Abstract
Imminent upper airway obstruction due to life-threatening tracheal stenosis of any cause is challenging. A 77-year-old woman, with a history of temporal tracheostomy for prolonged mechanical ventilation, presented with life-threatening tracheal stenosis to the emergency department. After failed intubation with a 5.0 mm internal diameter endotracheal tube, the patient was ventilated via a tube exchanger using Ventrain. Ventrain is a manual ventilation device that, in addition to oxygen supply during inspiration, initiates expiration by actively removing gas from the lungs by suction. Despite the nearly obstructed airway the patient was adequately ventilated with ‘permissive’ hypercarbia of 50 mm Hg and Saturation of peripheral Oxygen (SpO2) 95%–98% until surgical re-tracheostomy was performed. The haemodynamic stability of the patient indicated that the active expiration prevented intrapulmonary pressure build-up by air trapping and subsequent barotrauma and/or haemodynamic deterioration, which may well be observed during traditional jet ventilation especially in case of a completely obstructed airway.
Keywords: Anaesthesia, Emergency Medicine
Background
Managing a life-threatening upper airway obstruction due to tracheal stenosis of any cause is extremely challenging. Guidelines for the anticipated or unanticipated cases of difficult ventilation, difficult intubation or ‘can’t intubate – can’t ventilate’ (CICV) scenarios1 are currently lively debated.2
In the relatively rare event of an awake, still spontaneously breathing patient with near complete upper airway obstruction due to tracheal stenosis, immediate intervention is required to ensure oxygenation. Once the upper airway is completely closed, only a few techniques like the percutaneous dilatative, the needle and the scalpel based technique1 are left to access the airway and ensure ventilation. This, although a needle based technique, may be a challenging option for physicians encountering such a life-threatening situation. Alternatively, a small lumen tube, like a tube exchanger or hollow bougie, could enhance oropharyngeal intubation in case the airway is not fully obstructed yet. This would reduce the risk of tissue damage and time loss as compared with intubation attempts with a large-bore endotracheal tube.
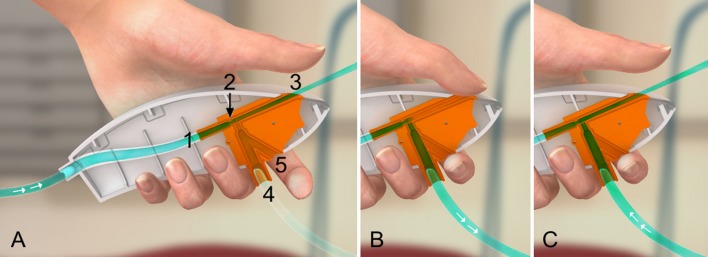
The manual small lumen ventilator, Ventrain3 (figure 1) was initially developed to ventilate patients with complete upper airway obstruction following needle cricothyrotomy. In addition to oxygen supply during inspiration, Ventrain initiates expiration by actively removing gas from the lungs due to its expiratory ventilation assistance (EVA) technology. This EVA technology considerably reduces the risk of intrapulmonary pressure build-up/air trapping/barotrauma when compared with traditional jet ventilation, especially in situations of a fully obstructed airway.4 5
Figure 1.
Working mechanism of Ventrain (expiratory ventilation assistance technology). (A) Equilibration mode. The gas flows via the inlet (1) through a very narrow nozzle (2) towards the exhaust pipe (3). No flow from or to the patient. (B) Closing both the exhaust pipe (3) and safety bypass (5) forces the oxygen to flow via the inlet (1) through the narrow nozzle (2) towards the patient via port (4): inspiration. (C) Expiration: The gas flows via the inlet (1) through a very narrow nozzle (2) and exhaust pipe (3) to the outside. The flow entrains gas from port (4), which is connected to a catheter: active expiration. The bypass (5) functions as an on/off switch. When opened, there is no significant positive or negative pressure at the catheter tip, resulting in equilibration/safety mode.
However, in using Ventrain in an emergency situation it has to be considered that, depending on the driving pressure of the oxygen source, clinically different insufflation pressures and tidal volumes may result.6
Ventrain can ventilate through any small lumen (eg, a transtracheal catheter, an airway exchange catheter, a bougie or a working channel of a bronchoscope) independent of the route of airway access. Therefore, Ventrain in combination with a transtracheal catheter was electively used during upper airway surgery, increasing surgical working space.6 In the current case, describing imminent tracheal stenosis, difficulties regarding airway management were anticipated and therefore Ventrain was present in advance. For the first time it was demonstrated that in a deteriorating airway situation a quick act with Ventrain in combination with a tube exchanger could prevent a real emergency CICV situation.
Case presentation
A 77-year-old woman was admitted to the hospital after collapsing at home. A head CT, after admission to the intensive care unit, revealed diffuse subarachnoidal haemorrhage due to cerebral aneurysm following a hypertensive crisis. She underwent immediate clipping and external ventricular drain insertion. Postoperative pulmonary complications required long-term ventilation, and percutaneous dilational tracheostomy was performed on postoperative day 12. After 3 months, the patient was transferred from the intensive care unit to the ward and discharged to long-term care 1 week later. The tracheostomy was closed after 6 months. Four weeks later, she presented to the emergency department with acute dyspnoea, indicating severe upper airway obstruction.
Investigations
An emergency CT scan was performed indicating that intubation of a 5.5 mm inner diameter (ID) endotracheal tube is possible (figure 2). The patient's history was otherwise unremarkable with respect to potential intubation or ventilation problems. Assessment of the upper airway as well as anaesthetic record from the previous operation did not reveal any signs predictive of a difficult intubation.
Figure 2.
CT of the thorax shows the sternoclavicular joint with tracheal stenosis.
Due to progressive signs of upper airway obstruction, the attending ENT surgeon shifted the patient immediately to the theatre for surgical re-tracheostomy.
Treatment
The initial intubation attempt, with a 5.0-mm ID endotracheal tube by direct laryngoscopy under spontaneous ventilation with 50 mg ketamine and 20 mg propofol intravenously, failed due to subglottic stenosis. Direct laryngoscopy was chosen over fibre-optic intubation for concerns of provoking complete airway obstruction during advancement of the tracheal tube through the stenosis. The endotracheal tube easily passed through the vocal cords, however the intubation failed due to the subglottic stenosis. Following that some bleeding from trauma to the subglottic tissue was noticed.
A prepared tube exchanger with 6.3 mm outer diameter, 4.4 mm inner diameter and 80 cm length (Volker Bertram Medizintechnik (VBM)) was immediately introduced under a direct vision, gentle pressure and spiral movement up to 20 cm front tooth. Ventrain was attached and connected to the oxygen outlet of a Draeger anaesthesia machine with a flow set at 18 L/min. Ventilation was started with an inspiration time of 2 s and an expiration time of 4 s, while the clearly visible thorax excursions were leading.
The surgical re-tracheostomy was performed. After the trachea was completely reopened the inspiration-to-expiration ratio was changed to 1:1 of 2 s each.
Outcome and follow-up
Re-tracheostomy, with a Portex transtracheal tube (ID 7.5 mm) was completed after about 20 min. Even though normal communication with the patient was not possible due to previous subarachnoidal haemorrhage with impaired mental status, neither facial expressions nor vital signs conveyed the impression of any stress during the procedure.
Throughout this surgical period, adequate ventilation with stable haemodynamics was easily achieved. Sidestream capnography of the actively expired gases showed stable CO2 readings of 50 mm Hg. These values were used for trend monitoring and were indicative for adequate ventilation. The patient was shifted to the surgical intensive care unit and was haemodynamically stable under spontaneous respiration with 95%–98% saturation on room air. A postoperative chest X-ray did not reveal any pathology. The patient was transferred back to long-term care the following day and was discharged home 9 days after the incident.
Discussion
To the best of our knowledge, this is the first case report describing the use of Ventrain in combination with an airway exchanger in a case of almost complete upper airway obstruction in an adult patient. It was demonstrated that in a deteriorating airway situation a quick act with Ventrain in combination with a tube exchanger could prevent a real emergency CICV situation.
Earlier Ventrain has been used electively in combination with a transtracheal catheter during upper airway surgery, providing an increased surgical working space and adequate ventilation.7–9 In two newborns, Ventrain proved to be a live-saver managing the critical paediatric airway using small lumen intubation and exchange catheters.10
In adults various emergency medical conditions might lead to life-threatening upper airway obstruction, including allergic or anaphylactic reactions, neoplasms of the trachea, or extratracheal compression by a mass. Postintubation tracheal stenosis is a rare (4.9 cases per million per year) but serious condition.11 Clinicians dealing with these cases also have to consider the quality of underlying tissue (oedema, granulation tissue, neoplasm, scars) causing tracheal obstruction.
In any case of swollen but still soft tissue (allergic or anaphylactic reaction) the insertion of a larger endotracheal tube and therefore the initial use of a flexible fibre-optic should be considered. However, situations involving a neoplasm or, as in the present case, a scar with granulation tissue will have to be approached differently.
Since they are trained to cope with difficult situations, anaesthetists should instinctively know what to do in each case based on the severity of the obstruction and stability of the patient. Surgical or needle cricothyroidotomy is the method of choice in these cases. In cases with a nearly obstructed airway, the choice of the anaesthetic might be important. The influence of different anaesthetics on smooth airway muscles is well known.12 To increase the likelihood of persistent spontaneous respiration, small doses of ketamine combined with low-dose remifentanil infusion might be a good combination for intubation attempts.
In cases involving unexpectedly difficult intubation before invention of Ventrain, the only option for achieving non-surgical or non-needle cricoidotomy access was jet ventilation, a technique introduced in the 1950s.13 The major disadvantage of jet ventilation, especially in cases involving a partially or completely obstructed upper airway, is the potential for barotrauma (subcutaneous emphysema or pneumothorax) if exhalation is inadequate and airway pressure is elevated.14 In addition, monitoring of CO2 elimination during jet ventilation can only be performed by means of blood-gas measurement. In contrast, Ventrain offers the possibility of insufflating oxygen, and allows active removal of gas from the lungs to reduce the chance of intrapulmonary pressure build-up and risks of barotrauma and circulatory collapse. On the basis of the manufacturer's recommendation, ventilation was interrupted in between (every 5 min) to allow equilibration in order to prevent a rise in airway pressure. In addition, the unique possibility of connecting a sidestream capnometry device provides the physician with additional valuable information in this critical and life-threatening situation.
In our opinion this case report clearly demonstrates that even for less experienced users Ventrain is virtually self-explaining and therefore an ideal backup tool in cases of a nearly completely obstructed upper airway via a tube exchanger or any other small lumen tube.
Learning points.
Advanced airway management training should consider direct and indirect optical devices, supraglottic airway devices, and surgical access and focus on the best options for ventilation after obtaining tracheal access, taking into account ventilation performance and safety.
Since ventilation can easily be achieved with Ventrain, regular training and availability should also be considered in emergency departments.
Ventrain in combination with a tube exchanger or hollow bougie should be considered as a serious alternative for repeated attempts of endotracheal intubation with large bore tubes. This could save crucial time and prevent intubation related damage.
Ventrain is a viable and safe alternative to jet ventilation in cases involving almost complete upper airway obstruction.
Footnotes
Contributors: BMW contributed substantially to conception and design of the article, drafting the article and final approval. HAT was involved in drafting the article, revised it critically and also approved the final version. AE-M revised the article and approved the final version.
Competing interests: None declared.
Patient consent: Guardian consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Frerk C, Mitchell VS, McNarry AF, et al. . Difficult Airway Society intubation guidelines working group. Difficult Airway Society 2015 Guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Timmermann A, Chrimes N, Hagberg CA. Need to consider human factors when determining first-line technique for emergency front-of-neck access. Br J Anaesth 2016;117:5–7. 10.1093/bja/aew107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hamaekers AE, Borg PA, Enk D. Ventrain: an ejector ventilator for emergency use. Br J Anaesth 2012;108:1017–21. 10.1093/bja/aes033 [DOI] [PubMed] [Google Scholar]
- 4.Berry M, Tzeng Y, Marsland C. Percutaneous transtracheal ventilation in an obstructed airway model in post-apnoeic sheep. Br J Anaesth 2014;113:1039–45. 10.1093/bja/aeu188 [DOI] [PubMed] [Google Scholar]
- 5.Paxian M, Preussler NP, Reinz T, et al. . Transtracheal ventilation with a novel ejector-based device (Ventrain) in open, partly obstructed, or totally closed upper airways in pigs. Br J Anaesth 2015;115:308–16. 10.1093/bja/aev200 [DOI] [PubMed] [Google Scholar]
- 6.Schmidt AR, Ruetzler K, Haas T, et al. . Impact of oxygen sources on performance of the Ventrain® ventilation device in an in vitro set-up. Acta Anaesthesiol Scand 2016;60:241–9. 10.1111/aas.12663 [DOI] [PubMed] [Google Scholar]
- 7.Borg PA, Hamaekers AE, Lacko M, et al. . Ventrain® for ventilation of the lungs. Br J Anaesth 2012;109:833–4. 10.1093/bja/aes366 [DOI] [PubMed] [Google Scholar]
- 8.Fearnley RA, Badiger S, Oakley RJ, et al. . Elective use of the Ventrain for upper airway obstruction during high-frequency jet ventilation. J Clin Anesth 2016;33:233–5. 10.1016/j.jclinane.2016.03.024 [DOI] [PubMed] [Google Scholar]
- 9.Rosenblatt WH. Elective Percutaneous Translaryngeal E V A Ventilation: case 2 from AOD. https://www.youtube.com/watch?v=AgOGo2Yk544
- 10.Willemsen MG, Noppens R, Mulder AL, et al. . Ventilation with the Ventrain through a small lumen catheter in the failed paediatric airway: two case reports. Br J Anaesth 2014;112:946–7. 10.1093/bja/aeu125 [DOI] [PubMed] [Google Scholar]
- 11.Nouraei SA, Ma E, Patel A, et al. . Estimating the population incidence of adult post-intubation laryngotracheal stenosis. Clin Otolaryngol 2007;32:411–2. 10.1111/j.1749-4486.2007.01484.x [DOI] [PubMed] [Google Scholar]
- 12.Yamakage M, Hirshman CA, Croxton TL. Inhibitory effects of thiopental, ketamine, and propofol on voltage-dependent Ca2+ channels in porcine tracheal smooth muscle cells. Anesthesiology 1995;83:1274–82. 10.1097/00000542-199512000-00018 [DOI] [PubMed] [Google Scholar]
- 13.Flory FA, Hamelberg W, Jacoby JJ, et al. . Transtracheal resuscitation. J Am Med Assoc 1956;162:625–8. [DOI] [PubMed] [Google Scholar]
- 14.Craft TM, Chambers PH, Ward ME, et al. . Two cases of barotrauma associated with transtracheal jet ventilation. Br J Anaesth 1990;64:524–7. 10.1093/bja/64.4.524 [DOI] [PubMed] [Google Scholar]