Abstract
Background:
To evaluate the feasibility and clinical preliminary results of weekly cisplatin and volumetric-modulated arc therapy to the pelvis with simultaneous integrated boost to macroscopic disease in a cohort of elderly patients.
Materials and Methods:
Inclusion criteria of this prospective study were age ≥70 years, Karnofsky performance status 70 to 100, locally advanced histologically proven squamous cervical carcinoma, and patients unable to undergo brachytherapy. Radiation doses prescribed were 66 Gy to the macroscopic disease and 54 Gy to the pelvic nodes in 30 fractions. Weekly cisplatin dose was 40 mg/mq.
Results:
A total of 30 patients were recruited. Median follow-up was 32 months (range: 8-48 months). Median age was 72 years (range: 70-84 years). The 3-year overall survival and local control were 93% and 80%, respectively. The median time to progression was 24 months (range: 6-30 months). Analyzing clinical outcome grouping based on the stage of disease, II versus III, the 3-year overall survival was 100% and 85%, respectively. The 3-year local control was 91% for stage II and 67% for stage III. Acute and late toxicities were acceptable without severe events.
Conclusion:
Weekly cisplatin and volumetric-modulated arc therapy–simultaneous integrated boost for radical treatment of advanced cervical cancer in the current cohort of elderly patients were feasible. Long-term results and prospective randomized trials are advocated.
Keywords: advanced cervical cancer, VMAT, elderly patients, gynecological malignancies
Introduction
In patients affected by locally advanced cervical carcinoma, definitive chemoradiotherapy (ChT-RT) guarantees long-term local control (LC) rates ranging between 88% and 95% for stage IB, 70% and 80% for stage II, and 30% and 40% for stage III. The combination of external beam radiotherapy (EBRT) and brachytherapy (BRT) represents the mainstay in the primary treatment of patients with cervical cancer.1–3 Unfortunately, compared to EBRT, BRT is less widespread in radiation departments. Additionally, some criticisms are related to the feasibility of BRT, including: (1) a long learning curve for radiation oncologist,4 (2) some patients eligible to radiotherapy (RT) are not able to receive BRT for some contraindications to invasive procedures, and (3) some patients refuse to move in other RT facilities for logistic problems (especially elderly patients). Thus, in all these cases, an alternative RT option should be offered. Several authors have already investigated the use of different EBRT techniques as a reasonable option after EBRT to the pelvis when BRT was not feasible.5–7 Volumetric-modulated arc therapy (VMAT) showed a great potential for highly conformal dose to target volume, maintaining a low–moderate toxicity profile in pelvic irradiation.8,9
The aim of the present study was to evaluate the feasibility and clinical preliminary results of weekly cisplatin and VMAT to the pelvis with simultaneous integrated boost (SIB) to macroscopic disease in a cohort of elderly patients.
Materials and Methods
In our institution, a prospective study was approved by the internal review board (RT-02/2011). Inclusion criteria were age ≥70 years old, Karnofsky performance status of 70 to 100, locally advanced histologically proven squamous cervical carcinoma, patients refusing BRT or not suitable to invasive treatment procedures due to comorbidities, and a signed specific informed consent.
All patients recruited in the study accepted the RT protocol proposed: a dose of 66 Gy to the macroscopic disease and 54 Gy to the pelvis in 30 fractions with SIB-VMAT technique. According to the study protocol, all patients were staged with gynecologic examination, pelvic magnetic resonance imaging (MRI) with contrast, and 18fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) before treatment. The stage system used was the International Federation of Gynecology and Obstetrics 2009 criteria. Clinical outcomes and toxicity data according to the Common Terminology Criteria for Adverse Events (CTCAE version 4.0) were collected prospectively.
Treatment Procedure
After patient immobilization in supine position by Combifix frame (Civco Inc., Orange City, Iowa, US), CT planning of abdomen–pelvis (3-mm-thickness slice) without intravenous contrast media was performed. The lower limit of the scanned area was set to 2 cm below the lower limit of the lesser trochanter, and the upper limit was the L2-L3 interspace. Patients were simulated and treated with full bladder: they were asked to drink 500 mL of water 30 minutes before CT planning and before each treatment session. If the rectum was abnormally full or distended, CTs were carried out following enema. The 18FDG PET/CT and MRIs were merged separately with the CT planning to define the clinical target volume-SIB (CTV-SIB), using intermediate/high signal seen on T2-weighted MRIs and including the hypermetabolic areas of 18FDG PET/CT (primary tumor or pelvic nodes). The planning target volume-SIB (PTV-SIB) was generated using a 5-mm isotropic expansion on CTV-SIB. A total dose of 66 Gy in 30 fractions was prescribed to PTV-SIB.
According to consensus guidelines for the delineation of CTV for intensity-modulated pelvic RT in the treatment of cervix cancer,10 CTV was defined including (1) CTV-SIB; (2) cervix, if not already included within CTV-SIB contour; (3) uterus, parametrium, including ovaries; (4) the entire mesorectum if uterosacral ligament was involved; (5) the upper two-thirds of the vagina; and (6) locoregional lymph nodes: common, internal, and external iliac, obturator, and presacral. Isotropic CTV to PTV margins of 8 mm to primary tumor (cervical cancer region) and 7 mm to nodal region were adopted. A total dose of 54 Gy in 30 fractions was prescribed to PTV. Organs at risk (OARs) were bladder, bowel defined as intestinal cavity, rectum, and femoral heads. Radiotherapy was delivered 1 fraction/d for 5 d/wk. Before each daily session, patients were submitted to an image-guided radiotherapy (IGRT) procedure by means of a daily kV cone-beam CT (CBCT) to check and to correct setup errors. Radiotherapy was delivered concomitantly with the administration of weekly cisplatin 40 mg/mq, if no individual contraindications (neutrophil count <1.5 × 109/L and/or a platelet count <100 × 109/L and/or hemoglobin level ≤110 g/L and/or serum creatinine >140 µm/L).
Planning Objectives
RapidArc (Varian Inc, Palo Alto, California) VMAT treatments by two 360° arcs with 6-MV photon beams from a Trilogy (Varian Inc) linac were optimized by PRO (version 10.0.28; Varian Inc) algorithm. Necessary constraints for planning approval in terms of target dose coverage were a PTV volume ≥95% receiving a dose ≥95% of the prescribed dose for both PTV and PTV-SIB and a near-maximum dose to PTV-SIB not >70.6 Gy. The near-maximum dose to PTV was minimized while giving priority to PTV-SIB dose coverage.
The following OARs constraints were adopted: maximum dose to 1 mL (Dmax) of the rectum, bladder, and intestinal cavity ≤66 Gy; Dmax ≤50 Gy for femoral heads; V46.5 Gy < 50% and V64.5 Gy < 15% for rectum; V46.5 Gy < 50% and V64.5 Gy < 20% for bladder; and V40 Gy < 30% for intestinal cavity.
Dose calculation was then performed by AAATM (version 10.0.28; Varian Inc) algorithm, using a dose calculation grid size equal to 2 mm and by including CT-based heterogeneity corrections.
Follow-Up
During RT, physical examination and complete blood count were performed weekly. Gynecological examination including Pap-test was usually performed every 3 to 4 months for the first 2 years, every 6 months for the next 3 years. The 18FDG PET/CT and pelvic MRI were performed during the first year after RT. From the second year after RT, CT scan or 18FDG PET/CT was performed when clinically indicated.
Complete response (CR) was defined as the disappearance of the lesions at imaging; a reduction more than 30% was considered partial remission; no modification was considered stable disease; and any growing lesion not imputable clearly to fibrosis was reported as progression of disease, according to Response Evaluation Criteria in Solid Tumors.11 Reduced metabolic activity was evaluated based on decreases in Standardized Uptake Value (SUV) from pre- to posttreatment and on the SUV measurements obtained in each 18FDG PET/CT examination. A complete metabolic response was defined as the complete normalization of SUV in the target lesions, with mean lesion SUV being similar to that of the surrounding tissue. Progressive metabolic disease was defined as an increase of at least 30% in the mean SUV of target lesions. A reduction of at least 30% in the mean SUV of target lesions was considered a partial metabolic response, whereas an increase or decrease in SUV that did not exceed 30% was indicative of stable metabolic disease.12
Statistical Analyses
Local control and overall survival (OS) rates were estimated using the Kaplan-Meier method. Local control was defined from the beginning of the treatment to the locoregional relapse date. Local recurrence was defined as any relapse in the field (pelvis or cervix). Time to progression (TTP) was considered from the beginning of the treatment to the time of any recurrence or distant metastasis. The OS was calculated from the date of diagnosis to the death or last follow-up date. Statistical analyses were carried out using R-software 3.1.2 version.
Results
From September 2011 to April 2015, 30 patients affected by histologically proven squamous cervical carcinoma were recruited in the protocol. The median follow-up was 32 months (range: 8-50 months). The median age was 72 years (range: 70-84 years). The Karnofsky performance status ranged between 80 and 100. No patient interrupted the RT course. Conversely, in 5 patients, weekly cisplatin was not administered as programmed in the protocol (in 3 cases for age ≥80 years, in 1 case for renal dysfunction pretreatment, and in 1 case for renal dysfunction during treatment). Patients’ baseline characteristics are detailed in Table 1.
Table 1.
Patients Baseline Characteristics.
| Parameters | No. (%) |
|---|---|
| Diabetes | 10 (33) |
| Hypertension | 12 (36) |
| Reasons for omission of brachytherapy | |
| Patents refusal (for logistic problems to move in other RT facilities or because of virginity) | 25 (83) |
| Vaginal stenosis | 5 (17) |
| Histology | |
| Squamous cell carcinoma | 30 (100) |
| Grading | |
| G1 | 3 (10) |
| G2 | 18 (60) |
| G3 | 9 (30) |
| FIGO 2009 stage | |
| II | 16 (53) |
| III | 14 (47) |
| Pelvic nodes statusa | |
| Positive | 8 (27) |
| Negative | 22 (73) |
| Weekly cisplatin | 25 (83) |
| Median overall treatment time, days | 42 (range: 42-44) |
Abbreviations: FIGO, International Federation of Gynecology and Obstetrics; FDG, fluorodeoxyglucose; MRI, magnetic resonance imaging; PET, positron emission tomography.
aAt imaging (MRI and/or 18FDG-PET-scan).
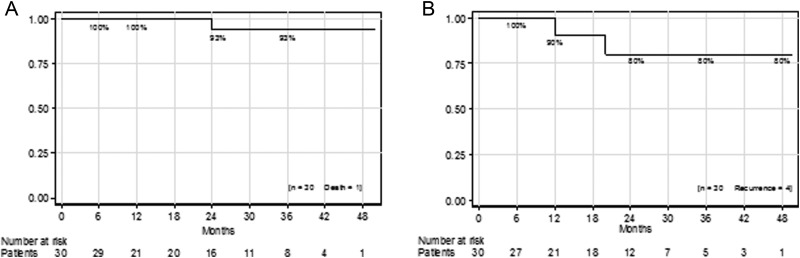
At the time of the analysis, the 3-year OS and LC were 93% and 80%, respectively (Figure 1). Only 1 cancer-related death was recorded in a patient with a stage III disease. Four recurrences in cervix were observed in 3 cases of stage III group and in 1 case of stage II group.
Figure 1.
Kaplan-Meier curves for the population of the study: (A) overall survival, (B) local control.
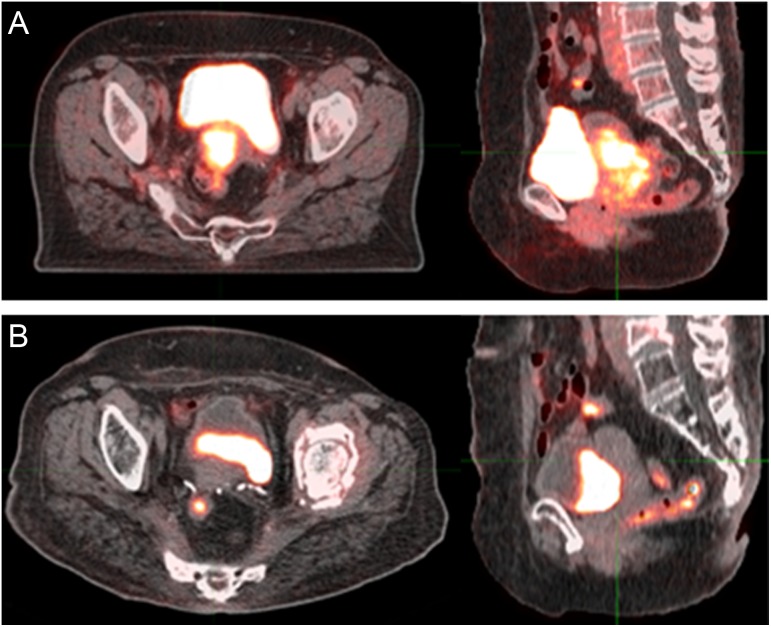
The probabilities of local failure at 1, 2, and 3 years were 6.7%, 13.3%, and 13.3%, respectively. The probabilities of distant progression at 2 and 3 years were 13.3% and 16.7%, respectively. The median TTP was 24 months (range: 6-30 months). Sites of distant metastases were liver (in 2 cases of stage III group), lung (in 1 case of stage III group), and abdomen nodes (in 2 cases of stage II group). One patient with abdomen node metastases was not a candidate to concomitant cisplatin for advanced age (>80 years); in a patient with liver metastases, cisplatin was interrupted after 2 cycles for renal dysfunction. Figure 2 shows an example of durable CR at 18FDG PET/CT.
Figure 2.
An example of complete response at 18FDG PET/CT during follow-up: (A) pretherapy, (B) posttherapy. FDG, 18-fluorodeoxyglucose positron emission tomography–computed tomography.
Analyzing clinical outcomes grouping based on the stage of disease, stage II versus stage III, the 3-year OS was 100% and 85%, respectively. The 3-year LC was 91% for stage II and 67% for stage III (Figure 3). Toxicity was registered in all cases. Table 2 reports acute/late adverse events recorded, according to CTCAE version 4.0. Organs at risk constraints were respected in the majority of cases.
Figure 3.
Kaplan-Meier curves grouping based on stage of disease II versus III: (A) overall survival, (b) local control.
Table 2.
Acute and Late Adverse Events, According to Common Terminology Criteria for Adverse Events version 4.0 (CTCAE).
| Toxicity | Acute No. Patients (%) | Late No. Patients (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| G0 | G1 | G2 | G3 | G4 | G0 | G1 | G2 | G3 | G4 | |
| Gastrointestinal | 9 (30) | 8 (27) | 13 (43) | - | - | 21 (70) | 9 (30) | - | - | - |
| Urinary | 7 (23) | 12 (40) | 11 (37) | - | - | 27 (90) | 3 (10) | - | - | - |
| Vaginal | 1 (7) | 19 (63) | 10 (30) | - | - | 23 (77) | 7 (23) | - | - | - |
| Rectal | 14 (47) | 9 (30) | 7 (23) | - | - | 22 (73) | 6 (20) | 2 (7) | - | - |
| Hematologic | 20 (70) | 10 (30) | - | - | - | 26 (87) | 4 (13) | - | - | - |
Discussion
In locally advanced cervical cancer, BRT in combination with pelvic EBRT allows to deliver high doses to target volume while sparing bladder and rectum, reaching very encouraging clinical outcomes and minimizing the risk of serious adverse events.2,3 In the past years, the possibility to omit BRT in this setting of disease, delivering the entire treatment course with EBRT alone, has been explored with poor outcomes.13 Recent advances in EBRT are facing the inevitable question whether the intensity-modulated techniques could represent a potential alternative to BRT in the management of cervical cancer. Volumetric-modulated arc therapy, a rotational intensity-modulated RT (IMRT), potentially offers an optimal conformal dose to the target with improved homogeneity and conformity in several settings, including pelvis.14,15 The VMAT planning studies showed a short delivery time that could reduce the intrafraction uncertainties and a satisfactory OARs sparing, with an average 12% integral dose reduced to healthy tissues.9,16 To date, the general consensus is that the intensity-modulated techniques will not replace the role of BRT in cervical cancer due to the clear advantages of BRT in terms of organ immobilization with steep dose gradients and highly conformal dose distribution. However, the American Brachytherapy Society Gynecologic Cervical Cancer Task group has developed general criteria for the management of cervical cancer.17 There are situations in which BRT cannot be feasible, such as prior RT with BRT and life expectancy <6 months.
The present study was designed to evaluate an alternative option for patients who refused or were not able to receive BRT (most of them due to logistic problems to move in other distant RT facilities or because of virginity or because of vaginal stenosis). Generally, in many countries, due to the few centers with expertise in BRT, patients are generally sent to a reference center for BRT boost after external IMRT/3-dimensional (3D) EBRT, and this is our policy. Patients eligible for the current study were not candidate to BRT for the reasons detailed in Table 1. To our knowledge, this is the first report for elderly patients affected by locally advanced cervical cancer in terms of RT technique and adopted schedule. The findings of the present analysis appear promising in terms of preliminary clinical outcomes and tolerability. Thus, the current schedule of weekly cisplatin and VMAT-SIB for the radical treatment of advanced cervical cancer could be a viable therapeutic option in the elderly setting, here defined as age ≥70 years. In fact, in the population of study, the 3-year OS and LC were 93% and 80%, respectively. Although the data are preliminary, these results seem to be unexpected when compared to what is suggested in the literature.2,3 In fact, it is well known that in the treatment of cervical cancer, the LC rates are related to the biologically equivalent dose: high doses (80-95 Gy to the primary tumor) administered over a short time (inferior to 50-55 days) significantly impact on LC and OS.
The rationale to deliver the here reported radiation doses derives from the assessment that in the radical treatment of squamous cell carcinoma in other anatomic district, for example, in head and neck, 66 Gy in 30 fractions represents an effective schedule of radical RT.18 Moreover, the SIB approach, adopted to irradiate a prophylactic volume with conventional daily fractions while simultaneously treating the primary tumor or positive pelvic lymph nodes with a higher dose per fraction, reduces the overall treatment time. Hypothetically, this latter aspect could have a potential effect on cellular repopulation. Preclinical data suggest that modest increase in fraction size improves the cells killing in patients having cervical cancer treated with concurrent ChT-RT.19 The choice of isotropic CTV to PTV margins of 8 mm to primary tumor (cervical cancer region) was related to the daily IGRT procedure by means of daily kV-CBCT to check and to correct setup errors. A recent study, designed to analyze the nature and extent of the intrafraction motion of the cervix–uterus and, thus, their contributions to the CTV to PTV margins, estimated that the mean intrafraction cervix–uterus displacements were up to 5.8 mm posteriorly and up to 4.9 mm cranially.20 Additionally, a uniform 3D PTV expansion of 7 mm is recommended for the lymph node areas.21 Concerning concomitant chemotherapy, weekly single-agent cisplatin at 40 mg/mq during EBRT has been widely used to enhance the effect of RT.1
Interestingly, in the present study, analyzing clinical outcomes grouping based on the stage of disease, the 3-year LC was not satisfactory for stage III comparing to stage II (67% vs 91%, respectively), suggesting that in this cohort of elderly patients, stage II was the category of risk that has really benefited this approach. Conversely, in patients with stage III, clinical outcomes could be most dependent on higher-dose effect. However, the absence of pelvic nodal recurrences in both stages could be a strength of the study, suggesting that an higher dose to nodes PET positive by means of SIB approach could be an effective strategy. Currently, 18FDG PET/CT is commonly used to detect lymph node involvement and/or distant metastasis in patients affected by cervical cancer due to its accuracy and sensitivity for initial staging.22 High radiation dose to 18FDG PET/CT pelvic-positive nodes by means of intensity-modulated technique is a feasible treatment with a potential improvement of locoregional control in cervical cancer.23
Several shortcomings remain unresolved in the present study: (1) whether the doses adopted are high enough to allow a durable LC rate, at least for stage II. Since the biological total dose of the explored RT schedule remains lower than that obtained with BRT, the risk of local relapse beyond the median follow-up of 32 months remains; (2) whether the more homogeneous dose distributions achieved with VMAT are as effective as the inhomogeneous ones produced by BRT; and (3) the limited sample size, although it is difficult to recruit many patients ≥70 years refusing BRT in a single center, because BRT represents the standard of care that we daily recommend in this setting of disease.
Conclusion
Weekly cisplatin and VMAT-SIB for radical treatment of advanced cervical cancer in the current cohort of elderly patients was feasible. Long-term results and prospective randomized trials are advocated.
Abbreviations
- BRT
brachytherapy
- CBCT
cone-beam computed tomography
- ChT-RT
chemo-radiotherapy
- CR
complete response
- CT
computed tomography
- CTCAE
Common Terminology Criteria for Adverse Events
- CTV
clinical target volume
- EBRT
external beam radiotherapy
- FDG
fluorodeoxyglucose
- IGRT
image-guided radiotherapy
- IMRT
intensity-modulated radiotherapy
- LC
local control
- MRI
magnetic resonance imaging
- OARs
organs at risk
- OS
overall survival
- PET
positron emission tomography
- PTV
planning target volume
- RT
radiotherapy
- SIB
simultaneous integrated boost
- TTP
time to progression
- VMAT
volumetric-modulated arc therapy
Footnotes
Authors’ Note: The current study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All persons gave their informed consent prior to their inclusion in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article..
References
- 1. Colombo N, Carinelli S, Colombo A, et al. Cervical cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23(suppl 7):vii27–vii32. [DOI] [PubMed] [Google Scholar]
- 2. Barillot I, Horiot JC, Pigneux J, et al. Carcinoma of the intact uterine cervix treated with radiotherapy alone: a French cooperative study: update and multivariate analysis of prognostics factors. Int J Radiat Oncol Biol Phys. 1997;38(5):969–978. [DOI] [PubMed] [Google Scholar]
- 3. Perez CA, Grigsby PW, Chao KS, Mutch DG, Lockett MA. Tumor size, irradiation dose, and long-term outcome of carcinoma of uterine cervix. Int J Radiat Oncol Biol Phys. 1998;41(2):307–317. [DOI] [PubMed] [Google Scholar]
- 4. Mahantshetty U, Shrivastava S, Kalyani N, Banerjee S, Engineer R, Chopra S. Template-based high-dose-rate interstitial brachytherapy in gynecologic cancers: a single institutional experience. Brachytherapy. 2014;13(4):337–342. [DOI] [PubMed] [Google Scholar]
- 5. Barraclough LH, Swindell R, Livsey JE, Hunter RD, Davidson SE. External beam boost for cancer of the cervix uteri when intracavitary therapy cannot be performed. Int J Radiat Oncol Biol Phys. 2008;71(3):772–778. [DOI] [PubMed] [Google Scholar]
- 6. Alongi F, Mazzola R, Ricchetti F, et al. Volumetric-modulated arc therapy with vaginal cuff simultaneous integrated boost as an alternative to brachytherapy in adjuvant irradiation for endometrial cancer: a prospective study. Anticancer Res. 2015;35(4):2149–2155. [PubMed] [Google Scholar]
- 7. Macchia G, Cilla S, Morganti AG, et al. Adjuvant volumetric-modulated arc therapy with simultaneous integrated boost in endometrial cancer. Planning and toxicity comparison. Acta Oncol. 2014;53(2):251–258. [DOI] [PubMed] [Google Scholar]
- 8. Mazzola R, Fersino S, Fiorentino A, et al. The impact of prostate gland dimension in genitourinary toxicity after definitive prostate cancer treatment with moderate hypofractionation and volumetric modulated arc radiation therapy. Clin Transl Oncol. 2016;18(3):317–321. [DOI] [PubMed] [Google Scholar]
- 9. Cozzi L, Dinshaw KA, Shrivastava SK, et al. A treatment planning study comparing volumetric arc modulation with RapidArc and fixed field IMRT for cervix uteri radiotherapy. Radiother Oncol. 2008;89(2):180–191. [DOI] [PubMed] [Google Scholar]
- 10. Lim K, Small W, Jr, Portelance L, et al. Consensus guidelines for delineation of clinical target volume for intensity-modulated pelvic radiotherapy for the definitive treatment of cervix cancer. Int J Radiat Oncol Biol Phys. 2011;79(2):348–355. [DOI] [PubMed] [Google Scholar]
- 11. Eisenhauera EA, Therasseb P, Bogaertsc J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–247. [DOI] [PubMed] [Google Scholar]
- 12. Martins EB, Chojniak R, Kowalski LP, Nicolau UR, Lima EN, Bitencourt AG. Diffusion-weighted MRI in the assessment of early treatment response in patients with squamous-cell carcinoma of the head and neck: comparison with morphological and PET/CT findings. PLoS One. 2015;10(11):e0140009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ulmer HU, Frischbier HJ. Treatment of advanced cancers of the cervix uteri with external irradiation alone. Int J Radiat Oncol Biol Phys. 1983;9(6):809–812. [DOI] [PubMed] [Google Scholar]
- 14. Alongi F, Cozzi L, Fogliata A, et al. Hypofractionation with VMAT versus 3DCRT in post-operative patients with prostate cancer. Anticancer Res. 2013;33(10):4537–4543. [PubMed] [Google Scholar]
- 15. Alongi F, Fogliata A, Clerici E, et al. Volumetric modulated arc therapy with flattening filter free beams for isolated abdominal/pelvic lymph nodes: report of dosimetric and early clinical results in oligometastatic patients. Radiat Oncol. 2012;7:204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Otto K. Volumetric modulated arc therapy: IMRT in a single gantry arc. Med Phys. 2008;35(1):310–316. [DOI] [PubMed] [Google Scholar]
- 17. Viswanathan AN, Thomadsen B; American Brachytherapy Society Cervical Cancer Recommendations Committee; American Brachytherapy Society. American Brachytherapy Society consensus guidelines for locally advanced carcinoma of the cervix. Part I: general principles. Brachytherapy. 2012;11(1):33–46. [DOI] [PubMed] [Google Scholar]
- 18. Merlotti A, Alterio D, Vigna-Taglianti R, et al. Italian Association of Radiation Oncology. Technical guidelines for head and neck cancer IMRT on behalf of the Italian association of radiation oncology—head and neck working group. Radiat Oncol. 2014;9:264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kavanagh BD, Schefter TE, Wu Q, et al. application of intensity-modulated radiotherapy for locally advanced cervical cancer. Semin Radiat Oncol. 2002;12(3):260–271. [DOI] [PubMed] [Google Scholar]
- 20. Heijkoop ST, Langerak TR, Quint S, et al. Quantification of intra-fraction changes during radiotherapy of cervical cancer assessed with pre- and post-fraction cone beam CT scans. Radiother Oncol. 2015;117(3):536–541. [DOI] [PubMed] [Google Scholar]
- 21. Small W, Jr, Mell LK, Anderson P, et al. Consensus guidelines for delineation of clinical target volume for intensity-modulated pelvic radiotherapy in postoperative treatment of endometrial and cervical cancer. Int J Radiat Oncol Biol Phys. 2008;71(2):428–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wong TZ, Jones EL, Coleman RE. Positron emission tomography with 2-deoxy-2-[(18)F]fluoro-D-glucose for evaluating local and distant disease in patients with cervical cancer. Mol Imaging Biol. 2004;6(1):55–62. [DOI] [PubMed] [Google Scholar]
- 23. Cihoric N, Tsikkinis A, Tapia C, Aebersold DM, Zlobec I, Lössl K. Dose escalated intensity modulated radiotherapy in the treatment of cervical cancer. Radiat Oncol. 2015;10(1):240. [DOI] [PMC free article] [PubMed] [Google Scholar]