Abstract
TicHelper.com (“TicHelper”) is an interactive online treatment program for youth with chronic tic disorders (CTDs) or Tourette Syndrome (TS) and their parents. It is based on Comprehensive Behavioral Intervention for Tics (CBIT), an individual, outpatient therapy protocol shown to effectively reduce tics in randomized controlled trials. The TicHelper website offers a user-friendly dashboard that is effective in making it easy to navigate through different treatment modules. Modules parallel core CBIT procedures and consist of interactive exercises, informational videos, and self-report ratings. TicHelper has some weaknesses (e.g., no outcomes research specific to the program has been published to date); however, its strengths (easily navigable, clear instructions, appropriate content) outweigh its weaknesses, making it a potentially useful dissemination tool to make CBIT more accessible to families and youth with tics.
Keywords: tic, Tourette, self-help, web-based therapy
Description
TicHelper.com (“TicHelper”) is an online, interactive self-help program for youth with tics ages 8 years through late adolescence. The program’s stated goal “is to help parents and children with chronic tic disorders (CTDs) or Tourette Syndrome (TS) to learn about tics, to learn about situations that trigger tics, and to learn how to recognize and block tics” (Tichelper.com, 2015, “Our Goals”). The program is intended to be family-based (i.e., completed jointly by the child and parent) and includes parent skills training, although the website specifies that adolescents older than 15 years of age can follow the program more independently. TicHelper is designed to be completed in 8 weeks. Initial registration takes approximately 30 minutes, and daily time spent on the program is estimated at 30 to 60 minutes (approximately 10 to 20 minutes of website activity and the remainder for skill practice). Development of TicHelper was funded by the NIMH (R43MH096344, R44MH096344: PI: Suzanne Mouton-Odum) as a collaboration between PsychTech, Ltd. (Drs. Suzanne Mouton-Odum, Robin Reamer), Dr. Douglas Woods, and Dr. Michael Himle.
TicHelper is based on the therapist-guided protocol for Comprehensive Behavioral Intervention for Tics (CBIT; Woods, 2008). TicHelper contains four primary modules that parallel core CBIT procedures: (1) “Tic Education,” which includes psychoeducation about tic prevalence, etiology, and phenomenology; (2) “Reducing Tic Triggers,” which focuses on function-based interventions to mitigate the impact of contextual factors that worsen tics; (3) “Tic Awareness,” which targets improved awareness of tics and corresponding premonitory urges; and (4) “Tic Blocking,” which involves training competing responses to prevent tic occurrence.
The website is anchored around a “dashboard” that unlocks modules as one progresses through the program, thus ensuring that the program is followed in sequence while allowing flexibility to review previous material (Figure 1). Modules include videos, written text, and interactive elements that mimic assessment measures and the CBIT manual worksheets. Videos feature an actress called the “TicHelper,” who provides didactic information with the aid of animations to illustrate key concepts. Other videos provide examples of tics, competing responses, and parent-child interactions (e.g., demonstrations of how parents should react to tics). Weekly self-assessment occurs via a modified Parent Tic Questionnaire (PTQ; Chang, Himle, Tucker, Woods, & Piacentini, 2009), which instructs parents to rate tic severity as well as reflect on their own actions related to their child’s tics. A “Tic Drill” questionnaire assesses homework compliance, and a calendar tracks progress and PTQ ratings. Several CBIT therapy worksheets and in-session activities were adapted to an interactive, computerized format. One example of this is an individually created “tic hierarchy” in which the child identifies and ranks current tics, such that the tic the child wants to work on is at the top (rankings can be changed at any time; see Figure 2). Rankings in turn drive program content. For example, if “eye blinking” is the top tic, the “Awareness” module will depict videos of eye blinking and prompt the user to create a detailed written description of the eye blinking tic. As another example, in the “Awareness” module, the user is shown a picture of a person and clicks on the parts of the body where an urge to tic is experienced (Figure 3).
Figure 1.

TicHelper dashboard.
Figure 2.
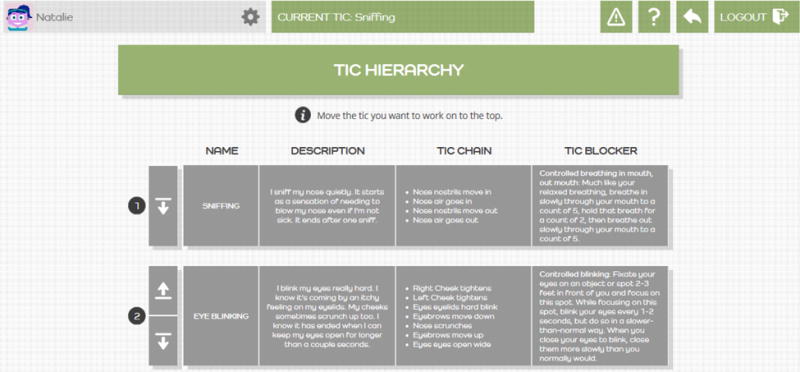
Tic hierarchy.
Figure 3.
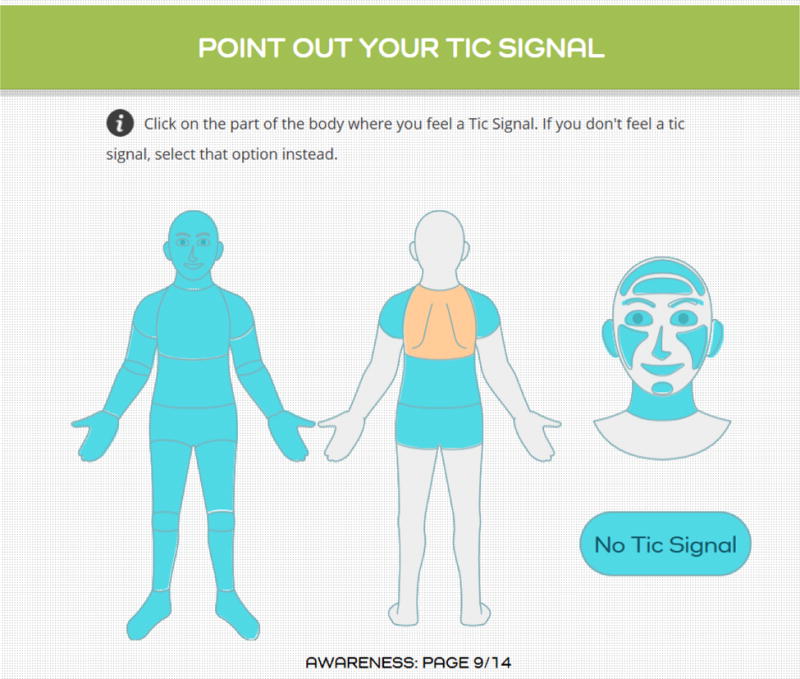
Urge identification module.
The site states that TicHelper is the only interactive self-help program for tics on the market. While costs may change, the fee listed on the website is $149.99 for the 8-week program. At the end of the 8 weeks, users have the option to continue using the program as a monthly subscription (price is currently unspecified). A shorter duration option is not currently available.
Background
TicHelper is based on the published CBIT therapist-guided manual and patient workbook (Woods, 2008; Woods et al., 2008). The CBIT protocol consists of eight individual outpatient sessions delivered over 10 weeks. Sessions involve Habit Reversal Therapy (HRT, including tic awareness and competing response training [Azrin & Nunn, 1973], relaxation training, and function-based intervention).
CBIT has demonstrated efficacy for youth aged 9–17 years with CTD or TS (Piacentini et al., 2010). In a large randomized trial, CBIT led to significantly greater reductions in tic severity than supportive psychotherapy (mean reduction in Yale Global Tic Severity Scale of 7.6 points in CBIT, effect size = 0.68). Within the CBIT group, 52.5% of youth were classified as treatment responders, and treatment gains were durable for 87% of responders through 6-month follow-up (Piacentini et al., 2010). Meta-analysis of randomized trials testing HRT-based behavioral interventions for tics demonstrated a medium effect size relative to comparison conditions (SMD = 0.67; McGuire et al., 2014). Effect sizes in these trials were comparable to pharmacological interventions. Further, behavioral treatment has fewer associated adverse effects than pharmacotherapy. In the Piacentini et al. (2010) study, no treatment-related significant adverse events occurred in the CBIT group.
Although CBIT is efficacious, there are some significant barriers to those seeking treatment. Woods, Conelea, and Himle (2010) surveyed 487 parents of children with tics and found that only 6% had actually received behavioral therapy. In describing reasons for not engaging in behavior therapy, 42% reported difficulty finding knowledgeable treatment providers, 41% identified a financial burden, 33% had no tic specialist in their area, and 26% found the time commitment a barrier to treatment.
Various dissemination studies have explored strategies to counter the inaccessibility and expense associated with CBIT. CBIT delivered via video conference or voice over Internet with a therapist has been shown to yield similar results to in-person CBIT (Himle et al., 2012; Ricketts et al., 2015). Although this method has the potential to increase access for families who cannot find local tic specialists, telehealth still requires a live therapist, does not address barriers related to time commitment and expense, and involves potentially challenging legal and ethical considerations (e.g., licensure when delivering therapy across state lines, need for HIPAA compliant transmission; American Psychological Association, 2015, “Practicing Distance Therapy, Legally and Ethically”). Another dissemination project examined delivery of abbreviated CBIT by non-mental health providers (pediatricians and neurologists; Ricketts et al., 2015). Although treatment was associated with a significant decrease in tic severity, the study was small (n = 9) and still relied on in-person treatment with a professional.
TicHelper developers created the program in an effort to disseminate CBIT in a format that eliminates the need for a live provider while also being easily accessible, low-cost, and flexible. There are currently no other commercialized products involving computerized CBIT. The only roughly comparable resources are CBIT-based therapist manuals, informational videos, informative websites, and self-help books. None of these resources disseminate CBIT in an interactive, self-administered format. Similar programs include variations of HRT for other conditions and have demonstrated efficacy for web-delivered treatment of hair-pulling (stoppulling.com; Mouton-Odum, Keuthen, Wagener, & Stanley, 2006) and skin picking (stoppicking.com; Mouton-Odum et al., 2006).
Appropriateness of Content
TicHelper is consistent with CBIT principles and content. The website “brings to life” the therapist-guided manual and accompanying parent workbook via videos and interactive components (Woods, 2008; Woods et al., 2008). The actress in the videos fills in the therapist role nicely for the psychoeducational elements of the treatment. Modules closely parallel core CBIT procedures and are programmed to occur in sequence by “unlocking” after prior module completions or reaching certain criteria. For example, competing response training cannot be accessed until the child identifies tic occurrences with 80% accuracy during awareness training (the same criterion in the therapist manual). Similarly, youth must complete the homework form upon login to unlock other modules.
Modules retain the intent of CBIT to focus on teaching principle-based application of CBIT strategies rather than rotely training techniques. For example, the program provides suggestions for competing responses based on the identified tics but emphasizes idiographic adaptation by teaching the process of competing response selection and modification. TicHelper also contains an impressive degree of individualization based on user input about specific tic symptoms, particularly in the Awareness and Tic Skills modules. Users watch videos of children with similar tics and see them implement CBIT skills. There are multiple potential benefits of this feature, including improved tic awareness and implicit normalization of symptoms. In our clinical experience, many youth presenting to individual therapy often describe a sense of isolation. Seeing other children with similar symptoms may have a positive impact on youth, especially given the rarity of the disorder and the often stigmatizing portrayal of tics in other media.
There is evidence throughout TicHelper that efforts were made to make the program content and format developmentally appropriate. Visuals have a “kid friendly” feel with features such as bright colors, crisp graphics, animations embedded in didactic videos, and a user-selected cartoon avatar. Information is presented in language that is easy to understand. CBIT jargon was replaced with catchy terms, such as “tic blocker” instead of “competing response.” Parent-directed content is equally accessible. Videos depicting parent-child interactions are particularly useful in demonstrating CBIT-consistent and inconsistent parent behaviors, and child actors encompass a range of ages. Of note, while the developers’ target audience is children and parents, we believe that adults with tics may also find benefit from the program, especially since there is currently no parallel program targeted to adults.
Although the interactive and individualized features in TicHelper are an overall strength, function-based intervention is not individually tailored in the program. In CBIT, the purpose of function-based intervention is to isolate factors that exacerbate tics and modify those factors to bring about tic reduction and reduced impairment (Woods et al., 2008). An important aspect of function-based intervention is its idiographic nature—it is widely accepted that contextual factors have an impact on tics, but the precise impact of certain factors varies from person to person (Conelea & Woods, 2008). Translating idiographic intervention to a standardized self-help program is certainly challenging. TicHelper approaches this challenge by giving all users the same set of recommendations for “reducing tic triggers” (e.g., parent strategies such as not reacting to tics; child strategies such as relaxation techniques, exercise, and sleep hygiene). Parents and children each select three tic-reducing strategies to work on each day using a form, and they are also asked to identify strategies used in the homework monitoring module. Therefore, TicHelper trades off highly individualized function-based intervention for training in a broad set of many possibly beneficial interventions. Individualization around problem solving is also lacking in TicHelper. For example, if a child is unable to catch 80% of their tics (due, potentially, to age or comorbidities), they would not be able to move forward in the program. In traditional in-person CBIT, additional strategies are typically tried to help improve awareness (e.g., practice noticing tics while in front of a mirror or watch a video of oneself).
Of note, TicHelper does not include a separate module addressing relapse prevention. In CBIT, relapse prevention is typically introduced near the end of treatment and includes psychoeducation and strategies for ongoing tic monitoring and competing response implementation for new-onset tics.
Research Evidence
Research on TicHelper has not been published to date. The site is based on the therapist manual used in the largest randomized trial of CBIT (Piacentini et al., 2010). Whether response is comparable remains to be seen.
TicHelper was developed in the context of two NIMH-funded Small Business Innovation Research Grants (SBIR). The Phase I SBIR (R43MH096344; PI: Mouton-Odum) involved the creation of a TicHelper prototype and review of the prototype by experts in tic disorders/CBIT and potential end-users (i.e., children with tic disorders and their parents). Although data from Phase I have yet to be published, developers have preliminarily reported that the prototype received high ratings from professionals and end-users on indices of feasibility, acceptability, and usability. The program also showed initial indication of being effective for reducing tic symptoms, although detailed treatment outcome data have not yet been published (Hayes et al., 2015; Mouton-Odum, Woods, & Himle, 2015).
Phase II of the SBIR is currently under way (M. Himle & D. Woods, personal communication, November 5, 2015). The Phase I prototype was expanded using an iterative feedback process with expert reviewers and end-users. The current version of TicHelper includes all elements of the CBIT therapist manual, interactive features, and a child-friendly graphic design. A randomized control trial comparing TicHelper to an Internet-based resources condition is ongoing (M. Himle & D. Woods, personal communication, November 5, 2015). In the comparison condition, families are given links to publically available web resources about tics and tic treatment and are asked to review these sites together on a daily basis for 8 weeks.
There are no comparable programs available to consumers, meaning that the only evidence-based option for families is to receive CBIT from a trained provider. Although a CBIT manual and accompanying parent/adult workbook are available for purchase at a relatively low cost (approximately $60 for both at present; Woods, 2008; Woods et al., 2008), these materials are designed to be used in the therapy context by therapists with specialized knowledge and training.
Utility
TicHelper was developed to disseminate CBIT, and we believe it has strong potential in this regard. The program is a good middle ground between a self-help book and traditional therapy. The program does not require a live provider, can be accessed from anywhere with Internet, has a low time burden, and may be lower-cost to users than therapy (depending on insurance coverage/co-pay, travel cost, etc.). TicHelper offers much more to users than other commercially available self-help books and informational websites and videos, particularly because of features that are individualized and interactive.
There are, however, some limitations of the program. First, the program seems to be targeted to a “textbook case” and may have less utility for “complex cases.” Although up to 80% of youth with tics have co-occurring psychopathology (Centers for Disease & Prevention, 2009), TicHelper does not address comorbid disorders or provide guidance about how to adjust CBIT strategies in the context of other emotional or behavioral problems. Disorders that commonly co-occur with tic disorders could potentially prevent users from benefiting from the program. Importantly, TicHelper does clearly tell parents up front that it is designed specifically to treat tics. A preregistration form screens for co-occurring psychiatric disorders and factors that may lead to reduced benefit (e.g., younger age) and fully informs parents about program fit prior to parents subscribing or paying for the program. Other “complex” clinical characteristics that may not be adequately addressed by the program include tics that put the child at risk, such as self-injurious tics or tics that impact co-occurring medical conditions. These types of tics may require therapist expertise and collaboration with medical providers to ensure appropriate adaptation of CBIT strategies.
Second, some of the clinical nuance in CBIT may be missed when administered without a therapist. For example, competing responses often need subtle tweaking to fit different contexts (e.g., adapting a hand tic competing response to not disrupt writing), and youth with particularly aversive urges may require instruction in adjunctive coping or motivational strategies. It is also possible that users will follow competing response instructions “to the letter” but miss the “essence” of what competing responses are intended to do (e.g., pick a competing response that relieves a premonitory urge rather than one that enables natural urge reduction). A clinician may also bring insight that clients themselves lack, such as identifying tics that the family does not endorse, the presence of a comorbid condition, or family systems issues that adversely impact tics or treatment adherence. Finally, therapist interaction with schools is often beneficial when tics are disruptive in that setting.
Third, the program’s strict focus on tic severity reduction may be a limitation for youth who experience tic-related psychosocial problems, such as tic-related avoidance, bullying, poor self-esteem, or limited social or emotion regulation skills. These problems are important to address clinically, particularly because tic severity is not the sole driver of functional impairment and diminished quality of life in youth with tic disorders (Cavanna et al., 2013). Moreover, tic reduction may not be the only path to positive global outcome. Intervention targeting tic-related psychosocial problems has shown initial promise in improving quality of life and psychosocial functioning in youth with tics (McGuire et al., 2015). Reducing tics may not have the desired effect of reducing impairment in school, and this intervention does not give recommendations regarding communications with schools. Thus, TicHelper may have less utility for those who need help addressing the psychosocial consequences of tics.
The preregistration process for TicHelper specifies that users who are likely to be a good fit are youth with tics who do not have intellectual disability, severe oppositional behavior, or impairment primarily attributable to a co-occurring disorder. We agree that TicHelper, if shown to be efficacious, may be a valuable resource for those who are not otherwise able to access CBIT from a qualified provider, such as those with geographic or financial barriers to care. If parents are deciding between TicHelper and seeing a CBIT specialist, they should consider individual characteristics of their child, such as comorbidity, psychosocial impairment, tic complexity, and the need for adjunctive family or school-based support. As mentioned above, youth with a more complex psychiatric profile may be better served by traditional therapy.
The current version of TicHelper does not include clear guidance or troubleshooting for those who do not achieve desired response or those who identify a need for further or different therapeutic support. Developers informed us that they are addressing this issue in their ongoing study by asking participants what they would find most useful at the end of the program (M. Himle & D. Woods, personal communication, November 5, 2015). For now, users have the option of using the program as a monthly subscription after the 8-week treatment period.
Although not a stated goal of the program, it is our opinion that TicHelper may have potential utility in a stepped-care treatment model. Given that the program contains all of the key components of CBIT, it is possible that this can be utilized as a first-line treatment, although research is needed to determine if it is effective for the target population. If shown to be effective, clinics could refer families to the program as a first step in care, or families could use the program while on a waitlist to see a CBIT specialist. This stepped-care approach may eliminate the need for individual therapy for responders. Even for youth who do not satisfactorily respond, it is possible that completion of TicHelper may reduce the number of contact hours needed with a live therapist (e.g., therapy could immediately focus on troubleshooting or co-occurring difficulties). TicHelper could also be an adjunctive resource for youth whose medication is being managed by a neurologist or pediatrician or those seeing a mental-health provider for other problems.
Ease of Use/Overall Appeal
TicHelper is easy to navigate, visually appealing, and informative. The program strikes a nice balance between maintaining simplicity and “kid appeal” without sacrificing appropriate depth of content or appearing too juvenile. Thus, we anticipate that youth across the targeted age range will find the site appealing.
The program dashboard is crisp in design and easy to navigate. The top of the screen has a pane with the phrase “Working On: (module)” to remind users of their place within the program. Although program navigation is easy at the beginning, navigation becomes clunkier when one tries to review previously learned material. It is not easy to navigate back to specific videos for a refresher or when starting work with a new tic. In the absence of a site content list, a user has to click through all of the videos to find a specific video previously watched.
Each module contains well-produced videos that demonstrate concepts and examples of tics and other child and parent CBIT skills. The site is visually appealing throughout, with bold colors and artistic graphics to help orient users to sections and illustrate concepts. Further, the bright color scheme contributes to the appeal and ease of navigating the program.
Conclusions
Strengths
TicHelper has a number of laudable strengths: it was created by treatment experts to closely parallel an empirically based treatment, it was developed in the context of an NIMH-funded project using feedback from experts and target users, it is easy to access and navigate, and it contains interactive and individualized elements. The content clearly mirrors the CBIT therapist manual but is adapted to be more easily understood by a self-help audience. Skills have catchy, memorable names, and information is delivered by simple written materials, interactive forms, and videos that feature an enthusiastic actress and realistic, relatable portrayals of kids with tics and their parents. The program is visually attractive with a modern aesthetic, bright colors, and crisp graphics and animations.
Overall, TicHelper is an important step forward for CBIT dissemination. It is a much needed resource for youth with tics and their families, especially given that there is no comparable program on the market. TicHelper has strong potential for bringing CBIT to those who face barriers to accessing traditional therapy. TicHelper could also potentially play in a role in a stepped-care model of treatment. The program may help triage therapist resources, which are often limited given the rarity of expertise in tic disorders. Although the clinical outcomes of TicHelper are still under investigation, it is possible that the program may still be beneficial for those who do not gain full desired improvement, particularly in a stepped-care approach.
Weaknesses
The TicHelper site states that the program provides “the most comprehensive approach available on the internet.” While we agree that TicHelper is the most comprehensive tic treatment program of this modality, its primary weakness is that it is not comprehensive in the global sense. Its aim parallels that of the CBIT manual: tic reduction. Research suggests that this narrow focus on tic reduction is not necessarily problematic. Youth who respond positively to CBIT do not show deterioration in secondary psychiatric symptoms over the course of acute treatment, and positive response is actually associated with improved behavioral, social, and familial functioning 6 months posttreatment (Woods et al., 2011). However, for potential users with clinically significant co-occurring psychopathology or tic-related psychosocial problems, the program’s narrow focus may be a limitation. Other weaknesses are reflective of the inherent nature of web-based intervention, such as the program’s nonidiographic approach to function-based intervention and the absence of therapist feedback to troubleshoot skills implementation. Finally, at the time of this review, data on program outcomes, feasibility, acceptability, and usability have not been published. The absence of these data is reflected in our research evidence rating. However, given that research on TicHelper is ongoing, we encourage readers to stay tuned for future research developments.
Overall Conclusions
Overall, TicHelper is a valuable resource for families seeking empirically derived tic treatment, particularly those who face barriers to receiving CBIT. The program fills a critical treatment accessibility gap. Evaluative ratings are provided in Table 1. Program strengths outweigh weaknesses, especially given that there is no comparable resource on the market today. Although research support for TicHelper is forthcoming, the interactive and individualized nature of the program firmly place it a step above existing informational resources and self-help books.
Table 1.
Evaluative Ratings for TicHelper.com
| Criterion | Score |
|---|---|
| Appropriateness of Content | 1 |
| Research Evidence | 3 |
| Utility | 2 |
| Ease of Use/Overall Appeal | 2 |
Note. 1 = Outstanding, 2 = Very Good, 3 = Satisfactory, 4 = Marginal, 5 = Poor, NP = Not Present, NA = Not Applicable
Table 2.
Summary of TicHelper.com
| Resource name | Web Homepage | Target Audience and Purpose | Strengths | Weaknesses | Overall Conclusions |
|---|---|---|---|---|---|
| TicHelper | www.tichelper.com |
|
|
|
|
Highlights.
TicHelper is an interactive online treatment program for youth with tic disorders
Treatment is based on Comprehensive Behavioral Intervention for Tics (CBIT)
Primary strengths are that TicHelper is interactive, easily navigable, and developmentally tailored.
TicHelper focuses on tic reduction and does not address comorbidities or tic-related psychosocial difficulties
TicHelper holds promise for CBIT dissemination
Acknowledgments
Disclosure Statement: Dr. Conelea served as a professional reviewer on the TicHelper.com development project and was compensated for that role. Neither author has any current financial arrangement with TicHelper.com. Dr. Conelea is supported by a grant from the NIMH (K23MH103617).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Azrin N, Nunn R. Habit-reversal: A method of eliminating nervous habits and tics. Behaviour Research and Therapy. 1973;11(4):619–628. doi: 10.1016/0005-7967(73)90119-8. [DOI] [PubMed] [Google Scholar]
- Cavanna AE, Luoni C, Selvini C, Blangiardo R, Eddy CM, Silvestri PR, Termine C. Disease-specific quality of life in young patients with tourette syndrome. Pediatric Neurology. 2003;48(2):111–114. doi: 10.1016/j.pediatrneurol.2012.10.006. [DOI] [PubMed] [Google Scholar]
- Centers for Disease & Prevention. Prevalence of diagnosed Tourette syndrome in persons aged 6–17 years—United States, 2007. MMWR. Morbidity and Mortality Weekly Report. 2009;58(21):581–585. [PubMed] [Google Scholar]
- Chang S, Himle MB, Tucker BT, Woods DW, Piacentini J. Initial psychometric properties of a brief parent-report instrument for assessing tic severity in children with chronic tic disorders. Child & Family Behavior Therapy. 2009;31(3):181–191. [Google Scholar]
- Conelea CA, Woods DW. The influence of contextual factors on tic expression in Tourette's syndrome: a review. Journal of Psychosomatic Research. 2008;65(5):487–496. doi: 10.1016/j.jpsychores.2008.04.010. [DOI] [PubMed] [Google Scholar]
- Hayes LP, Bauer CC, Houghton DC, Ramanujam K, Alexander J, Himle MB, Mouton-Odum S. Iterative development of an internet-based self-guided behavior therapy program for tics. Poster presented at Association for Behavioral and Cognitive Therapies; Chicago, IL. 2015. [Google Scholar]
- Himle MB, Freitag M, Walther M, Franklin SA, Ely L, Woods DW. A randomized pilot trial comparing videoconference versus face-to-face delivery of behavior therapy for childhood tic disorders. Behaviour Research and Therapy. 2012;50(9):565–570. doi: 10.1016/j.brat.2012.05.009. [DOI] [PubMed] [Google Scholar]
- McGuire JF, Arnold E, Park JM, Nadeau JM, Lewin AB, Murphy TK, Storch EA. Living with tics: Reduced impairment and improved quality of life for youth with chronic tic disorders. Psychiatry Research. 2015;225(3):571–579. doi: 10.1016/j.psychres.2014.11.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire JF, Piacentini J, Brennan EA, Lewin AB, Murphy TK, Small BJ, Storch EA. A meta-analysis of behavior therapy for Tourette Syndrome. Journal of Psychiatric Research. 2014;50:106–112. doi: 10.1016/j.jpsychires.2013.12.009. [DOI] [PubMed] [Google Scholar]
- Mouton-Odum S, Keuthen NJ, Wagener PD, Stanley MA. StopPulling.com: An interactive, self-help program for trichotillomania. Cognitive and Behavioral Practice. 2006;13(3):215–226. [Google Scholar]
- Mouton-Odum S, Woods D, Himle M. Tic Helper. 2014 Retrieved 12.9.15, 2015, from tichelper.com.
- Mouton-Odum S, Woods D, Himle M. Project Information for 5R44MH096344-03. 2015 Retrieved from: https://projectreporter.nih.gov/project_info_description.cfm?aid=8848891&icde=27209465.
- Piacentini J, Woods DW, Scahill L, Wilhelm S, Peterson AL, Chang S, Walkup JT. Behavior therapy for children with Tourette disorder: A randomized controlled trial. JAMA. 2010;303(19):1929–1937. doi: 10.1001/jama.2010.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricketts EJ, Goetz AR, Capriotti MR, Bauer CC, Brei NG, Himle MB, Woods DW. A randomized waitlist-controlled pilot trial of voice over Internet protocol-delivered behavior therapy for youth with chronic tic disorders. Journal of Telemedicine and Telecare. 2015 doi: 10.1177/1357633X15593192. 1357633X15593192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods DW. Managing Tourette syndrome: A behavioral intervention for children and adults therapist guide. New York: Oxford University Press; 2008. [Google Scholar]
- Woods D, Piacentini J, Chang S, Deckersbach T, Ginsberg G, Peterson AL, Wilhelm S. Managing Tourette Syndrome. Oxford University Press; 2008. [Google Scholar]
- Woods DW, Conelea CA, Himle MB. Behavior therapy for Tourette syndrome: Utilization in a community sample and an emerging area of practice for psychologists. Professional Psychology: Research and Practice. 2010;41:518–525. [Google Scholar]
- Woods DW, Piacentini JC, Scahill L, Peterson AL, Wilhelm S, Chang S, Walkup JT. Behavior therapy for tics in children: Acute and long-term effects on psychiatric and psychosocial functioning. Journal of Child Neurology. 2011;26(7):858–865. doi: 10.1177/0883073810397046. [DOI] [PMC free article] [PubMed] [Google Scholar]


