Abstract
Involuntary unemployment due to job loss has been associated with increased risk of cardiovascular events. Whether it also is associated with increased risk of atrial fibrillation (AF) is currently unknown. Therefore, we examined this association in 8,812 participants residing mainly in the Southeastern United States (mean age 58.1 ± 7.8 years; 63.2%; women; 43.2% black) with data on employment status who were enrolled in the REasons for Geographic And Racial Differences in Stroke (REGARDS) study between 2003 and 2007 after excluding those with voluntary unemployment (e.g. retiree and students). AF was identified by electrocardiogram and past medical history at the same period. The cross-sectional association between status and type of unemployment with AF was examined in multivariable logistic regression models. Additional analysis in 4,273 participants without baseline AF and with data on incident AF collected in a follow up visit occurred after a median of 9.4 years from baseline was also conducted. In a model adjusted for socio-demographics, health insurance, income, perceived stress and cardiovascular risk factors, unemployment was associated with 60% increased odds of AF (OR (95%CI): 1.60 (1.24, 2.07). This association was consistent in subgroups stratified by median age, sex, race, education, income, and health insurance status. Similarly, unemployment was associated with AF in those without AF at baseline who developed incident AF (OR (95%CI):1.54 (1.04, 2.37). In conclusion, involuntary unemployment is associated with increased risk of AF. This may call for considering socio-economic determinants such as unemployment as part of the preventive strategies for AF.
Keywords: Atrial fibrillation, Unemployment, Job loss
Introduction
Employment instability affects an increasing number of adults in the United States. The psychological stress that comes with involuntary job loss or inability to find a job (i.e. unemployment) has a significant long term consequences on cardiovascular health (1). Previous reports have shown that unemployment and job loss are significant risk factors for acute cardiovascular events including myocardial infarction and stroke (2, 3, 4). Whether, unemployment is associated with increased risk of atrial fibrillation (AF) as well is currently unknown. Psychological stress has been implicated as a risk factor for AF (5–7), and hence it is possible that unemployment predisposes to development of AF. Looking for new modifiable risk factors for AF is becoming of significant importance from the public health perspective since its prevalence is expected to double by 2050 (8). Therefore, we sought to examine the association between involuntary unemployment and AF in the REasons for Geographic And Racial Differences in Stroke (REGARDS) study.
Methods
The goals and design of the REGARDS study, a U.S. national longitudinal study, have been published. REGARDS was designed to investigate causes of regional and racial disparities in stroke mortality, oversampling blacks and residents of the southeastern states “stroke belt region” (9). Individuals were recruited from a commercially available list of residents using mail and telephone contact. Demographic information and medical history including perceived stress measured by the Cohen Perceived Stress 16-point Scale (10) were obtained by telephone interview. All methods were approved by Institutional Human Subjects Review Boards. A brief physical examination was conducted 3 to 4 weeks after the telephone interview, including standardized measurements of risk factors, collection of blood and urine, and recording of resting electrocardiogram.
Of 30 239 REGARDS participants enrolled between 2003 and 2007, employment status was evaluated in 18,800 REGARDS participants. Participants were specifically asked: “Are you currently employed for wages, self-employed, out of work for >1 year, out of work for <1 year, a homemaker, a student, retired, or unable to work?” For the purpose of this analysis, we excluded those who refused to answer (n=9) and unemployed voluntarily (retired (n=8,655), homemaker (n=1,046) and student (n=47)) as well as those with missing AF data (n=231).
AF was identified in study participants at baseline by the scheduled electrocardiogram (ECG) and also from self- reported history of a physician diagnosis during the computer-assisted telephone interview surveys. The ECGs were read and coded at a central reading center by electrocardiographers who were blind to other REGARDS data. Self-reported AF was defined as an affirmative response to the following question: “Has a physician or a health professional ever told you that you had atrial fibrillation? (11).
The cross-sectional association between status and type of unemployment with AF was examined in multivariable logistic regression models. Multivariable models were constructed with incremental adjustments as follows: Model 1 adjusted for age, sex, race, region of residence, and education level; Model 2 adjusted for Model 1 covariates plus income, and insurance status; Model 3 adjusted for Model 2 covariates plus perceived stress; Model 4 adjusted for model 3 plus Systolic blood pressure, high density lipoprotein cholesterol, low density lipoprotein cholesterol, body mass index, smoking status, diabetes, blood pressure lowering medications use, lipid-lowering medications use, history of coronary heart disease, history of stroke, high-sensitivity C-reactive protein levels, albumin-to-creatinine ratio, history of heart failure, history of stroke, and electrocardiographic left ventricular hypertrophy using Sokolow-Lyon criteria. Additional analysis in those without baseline AF and with data on incident AF collected during REGARDS second in-home visit was also conducted.
Results
This analysis included 8,812 participants residing mainly in the Southeastern United States (mean age 58.1 ± 7.8 years; 63.2%; women; 43.2% black). Hypertension, dyslipidemia and diabetes were common (prevalence 52.2%, 54.5% and 19.5% respectively) and most participants (88.6%) had health insurance. Unemployed participants (total n=2095; out of work >1 year n=295; out of work <1 year n=287; unable to work n=1513) were more likely to be slightly older, women, black, with lower levels of socio-economic markers, and higher prevalence of cardiovascular risk factors compared to employed participants (total n=6717; employed for wages n=5009; self-employed n=1708) (Table 1).
Table 1.
Characteristics of the study participants by employment status
| Characteristic | Unemployed (n=2,095) | Employed (n=6,717) | P-value |
|---|---|---|---|
| Age (years) | 58.6 ± 7.8 | 58.0 ± 7.8 | .002 |
| Women | 68.1% | 61.7% | <.001 |
| Black | 55.0% | 34.7% | <.001 |
| Region of residence* | <.001 | ||
| Stroke Belt | 37.6% | 34.7% | |
| Stroke Buckle | 29.4% | 25.4% | |
| Non-belt | 33.1% | 39.9% | |
| Education | <.001 | ||
| High school or less | 49.4 % | 22.4% | |
| Some college | 30.8 % | 28.1% | |
| College graduate and above | 19.8 % | 49.5% | |
| Annual income | <.001 | ||
| < $20k | 41.6% | 7.6% | |
| $20k to $74k | 37.3% | 54.3% | |
| >$75k | 4.8% | 29.5% | |
| Refused to answer | 16.3% | 8.7% | |
| Health insurance | 82.8% | 90.3% | <.001 |
| Perceived stress score | 5.2 ± 3.4 | 3.1 ± 2.6 | <.001 |
| Smoker | <.001 | ||
| Current | 26.5% | 14.8% | |
| Past | 33.1% | 33.6% | |
| Body mass index (kg/m2) | 31.7 ± 7.8 | 29.6 ± 6.2 | <.001 |
| Diabetes mellitus | 34.1% | 14.0% | <.001 |
| Systolic blood pressure (mm Hg) | 126 ± 16.6 | 123.0 ± 15.1 | <.001 |
| Blood pressure lowering medications use | 67.2% | 47.3% | <.001 |
| Left ventricular hypertrophy | 9.8% | 6.3% | <.001 |
| LDL-cholesterol (mg/dL) | 113.7 ± 37.5 | 116.6± 34.4 | .002 |
| HDL-cholesterol (mg/dL) | 51.3 ± 15.8 | 53.1 ± 16.2 | .002 |
| Lipid-lowering medication use | 35.7% | 25.8% | <.001 |
| Log(hs-CRP) (mg/L) | 1.2 ± 1.2 | 0.70 ± 1.2 | <.001 |
| Log (ACR) (mg/g) | 2.6 ± 1.5 | 2.1 ± 1.0 | <.001 |
| Prior coronary heart disease | 21.4% | 9.5% | <.001 |
| Prior stroke | 12.3% | 2.2% | <.001 |
| Prior heart failure | 21.4% | 8.0% | <.001 |
Stroke Belt (southeast states of North Carolina, South Carolina, Georgia, Tennessee, Alabama, Mississippi, Louisiana, and Arkansas) Stroke Buckle (coastal plains of North Carolina, South Carolina, and Georgia)
Perceived stress was measured by the Cohen Perceived Stress 16-point Scale
ACR=urine albumin-to-creatinine ratio; HDL=high-density lipoprotein; LDL=Low-density lipoprotein; hs-CRP=high-sensitivity C-reactive protein
AF was detected in 673 (7.6%) participants (13.4% in unemployed vs. 5.8% in employed; p-value <0.001). In a socio-demographic model, unemployment was associated with more than double the odds of AF. This association was attenuated to be 60% (p<0.001) by further adjustment for health insurance, income, perceived stress cardiovascular risk factors (Table 2). These results were consistent in subgroups stratified by median age (57 years), sex, race, education, income, and health insurance status (Figure 1). Compared to the employed participants, the highest odds of AF were observed in those unable to work, then lost job for > a year then lost job for < a year (Odd ratio (95% Confidence Interval) (OR (95% CI):1.77(1.33, 2.36); 1.45(0.84, 2.49); 1.09(0.61, 1.93), respectively; trend p-value <0.01).
Table 2.
Association of unemployment with atrial fibrillation
| Model | Odds ratio (95% Confidence Interval) * | p-value | |
|---|---|---|---|
| 1: | Socio-demographic variables † | 2.44 (2.05, 2.90) | <.001 |
| 2: | Model 2 plus economic variables‡ | 2.31 (1.88, 2.83) | <.001 |
| 3: | Model 2 plus perceived stress § | 2.02 (1.63, 2.50) | <.001 |
| 4: | Model 3 plus cardiovascular risk factors|| | 1.60 (1.24, 2.07) | <.001 |
Odds ratio for AF in unemployed vs. employed participants using logistic regression analysis.
Age, sex, race, region of residence, education level
Income and health insurance status
Perceived stress measured by the Cohen Perceived Stress 16-point Scale
Systolic blood pressure, high density lipoprotein cholesterol, low density lipoprotein cholesterol, body mass index, smoking status, diabetes, blood pressure lowering medications use, lipid-lowering medications use, history of coronary heart disease, history of stroke, high-sensitivity C-reactive protein levels, albumin-to-creatinine ratio, history of heart failure, history of stroke, and electrocardiographic left ventricular hypertrophy.
Figure 1. Association of unemployment with atrial fibrillation in subgroups.
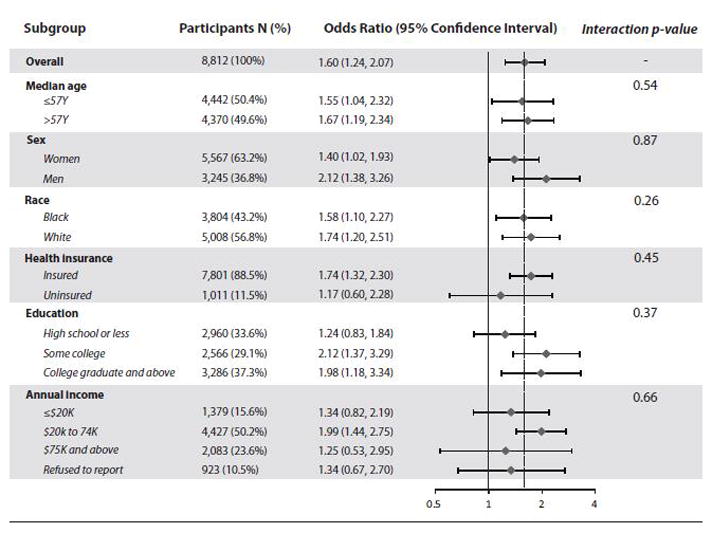
Odds ratio for AF in unemployed vs. employed participants using logistic regression analysis in model adjusted for age, sex, race, region of residence, education level, income and health insurance status, perceived stress, systolic blood pressure, high density lipoprotein cholesterol, low density lipoprotein cholesterol, body mass index, smoking status, diabetes, blood pressure lowering medications use, lipid-lowering medications use, history of coronary heart disease, history of stroke, high-sensitivity C-reactive protein levels, albumin-to-creatinine ratio, history of heart failure, history of stroke, and electrocardiographic left ventricular hypertrophy.
In additional analysis limited to 4,273 participants without AF at baseline and with follow up data, AF (n=227) developed more often during a median follow up of 9.4 years in the unemployed compared to the employed (6.4% vs. 5.1%, p<0.001). The OR (95% CI) was 1.73 (1.15, 2.58) in the socio-demographics and economic factors model, which became 1.66 (1.09, 2.50) with further adjustment for perceived stress, then 1.54 (1.04, 2.37) with further adjustment for key CVD risk factors (hypertension, diabetes, dyslipidemia, smoking and electrocardiographic left ventricular hypertrophy).
Discussion
The prevalence of AF is expected to double by 2050 (8), and hence identifying new risk factors for AF is becoming of a significant public health importance. Up to our knowledge, this is the first report that links unemployment, a socio-economic problem that concerns a large sector of the United States population, with AF. This may suggest considering the socio-economic factors not only the traditional risk factors when it comes to discussing potential preventive strategies for AF.
Psychological stress and lack of financial resources have been suggested as key factors contributing to increased risk of cardiovascular events in individuals losing their jobs or unable to work (2, 3). This could be the case too with AF, given the observed attenuation after adjustments for these factors in our study. Notably, the association remained strong despite adjustment for dozen potential confounders suggesting that the impact of unemployment on AF is more complex than being mediated by common risk factors. Further studies should investigate the mechanisms by which unemployment leads to AF and to identify viable targets for successful interventions.
Our results should be read in the context of certain limitations. Residual confounding and inability to confirm temporal relationship, which we tried to address by adjusting for several potential confounders and supplementing our results by additional longitudinal analysis, should be noted. Also, one of the methods we used in AF ascertainment was self-reported history of past physician diagnosis which is subject to recall bias. Since not all of the participants had health insurance, we might have missed some paroxysmal AF cases that might have occurred in those uninsured which would have been picked by self-reported past medical history and unlikely be picked by study scheduled ECG. Despite these limitations, this is the first report linking unemployment to AF using data from a racially diverse cohort that has a large sample size and with well-ascertained outcomes.
Acknowledgments
Funding Support: This research project is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke, National Institutes of Health, Department of Health and Human Service. The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Weber A, Lehnert G. Unemployment and cardiovascular diseases: a causal relationship? Int Arch Occup Environ Health. 1997;70:153–160. doi: 10.1007/s004200050201. [DOI] [PubMed] [Google Scholar]
- 2.Dupre ME, George LK, Liu G, Peterson ED. The cumulative effect of unemployment on risks for acute myocardial infarction. Arch Intern Med. 2012;172:1731–1737. doi: 10.1001/2013.jamainternmed.447. [DOI] [PubMed] [Google Scholar]
- 3.Gallo WT, Teng HM, Falba TA, Kasl SV, Krumholz HM, Bradley EH. The impact of late career job loss on myocardial infarction and stroke: a 10 year follow up using the health and retirement survey. Occup Environ Med. 2006;63:683–687. doi: 10.1136/oem.2006.026823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Henriksson KM, Lindblad U, Agren B, Nilsson-Ehle P, Rastam L. Associations between unemployment and cardiovascular risk factors varies with the unemployment rate: the Cardiovascular Risk Factor Study in Southern Sweden (CRISS) Scand J Public Health. 2003;31:305–311. doi: 10.1080/14034940210164948. [DOI] [PubMed] [Google Scholar]
- 5.Eaker ED, Sullivan LM, Kelly-Hayes M, D’Agostino RB, Sr, Benjamin EJ. Anger and hostility predict the development of atrial fibrillation in men in the Framingham Offspring Study. Circulation. 2004;109:1267–1271. doi: 10.1161/01.CIR.0000118535.15205.8F. [DOI] [PubMed] [Google Scholar]
- 6.Eaker ED, Sullivan LM, Kelly-Hayes M, D’Agostino RB, Sr, Benjamin EJ. Tension and anxiety and the prediction of the 10-year incidence of coronary heart disease, atrial fibrillation, and total mortality: the Framingham Offspring Study. Psychosom Med. 2005;67:692–696. doi: 10.1097/01.psy.0000174050.87193.96. [DOI] [PubMed] [Google Scholar]
- 7.Lampert R, Jamner L, Burg M, Dziura J, Brandt C, Liu H, Li F, Donovan T, Soufer R. Triggering of symptomatic atrial fibrillation by negative emotion. J Am Coll Cardiol. 2014;64:1533–1534. doi: 10.1016/j.jacc.2014.07.959. [DOI] [PubMed] [Google Scholar]
- 8.Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285:2370–2375. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 9.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, Graham A, Moy CS, Howard G. The reasons for geographic and racial differences in stroke study: Objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 10.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 11.Soliman EZ, Howard G, Meschia JF, Cushman M, Muntner P, Pullicino PM, McClure LA, Judd S, Howard VJ. Self-reported atrial fibrillation and risk of stroke in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. Stroke. 2011;42:2950–2953. doi: 10.1161/STROKEAHA.111.621367. [DOI] [PMC free article] [PubMed] [Google Scholar]


