Abstract
Aripiprazole is an atypical antipsychotic agent commonly used in the management of schizophrenia. Aripiprazole has not been reported to have an association with interstitial lung disease. We describe a case of a 36-year-old woman who began to experience respiratory issues shortly after starting aripiprazole and presented to us 4 years later with progressive exertional shortness of breath. High-resolution CT of the chest showed a bilateral ground glass pattern. Video-assisted thoracoscopy with biopsy revealed alveolar septal thickening and an inflammatory infiltrate composed mainly of lymphocytes, suggestive of chronic hypersensitivity pneumonitis. After discontinuing aripiprazole and initiating prednisolone therapy, the patient’s pulmonary symptoms improved. This case highlights that aripiprazole can cause hypersensitivity pneumonitis in susceptible individuals.
Keywords: psychiatry (drugs and medicines), exposures, unwanted effects / adverse reactions, interstitial lung disease
Background
Many drugs have been associated with pulmonary toxicities that can manifest as bronchospasm, pulmonary oedema, pleural effusions, interstitial inflammation and fibrosis. Although the agents are typically inhaled and organic in nature, several drugs in tablet form have been reported to be associated with hypersensitivity pneumonitis. Hypersensitivity pneumonitis is an immunological reaction that results in inflammation of the lung parenchyma. The antipsychotic agent, aripiprazole, has not been reported to have an association with interstitial lung disease. We present a case of aripiprazole-associated hypersensitivity pneumonitis that went unrecognised for several years.
Case presentation
A 36-year-old woman with a history of bipolar disorder, depression and hypothyroidism came to the clinic for progressive exertional shortness of breath. The patient had developed a non-productive cough and frequent wheezing for several months, especially during exertion, that was relieved with albuterol inhalation and oxygen use. She denied chest pain, productive cough or haemoptysis. She did not have any recent infection, recent hospitalisation, history of pulmonary embolism, recent long-distance air or road travel, personal history of cancers, or exposure to tuberculosis, moulds or asbestos. She was a former smoker with a 10 pack-years history and had quit in 2009. Her medications included albuterol, aripiprazole, levothyroxine and citalopram. She had been on aripiprazole for more than 4 years for her bipolar disorder.
Physical examination revealed blood pressure of 110/70 mm Hg, pulse 80 beats/min, oral temperature 36.5°C (97.7°F), respirations 22 breaths/min, and oxygen saturation of 91% on room air that dropped to 78% on walking about 200 ft, which improved with 3 L of oxygen. She was noted to be in mild distress due to shortness of breath. She had adequate air movement with no wheeze, crackles or use of accessory muscles. She was admitted for further investigation.
Investigations
Initial laboratory studies showed a normal white blood cell count of 6.8 x 109/L (4–11) (neutrophils 60.9%, lymphocytes 27.5%, monocytes 7.2%, eosinophils 3.2% and basophils 0.9%), b-type natriuretic peptide of 119 pg/ml (<125), erythrocyte sedimentation rate of 5 mm/hour (0–15), C-reactive protein of 0.6 mg/dL (0.3–1.0) and α-1-antitrypsin of 168 mg/dL (100–190). Thyroid-stimulating hormone was high at 12.20 µIU/ml (0.3–3.0), and D-dimer was lower at 180 ng/ml (190–499). HIV, cytomegalovirus and antinuclear antibody were negative. A chest X-ray showed the minimal non-specific prominence of interstitial markings. CT of the chest demonstrated a diffuse multifocal mosaic pattern of lung attenuation throughout both lungs (figure 1A).
Figure 1.
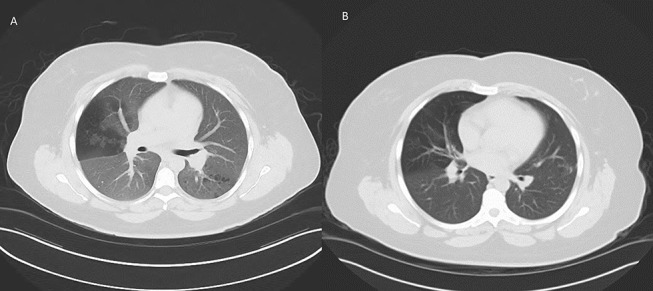
(A) CT scan showing multifocal mosaic pattern of lung attenuation throughout the bilateral lungs. (B) CT scan 10 months later shows significant improvement in the ground glass attenuation after discontinuing aripiprazole and completion of a prednisone regimen.
Differential diagnosis
The diagnostic considerations included infection, interstitial pneumonitis, eosinophilic pneumonia or hypersensitivity pneumonitis.
Treatment
The patient underwent bronchoscopy with bronchial washings and brushing that were negative for malignant cells, pneumocystis, fungi and acid-fast bacilli. Bronchoalveolar lavage showed lymphocytes 46%, monocytes 5%, polymorphs 26% and eosinophils 1%. A surgical lung biopsy showed diffuse interstitial chronic inflammation with thickening of alveolar septa by an inflammatory infiltrate composed mainly of lymphocytes, which was suggestive of chronic hypersensitivity pneumonitis (figure 2).
Figure 2.
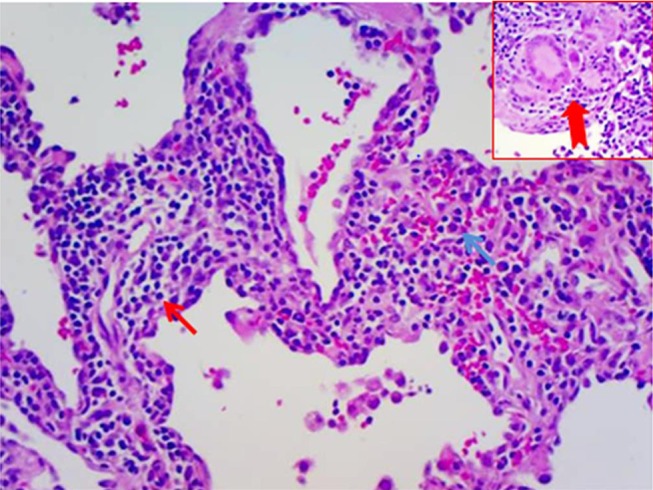
H&E, 10×, histological features of hypersensitivity pneumonitis. Diffuse interstitial chronic inflammation with thickening of alveolar septa (interstitium) by an inflammatory infiltrate composed mainly of lymphocytes (red arrow) and scattered plasma cells (blue arrow), along with multinucleated giant cells and aggregates of histiocytes (red notched arrow in inset).
A diagnosis of aripiprazole-induced hypersensitivity pneumonitis was made due to the temporal relationship between initiation of aripiprazole and abnormal lung findings; and the absence of an alternative diagnosis. She had been taking aripiprazole for 4 years, but she was symptomatic shortly after starting the drug and had frequent nurse visits for symptomatic treatment. Her other medications of albuterol, levothyroxine and citalopram are not associated with pulmonary toxicity. Aripiprazole was discontinued and she was started on a prednisone (60 mg) tapering regimen.
Outcome and follow-up
After 3 months, she had significant subjective improvement in her shortness of breath and no longer required oxygen at rest. CT scan performed after 10 months showed significant improvement in the pulmonary parenchyma (figure 1B). She was continued on prednisone for 1 year with slow tapering. She underwent psychotherapy for her mood disorders that helped with the psychiatric symptoms. As she remained asymptomatic, she was not started on any other psychotropic medications and was not rechallenged with aripiprazole.
Discussion
Aripiprazole is an atypical antipsychotic agent that has been widely used for acute and long-term management of schizophrenia. The mechanism of action includes partial agonistic activity at dopamine D2 receptors and serotonin 5-HT1A receptors and antagonistic activity at 5-HT2A receptors.1
Aripiprazole is generally well tolerated in patients and associated with a lower incidence of extrapyramidal symptoms and fewer weight gain issues than with other antipsychotics. The few reported pulmonary side effects include non-cardiogenic pulmonary oedema and hiccoughs, with no cases of interstitial lung disease.2–4
Hypersensitivity pneumonitis is a specific immunologic lung injury characterised by lymphocytic and granulomatous inflammation of lung parenchyma and associated airways.5 It is caused by a cell-mediated immunological reaction in response to repeated exposure to a variety of aetiological agents that are typically organic.6 An increasing number of drugs have been reported to cause hypersensitivity pneumonitis, but to our knowledge this is the first reported case of aripiprazole-induced hypersensitivity pneumonitis.
One important criterion for a drug-induced reaction is a history of exposure to that agent. The diagnosis of drug-induced hypersensitivity pneumonitis is a challenge because often a particular agent cannot be identified. Without an obvious agent, a multidisciplinary approach including clinicians, radiologists and pathologists becomes important for diagnostic clarity. While there are no universally accepted standards, criteria for drug-induced lung disease include an appropriate history of drug exposure, histological evidence of lung injury and clinical improvement after drug discontinuation, provided other causes have been ruled out.7 8
In our case, the patient developed respiratory symptoms after aripiprazole was initiated, which supports the temporal relation between drug commencement and development of respiratory symptoms. The specific diagnosis of hypersensitivity pneumonitis was further established based on the characteristic findings of ground glass appearance on high-resolution CT scan, the chronic inflammation pattern on histopathology and the lymphocytic predominance in the absence of infection in the bronchoalveolar lavage sample. After discontinuation of aripiprazole and administration of a corticosteroid, her symptoms and radiological findings improved. Thus, the diagnosis of aripiprazole-induced hypersensitivity pneumonitis was made.
Symptoms of hypersensitivity pneumonitis include dry cough, dyspnoea, fever and weight loss. CT scans may show ground glass opacity with or without centrilobular nodules; sometimes mosaic patterns are also seen. Bronchoalveolar lavage may show lymphocytosis and decreased CD4/CD8 ratio, but this finding has a low sensitivity and specificity.9 10 A biopsy might show chronic interstitial inflammation composed mainly of lymphocytes, peribronchial fibrosis, bronchiolar epithelial hyperplasia, and the presence of granulomas or multinucleated giant cells. The differential diagnosis to be considered includes idiopathic pulmonary fibrosis, diffuse interstitial pneumonitis, connective tissue diseases and sarcoidosis.9 10
Treatment of drug-induced hypersensitivity pneumonitis depends on the severity of clinical symptoms. Drug discontinuation is the essential step in its management. In the case of moderate to severe symptoms, the treatment of choice is systemic corticosteroid therapy.11 The usual regimen consists of initial high doses followed by gradual tapering. Steroids have been shown to be of limited long-term benefit in the absence of antigen removal.
Classically, hypersensitivity pneumonitis is an immunological response to an organic agent. Aripiprazole is not organic but still caused hypersensitivity pneumonitis. Other non-organic agents reported to cause hypersensitivity pneumonitis include amiodarone,12 azathioprine, 6-Mercaptopurine, beta-blockers, busulfan, fluoxetine, nitrofurantoin and procarbazine.13
Learning points.
Hypersensitivity pneumonitis should be considered in the differential diagnosis in patients who present with respiratory symptoms after starting treatment with aripiprazole.
The relationship between the drug exposure and onset of symptoms is useful for diagnosis.
A multidisciplinary approach including clinicians, radiologists and pathologists becomes important for diagnostic precision in challenging cases.
The main action of treatment is antigen avoidance and the mainstay of treatment is steroids.
Acknowledgments
The authors would like to thank Judith Jebastin, M.D. for her help with editing and formatting the pathology slide.
Footnotes
Contributors: KG, the primary author, was responsible for data acquisition, analysis, interpretation and manuscript preparation. SM participated in manuscript preparation and edition. JJ supervised development of the manuscript and final evaluation. NL participated in data interpretation and manuscript evaluation. All authors read and approved the final version of the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Croxtall JD. Aripiprazole: a review of its use in the management of schizophrenia in adults. CNS Drugs 2012;26:155–83. 10.2165/11208400-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 2. Thornton C, Maher TM, Hansell D, et al. . Pulmonary fibrosis associated with psychotropic drug therapy: a case report. J Med Case Rep 2009;3:126 10.1186/1752-1947-3-126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cetin M, Celik M, Cakıcı M, et al. . Aripiprazole induced non-cardiogenic pulmonary edema: a case report. Turk Psikiyatri Derg 2014;25:287–9. [PubMed] [Google Scholar]
- 4. Ray P, Zia Ul Haq M, Nizamie SH. Aripiprazole-induced hiccups: a case report. Gen Hosp Psychiatry 2009;31:382–4. 10.1016/j.genhosppsych.2008.09.014 [DOI] [PubMed] [Google Scholar]
- 5. Tonelli AR, Lottenberg R, Allan RW, et al. . Rituximab-induced hypersensitivity pneumonitis. Respiration 2009;78:225–9. 10.1159/000163069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sibertin-Blanc C, Norguet E, Duluc M, et al. . Severe hypersensitivity pneumonitis associated with everolimus therapy for neuroendocrine tumour: a case report. BMC Res Notes 2013;6:471 10.1186/1756-0500-6-471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Oh S, Cha SI, Kim H, et al. . A case of venlafaxine-induced interstitial lung disease. Tuberc Respir Dis 2014;77:81 10.4046/trd.2014.77.2.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Guilleminault L, Carré P, Diot P. Hypersensitivity pneumonitis associated with temozolomide. Eur Respir J 2009;34:526 10.1183/09031936.00065909 [DOI] [PubMed] [Google Scholar]
- 9. Elicker BM, Jones KD, Henry TS, et al. . Multidisciplinary approach to hypersensitivity pneumonitis. J Thorac Imaging 2016;31:92–103. 10.1097/RTI.0000000000000186 [DOI] [PubMed] [Google Scholar]
- 10. Wuyts W, Sterclova M, Vasakova M. Pitfalls in diagnosis and management of hypersensitivity pneumonitis. Curr Opin Pulm Med 2015;21:490–8. 10.1097/MCP.0000000000000199 [DOI] [PubMed] [Google Scholar]
- 11. Agache IO, Rogozea L. Management of hypersensivity pneumonitis. Clin Transl Allergy 2013;3:5 10.1186/2045-7022-3-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schwaiblmair M, Behr W, Haeckel T, et al. . Drug induced interstitial lung disease. Open Respir Med J 2012;6:63–74. 10.2174/1874306401206010063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Akoun GM, Gauthier-Rahman S, Milleron BJ, et al. . Amiodarone-induced hypersensitivity pneumonitis. Chest 1984;85:133–5. 10.1378/chest.85.1.133 [DOI] [PubMed] [Google Scholar]


