Abstract
Context:
Breast cancer incidence is increasing rapidly in India. The lifestyle, built, genetic makeup, reproductive and breastfeeding patterns are quite different in Indian females when compared to the Western population. Generalizing the Western data to the population residing in the Himalayan region would breed inaccuracies.
Aim:
The aim of our study was to identify risk factors in our own population in a Western Himalayan state of Himachal Pradesh, India.
Subjects and Methods:
A case–control study with 377 cases of invasive breast cancer and 346 hospital-based controls was conducted for 1 year. The data were collected by interviewing the individuals during their visit to hospital using a questionnaire. The data were analyzed using standard statistical techniques using SPSS version 17 software.
Results:
Factors found to have strong association with invasive breast cancer on multivariate analysis are late age at first childbirth >30 years, which is the strongest risk factor associated, late age of menopause > 50 years, high socioeconomic class, and age of female above 50 years.
Conclusion:
In our females, age >50 years, late age of menopause (>50 years), late age at first childbirth (>30 years), and high socioeconomic status were found to be major risk factors associated with breast cancer. Several factors implicated in the Western data were not found to be significant in our study. We need to identify such aspects in reproductive and breastfeeding patterns of women and spread awareness regarding the same.
Keywords: Breast cancer risk factors, breastfeeding, childbearing, Himalayan population, urbanization
Introduction
Throughout Asia, the incidence of breast cancer is increasing rapidly, in contrast to Western countries where it is now relatively stable.[1] The same range of hormonal, acquired, and intrinsic risk factors has been identified for both Asians and Western women although the level of exposure to each specific factor may vary according to a woman's ethnicity, culture, and place of residence.
India is a subcontinent with wide cultural, religious, and economic diversity and variation in the healthcare infrastructure. Himachal Pradesh is a small North Indian state situated in the Western Himalayas with better life expectancy as compared to the rest of India. The risk factors postulated in many studies on Western females are not commonly seen in the majority of Indian females. Despite this, the incidence of breast cancer in this Himalayan belt is rising and needs to be studied.
No similar evaluation has been conducted in the Himalayan regions on the epidemiology of breast cancer. This led us to undertake this study to identify risk factors in female breast cancer patients of Himachal Pradesh.
This hospital-based, case–control study was conducted at the Regional Cancer Centre, Shimla, with an aim to identifying the distribution of potential lifestyle-related variables in Himachal that are possibly associated with breast cancer risk.
Subjects and Methods
An unmatched case–control study was conducted at the Regional Cancer Centre, Department of Radiotherapy, Indira Gandhi Medical College and Hospital, Shimla, Himachal Pradesh. This study was conducted for 12 months, i.e., from January 1, 2014, to December 31, 2014. Ethical approval was obtained from the Ethical Committee.
In this study, female patients with invasive breast cancer visiting our institution during the study period of 1 year for treatment and follow-up constituted the participants for the study. The patients on follow-up during the period 2010–2014 (5 years) were recalled. The required information and contact number were collected from the central registration office of the institute.
Patients having any cancer other than breast cancer (except for ovarian cancer, thyroid cancer, and Hodgkin's lymphoma) were excluded as cases. Furthermore, patients who were not mentally sound to give relevant history and those who were not willing to get enrolled into the study were excluded from the study.
A total of 377 cases and 346 hospital-based controls were enrolled into the study after taking their consent.
Controls were identified and selected from the various female wards of the hospital including the oncology ward. Those patients with either carcinoma of the cervix, ovary, or uterus as their main diagnosis were excluded as controls.
The data were collected by interviewing the individuals during their visit to hospital using a detailed, predesigned and pretested, self-prepared questionnaire.
The data so collected were entered and analyzed using standard statistical techniques using SPSS Statistics for Windows, Version 17.0 (SPSS Inc. Released 2008. Chicago) software.
Results
Characteristics of cases and controls
The data of 377 cases and 346 controls were evaluated in this study. The hospital-based prevalence of breast cancer in Himachal is 1.24 per 1 million female population.
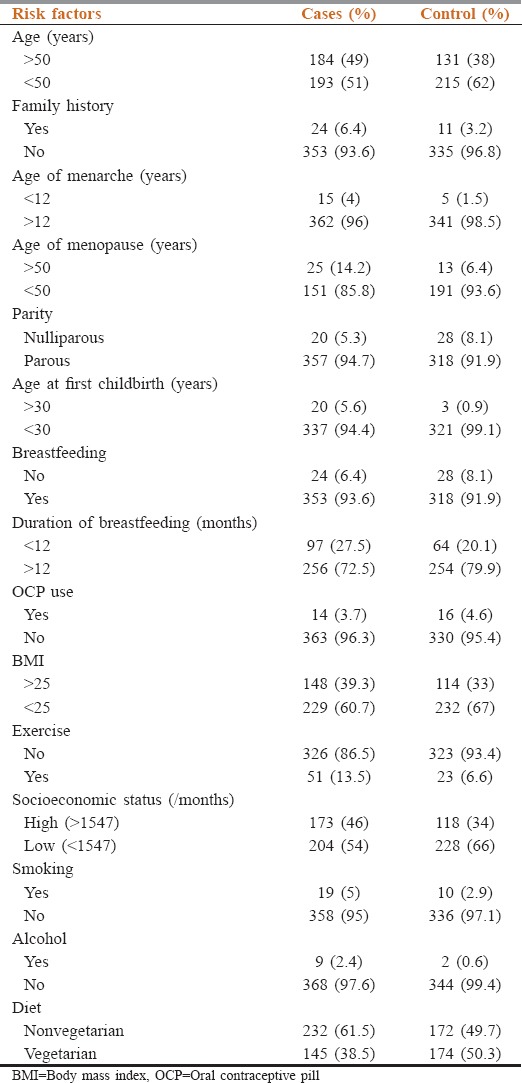
The cases and controls were comparable in terms of age groups and rural and urban background. Table 1 shows the comparison of cases and controls according to their frequency of exposure to various risk factors. Exposure to maximum risk factors is more in cases as compared to controls, except for few risk factors such as nulliparity, not breastfeeding, physical inactivity, and oral contraceptive pill (OCP) use which was seen more in controls.
Table 1.
Comparison of cases and controls according to their exposure to various risk factors
Maximum numbers of patients are in the age group of 46–50 years (22.5%). The mean age in our study is 51.1 ± 10.34 years.
Most of our patients never went to school (32.4%), while 23.3% patients studied only till primary. This further reflects that education is not a priority for females in rural areas.[2] The study group mainly comprises females above 50 years, so majority of females belong to the era when primary education was considered adequate for females.[2]
Majority of patients presented in Stage IIB, i.e., 29.4% cases. 22.8% cases presented in Stage IIIA and 19.4% cases presented in Stage IIA. Only 2.1% cases presented in early stage (Stage IA). The most common symptom at presentation is painless breast lump, and the most common histology in our patients is duct cell histology.
The most common site of disease is the upper outer quadrant. In 0.5% cases, disease was involving both breasts.
Although a positive family history was present in 24 patients, only five patients got screening mammography done before their diagnosis for suspicion of a breast lump and 98.7% patients did not get this investigation done.
Only 13 cases went for clinical breast examination (CBE) before their diagnosis, while only three among controls went for CBE. This reflects that negligible numbers of females go for CBE until they suspect any lump even in high-risk group probably due to shyness, lack of awareness, and primary prevention.
Evaluation of risk factors
Table 2 shows the relative risk of breast cancer associated with various risk factors on univariate analysis. Late age at first childbirth is the strongest and statistically most significant risk factor associated with breast cancer risk, with relative risk more than six times (odds ratio [OR] = 6.34, 95% confidence interval [CI] = 2.04–27), followed by alcohol intake, which is associated with 4.2 times the risk (OR = 4.2, 95% CI = 1–28.7), and also, early age of menarche, which is associated with more than two times the risk (OR = 2.83, 95% CI = 1.02–7.86).
Table 2.
Univariate analysis of risk factors of breast cancer
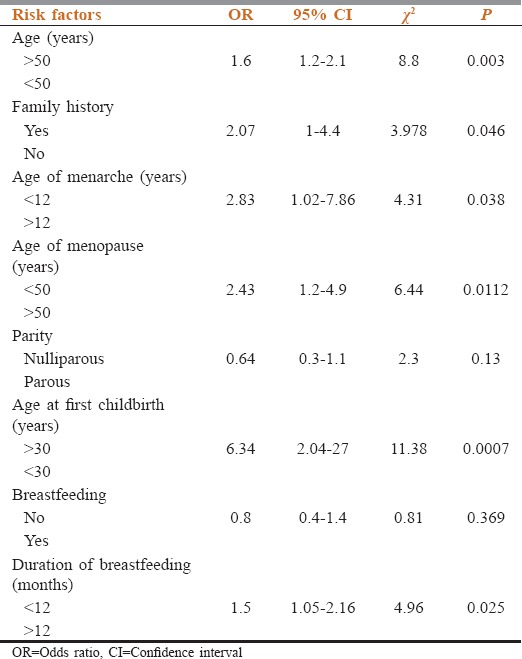
The other identifiable risk factors which proved to be statistically significant on univariate analysis are late age of menopause (OR = 2.43, 95% CI = 1.2–4.9), positive family history (OR = 2.07, 95% CI = 1–4.4), nonvegetarian diet (OR = 1.6, 95% CI = 1.2–2.2), high socioeconomic status (SES) (OR = 1.6, 95% CI = 1.2–2.2), older age (OR = 1.6, 95% CI = 1.2–2.1), and lesser duration of breastfeeding (OR = 1.5, 95% CI = 1.05–2.16).
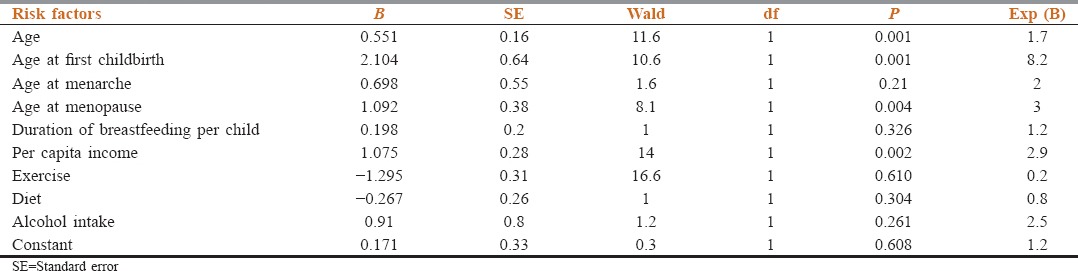
The risk factors which were found to be statistically significant on univariate analysis were evaluated by the multiple logistic regression analysis to identify the most potential risk factors after removing the confounding effect of various factors.
The final model of multiple logistic regression analysis [Table 3] identified four important risk factors, which have strong association with the ultimate development of invasive breast cancer. These factors are late age at first childbirth (>30 years), which is the strongest risk factor associated, with risk more than eight times as compared to other factors, late age of menopause (>50 years), having three times more risk as compared to other factors, high socioeconomic class, associated with around three times more risk, and age of the female more than 50 years, which was associated with a risk 1.7 times more as compared to other risk factors. All these factors seem to have an important influence on the outcome of breast cancer in our society.
Table 3.
Multiple logistic regression analysis of the risk factors associated with carcinoma breast
The mean age of cases is 51.1 ± 10.34 years. The risk of breast cancer increases with increasing age. The OR of breast cancer risk is 1.39 in patients with age 40–50 years, as compared to those with age <40 years. In addition, the risk of breast cancer is two times more in patients with age more than 50 years as compared to those with age <40 years. This test of association is highly significant with P = 0.001.
The socioeconomic class is taken according to the modified Prasad's classification, 2013.[3] Socioeconomic Class I is taken as reference for the test of association. As the socioeconomic class increases, the risk of breast cancer increases. The risk of cancer was found to be maximum in Class III and Class II.
This study depicts that there was no association of breast cancer with nulliparity as compared to parous women with OR of 0.64 (95% CI = 0.3–1.1). Further, there was no association of developing cancer with fewer number of childbirth as compared to number of children more than 3 (OR = 0.86; 95% CI = 0.64–1.25).
No association was found between not breastfeeding and breast cancer risk, OR = 0.8 (95% CI = 0.4–1.4). Our study results did not find any positive association between OCP use and the risk of breast cancer. The role of OCP as a risk factor is controversial with varying results in different studies. In our study, it shows a protective effect on univariate analysis, OR = 0.8 (95% CI = 0.3–1.7), but an insignificant P value (0.54).
Discussion
Four important risk factors were identified to have a significant association with the development of breast cancer in the Himalayan population:
Age >50 years
Late age of menopause (>50 years)
Late age at first childbirth(>30 years)
High SES.
Age is the strongest proven risk factor after female gender. In our females also, age was found to be a significant risk factor in univariate analysis as well as the multiple logistic regression analysis. The mean age of cases was 51.1 ± 10.34 years. As per the Chi-square for linear trend, the risk of breast cancer increases with increasing age.
Late age of menopause is one of the strongest risk factors identified in this study. This is consistent with many studies which establish late menopause as a risk factor.[4,5] Association of reproductive factors and breast cancer is related to the effect of ovarian hormones, which start at the age of puberty, continue with monthly cycles, are influenced by the number of pregnancies, and decrease at menopause.[6] In India, the median age of natural menopause is considerably earlier at 44 years, while women in the USA report an average age at menopause of >55 years. We can thus suggest that increasing incidence in our region can be attributed to delayed menopause due to urbanization of lifestyle and dietary factors.
Early menarche is an established risk factor.[7,8] In our evaluation, it appears to be a significant risk factor on univariate analysis, but it has not been found as a statistically significant risk factor on multivariate analysis.
Late age at first childbirth is another attributable risk factor. An international collaborative study[6] of breast cancer has been carried out in seven areas of the world. In all areas studied, a striking association between the age at first childbirth and breast cancer risk was observed. In our population, relative risk was found >6 times in females with first childbirth after 30 years of age. Hormonal stimulation of the breast tissue during pregnancy can often promote proliferation of the transformed cells. The protective effect of early full-term pregnancy is probably related to the prevention of tumor initiation.
Getting married and bearing children are a tradition in Indian culture in contrast to Western population where nulliparity is more common. With increasing urbanization, late age at first childbirth is becoming a trend in educated Himachali females, but nulliparity is not common here.[2] Thus, nulliparity which is considered to be an important risk factor in Western population is not a risk factor in this Himalayan population.
It has been seen that breast cancer is more common in females with high SES.[9,10] This has an indirect association as important risk factors such as nulliparity, late age at first birth, and late age at menopause may be partially responsible for this positive association because these characteristics are more prevalent in women of high-income groups. Furthermore, sedentary lifestyle and high-fat diet including nonvegetarian diet are more common in high SES, which directly or indirectly influences body habitus and menstrual characteristics of a female.
In Himachal, the high-income families are mainly those who are orchardists with high per capita income (PCI). Although SES is usually measured by the highest level of education, occupational history, and PCI, we have taken PCI as a measure of SES. We conclude that females belonging to high-income families are identified as a risk group in our population. In addition, pesticide use is very common in apple orchards, so these females also have a history of comparatively higher exposure to organophosphorus compounds (insecticides) which also has to be taken into account. Although none of the currently available studies clearly implicate such an exposure as a risk factor, it is only a hypothesis and our study did not address the specific question of exposure to such chemicals.
Other factors, which have shown to play an important role in other studies conducted on Western females, such as lack of breastfeeding, family history, previous radiation exposure, nulliparity, and obesity, are not common among Himalayan females. The absence of not breastfeeding as a risk factor in this study may be related to the frequent breastfeeding practiced by most women as a tradition in India.
Obese women are high-risk group and more likely to have large tumors, greater lymph node involvement, and poorer breast cancer prognosis. In our population, although regular exercise is not a trend, most of the women do daily outdoor work, being in a rural setting. Therefore, most women have body mass index within a normal range in contrast to the Western population.
We did not find any statistically significant association of OCP use and hormone replacement therapy (HRT) with breast cancer. Instead of OCPs, barrier methods are common as a method of contraception. Our finding is consistent with the study by Women's Contraceptive and Reproductive Experiences.[11] None of the women in our study population were taking or ever had used HRT in the past. This is probably because females in our setup accept postmenopausal symptoms and are shy of presenting these symptoms to the doctor.
Thus, we can infer that elderly women belonging to high-income group with late age of menopause and bearing children at a later age are found to be at higher risk for breast cancer in this Himalayan population as compared to others. All these factors, except for age, are directly or indirectly related to the urbanization of lifestyle.
The percentage share of urban population in Himachal has been increasing continuously over the years with figures of 7.61% in 1981, 8.69% in 1991, 9.80% in 2001, and 10.03% in 2011 census.[12] From these data, we may attribute the rising incidence of breast cancer in our population to urbanization.
Conclusion
Every woman wants to know what she can do to lower her risk of breast cancer. Age >50 years, late age of menopause (>50 years), late age at first childbirth (>30 years), and high SES were found to be major risk factors in our females. In addition, association of breast cancer with insecticide exposure has been observed and more studies are needed on this aspect to come to a definite conclusion. When compared to Western data from various studies,[7,8] we can say that positive family history, nulliparity, hormonal replacement therapy, previous radiation exposure, early menarche, HRT, obesity, and alcohol intake, which are significant risk factors identified in Western women, are not important for the population in our Western Himalayan state; however, with the urbanization and increasing literacy rate, more of our females are marrying late and bearing children at a later age,[2] being busy with their careers. Furthermore, the factors causing increase in the age of menopause need to be studied. We need to identify these changing aspects in reproductive and lifestyle patterns and thus making women aware of the importance of early childbearing, which can lower their risk of breast cancer.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kim Y, Yoo KY, Goodman MT. Differences in incidence, mortality and survival of breast cancer by regions and countries in Asia and contributing factors. Asian Pac J Cancer Prev. 2015;16:2857–70. doi: 10.7314/apjcp.2015.16.7.2857. [DOI] [PubMed] [Google Scholar]
- 2.International Institute for Population Sciences (IIPS) and ORC Macro. National Family Health Survey (NFHS-2), India, 1998-99. Himachal Pradesh, Mumbai: IIPS; 2002. [Google Scholar]
- 3.Dudala SR, Arlappa N. An updated Prasad's socio economic status classification for 2013. Int J Res Dev Health. 2013;1:26–8. [Google Scholar]
- 4.Lacey JV, Jr, Kreimer AR, Buys SS, Marcus PM, Chang SC, Leitzmann MF, et al. Breast cancer epidemiology according to recognized breast cancer risk factors in the Prostate, Lung, Colorectal and Ovarian (PLCO) cancer screening trial cohort. BMC Cancer. 2009;9:84. doi: 10.1186/1471-2407-9-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Colditz GA, Rosner B. Cumulative risk of breast cancer to age 70 years according to risk factor status: Data from the Nurses’ Health Study. Am J Epidemiol. 2000;152:950–64. doi: 10.1093/aje/152.10.950. [DOI] [PubMed] [Google Scholar]
- 6.MacMahon B, Cole P, Lin TM, Lowe CR, Mirra AP, Ravnihar B, et al. Age at first birth and breast cancer risk. Bull World Health Organ. 1970;43:209–21. [PMC free article] [PubMed] [Google Scholar]
- 7.Brinton LA, Sherman ME, Carreon JD, Anderson WF. Recent trends in breast cancer among younger women in the United States. J Natl Cancer Inst. 2008;100:1643–8. doi: 10.1093/jnci/djn344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson WF, Matsuno RK, Sherman ME, Lissowska J, Gail MH, Brinton LA, et al. Estimating age-specific breast cancer risks: A descriptive tool to identify age interactions. Cancer Causes Control. 2007;18:439–47. doi: 10.1007/s10552-006-0092-9. [DOI] [PubMed] [Google Scholar]
- 9.Wagener DK, Schatzkin A. Temporal trends in the socioeconomic gradient for breast cancer mortality among US women. Am J Public Health. 1994;84:1003–6. doi: 10.2105/ajph.84.6.1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lawson JS. The link between socioeconomic status and breast cancer – A possible explanation. Scand J Public Health. 1999;27:203–5. [PubMed] [Google Scholar]
- 11.Marchbanks PA, Mcdonald JA, Wilson HG, Burnett NM, Daling JR, Bernstein L, et al. The NICHD Women's Contraceptive And Reproductive Experiences Study: Methods and operational results. Ann Epidemiol. 2002;12:213–21. doi: 10.1016/s1047-2797(01)00274-5. [DOI] [PubMed] [Google Scholar]
- 12.Department of Economics and Statistics, Himachal Pradesh. Socio Economic Indicators of Himachal Pradesh. 2013. [Last cited on 2016 Sep 28]. Available from: http://www.admis.hp.nic.in/himachal/economics/REPORTS/Socio2013_A1b .


