Abstract
Introduction
College students are at higher than average risk for nonmedical use of prescription stimulants (NPS). A commonly identified motive among students who engage in NPS is to improve grades. Several research studies have observed that NPS most likely does not confer an academic advantage, and is associated with excessive drinking and other drug use. This study documents the proportion of the general college student population who believe that NPS will lead to improvements in academic performance.
Methods
This study gathered online survey data from a large, demographically diverse sample of college students to document the prevalence of perceived academic benefit of NPS for improving grades and to examine the association between such belief and NPS.
Results
Overall, 28.6% agreed or strongly agreed that NPS could help students earn higher grades, and an additional 38.0% were unsure. Students with a higher level of perceived academic benefit of NPS and more frequent patterns of drinking and marijuana use were more likely to engage in NPS, even after adjustment for a wide range of covariates.
Conclusions
The results underscore the need for interventions that simultaneously correct misperceptions related to academic benefit and target alcohol and marijuana use to reduce NPS.
Keywords: Academic achievement, motives for nonmedical use of prescription stimulants, alcohol use, marijuana use, undergraduates
1. Introduction
Nonmedical use of prescription stimulants (NPS) is defined as the use of a medication usually prescribed to treat Attention-Deficit/Hyperactivity Disorder (ADHD) without a prescription or in a way that is inconsistent with a doctor's orders (Colliver, Kroutil, Dai, & Gfroerer, 2006; DeSantis, Webb, & Noar, 2008; McCabe, West, & Wechsler, 2007; Substance Abuse and Mental Health Services Administration, 2006). In the US, 3.7% of full-time college students are estimated to have engaged in NPS during the past month (Substance Abuse and Mental Health Services Administration, 2016). Lifetime prevalence estimates of NPS vary, but studies among college students have found the range to be between 5.3% and 35% (DeSantis et al., 2008; DuPont, Coleman, Bucher, & Wilford, 2008; Weyandt et al., 2013). The Monitoring the Future study reported that college students are more likely than their non-college attending peers to use Adderall® nonmedically [10.7% vs. 7.1%, respectively; (Johnston, O'Malley, Bachman, Schulenberg, & Miech, 2016)]. NPS is more prevalent among college students who are white, male, members of a Greek organization, and whose parents have at least a four-year college degree (Johnston et al., 2016; McCabe, Knight, Teter, & Wechsler, 2005). Attending a college located in the Northeast or with highly competitive admission standards is also significantly associated with NPS (McCabe et al., 2005).
While prescription stimulants such as Adderall® and Ritalin® are beneficial for the treatment of ADHD (Chan, Fogler, & Hammerness, 2016; Wilens et al., 2006) using these drugs nonmedically is associated with risk for dependence and other substance use. McCabe et al. (2007) found that 12.6% of individuals who began engaging in NPS at age 19 became stimulant dependent, with lifetime stimulant dependence increasing with earlier initiation. Several cross-sectional studies have observed that nonmedical users of prescription stimulants also drink alcohol excessively and use illicit drugs, particularly cannabis (Arria et al., 2008a; DeSantis, Noar, & Webb, 2009; McCabe et al., 2005; Teter, McCabe, Boyd, & Guthrie, 2003). McCabe et al. (2005) found that students who engaged in NPS were more than ten times more likely to use cannabis during the past year than non-users.
The cognitive benefit of NPS has been called into question. Experimental studies have demonstrated that among individuals without an ADHD diagnosis, taking prescription stimulants does not result in marked cognitive improvement compared with controls (Advokat, 2010; Chamberlain et al., 2011; Ilieva, Boland, & Farah, 2013; Volkow et al., 2008). For example, Ilieva and colleagues (2013) conducted a double-blind placebo-controlled trial and found that Adderall® was not associated with enhancement of any of the thirteen cognitive measures assessed. One experimental study using a balanced placebo design reported a deterioration in performance associated with methylphenidate administration among individuals without ADHD (Volkow et al., 2008). The authors concluded that NPS might slow metabolic activation in an already optimally focused brain when performing cognitive tasks, thereby actually weakening cognitive performance.
One naturalistic longitudinal study of college students linked NPS with a pattern of increasing marijuana and alcohol use accompanied by increases in skipping class and decreases in grade point average [GPA; (Arria et al., 2013)]. Other cross-sectional research has also shown that college students who engage in NPS have lower GPAs and skip more classes (Clegg-Kraynok, McBean, & Montgomery-Downs, 2011; McCabe et al., 2005; McCabe, Teter, & Boyd, 2006; Rabiner et al., 2009). Nonmedical users of prescription stimulants also spend less time studying and more time socializing with their counterparts, patterns of behavior that would appear to impede academic performance (Arria, O'Grady, Caldeira, Vincent, & Wish, 2008b). A more recent study observed that students who initiate NPS show no statistically significant improvement in their GPA and gain no detectable advantages over their peers academically (Arria et al., 2017).
Although research studies have cast substantial doubt regarding the academic benefit of NPS, the belief that these drugs, when taken nonmedically, can improve academic performance appears to be widespread among college students who engage in NPS. Teter and colleagues (2006) examined student's motivations for NPS and found students believe that the drugs will enhance their concentration (65%), help with studying (60%), and increase alertness (48%). Consistently, academic motives are commonly reported among students who engage in NPS (Clegg-Kraynok et al., 2011; DeSantis et al., 2009; DeSantis et al., 2008; DuPont et al., 2008; Garnier-Dykstra, Caldeira, Vincent, O'Grady, & Arria, 2012; Low & Gendaszek, 2002; McCabe et al., 2005; Rabiner et al., 2009; Teter, McCabe, Cranford, Boyd, & Guthrie, 2005; Teter et al., 2006; White, Becker-Blease, & Grace-Bishop, 2006). However, the literature does not provide information about the range of beliefs that exist among the general college student population regarding the putative academic benefit of NPS. Studies examining motives for NPS can only be conducted among individuals who engage in use. Therefore, there is limited information about the perceived academic benefit of NPS among college students in general. The present study makes an important distinction by measuring how widespread the perceived academic benefit of NPS really is among a large college student sample.
Perceived benefits of using a substance influence the desire to initiate and maintain use of that substance (Cox & Klinger, 1988; Goldman, Brown, & Christiansen, 1987; Leigh, 1989). Positive or negative expectancies can mediate behavior and might have reinforcing effects on behavior over time (Jones, Corbin, & Fromme, 2001). Researchers have found the expected positive and negative consequences of NPS can be measured and classified (Labbe & Maisto, 2010; Looby & Earleywine, 2010), similar to other substances. Nonusers, recreational users, and medical users can be discriminated on the basis of expectancies (Looby & Earleywine, 2010). An exploratory factor analysis performed on the Prescription Stimulant Expectancy Questionnaire II revealed that nonusers of prescription stimulants held significantly weaker expectancies for cognitive enhancement and stronger expectancies for guilt and dependence compared with user groups. Combining positive items together and negative items together to create composite scales confirmed that nonusers of prescription stimulants held the strongest negative expectancies and recreational/medical users held the strongest positive expectancies. If predictive of use, the expectancy that NPS will confer academic advantages might be a valuable prevention target, both to avert initiation and to discourage continued use after initiation.
This study of a large, demographically diverse sample of college students sought to: a) describe the prevalence of perceived academic benefit of NPS as a viable means of improving grades, and b) examine the explanatory power of such belief for predicting NPS. We hypothesized that three constructs would be associated with NPS—namely, higher levels of perceived academic benefit, alcohol use, and marijuana use patterns after holding constant demographic variables.
2. Methods
2.1. Multi-site design
This multi-site study uses data collected from 8,039 full-time undergraduate students at nine colleges and universities in the US during the 2015-2016 academic year (see Table 1). The sites were selected based on variability by size, type, and geographic location. Students were randomly selected at every site, and eligibility was restricted to individuals between the ages of 18 and 25. A categorical variable for school was used to account for regional differences in prevalence of NPS.
Table 1. Sample size and response rate, by site.
| School | Description | N | Response rate | n for present analysis |
|---|---|---|---|---|
| A | Large public university, Pacific Northwest | 1538 | 28.7% | 1390 |
| B | Large public university, Mid-Atlantic | 3892 | 40.4% | 3312 |
| C | Large public university, Northeast | 1258 | 21.6% | 1108 |
| D | Small private college, Mountain-West | 128 | 32.8% | 102 |
| E | Small private college, Northeast | 106 | 20.8% | 92 |
| F | Large public university, Southeast | 388 | 10.1% | 339 |
| G | Medium-sized public university, Mountain-West | 138 | 21.4% | 114 |
| H | Large public university, Southeast | 440 | 15.6% | 369 |
| I | Small private college, Pacific Northwest | 151 | 39.0% | 136 |
|
| ||||
| Overall | 8039 | 27.3% | 6962 | |
2.2. Participant recruitment
Lists of randomly selected enrolled students were obtained from Registrar's Offices at each site. Students were invited via e-mail to participate in a 10- or 20-minute (varied by site) confidential online survey. Up to eight email reminders were sent to those who had not responded. At one site, items for the present study were administered as part of a larger survey measuring campus climate, and therefore recruitment emails originated from the university's Title IX office; at the other eight sites, recruitment emails originated from the principal investigators. The overall response rate was modest (27.3%, see Table 1). Students were paid $5 or $10 (depending on the length of the survey) for completing the assessment; at one site, $10 payments were offered to the first 3,000 participants. All procedures were approved by the Institutional Review Boards at each University, and participants received further protection under a federal Certificate of Confidentiality.
2.3. Participants
For the present study, the sample was restricted to the 7,287 individuals who indicated that they had never been diagnosed with ADHD. The decision to exclude students with an ADHD diagnosis was based on the notion that their perceptions about NPS might differ in meaningful ways from those of other students, as a result of their personal experiences with taking ADHD medications for their diagnosed condition. The final analytic sample was further restricted to the 6,962 individuals who had valid responses on all variables of interest for the present study (see Table 2). Missing data were minimal (≤2%). Self-reported gender was dichotomized as male (40.9%) and female (59.1%); transgendered and other responses were treated as missing due to small cell sizes (<1% of sample). Participants had a mean age of 19.94 (SD=1.46) years of age. Multiple response options were permitted for race, and later collapsed into four categories (62.1% White, 19.5% Asian, 9.9% Black or African-American, and 8.5% other or multiple). Ethnicity was assessed separately as Hispanic (9.3%) and not Hispanic.
Table 2. Sample characteristics by nonmedical use of prescription stimulants (NPS) during the past six months.
| Total (N=6962) | No NPS (n=6180) | NPS (n=782) | |
|---|---|---|---|
| Race | |||
| % (n) White | 62.1 (4320) | 60.4 (3734) | 74.9 (586) |
| % (n) Asian | 19.5 (1358) | 20.6 (1275) | 10.6 (83) |
| % (n) Black or African-American | 9.9 (692) | 10.4 (645) | 6.0 (47) |
| % (n) Multiple or other races | 8.5 (592) | 8.5 (526) | 8.4 (66) |
| Gender: % (n) Male | 40.9 (2844) | 39.7 (2455) | 49.7 (389) |
| Ethnicity: % (n) Hispanic or Latino/a | 9.3 (644) | 9.1 (560) | 10.7 (84) |
| Perceived academic benefit of NPS | |||
| % (n) Strongly disagree | 13.6 (948) | 15.0 (929) | 2.4 (19) |
| % (n) Disagree | 19.7 (1372) | 21.3 (1319) | 6.8 (53) |
| % (n) Unsure | 38.0 (2648) | 39.6 (2446) | 25.8 (202) |
| % (n) Agree | 23.3 (1623) | 20.6 (1271) | 45.0 (352) |
| % (n) Strongly agree | 5.3 (371) | 3.5 (215) | 19.9 (156) |
| Mean (SD) perceived academic benefit score | 2.9 (1.1) | 2.8 (1.1) | 3.7 (0.9) |
| Mean (SD) total drinks per week | 6.9 (8.3) | 5.9 (7.4) | 15.0 (10.4) |
| Mean (SD) days used marijuana during the past six months | 10.8 (32.3) | 6.8 (24.8) | 42.9 (56.8) |
Note. Perceived academic benefit of NPS was scored 1 (strongly disagree) through 5 (strongly agree).
2.4. Measures
2.4.1. Nonmedical use of prescription stimulants (NPS)
Participants were asked the number of days they had used prescription stimulants nonmedically during the past six months. NPS was defined as using a prescription stimulant that was not prescribed to you or that you took only for the experience or feeling it caused, as well as overusing a stimulant that you had been prescribed (Colliver et al., 2006; McCabe, 2008; Substance Abuse and Mental Health Services Administration, 2014). Along with this standard definition, the names of five different stimulant medications students might have used were provided as examples (e.g., “Ritalin®, Dexedrine®, Adderall®, Concerta®, methylphenidate”). Responses were later dichotomized as using at least once versus no use.
2.4.2. Perceived academic benefit of NPS
Students were asked to rate the degree to which they agree or disagree with the statement that “prescription stimulants will help people without a prescription get better grades.” Likert-type response options were scored one through five (i.e., strongly disagree, disagree, unsure, agree, strongly agree). This item was created for this study.
2.4.3. Alcohol use
Alcohol use was operationalized as the total number of drinks consumed in a typical week during the past six months, which was computed from responses to the Daily Drinking Questionnaire (Collins, Parks, & Marlatt, 1985). To minimize the excessive influence of extremely large values, 40 was selected as the maximum valid value, based on examination of the sample variance (i.e., approximately three standard deviations above the mean) combined with clinical experience validating the plausibility of 40 drinks per week. Values exceeding 40 were automatically recoded to 40 (n=61). Nondrinkers were coded as having zero drinks per week (30.9% of sample).
2.4.4. Marijuana use frequency
Students were asked the number of days they had used marijuana during the past six months. Valid values ranged from zero to 183.
2.5. Statistical analysis
First, descriptive statistics were computed for the overall sample and within the subsets of students who did and did not engage in NPS during the past six months. Second, a multivariate logistic regression model was developed with NPS as the binary dependent variable, and including three hypothesized explanatory variables (perceived academic benefit, alcohol use, marijuana use) and four demographic control variables (gender, race, ethnicity, school). Perceived academic benefit of NPS was operationalized as a continuous variable and as an ordinal variable in two alternative versions of the logistic regression, respectively.
3. Results
3.1. Prevalence of NPS
11.2% of the overall sample engaged in NPS during the past six months.
3.2. Prevalence of perceived academic benefit of NPS
Among the overall sample, 28.6% endorsed the belief that NPS could help students earn higher grades (23.3% agree + 5.3% strongly agree), and an additional 38.0% were unsure (see Table 2). Not surprisingly, compared with non-users, the proportion endorsing academic benefit was considerably higher (64.9%) among the subset who had engaged in NPS during the past six months (45.0% agree + 19.9% strongly agree), whereas the proportion who were unsure was somewhat lower (25.8%). It is noteworthy that, even among students who refrained from NPS, perceived academic benefit was relatively high, with the majority either endorsing such beliefs or at least remaining open-minded about them (20.6% agree + 3.5% strongly agree + 39.6% unsure=63.7%).
3.3. Intercorrelations
All correlations amongst the three hypothesized explanatory variables were modest (all rs<0.3) but statistically significant (all ps<.001; data not shown in a table).
3.4. Logistic regression on NPS
All three of the hypothesized explanatory variables were significantly and positively associated with NPS (see Table 3, Model A). Even accounting for the effects of school, demographics, and alcohol and marijuana use, students with higher perceived academic benefit of NPS were significantly more likely to engage in NPS (AOR=2.17, 95% CI=1.99 to 2.37, p<.001).
Table 3. Results of logistic regression predicting nonmedical use of prescription stimulants (NPS; N=6929).
| Model A | Model B | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| AOR | 95% CI | p | AOR | 95% CI | p | |||
| LB | UB | LB | UB | |||||
| Race | ||||||||
| Multiple, Other | 1.05 | 0.78 | 1.41 | 0.755 | 1.05 | 0.78 | 1.40 | 0.768 |
| Asian | 0.93 | 0.72 | 1.19 | 0.539 | 0.94 | 0.73 | 1.20 | 0.611 |
| Black or African-American | 0.75 | 0.55 | 1.03 | 0.078 | 0.76 | 0.55 | 1.04 | 0.086 |
| White (Ref.) | 1.00 | 1.00 | ||||||
| Gender | ||||||||
| Female | 1.20 | 1.02 | 1.42 | 0.026 | 1.21 | 1.03 | 1.42 | 0.024 |
| Male (Ref.) | 1.00 | 1.00 | ||||||
| Ethnicity | ||||||||
| Hispanic | 0.93 | 0.71 | 1.22 | 0.591 | 0.94 | 0.71 | 1.23 | 0.628 |
| Non-Hispanic (Ref.) | 1.00 | 1.00 | ||||||
| Alcohol use (drinks/week) | 1.08 | 1.07 | 1.08 | <.001 | 1.08 | 1.07 | 1.09 | <.001 |
| Marijuana use (frequency during the past six months) | 1.01 | 1.01 | 1.02 | <.001 | 1.01 | 1.01 | 1.02 | <.001 |
| Perceived academic benefit of NPS (score) | 2.17 | 1.99 | 2.37 | <.001 | ||||
| Perceived academic benefit of NPS (categorical) | ||||||||
| Disagree vs. Strongly disagree | 1.57 | 0.95 | 2.57 | 0.077 | ||||
| Unsure vs. Disagree | 1.89 | 1.41 | 2.54 | <.001 | ||||
| Agree vs. Unsure | 2.52 | 2.10 | 3.03 | <.001 | ||||
| Strongly agree vs. Agree | 2.14 | 1.67 | 2.74 | <.001 | ||||
Note. Results adjusted for school and all other effects shown. The overall effect of school was statistically significant (Wald X2 > 47.5, df=8, p<.001).
Post-hoc analysis
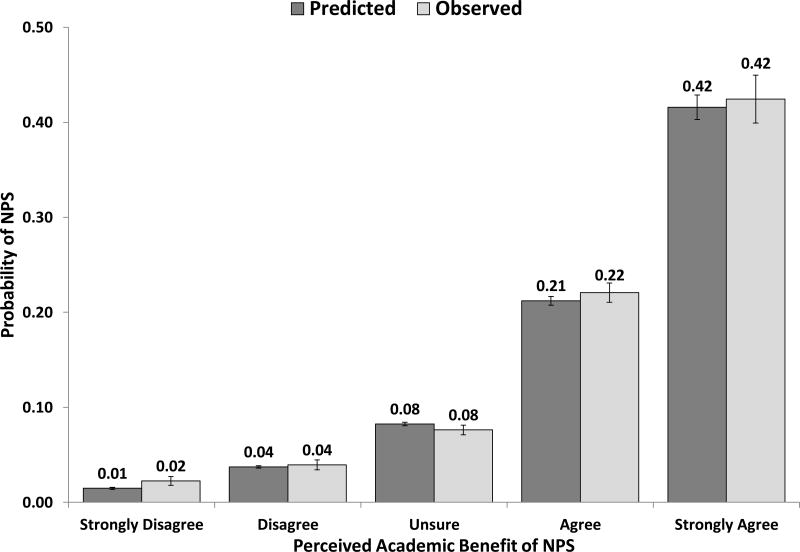
Examination of the model predicted probabilities of NPS suggested a non-linear relationship between perceived academic benefit and NPS (see Figure 1), such that the magnitude of change in risk varied depending on the level of perceived academic benefit. To elucidate this relationship, an alternative model was developed with perceived academic benefit entered as a categorical variable (see Table 3, Model B). With the sole exception of the contrast between Disagree and Strongly disagree, each increase in perceived academic benefit was associated with a significant increase in the adjusted odds of NPS, ranging from 1.89 (95% CI=1.41 to 2.54) for Unsure relative to Disagree, to 2.52 (95% CI=2.10 to 3.03) for Agree relative to Unsure.
Fig 1. Predicted and observed probabilities of engaging in nonmedical use of prescription stimulants (NPS) at least once during the past six months, by perceived academic benefit of NPS (N=6929).
Note. Model predicted probabilities are adjusted for the effects of alcohol use, marijuana use, school, gender, race, and ethnicity.
4. Discussion
In the present study, college students with the highest perceived academic benefit of NPS were more likely to report use, even after accounting for other factors. However, the belief of students observed in this study is in direct contrast to what is known from the scientific literature, namely, that no academic advantage or benefit of NPS seems to exist (Arria et al., 2017). Simply alerting students to this finding will likely not result in behavior change. However, when prevention opportunities and even successes with other substances, including alcohol, are considered, some potential opportunities to address NPS emerge.
On a broader scale, colleges and universities could consider targeting injunctive norms related to perceived academic benefit of NPS (e.g., “Most students don't think misusing prescription stimulants will help get better grades…They are right…Research shows no increase in GPA when people start or keep taking ADHD prescription stimulants that aren't prescribed to them”). Certainly, if a contributor to initiation of use is the belief that “everyone” does this during midterms and finals a social norms campaign highlighting that the majority of students on campus refrain from engaging in NPS could be implemented as well to address those descriptive norms. Although recent literature suggests that social norms campaigns have varying degrees of success in reducing excessive drinking during college, several studies support their impact (DeJong et al., 2006; Fitzpatrick, Martinez, Polidan, & Angelis, 2016; Scribner et al., 2011). Of course, such efforts require appropriate “dosing” (i.e., proper visibility for a media campaign), and could be evaluated for impact at potential high-risk times (e.g., prior to exams or project deadlines at the end of the quarter or semester).
The college student alcohol prevention and intervention literature is replete with examples of how increasing knowledge alone is insufficient to change behavior (National Institute on Alcohol Abuse and Alcoholism, 2015). However, information still has a place, particularly when delivered in the context of a motivational enhancement approach (National Institute on Alcohol Abuse and Alcoholism, 2015). Applications of Miller and Rollnick's (2013) Motivational Interviewing have consistently shown that developing discrepancies between values and goals (e.g., “I want to do better academically”) and the status quo (e.g., “it looks like nonmedical use of prescription stimulants isn't really resulting in better grades for me”) could prompt contemplation of or commitment to change within the context of a brief intervention. One means of connecting students to a brief intervention involves screening.
Using a public health framework to intervene early with students who have initiated NPS could be accomplished through Screening and Brief Intervention (SBI). SBI is a strategy through which college students are screened for alcohol and other drug use via assessment tools that can be presented via interview or online, and such screenings are recommended for integration into routine health visits (Moyer, 2013). They could also be integrated into counseling visits and dedicated screening days on campus. If screening results in positive identification of students engaging in NPS, they could be referred for follow-up interventions as indicated, either on or off campus. There is a voluminous literature on the efficacy of brief interventions with both general and target populations of college students in reducing or mitigating alcohol and drug use and its consequences (Carey, Scott-Sheldon, Carey, & DeMartini, 2007; Carey, Scott-Sheldon, Garey, Elliott, & Carey, 2016; National Institute on Alcohol Abuse and Alcoholism, 2015; Scott-Sheldon, Carey, Elliott, Garey, & Carey, 2014).
Once connected with a provider, a motivational interviewing-based brief intervention could be offered. This study observed that perceived academic benefit is one of the distinctions between individuals who engage in NPS and those that do not. Utilizing such information could be an important aspect of a motivational enhancement intervention because if the student is genuinely seeking academic improvement or success, findings that demonstrate a discrepancy (i.e., NPS is not providing this improvement) could result in behavior change. Especially during periods of high stress around midterms and final exams—times during which students are likely to seek services from campus health, counseling, and academic assistance centers for academic performance-related concerns—students might be even more likely to be receptive to such valuable information, particularly if paired with alternative behavioral strategies when they are of interest to the student. Expanding screening and intervention for substance use beyond traditional health and counseling centers to academic assistance centers would increase the likelihood of identifying students in need of such interventions. Because personalized feedback interventions have demonstrated success with reducing alcohol use and associated consequences (National Institute on Alcohol Abuse and Alcoholism, 2015) and similar interventions have shown promise with reducing cannabis use and related harms (Lee et al., 2013), such approaches to impact NPS can be developed and evaluated.
Finally, if academic motives are primarily driving NPS, connecting students who might be struggling academically to support services should be prioritized. Among a sample of students who screened positive for depression who felt like they needed help, but did not get help, the primary factor associated with not getting support was not knowing what was available to them (Eisenberg, Golberstein, & Gollust, 2007). If similar trends hold for NPS, raising student awareness of on-campus support services could be a step in the right direction, as could informing students of these services following a positive screen in a health or counseling center setting.
Study findings must be interpreted in the context of the limitations. Despite the variation in location, size, and type of the nine schools sampled, all of the schools were four-year institutions. Two-year institutions could provide a unique comparison given that community college students might have additional financial or familial responsibilities that could put additional pressures on their academic success. Future studies should compare the perceived academic benefit of NPS among students of both traditional four-year colleges and community colleges. The present study did not include students who ever had a diagnosis of ADHD. This is a potentially valuable population for future research, including both students who are not on medications and students with prescriptions who might divert their medication to students without an ADHD diagnosis. The perceived academic benefit of NPS is likely to be high among students with prescribed medication, but these students might not be aware that there are no cognitive benefits of prescription stimulant use among students without an ADHD diagnosis. Therefore, measuring the perceived academic benefit of NPS, alcohol use, and marijuana use among students with prescribed stimulants might be a useful way to identify the individuals most at risk for diversion. These students could be targeted in education and social norms campaigns to encourage them to not share their medication. The cross-sectional nature of the data collected prevents the researchers from making any inferences about the relationship between NPS and the perceived academic benefit of NPS, alcohol use, or marijuana use over time. Moreover, our measure of perceived academic benefit is novel, and has yet to be fully validated. Expanding the assessment of the construct beyond our single item measure would be useful to more fully understand nuances in student perceptions. Despite the diversity of our sample, representativeness is uncertain given the modest response rates; nevertheless, we are encouraged by the broad distribution of substance use patterns represented among this sample. Finally, NPS was dichotomized as using at least once versus no use during the last six months. This does not allow for analysis of different levels of NPS which might reveal important differences in perceived academic benefit, alcohol use, or marijuana use between frequent and occasional users.
The present study holds promise for both future research and practice. Future studies could examine the efficacy of SBI for students at risk for NPS, targeting perceived academic benefit of NPS, as well as alcohol and marijuana comorbidity with NPS. It could also be beneficial to examine the efficacy of such early interventions if and when offered within academic advising settings as part of routine meetings with college students focused on academic planning. Possible outcomes of such interventions might be altering the trajectory of intent to use stimulants nonmedically or actual NPS. Additional longitudinal research to further explore the relationship of perceived benefits (and harms) to future use and academic outcomes would also be beneficial.
Acknowledgments
Special thanks are extended to Brittany Bugbee, Christina Parisi, and the participants.
Role of Funding Source: Funding for this study was provided by the National Institute on Drug Abuse (U01DA040219, Drs. Geisner, Arria, Cimini, and Kilmer, Co-PIs). The findings and conclusions of this study are those of the authors and do not necessarily reflect the views of the National Institute on Drug Abuse, the National Institutes of Health, or the U.S. Department of Health and Human Services. Geetha Subramaniam and David Liu are employees of the Center for the Clinical Trials Network (CCTN), National Institute on Drug Abuse (NIDA), which is the funding agency for the National Drug Abuse Treatment Clinical Trials Network; their participation in this publication arises from their role as a project scientist on a cooperative agreement 1U01DA040219 for this study.
Footnotes
Conflicts of Interest: No conflicts declared.
References
- Advokat C. What are the cognitive effects of stimulant medications? Emphasis on adults with attention-deficit/hyperactivity disorder (ADHD) Neuroscience and Biobehavioral Reviews. 2010;34(8):1256–1266. doi: 10.1016/j.neubiorev.2010.03.006. [DOI] [PubMed] [Google Scholar]
- Arria AM, Caldeira KM, O'Grady KE, Vincent KB, Johnson EP, Wish ED. Nonmedical use of prescription stimulants among college students: Associations with ADHD and polydrug use. Pharmacotherapy. 2008a;28(2):156–169. doi: 10.1592/phco.28.2.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM, Caldeira KM, Vincent KB, O'Grady KE, Cimini MD, Geisner IM, Fossos-Wong N, Kilmer JR, Larimer ME. Do college students improve their grades by using prescription stimulants nonmedically? Addictive Behaviors. 2017;65:245–249. doi: 10.1016/j.addbeh.2016.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM, O'Grady KE, Caldeira KM, Vincent KB, Wish ED. Nonmedical use of prescription stimulants and analgesics: Associations with social and academic behaviors among college students. Journal of Drug Issues. 2008b;38(4):1045–1060. doi: 10.1177/002204260803800406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM, Wilcox HC, Caldeira KM, Vincent KB, Garnier-Dykstra LM, O'Grady KE. Dispelling the myth of “smart drugs”: Cannabis and alcohol use problems predict nonmedical use of prescription stimulants for studying. Addictive Behaviors. 2013;38(3):1643–1650. doi: 10.1016/j.addbeh.2012.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Carey MP, DeMartini KS. Individual-level interventions to reduce college student drinking: A meta-analytic review. Addictive Behaviors. 2007;32(11):2469–2494. doi: 10.1016/j.addbeh.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Garey L, Elliott JC, Carey MP. Alcohol interventions for mandated college students: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2016 doi: 10.1037/a0040275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamberlain SR, Robbins TW, Winder-Rhodes S, Müller U, Sahakian BJ, Blackwell AD, Barnett JH. Translational approaches to frontostriatal dysfunction in attention-deficit/hyperactivity disorder using a computerized neuropsychological battery. Biological Psychiatry. 2011;69(12):1192–1203. doi: 10.1016/j.biopsych.2010.08.019. [DOI] [PubMed] [Google Scholar]
- Chan E, Fogler JM, Hammerness PG. Treatment of attention-deficit/hyperactivity disorder in adolescents: A systematic review. Journal of the American Medical Association. 2016;315(18):1997–2008. doi: 10.1001/jama.2016.5453. [DOI] [PubMed] [Google Scholar]
- Clegg-Kraynok MM, McBean AL, Montgomery-Downs HE. Sleep quality and characteristics of college students who use prescription psychostimulants nonmedically. Sleep Medicine. 2011;12(6):598–602. doi: 10.1016/j.sleep.2011.01.012. [DOI] [PubMed] [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53(2):189–200. doi: 10.1037/0022-006X.53.2.189. [DOI] [PubMed] [Google Scholar]
- Colliver JD, Kroutil LA, Dai L, Gfroerer JC. Misuse of prescription drugs: Data from the 2002, 2003 and 2004 National Surveys on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2006. (No. DHHS Publication No. SMA 06-4192) [Google Scholar]
- Cox WM, Klinger E. A motivational model of alcohol use. Journal of Abnormal Psychology. 1988;97(2):168–180. doi: 10.1037/0021-843x.97.2.168. [DOI] [PubMed] [Google Scholar]
- DeJong W, Schneider SK, Towvim LG, Murphy MJ, Doerr EE, Simonsen NR, Mason KE, Scribner RA. A multisite randomized trial of social norms marketing campaigns to reduce college student drinking. Journal of Studies on Alcohol. 2006;67(6):868–879. doi: 10.15288/jsa.2006.67.868. [DOI] [PubMed] [Google Scholar]
- DeSantis A, Noar SM, Webb E. Nonmedical ADHD stimulant use in fraternities. Journal of Studies on Alcohol and Drugs. 2009;70(6):952–954. doi: 10.15288/jsad.2009.70.952. [DOI] [PubMed] [Google Scholar]
- DeSantis AD, Webb EM, Noar SM. Illicit use of prescription ADHD medications on a college campus: A multimethological approach. Journal of American College Health. 2008;57(3):315–323. doi: 10.3200/JACH.57.3.315-324. [DOI] [PubMed] [Google Scholar]
- DuPont RL, Coleman JJ, Bucher RH, Wilford BB. Characteristics and motives of college students who engage in nonmedical use of methylphenidate. American Journal on Addictions. 2008;17(3):167–171. doi: 10.1080/10550490802019642. [DOI] [PubMed] [Google Scholar]
- Eisenberg D, Golberstein E, Gollust SE. Help-seeking and access to mental health care in a university student population. Medical Care. 2007;45(7):594–601. doi: 10.1097/MLR.0b013e31803bb4c1. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick BG, Martinez J, Polidan E, Angelis E. On the effectiveness of social norms intervention in college drinking: The roles of identity verification and peer influence. Alcoholism, Clinical And Experimental Research. 2016;40(1):141–151. doi: 10.1111/acer.12919. [DOI] [PubMed] [Google Scholar]
- Garnier-Dykstra LM, Caldeira KM, Vincent KB, O'Grady KE, Arria AM. Nonmedical use of prescription stimulants during college: Four-year trends in exposure opportunity, use, motives, and sources. Journal of American College Health. 2012;60(3):226–234. doi: 10.1080/07448481.2011.589876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman MS, Brown SA, Christiansen BA. Expectancy theory - Thinking about drinking. In: Blane HT, Leonard KE, editors. Psychological theories of drinking and alcoholism. New York, NY: Guilford Publications; 1987. pp. 181–226. [Google Scholar]
- Ilieva I, Boland J, Farah MJ. Objective and subjective cognitive enhancing effects of mixed amphetamine salts in healthy people. Neuropharmacology. 2013;64:496–505. doi: 10.1016/j.neuropharm.2012.07.021. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE, Miech RA. Monitoring the Future: National survey results on drug use, 1975–2015: Volume 2, college students and adults ages 19–55. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2016. [Google Scholar]
- Jones BT, Corbin W, Fromme K. A review of expectancy theory and alcohol consumption. Addiction. 2001;96(1):57–72. doi: 10.1080/09652140020016969. [DOI] [PubMed] [Google Scholar]
- Labbe AK, Maisto SA. Development of the Stimulant Medication Outcome Expectancies Questionnaire for college students. Addictive Behaviors. 2010;35(7):726–729. doi: 10.1016/j.addbeh.2010.03.010. [DOI] [PubMed] [Google Scholar]
- Lee CM, Kilmer JR, Neighbors C, Atkins DC, Zheng C, Walker DD, Larimer ME. Indicated prevention for college student marijuana use: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2013;81(4):702–709. doi: 10.1037/a0033285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh BC. In search of the seven dwarves: Issues of measurement and meaning in alcohol expectancy research. Psychological Bulletin. 1989;105(3):361–373. doi: 10.1037/0033-2909.105.3.361. [DOI] [PubMed] [Google Scholar]
- Looby A, Earleywine M. Psychometric evaluation of a Prescription Stimulant Expectancy Questionnaire. Experimental and Clinical Psychopharmacology. 2010;18(4):375–383. doi: 10.1037/a0019347. [DOI] [PubMed] [Google Scholar]
- Low KG, Gendaszek AE. Illicit use of psychostimulants among college students: A preliminary study. Psychology, Health and Medicine. 2002;7(3):283–287. doi: 10.1080/13548500220139386. [DOI] [Google Scholar]
- McCabe SE. Screening for drug abuse among medical and nonmedical users of prescription drugs in a probability sample of college students. Archives of Pediatrics and Adolescent Medicine. 2008;162(3):225–231. doi: 10.1001/archpediatrics.2007.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Knight JR, Teter CJ, Wechsler H. Non-medical use of prescription stimulants among US college students: Prevalence and correlates from a national survey. Addiction. 2005;99(1):96–106. doi: 10.1111/j.1360-0443.2005.00944.x. [DOI] [PubMed] [Google Scholar]
- McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use and diversion of prescription stimulant medication. Journal of Psychoactive Drugs. 2006;38(1):43–56. doi: 10.1080/02791072.2006.10399827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Morales M, Cranford JA, Boyd CJ. Does early onset of non-medical use of prescription drugs predict subsequent prescription drug abuse and dependence? Results from a national study. Addiction. 2007;102(12):1920–1930. doi: 10.1111/j.1360-0443.2007.02015.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Wechsler H. Trends and college-level characteristics associated with the non-medical use of prescription drugs among US college students from 1993 to 2001. Addiction. 2007;102(3):455–465. doi: 10.1111/j.1360-0443.2006.01733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Helping people change. 3rd. New York, NY: Guilford Press; 2013. [Google Scholar]
- Moyer VA. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: U.S. Preventive Services Task Force recommendation statement. Annals of Internal Medicine. 2013;159(3):210–218. doi: 10.7326/0003-4819-159-3-201308060-00652. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Planning alcohol interventions using NIAAA's CollegeAIM (Alcohol Intervention Matrix) Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2015. [Google Scholar]
- Rabiner DL, Anastopoulos AD, Costello EJ, Hoyle RH, McCabe SE, Swartzwelder HS. Motives and perceived consequences of nonmedical ADHD medication use by college students: Are students treating themselves for attention problems? Journal of Attention Disorders. 2009;13(3):259–270. doi: 10.1177/1087054708320399. [DOI] [PubMed] [Google Scholar]
- Scott-Sheldon LAJ, Carey KB, Elliott JC, Garey L, Carey MP. Efficacy of alcohol interventions for first-year college students: A meta-analytic review of randomized controlled trials. Journal of Consulting and Clinical Psychology. 2014;82(2):177–188. doi: 10.1037/a0035192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scribner RA, Theall KP, Mason K, Simonsen N, Schneider SK, Towvim LG, Dejong W. Alcohol prevention on college campuses: The moderating effect of the alcohol environment on the effectiveness of social norms marketing campaigns. Journal of Studies on Alcohol and Drugs. 2011;72(2):232–239. doi: 10.15288/jsad.2011.72.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2005 National Survey on Drug Use and Health: National findings. Rockville, MD: Office of Applied Studies; 2006. (NSDUH Series H-30). [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2013 national survey on drug use and health: Summary of national findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2015 National Survey on Drug Use and Health: Detailed tables. Rockville, MD: US Department of Health and Human Services, Office of Applied Studies; 2016. [Google Scholar]
- Teter CJ, McCabe SE, Boyd CJ, Guthrie SK. Illicit methylphenidate use in an undergraduate student sample: Prevalence and risk factors. Pharmacotherapy. 2003;23(5):609–617. doi: 10.1592/phco.23.5.609.34187. [DOI] [PubMed] [Google Scholar]
- Teter CJ, McCabe SE, Cranford JA, Boyd CJ, Guthrie SK. Prevalence and motives for illicit use of prescription stimulants in an undergraduate student sample. Journal of American College Health. 2005;53(6):253–262. doi: 10.3200/JACH.53.6.253-262. [DOI] [PubMed] [Google Scholar]
- Teter CJ, McCabe SE, LaGrange K, Cranford JA, Boyd CJ. Illicit use of specific prescription stimulants among college students: Prevalence, motives, and routes of administration. Pharmacotherapy. 2006;26(10):1501–1510. doi: 10.1592/phco.26.10.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Fowler JS, Wang GJ, Telang F, Logan J, Wong C, Ma J, Pradhan K, Benveniste H, Swanson JM. Methylphenidate decreased the amount of glucose needed by the brain to perform a cognitive task. PLoS ONE. 2008;3(4):e2017–e2017. doi: 10.1371/journal.pone.0002017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weyandt LL, Marraccini ME, Gudmundsdottir BG, Zavras BM, Turcotte KD, Munro BA, Amoroso AJ. Misuse of prescription stimulants among college students: A review of the literature and implications for morphological and cognitive effects on brain functioning. Experimental and Clinical Psychopharmacology. 2013;21(5):385–407. doi: 10.1037/a0034013. [DOI] [PubMed] [Google Scholar]
- White BP, Becker-Blease KA, Grace-Bishop K. Stimulant medication use, misuse, and abuse in an undergraduate and graduate student sample. Journal of American College Health. 2006;54(5):261–268. doi: 10.3200/JACH.54.5.261-268. [DOI] [PubMed] [Google Scholar]
- Wilens TE, McBurnett K, Bukstein O, McGough J, Greenhill L, Lerner M, et al. Multisite controlled study of OROS methylphenidate in the treatment of adolescents with attention-deficit/hyperactivity disorder. Archives of Pediatrics and Adolescent Medicine. 2006;160(1):82–90. doi: 10.1001/archpedi.160.1.82. [DOI] [PubMed] [Google Scholar]