Abstract
A 9-year-old girl from black ethnic origin presented with a history of fever, cough, loss of weight and right-sided chest wall pain for 2 weeks. Chest X-ray demonstrated an effusion, which was shown to be loculated on chest CT scan. She was not responding to medical treatment and at thoracotomy loculated pus was drained. Mycobacterium tuberculosis (TB) was cultured from the pus. TB is a rare cause of loculated empyema with an overlapping clinical and radiological picture with pyogenic infections.
Keywords: infections, Tb and other respiratory infections, paediatrics, radiology
Background
Previously healthy child presents with persistent symptoms. She was diagnosed with loculated empyema. This is a very rare presentation of tuberculosis in children.
Case presentation
A 9-year-old girl from black ethnic origin presented with a history of fever, cough, loss of weight and right-sided chest wall pain for 2 weeks. She did not improve after 5 days of amoxicillin. Her previous history was not significant and she was HIV negative. She had no known tuberculosis (TB) contacts. She had a BCG vaccine scar on her arm. Mantoux skin test was not performed as it is not currently available. On examination, she had dullness to percussion on the right side and had reduced aeration on the right side.
Investigations
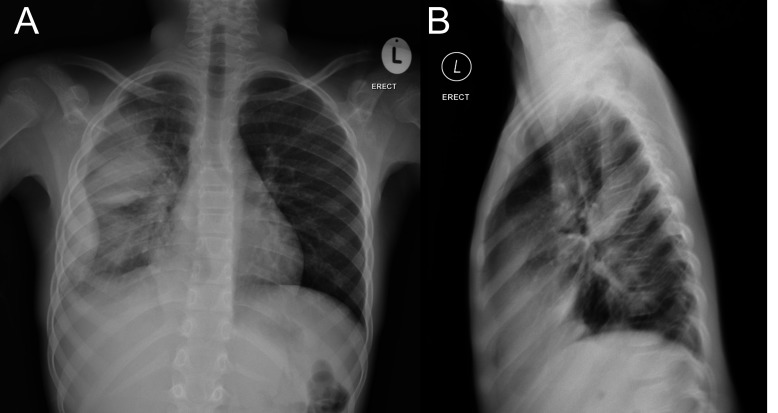
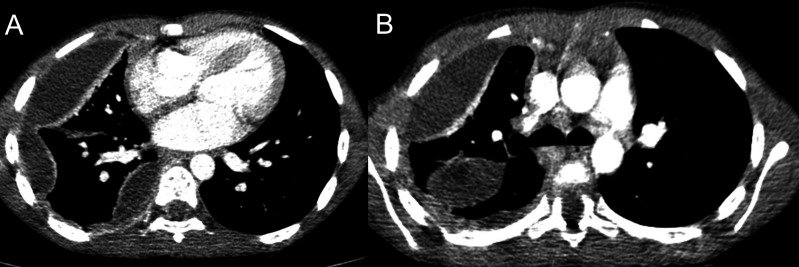
The chest X-ray demonstrated a pleural-based lobular density which was more pronounced at the right lower zone, demonstrated a convex inner margin and presented with a pseudotumour sign on the frontal radiographs (which proved to be an elliptical density located at the posterior portion part of the major fissure on the lateral view) (figure 1A,B). Contrast enhanced CT was indicated when the patient failed to respond to antibiotics to evaluate for any suppurative pleural or parenchymal complications. The CT confirmed the presence of loculated collections over the inferolateral portions and posteromedial portions of the right chest but also demonstrated enhancement of a thick medial edge in keeping with an empyema. It also confirmed that the pseudotumour was indeed a loculated collection in the right major fissure but this did not demonstrate any enhancement of the margin. No parenchymal abnormality was identified to suggest that the empyema was a complication of pneumonia as previously suspected (figure 2A,B).
Figure 1.
Chest X-ray in a 9-year-old girl with fever not responding to antibiotics. (A) Anteroposterior radiograph demonstrates lobulated density with a convex intrathoracic margin along the lateral aspect of the chest with a broad base in keeping with pleural pathology. This is continuous with the lamellar effusion extending to the apex. In addition, there is a well-defined elliptical density in the mid portion of the right chest and no air-bronchogram within it consistent with a ‘pseudotumour’. (B) Lateral radiograph serves to confirm that the elliptical density lies within the major fissure and that it is also pleural based.
Figure 2.
Non-sequential CT scan slices in the same patient as (figure 1A). (A) A more cranial slice at the level of the carina confirms that there is a right-sided effusion with a loculated component and that in addition the pseudotumour on chest X-ray is indeed a loculated collection in the major fissure. The lateral loculation demonstrates a thick enhancing medial edge consistent with an empyema. (B) A more caudal slice at the level of the cardiac ventricular chambers demonstrates that the pleural collection is multiloculated with lateral and medial components adjacent to the spine and heart, all demonstrating enhancing inner margins. This was important for making management decisions. No air-space consolidation was demonstrated to suggest an underlying pneumonia on lung windows (not shown here).
Aspiration of the fluid was attempted under ultrasound guidance, but this was not successful.
Sputum cultures remained negative (including TB cultures and GeneXpert testing). Primary immunodeficiency testing was done with the following results: IgG 15 g/L, IgA 1.29 g/L and IgM 0.77 g/L all normal. Lymphocyte subsets: absolute CD4 count 1214 cells/uL. Vaccination status was normal for the following vaccines: Bordetella pertussis, Clostridium tetani, Haemophilus influenza B, Streptococcus pneumoniae and Corynebacterium diphtheria.
Outcome
She had persistent symptoms with high swinging fever and the C reactive protein remained high (345 mg/L).
The child had a right-sided posterolateral thoracotomy performed. The lung had dense, fibrous adhesions. The entire lung was mobilised with much difficulty due to the adhesions. Loculated empyema was found, a number of pus loculations were drained and a full decortication was done. Samples were sent for culture and histology. The cultures were negative for pyogenic bacterial organisms but drug sensitive Mycobacterium tuberculosis was cultured from the pleural material.
She was seen after 1 month of four drug anti-TB treatment, with clinically improved aeration of the right side as well as radiological improvement which only showed mild residual pleural thickening on chest radiograph.
The child was screened for other causes of primary immunodeficiency, which was negative.
Discussion
Complicated pleural effusions due to TB are rare in children. Pleural involvement due to TB is believed to result from direct spread of caseous material from a subpleural parenchymal or lymph node focus or from haematogenous spread. The degree of pleural pathology depends on the dose and virulence of bacilli that enter the pleural space and the immune status of the patient.
The presence of caseous material in the pleural space triggers a hypersensitivity inflammatory response which leads to the accumulation of serous straw-coloured fluid containing few TB bacilli. If there is active caseation in the pleural space, thick loculated pus, containing many TB bacilli will develop.1
The chest CT scan picture includes pleural thickening with enhancement, fluid collections with mediastinal lymph nodes and parenchymal lesions.2 The presence of caseating empyema is normally indicated by a persistent high swinging fever, and aspiration of pus can be very difficult due to the fact that it is very thick. This case is unusual as the chest CT scan did not demonstrated any other signs of tuberculosis—there was no mediastinal lymphadenopathy or parenchymal caseating necrosis. Due to the lack of lymphadenitis and parenchymal disease as well as unusual aggressive course of the infection with M. tuberculosis, other causes of primary immunodeficiency must be considered. This included HIV and primary immunodeficiency and conditions with a lack of interferon-gamma (IFN-γ) production.3 This child did not have a history of previous infections suggestive of immunodeficiency. It is important to do a complete immunodeficiency investigation in children presenting with atypical and aggressive forms of pulmonary TB. This must include immunoglobulins, lymphocyte subsets, vaccination status as well as IFN-γ production studies.
She was seen at follow-up and had a very good response on TB treatment with a significant improvement in the radiological picture. This case enforces the value of obtaining specimens for TB culture even if this has to be achieved surgically, because all the cultures other than the pleural biopsy remained negative for TB. In countries with a high burden of TB, empyema due to TB must be considered as the clinical and radiological pictures may overlap with pyogenic infections. Most information about TB empyema in children date back many years, with no new cases recently described. Cases of empyema necessitatis due to TB has recently been described.4 Prognosis of TB empyema is variable, with slow disease progression and even death or slow resolution with pleural calcification and fibrosis.5 This makes it important to for a correct diagnosis to be reached rapidly as TB empyema may need early surgical intervention to prevent this complication.
Learning points.
The chest CT scan picture includes pleural thickening with enhancement, fluid collections with mediastinal lymph nodes and parenchymal lesions.
Empyema due to tuberculosis (TB) must be considered as the clinical and radiological pictures may overlap with pyogenic infections.
Primary immunodeficiency must be considered in unusual and severe forms of tuberculosis.
Footnotes
Contributors: PG was responsible for the management of this patient. JM for daily care and INA the intensive care doctor. SA did the radiology.
Competing interests: None declared.
Patient consent: Obtained from guardian.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Moon WK, Kim WS, Kim IO, et al. . Complicated pleural tuberculosis in children: CT evaluation. Pediatr Radiol 1999;29:153–7. doi:10.1007/s002470050561 [DOI] [PubMed] [Google Scholar]
- 2. Marais BJ, Gie RP, Schaaf HS, et al. . The natural history of childhood intra-thoracic tuberculosis: a critical review of literature from the pre-chemotherapy era. Int J Tuberc Lung Dis 2004;8:392–402. [PubMed] [Google Scholar]
- 3. Boisson-Dupuis S, Bustamante J, El-Baghdadi J, et al. . Inherited and acquired immunodeficiencies underlying tuberculosis in childhood. Immunol Rev 2015;264:103–20. doi:10.1111/imr.12272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Acar M, Sutcu M, Akturk HG, et al. . A case of empyema necessistatis in a child with Mycobacterium tuberculosis . Clin Pediatr 2016;12:1165–7. [DOI] [PubMed] [Google Scholar]
- 5. Miller FJW, Seal RME, Taylor MD. Tuberculosis in children. London, UK: J and A Churchill Ltd, 1963:163–275. 466–587. [Google Scholar]