate HA synthesis, driving the secretion of HA by the synovial fibroblasts.14 Synovial cells were isolated from 10 osteoarthritic patients and cultured in serum-free media (basal conditions) and exposed to either a platelet-poor preparation or PRGF (no or very low leukocyte penetration) for 72 hours. Cells activated with interleukin-1 for 48 hours were also exposed to PRGF. They found that PRGF significantly enhanced HA secretion compared with platelet-poor preparations. PRGF also significantly enhanced the secretion of HA induced by interleukin-1 activation, suggesting that pure platelet rich plasma could serve to induce chondroprotection and joint lubrication after intraarticular application even in the face of inflammation. These data support the therapeutic potential for PRP in the articular environment with anabolic effects on cartilage, mesenchymal stem cells, and synovial coverage.
Methods
Two independent reviewers performed a search using the PubMed/MEDLINE and Cochrane electronic databases till May 2015. Combinations of the terms “platelet-rich plasma OR PRP OR autologous conditioned plasma OR ACP AND cartilage OR chondrocyte OR chondrogenesis OR osteoarthritis OR arthritis” were used. Our inclusion criteria were studies evaluating the effect of PRP or any blood product with platelet concentration higher than baseline values published in peer-reviewed journals in the English language. We included different variations of PRP preparations in this study: activated and nonactivated PRP, PRP releasate, and PRP gels. Of all the articles, we selected only articles reporting on clinical studies which had utilized PRP, PRGF, or autologous conditioned plasma (ACP) for the treatment of degenerative cartilage pathology or OA of the knee or hip joint in humans and those articles that were published in the English language. Exclusion criteria were (1) animal studies; (2) patients with previous surgical intervention (i.e., total knee arthroplasty or anterior cruciate ligaments reconstruction); (3) articles involving nonosteoarthritic indications (osteonecrosis, osteochondral lesions, etc.); and (3) articles not published in English. In addition, articles that used PRP as a supplemental treatment to alternative modalities like bone marrow aspirate concentrate, scaffold-based cartilage repair, and mesenchymal stem cells were also excluded, as well as articles that included PRP as augmentation for different cartilage-related procedures (microfractures, cartilage implantation). Reference lists of included studies were also reviewed to ensure that no relevant articles were overlooked/missed. Review articles, expert opinions, case reports, and letters to editors were excluded from this review. Two authors performed the literature search, and 4 authors independently reviewed the search results. For the search results, articles titles and abstracts were reviewed, and potentially eligible studies received full-text review. Final agreement on inclusion was discussed among all authors, and the main author had the definitive decision vote in controversial cases. The initial search included 288 articles, from which 259 were excluded after screening for duplicates, title, and/or abstract. The final result yielded 29 articles ( Fig. 1 ) in which PRP was a prime treatment and are described in brief in Tables 1 and 2 .
Figure 1.
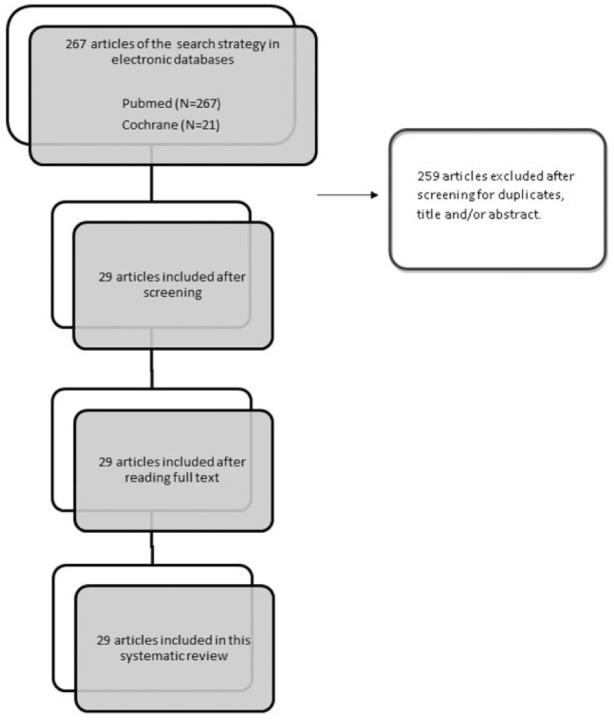
Study flow diagram.
Table 1.
Clinical Studies.
| Authors | Diagnosis | Study Design | Age Group | PRP Preparation (Number of Injections and Intervals) | Control Group (Number of Injections and Intervals) | Leucocytes | Activator | Follow-Up | Outcome Measures | Adverse Effects |
|---|---|---|---|---|---|---|---|---|---|---|
| Raeissadat et al.15 (2015) | Knee OA, Kellgren-Lawrence grades 1-4 | Randomized controlled clinical trial (160 patients) | 40-70 years | Rooyagen Kit for PRP—concentrations of 4 to 6 times (n = 87), 2 intraarticular injections at 4-week interval | HA group. Hyalgan (n = 73), 3 doses of intraarticular injection at 1-week interval | PRP containing leukocytes | No activator | 12 months after treatment | WOMAC and SF-36 questionnaires | No adverse reactions |
| Raeissadat et al.16 (2014) | Knee OA, Kellgren-Lawrence grades 1-4 | Randomized controlled clinical trial. Not blinded. 31 patients in the PRP group and 31 patients in the control group. | 44-67 years | Rooyagen Kit for PRP - concentrations of x 4-6. Two intra-articular injections at 4-week interval. + Exercise. | Exercise and acetaminophen 500 mg (without codeine). No injections. | PRP containing leukocytes | No activator. | 6m after treatment | WOMAC and SF-36 questionnaires | No adverse reactions |
| Guler et al.17 (2014) | Knee OA, Kellgren-Lawrence grades 1-2 | Retrospective case series; 132 patients; 63 patients (86 knees) were in the HA group and 69 patients (89 knees) were in the PRP group | 46-63 years | Independent technique; 3 intraarticular injections at 1-week intervals | HA group. Ostenil plus 40 mg/2.0 mL (Bio-gen, TRB Chemedica SA, Switzerland); 3 intraarticular injections at 1-week intervals | Leucocyte rich PRP | NA | 2, 6 months after treatment | Knee Society’s Knee Scoring System (KSS) and the visual analog scale (VAS) scoring system | No adverse reactions |
| Mangone et al.18 (2014) | Knee OA, Kellgren-Lawrence grades 2-3 | Prospective case Series; 72 patients | 50-85 years | Regen Kit Athena for PRP; 3 injections; 3-week interval | None | Leucocyte rich PRP | Calcium gluconate | Baseline, 1, 3, 6, 12 months after last injection | WOMAC scale for the knee, VAS at rest and VAS in movement | No adverse reactions |
| Gobbi et al.19 (2014) | Early knee OA. Kellgren-Lawrence grades 1-2 | Prospective, randomized study initiated in 2009; 50 knees were randomly selected from 119 knees and received a second cycle of PRP injection at the completion of 1 year from first cycle | 40 and 65 years | Regen ACR-C. A cycle consisted of 3 injections, each given at a monthly interval | Knees received only first cycle of PRP | Leucocyte poor PRP | NA | Baseline, 12, 18, and 24 months after treatment | KOOS,VAS, Tegner and Marx scoring systems | No adverse reactions |
| Filardo et al.20 (2014) | Knee OA, Kellgren-Lawrence grades 0-4 | Therapeutic case series of 51 knees; 2 interventional groups; early-moderate OA (K-L 0-3) in 41 knees vs. severe OA (K-L 4) in 10 knees; both groups received 3 injections of PRP | Mean age 59 years, range: 20-87 years | ACP Kit (Arthrex Inc). 3 weekly intraarticular injections of PRP | 2 interventional groups: early-moderate OA (K-L 0-3) vs. severe OA (K-L 4); both received the same PRP protocol | Leucocyte poor PRP | NA | Mean follow-up of 14.5 months (range: 6-24 months) | IKDC-Subjective, EQ-VAS, Tegner, and KOOS scores | Mild pain and/or slight swelling were reported which resolved spontaneously within 24-48 hours |
| Battaglia et al.21 | Hip OA | Randomized controlled clinical trial (100 patients) | Mean age: 53 ± 12, range: 25-76 years | Independent technique | HA (Hyalubrix) administered via intraarticular ultrasound-guided injections | PRP containing leukocytes | Calcium chloride | Baseline, 1, 3, 6, and 12 months after treatment | the Harris Hip Score (HHS) and VAS | |
| Vaquerizo et al.22 (2013) | Knee OA, Kellgren-Lawrence grades 2-4 | Multicenter, randomized controlled, clinical trial (96 patients: 48 in each group) | >50 years | PRGF-Endornet (3 injections of 8 mL at 1-week intervals) | Durolane HA 48 patients (1 injection) | Avoided leucocyte pick up | Calcium chloride | Baseline, 6 months, and 12 months after treatment | WOMAC and Lesquene scores; OMERACT-OARSI responders | Mild postinjection pain after PRGF (8 patients); mild postinjection pain after Duralane (6 patients); Pseudo-septic reaction after Duralane (2 patients) |
| Patel et al.23 (2013) | Early OA | Randomized, controlled trial (148 knees) | Range: 33-80 years | Independent technique: single injection—52 knees; 2 injections (3 weeks apart)—50 knees | Saline injections (46 knees) | WBC filtered PRP | NA | 6 weeks, 3 months, and 6 months after treatment | WOMAC and VAS scores | Nausea and dizziness in 22.2% and 44% patients in single and double injection groups, respectively |
| Hart et al.24 (2013) | Grade 2 and 3 chondromalacia | Prospective case series (50 patients) | Range: 31-75 years | Independent technique: (2-2.5 fold platelet conc.) 9 injections in 1 year | None | NA | NA | Baseline and 12 months | Lysholm, Tegner, IKDC, Cincinnati scores, and MRI with a 12-month follow-up | No adverse effects |
| Torrero et al.25 (2013) | Grade 1-3 Outerbridge chondropathy | Prospective case series (30 patients) | 18-65 years | GPS mini set (BIOMET) 1 intraarticular injection | None | NA | Calcium chloride | Baseline, 1, 3, and 6 months after treatment | KOOS and VAS scores | No severe adverse reactions |
| Jang et al.26 (2013) | Degenerative OA | Prospective case series (65 patients) | NA | Independent technique; 1 intraarticular injection | None | NA | NA | Baseline, 1, 3, 6, 9, and 12 months after treatment | IKDC and VAS scores | No severe adverse reactions |
| Say et al.27 (2013) | Symptomatic (pain) mild to moderate osteoarthritis (Kellgren-Lawrence grades 1-3) | Prospective study,90 patients | 47-63 years | (PRGF)a: a single 2.5-mL PRP injection | 3 Injections of LMW hyaluronic acid at weekly intervals | Leucocyte poor PRP | Calcium chloride | Baseline, 3 and 6 months after treatment | KOOS and VAS scores | No adverse reactions |
| Halpern et al.28 (2013) | Symptomatic early knee OA (Kellgren-Lawrence grades 0-2) | Prospective case series (22 patients) | 30-70 years | MTF Cascade system; a single 6-mL PRP injection | None | NA | Calcium chloride | Baseline, 1 week, 1, 3, 6, 12 months after treatment; MRI follow-up at 12 months | WOMAC and VAS scores, and MRI at 1 year | No adverse reactions |
| Gobbi et al.29 (2012) | Symptomatic knee OA (Kellgren-Lawrence grades 1-3) | Prospective case series (50 patients) | 40-70 years | Regenlab-ACR C (2 intraarticular injections at monthly intervals) | None | Leucocyte poor PRP | None | Baseline, 6 and 12 months after treatment | VAS, IKDC Subjective, KOOS, and Tegner scores | No adverse reactions |
| Filardo et al.30 (2012) | Symptomatic knee degenerative lesions and OA (Kellgren-Lawrence grades 0-4) | Prospective clinical study (144 patients) | 30-80 years | Independent technique: single spin preparation (PRGF): 72 patients (3 injections); double-spinning preparation: 72 patients (3 injections) | None | PRP with leucocytes | NA | Baseline, 2, 6, and 12 months after treatment | IKDC, EQ-VAS, and Tegner scores | More pain reaction and swelling following PRP injection compared to PRGF |
| Napilitano et al.31 (2012) | Knee OA (Kellgren-Lawrence grades 1-3 and Outerbridge grades 1-2) | Prospective case series (27 patients) | (18-81 years) | RegenLab 3 injections of PRP at weekly intervals | None | Leucocyte poor PRP | Calcium gluconate | 1 week and at 6m after treatment | NRS and WOMAC scores | No adverse effects |
| Spakova et al.32 (2012) | Knee OA (Kellgren-Lawrence grades 1-3) | Prospective, comparative study | 19-77 years | Independent technique: 3 injections of PRP at weekly intervals (4.5-times increase in platelet concentration) | 3 injections of HA at weekly intervals | Leucocyte rich PRP | NA | 3 and 6 months after treatment | WOMAC and the 11-point pain intensity Numeric Rating Scale | No severe adverse events |
| Cerza et al.33 (2012) | Knee gonarthrosis | Randomized, controlled clinical trial (120 patients) | NA | PRP (Arthrex ACP): 60 patients, 4 PRP injections at weekly intervals | HA: 60 patients, 4 injections at weekly intervals | NA | NA | 1, 2, and 6 months after treatment | WOMAC score | No adverse reactions |
| Filardo et al.34 (2012) | Knee OA (Kellgren-Lawrence grades 1-3) | Prospective, randomized trial | NA (exclusion beyond 80 years); mean age 55 and 58 years in each group | Independent technique: 54 PRP injections weekly for 3 weeks | 55 HA injections weekly for 3 weeks | PRP with leucocytes | 10% Calcium chloride | 2, 6, and 12 months after treatment | IKDC, EQ-VAS, Tegner, and KOOS scores | No major adverse effects |
| Sanchez et al.35 (2012) | Symptomatic knee OA (Ahlback grades 1-3) | Prospective, randomized, controlled, multicenter trial (176 patients) | 41-74 years | PRGF-Endoret 3 injections at weekly intervals | 3 HA injections; each at a weekly interval | Leucocyte poor plasma | Calcium chloride 400µL | 6 months after treatment | WOMAC and VAS pain subscale | 1 patient who received HA felt numbness in the infiltration area, and another patient had itching on the outside area of both thighs; 1 treated with PRGF-Endoret had pain after the third infiltration |
| Sanchez et al.36 (2012) | Monolateral severe hip OA | Prospective case series (40 patients) | 33-84 years | PRGF, Vitoria, Spain; 3 intra articular PRP injections, administered weekly | None | NA | Calcium chloride | 7 weeks and 6 months after treatment | WOMAC, VAS, and Harris hip score | 1 case of mild rash; transient sensation of heaviness in few |
| Battaglia et al.37 (2011) | Hip OA (Kellgren-Lawrence grades 2-4) | Prospective case series (20 patients) | 28-69 years | Independent technique: 3 US-guided PRP injections | None | NA | NA | Baseline, 1, 3, 6, and 12 months after treatment | Harris Hip Score and WOMAC scores | No severe adverse reactions |
| Kon et al.38 (2011) | Cartilage degenerative knees and mild to severe knee OA (Kellgren-Lawrence grades 0-4) | Prospective, randomized study (150 patients) | 30-81 years | 50 patients: 3 autologous PRP injections | 50 patients high molecular weight HA; 50 patients low molecular weight HA | PRP with leucocytes | 10% Calcium chloride | 2 and 6 months after treatment | IKDC and EQ-VAS scores | No adverse reactions |
| Wang-Saegusa et al.39 (2011) | Knee OA (Outerbridge grades 1-4) | Prospective case series study (261 patients) | 48.39 ± 16.65 years | PRGF (BTI, Vitoria, Spain): 3 intraarticular injections at 2-week intervals | None | NA | NA | 6 months after treatment | VAS, SF-36, WOMAC Index and Lequesne Index | No adverse reactions |
| Kon et al.40 (2010) | Degenerative cartilage lesions and OA knee (Kellgren-Lawrence grade 0-4) | Prospective case series (91 patients) 3 PRP injections | 24-82 years | Independent technique: 3 injections at 3-week intervals | None | NA | 10% Calcium chloride | 6, 12 months after treatment | IKDC Objective and Subjective, EQ-VAS scores | No adverse reactions |
| Filardo et al.41 (2011)b | Degenerative cartilage lesions and OA knee (Kellgren-Lawrence grades 0-4) | Prospective case series (91 patients) 3 PRP injections, 90 patients available at 2 years follow-up | 24-82 years | Independent technique: 3 injections at 3-week intervals | None | NA | 10% Calcium chloride | 24 months | IKDC Objective and Subjective, EQ-VAS scores | No adverse reactions |
| Sampson et al.42 (2009) | Primary and secondary knee OA | Prospective case series (14 patients) | 18-87 years | GPS system (BIOMET); 3 PRP injections at 4 weekly intervals | None | NA | 10% Calcium chloride | 2, 5, 11, 18, and 52 weeks after treatment | VAS, KOOS, and cartilage ultrasound | Modest pain caused by the injection in a few; no long-term adverse effects |
| Sanchez et al.43 (2008) | Knee OA (Ahlback grades 1-4) | Observational retrospective cohort study (60 patients) | PRGF: 63.53 ± 8.91 years; hyaluronan: 60.90 ± 8.63 years | PRGF (BTI, Vitoria, Spain): 30 patients; 3 injections at weekly intervals | Hyaluronan injections: 30 patients; 3 injections at weekly intervals | WBC content below detection level of the haematological analyzer | Calcium chloride | 5 weeks after treatment | WOMAC score | Mild pain and inflammation for short duration in both groups in a few patients |
PRP = platelet-rich plasma; WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index; OMERACT-OARSI = Outcome Measures for Rheumatology Committee and Osteoarthritis—Research Society International Standing Committee for Clinical Trials Response Criteria Initiative; NA = not available in abstract or full text; SF-36 = Short Form-36; OA = osteoarthritis; HA = hyaluronic acid; KOOS = Knee Injury and Osteoarthritis Outcome Scores; IKDC = International Knee Documentation Committee; EQ-VAS = EuroQoL Visual Analog Scale; WBC = white blood cells; PRGF = platelet-derived preparation rich in growth factors; MRI = magnetic resonance imaging; LMW = low molecular weight; NRS = Numerical Rating Scale; US = ultrasound.
Referred to in the article as “Anitua’s Method.”
Same cohort as Kon et al. (2010)40 investigated at follow-up of 2 years.
Table 2.
Randomized Controlled Trials.
| Authors | Diagnosis | Number of Patients | Age Group | PRP Preparation (Number of Injections and Intervals) | Control Group (Number of Injections and Interval) | Leucocytes | Activator | Follow-Up | Outcome Measures | Adverse Effects |
|---|---|---|---|---|---|---|---|---|---|---|
| Raeissadat et al.15 (2015) | Knee OA, grade 1-4 of Kellgren-Lawrence scale | Controlled randomized clinical trial (160 patients) | 40-70 years | Rooyagen Kit for PRP—concentrations of 4 to 6 times (n = 87), 2 intr-articular injections at 4-week intervals | HA group; Hyalgan (n = 73), 3 doses of intraarticular injection at 1-week interval | PRP containing leukocytes | NA | 12 months after the treatment | WOMAC and SF-36 questionnaires | No adverse reactions |
| Raeissadat et al.16 (2014) | Knee osteoarthritis; grades 1-4 of Kellgren-Lawrence scale | Randomized clinical trial with control group; not blinded; 31 patients in the PRP group and 31 patients in the control group | 44-67 years | Rooyagen Kit for PRP—concentrations of 4 to 6 times (n = 87), 2 intraarticular injections at 4-week intervals; plus exercise | Exercise and acetaminophen 500 mg (without codeine); no injections | PRP containing leukocytes | No activator | 6 months after the treatment | WOMAC and SF-36 questionnaires | No adverse reactions |
| Battaglia et al.21 (2013) | Hip OA | Controlled randomized clinical trial (100 patients) | 25-76 years | Independent technique; consecutive (once every 2 weeks) intraarticular ultrasound-guided injections of 5 mL autologous PRP—5 ml | Consecutive (once every 2 weeks) intraarticular ultrasound-guided injections of vial (30 mg/2 mL) of high-molecular-weight (1500 kD) HA (Hyalubrix; Fidia Farmaceutici Spa, Padova, Italy) | PRP containing leukocytes | Calcium chloride | 1, 3, 6, and 12 months | The Harris Hip Score (HHS) and Visual Analog Scale (VAS) | No adverse reactions |
| Vaquerizo et al.22 (2013) | OA of the knee (Kellgren-Lawrence grades 2-4) | 96 patients | >50 years | PRGF-Endornet (3 injections of 8 mL at 1-week interval) | Durolane HA 48 patients (1 injection) | Avoided leucocyte pick up | Calcium chloride | 24 weeks and 48 weeks | WOMAC and Lesquene scores. OMERACT-OARSI responders | Mild postinjection pain after PRGF (8 patients); mild postinjection pain after Duralane (6 patients); pseudo-septic reaction after Duralane (2 patients) |
| Patel et al.23 (2013) | Early OA | 148 knees | NA in abstract | Independent technique: single injection—52 knees; 2 injections (3 weeks apart)—50 knees | Saline injections (46 knees) | WBC filtered PRP | NA | 6 weeks, 3 months, and 6 months posttreatment | WOMAC and VAS scores | Nausea and dizziness in 22.2% and 44% patients in single and double injection groups |
| Cerza et al.33 (2012) | Gonarthrosis of the knee | 120 patients | NA | PRP (Arthrex ACP): 60 patients, 4 PRP injections at weekly intervals | Hyaluronic acid: 60 patients 4 injections at weekly intervals | NA | NA | 1, 2, and 6 months | WOMAC score | No adverse reactions |
| Filardo et al.34 (2012) | OA knee (Kellgren-Lawrence grades 1-3) | 109 knees | NA (exclusion beyond 80 years); mean age 55 and 58 years in each group | Independent technique: 54 PRP injections weekly for 3 weeks | 55 Hyaluronan injections weekly for 3 weeks | NA | 10% Calcium chloride | 2, 6, and 12 months | IKDC, EQ-VAS, Tegner, and KOOS scores | No major adverse effects |
| Sanchez et al.35 (2012) | Symptomatic OA of knee Ahlback grades 1-3 | 176 patients | 41-74 years | PRGF-Endoret; 3 injections at weekly intervals | 3 HA injections; each at a weekly interval | Leucocyte poor plasma | 400 µL calcium chloride | 6 months | WOMAC and VAS pain subscale | 1 patient who received HA felt numbness in the infiltration area, and another patient had itching on the outside area of both thighs; 1 treated with PRGF-Endoret had pain after the third infiltration |
| Kon et al.38 (2011) | Cartilage degenerative knees and mild to severe OA knees (Kellgren-Lawrence grades 0-4) | 150 patients | 30-81 years | Independent technique: 50 patients; 3 autologous PRP injections | 50 patients; high molecular weight HA; 50 patients low molecular weight HA | NA | 10% Calcium chloride | 2 and 6 months | IKDC and EQ-VAS scores | No adverse reactions |
PRP = platelet-rich plasma; WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index; OMERACT-OARSI = Outcome Measures for Rheumatology Committee and Osteoarthritis—Research Society International Standing Committee for Clinical Trials Response Criteria Initiative; NA = not available in abstract or full text; SF-36 = Short Form-36; OA = osteoarthritis; HA = hyaluronic acid; KOOS = Knee Injury and Osteoarthritis Outcome Scores; IKDC = International Knee Documentation Committee; EQ-VAS = EuroQoL Visual Analog Scale; WBC = white blood cells; PRGF = platelet-derived preparation rich in growth factors.
Results
The results of our systematic review yielded 29 clinical studies ( Tables 1 and 2 ). The majority of these studies (26) examined PRP administration for knee OA, while only 3 of the studies involved PRP administration for hip OA. The results included 9 prospective randomized controlled trials (RCTs), 4 prospective comparative studies, 14 case series, and 2 retrospective comparative studies. One of the studies, by Hart et al., was not clear with regard to whether a randomization process was involved and was therefore regarded as a prospective comparative study. Eight of the RCTs were conducted for knee OA and 1 for hip OA. Hyaluronic acid was used for the control groups in 7 RCTs, saline was used in 1 study, and an exercise program was used in 1 study. In the prospective comparative studies, HA was used for the control group in 2 studies, mesocaine was used in 1 study,24 and in another study19 the control group consisted of knees not receiving a second cycle of PRP injection at the completion of 1 year from first cycle. In the retrospective comparative studies group HA was used for the control group.
Age range in the studies was wide and not uniform. Various studies included patients as young as 18 years and as old as 85 years, with different age ranges. Four studies did not report age range.
Nineteen studies used the Kellgren Lawrence scale for the quantification of OA changes of which 7 studies included patients with Kellgren Lawrence grades 0 to 4, and 6 studies included patients with Kellgren Lawrence grades 0 to 3. Three studies used the Outerbridge condromalacia scale, while 1 study used the Ahlback scale, and 5 studies did not report the OA scale used. Within the RCTs group, 4 used the Kellgren Lawrence scale, 1 used the Ahlback scale, and the rest did not report the usage of any scale.
The follow-up period in the different studies ranged from 5 weeks to 24 months, with the majority of studies reporting outcomes with a follow-up period of 12 months (13 studies) and 6 months (12 studies). Only 2 studies reported a follow-up of 24 months.
The studies included in this review vary in the PRP preparation method and different production techniques yielding different resulting preparations. Twelve different preparation techniques—commercial and independent noncommercial methods—were used in the different studies. Table 3 summarizes the different types of solutions used in the studies included in this systematic review according to currently used classification systems.
Table 3.
PRP Preparation, Concentration, Number of Injections, Interval, and Classifications.
| Authors | PRP Preparation | PRP Volume | PRP Concentration | Number of Injections | Interval Between Injections | Leucocytes | Activator | PAW Classification | Dohan Ehrenfest Classification | Mishra Classification |
|---|---|---|---|---|---|---|---|---|---|---|
| Raeissadat et al.15 (2015) | Rooyagen Kit | 4-6 mL | 4x-6x | 2 | 4 weeks | PRP containing leukocytes | No | P3B | LP-PRPa | 1A/B |
| Rayegani et al.16 (2014) | Rooyagen Kit | 4-6 mL | 4x-6x | 2 | 4 weeks | PRP containing leukocytes | No | P3B | LP-PRPa | 1A/B |
| Guler et al.17 (2014) | Autologous PRP | 2 mL | 4.3x | 3 | 1 week | Leucocyte rich PRP; X4.7 | NA | P3A | LR-PRP | 1/2A |
| Mangone et al.18 (2014) | Regen Kit Athena for PRP | 2-2.5mL | 3x-5x | 3 | 3 weeks | Leucocyte rich PRP | Calcium gluconate | P2xA | LR-PRP | 2A |
| Gobbi et al.19 (2014) | Regen ACR-C | 4 mL | 2x | 3 | 1 month | Leukocytes poor PRP | NA | P2 Bβ | LP-PRPa | 3A |
| Filardo et al.20 (2014) | ACP Preparation Kit (Arthrex Inc., Naples, FL) | 2-4 mL | 2x-3x | 3 | 1 week | Leukocytes poor PRP | NA | P2B | LP-PRPa | 3B |
| Battaglia et al.21 (2014) | Autologous PRP | 5 mL | 6x | 3 | 2 weeks | 8300/µL | Calcium chloride | P3xB | LP-PRP | 4A |
| Vaquerizo et al.22 (2013) | PRGF-Endornet | 8 mL | 2x-3x | 3 | 1 week | Minimal-none | Calcium chloride | P2xBβ | P-PRP | 4B |
| Patel et al.23 (2013) | PRP | NA | Mean platelet count: 310.14 × 103/µL | 1 or 2 | 3 weeks | Minimal-none | NA | P4B | P-PRP | 4B |
| Hart et al.24 (2013) | Autologous PRP | NA | 2x-2.5x | 9 | 1 week (1st 6 injections) 3 months between 6 and 7 and 1 month between next 3 | NA | NA | NA | NA | NA |
| Torrero et al.25 (2013) | GPS mini set (BIOMET) | NA | 2x-8x | 1 | Not applicable | Minimal-none | Calcium chloride | P2Aα | P-PRP | 4A/B |
| Jang et al.26 (2013) | Magellan Autologous Platelet Separator | 3 mL | 2.8x-7x | 1 | Not applicable | NA | Nil | P3Aα | P-PRPa | 3A/B |
| Halpern et al.27 (2013) | PRP cascade system | 6 mL | 1.3x-1.7x | 1 | Not applicable | Minimal-none | Calcium chloride | P2Bβ | P-PRP | 4B |
| Say et al.28 (2013) | Anitua method | 2.5 mL | 4x | 1 | Not applicable | Minimal | Calcium chloride | P2Bβ | P-PRP | 4B |
| Gobbi et al.29 (2012) | Regen Lab-ACR C | 4 mL | 2x-2.5x | 2 | 4 weeks | Decreased below baseline | Nil | P2Bβ | LP-PRP | 3B |
| Filardo et al.30 (2012) | PRP and (PRGF) | 5 mL | 4.5x (1.5x) | 3 | 3 weeks | 1.4x (none) | Calcium chloride | P3A (P2B) | L-PRP (P-PRP) | 2B (4B) |
| Napilitano et al.31 (2012) | Regen Lab | 5 mL | 2x-2.5x | 3 | 1 week | Decreased below baseline | Calcium gluconate | P3B | LP-PRP | 4B |
| Spakova et al.32 (2012) | Independent technique | 3 mL | 4.5x | 3 | 1 week | 3.6x | NA | P3A | LR-PRPa | 1B |
| Cerza et al.33 (2012) | PRP (Arthrex ACP) | 5x | 4 | 1 week | Minimal-none | Nil | P3Bβ | P-PRPa | 3A | |
| Filardo et al.34 (2012) | Independent technique | 5 mL | 5x | 3 | 1 week | 1.2x | 10% Calcium chloride | P4xA | P-PRP | 2A |
| Sanchez et al.35 (2012) | PRGF-Endoret | 8 mL | 2x-3x | 3 | 1 week | Minimal-none | 400 µL Calcium chloride | P2Bβ | P-PRP | 4B |
| Sanchez et al.36 (2012) | PRGF, Vitoria, Spain | 6-8 mL | 2x-3x | 3 | 1 week | Minimal-none | 10% Calcium chloride | P2Bβ | P-PRP | 4B |
| Battaglia et al.37 (2011) | Independent technique | 5 mL | NA | 3 | 2 weeks | NA | NA | NA | NA | NA |
| Kon et al.38 (2011) | Autologous PRP injections | 5 mL | 6x | 3 | 2 weeks | With WBC | 10% Calcium chloride | P4xNA | L-PRP | 2A |
| Wang-Saegusa et al.39 (2011) | PRGF | 5 mL | 2x-3x | 3 | 2 weeks | Minimal-none | 10% Calcium chloride | P2Bβ | P-PRP | 4B |
| Kon et al.40 (2010); Filardo et al.41 (2011) | Autologous PRP | 5 ml | 6x | 3 | 3 weeks | With WBC | 10% Calcium chloride | P4xNA | L-PRP | 2A |
| Sampson et al.42 (2009) | GPS system (BIOMET) | 6 mL | 2x-8x | 3 | 4 weeks | Minimal-none | 10% Calcium chloride | P4Aα | P-PRP | 4B |
| Sanchez et al.43 (2008) | PRGF | 6-8 mL | 2x-3x | 3 | 1 week | Minimal-none | 10% Calcium chloride | P2Bβ | P-PRP | 4B |
PRP = platelet-rich plasma; LP-PRP = leukocytes poor PRP; LR-PRP = leukocytes rich PRP; WBC = white blood cell; PRGF = platelet-derived preparation rich in growth factors.
No activation used.
Platelet concentration in these studies ranged between 1.3 times to 8 times the blood concentration, with the majority ranging between 2 and 4 times the blood concentration. Sixteen studies reported use of an activator prior to injection, and 14 of these studies used calcium chloride 10%. Fourteen studies used white blood cell (WBC)–containing preparations, 5 of which studies reported the use of PRP preparations with WBC content above blood concentration (1.2 to 4.7 times the blood concentration). Thirteen studies used WBC-free or minimal WBC preparations. Two studies did not report on WBC content.
As for adverse effects, no severe adverse effects of intraarticular PRP injections were reported in any of the studies. Most studies reported no adverse effects at all. Mild and self-limiting adverse effects were reported in a small number of patients in 7 studies (see Tables 4 and 5 ).
Table 4.
PRP Preparation Systems.
| System | Volume of Whole Blood (mL) | Centrifugation Force | Spin Time (Minutes) | Volume of PRP (mL) | Platelet Concentration (Fold Change) | Activation | Leukocyte Concentration |
|---|---|---|---|---|---|---|---|
| Rooyagen Kit | 35-40 | 1,600 rpm | 15 | 4-6 | X4-6 | No activation | Yes |
| 2,800 rpm | 7 | ||||||
| Double spin | |||||||
| AG Curasan | 10 | 1,200g | 10 | 6-7 | 2x | CaCl2 | Yes |
| Arthrex ACP System (Naples, FL) | 9 | 1,500 rpm single spin | 5 | 2-4 | 2x-3x | None if used within 30 minutes | No |
| Regenlab | 8 | 1,500g single spin | 5 | 4 | 1.7x | Autologous thrombin or calcium gluconate | Yes |
| Biomet GPS Recover Platelet separation Kit (Warsaw, IN) | Mini GPS3 27 mL or 54 mL | 3,200 rpm single spin | 15 | 3-6 | 2.07x | Thrombin CaCl2 | Yes (fold change 5.4); platelet concentrate buffered by adding 0.05 mL of 8.4% sodium bicarbonate to each mL of platelet concentrate |
| Cascade Fibrinet Platelet Rich fibrin Matrix (PRFM) | 9-18 | 1,100g and 1,450g single spin for PRP, double spin for PRFM | 6 minutes for PRP + 15 minutes for PRFM | 4-9 | 1.6x | CaCl2 | No |
| Plateltex | 16 | 160-180g and 100-1,200g | 10 and 10 | 6 and 10 | 1x-2x | Batroxobin for gel | Yes |
| Cytomedix Angel | 40-180 | 3,200 rpm | 15-28 | 2-5 | 4.3x | None | Yes |
| Harvest (Plymouth, MA); Smart PReP2APC (Warsaw, IN) | 50 or 100 | 3,650 rpm double spin | 14 | 3-9 or 10-20 | 7x | Thrombin CaCl2 | Yes (fold change 2.3) |
| Magellan-Medtronic (Minneapolis, MN) | 30-60 | 3,800 rpm double spin | 4-6 | 6 | 2.8x to 7x | CaCl2 | Yes (fold change 3.2) |
| Emcyte (Fort Myers, FL)/Genesis CS/Exactech (Gainesville, FL) Accelerate | 30 or 60 | 12 | 3 or 10 | 7x to 10x | Yes | ||
| BTI PRGF (Vitoria-Gasteiz, Spain) | 9-72 | 460g single spin | 8 | 4-32 | 2x-3x | CaCl2 | No |
PRP = platelet-rich plasma; PRGF = platelet-derived preparation rich in growth factors.
Table 5.
Studies Included in This Systematic Review: Description and Results.
| Authors | Diagnosis | Design | Purpose | PRP Preparation | PRP Concentration | Outcome Measures | Results |
|---|---|---|---|---|---|---|---|
| Raeissadat et al.15 (2015) | Knee OA, Kellgren-Lawrence grades 1-4 | Randomized controlled clinical trial (160 patients); 87 patients received 2 PRP injections; 73 received 3 HA injections. | To study the long-term clinical effect of intraarticular injections of PRP and HA and quality of life in patients with knee OA | Rooyagen Kit | 4x-6x | WOMAC and SF-36 questionnaires | At 12-month follow-up, WOMAC pain score and bodily pain significantly improved in both groups; however, the PRP group showed better results compared to the HA group (P < 0.001). Other WOMAC and SF-36 parameters improved only in the PRP group. More improvement (not statistically significant) was achieved in patients with grade 2 OA in both groups. |
| Raeissadat et al.16 (2014) | Knee OA, Kellgren-Lawrence grades 1-4 | Randomized controlled clinical trial; 31 patients per group. Same therapeutic exercise program was prescribed for both groups. The PRP group received 2 courses of leukocyte rich PRP with a 4-week interval. | To investigate the effects of PRP on pain, stiffness, function and quality of life in patients with knee OA | Rooyagen Kit | 4x-6x | WOMAC and SF-36 questionnaires | At 6-month follow-up mean changes in total WOMAC, physical component summery and the mental component summery of SF-36 in the PRP group showed better improvements than the control group (P < 0.05). |
| Guler et al.17 (2014) | Knee OA, Kellgren-Lawrence grades 1-2 | Retrospective study. 132a patients; 63 (86 knees) in the HA group and 69 (89 knees) in the PRP group. Patients received 3 injections at 1-week interval. | To compare short-term clinical outcomes between intraarticular PRP and HA in early-stage OA patients | Independent technique | 4.3x | Knee Society’s Knee Scoring System (KSS) and the Visual Analog Scale (VAS) scoring system | The PRP group had significantly higher KSS scores at the 2- and 6-month follow-up. Pretreatment, 2 months, and 6 months VAS scores were significantly lower in the PRP group than in the HA group: Pretreatment VAS mean difference of 0.46; 2 and 6 months VAS mean difference of 1.64 and 1.67. respectively |
| Mangone et al.18 (2014) | Knee OA. Kellgren-Lawrence grades 2-3 | Prospective case series; 72 patients | To evaluate and quantify the effects of PRP on QOL and pain in patients with OA (3 injections of PRP) | Regen Kit Athena for PRP | 3x-5x | WOMAC, VAS at rest and VAS in movement | Significant improvement both in functional and pain scores (P < 0.005). The improvement lasted for almost 1 year. Stiffness decreased significantly (P < 0.005) during the first month, but afterwards there was no sizable improvement. |
| Gobbi et al.19 (2014) | Early knee OA. Kellgren-Lawrence Grades 1-2 | Randomized prospective, study. 119 knees were followed for 2 years with 50 knees randomly selected to receive a second cycle of PRP injections 1 year from first cycle | To assess the outcome of intraarticular PRP injections in patients with early stages of knee OA and the effect of cyclical dosing after 1 year | Regen ACR-C. A cycle consisted of 3 injections, given at a monthly intervals | 2x | KOOS, VAS, Tegner and Marx scores | At 12 months, both groups showed similar and significant improvement. At 18 months, except for KOOS (Symptoms) and Tegner scores, all other parameters showed a significant difference between the 2 groups in favor of the second cycle group (P < 0.001). At 2 years, the scores declined in both groups but remained above the pretreatment values with no significant difference between groups |
| Filardo et al.20 | Knee OA. Kellgren-Lawrence grades 1-4 | Therapeutic case series of 51 knees | To describe the clinical results obtained after intraarticular injection of a leukocyte-poor PRP preparation for the treatment of knee OA | Autologous Conditioned Plasma (ACP) Preparation Kit (Arthrex Inc.) | 2x-3x | IKDC-Subjective, EQ-VAS, Tegner, and KOOS scores | The overall clinical outcome was positive and the treatment proved to be safe. In the “early/moderate OA” group, the IKDC-Subjective score increased from 36.4 at baseline evaluation to 57.3 at the mean 14.5-month follow-up (P < 0.0005) and a similar trend was shown by the EQ-VAS, Tegner, and KOOS scores. Although an improvement was also recorded in the “severe OA” group, the clinical outcome of patients in this group was poorer, less benefit was reported. In the “early/moderate OA” group, BMI and longer symptom duration before treatment were found to be correlated with clinical outcomes. |
| Battaglia et al.21 | Hip OA; Kellgren-Lawrence grades 2-4 | Randomized controlled clinical trial (100 patients) | To compare the clinical efficacy of PRP versus HA at 12 months of follow-up in patients with hip OA | Autologous PRP—Independent technique | 6x | Harris Hip Score (HHS) and VAS | An overall improvement was detected in both groups between 1- and 3-month follow-up. Despite a slightly progressive worsening between 6- and 12-month follow-up, the final clinical scores remained higher compared to baseline values (P < 0.0005), with no significant differences between PRP and HA groups. |
| Vaquerizo et al.22 (2013) | Knee OA | Randomized controlled trial; 48 patients received 3 injections of PRP (PRGF). 46 patients received 1 HA injection. | To compare the efficacy and safety of 3 injections of PRP versus a single intraarticular injection of HA for reducing symptoms in patients with knee OA | PRGF (BTI, Vitoria, Spain) | 2x-3x | WOMAC and Lesquene scores | Treatment with PRGF was significantly more efficient than HA in reducing knee pain and stiffness and improving function in knee OA patients. Response rate to PRGF was significantly higher than the rate of response to HA in all scores including pain, stiffness, and function on WOMAC, Lequesne index, and OMERACT-OARSI responders at 24 and 48 weeks. |
| Patel et al.23 (2013) | Early knee OA | Randomized, controlled trial; single (52 knees) versus double PRP (50 knees) injections versus saline injection (46 knees) | To compare outcomes following single and double PRP injections compared to a control group receiving placebo (saline) | Independent technique | Mean platelet count: 310.14 × 103/µL | WOMAC and VAS scores | Significant improvements in WOMAC scores at all follow ups when PRP was administered, with no difference between single and double injections. Deterioration in WOMAC from baseline values when saline was used. |
| Hart et al.24 (2013) | Grades 2-3 knee chondromalacia | Prospective study; 50 patients, 9 injections administered over 1 year | To assess if PRP can increase tibiofemoral cartilage regeneration and improve knee function | Autologous PRP—Independent technique (2-2.5 fold platelet concentration) | 2x-2.5x | Lysholm, Tegner, IKDC, Cincinnati scores and MRI at 12 months | Significant improvement in all scores at 12 months, P < 0.05. No significant cartilage regeneration. MRI did not confirm any significant cartilage condition improvement. |
| Torrero et al.25 (2013) | Knee OA. Outerbridge grades 1-3 | Prospective study; 30 patients (18-65 years) 1 intraarticular injection; 6-month follow-up | To assess single PRP injection as a treatment for early moderate chondropathy | GPS mini set, (BIOMET) | 2x-8x | KOOS, VAS scores | Significant improvement in KOOS and VAS scores at 1, 3, and 6 months (P < 0.05) follow-up. |
| Jang et al.26 (2013) | Knee OA (grade not mentioned) | Prospective study; 65 patients; 12-month follow-up | To determine effect duration of a single PRP injection for knee OA | Independent technique | 2.8x-7x | IKDC and VAS scores | VAS score decreased from 7.4 at baseline to 4.2 at 6 months, but increased slightly to 5 at 1 year. Pain relapse was noticed at 8.8 months after the injection. Advanced degeneration stage according to the Kellgren-Lawrence grade reduced the clinical effects of PRP (P < 0.05) and also accelerated the time for relapsing pain (P < 0.05). |
| Halpern et al.27 (2013) | Knee OA. Kellgren-Lawrence grades 1-2 | Prospective cohort study; 22 patients (30-70 years); 1-year follow-up | To investigate whether a single PRP injection for early knee OA is associated with good clinical outcomes and a change in MRI structural appearances | MTF Cascade system | 1.3x-1.7x | WOMAC and VAS scores, and MRI at 1 year | VAS scores significantly decreased, whereas functional and clinical scores (WOMAC and Functional VAS) significantly improved at 6 months and 1 year from baseline. Qualitative MRIs demonstrated no change in at least 73% of cases at 1 year. |
| Say et al.28 (2013) | Symptomatic mild to moderate knee OA (Kellgren-Lawrence grades 1-3) | Prospective study; 90 patients; 3 and 6 months follow-up | To compare the effects of a single PRP versus 3 HA injections in knees with degenerative arthritis | PRGF (BTI, Vitoria, Spain)b | 4x | KOOS and VAS scores | Improved KOOS and VAS scores in the PRP group at 3 and 6 months follow-up. |
| Gobbi et al.29 (2012) | Knee OA. Kellgren-Lawrence grades 1-3 | Prospective case series; 50 patients with 2 intraarticular autologous PRP injections; 25 patients had undergone prior surgical intervention | To determine the effectiveness of intraarticular PRP injections in active patients with knee OA and to evaluate clinical outcomes in patients with and without previous surgical treatment for cartilage lesions. | Regen Lab-ACR C | 2x-2.5x | VAS, IKDC Subjective, KOOS, and Tegner scores | Significant improvement in all scores at 6 and 12 months (P < 0.01); all returned to previous activities. No significant difference in improvement between subgroups (P < 0.01). |
| Filardo et al.30 (2012) | Symptomatic knee degenerative lesions and OA | Prospective clinical study; 144 patients: 72 treated with 3 PRP injections prepared with a single-spinning procedure; 72 with 3 PRP injections prepared with a double-spinning approach. | To compare the safety and efficacy of 2 different approaches of PRP production methods as intraarticular injection treatment for knee cartilage degenerative lesions and osteoarthritis (OA) | Independent technique: Single-spin—580 rpm 8 minutes, 5 mL PRGF. Double-spin—PRP product: 1,800 rpm 15 minutes and 3,500 rpm 10 minutes, 5 mL PRP | 4.5x (1.5x) | IKDC, EQ-VAS, and Tegner scores | Significant clinical improvement with respect to the baseline level in both groups. Better results in younger patients with less cartilage degeneration. |
| Napilitano et al.31 (2012) | Knee OA >1 year | Prospective study; 27 patients (18-81 years) 3 infiltrations of PRP at weekly intervals | To evaluate 3 PRP injections as a treatment for knee OA (first group, Kellgren Lawrence grades 1-3) and degenerative cartilage lesions (second group, Outerbridge grades 1-2) | Regen Lab | 2x-2.5x | NRS and WOMAC scores | Significant improvement in NRS and WOMAC scores at 1 week in both groups; substantial decrease in pain right after the first infiltration (1 week). Improvement in WOMAC scores at 1 week and 6 months in both groups (NRS not measured at 6 months). |
| Spakova et al.32 (2012) | Knee OA; Kellgren Lawrence grades 1-3 | Prospective, cohort study with a control group; 120 patients: 3 injections of PRP versus 3 injections of HA | To find a simple, cost-effective, and time-efficient method for the preparation of PRP and to explore the safety and efficacy PRP application to treat knee OA | Independent technique | 4.5x | WOMAC and the 11-point pain intensity Numeric Rating Scale | Statistically significantly better results in the WOMAC and Numeric Rating Scale scores were recorded in a group of patients who received PRP injections after a 3- and 6-month follow-up. |
| Cerza et al.33 (2012) | Knee gonarthrosis | Randomized controlled trial; 60 patients; 4 PRP injections at weekly intervals versus 60 patients with 4 HA injections at weekly intervals | To compare the clinical response of PRP hyaluronic and HA treatment in 2 groups of patients affected by gonarthrosis | Arthrex ACP | 5x | WOMAC score | PRP had a significant effect which continuously improved up to 24 weeks (P < 0.001). In the HA group, the worst results were obtained for grade III gonarthrosis, whereas the clinical results obtained in the PRP group did not show any statistically significant difference in terms of the grade of gonarthrosis (P < 0.001). |
| Filardo et al.34 (2012) | Knee OA; Kellgren-Lawrence grades 1-3 | Prospective randomized controlled double-blinded trial; 54 PRP injections weekly for 3 weeks versus 55 HA injections weekly for 3 weeks | To compare the clinical efficacy of a series of PRP injections versus a series of HA injections for treatment of knee OA | Independent technique: 150 mL whole blood, 1,480 rpm 6 minutes and 3,400 rpm 15 minutes, 5 mL PRP | 5x | IKDC, EQ-VAS, Tegner, and KOOS scores | Both groups showed clinical improvement but the comparison between the 2 groups showed statistically insignificant difference in all scores. Favorable results for the PRP group in patients with low-grade articular degeneration (Kellgren-Lawrence score up to 2). |
| Sanchez et al.35 (2012) | Knee OA | Randomized, double-blind, HA-controlled, multicenter trial; 176 patients (41-74 years) | To evaluate the efficacy and safety of intraarticular injections of PRGF-Endoret in the treatment of knee OA | PRGF-Endoret (BTI, Vitoria, Spain) | 2x-3x | WOMAC and VAS Pain subscale | Rate of response to PRGF-Endoret (50% decrease in knee pain from baseline to week 24) was 14.1 percentage points higher compared to the HA-treated group. No statistically significant difference between groups in secondary outcomes. |
| Sanchez et al.36 (2012) | Hip OA | Prospective case series; 40 patients; 3 PRP injections, administered weekly | To assess the safety and symptomatic changes of PRP injections in patients with hip OA | PRGF (BTI, Vitoria, Spain) | 2x-3x | WOMAC, VAS, and Harris hip score subscale | Statistically significant reductions in VAS, WOMAC, and Harris hip scores for pain and function at 7 weeks and 6 months. 23 (57.5%) patients reported a clinically relevant reduction of pain. 16 (40%) of these were classified as excellent responders who showed early pain reduction at 6 weeks, which was sustained at 6 months and a parallel reduction of disability. |
| Battaglia et al.37 (2011) | Hip OA; Kellgren Lawrence grades 1-3 | Prospective case series; 20 patients; 3 US-guided injections | To assess efficacy of PRP for hip OA | Independent technique | NA | Harris Hip Score and WOMAC scores | Both HHS and WOMAC scores improved at the 12-month follow-up. An initial clinical improvement was observed at the 1-month and 3-month follow-up, which then decreased, but remained significantly higher at 12 months with respect to the baseline values. |
| Kon et al.38 (2011) | Cartilage degenerative knees and mild to severe knee OA | Prospective comparative study; 50 patients—3 PRP injections; 50 patients—high molecular weight HA injections; 50 patients—low molecular weight HA injections | To compare the efficacy of PRP and HA intraarticular injections for the treatment of knee cartilage degenerative lesions and OA | Independent technique: 150 mL whole blood, 1,480 rpm 6 minutes and 3,400 rpm 15 minutes, 20 mL PRP | 6x | IKDC and EQ-VAS scores | At 2m both PRP and LMW HA groups improved, with better results compared to the HMW HA group (P < 0.005). At 6 months better results were observed in the PRP group (P < 0.005). PRP showed better results in younger patients and early OA stages. |
| Wang-Saegusa et al.39 (2011) | Knee OA; Outerbridge grades 1-4 | Nonrandomized prospective study; 261 patients; 3 intraarticular PRGF injections at 2-week intervals | To assess quality of life and functional capacity following a series of PRP injections for knee OA | PRGF (BTI, Vitoria, Spain) | 2x-3x | VAS, SF-36, WOMAC score, and Lequesne Index | Statistically significant differences (P < 0.0001) between pretreatment and follow-up values were found for pain, stiffness, and functional capacity in the WOMAC Index; pain and total score, distance and daily life activities in the Lequesne Index, the VAS pain score, and the SF-36 physical health domain. |
| Kon et al.40 (2010) | Degenerative cartilage lesions and knee OA | Prospective clinical trial; 91 patients received 3 PRP injections | To investigate the continuous outcomes of PRP injections in knee OA | Independent technique: 150 mL whole blood, 1,800 rpm 15 minutes and 3,500 rpm 10 minutes, 20 mL PRP (15 mL used) | 6x | IKDC Objective and Subjective scores and EQ-VAS score | A statistically significant improvement of all clinical scores was obtained from the basal evaluation to the end of the therapy and at 6 to 12 months follow-up. The results remained stable from the end of the therapy to 6 months follow-up, whereas deterioration of scores was noted and they became significantly worse at 12 months follow-up (P = 0.02), even if still significantly better in respect to the basal level (P < 0.0005). |
| Filardo et al.41 (2011)c | Degenerative cartilage lesions and knee OA | Prospective clinical trial; 91 patients received 3 PRP injections (90 patients available at 2 years) | To investigate the continuous outcomes of PRP injections in knee OA at 2 years | Independent technique; mentioned above | 6x | IKDC Objective and Subjective scores and EQ-VAS score | All parameters deteriorated at 2 years with significantly lower levels with respect to the 12-month evaluation (IKDC Objective dropped from 67% to 59% of normal and nearly normal knees; IKDC Subjective score dropped from 60 to 51), though remaining higher than the basal level; better results in young patients with less cartilage degeneration (P < 0.0005). The median duration of the clinical improvement was 9 months. |
| Sampson et al.42 (2009) | Primary and secondary knee OA | Single-center, uncontrolled prospective preliminary study; 14 patients; 3 PRP injections at 4 weekly intervals | To evaluate the efficacy of PRP injections in treatment of knee OA | GPS system (BIOMET) | 2x-8x | Brittberg-Peterson VAS, and KOOS scores, and cartilage ultrasound at 2, 5, 11, 18, and 52 weeks | Most patients expressed a favorable outcome at 12 months after treatment. Significant and almost linear improvements in KOOS, including pain and symptom relief. Brittberg-Peterson VAS showed many improvements including reduced pain after knee movement and at rest. Cartilage assessment was limited due to a small sample size. The majority of patients expressed a favorable outcome at 12 months after treatment. |
| Sanchez et al.43 (2008) | Knee OA | Observational retrospective cohort study using HA injections as control; 2 groups of 30 patients with 3 weekly injections of PRP or HA | To assess effectiveness of intraarticular injections of PRP (PRGF) versus HA for knee OA | PRGF (BTI, Vitoria, Spain) | 2x-3x | WOMAC score | WOMAC and pain scales improvement at 5 weeks was associated solely with treatment modality in favor of PRGF. |
OA = osteoarthritis; PRP = platelet-rich plasma; HA = hyaluronic acid; WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index; SF-36 = Short Form-36; QOL = quality of life; NA = not available in abstract or full text; KOOS = Knee Injury and Osteoarthritis Outcome Scores; IKDC = International Knee Documentation Committee; EQ-VAS = EuroQoL Visual Analog Scale; BMI = body mass index; PRGF = platelet-derived preparation rich in growth factors; OMERACT-OARSI = Outcome Measures for Rheumatology Committee and Osteoarthritis—Research Society International Standing Committee for Clinical Trials Response Criteria Initiative; MRI = magnetic resonance imaging; NRS = Numerical Rating Scale; US = ultrasound; LMW = low molecular weight; HMW = high molecular weight.
Some patients had both knees included.
Referred to in the article as “Anitua’s Method.”
Same cohort as Kon et al. (2010)40 investigated at follow-up of 2 years.
Discussion
When analyzing the results of our search, what stood out most was the lack of uniformity in treatment protocol with respect to PRP preparation, administration, and dosing. While some articles have mentioned the specific company product that was used for the preparation and reported the platelets concentrations, others have not, presenting an obstacle in the attempts to understand and interpret the results. The large spectrum of variations in treatment protocols included more than 12 different preparation techniques (commercially available and independent noncommercially available methods), different administration protocols varying in number of total injections (from 1 injections up to 9), and intervals between injections (1 week to 1 month). A total of 3 injections was the common protocol used in 18 studies. A 1-week interval was the common protocol used in 10 studies. Additional major differences were noticed in the volumes of PRP injections, which varied from 2 mL to 8 mL; platelet concentrations, which varied from 1.3 times to 8 times the blood concentration; WBC concentration, which varied from none to 4.7 times the blood concentration; and the use of an activator, which varied from none, calcium gluconate, and calcium chloride (the most commonly used, 14 studies). In addition, it is important to mention that some studies did not report all of the above-mentioned parameters (PRP kit used, platelets and WBC concentration, PRP volume, activator used, etc.) as illustrated in Tables 1 and 3 . One study included in our results differed significantly in the administration protocol.24 The authors administered 9 injections of PRP over a 12-month period (6 injections in 6 weeks, a 3-month interruption, followed by 3 additional injections at 1-month intervals). This raises questions regarding the number and frequency of injections, considering there have been reports of improved knee function following protocols that involved less injections and even after only a single injection.25 The injections were initiated 6 weeks after a diagnostic arthroscopy, in which the grade of chondromalacia was determined. The study included a control group, in which mesocaine was injected at the same time points. The PRP preparation method, although described, was independent and data were lacking regarding the leukocytes profile in the preparation and activation. As portrayed in Table 1 , there was lack of consistency with regard to the PRP preparation techniques in the studies in our review. Eleven different types of PRP preparation techniques were used, with the PRGF technique (PRGF-Endoret, BTI, Vitoria, Spain) being the most common (6 studies). Filardo and Kon used a reproducible independent technique in 3 interventions, leading to 4 studies. The rest of the studies separately used 9 different preparation methods, 4 of which were independent and 5 were commercially available systems. There was also variability in terms of the resulting volumes in each injection in different studies, ranging from 3 mL up to 8 mL per injection. Two studies did not report the injected volume. Platelet concentration or level in relation to the basal platelet count were reported in only 12 studies, while information was lacking in 9 studies. The significant differences mentioned above emphasize the great difficulty of analyzing the results of the studies included in this review, as all the parameters mentioned have a direct biological effect on the activity of the administrated PRP preparation. When trying to understand the biological activity of PRP, it should be taken into consideration that PRP contains many prochondrogenic growth factors, including TGF-β1, IGF-1, bFGF, and bone morphogenetic protein-2; however, most preparations also contain high levels of antichondrogenic growth factors, such as VEGF, IGF binding proteins, PDGFs, and EGF. Investigations have shown that although chondrogenic growth factors such as TGF-β1 directly stimulate COL1 production in skin, synovium, and tendons, PRP preparations containing the same amount of TGF-β1 actually inhibit collagen production.43 An insight to this paradoxical action suggests that the platelet concentration of PRP preparations is crucial to its potency and its effect on different conditions and injuries. Preparations containing only moderately elevated platelet concentrations have been suggested to induce optimal biological benefit, whereas lower platelet concentrations produce suboptimal effects and higher concentrations produce inhibitory effects. The “therapeutic dose” of PRP is considered at a range of at least 2 to 6 times higher than the normal platelet count. These observations reflect the complex molecular pool contained in PRP. It is therefore believed that maintaining what can be a delicate balance between pro-chondrogenic and anti-chondrogenic effects is crucial and the volumes of the PRP preparations and platelet concentrations play an important role, emphasizing the importance of optimal characterization of the studied PRP preparations. An additional factor contributing to the biologic characteristics of the PRP preparation is the activation method. Platelet activation triggers degranulation and release of the growth factors. The activation method (endogenous or exogenous with CaCl or CaG) determines the timing and cumulative release of the growth factors. However, this release may continue throughout the platelets’ 7- to 10-day life span,1 thus offering the benefit of maintaining the normal physiologic ratios of these molecules.
Proper terminology for classifying and describing the many different variations of platelet concentrates are essential, especially when comparing results of several studies and analyzing the benefits of these treatments. The need for clarification, terminology, categorization, or classification was highlighted in recent years and yielded several classification systems. The first described and most comprehensive classification system, also known as the Dohan Ehrenfest classification,44 is based on the presence of cell content (mostly leukocytes) and the fibrin architecture. Four main families were defined: Pure Platelet-Rich Plasma (P-PRP)—or Leukocyte-Poor Platelet-Rich Plasma—products are preparations without leukocytes and with a low-density fibrin network after activation; Leukocyte- and Platelet-Rich Plasma (L-PRP) products are preparations with leukocytes and with a low-density fibrin network after activation; Pure Platelet-Rich Fibrin (P-PRF)—or Leukocyte-Poor Platelet-Rich Fibrin—are preparations without leukocytes and with a high-density fibrin network; and Leukocyte- and Platelet-Rich Fibrin (L-PRF) products are preparations with leukocytes and with a high-density fibrin network. This terminology and classification are now considered as a basis of consensus in many fields. Another 2 classification systems were proposed in recent years, but are considered limited and applicable for sports medicine applications only. These are the Mishra classification and the PAW classification. Mishra et al.45 proposed a classification that takes into consideration the presence of leukocytes, activation of platelets, and platelets concentration. This classification established 4 types of PRP: type 1 PRP is an L-PRP solution, type 2 PRP is an L-PRP gel (with activation), type 3 PRP is P-PRP solution, type 4 PRP is a P-PRP gel (with activation). Each type can be described as an A or B subtype. A subtype is 5 times or more the blood concentration of platelets, and B subtype is less than 5 times the blood concentration of platelets. The PAW classification46 is similar to the Mishra classification and is based on the absolute number of platelets, the manner in which platelet activation occurs, and the presence or absence of white cells. Table 3 illustrates the different PRP preparations used in the studies included in this review according to currently used classifications.
Only 2 studies were PRP controlled, one comparing different PRP administration protocol: 1 versus 2 PRP injections23 and the other comparing different preparation method: single spinning versus double spinning procedures.30 Both studies showed no significant changes between groups. These studies emphasize the fact that current literature is lacking randomized controlled studies aimed to introduce the optimal PRP treatment (preparation characteristics, administration protocol, etc.) for knee or hip OA.
Randomized Controlled Trials
Nine RCTs were included in the results,15,16,21-23,33-35,38 3 of which were double blinded ( Table 2 ). Hyaluronic acid was used for the control groups in 7 RCTs, saline was used in 1 study, and an exercise program was used in another.
Eight studies targeted knee OA whereas 1 study targeted hip OA.21 The follow-up period in these studies ranged from 6 to 12 months.
Overall, all RCTs reported on improved symptoms at the last follow-up when compared to the baseline scores; however, 2 RCTs—one for knee OA34 and one for hip OA21—did not report significantly superior results for the PRP group compared to the control group (HA). All other studies showed significantly better results for the PRP group.
In a multicenter study,35 the efficacy and safety of intraarticular injections of PRGF were evaluated in 176 patients with knee OA (aged 41-74 years). At 6-month follow-up, the PRGF group had significantly more patients who achieved greater than 50% decrease in the WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) pain score, compared to the HA group; however, although absolute WOMAC and VAS (Visual Analog Scale) scores were better in the PRGF group, there was almost no statistical significance compared to the HA hyaluronan group. In a double-blinded RCT,34 Filardo et al. found no statistically significant difference between the PRP and the HA treated groups. A trend favorable of the PRP group was only found in patients with low-grade articular degeneration (Kellgren-Lawrence score up to 2) at 6 and 12 months of follow-up. In another RCT, Cerza et al.33 compared treatment with ACP in 60 patients with knee OA to 60 patients treated with HA. The PRP showed a significant effect using the WOMAC score, which continuously improved up to 24 weeks (P < 0.001). In the HA group, the worst results were obtained for grade III gonarthrosis, whereas the clinical results obtained in the PRP group did not show any statistically significant difference in terms of the grade of gonarthrosis (P < 0.001). In their RCT, Patel et al.23 used saline injections for the control group. The study included 78 patients with bilateral knee OA, divided into 3 groups: single PRP injection (n = 52 knees); 2 PRP injections (n = 50 knees); single saline injection (n = 46 knees). Significant improvement in WOMAC score was recorded at all follow-ups (1.5, 3, and 6 months) when PRP was administered, compared to the saline group, with no difference between the single and double injections groups. An interesting finding in this study was that the improvement was maximal at first follow-up with deterioration in the second and third follow-ups, suggesting a temporary nature of the benefits of PRP injections. In their multicenter RCT, Vaquerizo et al.22 compared 3 injections of PRGF to one single intraarticular injection of HA. Each group included 48 patients. They reported that PRGF was significantly more efficient than treatment with Durolane HA in reducing knee pain and stiffness and improving function in patients with knee OA. The rate of response to PRGF was significantly higher than the rate of response to HA for all scores including pain, stiffness, and function on the WOMAC, Lequesne index, and OMERACT-OARSI responders at 24 and 48 weeks. In the most recent RCT,15 Raeissadat et al. compared 2 intraarticular injections of PRP (Rooyagen Kit) to 3 injections of Hyalgan HA for patients with knee OA. The PRP group included 87 patients and the HA group 73 patients. At the 12-month follow-up, WOMAC pain score and bodily pain significantly improved in both groups; however, better results were determined in the PRP group compared to the HA group (P < 0.001). Other WOMAC and SF-36 (Short Form-36) parameters improved only in the PRP group. Another interesting RCT by Raeissadat et al.16 compared intraarticular PRP injections and a prescribed exercise program with a prescribed exercise program alone. After 6 months, the mean changes of total WOMAC, physical component summery, and mental component summery of SF-36 in the PRP group showed better improvement than the control group (P < 0.05). Only 1 RCT by Battaglia et al.21 investigated intraarticular injections of PRP and HA in hip OA. One hundred patients with symptomatic hip OA were randomly assigned to 1 of 2 groups: group A received PRP and group B received HA intraarticular injections. Patients were evaluated at baseline and after 1, 3, 6, and 12 months using the Harris Hip Score (HHS) and visual analog scale (VAS). An overall improvement was detected in both groups between 1- and 3-month follow-up. Despite a slightly progressive worsening between 6- and 12-month follow-up, the final clinical scores remained higher compared with baseline (P < 0.0005), with no significant differences between PRP and HA.
HA Controlled Studies
Nine out of 11 HA controlled studies (7 RCTs, 2 prospective comparative studies, and 2 retrospective cohorts) showed significantly better results in the PRP groups. In most of the studies, improvement in pain and functional scales was noted in both the HA and PRP groups, with significantly better results in the PRP groups. Most studies in this subgroup followed the participants up to 6 months (6 studies), while 4 studies had a follow-up of up to 12 months. One study followed the patients only for 5 weeks.43 In a prospective double-blinded RCT34 both groups showed clinical improvement, and the comparison between the 2 groups showed statistically insignificant difference in all scores. In a recently published randomized controlled clinical trial (160 patients),15 87 patients received 2 PRP injections and 73 received 3 HA injections. At the 12-month follow-up, WOMAC pain score and bodily pain significantly improved in both groups; however, better results were determined in the PRP group compared to the HA group (P < 0.001). Other WOMAC and SF-36 parameters improved only in the PRP group. More improvement (not statistically significant) was achieved in patients with grade 2 OA in both the groups.
Prospective Case Series
Positive results for PRP treatment in knee and hip OA was evident in all 14 prospective case series studies included. These studies showed improvement in pain and functional performance compared to pretreatment measurements for follow-ups of up to 24 months. The majority of studies followed the patients up to 12 months. However, a deterioration in the positive effect of PRP was also noted during follow-up time. Kon et al.40 showed a 9-month median duration of clinical improvement for knee OA patients treated with PRP. Despite this deterioration, functional and pain scores remained higher than the basal level of pretreatment in all studies.
Follow-Up Period
The majority of studies reported a follow-up period of 12 months (13 studies) or 6 months (12 studies). The shortest follow-up was 5 weeks in one study.43 In a prospective study including 91 patients, a follow-up of 24 months has been reported.40,41 In this study group, patients received 3 intraarticular PRP injections at monthly intervals showed symptomatic improvement at 12 months but significant worsening of symptoms at 2 years with respect to the 12-month evaluation (IKDC [International Knee Documentation Committee] objective decreased from 67% to 59% of normal and nearly normal knees; IKDC subjective score decreased from 60 to 51), although they remained higher than the basal level. This is an interesting finding and reiterates the need for studies with longer follow-ups. A closer analysis of the data in this study revealed that older patients had a weaker response compared to younger patients (P = 0.049) and that only 30% of patients over 65 years of age with advanced OA showed significant improvement. In another study with a follow-up of 24 months, 50 knees were randomly selected from 119 knees and received a second cycle of PRP injection at the completion of 1 year from first cycle. At 12 months, both groups showed similar and significant improvement. At 18 months, except for KOOS (Knee Injury and Osteoarthritis Outcome Score–Symptoms) and Tegner score, all other parameters showed a significant difference between the 2 groups in favour of the patients who had received the second cycle (P < 0.001). At 2 years, the scores declined in both groups but remained above the pretreatment value with no significant difference between the groups. This study raises many questions with regard to the temporary effect of PRP treatment and the proper ways of prolonging its positive effect.
Level of OA
A trend toward better results for PRP injections in patients with early knee OA changes and young age was observed in several studies.15,20,26,30,34,38 This might suggest that PRP treatment should be considered more seriously in this subgroup. It is important to mention that improved outcomes have been shown in up to grade 3 OA (according to the Kellgren-Lawrence classification).25,26
Lack of uniformity was evident in terms of indications, inclusion criteria, pathology definitions, and classifications used in the different studies. In the knee studies, not all authors reported the degree of OA or degeneration, using a general description such as “degenerative joint disease,” or “primary and secondary OA,” or even “osteoarthritis,” whereas others varied in the classifications used to quantify the level of OA. Another variable posing difficulty in uniformly assessing the data was regarding the methods of reporting the level of OA treated. The Outerbridge classification47 was used to describe the lesions in 2 studies,4,25 and another study35 used the Ahlback classification,48 whereas the Kellgren-Lawrence classification49 was used in most others (18 studies). Some studies have simply used the broad term “early to severe OA.”23,33,26 Although most authors used the Kellgren-Lawrence classification, there was variability in the grades included in the studies, with some focusing only on grades 0 to 2 and others including also grade 3 and even grade 4. Six studies included patients with grade 0 Kellgren-Lawrence,20,27,30,38,40,41 meaning symptomatic knees with no radiographic signs of OA, which could potentially add additional confounding factors to the results. Not all studies describe the distribution of the study population according to the OA grades. Although these studies have targeted degenerative cartilage pathology, the range of the age group included has been as wide as from 18 years to 81 years,25,31 which could possibly generate a bias in the results.
Activator Use
Fourteen studies reported use of an activator right before PRP injection, with the majority14 using calcium chloride 10%. Platelet activation triggers degranulation and release of the growth factors. The activation method determines the timing and cumulative release of the growth factors. However, this release may continue throughout the platelets’ 7- to 10-day life span,1 thus offering the benefit of maintaining the normal physiologic ratios of these molecules.
Imaging Evaluation
Two studies were using imaging modalities to evaluate cartilage changes following PRP administration. In an uncontrolled prospective study, in which 14 patients with knee OA were treated with PRP, the authors reported improvement using ultrasonographic measurement of femoral articular cartilage thickness in 6 out of 13 patients at 6-month follow-up.42 In a prospective study by Halpern et al.27 involving 22 patients, qualitative magnetic resonance imaging was performed at baseline and at 1 year of follow-up, demonstrated no change in at least 73% of cases at 1 year. Although these studies involved a small sample size and a short-term follow-up period, they point out the need for a more objective measure to evaluate the effects of PRP on cartilage, as none of the other studies used an arthroscopic or consistent radiological evaluation after treatment administration to assess cartilage regeneration and tissue histopathology for regenerative features.
Adverse Effects
Only 7 studies reported on mild and self-limiting adverse effects in a small number of patients.
Filardo et al.20 reported mild pain and/or slight swelling, which resolved spontaneously within 24 to 48 hours, without reporting number of patients. Vaquerizo et al.22 reported mild postinjection pain after PRGF injection in 8 patients (out of 48). Patel et al.23 reported nonspecific 19 adverse effects during the course of PRP treatment (148 knees). These included local pain, stiffness, syncope, dizziness, headache, nausea, sweating, and tachycardia, all self-limited. Filardo et al.30 reported temporary pain and swelling reaction for the PRP treatment (number of patients not mentioned). Spakova et al.32 documented temporary mild worsening of pain in the knee joint after application of PRP in 6 cases (out of 60), which was spontaneously resolved after 2 days. Sporadic adverse effects of temporary mild rash, local numbness, and itching sensation were also reported.35,36
PRP for Hip OA
Only 3 studies21,36,37 have been conducted to assess the efficacy of PRP for OA of the hip joint. While the first, published in 2011, showed clinical improvement in the short term, follow-up at 1 year was not as good. In a larger group of 40 patients, Sanchez et al.36 reported 57.5% patients had clinically relevant relief of pain, assessed by the WOMAC subscale. Of these, 40% were classified as excellent responders who showed early pain reduction at 6 weeks, which was sustained at 6 months, with a parallel reduction of disability. A notable observation in this study was that 10 of the 11 patients in which treatment was not effective had a higher grade of hip OA (Tonnis grade 3). The authors concluded that PRP was effective for the management of pain from OA of the hip. However, the criteria for significance defined in the study was a 30% reduction in pain and disability, which, as shown by Richette et al.,50 can also be achieved with a placebo. In a recent randomized controlled clinical trial (100 patients),21 Battaglia et al. compared the clinical efficacy of PRP versus HA at 12 months of follow-up in patients with hip OA. They showed that an overall improvement was detected in both groups between 1- and 3-month follow-up. Despite a slightly progressive worsening between 6- and 12-month follow-up, the final clinical scores remained higher compared with baseline (P < 0.0005), with no significant differences between PRP and HA.
Leukocyte Concentration
Leukocyte concentration in PRP preparations is another major confounding factor when analyzing the results included in this study. There is no doubt that leukocytes have a biological effect that must be understood. The difficulty of reaching an acceptable conclusion or trend when considering the optimal leukocyte concentration is based on the large spectrum of leukocytes content in PRP preparations injected in the studies reviewed and the lack of an acceptable and clear definition of what can be considered leukocyte rich or poor concentration. As reported in the studies included in this review, 5 studies used PRP preparations with leukocytes content above blood concentration (1.2 to 4.7 times the blood concentration), 9 used leukocytes containing preparations, 13 used minimal or no leukocytes preparations, and 2 studies did not report on leukocyte content. No trend related to leukocyte content and better or worse results was identifiable. This issue is of major relevance in future studies to better understand the role of leukocytes content in PRP preparations. It is essential that the terms “leukocyte rich” and “leukocyte poor” be defined more precisely and perhaps a third group of leukocyte blood concentration should be introduced for that matter.
Despite the obvious methodological variability, all studies seem to show overall positive results and a clinical benefit for the use of PRP. These benefits are emphasized in RCTs when compared to HA as a control15,22,33-35 and even saline.23 The duration of these benefits is still very controversial, as long-term follow-up studies are lacking, and many of the existing studies report only up to 6 months of follow-up. Studies with 1 year of follow-up are inconsistent in terms of the outcomes at this time point, with some reporting an improvement trend and others already showing deterioration at this time point. One study26 observed relapsed pain 8.8 months after PRP treatment. This is an important aspect when assessing the benefits of PRP treatment, suggesting it has a limited or short-term effect that might necessitate further treatment cycles to maintain and prolong these effects.
It should be emphasized that no correlation was found between better results and any specific type of PRP characteristics and/or administration protocol. Any discussion involving PRP therapies should carefully acknowledge the differences between the preparations and the administration procedures used. Regardless of the fact that pure PRP and leukocyte PRP formulations are not comparable in terms of leukocyte content, platelet count, or plasma volume, the resulting improvements in pain and function were not exclusive to any type of formulation. This finding leaves the mystery of the optimal PRP treatment (protocol and formulation) as an exciting challenge for future research.
As described earlier, intraarticular PRP injections are as safe as other intraarticular injection treatments and present no significant risk for serious adverse effect. In a minority of patients, adverse effects were minor and temporary, with no long-term implications.
Conclusion
Current clinical studies evidence support the concept that PRP treatment can be beneficial for degenerative joint pathology in the knee and hip. It has been proven to temporarily relieve pain and function of the involved joint with superior results compared with several alternative treatments. Current variability in methodologies used in different studies and the numerous PRP preparation methods, in addition to the highly inconsistent systems to classify PRP formulations, make it difficult to establish firm and uniform recommendations and guidelines regarding which type of PRP to use and for which indications. A broad overview of the results clearly implies a positive influence of PRP on knee OA with encouraging clinical results in almost all the studies included in this review. The simplicity and safety of PRP use makes it an interesting and promising option for both researchers and clinicians. Further research with RCTs that will address the issues of the optimal preparation protocol and formulation of intraarticular PRP injections for OA of the knee, hip, and other joints, as well as longer follow-ups and larger population sizes is of major need.
Footnotes
Acknowledgments and Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1. Foster TE, Puskas BL, Mandelbaum BR, Gerhardt MB, Rodeo SA. Platelet-rich plasma: from basic science to clinical applications. Am J Sports Med. 2009;37(11):2259-72. [DOI] [PubMed] [Google Scholar]
- 2. Curl WW, Krome J, Gordon ES, Rushing J, Smith BP, Poehling GG. Cartilage injuries: a review of 31,516 knee arthroscopies. Arthroscopy. 1997;13(4):456-60. [DOI] [PubMed] [Google Scholar]
- 3. Buckwalter JA, Brown TD. Joint injury, repair, and remodeling: roles in post-traumatic osteoarthritis. Clin Orthop Relat Res. 2004;(423):7-16. [PubMed] [Google Scholar]
- 4. Kon E, Filardo G, Drobnic M, Madry H, Jelic M, van Dijk N, et al. Non-surgical management of early knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2012;20(3):436-49. [DOI] [PubMed] [Google Scholar]
- 5. Hochberg MC, Altman RD, Brandt KD, Clark BM, Dieppe PA, Griffin MR, et al. Guidelines for the medical management of osteoarthritis. Part II. Osteoarthritis of the knee: American College of Rheumatology. Arthritis Rheum. 1995;38(11):1541-6. [DOI] [PubMed] [Google Scholar]
- 6. Ulrich-Vinther M, Maloney MD, Schwarz EM, Rosier R, O’Keefe RJ. Articular cartilage biology. J Am Acad Orthop Surg. 2003;11(6):421-30. [DOI] [PubMed] [Google Scholar]
- 7. Chubinskaya S, Hakimiyan A, Pacione C, Yanke A, Rappoport L, Aigner T, et al. Synergistic effect of IGF-1 and OP-1 on matrix formation by normal and OA chondrocytes cultured in alginate beads. Osteoarthritis Cartilage. 2007;15(4):421-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Longobardi L, O’Rear L, Aakula S, Johnstone B, Shimer K, Chytil A, et al. Effect of IGF-I in the chondrogenesis of bone marrow mesenchymal stem cells in the presence or absence of TGF-beta signaling. J Bone Miner Res. 2006;21(4):626-36. [DOI] [PubMed] [Google Scholar]
- 9. Shi S, Mercer S, Eckert GJ, Trippel SB. Growth factor regulation of growth factors in articular chondrocytes. J Biol Chem. 2009;284(11):6697-704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dohan Ehrenfest DM, Rasmusson L, Albrektsson T. Classification of platelet concentrates: from pure platelet-rich plasma (P-PRP) to leucocyte- and platelet-rich fibrin (L-PRF). Trends Biotechnol. 2009;27(3):158-67. [DOI] [PubMed] [Google Scholar]
- 11. Akeda K, An HS, Okuma M, Attawia M, Miyamoto K, Thonar EJ, et al. Platelet-rich plasma stimulates porcine articular chondrocyte proliferation and matrix biosynthesis. Osteoarthritis Cartilage. 2006;12(12):1272-80. [DOI] [PubMed] [Google Scholar]
- 12. Spreafico A, Chellini F, Frediani B, Bernardini G, Niccolini S, Serchi T, et al. Biochemical investigation of the effects of human platelet releasates on human articular chondrocytes. J Cell Biochem. 2009;108(5):1153-65. [DOI] [PubMed] [Google Scholar]
- 13. Bendinelli P, Matteucci E, Dogliotti G, Corsi MM, Banfi G, Maroni P, et al. Molecular basis of anti-inflammatory action of platelet rich plasma on human chondrocytes: mechanisms of NF-kB inhibition via HGF. J Cell Physiol. 2010;225(3):757-66. [DOI] [PubMed] [Google Scholar]
- 14. Anitua E, Sánchez M, Nurden AT, Zalduendo MM, de la, Fuente M, Azofra J, et al. Platelet-released growth factors enhance the secretion of hyaluronic acid and induce hepatocyte growth factor production by synovial fibroblasts from arthritic patients. Rheumatology (Oxford). 2007;46(12):1769-72. [DOI] [PubMed] [Google Scholar]
- 15. Raeissadat SA, Rayegani SM, Hassanabadi H, Fathi M, Ghorbani E, Babaee M, et al. Knee osteoarthritis injection choices: platelet-rich plasma (PRP) versus hyaluronic acid (a one-year randomized clinical trial). Clin Med Insights Arthritis Musculoskelet Disord. 2015;8:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rayegani SM, Raeissadat SA, Taheri MS, Babaee M, Bahrami MH, Eliaspour D, et al. Does intra articular platelet rich plasma injection improve function, pain and quality of life in patients with osteoarthritis of the knee? A randomized clinical trial. Orthop Rev (Pavia). 2014;6(3):5405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Guler O, Mutlu S, Isyar M, Seker A, Kayaalp ME, Mahirogullari M. Comparison of short-term results of intraarticular platelet-rich plasma (PRP) and hyaluronic acid treatments in early-stage gonarthrosis patients. Eur J Orthop Surg Traumatol. 2015;25(3):509-13. [DOI] [PubMed] [Google Scholar]
- 18. Mangone G, Orioli A, Pinna A, Pasquetti P. Infiltrative treatment with platelet rich plasma (PRP) in gonarthrosis. Clin Cases Miner Bone Metab. 2014;11(1):67-72. [PMC free article] [PubMed] [Google Scholar]
- 19. Gobbi A, Lad D, Karnatzikos G. The effects of repeated intra-articular PRP injections on clinical outcomes of early osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2015;23(8):2170-7. [DOI] [PubMed] [Google Scholar]
- 20. Filardo G, Kon E, DI Matteo B, DI Marino A, Sessa A, Merli ML, et al. Leukocyte-poor PRP application for the treatment of knee osteoarthritis. Joints. 2014;1(3):112-20. [PMC free article] [PubMed] [Google Scholar]
- 21. Battaglia M, Guaraldi F, Vannini F, Rossi G, Timoncini A, Buda R, et al. Efficacy of ultrasound-guided intra-articular injections of platelet-rich plasma versus hyaluronic acid for hip osteoarthritis. Orthopedics. 2013;36(12):e1501-8. [DOI] [PubMed] [Google Scholar]
- 22. Vaquerizo V, Plasencia MÁ, Arribas I, Seijas R, Padilla S, Orive G, et al. Comparison of intra-articular injections of plasma rich in growth factors (PRGF-Endoret) versus Durolane hyaluronic acid in the treatment of patients with symptomatic osteoarthritis: a randomized controlled trial. Arthroscopy. 2013;29(10):1635-43. [DOI] [PubMed] [Google Scholar]
- 23. Patel S, Dhillon MS, Aggarwal S, Marwaha N, Jain A. Treatment with platelet-rich plasma is more effective that placebo for knee osteoarthritis: a prospective, double-blind, randomized trial. Am J Sports Med. 2013;41(2):356-64. [DOI] [PubMed] [Google Scholar]
- 24. Hart R, Safi A, Komzák M, Jajtner P, Puskeiler M, Hartová P. Platelet-rich plasma in patients with tibiofemoral cartilage degeneration. Arch Orthop Trauma Surg. 2013;133(9):1295-301. [DOI] [PubMed] [Google Scholar]
- 25. Torrero JI, Aroles F, Ferrer D. Treatment of knee chondropathy with platelet rich plasma. Preliminary results at 6 months of follow up with only one injection. J Biol Regul Homeost Agents. 2012;26(2 Suppl. 1):71s-78s. [PubMed] [Google Scholar]
- 26. Jang SJ, Kim JD, Cha SS. Platelet rich plasma (PRP) injections as an effective treatment for early osteoarthritis. Eur J Orthop Surg Traumatol. 2013;23(5):573-80. [DOI] [PubMed] [Google Scholar]
- 27. Say F, Gürler D, Yener K, Bülbül M, Malkoc M. Platelet-rich plasma injection is more effective than hyaluronic acid in the treatment of knee osteoarthritis. Acta Chir Orthop Traumatol Cech. 2013;80(4):278-83. [PubMed] [Google Scholar]
- 28. Halpern B, Chaudhury S, Rodeo SA, Hayter C, Bogner E, Potter HG, et al. Clinical and MRI outcomes after plateletrich plasma treatment for knee osteoarthritis. Clin J Sport Med. 2013;23(3):238-9. [DOI] [PubMed] [Google Scholar]
- 29. Gobbi A, Karnatzikos G, Mahajan V, Malchira S. Treatment in symptomatic patients with knee osteoarthritis: preliminary results in a group of active patients. Sports Health. 2012;4(2):162-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Filardo G, Kon E, Pereira Ruiz MT, Vaccaro F, Guitaldi R, Di Martino A, et al. Platelet-rich plasma intra-articular injections for cartilage degeneration and osteoarthritis: single- versus double-spinning approach. Knee Surg Sports Traumatol Arthrosc. 2012;20(10):2082-91. [DOI] [PubMed] [Google Scholar]
- 31. Napolitano M, Matera S, Bossio M, Crescibene A, Costabile E, Almolla J, et al. Autologous platelet gel for tissue regeneration in degenerative disorders of the knee. Blood Tranfus. 2012;10(1):72-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Spaková T, Rosocha J, Lacko M, Harvanová D, Gharaibeh A. Treatment of knee joint osteoarthritis with autologous platelet-rich plasma in comparison with hyaluronic acid. Am J Phys Med Rehabil. 2012;91(5):411-7. [DOI] [PubMed] [Google Scholar]
- 33. Cerza F, Carnì S, Carcangiu A, Di Vavo I, Schiavilla V, Pecora A, et al. Comparison between hyaluronic acid and platelet-rich plasma, intra-articular infiltration in the treatment of gonarthrosis. Am J Sports Med. 2012;40(12):2822-7. [DOI] [PubMed] [Google Scholar]
- 34. Filardo G, Kon E, Di Martino A, Di Matteo B, Merli ML, Cenacchi A, et al. Platelet-rich plasma vs hyaluronic acid to treat knee degenerative pathology: study design and preliminary results of a randomized controlled trial. BMC Musculoskeletal Disord. 2012;13:229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sánchez M, Fiz N, Azofra J, Usabiaga J, Aduriz Recalde E, Garcia Gutierrez A, et al. Randomized clinical trial evaluating plasma rich in growth factors (PRGF-Endoret) versus hyaluronic acid in the short-term treatment of symptomatic knee osteoarthritis. Arthroscopy. 2012;28(8):1070-8. [DOI] [PubMed] [Google Scholar]
- 36. Sánchez M, Guadilla J, Fiz N, Andia I. Ultrasound-guided platelet-rich plasma injections for the treatment of osteoarthritis of the hip. Rheumatology (Oxford). 2012;51(1):144-50. [DOI] [PubMed] [Google Scholar]
- 37. Battaglia M, Guaraldi F, Vannini F, Buscio T, Buda R, Galletti S, et al. Platelet-rich plasma (PRP) intra-articular ultrasound-guided injections as a possible treatment for hip osteoarthritis: a pilot study. Clin Exp Rheumatol. 2011;29(4):754. [PubMed] [Google Scholar]
- 38. Kon E, Mandelbaum B, Buda R, Filardo G, Delcogliano M, Timoncini A, et al. Platelet-rich plasma intra-articular injection versus hyaluronic acid viscosupplementation as treatments for cartilage pathology: from early degeneration to osteoarthritis. Arthroscopy. 2011:27(11):1490-501. [DOI] [PubMed] [Google Scholar]
- 39. Wang-Saegusa A, Cugat R, Ares O, Seijas R, Cuscó X, Garcia-Balletbó M. Infiltration of platelet rich in growth factors for osteoarthritis of the knee short-term effects on function and quality of life. Arch Orthop Trauma Surg. 2011;131(3):311-7. [DOI] [PubMed] [Google Scholar]
- 40. Kon E, Buda R, Filardo G, Di Martino A, Timoncini A, Cenacchi A, et al. Platelet-rich plasma: intra-articular knee injections produced favorable results on degenerative cartilage lesions. Knee Surg Sports Traumatol Arthrosc. 2010;18(4):472-9. [DOI] [PubMed] [Google Scholar]
- 41. Filardo G, Kon E, Buda R, Timoncini A, Di Martino A, Cenacchi A, et al. Platelet-rich plasma intra-articular knee injections for the treatment of degenerative cartilage lesions and osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2011;19(4):528-35. [DOI] [PubMed] [Google Scholar]
- 42. Sampson S, Reed M, Silvers H, Meng M, Mandelbaum B. Injection of platelet-rich plasma in patients with primary and secondary knee osteoarthritis: a pilot study. Am J Phys Med Rehabil. 2010;89(12):961-9. [DOI] [PubMed] [Google Scholar]
- 43. Sánchez M, Anitua E, Azofra J, Aguirre JJ, Andia I. Intra-articular injection of an autologous preparation rich in growth factors for the treatment of knee OA: a retrospective cohort study. Clin Exp Rheumatol. 2008;26(5):910-3. [PubMed] [Google Scholar]
- 44. Dohan Ehrenfest DM, Andia I, Zumstein MA, Zhang CQ, Pinto NR, Bielecki T. Classification of platelet concentrates (platelet-rich plasma—PRP, platelet-rich fibrin—PRF) for topical and infiltrative use in orthopedic and sports medicine: current consensus, clinical implications and perspectives. Muscles Ligaments Tendons J. 2014;4(1):3-9. [PMC free article] [PubMed] [Google Scholar]
- 45. Mishra A, Harmon K, Woodall J, Vieira A. Sports medicine applications of platelet rich plasma. Curr Pharm Biotechnol. 2012;13(7):1185-95. [DOI] [PubMed] [Google Scholar]
- 46. DeLong JM, Russell RP, Mazzocca AD. Platelet-rich plasma: the PAW classification system. Arthroscopy. 2012;28(7):998-1009. [DOI] [PubMed] [Google Scholar]
- 47. Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43-B:752-7. [DOI] [PubMed] [Google Scholar]
- 48. Ahlbäck S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh). 1968:Suppl 277:7-72. [PubMed] [Google Scholar]
- 49. Kellgern JH, Lawrence JS. Radiological assessment of osteoarthrosis. Ann Rheum Dis. 1957;16(4):494-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Richette P, Ravaud P, Conrozier T, Euller-Ziegler L, Mazières B, Maugars Y, et al. Effect of HA in symptomatic hip osteoarthritis: a multicenter, randomized, placebo-controlled trial. Arthritis Rheum. 2009;60(3):824-30. [DOI] [PubMed] [Google Scholar]


