Abstract
Background and Objectives
Trapped thrombus in patent foramen ovale (PFO) is a rare complication of pulmonary embolism that may lead to tragic clinical events. The aim of this study was to identify the optimal treatment for different clinical situations in patients with trapped thrombus in a PFO by conducting a literature review.
Subjects and Methods
A PubMed database search was conducted from 1991 through 2015, and 194 patients (185 articles) with trapped thrombus in a PFO were identified. Patient characteristics, paradoxical embolic events, and factors affecting 60-day mortality were analyzed retrospectively.
Results
Among all patients, 112 (57.7%) were treated with surgery, 28 with thrombolysis, and 54 with anticoagulation alone. Dyspnea (79.4%), chest pain (33.0%), and syncope (17.5%) were the most common presenting symptoms. Pretreatment embolism was found in 37.6% of cases, and stroke (24.7%) was the most common event. Surgery was associated with fewer post-treatment embolic events than were other treatment options (p=0.044). In the multivariate analysis, initial shock or arrest, and thrombolysis were independent predictors of 60-day mortality. Thrombolysis was related with higher 60-day mortality compared with surgery in patients who had no initial shock or arrest.
Conclusion
This systematic review showed that surgery was associated with a lower overall incidence of post-treatment embolic events and a lower 60-day mortality in patients with trapped thrombus in a PFO. In patients without initial shock or arrest, thrombolysis was related with a higher 60-day mortality compared with surgery.
Keywords: Foramen ovale, patent; Pulmonary embolism; Review, systematic
INTRODUCTION
The incidence of pulmonary embolism in the general population has risen along with increases in lifespan and chronic disease. The clinical presentation of pulmonary embolism is variable and the condition can lead to fatal clinical events. Patent foramen ovale (PFO) is a common congenital defect that is associated with increased incidence of stroke.1),2) In patients with pulmonary embolism, PFO is known to be related to high mortality.3) The transient increase in right heart pressure caused by pulmonary embolism is believed to facilitate right-to-left shunting and paradoxical embolism through a PFO. However, reports of trapped thrombus in a PFO that would provide direct evidence of paradoxical embolism are few, and treatment options are unclear.
We report 1 case of a trapped thrombus in a PFO that occurred in a patient with pulmonary embolism. In addition, we conducted a literature review of related reports in order to identify the clinical presentation, incidence of paradoxical embolism, and treatment options related to mortality in these patients.
SUBJECTS AND METHODS
Case presentation
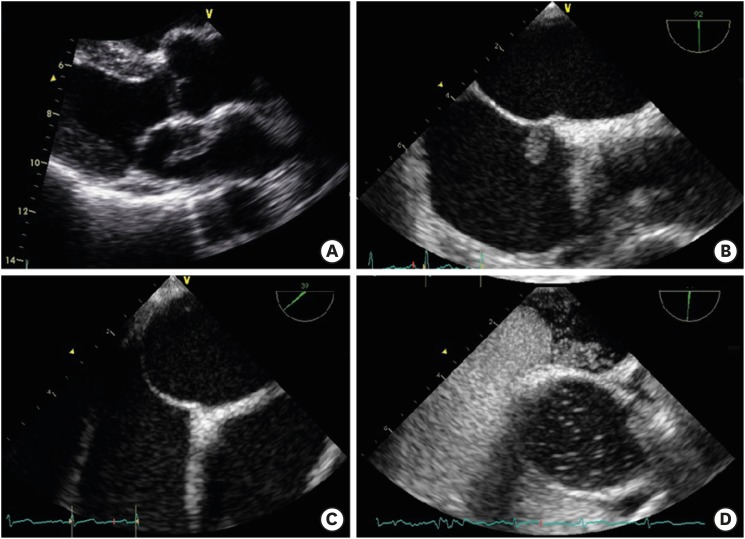
A 55-year-old woman presented to the emergency department with a 10-day history of progressive dyspnea. She had no significant past medical history. The initial electrocardiogram showed normal sinus rhythm with an S1Q3T3 pattern. She complained of severe dyspnea and her oxygen saturation in room air was 84%. Initial laboratory test results showed elevated serum D-dimer at 4.68 mg/L. Computed tomography confirmed extensive pulmonary embolism. Transthoracic echocardiography showed a large hypermobile mass in the left atrium. The mass was consistent with a thrombus trapped in the PFO, meaning that it was adherent to the atrial septum and prolapsed into the left ventricle (Figure 1A).
Figure 1.
Echocardiographic images of trapped thrombi in the PFO. (A) Initial transthoracic echocardiography shows a large hypermobile mass that was consistent with a thrombus trapped in a PFO. (B) Transesophageal echocardiography obtained 1 day after thrombolysis with intravenous alteplase shows a small remnant thrombus trapped in the PFO. (C) Repeat transesophageal echocardiography obtained after 1-month of oral anticoagulation therapy confirmed complete resolution of the thrombus trapped in the PFO, and (D) agitated saline test shows a positive result for the PFO.
PFO = patent foramen ovale.
Because of severe dyspnea and a high risk of paradoxical embolism, the patient underwent thrombolysis with intravenous alteplase. After thrombolysis, the symptoms were significantly relieved without bleeding or embolic complications. One day after thrombolysis, transesophageal echocardiography showed a small remnant thrombus trapped in the PFO (Figure 1B). The patient was discharged on anticoagulation therapy with dabigatran. One month later, repeat transesophageal echocardiography confirmed complete resolution of the thrombus trapped in the PFO, with a positive agitated saline PFO test (Figure 1C and D).
Collection of data
We searched the PubMed database from 1991 through September 2015, by using the combined search terms “thrombus” and “patent foramen ovale” or “paradoxical embolism” or “biatrial.” In addition, the references cited in all the selected articles were identified through a manual search. We selected only English language reports of thrombus trapped in the PFO that were clearly visualized, with or without paradoxical embolism. We only accepted studies that had information on patient demographics, presentation symptoms or signs, diagnostic imaging tools, treatment options, and treatment outcomes. From 2,737 potentially relevant studies, 185 were selected, yielding 194 patients (including the current case) with trapped thrombus in the PFO (listed in Supplementary References).
Essential data elements that were recorded for each patient included the following: age, sex, cause of pulmonary embolism (provoked, unprovoked, or cancer related), presentation symptom or sign, paradoxical embolic event, primary treatment option (surgery, thrombolysis, or anticoagulation), and clinical outcome (survival or death). Unprovoked pulmonary embolism included cases of unknown definite cause of the first or recurring event, antiphospholipid syndrome, and inherited thrombophilia (i.e., factor V Leiden mutation, protein S/C deficiency, and antithrombin deficiency). Provoked embolism included cases of prolonged hospitalization because of acute or chronic illness, post-operative, major trauma, venous external compression (i.e., May-Thurner syndrome, large myoma, or ovarian mass), pregnancy, and economic class syndrome. The treatment option described as conservative management was classified in the anticoagulation group. The patients who received multiple treatments were classified based on the last treatment option.
Statistical analysis
Continuous variables are presented as the mean±standard deviation, while categorical variables are presented as numbers and percentages. Differences among continuous variables were analyzed by one-way analysis of variance, and those among categorical variables by the χ2 test. Post-hoc analysis of variance was done using Bonferroni correction for the variables that showed overall significance. Cumulative mortality was assessed using the Kaplan-Meier method and compared using the log-rank test. Multivariable Cox regression analysis was used to evaluate the adjusted relative risk of each variable, including treatment option. All statistical analyses were performed using SPSS for Windows, version 24.0 (IBM Corp., Armonk, NY, USA), and a p value <0.050 was considered statistically significant.
RESULTS
Clinical characteristics are summarized in Table 1. The 194 patients who were reported to have trapped thrombus in a PFO were comprised of 100 men (51.5%) and 94 women. Eighty-four patients (43.3%) were reported from 1991–2005, while 110 patients (56.7%) were reported from 2006–2015. The mean age of the overall population was 59.3±16.4 years; age was significantly higher in the patient group treated with anticoagulation than in the other treatment groups. A total of 112 patients (57.7%) were treated with surgery, 28 patients (14.4%) with thrombolysis, and 54 patients (27.8%) with anticoagulation. The most common cause of pulmonary embolism was unprovoked origin. Forty patients presented with cardiogenic shock or arrest, and thrombolysis treatment was chosen more often for these patients (p<0.001).
Table 1. Baseline characteristics of patients with trapped thrombus in PFO.
| Characteristics | Overall population (n=194) | Treatment option | ||||
|---|---|---|---|---|---|---|
| Surgery (n=112, 57.7%) | Thrombolysis (n=28, 14.4%) | Anticoagulation (n=54, 27.8%) | p value | |||
| Age | 59.3±16.4 | 56.5±15.7 | 57.8±16.0 | 66.1±16.4 | 0.002* | |
| Men | 100 (51.5) | 57 (50.9) | 12 (42.9) | 31 (57.4) | 0.447 | |
| Cause of pulmonary embolism | - | - | - | - | 0.848 | |
| Unprovoked | 129 (66.5) | 73 (65.2) | 20 (71.4) | 36 (66.7) | - | |
| Provoked | 51 (26.3) | 29 (25.9) | 7 (25.0) | 15 (27.8) | - | |
| Cancer related | 14 (7.2) | 10 (8.9) | 1 (3.6) | 3 (5.6) | - | |
| Initial shock or arrest | 40 (20.6) | 18 (16.1) | 14 (50.0) | 8 (14.8) | <0.001† | |
| Pre-treatment embolism | 73 (37.6) | 36 (32.2) | 10 (35.7) | 27 (50.0) | 0.134 | |
| Stroke (including TIA) | 48 (24.7) | 19 (17.0) | 6 (21.4) | 23 (42.6) | - | |
| Non-stroke embolism | 25 (12.9) | 17 (15.2) | 4 (14.3) | 4 (7.4) | - | |
| IVC filter | 39 (20.1) | 32 (28.6) | 3 (10.7) | 4 (7.4) | 0.003‡ | |
| Publication year | - | - | - | - | 0.483 | |
| ≤2005 | 84 (43.3) | 50 (44.6) | 14 (50.0) | 20 (37.0) | - | |
| >2005 | 110 (56.7) | 62 (55.4) | 14 (50.0) | 34 (63.0) | - | |
Values are presented as mean±standard deviation or number (%).
IVC = inferior vena cava; PFO = patent foramen ovale; TIA = transient ischemic attack.
*Post-hoc analysis: surgery vs. anticoagulation, p<0.010; †Post-hoc analysis: thrombolysis vs. surgery, p<0.010; thrombolysis vs. anticoagulation, p<0.010; ‡Post-hoc analysis: surgery vs. anticoagulation, p<0.010.
Transthoracic echocardiography was performed in 166 of the patients, of whom 145 (diagnostic accuracy rate, 87.3%) were suspected to have trapped thrombus in a PFO. One-hundred seventy-six patients underwent transesophageal echocardiography and all of these patients were diagnosed as having trapped thrombus in a PFO (diagnostic accuracy rate, 100%). Follow-up echocardiography was performed in 12 (42.9%) of the 28 patients treated with thrombolysis and in 34 (63.0%) of the 54 patients treated with anticoagulation (Table 2). The mean follow-up time was 3.0±2.7 days in the thrombolysis group and 12.9±9.6 days in the anticoagulation group. The overall rate of complete resolution of thrombus was 67% in both groups.
Table 2. Diagnostic accuracy of echocardiography for trapped thrombus in PFO and follow-up echocardiography result.
| Initial diagnostic tool | Performed in patients (n=194) | Diagnostic accuracy | |
|---|---|---|---|
| Transthoracic echocardiography | 166 (85.5%) | 145 (87.3%) | |
| Transesophageal echocardiography | 176 (90.7%) | 176 (100%) | |
| Follow-up echocardiography | Thrombolysis (n=28) | Anticoagulation (n=54) | |
| Follow-up performed patients | 12 (42.9%) | 34 (63.0%) | |
| Time to mean follow-up, day | 3.0±2.7 | 12.9±9.6 | |
| Complete resolution of thrombus | 8 (66.7%) | 23 (67.6%) | |
The most common presenting symptom was dyspnea, followed by chest pain, lower extremity edema, and syncope (Table 3). Clinical signs of paradoxical embolism, such as stroke or peripheral arterial occlusion, were present in 49 patients, and 6 patients presented with cardiac arrest. The most common cause of pulmonary embolism was idiopathic first or recurring event (117 patients), followed by post-operative, prolonged hospitalization due to acute or chronic illness, and cancer-related causes. Seventy-three patients had a previous paradoxical embolic event prior to the diagnosis of trapped thrombus in a PFO, and the most frequent site of paradoxical embolism was the brain (stroke, including transient ischemic attacks: 48 patients), followed by a peripheral artery (15 patients), a visceral organ (7 patients), and a coronary artery (6 patients) (Tables 1 and 3). A trend towards more frequent use of anticoagulation therapy was observed in patients who had a stroke event.
Table 3. Presenting symptoms or signs, cause of pulmonary embolism, and sites of pre-embolization in patients with trapped thrombus in PFO.
| Symptom or sign | No. (%) of patients (n=194) | |
|---|---|---|
| Dyspnea | 154 (79.4%) | |
| Chest pain | 64 (33.0%) | |
| Lower extremity edema | 28 (14.4%) | |
| Syncope | 34 (17.5%) | |
| Focal neurological deficit | 32 (16.5%) | |
| Peripheral arterial occlusion | 17 (8.8%) | |
| Cardiac arrest | 6 (3.1%) | |
| Cause of pulmonary embolism | No. (%) of patients (n=194) | |
| Unprovoked | ||
| Unknown first embolism | 109 (56.2%) | |
| Recurred thromboembolism | 8 (4.1%) | |
| Antiphospholipid syndrome | 4 (2.1%) | |
| Inherited thrombophilia | 8 (4.1%) | |
| Provoked | ||
| Prolonged hospitalization | 19 (9.8%) | |
| Post-operative | 22 (11.3%) | |
| Major trauma | 3 (1.5%) | |
| Venous external compression | 4 (2.1%) | |
| Pregnancy | 2 (1.0%) | |
| Economy class syndrome | 1 (0.5%) | |
| Cancer related | 14 (7.2%) | |
| Site of embolism | No. (%) of patients (n=194) | |
| Brain (Stroke or TIA) | 48 (24.7%) | |
| Peripheral artery | 15 (7.7%) | |
| Visceral organ | 7 (3.6%) | |
| Coronary artery | 6 (3.1%) | |
PFO = patent foramen ovale; TIA = transient ischemic attack.
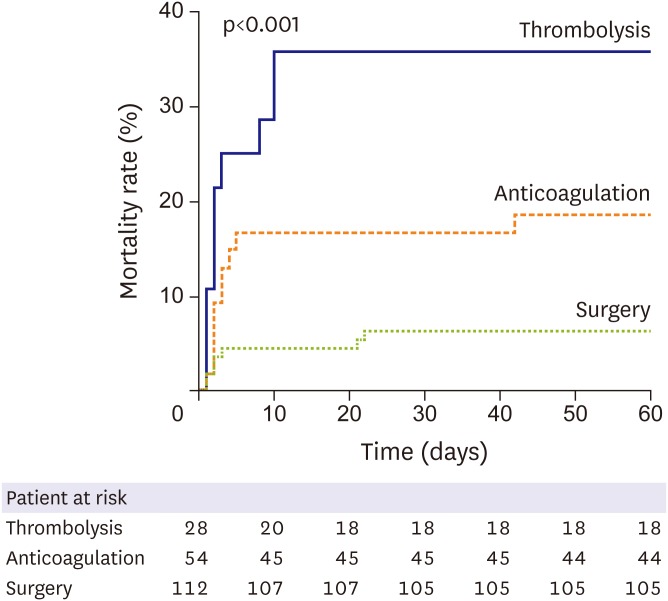
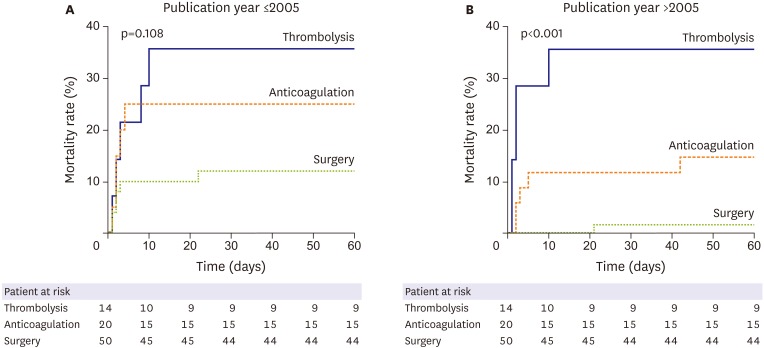
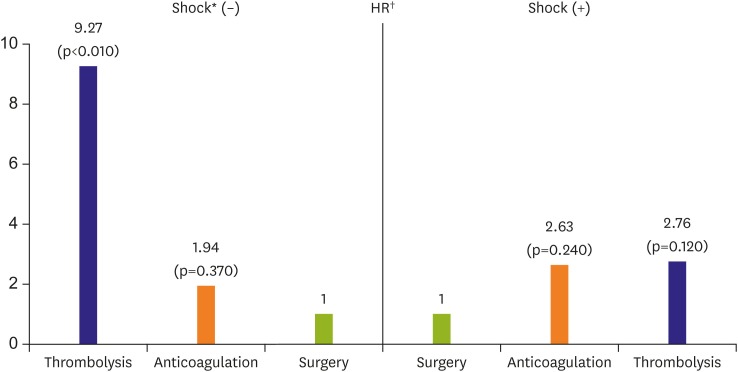
Many of the treating physicians chose surgery as a treatment option because of concern about fragmented emboli during antithrombotic treatment. Twenty-eight patients (14.4%) were treated with thrombolysis, and 54 (27.8%) were treated with anticoagulation only because of important comorbidities or patient refusal to undergo an invasive strategy. Although the incidence of post-treatment embolism was low, surgical treatment was associated with fewer embolic events than was thrombolysis or anticoagulation (p=0.044) (Table 4). The overall mortality of patients with trapped thrombus in a PFO was 13.9%. The most common cause of death was refractory cardiogenic shock, followed by stroke and treatment related complications. The Kaplan-Meier curve showed that among all patients, thrombolysis was associated with a significantly higher 60-day cumulative mortality compared with other treatment options (log-rank p<0.001) (Figure 2). No significant difference in mortality rates was found among patients in reports published in 2005, or earlier, but according to reports published after 2005, thrombolysis was significantly related with a higher mortality rate than other treatment option (Figure 3). The multivariate Cox regression analysis demonstrated that initial shock or cardiac arrest (hazard ratio [HR], 4.90; confidence interval [CI], 1.99–12.01; p=0.001) and thrombolysis (HR, 3.40; CI, 1.21–9.61; p=0.021) were independent predictors of 60-day mortality in all patients (Table 5). In addition, no significant difference according to treatment options was found among patients in reports published in 2005, or earlier. However, thrombolysis was more significantly associated with 60-day mortality than other treatment options among patients in reports published after 2005 (HR, 22.99; CI, 2.26–233.93; p=0.008). When patients were stratified into 2 groups according to the presence of initial shock or cardiac arrest, thrombolysis was associated with significantly higher 60-day mortality than other treatment options in patients without initial shock or cardiac arrest. However, in patients with initial shock or cardiac arrest, there were no significant differences in outcome among the various treatment options (Figure 4).
Table 4. Treatment result according to treatment options.
| Characteristics | Overall population (n=194) | Treatment option | ||||
|---|---|---|---|---|---|---|
| Surgery (n=112, 57.7%) | Thrombolysis (n=28, 14.4%) | Anticoagulation (n=54, 27.8%) | p value | |||
| Post-treatment embolism | 16 (8.3) | 5 (4.5) | 4 (14.3) | 7 (13.0) | 0.044 | |
| Stroke (including TIA) | 11 (5.7) | 4 (3.6) | 2 (7.1) | 5 (9.3) | - | |
| Non-stroke embolism | 5 (2.6) | 1 (0.9) | 2 (7.1) | 2 (3.7) | - | |
| Total deaths | 27 (13.9) | 7 (6.3) | 10 (35.7) | 10 (18.5) | <0.001 | |
| Cardiogenic shock | 18 (9.3) | 4 (3.6) | 7 (25.0) | 7 (13.0) | - | |
| Stroke | 5 (2.6) | 1 (0.9) | 2 (7.1) | 2 (3.7) | - | |
| Bleeding | 2 (1.0) | - | 1 (3.6) | 1 (1.9) | - | |
| Post-surgery ARDS | 2 (1.0) | 2 (1.8) | - | - | - | |
Values are presented as number (%).
ARDS = acute respiratory distress syndrome; TIA = transient ischemic attack.
Figure 2.
Mortality rate according to treatment options published from 1991 through 2015.
Figure 3.
Treatment-related mortality rate according to publication year (A) from 1991 to 2005, and (B) from 2006 to 2015.
Table 5. Multivariable Cox regression analysis for 60-day mortality.
| Variables | HR | CI | p value | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Aged ≥60 years | 2.04 | 0.84 | 4.97 | 0.117 | |
| Men | 0.58 | 0.25 | 1.37 | 0.220 | |
| Initial shock or arrest | 4.90 | 1.99 | 12.01 | 0.001 | |
| Pre-embolization | 1.45 | 0.66 | 3.21 | 0.360 | |
| Cause of pulmonary embolism | - | - | - | - | |
| Unprovoked | 1.00 | - | - | - | |
| Provoked | 1.13 | 0.49 | 2.62 | 0.770 | |
| Cancer related | 1.32 | 0.59 | 2.93 | 0.490 | |
| IVC filter | 0.39 | 0.09 | 1.71 | 0.210 | |
| Treatment option (overall) | - | - | - | - | |
| Surgery | 1.00 | - | - | - | |
| Thrombolysis | 3.40 | 1.21 | 9.61 | 0.021 | |
| Anticoagulation | 1.99 | 0.70 | 5.69 | 0.190 | |
| Treatment option (publication year ≤2005)* | |||||
| Surgery | 1.00 | - | - | - | |
| Thrombolysis | 1.39 | 0.38 | 5.04 | 0.618 | |
| Anticoagulation | 1.03 | 0.28 | 3.78 | 0.960 | |
| Treatment option in overall (publication year >2005)* | |||||
| Surgery | 1.00 | - | - | - | |
| Thrombolysis | 22.99 | 2.26 | 233.93 | 0.008 | |
| Anticoagulation | 5.60 | 0.59 | 53.27 | 0.134 | |
CI = confidence interval; HR = hazard ratio; IVC = inferior vena cava.
*Result of the multivariate analysis after adjustment for age, sex, pre-embolization, cause of pulmonary embolism, and IVC filter replacement.
Figure 4.
Mortality rate according to treatment options, with or without cardiogenic shock.
HR = hazard ratio; IVC = inferior vena cava.
*Shock means initially presented with cardiogenic shock or cardiac arrest, †Result of the multivariate analysis after adjustment for age, sex, pre-embolization, cause of pulmonary embolism, and IVC filter replacement.
DISCUSSION
We report, along with one new case, the largest systematic case review of trapped thrombus in a PFO published since 1991. The systematic review showed that surgical treatment was associated with fewer post-treatment embolic events and had a lower 60-day mortality compared with thrombolysis or anticoagulation therapy.
A few systematic review papers concerning the treatment of trapped thrombus in a PFO have been published previously; however, the results were inconsistent and they did not demonstrate statistical significance.4),5),6) The latest review by Myers et al.6) reported that surgical treatment showed a non-significant trend toward improving survival. Further, thrombolysis had a non-significant opposite effect when compared with anticoagulation therapy for the treatment of trapped thrombus in a PFO. No randomized trial has been conducted to compare treatment options in these patients, as such a trial is difficult to perform. As far as we know, the present report includes the largest sample of cases published to date. We included reports that were published since 1991 on trapped thrombus in a PFO. In the past, pulmonary embolectomy was the last treatment option for unstable patients with massive pulmonary embolism because of its high mortality rate.7) However, surgical outcomes have significantly improved because of advances in diagnostic and surgical techniques.8) For this reason, we did not include cases published during or prior to the 1990s. In this study, a subgroup analysis was also performed according to publication year (reports published in 2005 or earlier and those published after 2005). The result showed no significant difference among patients in reports published in 2005 or earlier, but surgery was superior among patients in reports published after 2005. This result may also be related to the advancement of surgical technique or improvements in post-operative management processing.
This review demonstrates that surgical treatment, compared with anticoagulation or thrombolysis, is associated with significantly lower 60-day mortality. Many of the physicians chose surgery as the first treatment option because of concerns about fragmented embolization during antithrombotic treatment. A post-treatment embolic event occurred in 8.3% of the overall patient population, and surgery was related with a lower event rate compared with other treatment options. The most common cause of death was cardiogenic shock related with massive pulmonary embolism. Thrombolysis has been recommended as a treatment choice for massive pulmonary embolism in the absence of any contraindication.9) In this review, thrombolysis was more often chosen as the first-line therapy for patients with initial hemodynamic instability. Thrombolysis can be administered quickly and simultaneously treats trapped thrombus in a PFO and pulmonary embolism, as well as other types of systemic embolization. However, this review showed that thrombolysis was related with greater mortality and a higher rate of post-treatment embolic events than were other treatment options. Thrombolysis was significantly associated with higher mortality in patients without initial shock or cardiac arrest, but there was only a non-significant trend toward greater mortality in patients with initial shock or cardiac arrest. This result suggests that surgery is the most appropriate treatment choice for a hemodynamically stable patient with trapped thrombus in a PFO, while thrombolysis should be considered for patients with hemodynamic instability who cannot tolerate surgery.
Echocardiography plays an essential role in the diagnosis of trapped thrombus in a PFO. It is usually not routinely performed, except for risk stratification of pulmonary embolism or presumptive diagnosis in hemodynamically unstable patients with suspected pulmonary embolism.10) It is notable that 60% of patients in this review presented, not with a paradoxical embolic event, but with dyspnea or chest pain. This finding lends additional support to the routine performance of echocardiographies in patients with pulmonary embolism. In this review, in 12.7% of patients, the diagnosis was not made by transthoracic echocardiography. Transesophageal echocardiography was superior to transthoracic echocardiography for direct visualization of the thrombus and should be considered in patients who develop pulmonary embolism with a paradoxical embolic event. Surprisingly, follow-up echocardiography showed that 33.3% of the patients treated with thrombolysis had not achieved full resolution after a mean of 3.0±2.7 days of follow-up. This incomplete resolution of thrombus may be linked to the higher mortality and embolic event rate in patients treated with thrombolysis.
Although trapped thrombus in a PFO is an extremely rare finding, right heart thrombus is occasionally found in patients with pulmonary embolism. Echocardiography studies found right ventricular thrombus in 3%–23% of patients with pulmonary embolism.11),12),13) Rose et al.14) reported that thrombolysis is associated with a better survival rate when compared to either anticoagulation or surgery. The paradoxical embolic events in patients with a PFO may be associated with this different result. In choosing the best treatment, it is essential to determine whether patients with right heart thrombus have a trapped thrombus in a PFO.
This systematic review had important limitations, and the results need to be interpreted with caution. Most of the clinical data are based on individual published cases and multivariate analysis could not adjust for the heterogeneity among patients. In particular, among patients treated with anticoagulation, not only those who refused an invasive strategy, but also those who could not tolerate such a strategy because of a severe comorbidity were included. Furthermore, the individual patients had different thromboembolic risk factors, which could affect the mortality rate. However, because of the lack of sufficient information, patients were categorized into provoked, unprovoked, and cancer related groups only. In addition, only 124 of 194 cases reported the size of the thrombus, and a large discrepancy was found between the size measured using ultrasonography and the actual size of the surgical specimens. Accordingly, the size of the thrombus, which could be an important prognostic factor, was not adjusted among the patients of the treatment group. Lastly, there may be unpublished cases with favorable or unfavorable outcomes. Despite these potential limitations, this systematic review examined the clinical results associated with trapped thrombus in a PFO in the largest sample of patients thus far reported in the literature.
In conclusion, trapped thrombus in a PFO is a rare complication of pulmonary embolism, but it may lead to tragic clinical events. This systematic review showed that surgical treatment of patients with trapped thrombus in a PFO is associated with a lower rate of post-treatment embolic events and lower overall 60-day mortality in patients with trapped thrombus in PFO. In particular, compared to surgery, thrombolysis was related with higher 60-day mortality in patients who presented without initial shock or cardiac arrest. Although this systematic review had several methodological limitations, results from this study may help in determining the best treatment option for patients with trapped thrombus in a PFO.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
Supplementary Material
References
- 1.Kent DM, Ruthazer R, Weimar C, et al. An index to identify stroke-related vs incidental patent foramen ovale in cryptogenic stroke. Neurology. 2013;81:619–625. doi: 10.1212/WNL.0b013e3182a08d59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hagen PT, Scholz DG, Edwards WD. Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc. 1984;59:17–20. doi: 10.1016/s0025-6196(12)60336-x. [DOI] [PubMed] [Google Scholar]
- 3.Konstantinides S, Geibel A, Kasper W, Olschewski M, Blümel L, Just H. Patent foramen ovale is an important predictor of adverse outcome in patients with major pulmonary embolism. Circulation. 1998;97:1946–1951. doi: 10.1161/01.cir.97.19.1946. [DOI] [PubMed] [Google Scholar]
- 4.Meacham RR, 3rd, Headley AS, Bronze MS, Lewis JB, Rester MM. Impending paradoxical embolism. Arch Intern Med. 1998;158:438–448. doi: 10.1001/archinte.158.5.438. [DOI] [PubMed] [Google Scholar]
- 5.Fauveau E, Cohen A, Bonnet N, Gacem K, Lardoux H. Surgical or medical treatment for thrombus straddling the patent foramen ovale: impending paradoxical embolism? Report of four clinical cases and literature review. Arch Cardiovasc Dis. 2008;101:637–644. doi: 10.1016/j.acvd.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 6.Myers PO, Bounameaux H, Panos A, Lerch R, Kalangos A. Impending paradoxical embolism: systematic review of prognostic factors and treatment. Chest. 2010;137:164–170. doi: 10.1378/chest.09-0961. [DOI] [PubMed] [Google Scholar]
- 7.Mattox KL, Feldtman RW, Beall AC, Jr, DeBakey ME. Pulmonary embolectomy for acute massive pulmonary embolism. Ann Surg. 1982;195:726–731. doi: 10.1097/00000658-198206000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yalamanchili K, Fleisher AG, Lehrman SG, et al. Open pulmonary embolectomy for treatment of major pulmonary embolism. Ann Thorac Surg. 2004;77:819–823. doi: 10.1016/j.athoracsur.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 9.Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141:e419S–e496S. doi: 10.1378/chest.11-2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Giannitsis E, Katus HA. Risk stratification in pulmonary embolism based on biomarkers and echocardiography. Circulation. 2005;112:1520–1521. doi: 10.1161/CIRCULATIONAHA.105.566182. [DOI] [PubMed] [Google Scholar]
- 11.Torbicki A, Galié N, Covezzoli A, et al. Right heart thrombi in pulmonary embolism: results from the International Cooperative Pulmonary Embolism Registry. J Am Coll Cardiol. 2003;41:2245–2251. doi: 10.1016/s0735-1097(03)00479-0. [DOI] [PubMed] [Google Scholar]
- 12.Casazza F, Bongarzoni A, Centonze F, Morpurgo M. Prevalence and prognostic significance of right-sided cardiac mobile thrombi in acute massive pulmonary embolism. Am J Cardiol. 1997;79:1433–1435. doi: 10.1016/s0002-9149(97)00162-8. [DOI] [PubMed] [Google Scholar]
- 13.Chartier L, Béra J, Delomez M, et al. Free-floating thrombi in the right heart: diagnosis, management, and prognostic indexes in 38 consecutive patients. Circulation. 1999;99:2779–2783. doi: 10.1161/01.cir.99.21.2779. [DOI] [PubMed] [Google Scholar]
- 14.Rose PS, Punjabi NM, Pearse DB. Treatment of right heart thromboemboli. Chest. 2002;121:806–814. doi: 10.1378/chest.121.3.806. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.