Abstract
Objective:
To report the distinctive clinical features of cryptogenic new-onset refractory status epilepticus (C-NORSE) and the C-NORSE score based on initial clinical assessments.
Methods:
A retrospective study was conducted for 136 patients with clinically suspected autoimmune encephalitis who underwent testing for autoantibodies to neuronal surface antigens between January 1, 2007, and August 31, 2016. Eleven patients with C-NORSE were identified. Their clinical features were compared with those of 32 patients with anti-NMDA receptor encephalitis (NMDARE).
Results:
The clinical outcome of 11 patients (median age, 27 years; 7 [64%] women) with C-NORSE was evaluated after a median follow-up of 11 months (range, 6–111 months). Status epilepticus was frequently preceded by fever (10/11 [91%]). Brain MRIs showed symmetric T2/fluid-attenuated inversion recovery hyperintensities (8/11 [73%]) and brain atrophy (9/11 [82%]). Only 2 of the 10 treated patients responded to the first-line immunotherapy, and 4 of the 5 patients treated with IV cyclophosphamide responded to the therapy. The long-term outcome was poor in 8 patients (73%). Compared with 32 patients with NMDARE (median age, 27 years; 24 [75%] women), those with C-NORSE had more frequent prodromal fever, status epilepticus, ventilatory support, and symmetric brain MRI abnormalities, had less frequent involuntary movements, absent psychobehavioral symptoms, CSF oligoclonal bands, or tumor association, and had a worse outcome. The C-NORSE score was higher in patients with C-NORSE than those with NMDARE.
Conclusions:
Patients with C-NORSE have a spectrum of clinical-immunological features different from those with NMDARE. The C-NORSE score may be useful for discrimination between them. Some patients could respond to immunotherapy.
New-onset refractory status epilepticus (NORSE) is a rare but neurologic emergency condition characterized by refractory status epilepticus (RSE) without readily identifiable cause in otherwise healthy individuals.1–3 “NORSE” is currently viewed as a syndrome,2 not a distinct entity, and has received several names, including devastating epileptic encephalopathy in school-age children (DESC),4 febrile infection-related epilepsy syndrome (FIRES),5 acute encephalitis with refractory repetitive partial seizures (AERRPS),6 or NORSE.3 DESC, FIRES, and AERRPS are terms more frequently used in pediatric patients, whereas NORSE is more frequently used in adults. The concept of “acute encephalopathy with inflammation-mediated status epilepticus (AEIMSE)” has also been proposed.7
Since the discovery of autoimmune encephalitis (AE) and autoantibodies against neuronal cell-surface antigens or synaptic proteins (NSA antibodies),8–14 a few cases of FIRES15 or NORSE16 associated with NSA antibodies have been documented. Furthermore, a recent large cohort2 demonstrated that a half of 130 patients with NORSE remained cryptogenic, but 37% were immune mediated; among those, the most common etiology was anti-NMDA receptor (NMDAR) encephalitis (NMDARE).
Therapeutic approach with IV cyclophosphamide (IVCPA) has also been proposed in even cryptogenic cases.7,17–20 However, only 1 of 63 patients (2%) with cryptogenic NORSE (C-NORSE) received IVCPA in the cohort.2 In an emergency condition, antibody testing results may not be readily accessible, but it is important to differentiate C-NORSE from antibody-mediated encephalitis at an early stage.
Here, we report its distinctive clinical features and the C-NORSE score based on initial clinical assessments with conventional diagnostic tests and discuss the potential efficacy of IVCPA.
METHODS
Patient selection and antibody assays.
A retrospective observational study was conducted in the Department of Neurology at Kitasato University. We first reviewed the clinical information of 136 patients with clinically suspected AE who underwent testing for NSA antibodies between January 1, 2007, and August 31, 2016 to make a diagnosis. These patients were admitted to Kitasato University Hospital or other academic or referral hospitals between January 1, 1999, and August 31, 2016; in 7 patients admitted to Kitasato University Hospital before January 1, 2007, archived serum/CSF samples obtained at symptom presentation were used for antibody assays.
NSA antibodies were measured in all patients at the laboratory of Josep Dalmau (University of Barcelona) using both immunohistochemistry on rat brain tissue and cell-based assays8–14; they included antibodies to the NMDAR, α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor (AMPAR), γ-aminobutyric acid B receptor (GABAbR), γ-aminobutyric acid A receptor (GABAaR), metabotropic glutamate receptor (mGluR) 1, contactin-associated protein-like 2, dipeptidyl peptidase-like protein 6, and leucine-rich glioma-inactivated 1 (LGI1). Both serum and CSF were examined in all patients except 3 patients (CSF was not available).
NSA antibodies were detected in 39 patients; they included antibodies to NMDAR (n = 33), AMPAR (n = 3), LGI1 (n = 2), GABAbR (n = 1), GABAaR (n = 1), and unknown antigens (n = 2); however, 2 patients had multiple NSA antibodies (appendix e-1 at Neurology.org/nn). The other 2 developed autoimmune post–herpes simplex virus (HSV) encephalitis associated with NSA antibodies (NMDAR [n = 1], unknown antigens [n = 1]). The remaining seronegative 97 patients underwent further investigations for viral infection, collagen vascular disorders or other systemic autoimmune disorders, malignancy survey, or brain or skin biopsy when appropriate. After reasonable exclusion of alternative causes (appendix e-1), we identified 11 patients with C-NORSE. The final diagnoses of the seronegative 97 patients were described in appendix e-1.
Criteria for C-NORSE.
Patients were diagnosed with C-NORSE if those fulfilled the following 4 criteria: (1) age 17 years or older, (2) new-onset RSE in previously healthy individual, (3) refractoriness to conventional antiepileptic drug (AED) treatment, and (4) no etiology identified throughout the course of the disease. Status epilepticus (SE) was considered as refractory when it continued longer than 60 minutes, despite adequate administration of benzodiazepines and an adequate loading of standard IV AEDs.2,21,22
The etiology of NORSE was extensively investigated with CSF examination, malignancy survey, and serologic testing, including autoantibodies to NSA and classic paraneoplastic intracellular antigens (CV2/CRMP5, Ma2, Ri, Yo, Hu, GAD65, and amphiphysin), which were measured in serum with EUROLINE (Euroimmun AG).
Treatment modalities.
The treatment strategy was decided by individual patients' physicians. Treatments were classified into (1) conventional AED treatment (AED, and continuously infused anesthetic agents [midazolam, propofol, thiopental, thiamylal, phenobarbital, or pentobarbital]), (2) the first-line immunotherapy (IV high-dose methylprednisolone [IVMP], 1,000 mg/day, for 3–5 days; IV immunoglobulin [IVIg], 0.4 g/kg/day for 5 days; and plasma exchange [PLEX] alone or combined), (3) the second-line immunotherapy (IVCPA [500 mg/m2, monthly for 1–6 cycles] or rituximab [375 mg/m2, once weekly, 4 doses]), (4) chronic immunosuppression (prednisone, tacrolimus, cyclosporine, azathioprine, or mycophenolate mofetil), and (5) tumor resection when appropriate.
Outcome criteria and evaluation of clinical features.
The primary outcome was neurologic disability evaluated by the modified Rankin Scale (mRS) at the last follow-up period.23 Good outcome was defined as an mRS score of 0–2, and poor outcome was defined as an mRS score of 3 or higher. The SE severity score (STESS)24 at the onset of SE was obtained in patients with C-NORSE.
The clinical features of 11 patients with C-NORSE were compared with those of 32 patients with NMDARE as a disease control. One patient with autoimmune post-HSV encephalitis with NMDAR antibodies was excluded because depression was the sole symptom. The other 6 seropositive patients were also excluded because of the small sample size of each antibody group. None of these 6 patients developed EEG-confirmed RSE.
Response to immunotherapy.
In patients with C-NORSE, individual patients' physicians (authors) were requested to report whether their patients responded to immunotherapy or not, with either “yes” or “no” based on reduction in seizure frequency, decrement of IV anesthetic drugs, mental status improvement, or resolution of MRI abnormalities. Response of seizure to immunotherapy was not evaluated in the disease control because only 6 of the 32 patients with NMDARE developed EEG-confirmed SE.
Standard protocol approvals, registrations, and patient consents.
This study was approved by Institutional Review Boards of Kitasato University (B16-148). Written or oral informed consent was obtained from the patients or their family members. Information on symptoms, CSF, MRI, EEG, treatments, outcomes, and response to immunotherapy, were obtained from the authors or referring physicians.
Statistical analysis.
The Fisher exact test was performed for comparison of categorical variables, and the Mann-Whitney test was used for continuous variables. The statistical significance was set at p < 0.05. We used JMP, version 11.2.0 (SAS Institute Inc.) for statistical analyses.
RESULTS
Clinical and paraclinical features of patients with C-NORSE.
Eleven patients with C-NORSE were identified; 7 patients (64%) were women; median age at symptom onset was 27 years (range, 17–59 years). Clinical information is shown in tables 1, e-1 and e-2. The STESS was median 3 (range, 2–3).
Table 1.
Comparison of clinical features between C-NORSE and NMDARE
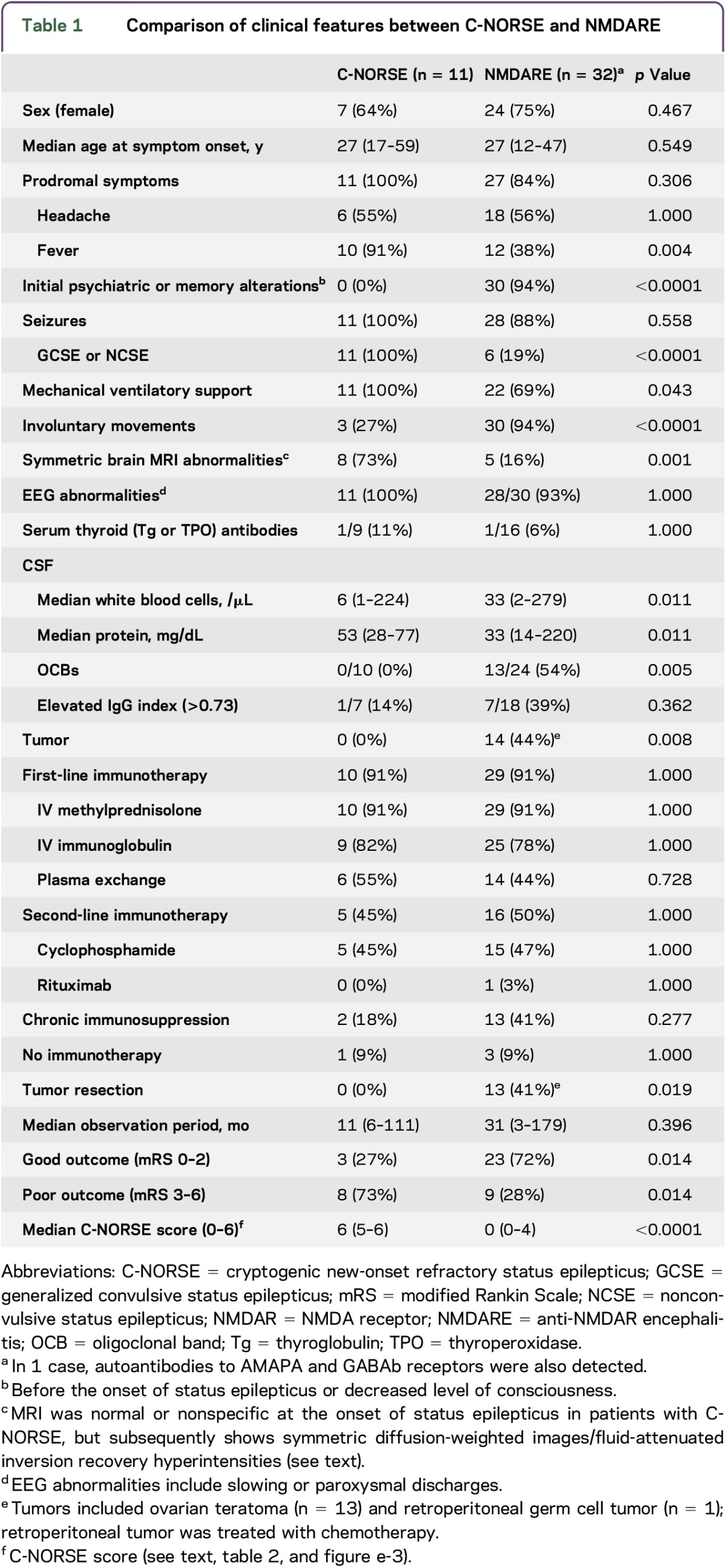
Three patients had a family history of febrile convulsion or seizure, and 1 had a history of febrile convulsion (table e-1). All patients had prodromal symptoms; among those, high fever of unknown origin was most frequently seen in 10 patients (91%), and headache in 6 (55%). Following prodromal symptoms, generalized convulsive SE (GCSE) developed within median 5 days (range, 4–14 days), but none of the 11 patients had psychobehavioral or memory symptoms before the onset of epileptic seizures.
CSF examination revealed mild inflammatory changes (median white blood cells 6/μL [range, 1–224/μL]), but 5 patients (45%) had no pleocytosis. The protein level was mildly elevated. Oligoclonal bands (OCBs) were not detected in 10 examined patients, and the IgG index was elevated in only 1 of 7 patients. No tumor was found in any individual.
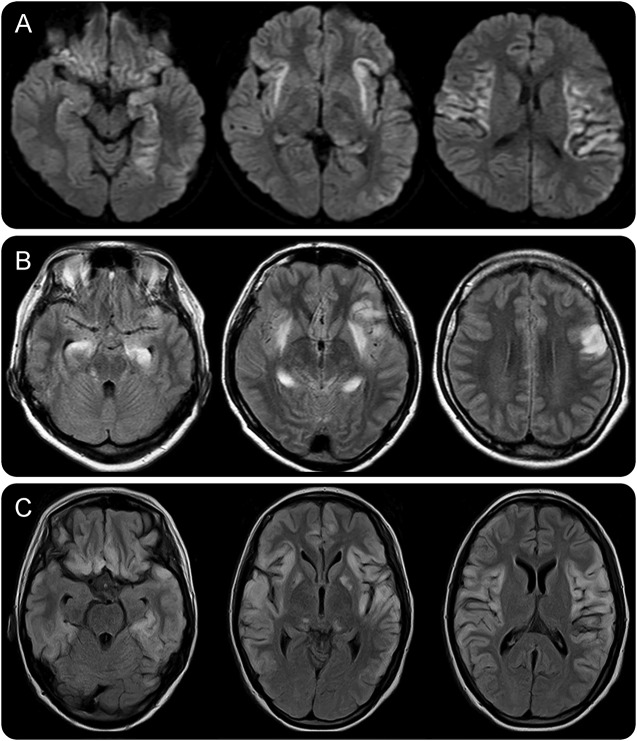
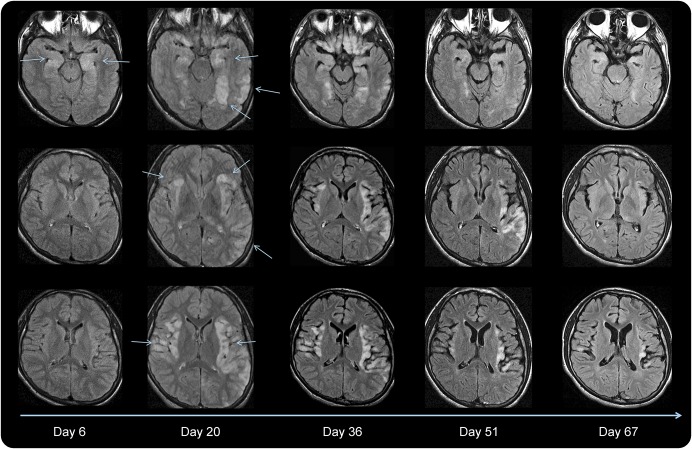
Brain MRIs were normal or nonspecific at the onset of SE, but follow-up MRIs showed symmetric increased diffusion-weighted images or T2/fluid-attenuated inversion recovery signals in the hippocampus, amygdala, insula, claustrum, thalamus, perisylvian operculum, and basal ganglia in 8 patients (73%) (figures 1 and 2, e-1). These MRI changes developed along with persistent seizure activity (figure e-2). Diffuse or frontotemporal atrophy developed in 9 patients (82%) and cerebellar atrophy in 3 (patients 1, 7, and 9).
Figure 1. MRI lesions in the acute stage of cryptogenic new-onset refractory status epilepticus.
Initial brain MRI at the onset of status epilepticus is unremarkable, but a few days later, MRI shows symmetric increased diffusion-weighted images (DWIs) or T2/fluid-attenuated inversion recovery (FLAIR) signals in the hippocampus, amygdala, insula, claustrum, thalamus, perisylvian operculum, and basal ganglia (A–C). These newly appearing lesions are likely associated with persistent seizure activity that was highly refractory to conventional antiepileptic treatments. Brain MRIs were obtained on day 20 of the onset of status epilepticus (A, patient 3), day 3 (B, patient 6), and day 74 (C, patient 9). (A) DWI and (B and C) FLAIR images.
Figure 2. Resolution of brain lesions following immunotherapies and conventional antiepileptic drug treatment (Patient 3).
Initial brain MRI on day 1 was normal, but follow-up MRIs show symmetric medial temporal fluid-attenuated inversion recovery (FLAIR) hyperintensities on day 6 (arrows), as well as follow-up MRIs show rapid spread of hyperintensities in a symmetric distribution involving the medial temporal lobes, claustrum, insula, and perisylvian opercular cortex on day 20 (arrows). Generalized convulsive status epilepticus was extremely refractory to antiepileptic drugs, continuously infused anesthetic agents, and the first-line immunotherapy (IVMP and IVIg). The patient was treated with IVCPA on days 20 and 52, with additional IVMP, IVIG, and PLEX, resulting in reduction in seizure frequency with gradual resolution of hyperintensities, but mild brain atrophy was seen on day 67. Note gradual resolution of FLAIR hyperintensities following 2 cycles of IVCPA (tables e-1 and e-2). IVCPA = IV cyclophosphamide; IVIg = IV immunoglobulin; IVMP = IV high-dose methylprednisolone; PLEX = plasma exchange.
GCSE that often began with facial twitching was highly refractory to the first-line and second-line AEDs and required continuous infusion of anesthetic drugs with mechanical ventilatory support. All patients were initially treated with IV acyclovir for possible HSV encephalitis, but HSV-DNA was not detected by PCR in any of them. Patient 1 admitted in 2001 was not treated with immunotherapy because the concept of AE had not been developed yet in 2001. However, the remaining 10 patients (91%) admitted in 2008 or later were treated with the first-line immunotherapy for presumed AE (tables e-1 and e-2); in 5 patients, IVCPA was added as recommended in refractory cases of NMDARE.25 In all 10 treated patients, IVMP was used first on median day 3 from the onset of SE (range, 1–15 days), followed by IVIg (n = 9), PLEX (n = 6), or IVCPA (n = 5).
The first-line immunotherapy was considered “not effective” in 8 of the 10 treated patients, but IVCPA was presumed to be “effective” in 4 of the 5 treated patients who failed to respond to the first-line immunotherapy. In IVCPA-responsive 4 patients (#3, 5, 9, and 11), IVCPA was started between days 20 and 59, but nonresponsive patient (#4) received IVCPA on day 173. In patient 3, the first-line immunotherapy started on day 6; nevertheless, symmetric brain lesions developed (figure 2). Because NMDARE was initially suspected, IVCPA was started on day 20, followed by PLEX, and IVCPA was repeated on day 52 with the first-line immunotherapy, resulting in marked improvement with resolution of brain MRI abnormalities. The patient became able to walk without assistance 11 months after the symptom onset; IVCPA was considered effective. By contrast, patient 4 was admitted to a city hospital and treated with conventional AED treatment and IVMP started on day 3. However, the patient became a state of unresponsive wakefulness with diffuse brain atrophy. Five months later, the patient was transferred to our hospital and treated with IVCPA (day 173) combined with the first-line immunotherapy because we had a few successful experiences of immunotherapy initiated 8–12 months after the symptom onset in patients with NMDARE with diffuse brain atrophy.26 Gadolinium enhancement disappeared after the immunotherapy (figure e-1), but IVCPA was considered not effective because this patient's mental status remained unchanged. In the other 3 treated patients, IVCPA was presumed to be effective.
Two patients had relapsing episodes of RSE. In patient 3, RSE relapsed twice after discharge at 40 and 44 months, resulting in severe motor disability (mRS 5). In patient 9, RSE relapsed at 9 months, and the patient is being treated with IVCPA and AEDs but remains bedridden. Only 3 of 11 patients considerably recovered after a median follow-up of 11 months (range, 6–111 months); however, seizure control remained poor even in these 3 recovering patients. Three patients became a state of unresponsive wakefulness on discharge; 1 patient (#4) subsequently died. Long-term neurologic disability at the last follow-up was poor in 8 patients (73%).
Comparisons of clinical features.
Female sex was predominant in patients with NMDARE, but sex difference was not significant (table 1). Median age at the symptom onset was 27 years in both groups. Prodromal symptoms developed frequently in both groups, but fever was more common in patients with C-NORSE than in those with NMDARE. Psychiatric or memory alterations did not develop before the onset of SE in patients with C-NORSE; by contrast, prominent psychiatric or memory alterations developed before the onset of seizures or altered level of consciousness in 30 patients (94%) with NMDARE. Seizures were common in both groups. However, only 6 patients (19%) with NMDARE showed EEG-confirmed SE, and none of these patients presented with NORSE as the first manifestation of encephalitic features. The extreme delta brush pattern, characteristic of NMDARE,27 was seen in 4 patients (13%) with NMDARE but not in any patient with C-NORSE. Patients with C-NORSE needed mechanical ventilatory support more frequently than those with NMDARE but showed involuntary movements less frequently and no sustained bizarre orofacial-limb dyskinesias. Symmetric MRI abnormalities were more frequently seen in patients with C-NORSE than in those with NMDARE (figures 1, 2, and e-1).
Serum thyroid antibodies were detected at low titer in small numbers of patients, and their detection rate was not significantly different between the 2 groups. Serum GAD65 antibodies were not detected in either group. CSF examination revealed mild inflammatory changes and no OCBs in 10 patients with C-NORSE, while half of the patients with NMDARE had OCBs. The rate of the elevated IgG index was not significantly different. Tumor was found in 14 patients (44%) with NMDARE. By contrast, no patients with C-NORSE had tumors. The first-line or second-line immunotherapy was used in both groups without significant difference in efficacy. Patients with C-NORSE had a worse long-term outcome than those with NMDARE (73% vs 28%, p = 0.014).
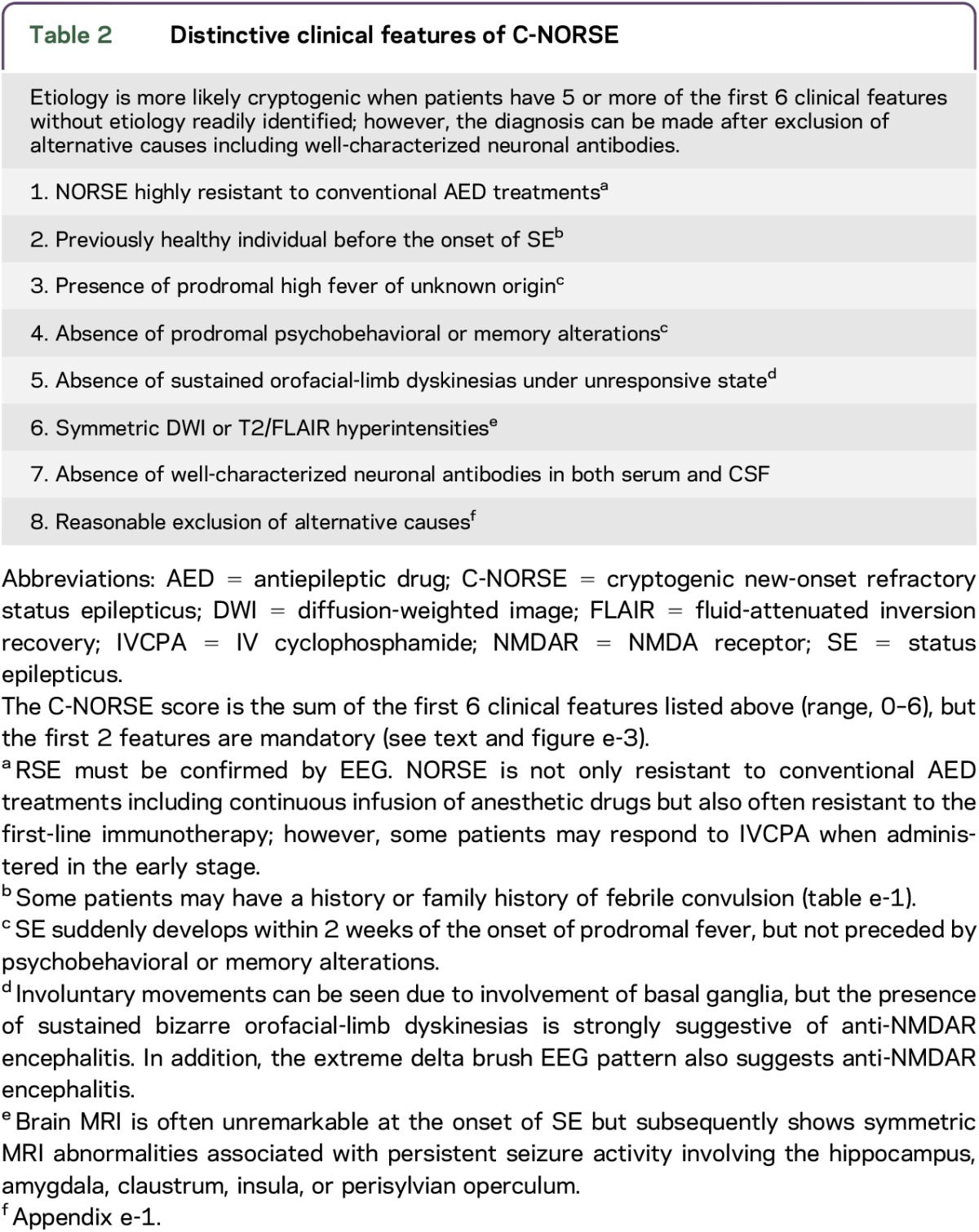
Distinctive clinical features and C-NORSE score.
We found 8 distinctive clinical features of C-NORSE (table 2). Etiology is more likely cryptogenic when patients have 5 or more of the first 6 clinical features when no etiology is readily identified. We also created the C-NORSE score (range, 0–6) based on the clinical characteristics, in which the first 2 features are mandatory; patients are scored 0 when either the first or second feature is absent. Seven patients were scored 6 and the remaining 4 patients were scored 5; the median C-NORSE score was higher in patients with C-NORSE than in those with NMDARE (6 vs 0, p < 0.0001), and none with NMDAR had scores of 5 or 6. It indicates that the C-NORSE score may be useful for differentiating these 2 disorders (table 1 and figure e-3). However, the diagnosis must be made after reasonable exclusion of alternative causes.
Table 2.
Distinctive clinical features of C-NORSE
DISCUSSION
This study showed that (1) patients with C-NORSE had a spectrum of clinical-immunological features different from NMDARE, (2) the C-NORSE score is useful for discriminating patients with C-NORSE from those with NMDARE, (3) some patients with C-NORSE may respond to immunotherapy, and (4) none of the 39 seropositive patients presented with NORSE as the first manifestation.
The term “NORSE” is currently used as a syndrome rather than a distinct entity, whose etiology can be viral, paraneoplastic, or AE,2 although the definition of NORSE varies in the literature depending on the criteria used.1–3,7,16,18–21 We used the term “C-NORSE” as a NORSE syndrome without identified etiologies.
One patient had a history of febrile convulsion, and 3 had a family history of seizures. This association with seizures may suggest a propensity for epilepsy. Another important feature is prodromal fever, which may trigger SE especially in patients susceptible to epileptic seizures or prone to activate innate and adaptive immune responses. Following high fever, SE suddenly developed without associated psychosis. The prodromal fever unassociated with psychobehavioral symptoms suggests cryptogenic rather than NMDARE or limbic encephalitis. Brain MRI was often unremarkable at the onset of SE but subsequently showed symmetric brain lesions. These MRI abnormalities may be nonspecific and presumed to be caused by prolonged seizure activities.28–31
The first-line immunotherapies are usually not effective in patients with NORSE,3 FIRES,5 or AERRPS.6 Lack of response is consistent with the absence of NSA antibodies; however, inflammation-mediated epileptogenesis has increasingly been proposed.7,17,32–34 One study34 showed upregulation of interleukin (IL)-6, C-X-C motif chemokine 10, and IL-8 in CSF of patients with AERRPS, suggesting a role for the innate and adaptive immune system,35 since IL-6 is a booster of adaptive immune mechanisms while IL-8 and CXC-10 enhance the innate immunity; IVCPA exerts its main activity rather on the T-cells than on the B-cells. Although we did not examine CSF cytokine or chemokine levels in our cases, IVCPA might have some beneficial effects on inflammation-mediated mechanisms.
In practice, physicians must judge whether their patients with NORSE are cryptogenic or immune mediated based on initial clinical assessments because antibody testing results are usually not readily accessible. Therefore, we listed 8 distinctive features in table 2 and created the C-NORSE score. When the patient has 5 or more of the first 6 clinical features without etiology readily identified, NSA antibodies would be less likely detected, and conventional AED treatments would not be expected to provide remarkable beneficial effects. In our cases, all had 5 or more C-NORSE scores. This scoring strategy may help physicians to identify cryptogenic cases, but this scoring system should be validated in the different cohort in the future.
It is known that 80% of patients with NMDARE achieve a good outcome at 24 months.36 Such a good outcome and lack of evident brain damage on MRI are strongly related to early and intensive immunotherapy, and the absence of a substantial infiltration of the brain with inflammatory cells and the lack of complement activation may protect the brain from massive structural damage.37 However, epilepsy-related irreversible brain damage occurs quickly in C-NORSE; therefore, it may require more aggressive and early initiation of immunotherapy such as IVCPA than antibody-mediated encephalitis.
The pathogenesis of C-NORSE remains unclear, and it may be a heterogeneous group of disorders, but immunohistochemistry using a rat brain or live hippocampal cultures did not disclose NSA antibodies in our patients. It indicates that antibody-mediated mechanisms are less likely to explain the C-NORSE. The treatment at the earlier phase of RSE aims to (1) immediately control seizure activity for preventing damages by excitotoxicity,38–40 (2) block the progression of secondary process triggered by initial excitotoxicity,7,32,33,38 and (3) avoid systemic complications associated with RSE or prolonged anesthesia.38 We consider that early initiation of combined immunotherapies with IVCPA and IVMP or IVIg (probably within 10 days after the onset of RSE) may provide beneficial effects by breaking the vicious cycle in inflammation-mediated epileptogenesis as postulated in super-refractory cases.7,32,33 However, such combined immunotherapies must be used cautiously under the critical condition with high fever. The use of rituximab in the absence of identified NSA antibodies and OCBs is questionable. Ketogenic diet can be an alternative opinion in patients with C-NORSE, although we did not use it.
This study has limitations of being retrospective and based on small numbers of patients. The efficacy of immunotherapy was not evaluated in either group of patients with a standard protocol, but we evaluated it on an individual basis in patients with C-NORSE. We compared the clinical features between C-NORSE and NMDARE because NMDARE is always listed in the differential diagnosis of RSE; however, C-NORSE was not compared with AE with other NSA antibodies because (1) only 7 patients had other NSA antibodies, (2) none of the patients developed RSE, and (3) most of cases of AE are NMDARE. RSE can be associated with various NSA antibodies,9–11,14 but RSE rarely develops without preceding memory or psychobehavioral alterations. By contrast, our patients with C-NORSE presented with the sudden onset of RSE without preceding encephalitic features except prodromal fever or headache. Although the results may not be simply generalized to other AE, the mode of presentation is clearly different between C-NORSE and seropositive AE. Further studies are required to compare clinical features between C-NORSE and AE with GABAbR or GABAaR antibodies because the latter group most closely resembles C-NORSE.
Many issues remain unknown, including etiology, epileptogenesis, and response to immunotherapy in C-NORSE. Genetic analysis was not performed in our patients. One might argue that these patients may include those with seronegative autoimmune limbic encephalitis or genetic epileptic disorder underdiagnosed or with some new antibodies not detected yet. We cannot rule out such possibilities. It remains to be determined whether early administration of IVCPA and IVMP or IVIg with conventional AED treatment would improve long-term outcomes. These issues should be addressed in the future.
Supplementary Material
ACKNOWLEDGMENT
The authors thank Professor Josep Dalmau in Service of Neurology, IDIBAPS Hospital Clínic, University of Barcelona, Casanova (Spain), for examining antibodies against neuronal cell-surface antigens and critical comments on this study. They are extremely grateful to all participants and physicians for their contribution to this study and acknowledge the efforts of research staff, who worked on the clinical and neuroimaging data collection.
GLOSSARY
- AE
autoimmune encephalitis
- AED
antiepileptic drug
- AERRPS
acute encephalitis with refractory repetitive partial seizures
- AMPAR
α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor
- C-NORSE
cryptogenic new-onset refractory status epilepticus
- DESC
devastating epileptic encephalopathy in school-age children
- FIRES
febrile infection-related epilepsy syndrome
- GABAaR
γ-aminobutyric acid A receptor
- GABAbR
γ-aminobutyric acid B receptor
- GCSE
generalized convulsive status epilepticus
- HSV
herpes simplex virus
- IL
interleukin
- IVCPA
IV cyclophosphamide
- IVIg
IV immunoglobulin
- IVMP
IV high-dose methylprednisolone
- LGI1
leucine-rich glioma-inactivated 1
- mRS
modified Rankin Scale
- NMDARE
anti-NMDA receptor encephalitis
- NSA
neuronal cell-surface antigen
- OCB
oligoclonal band
- PLEX
plasma exchange
- RSE
refractory status epilepticus
- SE
status epilepticus
- STESS
Status Epilepticus Severity Score
Footnotes
Supplemental data at Neurology.org/nn
AUTHOR CONTRIBUTIONS
Takahiro Iizuka and Naomi Kanazawa: study concept or design, data acquisition, analysis or interpretation of the data, statistical analysis, and drafting/revising the manuscript. Juntaro Kaneko: study concept or design, data acquisition, interpretation of the data, and drafting/revising the manuscript. Naomi Tominaga: data acquisition, interpretation of the data, and drafting/revising the manuscript. Yutaka Nonoda: data acquisition, analysis or interpretation of the data, and drafting/revising the manuscript. Atsuko Hara, Yuya Onozawa, Hiroki Asari, Takashi Hata, Junya Kaneko, Kenji Yoshida, and Yoshihiro Sugiura: data acquisition, interpretation of the data, and drafting/revising the manuscript. Yoshikazu Ugawa: study concept or design, data acquisition, analysis or interpretation of the data, and drafting/revising the manuscript. Masashi Watanabe, Hitomi Tomita, Arifumi Kosakai, Atsushi Kaneko, Daisuke Ishima, Eiji Kitamura, and Kazutoshi Nishiyama: data acquisition, interpretation of the data, and drafting/revising the manuscript.
STUDY FUNDING
This work was supported in part by grants from Mitsubishi Tanabe Pharma Corporation (MTPS20160504012) and the Japan Epilepsy Research Foundation (JERFTENKAN 17002).
DISCLOSURE
T. Iizuka is an editorial board member for Current Treatment Options in Neurology and Rinsho Shinkeigaku, received grants from Mitsubishi Tanabe Pharma Corporation and the Japan Epilepsy Research Foundation. N. Kanazawa, J. Kaneko, N. Tominaga, Y. Nonoda, A. Hara, Y. Onozawa, H. Asari, T. Hata, J. Kaneko, K. Yoshida, and Y. Sugiura report no disclosures. Y. Ugawa received grants from the Ministry of Education, Culture, Sports, Science and Technology of Japan, the Ministry of Health, Labour and Welfare of Japan, the Support Center for Advanced Telecommunications Technology Research, the Association of Radio Industries Businesses, Ministry of Internal Affairs and Communications/grants from the Committee of the Study of Human Exposure to EMF, and the Novartis Foundation (Japan) for the Promotion of Science, Nihon Kohden, Ltd., Takeda Pharmaceutical Company Limited, Nippon Boehringer Ingelheim Co., Ltd., and Mitsubishi Tanabe Pharma Corporation; received honoraria from the Taiwan Movement Disorders Society, Chinese Neurology Society, Astellas Pharma Inc., Eisai Co., Ltd., FP Pharmaceutical Corporation, Otsuka Pharmaceutical Co., Ltd., Elsevier Japan K. K., Kissei Pharmaceutical Co., Ltd., Kyorin Pharmaceutical Co., Ltd., Kyowa Hakko Kirin Co., Ltd., GlaxoSmithKline K. K., Sanofi-Aventis K.K., Daiichi Sankyo Co., Ltd., Dainippon Sumitomo Pharma Co., Ltd., Takeda Pharmaceutical Co., Ltd., Mitsubishi Tanabe Pharma Corporation, Teijin Pharma Ltd., Nippon Chemiphar Co., Ltd., Nihon Pharmaceutical Co., Ltd., Nippon Boehringer Ingelheim Co., Ltd., Novartis Pharma K.K., Bayer Yakuhin, Ltd., and Mochida Pharmaceutical Co., Ltd. Y. Ugawa also received royalties from CHUGAI-IGAKUSHA, Igaku-Shoin Ltd., Medical View Co. Ltd., and Blackwell Publishing K.K. M. Watanabe, H. Tomita, A. Kosakai, A. Kaneko, D. Ishima, and E. Kitamura report no disclosures. K. Nishiyama received grants from Nippon Boehringer Ingelheim Co., Ltd., Daiichi Sankyo Co., Ltd., Astellas Pharma Inc., Otsuka Pharmaceutical Co., Ltd., Kyorin Pharmaceutical Co., Ltd., Dainippon Sumitomo Pharma Co., Ltd., Teijin Pharma Limited., Nihon Pharmaceutical Co., Ltd., Pfizer Inc., Bristol-Myers Squibb, Japan Blood Products Organization, MSD, and Nihon Medi-Physics Co., Ltd. Go to Neurology.org/nn for full disclosure forms.
REFERENCES
- 1.Costello DJ, Kilbride RD, Cole AJ. Cryptogenic new onset refractory status epilepticus (NORSE) in adults: infectious or not? J Neurol Sci 2009;277:26–31. [DOI] [PubMed] [Google Scholar]
- 2.Gaspard N, Foreman BP, Alvarez V, et al. New-onset refractory status epilepticus: etiology, clinical features, and outcome. Neurology 2015;85:1604–1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilder-Smith EP, Lim EC, Teoh HL, et al. The NORSE (new-onset refractory status epilepticus) syndrome: defining a disease entity. Ann Acad Med Singapore 2005;34:417–420. [PubMed] [Google Scholar]
- 4.Mikaeloff Y, Jambaqué I, Hertz-Pannier L, et al. Devastating epileptic encephalopathy in school-aged children (DESC): a pseudo encephalitis. Epilepsy Res 2006;69:67–79. [DOI] [PubMed] [Google Scholar]
- 5.van Baalen A, Häusler M, Boor R, et al. Febrile infection-related epilepsy syndrome (FIRES): a nonencephalitic encephalopathy in childhood. Epilepsia 2010;51:1323–1328. [DOI] [PubMed] [Google Scholar]
- 6.Sakuma H, Awaya Y, Shiomi M, et al. Acute encephalitis with refractory, repetitive partial seizures (AERRPS): a peculiar form of childhood encephalitis. Acta Neurol Scand 2010;121:251–256. [DOI] [PubMed] [Google Scholar]
- 7.Nabbout R, Vezzani A, Dulac O, Chiron C. Acute encephalopathy with inflammation-mediated status epilepticus. Lancet Neurol 2011;10:99–108. [DOI] [PubMed] [Google Scholar]
- 8.Dalmau J, Tüzün E, Wu HY, et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol 2007;61:25–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lai M, Hughes EG, Peng X, et al. AMPA receptor antibodies in limbic encephalitis alter synaptic receptor location. Ann Neurol 2009;65:424–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lancaster E, Lai M, Peng X, et al. Antibodies to the GABA(B) receptor in limbic encephalitis with seizures: case series and characterisation of the antigen. Lancet Neurol 2010;9:67–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lai M, Huijbers MG, Lancaster E, et al. Investigation of LGI1 as the antigen in limbic encephalitis previously attributed to potassium channels: a case series. Lancet Neurol 2010;9:776–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lancaster E, Huijbers MG, Bar V, et al. Investigations of caspr2, an autoantigen of encephalitis and neuromyotonia. Ann Neurol 2011;69:303–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boronat A, Gelfand JM, Gresa-Arribas N, et al. Encephalitis and antibodies to dipeptidyl-peptidase-like protein-6, a subunit of Kv4.2 potassium channels. Ann Neurol 2013;73:120–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Petit-Pedrol M, Armangue T, Peng X, et al. Encephalitis with refractory seizures, status epilepticus, and antibodies to the GABAA receptor: a case series, characterisation of the antigen, and analysis of the effects of antibodies. Lancet Neurol 2014;13:276–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Illingworth MA, Hanrahan D, Anderson CE, et al. Elevated VGKC-complex antibodies in a boy with fever-induced refractory epileptic encephalopathy in school-age children (FIRES). Dev Med Child Neurol 2011;53:1053–1057. [DOI] [PubMed] [Google Scholar]
- 16.Hainsworth JB, Shishido A, Theeler BJ, Carroll CG, Fasano RE. Treatment responsive GABA(B)-receptor limbic encephalitis presenting as new-onset super-refractory status epilepticus (NORSE) in a deployed U.S. soldier. Epileptic Disord 2014;16:486–493. [DOI] [PubMed] [Google Scholar]
- 17.Specchio N, Claps D, Vigevano F, Fusco L. Refractory focal epilepsy following acute encephalopathy with inflammation-mediated status epilepticus. Seizure 2011;20:824–825. [DOI] [PubMed] [Google Scholar]
- 18.Gall CR, Jumma O, Mohanraj R. Five cases of new onset refractory status epilepticus (NORSE) syndrome: outcomes with early immunotherapy. Seizure 2013;22:217–220. [DOI] [PubMed] [Google Scholar]
- 19.Kaneko J, Iizuka T, Asari H, et al. Retrospective review of 6 patients with new-onset refractory status epilepticus (NORSE) syndrome: early intervention with intravenous cyclophosphamide may improve outcome. Neurology 2013;80:P07.171. [Google Scholar]
- 20.Khawaja AM, DeWolfe JL, Miller DW, Szaflarski JP. New-onset refractory status epilepticus (NORSE)–The potential role for immunotherapy. Epilepsy Behav 2015;47:17–23. [DOI] [PubMed] [Google Scholar]
- 21.Mayer SA, Claassen J, Lokin J, Mendelsohn F, Dennis LJ, Fitzsimmons BF. Refractory status epilepticus: frequency, risk factors, and impact on outcome. Arch Neurol 2002;59:205–210. [DOI] [PubMed] [Google Scholar]
- 22.Brophy GM, Bell R, Claassen J, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care 2012;17:3–23. [DOI] [PubMed] [Google Scholar]
- 23.van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 1988;19:604–607. [DOI] [PubMed] [Google Scholar]
- 24.Rossetti AO, Logroscino G, Bromfield EB. A clinical score for prognosis of status epilepticus in adults. Neurology 2006;66:1736–1738. [DOI] [PubMed] [Google Scholar]
- 25.Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol 2011;10:63–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Iizuka T, Kaneko J, Tominaga N, et al. Association of progressive cerebellar atrophy with long-term outcome in patients with anti-N-methyl-D-aspartate receptor encephalitis. JAMA Neurol 2016;73:706–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schmitt SE, Pargeon K, Frechette ES, et al. Extreme delta brush: a unique EEG pattern in adults with anti-NMDA receptor encephalitis. Neurology 2012;79:1094–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hocker S, Nagarajan E, Rabinstein AA, Hanson D, Britton JW. Progressive brain atrophy in super-refractory status epilepticus. JAMA Neurol 2016;73:1201–1207. [DOI] [PubMed] [Google Scholar]
- 29.Chevret L, Husson B, Nguefack S, Nehlig A, Bouilleret V. Prolonged refractory status epilepticus with early and persistent restricted hippocampal signal MRI abnormality. J Neurol 2008;255:112–116. [DOI] [PubMed] [Google Scholar]
- 30.Chatzikonstantinou A, Gass A, Förster A, Hennerici MG, Szabo K. Features of acute DWI abnormalities related to status epilepticus. Epilepsy Res 2011;97:45–51. [DOI] [PubMed] [Google Scholar]
- 31.Meletti S, Slonkova J, Mareckova I, et al. Claustrum damage and refractory status epilepticus following febrile illness. Neurology 2015;85:1224–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wilcox KS, Vezzani A. Does brain inflammation mediate pathological outcomes in epilepsy? Adv Exp Med Biol 2014;813:169–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Iori V, Frigerio F, Vezzani A. Modulation of neuronal excitability by immune mediators in epilepsy. Curr Opin Pharmacol 2016;26:118–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sakuma H, Tanuma N, Kuki I, Takahashi Y, Shiomi M, Hayashi M. Intrathecal overproduction of proinflammatory cytokines and chemokines in febrile infection-related refractory status epilepticus. J Neurol Neurosurg Psychiatry 2015;86:820–822. [DOI] [PubMed] [Google Scholar]
- 35.Antonelli A, Ferrari SM, Giuggioli D, Ferrannini E, Ferri C, Fallahi P. Chemokine (C-X-C motif) ligand (CXCL)10 in autoimmune diseases. Autoimmun Rev 2014;13:272–280. [DOI] [PubMed] [Google Scholar]
- 36.Titulaer MJ, McCracken L, Gabilondo I, et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol 2013;12:157–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Martinez-Hernandez E, Horvath J, Shiloh-Malawsky Y, Sangha N, Martinez-Lage M, Dalmau J. Analysis of complement and plasma cells in the brain of patients with anti-NMDAR encephalitis. Neurology 2011;77:589–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shorvon S, Ferlisi M. The treatment of super-refractory status epilepticus: a critical review of available therapies and a clinical treatment protocol. Brain 2011;134:2802–2818. [DOI] [PubMed] [Google Scholar]
- 39.Ferlisi M, Shorvon S. The outcome of therapies in refractory and super-refractory convulsive status epilepticus and recommendations for therapy. Brain 2012;135:2314–2328. [DOI] [PubMed] [Google Scholar]
- 40.Ferlisi M, Hocker S, Grade M, Trinka E, Shorvon S. Preliminary results of the global audit of treatment of refractory status epilepticus. Epilepsy Behav 2015;49:318–324. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.