Abstract
A 53-year-old man with ulcerative colitis (UC) suffered fatal acute interstitial pneumonitis (AIP) post completing an accelerated infliximab induction course. This is the first case reported in this setting. A literature review found four similar cases of infliximab-induced interstitial lung disease in the setting of treating patients with UC using standard infliximab regimens had successful treatment of the subjects post infliximab discontinuation. Unfortunately, the patient we are presenting, who had an accelerated infliximab induction course, did not survive. Although a prior small trial along more recent new small studies continue to show a benefit in reducing the need for early colectomy with the accelerated infliximab induction regimen as salvage therapy, it should be used cautiously until more safety data are available. Further larger trials are required to investigate rare side effects that may be associated with this regimen such as rapidly progressive lung toxicity as seen in this patient.
Keywords: Mechanical ventilation, Respiratory system, Ulcerative colitis, Interstitial lung disease, Mechanical ventilation
Background
Ulcerative colitis (UC) is an inflammatory bowel disease that causes chronic inflammation of the large bowel with flare relapses that vary in frequency rate and severity among affected patients.1 Although many treatment options exist for UC, some patients are intolerant to the different medication regimens available. Another common problem is that most regimens, aside from corticosteroids, take weeks to months to see their full effect in treating UC.1 2 Although surgery can sometimes be curative, most patients prefer other alternatives in hope for better quality of life.1 Among the salvage therapy options for severe flares, in efforts of avoiding surgery, is the use of biological agents, such as infliximab, in an accelerated dosing regimen as supported by some small studies.1–3 This may be at the expense of experiencing some more side effects, which rarely sometimes may be severe or fatal and should be considered when making that choice. To our knowledge, these rare and fatal side effects of biological agents, and more specifically infliximab, including lung toxicity in the form of rapidly progressive interstitial lung disease have not been examined in the few studies using the accelerated dosing regimen of this drug in the salvage therapy of severe UC to avoid total colectomy. We also review current medical literature related to the management of infliximab-induced acute interstitial lung disease in patients with severe UC.
Infliximab, a commonly used biological tumour necrosis factor alpha (TNF-α) monoclonal antibody agent, used in the treatment of severe UC is associated with many important adverse drug reactions.4–7 Although infusion-related reactions may be the most common, other side effects are related to their effect on the immune system and include opportunistic infections, reactivation of mycobacteria tuberculosis, developing lymphomas, and lupus-like syndromes.5 6 Infliximab binds both the soluble (free-form) and trans-membrane form of TNF-α with high affinity, and thus prevents it from binding to its receptors. Many immune cells including macrophages, monocytes and lymphocytes produce TNF-α in response to tumours, viruses, bacteria, fungal infections and parasites. Its immune system-related function consists of apoptosis of certain damaged or infected cells, propagating an inflammatory cascade and induction of cytokines involved in the recruitment of other inflammatory cells to the infection site, thereby cell activation. In addition, it is also involved in granuloma formation, which is a key component of the immune system in fighting off mycobacterial infections.5 8 By targeting this potent inflammatory factor as its beneficial therapeutic mechanism of action, infliximab also suppresses one of the main pathways that the immune system uses in fighting off infections.8
Case presentation
A 53-year-old man admitted for actively severe, recurrent left-sided UC was started on an accelerated induction regimen of Infliximab therapy in order to avoid requiring surgical intervention and total colectomy. With the exception of UC and successfully treated early adulthood active tuberculosis, the patient had no other cardiac or respiratory relevant medical history.
The patient has been battling recurrent flares of frequent loose bloody stools since his diagnosis of UC with proctitis in 2004. His gastroenterologist monitored the patient in the community with records indicating a normal appearing distal colon on sigmoidoscopy in September 2014. The patient had a history of severe intolerance to any of the commonly used anti-metabolite immunosuppressants, such as azathioprine and 6-mercaptopurines, as he developed severe vomiting to the point of dehydration while on them in the past. However, he has been managed well on oral Mesalamine (a 5-aminosalicylic acid derivative) up until 1 month prior to his present admission, when he developed frequent bloody bowel movements occurring two to three times per hour during the morning and as frequent as hourly overnight. The patient’s most recent colonoscopy in January 2015 demonstrated progression with severe colitis beginning at the distal portion of the transverse colon extending to the proximal rectum. His CRP was elevated at 54 mg/L and he showed signs of anaemia with a haemoglobin of 8.1 g/dL (baseline during remission was 12.5 g/dL) and hypoalbuminemia (albumin of 24 g/L). He had an overall Mayo clinical and endoscopic score of 11 out of 12 indicating severe disease. Despite aggressive outpatient treatment with a high-dose oral corticosteroid for over 3 weeks, the patient’s condition remained refractory to therapy and he continued to experience frequent bloody stools. As a result of his dehydration and severe exacerbation, his gastroenterologist referred him to the emergency department for admission and initiation of intravenous corticosteroids, nutritional management and consideration for treatment with infliximab. It is important to note that the patient refused the surgical treatment alternative, which was presented and discussed with him at the time. Instead, the patient preferred to attempt the induction therapy with Infliximab first.
In order to avoid surgery for his rapidly progressive disease flare-up, an accelerated induction regimen of infliximab was presented to the patient in an attempt to achieve control of his condition sooner. The recommendation and initiation of the accelerated infliximab regimen was based on a single retrospective study in Ireland.1 The small study, which was conducted over 8 years, from 2005 to 2013, in a single academic centre, found a reduction in need for early colectomy with the accelerated induction regimen after analysing 50 hospitalised patients who received infliximab for severe subacute UC refractory to steroid therapy.1 The accelerated induction regimen was over 24 days as opposed to the standard 42-day course.1 4 Since data were limited, the risks and benefits of the alternative treatment options were discussed extensively with the patient and his spouse prior to induction. The patient ended up receiving 3 doses of Infliximab over a 32-day period along with intravenous corticosteroids, which initially seemed to control his UC symptoms relatively well. His daily number of bowel movements, although still loose, was down to 3 to 4 per day and they were non-bloody in nature. His CRP, albumin and haemoglobin levels all improved to 7.5 mg/L, 29 g/L and 9.7 g/dL, respectively. However, 2 weeks after receiving the third dose of the accelerated infliximab regimen, the patient’s respiratory function quickly deteriorated, which required admission to the intensive care unit (ICU), endotracheal mechanical ventilation, full sedation and total paralysis for severely progressive dyspnoea and hypoxic respiratory distress.
Investigations
The patient had an elevation of white cell count of approximately 17x 109 cells/L and became febrile with a temperature as high as 39.3°C. Despite high suspicion for infectious causes, all initial cultures remained negative. Eventually, pneumocystis jiroveci pneumonia (PJP) was also ruled out with negative bronchial lavage samples. In addition, it is important to mention that repeated sputum acid-fast stain, influenza, herpes simplex (HSV) and cytomegalovirus (CMV) PCR and tuberculosis, viral and fungal bronchial cultures were also all negative. As seen in the attached chest radiograph, there is evidence of extensively progressive, diffuse bilateral ground-glass opacities (figure 1). A chest CT scan demonstrated a crazy-paving pattern consisting of interlobular septal thickening on a background of diffuse ground glass opacification (figure 2).
Figure 1.
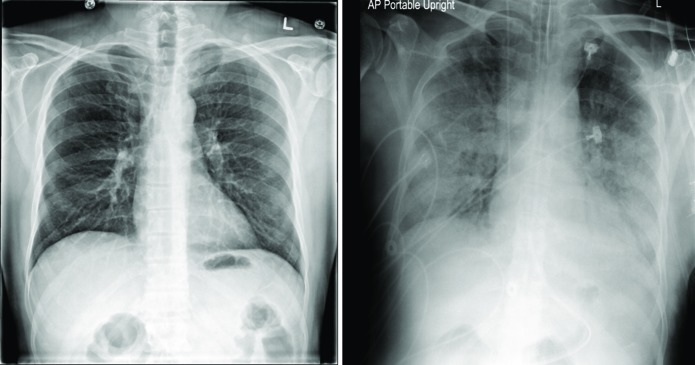
Portable chest radiographs with preinfliximab treatment on the left and diffuse ground-glass opacities as a complication after 2 weeks of receiving the third dose of the accelerated infliximab regimen in the treatment of severe ulcerative colitis on the right.
Figure 2.
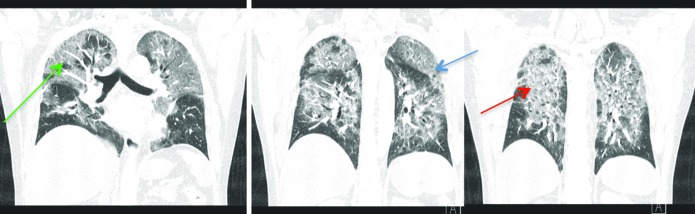
A chest CT portraying ground-glass opacities (red arrow) with interlobular septal thickening (green arrow), and intralobular reticular thickening (blue arrow) of the patient with infliximab-induced pneumonitis.
Differential diagnosis
This is the first reported case of fatal infliximab-induced lung toxicity following a rapid induction dosing schedule for the treatment of UC. This immunosuppressed patient presented to the ICU with subacute respiratory distress progressing over 2 weeks following an infliximab induction therapy for severe steroid-refractory UC. The patient also had an elevated white cell count and was febrile, while imaging studies showed a diffuse bilateral ground-glass appearance on a plain chest radiograph, and a characteristic pattern referred to as ‘crazy paving pattern’ on CT scan of the chest.9 Bronchoalveolar lavage was then conducted to further assess suspicious infectious aetiologies for this patient’s presentation.
Among the wide differential for this patient’s presentation are infectious causes, more specifically sepsis-induced acute respiratory distress syndrome, interstitial pneumonia, mycobacteria tuberculosis or pneumocystis jiroveci.10 Among other causes with similar radiological findings are extraintestinal pulmonary manifestations of UC, sarcoidosis or acute pulmonary haemorrhage.10 Finally, given the recent therapy with a biological agent, this may also be a case of drug-induced interstitial lung disease, which can encompass many forms including acute interstitial pneumonitis (AIP), usual interstitial pneumonia (a morphological pattern that can clinically present as idiopathic form of interstitial lung fibrosis), non-specific interstitial pneumonia (NSIP) or organising pneumonia.10–14
Infectious causes
This patient’s recent course of Infliximab, a common biological agent that strongly suppresses the immune system as discussed above, raised the suspicion of an infection being the culprit of this man’s progressive respiratory failure.4 More specifically, the rapid progression, fever and leucocytosis added more support of an infection being responsible. This patient had a history of active mycobacterial tuberculosis that was successfully treated in the past. Despite this, he did not display any other features of reactivation of the disease such as cavitation on chest imaging, cough, haemoptysis or constitutional symptoms such as weight loss, chills or night sweats. Although tuberculosis investigations with acid fast stain, and cultures of the sputum and bronchial lavage were conducted, but all tested negative.
Similarly, other infectious causes for this patient’s presentation could not be confirmed, with repeatedly negative microbiological results for viral, fungal and bacterial pneumonia, pneumocystis jiroveci or bacteraemia. Since the patient did display fever and leucocytosis along with his respiratory deterioration, he was empirically started on various broad-spectrum antibiotics over the 2 weeks leading to his ICU admission, while awaiting cultures and sensitivities. Nevertheless, since he failed to improve on empiric antibiotics and since his progression was subacute over weeks rather than acutely over days, sepsis-induced respiratory failure and acute hospital-acquired bacterial pneumonia became lower on the differential list. Also, the chest plain radiograph and CT-chest imaging raised the suspicion for possible PJP infection and the patient was promptly started on intravenous sulfamethoxazole/trimethoprim. More specifically, the widespread bilateral pulmonary infiltrate, alveolar septal thickening, hypoxia, elevated lactate dehydrogenase (LDH) and subacute nature of his presentation all suggested PJP.15 In addition, this is a commonly occurring infection in immunocompromised individuals, such as patients receiving chemotherapy, biological agents that suppress the immune system or in patients with AIDS.15 Despite the strong anticipation that the patient will improve on the initiated therapy, he continued to deteriorate, with subsequent alveolar lavage analysis being negative and ruling out PJP. Other common pathogens such as CMV and HSV in immunocompromised patients were ruled out by negative PCR, serology and cultures.
Extraintestinal manifestations
In addition to the usual inflammation of the colon, UC may also be associated with many extraintestinal manifestations such as arthropathies, uveitis, ankylosing spondylitis, primary sclerosing cholangitis, erythema nodosum, pyoderma gangrenosum and deep venous thromboembolism.16 More specifically to this patient’s respiratory failure, but very rare overall, UC may be associated with pulmonary embolism, vasculitis leading to pulmonary haemorrhage, interstitial fibrosis, pleuritis or bronchiectasis.17 Although these associated manifestations may not necessarily correlate directly to the severity of the disease, the lack of prior similar symptoms over the past 10 years since diagnosis, and the subacute length of progression of his presentation make extracolonic manifestations of UC a rare, less likely cause in this case.
Drug-induced pulmonary toxicity
Pulmonary complications associated with biologic therapies such as anti-TNF-α agents are rare, but well-documented phenomena. There is a clear caution of using these agents in patients with a pre-existing lung disease and the recommendation is to immediately discontinue therapy, should the patient present with suspicious worsening pulmonary symptoms.4 Drug-induced pneumonitis is generally a clinical diagnosis of exclusion after ruling out other causes such as infection, which was appropriately performed in this patient. However, more invasive testing such as lung biopsies are required to further classify the specific type of pneumonitis.10 18 19 Fibrosis of interstitial lung disease is the most common pulmonary toxicity associated with the use of infliximab, and it may present in many forms including AIP-like picture with a diffuse alveolar damage (DAD) pattern, bronchiolitis obliterans with organising pneumonia, NSIP or eosinophilic pneumonia.10 18–20
The lack of prominent eosinophils in the bronchoalveolar lavage points against eosinophilic pneumonia.21 This is further supported by the initial non-response to steroid therapy.21 The patient also did not display a classical organising pneumonia migrating patchy infiltrate, which should have been present on imaging studies.22 23 In addition, NSIP is unlikely because it was not a slow progression or chronic presentation as classically seen.20
Finally, AIP, another form of idiopathic interstitial lung disease, usually manifests with cough, dyspnoea and a rapidly progressive acute to subacute pulmonary fibrosis.24 Histologically, it would be expected to demonstrate a DAD pattern.24 Moreover, it may be refractory to steroids therapy as seen in this patient and usually has a very high fatality ratio.24 For these reasons combined together with timeframe of administering infliximab and the patient’s presentation, a DAD pattern induced by infliximab (similar to that seen in idiopathic AIP) is the most likely diagnosis in our case.
Treatment
The patient was initially treated with multiple antibiotic regimens over those 2 weeks, including azithromycin and piperacillin/tazobactam for suspicion of hospital acquired pneumonia, but had no significant improvement. The working diagnosis on admission to the ICU was severe PJP, given his prolonged immunosuppressed state, in addition to the bilateral suspicious findings on chest radiograph. At this point, viral causes were less likely with negative serology and PCR results. Therefore, after an infectious disease consultation, the patient was switched over to intravenous sulfamethoxazole/trimethoprim in efforts to target the suspected opportunistic infection, but again unfortunately, lacked any clinical improvement. Eventually, PJP was also ruled out with negative bronchial lavage samples, and sulfamethoxazole/trimethoprim was discontinued after 11 days of therapy. Given the continued deterioration and subacute progressive clinical presentation and radiological findings soon after initiating the Infliximab treatment, and after carefully ruling out the other more common potential causes, the patient was diagnosed with presumed infliximab-induced pneumonitis and transferred to a tertiary centre to obtain a confirming lung biopsy and further management with extracorporeal membrane oxygenation (ECMO).
Outcome and follow-up
The patient displayed initial improvement from an UC perspective with the accelerated infliximab scheduled doses, and subsequently avoided requiring total colectomy. However, his AIP picture worsened over the course of weeks. As a last resort, he was transferred to an ECMO centre, where he was expected to also undergo a lung biopsy, but unfortunately, the patient passed away soon after arrival.
Discussion
We conducted a literature search, which found similar cases of infliximab-induced interstitial lung disease in the setting of treating patients with UC. The results from the literature review of cases are reviewed in table 1.20 25–27 We conducted a Medline search using the terms ‘Infliximab’, ‘Ulcerative colitis or Proctocolitis’ and any term that may describe interstitial lung disease including ‘pneumonitis’, ‘Pulmonary fibrosis’ and ‘Alveolitis’. We then limited our search to articles available in English, yielding a total of four case reports that discuss infliximab-induced interstitial lung disease.
Table 1.
A summary of infliximab-induced interstitial lung disease in patients with ulcerative colitis
| Ref # | Case presentation | Infliximab use | Signs and symptoms | Investigations | Diagnosis and outcome |
| 120 | 29-year-old woman with a history of recently diagnosed UC started on infliximab presenting with progressive dyspnoea. | 3 months prior to admission. | Dyspnoea, non-productive cough, night sweats and hypoxaemia. | CXR—bibasilar infiltrates. CT chest—bilateral patchy infiltrates Bronchoscopy BAL and transbronchial biopsy—non-specific inflammation. Video-assisted thoracoscopic biopsy— acute lung injury pattern and interstitial pneumonia. |
Non-specific interstitial pneumonitis. Discontinuation of infliximab and corticosteroid initiation resulted in clinical improvement and complete radiological resolution at 3 months. |
| 225 | 32-year-old woman with a 14-year history of pulmonary biopsy proven Langerhan’s cell histiocytosis (in chronic remission) and an 8-year history of UC started on infliximab present with dyspnoea. | 6 weeks induction course prior to admission. | Fatigue, asthenia, dyspnoea, peripheral oedema, pruritus and fever. | CXR—bilateral, symmetric reticulonodular infiltrates. PFT—obstructive lung disease. CBC—eosinophilia. |
Langerhan’s cell histiocytosis reactivation secondary to infliximab therapy. Discontinuation of infliximab and initiation of corticosteroids resulted in complete remission. |
| 326 | 66-year-old man with a 4-year history of UC recently flared and started on infliximab therapy. | 14 weeks prior to admission. | Progressive dyspnoea on exertion. No other symptoms reported. | Echocardiogram—right ventricular hypertrophy, with normal left ventricle CT chest—diffuse bilateral ground-glass opacities. |
Infliximab-induced alveolitis. Discontinuation of infliximab resulted in slow improvement with complete resolution of ground-glass opacities at 6 months follow-up. |
| 427 | 63-year-old woman with UC maintained on azathioprine and infliximab therapy presenting with progressive dyspnoea for 3 weeks and hypoxaemia. | 6 months prior to admission | Bilateral wheezing and rhonchi and increased right basal dullness on percussion. | CXR—mild, bilateral diffuse air-space disease with no pleural effusions CT chest—bilateral peripheral ground-glass opacities. Bronchoscopy showed chronic inflammation with no sign of infection on BAL Open lung biopsy—lymphocytic interstitial pneumonitis and histiocytic pneumonia with eosinophils. |
Infliximab-induced interstitial lymphocytic pneumonitis and hypersensitivity histiocytic pneumonia. Discontinuation of infliximab and initiation of corticosteroids lead to complete resolution after slow tapering of steroid dose over a few months. |
BAL, bronchoalveolar lavage; CXR, chest plain radiograph; PFT, pulmonary function test; CBC, complete blood count.
All four case reports had successful treatment of the subject after infliximab was discontinued. Unfortunately, the patient we are presenting did not survive. In addition, a distinctive difference in this case report was the use of an accelerated infliximab induction course.
Learning points.
Although infusion-related reactions may be the most common infliximab adverse drug reactions, other side effects are related to their effect on the immune system and include opportunistic infections, reactivation of mycobacteria tuberculosis, developing lymphomas and lupus-like syndromes and, less commonly, interstitial lung disease.
There is some evidence indicating that accelerated infliximab induction regimen may be effective as salvage therapy in reducing the need for early colectomy in severe ulcerative colitis.
Further larger trials are required to investigate rare side effects such as rapidly progressive interstitial lung disease that may be more associated with the accelerated regimen of infliximab compared with standard dosing schedule.
Footnotes
Contributors: RR obtained patient’s next of kin consent, collected data and completed initial and final draft of manuscript including references and literature review.
SK assisted in collecting data and images as well as peer-reviewed initial and final draft prior to submission.
MM peer-reviewed initial and final draft of manuscript prior to submission.
SMH-M peer-reviewed final draft of manuscript prior to submission.
Competing interests: None declared.
Patient consent: Consent obtained from next of kin.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Gibson DJ, Heetun ZS, Redmond CE, et al. . An accelerated infliximab induction regimen reduces the need for early colectomy in patients with acute severe ulcerative colitis. Clin Gastroenterol Hepatol 2015;13:330–5. 10.1016/j.cgh.2014.07.041 [DOI] [PubMed] [Google Scholar]
- 2.Govani SM, Waljee AK, Stidham RW, et al. . 516 accelerated dosing of infliximab prevents colectomy within 90 days in only half of patients with severe ulcerative colitis. Gastroenterology 2016;150:S106 10.1016/S0016-5085(16)30462-0 [DOI] [Google Scholar]
- 3.Choy MC, Seah D, Gorelik A, et al. . Mo1878 comparison of accelerated infliximab induction vs standard induction treatment in acute severe ulcerative colitis. Gastroenterology 2016;150:S803 10.1016/S0016-5085(16)32720-2 [DOI] [Google Scholar]
- 4.Remicade (infliximab) [product monograph]. Toronto, Ontario, Canada: Janssen Inc, 2014. [Google Scholar]
- 5.Lopez-Olivo MA, Tayar JH, Martinez-Lopez JA, et al. . Risk of malignancies in patients with rheumatoid arthritis treated with biologic therapy: a meta-analysis. JAMA 2012;308:898–908. 10.1001/2012.jama.10857 [DOI] [PubMed] [Google Scholar]
- 6.Mayer L, Young Y. Infusion reactions and their management. Gastroenterol Clin North Am 2006;35:857–66. 10.1016/j.gtc.2006.09.006 [DOI] [PubMed] [Google Scholar]
- 7.Kim HS, You HS, Cho HH, et al. . Two cases of generalized pustular psoriasis: successful treatment with infliximab. Ann Dermatol 2014;26:787–8. 10.5021/ad.2014.26.6.787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Danese S. Mechanisms of action of infliximab in inflammatory bowel disease: an anti-inflammatory multitasker. Dig Liver Dis 2008;40(Suppl 2):S225–S228. 10.1016/S1590-8658(08)60530-7 [DOI] [PubMed] [Google Scholar]
- 9.De Wever W, Meersschaert J, Coolen J, et al. . The crazy-paving pattern: a radiological-pathological correlation. Insights Imaging 2011;2:117–32. 10.1007/s13244-010-0060-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thavarajah K, Wu P, Rhew EJ, et al. . Pulmonary complications of tumor necrosis factor-targeted therapy. Respir Med 2009;103:661–9. 10.1016/j.rmed.2009.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eugene JM, Victorine VM, Wiener CM. Case 33-2008 — A 63-Year-old woman with dyspnea on exertion. N Engl J Med 2008;359:1823–32. [DOI] [PubMed] [Google Scholar]
- 12.Hadjinicolaou AV, Nisar MK, Bhagat S, et al. . Non-infectious pulmonary complications of newer biological agents for rheumatic diseases-a systematic literature review. Rheumatology 2011;50:2297–305. 10.1093/rheumatology/ker289 [DOI] [PubMed] [Google Scholar]
- 13.Lynch DA, Travis WD, Müller NL, et al. . Idiopathic interstitial pneumonias: CT features. Radiology 2005;236:10–21. 10.1148/radiol.2361031674 [DOI] [PubMed] [Google Scholar]
- 14.Mueller-Mang C, Grosse C, Schmid K, et al. . What every radiologist should know about idiopathic interstitial pneumonias. Radiographics 2007;27:595–615. 10.1148/rg.273065130 [DOI] [PubMed] [Google Scholar]
- 15.Mori S, Sugimoto M. Pneumocystis jirovecii infection: an emerging threat to patients with rheumatoid arthritis. Rheumatology 2012;51:2120–30. 10.1093/rheumatology/kes244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Levine JS, Burakoff R. Extraintestinal manifestations of inflammatory bowel disease. Gastroenterol Hepatol 2011;7:235–41. [PMC free article] [PubMed] [Google Scholar]
- 17.Ji XQ, Wang LX, Lu DG. Pulmonary manifestations of inflammatory bowel disease. World J Gastroenterol 2014;20:13501–11. 10.3748/wjg.v20.i37.13501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Caccaro R, Savarino E, D'Incà R, et al. . Noninfectious interstitial lung disease during infliximab therapy: case report and literature review. World J Gastroenterol 2013;19:5377–80. 10.3748/wjg.v19.i32.5377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kakavas S, Balis E, Lazarou V, et al. . Respiratory failure due to infliximab induced interstitial lung disease. Heart Lung 2013;42:480–2. 10.1016/j.hrtlng.2013.07.005 [DOI] [PubMed] [Google Scholar]
- 20.Sen S, Peltz C, Jordan K, et al. . Infliximab-induced nonspecific interstitial pneumonia. Am J Med Sci 2012;344:75–8. 10.1097/MAJ.0b013e31824c07e8 [DOI] [PubMed] [Google Scholar]
- 21.Tazelaar HD, Linz LJ, Colby TV, et al. . Acute eosinophilic pneumonia: histopathologic findings in nine patients. Am J Respir Crit Care Med 1997;155:296–302. 10.1164/ajrccm.155.1.9001328 [DOI] [PubMed] [Google Scholar]
- 22.Al-Ghanem S, Al-Jahdali H, Bamefleh H, et al. . Bronchiolitis obliterans organizing pneumonia: pathogenesis, clinical features, imaging and therapy review. Ann Thorac Med 2008;3:67–75. 10.4103/1817-1737.39641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nakamura Y, Chida K, Suda T, et al. . [A comparative study of the prognosis for japanese patients with idiopathic interstitial pneumonia or BOOP based on histopathologic subsets]. Nihon Kokyuki Gakkai Zasshi 2000;38:442–6. [PubMed] [Google Scholar]
- 24.Vourlekis JS. Acute interstitial pneumonia. Clin Chest Med 2004;25:739–47. 10.1016/j.ccm.2004.07.001 [DOI] [PubMed] [Google Scholar]
- 25.Rodríguez HN, García I, Alba A, et al. . Infliximab-induced reactivated Langerhan's cell histiocytosis in a patient with ulcerative colitis. Inflamm Bowel Dis 2009;15:1286–7. 10.1002/ibd.20796 [DOI] [PubMed] [Google Scholar]
- 26.Veerappan SG, O'Morain CA. Infliximab-associated alveolitis after treatment for severe left-sided ulcerative colitis. Eur J Gastroenterol Hepatol 2009;21:830–2. 10.1097/MEG.0b013e32830fb700 [DOI] [PubMed] [Google Scholar]
- 27.Wiener CM, Muse VV, Mark EJ. Case records of the Massachusetts General Hospital. Case 33-2008. A 63-year-old woman with dyspnea on exertion. N Engl J Med 2008;359:1823–32. 10.1056/NEJMcpc0806979 [DOI] [PubMed] [Google Scholar]


