Graphical abstract
Abbreviation: RH, rural hospital; BPHC, Block Level Primary Health Centre; CMOH, Chief Medical Officer of Health; PHC, Primary Health Centre; ASV, antisnake venom; BMC, Burdwan Medical College; AchEIs, acetylcholinesterase inhibitors
Keywords: Snakebite, hospital -based data, Paschim Medinipur
Highlights
-
•
The present study highlights the medical problem of snakebite in Paschim Medinipur district, West Bengal.
-
•
The case fatality rate of snakebite from 10 block level hospitals have been reported in the study.
-
•
The symptoms and management of snakebite has been discussed.
Abstract
Objective
Snakebite is a serious medical problem in Paschim Medinipur district, West Bengal, India. In the present study, hospital based data on snakebite cases and deaths were collected from 10 blocks of the district to obtain a picture of this neglected public health issue.
Methods
Retrospective data of snakebite and deaths from 2012 to 2016 was collected from the 5 Rural hospitals (RH) and 5 Block level Primary Health Centres(BPHC) of the ten blocks of Paschim Medinipur district in a prescribed format addressing issues including the demographic factors regarding the victims, seasonal pattern, history of snakebite in previous 5 years, outcome of the bite, any reporting of death.
Results
A total number of 1633 snakebites were reported in the study during the period of 2012–2016. The hospital data from the ten blocks reported 17 deaths due to snakebite in the given period. It was found that about 34% of the snake bites occurred from June to September. The age-wise distribution of snakebite cases show that majority of snakebite affected cases were within the age of 21–45 years. Males(62%) suffered more than the females(38%). The case fatality rate reported from the hospital based data was 1.04%. 60% of the snakebites occurred during morning to noon hours. The clinical manifestation of snakebite included regional edema in the affected limb, hypotension, malaise, vomiting, abdominal pain and diarrhea. The bite to hospital time was found to be 120 ± 6.5 mins(n = 750 cases) and bite to ASV injection time was found to be 270 ± 3.5 mins(n = 750 cases).
Conclusion
Snakebite is a neglected health issue in Paschim Medinipur district. Lack of snakebite data is due to under reporting. In the present study we have attempted to investigate the official data available on snakebite from 10 blocks of Paschim Medinipur district which has been identified for high snakebite incidence.
1. Introduction
Snake bite was included in the list of neglected tropical diseases by World Health Organization in the year 2009 [1], [2]. Globally every year, an estimated more than 5 million people are bitten by snakes, [3], [4] resulting in approximately 20,000–1, 25,000 deaths [5]. West Bengal is one of the high snake bite prevalence states of India besides Andhra Pradesh, Kerala, Tamil Nadu and Maharashtra [6], [7], [8]. Rural West Bengal in India showed an average annual mortality rate of 16 per 100,000 population [6].
Accurate data are often difficult to find as bites affect rural populations in remote areas with limited access to formal health care [9]. There are very few community-based surveys on mortality related to snakebite, and these have shown high rates. Many estimates of snakebite incidence and mortality are based on hospital data, because other recording systems are unavailable or unreliable in most developing countries. However, hospital data may considerably underestimate the problem. In Africa, it is estimated that less than half the deaths due to snakebite are reported by the health services, and similar under-reporting is likely to occur in most African and Asian countries where snakebite is prevalent [10]. In remote rural areas of the tropics it is estimated that a third to more than half of snakebite victims do not receive treatment at a hospital. Thus, a proportion of snakebite deaths can occur before the victims can reach a hospital, and in some instances victims with fatal bites may not attempt to use formal health care services [11].
2. Methods & materials
To investigate the snakebite scenario of Paschim Medinipur district, West Bengal we have randomly selected 10 blocks (out of 29 blocks) for this study. The blocks are- Pingla, Chandrakona I, Chandrakona II, Debra, Kharagpur I, Kharagpur II, Salboni, Keshiary, Garbetta I and Garbetta III. This study was financially supported by Department of Science and Technology, West Bengal, India. There are 30 Primary Health Centres(PHC), 5 Block Primary Health Centres(BPHC) and 5 Rural hospitals(RH) in these ten blocks (Table 3). Prior permission was obtained from Chief Medical Officer of Health (CMOH) of Paschim Medinipur for this study. The snakebite data over past five years were collected from the BPHCs and PHCs. The information regarding seasonal pattern of snakebites, number of patients admitted and the number of deaths due to snakebite from 2012 to 2016 were collected from the databases of health centres of the ten blocks. The demographic information about the population, male: female ratio, percentage of rural and urban population of the study area was collected from District Magistrate’s office of Paschim Medinipur district.
Table 3.
List of BPHC, PHC and RH in 10 blocks of Paschim Medinipur district West Bengal.
| Block | Name of BPHC & RH | Name of PHC |
|---|---|---|
| Garhbeta I | Garhbeta RH |
|
| ||
| ||
| Garhbeta III | Dwarigeria BPHC |
|
| ||
| Chandrakona I | Khirpai BPHC |
|
| ||
| ||
| ||
| ||
| Chandrakona II | Chandrakona RH |
|
| ||
| Salboni | Salboni RH |
|
| ||
| ||
| Kharagpur I | Hijli RH |
|
| ||
| ||
| Kharagpur II | Changual BPHC |
|
| ||
| Debra | Debra RH |
|
| ||
| ||
| ||
| Keshiary | Keshiary BPHC |
|
| ||
| ||
| Pingla | Pingla BPHC |
|
| ||
|
The information collected from the Chief Medical Officer of Paschim Medinipur district included- names of the government health facilities (BPHC or Rural Hospitals) in the blocks, number of snake bite cases who had attended the government hospitals in the blocks under study, number of snake bite deaths reported from the study area.
Evidence of bite by a poisonous snake included: (i) fang marks, (ii) swelling, ecchymosis, blister formation and/or bleeding from local site, (iii) disturbances in coagulation mechanism with or without systemic bleeding, and (iv) identification of snake wherever possible (Table 1). Swelling confined only to the bite site was graded as mild; extension to more than half of the limb as moderate; and extensive swelling with tissue necrosis was graded severe [12], [13]. Neurotoxicity was defined as documented ptosis, external ophthalmoplegia, weakness of neck or bulbar muscles, use of neostigmine or ventilatory support (endotracheal intubation or a mechanical ventilator). The clinical gradation of snakebites and envenomations is crucial for evaluating and managing the condition of each victim [14]. According to the patient condition at the time of admission, it was classified as follows [15] (Table 2):
Table 1.
Types of Envenomations.
| Type of bite | No of cases reported (n = 950)(%) |
|---|---|
| Vipera russelli (Chandrabora) | 570(60%) |
| Common Krait | 238(25%) |
| Naja Kaouthia (Keute) | 143(15%) |
n- Number of cases where the type of snake was identified.
Table 2.
Clinical grades of envenomation.
| Grades of Envenomation | Number of cases(n = 820cases)(%) |
|---|---|
| Grade 0 | 51(6.2%) |
| Grade 1 | 250(30.5%) |
| Grade 2 | 335(40.8%) |
| Grade 3 | 159(19.4%) |
| Grade 4 | 25(3%) |
Grade 0: bite without envenomation (absence of edema or local reaction).
Grade 1: minor envenomation (local edema, absence of general signs).
Grade 2: moderate envenomation (regional edema in the affected limb and/or moderate general symptoms: moderate hypotension, malaise, vomiting, abdominal pain and diarrhea).
Grade 3: severe envenomation (extensive edema reaching the torso and/or severe general symptoms: prolonged hypotension, shock, anaphylactoid reaction and visceral trouble).
Grade 4: extremely severe envenomation (apparent systemic involvement with blood-tinged secretions, renal failure, coma and death).
Analysis was carried out using Excel® (Microsoft, USA). The case fatality rate of the hospital data were calculated by the following formulas-
Case fatality risk, case fatality ratio or just fatality rate — is the proportion of deaths within a designated population of “cases” (people with a medical condition), over the course of the disease.
| fatality rate = Notified deaths × 100/Notified cases = ɑ deaths/100 cases |
3. Results
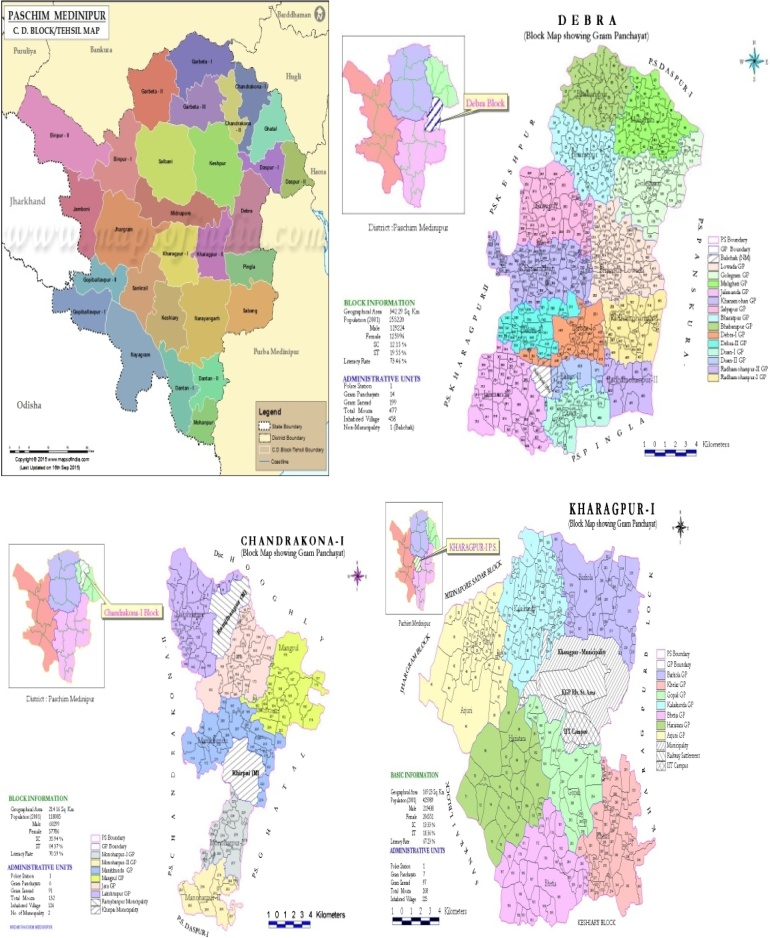
The study was conducted on a population of 2145572(32.5% of total population) from 10 blocks of Paschim Medinipur district(Fig. 1). The total population of the district is 6598469. The male to female ratio of these blocks is 1.03. From the survey the total number of snakebite cases reported from the block level health centres and rural hospitals were 1633. Of the total number of snakebite cases 1006(62%) were male and 627(38%) were female. A total of 17 deaths were reported from 5 years hospital based retrospective data of 10 blocks between 2012 and 2016 (Table 4). The case fatality rate reported from the hospital based data was 1.04%. Maximum(34%) snakebite cases were reported in June to September months. Most of the snakebites occurred in the rural areas during agricultural activities. The agewise distribution of snakebite cases show that majority of snakebite affected cases were within the age of 21–45 years. However due to lack of proper documentation in 850 cases the age was not mentioned in the report (Table 5). The bite to hospital time was found to be 120± 6.5 mins(n = 750 cases) and bite to ASV injection time was found to be 270 ± 3.5 mins(n = 750 cases). In 60% (n = 950 cases) the snakebite occurred between the early morning hours and 4pm.
Fig. 1.
Map of the study area covering blocks of Debra, Chandrakona- I, Kharagpur I.
Table 4.
Blockwise incidence rate of snakebite of Paschim Medinipur district (from official data of 2012–2016).
| Names of the blocks | Population in the block | Reported hospital attendance |
Reported hospital deaths (5yrs) |
Case fatality rate(of 5yrs) |
|
|---|---|---|---|---|---|
| Male | Female | ||||
| Garhbeta I | 256589 | 312 | 207 | 06 | 1.16 |
| Garhbetta III | 190743 | 117 | 64 | – | NA |
| Chandrakona I | 151083 | 30 | 20 | – | NA |
| Chandrakona II | 138500 | 152 | 100 | 09 | 3.5714 |
| Salboni | 211723 | 106 | 53 | – | NA |
| Kharagpur I | 286717 | 4 | 1 | – | NA |
| Kharagpur II | 205967 | 3 | 0 | – | NA |
| Debra | 320478 | 236 | 151 | 02 | 0.5167 |
| Keshiary | 166244 | 30 | 27 | – | NA |
| Pingla | 217528 | 15 | 4 | – | NA |
| Total | 1005 | 627 | 17 | ||
NA: Not applicable.
Table 5.
Agewise distribution of snake bite cases.
| Age-wise distribution (Years) | Male | Female | Total |
|---|---|---|---|
| 0–10 | 43 | 16 | 59 |
| 11–20 | 80 | 51 | 131 |
| 21–30 | 97 | 70 | 167 |
| 31–40 | 93 | 67 | 160 |
| 41–50 | 97 | 50 | 147 |
| 51–60 | 77 | 20 | 97 |
| 61–70 | 21 | 05 | 26 |
| 70+ | 08 | 02 | 10 |
| Age not provided | 512 | 338 | 850 |
3.1. Signs & symptoms of envenomation
Local pain at the site of bite was reported by 100% of cases admitted to the block level hospitals. Edema and coagulopathies were reported by 335(40%) along with moderate hypotension, malaise, vomiting, abdominal pain and diarrhea. Severe envenomations was characterized by prolonged hypotension, shock, anaphylactoid reaction and even death.
3.2. Treatment & follow-up
All patients received tetanus toxoid and antisnake venom (ASV).The patients were treated with polyvalent antisnake venom and most of them received single doses (10vials) and in severe envenomations single doses(10 vials) were repeated upto three hours. However about 20% of the cases developed anaphylactic and pyrogenic reactions. The pyrogenic response was treated with paracetamol and the anaphylactic response was managed by adrenaline(i.m), hydrocortisone(i.v) and ranitidine(i.v). The mean bleeding time was 10.55 ± 3.2 min(n = 862 cases). The mean clotting time was found to be 16.1 ± 2.55 min(n = 862 cases). Neostigmine was provided to 80(35%) of the patients who developed signs of neuroparalysis. The mean duration of stay of all patients at the hospital was 8.5 ± 2.2 days(n = 950 cases). Ventilatory support was provided to 30 patients.
4. Discussion
West Bengal is one of the high snake bite prevalence states of India besides Andhra Pradesh, Kerala, Tamil Nadu and Maharashtra8. Government of India official data showed only 1331 snake bite deaths in the year 2007. If compared with another highly attended public health problem, malaria, we see officially reported numbers of snake bite deaths are much higher than malaria death in West Bengal (340 and 96 in 2007 respectively) [16]. Epidemiological surveys on snake bite in India are primarily based on hospital records [6]. There is no snake bite data of Paschim Medinipur district for last 15 years that is based on demographic surveys and retrospective health centre surveys.
Paschim Medinipur is one of the eleven districts of West Bengal. Geographically located in 21°36′ to 22°57′North latitude to 86°33′ to 88°11′ East longitude, it covers an area of 9345 square kilometres. North and North west of this district is a part of Chotanagpur plateau. The area has a gentle slope from east to west. The sandy loam or loamy soil of reddish or reddish brown colour is a characteristics of this region. The maximum temperature recorded in April is 45°–46 °C and minimum temperature in winter is 6 °C. The average annual rainfall is about 1500 mm. Paschim Medinipur is diverse in geography, climate, flora and faunal resources. The tribal communities residing in this region are the Santhals, Mundas, Lodhas, Bhumijs, Oraon and Kherias.
Early initiation of treatment by anti-snake venom (ASV) serum is the key of low case fatality rate [17]. In the present study, the bite to hospital time was found to be 120 ± 6.5 mins(n = 750 cases) and bite to ASV injection time was found to be 270 ± 3.5 mins(n = 750 cases).In the present study the patients were treated with polyvalent antisnake venom and most of them received single doses (10vials) and in severe envenomations single doses(10 vials) were repeated upto three hours. A similar study, accomplished in northern Bangladesh, registered seven deaths (26%) among victims treated with anti-snake venom doses ranging from 20 ml to 40 ml [18]. A prospective study of hospital practice in the Gampaha district, Sri Lanka, documented only 0.43% mortality when at least ten vials (100 ml) of antivenom were initially given to victims [19]. These findings agree with Theakston et al., [20], who concluded that is prudent to give initial doses greater than 100 ml to patients with neurotoxic signs, as well as is necessary to repeat this dose every few hours, up to a total of at least 300 ml, if there is no response.
In this study the case fatality rate from the official hospital data was found to be 1.04%. Case fatality rate of a tertiary referral hospital of Pondicherry, JIPMER was 13.5% [21]. Hospital records of the Burdwan Medical College (BMC) of West Bengal for the year 2009 shows, out of 1424 venomous snake bite cases treated there, 74 died (case fatality rate 5.19%) [6]. From Table 4, it is evident from the present study that the maximum number of snakebites were reported from Garbetta I, Chandrakona II and Debra. From the other blocks there has been no reported cases of snakebite deaths from hospital data.
Snake bite and death rate is always high in the rainy season [22]. In the present study the maximum(34%) number of snakebite was reported in the months of June-September. Earlier in several studies the incidence of snake bite was found in the months of June-September [23]. The agewise distribution of snakebite cases show that majority of snakebite affected cases were within the age of 21–45 years. Previous reports show maximum number of snakebite in the age group of 15–45 years [6]. However due to under reporting in majority of the cases the age of the cases were not mentioned. In the present study about 20% patients developed pyrogenic responses and anaphylactic response after antiserum administration and were treated with adrenaline. This finding is consistent with a double-blind placebo-controlled trial, conducted in Polonnaruwa, Sri Lanka, the same ASV was utilized and it was established that premedication with adrenaline significantly reduces the risk of acute adverse reactions to antivenom sera [24]. Earlier Theakston et al., [20] also found in 33% cases of anaphylactic responses 50 min after the initial ASV dose which is also corroborated in this study. There are several reports showing benefit of acetylcholinesterase inhibitors(AchEIs) in envenoming by kraits [25]. PLA2 s from snake venom neurotoxins produce complex effects on the pre-synaptic nerve terminal. These include entry into nerve terminals after binding to specific receptors on the pre-synaptic membrane, morphological changes such as nerve terminal bulging, changes in mitochondrial morphology and permeability, increase in cytosolic calcium levels, changes in expression and interactions of SNARE proteins, increased vesicle fusion and neurotransmitter release, and impaired vesicle recycling. Montecucco and colleagues have shown that the effects produced by four different snake venom PLA2 s (beta-bungarotoxin, taipoxin, notexin, and textilotoxin) were similar, suggesting a similar mechanism of action for pre-synaptic neurotoxins. Hydrolysis of the phospholipids of the pre-synaptic membrane and membrane destabilization by the products of hydrolysis are likely to be key drivers in this process [26], [27], [28]. The envenoming snake species is highly likely to influence the clinical presentation and outcome, but many studies have considered together bites from different snake species [29]. Such differences are perhaps unavoidable as confirming the identity of the envenoming snake is often difficult. Only a few studies have reported snake identification by detection of venom antigens [30], [31], [32].
5. Conclusion
Snakebite in Midnapore is a public health problem which is worsened by the unavailability of antivenom. The burden of snakebite in this district perhaps due to underreporting is difficult to estimate because the victims donot seek medical help from government dispensaries. Besides, differing environments, human activities, such as resettlement, sheepherding, fire wood-collecting, defecating, sugar-cane cutting, honey collecting, timber working, encroaches to differing extents on the serene life of snakes. Underreporting of snake bite occurrences have contributed to the variations in observed incidence. But, considering the heterogeneity of medical care and reporting and traditional cultural attitudes to snakes and snake bites, it seems likely that snake bite in Midnapore is widely underreported. For example, in some countries, up to 80% of snake bite victims seek treatment with traditional healers [3] rather than government dispensaries or hospitals. There is an urgent need for case documentation and reporting of the snakebite incidence and determinants in Paschim Midnapore district, West Bengal. In the present study we have attempted to report the hospital based official snakebite statistics (2012–2016) from 10 blocks of this district which actually reflects part of the snakebite scenario of the district. Further documentation of snakebite data from community based surveys and information from traditional healers can provide substantial information about the snakebite statistics of this district.
Acknowledgements
Authors are grateful to Dr Kripasindhu Gantait; Associate Professor, Department of Medicine, Midnapur Medical College for his support for obtaining hospital data. Authors are indebted to Department of Science and Technology (Ref:607(Sanc)/ST/P/S&T/5G-3/2016 dated 17/10/2016) for the financial support.
Contributor Information
Sumana Sarkhel, Email: sumana.sarkhel@yahoo.in.
Rituparna Ghosh, Email: rituparnaghosh0491@gmail.com.
Koushik Mana, Email: koushik.lifescience@gmail.com.
Kripasindhu Gantait, Email: gkripasindhu@yahoo.in.
References
- 1.Warrell D.A. Snake bite. Lancet. 2010;375:77–88. doi: 10.1016/S0140-6736(09)61754-2. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organisation Neglected tropical diseases. Geneva, Switzerland. Available from: http://www.who.int/neglected_diseases/en. [Last accessed on 2013 Jan 7].
- 3.Chippaux J.P. Snake-bites: appraisal of the global situation. Bull. World Health Organ. 1998;76:515–524. [PMC free article] [PubMed] [Google Scholar]
- 4.Kasturiratne A., Wickremasinghe A.R., de Silva N., Gunawardena N.K., Pathmeswaran A. The global burden of snakebite: a literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Med. 2008;5:e218. doi: 10.1371/journal.pmed.0050218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Warrell D.A. Regional Office for South-East Asia − Delhi. WHO; 2010. Guidelines for the Management of Snake-bites; p. 37. [Google Scholar]
- 6.Hati A.K., Mandal M., De M.K., Mukherjee H., Hati R.N. Epidemiology of snake bite in the district of Burdwan, West Bengal. J. Indian Med. Assoc. 1992;90:145–147. [PubMed] [Google Scholar]
- 7.Government of West Bengalt . Vol. 1. Institute of Health & Family Welfare; Kolkata: 2012. p. 3. (A Module on the Management of Snakebite Cases for Medical Officers). [Google Scholar]
- 8.Philip E. Snake bite and scorpion sting. In: Srivatava R.N., editor. Vol. 28. Jaypee Brothers; New Delhi: 1994. pp. 227–234. (Pediatric and Neonatal Emergency Care). [Google Scholar]
- 9.Theakston R.D.G., Warrell D.A., Griffiths E. 2003. Report of a WHO Workshop on the Standardization and Control of Antivenoms. [DOI] [PubMed] [Google Scholar]
- 10.Chippaux J.P. Snake-bites: appraisal of the global situation. Bull. World Health Organ. 1998;76:515–524. [PMC free article] [PubMed] [Google Scholar]
- 11.Sawai Y., Toriba M., Itokawa H., de Silva A., Perera G.L.S., Kottegoda M.B. Death from snakebite in Anuradhapura district. Ceylon Med. J. 1983;28:163–169. [PubMed] [Google Scholar]
- 12.Kularatne S.A. Epidemiology and clinical picture of the Russell's viper (Daboia russelii russelii) bite in Anuradhapura, Sri Lanka: A prospective study of 336 patients. Southeast Asian J. Trop. Med. Public Health. 2003;34:855–862. [PubMed] [Google Scholar]
- 13.Suchithra N., Pappachan J.M., Sujathan P. Snakebite envenoming in Kerala, South India: clinical profile and factors involved in adverse outcomes. Emerg. Med. J. 2008;25:200–204. doi: 10.1136/emj.2007.051136. [DOI] [PubMed] [Google Scholar]
- 14.Kaouadji K., Kaker N., Vallet B. Morsures, griffures et envenimations: conduite à tenir en urgence. EMC-Médecine. 2004;1:337–351. [Google Scholar]
- 15.Castanet J., Guyetant R. Société herpétologique de France; 1989. Atlas de répartition des amphibians et reptiles de France Paris; pp. 1–191. [Google Scholar]
- 16.Government of West Bengalt . Vol. 1. Institute of Health & Family Welfare; Kolkata: 2012. p. 3. (A Module on the Management of Snakebite Cases for Medical Officers). [Google Scholar]
- 17.Simpson I.D. Snakebite management in India, the first few hours: a guide for primary care physicians. J. Indian Med. Assoc. 2007;105(324):326. [PubMed] [Google Scholar]
- 18.Islam Q.T., Faiz M.A., Azhar M.A., Ekram A.R.M.S., Alam M.T. Snake bite in northern Bangladesh: a hospital based study of 68 cases. TAJ. 1999;12:135–138. [Google Scholar]
- 19.Seneviratne S.L., Wickrama W.S.S., Opanayaka C.J., Ratneyake N.S.L., Gunatilake S.B., De Silva H.J. Use of antivenom serum in snake bite: a prospective study of hospital practice in the Gampaha district. Ceylon Med. J. 2000;45:65–68. doi: 10.4038/cmj.v45i2.8003. [DOI] [PubMed] [Google Scholar]
- 20.Theakston R.D., Phillips R.E., Warrell D.A., Galagedara Y., Abeysekera D.T., Dissankyaka P., De Silva A., Aloysius D.J. Envenoming by the common krait (Bungarus caeruleus) and Sri Lankan cobra (Naja naja naja): efficacy and complications of therapy with Haffkine antivenom. Trans. R. Soc. Trop. Med. Hyg. 1990;84:301–308. doi: 10.1016/0035-9203(90)90297-r. [DOI] [PubMed] [Google Scholar]
- 21.Lal P., Dutta S., Rotti S.B. Epidemiological profile of snake bite cases admitted in JIPMER hospital. Indian J. Commun. Med. 2001;6:45–48. [Google Scholar]
- 22.Brunda G., Sashidhar R.B. Epidemiological profile of snake-bite cases from Andhra Pradesh using immunoanalytical approach. Indian J. Med. Res. 2007;125:661–668. [PubMed] [Google Scholar]
- 23.Majumder D., Sinha A., Bhattacharya S.K., Ram R., Dasgupta U., Ram A. Epidemiological profile of snake bite in South 24 Parganas district of West Bengal with focus on underreporting of snake bite deaths. Indian J. Public Health. 2014;58:17–21. doi: 10.4103/0019-557X.128158. [DOI] [PubMed] [Google Scholar]
- 24.Premawardana A.P., De Silva C.E., Foneska M.M.D., Gunitalake S.B., De Silva H.J. Low dose subcutaneous adrenaline to prevent acute adverse reactions to antivenom serum in patients bitten by snakes: a randomized placebo controlled trial. Br. Med. J. 1999;318:1041–1043. doi: 10.1136/bmj.318.7190.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sethi P.K., Rastogi J.K. Neurological aspects of ophitoxemia (Indian krait) − A clinico-electromyographic study. Indian J. Med. Res. 1981;73:269–276. [PubMed] [Google Scholar]
- 26.Paoli M., Rigoni M., Koster G., Rossetto O., Montecucco C. Massspectrometry analysis of the phospholipase A(2) activity of snake pre-synaptic neurotoxins in cultured neurons. J. Neurochem. 2009;111:737–744. doi: 10.1111/j.1471-4159.2009.06365.x. [DOI] [PubMed] [Google Scholar]
- 27.Rigoni M., Paoli M., Milanesi E., Caccin P., Rasola A. Snake phospholipase A2 neurotoxins enter neurons, bind specifically to mitochondria, and open their transition pores. J. Biol. Chem. 2008;283:34013–34020. doi: 10.1074/jbc.M803243200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Montecucco C., Rossetto O. How do presynaptic PLA2 neurotoxins block nerve terminals? Trends Biochem. Sci. 2000;25:266–270. doi: 10.1016/s0968-0004(00)01556-5. [DOI] [PubMed] [Google Scholar]
- 29.Seneviratne U., Dissanayake S. Neurological manifestations of snake bite in Sri Lanka. J. Postgrad. Med. 2002;48:275–278. [PubMed] [Google Scholar]
- 30.Theakston R.D., Phillips R.E., Warrell D.A., Galagedera Y., Abeysekera D.T. Envenoming by the common krait (Bungarus caeruleus) and Sri Lankan cobra (Naja naja): efficacy and complications of therapy with Haffkine antivenom. Trans. R. Soc. Trop. Med. Hyg. 1990;84:301–308. doi: 10.1016/0035-9203(90)90297-r. [DOI] [PubMed] [Google Scholar]
- 31.Bawaskar H.S., Bawaskar P.H. Profile of snakebite envenoming in western Maharashtra, India. Trans. R. Soc. Trop. Med. Hyg. 2002;96:79–84. doi: 10.1016/s0035-9203(02)90250-6. [DOI] [PubMed] [Google Scholar]
- 32.Sharma S.K., Koirala S., Dahal G. Krait bite requiring high dose antivenom: a case report. Southeast Asian J. Trop. Med. Public Health. 2002;33:170–171. [PubMed] [Google Scholar]