Abstract
Burn injuries have been more prevalent among low socioeconomic populations and in less developed regions. Incredible advances in burn care and social development over the recent decades, however, should have placed the incidence and severity of burns in a downwards trend. The aim of this review was to give an overview on current trends in burn epidemiology across the world. Also the socioeconomic development in countries that have published epidemiological data used in this study has been taken into account when comparing the results. There was a worldwide downwards trend of burn incidence, burn severity, length of hospital stay, and mortality rate. These findings were particularly pronounced in very highly developed countries. Data from highly and medium developed countries were more heterogeneous. No studies could be obtained from low developed countries. Comparisons between the different studies were compromised by the fact that studies emerged from specialized facilities on one hand and general hospitals on the other. Analyzed studies were also frequently focusing on limited patient populations such as “children” or “elderly”. Our findings indicate the need for an international burn database with a minimal data-set in order to obtain objective and comparable results in respect of burn epidemiology.
Keywords: burn injury, trend, severity, mortality, development, epidemiology
1 Introduction
Burns are devastating injuries, often resulting in significant morbidity, impairment of emotional well-being, and experienced quality of life. In addition to the stressful immediate care, burns often require long-term treatment with numerous outpatient visits (dressing changes etc.) and multiple reconstructive surgical procedures ± concomitant hospital stays. These health-related consequences of burn injuries are often accompanied with additional socioeconomic burdens for burn victims and their families [1–5].
Socioeconomic development in different countries is a continuous process affecting basically every aspect of life. Its impact on human health is evident. According to the Human Development Reports 2015, the average mortality rate between very highly and low developed countries differ by a factor 3 (57:106 and 249:291 (women:men) per 1,000 respectively), while the access to physicians per 10,000 inhabitants differ with about a factor 10 (27.9 and 2.9 physicians per 10,000 inhabitants, respectively) [6]. It is not surprising that burn injuries are also more common in populations with lower socioeconomic status and delayed developmental growth [3,7–9], e. g. a lack of basic safety education has been associated with increased risk for burn injuries [10]. Furthermore, the majority of burn injuries are preventable. Measures such as educational programs, introduction of smoke alarms/detectors, and controlled hot water in households have contributed significantly to decrease burn incidence rates and severity when applied [3,10,11].
In pace with the increasing worldwide socioeconomic development there should be a decreasing trend of burn injuries. The aim of this literature review was to assess recent developments in burn epidemiology worldwide including changes in burn incidences, injury characteristics, length of hospital stay, and mortality. A similar study, previously published, regarding developments in severe burns only evaluated European populations [12]. This review intends to provide an overview of the burn epidemiology trends on a global level.
2 Material and Methods
A systematic search was performed in PubMed (March 2nd to 10th, 2016) to retrieve the included studies. The applied search strategy included the combination of the key words: “thermal”, “injury”, “trends”, “epidemiology”, “tbsa”, “size”, “depth”, and “mortality”. For additional studies, the references of the included articles have also been hand-searched. Only original articles, covering a period of at least 5 years, published from 2001 and onwards were included. The included studies were divided into (deriving from) very highly developed (VHD), highly developed (HD), medium developed (MD), and low developed (LD) countries according to the developmental status of the country of origin based on the Human Development Index (HDI) data published in the 2015 Human Development Report. The HDI measures average achievements in three basic qualities of human development: A long and healthy life, knowledge and decent standard of living. For classification of country development the HDI is split into quartiles: VHD countries are the ones in the top quartile whereas LD countries are located in the bottom quartile [6]. If available, the overall male:female ratio was assessed. All reported p-values <0.05 were considered as statistically significant. Statistical analysis was conducted with SPSS 23.0 for Windows and the t-test was used to ascertain the statistical significance of differences of the sex ratios.
3 Results
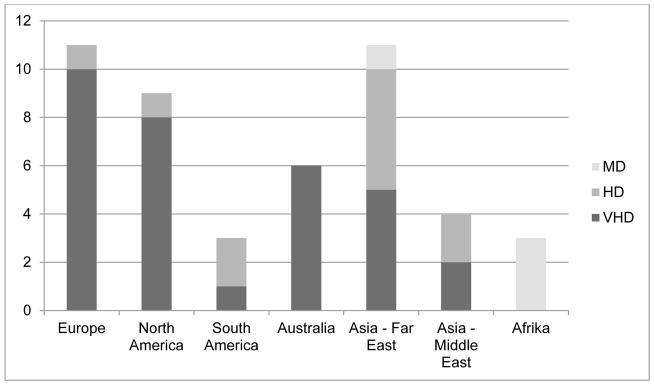
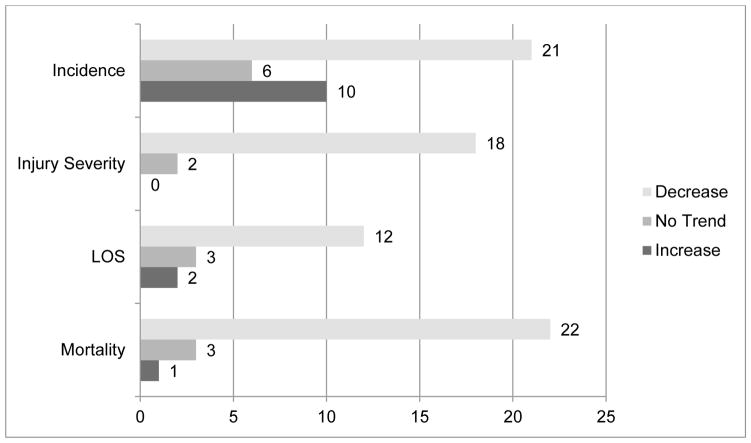
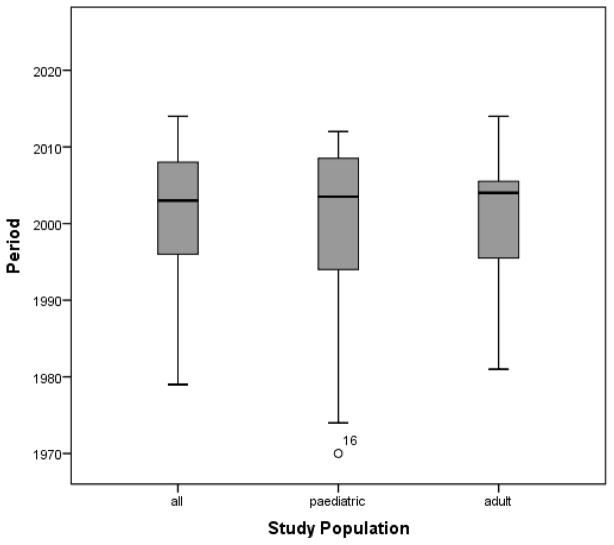
In total 46 studies were found fulfilling the inclusion criteria (Table 1). The absolute majority of studies were from VHD countries (69%, n=32). Twenty two per cent were from HD countries (n=10), only 4 (9%) studies from MD countries and no studies were available from LD countries (figure 1). There were 26 (57%) multicenter studies and 20 (43%) single-center studies. Figure 2 gives an overview on observed trends; figure 3 depicts which years were covered by the studies. Figure 4 is a political world map on which countries of which studies could be obtained are marked.
Table 1.
Studies and results;
| Study | Country | HDI | Period | Age (y) | Incidence | Severity | LOS | Mortality | M:F |
|---|---|---|---|---|---|---|---|---|---|
| Duke[25]a | Australia | VHD | 1983–2008 | all | Decline* | - | Decline | Decline | 2.1:1 |
| Duke[26]a | Australia | VHD | 1983–2008 | 0–5 | Decline | - | - | - | 1.5:1 |
| Duke[24]a | Australia | VHD | 1983–2008 | 15–29 | Decline | Decline (size) | - | - | 3.1:1 |
| Duke[23]a | Australia | VHD | 1983–2008 | ≥60 | Decline | - | Decline | Decline | 1.8:1 |
| Greenwood[13] | Australia | VHD | 1996–2004 | adult | Increase | Decline (size) | - | - | 1.8:1 |
| Pegg[14] | Australia | VHD | 1982–2002 | all | Increase | - | - | Decline | 3.8:1 |
| Trop[27] | Austria | VHD | 1988–2012 | ≤18 | Decline | Decline (depth) | Decline | Decline | 1.8:1 |
| Zayakova[15]a | Bulgaria | HD | 2002–2011 | all | Increase* | Decline* (size+depth) | Decline* | Increase | 1.4:1 |
| Burton[48]a | Canada | VHD | 1995–2004 | adult | No trend | - | No trend | - | 2.4:1 |
| Spinks[28]a | Canada | VHD | 1994–2003 | ≤19 | Decline* | - | No trend | Decline* | 2.0:1 |
| Gomez[29] | Canada | VHD | 1996–2005 | >15 | Decline | No trend (size) | - | Decline* | 2.5:1 |
| Goldsack[30] | Chile | VHD | 2001–2011 | <15 | Decline | Decline (depth) | - | - | 1.1:1 |
| Yongqiang[49] | China | HD | 2001–2005 | all | No trend | - | - | - | 3.0:1 |
| Zhu[16]a | China | HD | 2001–2010 | ≤14 | Increase* | Decline* (size) | No trend | Decline* | 1.5:1 |
| Cheng[31] | China | HD | 2000–2008 | all | Decline* | No trend (size) | No trend | No trend | 2.4:1 |
| Hai Jun[32]a | China | HD | 1970–2008 | <14 | Decline | Decline (size+depth) | Decline* | Decline | 1.7:1 |
| Celko[17]a | Czech Rep. | VHD | 1996–2006 | <15 | Increase | - | - | - | 1.8:1 |
| Ortiz-Prado[50] | Ecuador | HD | 2005–2014 | ≥16 | No trend | - | - | - | 2.3:1 |
| Laitakari[8]a | Finland | VHD | 1990–2011 | <1 | Increase | - | - | No trend | 1.5:1 |
| Theodorou[33] | Germany | VHD | 1991–2010 | all | Decline | Decline* (size) | Decline (ICUb) | Decline | 2.3:1 |
| Ying[34], Tse[35] | Hong Kong | VHD | 1993–2005 | ≤15 | Decline | - | - | - | 1.4:1 |
| Sarma[11]a | India | MD | 1994–2007 | all | Decline* | - | - | - | 1.1:1 |
| Karimi[18] | Iran | HD | 2005–2009 | <15 | Increase | - | - | - | 1.7:1 |
| Harats[19]a | Israel | VHD | 1997–2010 | all | Increase | Decline* (size+depth) | Decline | Decline | 2.1:1 |
| Haik[9]a | Israel | VHD | 1997–2003 | all | - | Decline* (size+depth) | No trend | Decline* | 2.1:1 |
| Akita[36] | Japan | VHD | 1983–2002 | <6 | Decline | - | - | - | 1.3:1 |
| Orozco-Valerio[37]a | Mexico | HD | 1979–2009 | all | Decline* | - | - | Decline* | - |
| Dokter[38]a | Netherlands | VHD | 1995–2011 | all | Decline* | Decline (size) | Decline* | Decline* | 1.9:1 |
| Vloemans[20]a | Netherlands | VHD | 1995–2007 | ≤17 | Increase | Decline* (size+depth) | Decline | No trend | - |
| Al-Shaqsi[21]a | Oman | HD | 1987–2011 | all | Increase | - | Decline | Decline | 1.5:1 |
| Song[39] | Singapore | VHD | 1997–2003 | all | Decline | - | No Trend | No Trend | 2.2:1 |
| Wesson[40] | South Africa | MD | 1995–2009 | <13 | Decline | - | - | - | 1.4:1 |
| Maritz[41] | South Africa | MD | 2003–2008 | all | Decline | - | - | No Trend | 1.8:1 |
| Herbert[42] | South Africa | MD | 1997–2006 | <13 | Decline | - | - | - | - |
| Seo[43]b | South Korea | VHD | 2003–2012 | all | Decline | - | - | Decline | 2.9:1 |
| Åkerlund[44]a, Jonsson[47]a | Sweden | VHD | 1987–2004 | all | Decline* | - | Decline* | Decline* | 2.2:1 |
| Tung[51]a | Taiwan | HD | 1997–2003 | all | No trend | Decline* (size) | - | - | 1.5:1 |
| Stylianou[22]a | UK | VHD | 2003–2011 | all | Increase | - | Decline | Decline | 1.7:1 |
| Hussain[54]a | UK | VHD | 2000–2010 | all | - | - | - | Decline* | |
| Fagenholz[45]a | US | VHD | 1993–2004 | all | Decline* | - | - | - | 1.4:1 |
| Saeman[46] | US | VHD | 1974–2010 | ≤18 | Decline | Decline* (size) | Decline* | Decline* | 2.0:1 |
| Macrino[52] | US | VHD | 1981–2006 | ≥65 | - | Decline* (size) | Decline* | Decline* | 1.2:1 |
| Lentz[53]a | US | VHD | 2005–2014 | all | - | - | Decline | - | 2.1:1 |
| Pham[55]a | US | VHD |
multicenter study,
results from intensive care units only,
statistically significant (p<0.05)
Figure 1.
Continents, Studies, and Development Status. Only 4 studies could be obtained from MD countries and none from LD countries.
Figure 2.
Worldwide trends in burns. Bars show the number of studies presenting a specific trend.
Figure 3.
Study periods of articles distributed according to study population (16 = Hai Jun et al., China, study period 1970–2008).
Figure 4.
Countries of which studies describing trends could be obtained (grey) [©Map template: www.outline-world-map.com].
3.1 Trends in Burn Incidence
There were 11 studies from 10 countries (Australia, Bulgaria, China, the Czech Republic, Finland, Iran, Israel, the Netherlands, the Oman and the United Kingdom) reporting an increase of burn admissions or burn incidence rates [8,13–22]. In the majority of the studies (26 studies from 16 countries – Australia, Austria, Canada, Chile, China, Germany, Hong Kong, India, Japan, Mexico, the Netherlands, Singapore, South Africa, South Korea, Sweden and the United States) a downwards trend of burn incidences has been described [11,23–47]. Four studies could not detect any burn incidence trends at all [48–51].
3.2 Trends in Burn Severity
Few studies focused on injury severity. The majority of the studies focused solely on burn size and did not take burn depth into account.
The attribute “inhalation injury” is not treated in this review since it is usually only applicable in flame burns and thus only relevant for a specific group of injuries.
However, 15 studies from 10 countries (Australia, Austria, Bulgaria, Chile, China, Germany, Israel, the Netherlands, Taiwan and the United States) reported a decrease of injury severity [9,13,15,16,19,20,24,27,30,32,33,38,46,51,52]. In 2 studies, one from Canada [29] and one from China [31], no trends of burn severity have been observed. There has been no study reporting an increase of burn severity over the past years.
3.3 Trends in Length of Hospital Stay (LOS)
A decline of LOS was seen in 16 studies from 11 countries (Australia, Austria, Bulgaria, China, Germany, Israel, the Netherlands, the Oman, Sweden, the United Kingdom, and the United States [15,19–23,25,27,32,33,38,44,46,47,52,53]). Six studies from 4 countries (Canada, China, Israel and Singapore) described no temporal trends in LOS [9,16,28,31,39,48].
Unfortunately, only 4 studies provided LOS/%TBSA. According to these LOS/%TBSA was 1.4–2.0 days at the beginning and declined to 0.5–1.4 days during the study periods [20,27,38,46].
There have been no studies reporting an increase of LOS over time.
3.4 Trends in Burn-Related Mortality
In 22 studies from 13 countries (Australia, Austria, Canada, China, Germany, Israel, Mexico, the Netherlands, the Oman, South Korea, Sweden, the United Kingdom and the United States) a decrease of burn-related mortality has been reported [9,14,16,19,21–23,25,27–29,32,33,37,38,43,44,46,47,52,54,55]. Four studies (from China, Finland, the Netherlands and Singapore) could not detect any trends [8,20,31,41], and only in 1 study from Bulgaria an increase of burn mortality has been observed [15].
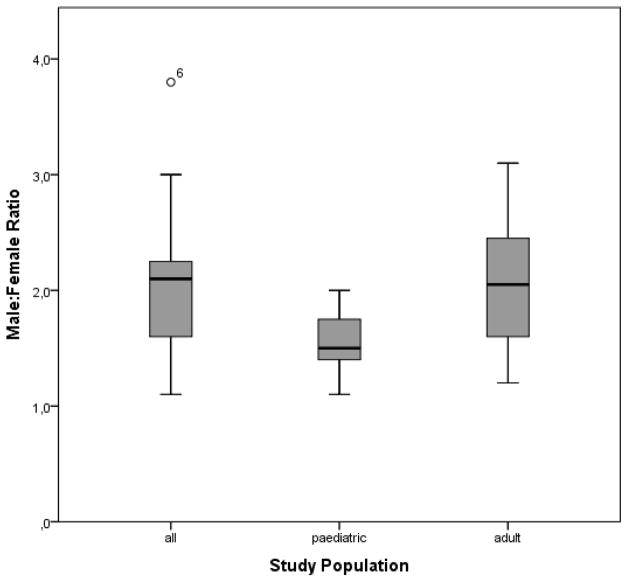
3.5 Male:Female Ratio
The mean male:female ratio of all studies together was 1.92: 1.
The mean ratio of studies including patients of all ages was 2.08: 1. The mean pediatric ratio was 1.56: 1 and thus significantly lower (p=0.021) than the mean sex ratio of studies including only adults (2.06: 1, Figure 5).
Figure 5.
Male: female ratio according to age group (6 = Pegg, Australia, sex ratio 3.8: 1).
The burn incident ratio according to countries’ developmental status was 1.98: 1 in VHD, 1.89: 1 in HD and 1.43: 1 in MD countries. These differences were not statistically significant.
4 Discussion
In general there has been a decrease of burn incidence and burn severity as well as an overall reduction of mortality rates and LOS in recent years. A reduction of burn admissions and mortality has initially also been described by Peck in an extensive review [56]. The results of our literature research do not only correspond with these findings but also show that these trends have been continuing.
Various explanations for the decrease of burn admissions could be found: In Australia, Duke et al. discussed the decrease of burn admissions as a consequence of legislative changes, successful prevention programs, and increased workplace safety [24]. In northeastern India there was a significant reduction of burn incidence (as well as burn severity) amongst students after they had undergone an elaborate burn prevention program. Sarma also found that participants showed better awareness and better recall of preventive measures upon questioning [11].
Also increases of burn admissions have reported, notably from VHD countries where one would normally have expected a decrease (e.g. England [22], the Netherlands [38] or Israel [19]). For these developments the following could be found as an explanation:
Stylianou et al. discussed in their review of the relatively young International Burn Injury Database (iBID) of England and Wales, that the recently pronounced increase in burn patient workload was possibly due to delayed documentation of earlier cases. On the other hand, also financial interests of burn units have been discussed as motivation for “overcorrect” documentation [22].
Israel represents a special case: There were 5.4% more burn admissions in Israel in 2004–2010 compared to 1997–2003 [19]; meanwhile the country’s population increased by 11.6% between 2001 and 2007. The population growth rate was also relatively stable in the 1990s and 2000s at approximately 2.5% per year [52]. So admission rates increased at a slower rate than the population grew during that time, thus it is likely that overall burn incidence rates were actually decreasing, while burn centers noticed an increase of admissions. The authors however also pointed out that only the five burn units in Israel were included in the study, so burn patients admitted to nonspecialized hospitals have not be taken into account [19].
Dokter et al. [38] found in their study in the Netherlands that admission rates to burn centers were increasing (in part due to new referral criteria recommending referral of children with burns > 5% TBSA), while admission rates to general hospitals as well as the overall burn-incidence rate decreased over the same period.
The findings above show clearly that admission numbers reflect the actual burn incidence rate only to certain extent. Furthermore, according to a study in North Carolina only 4% of burn injuries are admitted to hospitals and only further 4% are transferred to specialized burn units [57].
The increased referral of small burns has also contributed to the decrease of burn severity noticed in Dutch burn centers. The strict adherence of non-burn emergency hospitals and community physicians to the compulsory referral patterns of pediatric burns (changed from <10% TBSA to <5% TBSA during the study period) was discussed as major reason for this trend [20]. Similarly, lowering thresholds for referral of burns by community physicians were discussed as reason for the decline of average burn size in the United States [53]. Also Greenwood et al. took the increasing referral of small burns <10% to their burn unit in Adelaide as reason for the decrease of burn size. Those burns would not have been referred in the past while major burns have historically been the domain of specialized burn facilities [13].
All in all it was noticeable that ever more minor burns are being admitted to specialized burn facilities, be it compulsory by law or on one’s own authority. This development is certainly convenient; a deep partial thickness or full thickness hand burn may only account for 1–2% of the total body surface area. This injury may however cause severe physical (and further also social) impairment later in life if not treated properly by best possible standards.
HD countries like China seem to face a very specific problem which is described by Yongqiang et al. [49]: with the country’s development, also burn rates were increasing and current Chinese health care providers have to keep up with this development. Additionally there is no obligatory health insurance in China. As a result, patients with burns requiring professional treatment might not be able to afford expensive hospital stays and thus drop out of patient records. A factor leading to increased pediatric burn admission rates in China was discussed by Zhu et al. [16] who attributed this development to the increasing wealth of the population as well as expanding governmental healthcare coverage, especially reimbursements of hospital stays. Due to the one-child policy in China, it is possible that the parents’ concern for the health of their only child contributed to increasing admissions of also minor burns. Furthermore, Zhu and Hai Jun attributed the decrease of burn size in Chinese children to the increase of scald burns which normally result in less extensive injuries than flame burns [16,32].
According to the world health organization’s fact sheet of 2014, an estimated 265 000 fatal burns occur annually [58]. Quite similar to our findings, also Peck described that a decline in burn mortality rates had been observed in various regions [56].
There is a consensus that improved knowledge about the pathophysiology of burns and advances in treatment, especially intensive care, renal replacement therapy, and nutritional support are the main causes for the reduction of burn-related mortality [16,22,38]. Moreover, improvements in infection control have contributed largely to the decline [21]. Also the widely observed reduction of LOS was mainly due to advances in burn treatment (especially early surgical therapy), new wound dressings (allowing for less frequent dressing changes, and reduced infection rates), the increased referral of smaller burns mentioned earlier, and last but not least the widely adopted policy of earlier discharge to outpatient management [15,19,27,33,38,44,47].
Although one would think otherwise, Haik et al. found no evidence that a more aggressive surgical management results in improved survival rates [9]. Duke et al. further stated that there still is uncertainty whether elderly patients benefit in the same way of an early surgical therapy as young and middle-aged burn victims do [23]. Furthermore, Duke [23] as well as Macrino et al. [52] indicated that the improvement of mortality rates in older patients in their studies was only marginal and partly due to a decrease of burn severity.
Pegg discussed earlier referral of burn injuries to specialized facilities (allowing for earlier surgical treatment, nutritional support etc.) as main contributing factor to the decrease of burn mortality [14]. Gomez et al. (Canada) further emphasized the value of teams specialized in burn treatment: those include fellowship-trained burn surgeons working together with critical care, anesthetists, and nursing staff. A different approach to burn care has been pursued in Australia and the United Kingdom, where consultant burn surgeons solely take care of surgical procedures and are seemingly not integrated into critical care, quite the contrary to how burns are treated in Canada [29].
Burn mortality rates however, have to be treated with care, as most studies only take the in-patient mortality into account while a certain proportion of patients dies at the scene of injury. In Greater Manchester for instance 35% of burn deaths occurred at places of residence. Hussain et al. describe this phenomenon as “bi-modal distribution of burn mortality” [55]. This bi-modal mortality distribution could also be observed in Sweden, where in-hospital mortality declined over the past decades, while the number of patients dying on the scene remained fairly stable [44,47].
Concerning the gender distribution of burns, the findings of this review indicate that children of both genders are at near equal risk of sustaining burn injuries. Later in life, different working environments and possibly also different leisure time activities contribute to the relative increase of burn injuries in men. In older persons however, the differences seem to decline again, like Åkerlund et al. [44] could show in an 18 year retrospective study in Sweden. The unequal gender distribution is however in contrast to the latest report published by the world health organization according to which men and women have broadly similar burn rates [58].
4.1 Strengths and Limitations
To the best of our knowledge this is one of the few reviews of worldwide burn trends. Even though the material consisted of heterogeneous studies from numerous countries and settings we believe that the study provides a good overview over current trends in burns. However, there is a lack of studies from LD countries and thus, unfortunately many countries remain “white spots” on the imagined world map of epidemiologic burn research (figure 4). The lack of data from low development countries reflects the condition of medical supply these countries are currently facing.
This review also clearly shows the need for national or international databases for burn injuries for better evaluation of treatment and research. Examples are England and Wales’ international Burn Injury Database (iBID) [22], the American Burn Repository (ABR) [55], the Burn Registry of Australia and New Zealand (BRANZ) [59] or the Dutch Burn Repository [20,38].
5 Conclusions
Globally there has been a decrease of burn incidence, burn severity, burn mortality and LOS, especially in VHD, HD and MD countries. In LD countries, due to the lack of data and publications, it is hard to give an exact trend. Hence, studies on burn epidemiology should be conducted especially in LD countries.
According to development status, countries face different tasks: While in very high developed countries tertiary care is well established, there seems to be a lack of specialized facilities in less developed countries. High developed countries like China face the challenge of keeping up medically with the country’s rapid socioeconomic development.
Although the studies obtained for this review were heterogeneous regarding patient populations, assessed parameters and observation periods some general conclusions could still be made:
There has been a shift in burn care from general emergency hospitals to specialized burn units/centers.
Burn prevention programs seem to have a positive effect on both burn incidence and injury severity.
The decrease of injury severity is also created by the fact that there is a recent trend of admitting also minor burns to specialized burn units resulting in a relative increase of less severe injuries.
Advances in burn treatment contributed largely to improved outcome and lower in-hospital mortality.
The overall downwards trends in all categories reviewed are consistent with the hypothesis, that increasing development leads to decreases of injury incidence and hence also burns.
Highlights.
A literature review was conducted regarding trends in burn epidemiology worldwide.
There has been a downwards trend in burn incidence and injury severity.
Length of hospital stay and burn mortality have also declined.
There is a lack of data from low development countries.
Positive developments are due to advances in treatment and prevention of burns.
Acknowledgments
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Authors’ contributions
All authors made substantial contributions to the development or design of the work or to the acquisition, analysis, or interpretation of data for the work and the drafting of the work or revising the intellectual content. All authors have approved the final version of the article.
Conflicts of interest
None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lentz CW, Potenza BM, Bernal N, Reigart CL, Faraklas I, Bessey PQ, et al. 2014 National Burn Repository, Report Data from 2004–2013. n.d [Google Scholar]
- 2.Wasiak J, Lee SJ, Paul E, Mahar P, Pfitzer B, Spinks A, et al. Predictors of health status and health-related quality of life 12 months after severe burn. Burns J Int Soc Burn Inj. 2014;40:568–74. doi: 10.1016/j.burns.2014.01.021. [DOI] [PubMed] [Google Scholar]
- 3.Mistry RM, Pasisi L, Chong S, Stewart J, She RBW. Socioeconomic deprivation and burns. Burns J Int Soc Burn Inj. 2010;36:403–8. doi: 10.1016/j.burns.2009.05.021. [DOI] [PubMed] [Google Scholar]
- 4.Kilburn N, Dheansa B. Socioeconomic impact of children’s burns-a pilot study. Burns J Int Soc Burn Inj. 2014;40:1615–23. doi: 10.1016/j.burns.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 5.Sanchez JLA, Bastida JL, Martínez MM, Moreno JMM, Chamorro JJ. Socioeconomic cost and health-related quality of life of burn victims in Spain. Burns J Int Soc Burn Inj. 2008;34:975–81. doi: 10.1016/j.burns.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 6.United Nations Development Programme, editor. Work for human development. New York, NY: United Nations Development Programme; 2015. [Google Scholar]
- 7.Zoni AC, Domínguez-Berjón MF, Esteban-Vasallo MD, Velázquez-Buendía LM, Blaya-Nováková V, Regidor E. Socioeconomic inequalities in injuries treated in primary care in Madrid, Spain. J Public Health Oxf Engl. 2016 doi: 10.1093/pubmed/fdw005. [DOI] [PubMed] [Google Scholar]
- 8.Laitakari E, Koljonen V, Rintala R, Pyörälä S, Gissler M. Incidence and risk factors of burn injuries among infants, Finland 1990–2010. J Pediatr Surg. 2015;50:608–12. doi: 10.1016/j.jpedsurg.2014.05.034. [DOI] [PubMed] [Google Scholar]
- 9.Haik J, Liran A, Tessone A, Givon A, Orenstein A, Peleg K, et al. Burns in Israel: demographic, etiologic and clinical trends, 1997–2003. Isr Med Assoc J IMAJ. 2007;9:659–62. [PubMed] [Google Scholar]
- 10.Edelman LS. Social and economic factors associated with the risk of burn injury. Burns J Int Soc Burn Inj. 2007;33:958–65. doi: 10.1016/j.burns.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 11.Sarma BP. Prevention of burns: 13 years’ experience in Northeastern India. Burns J Int Soc Burn Inj. 2011;37:265–72. doi: 10.1016/j.burns.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 12.Brusselaers N, Monstrey S, Vogelaers D, Hoste E, Blot S. Severe burn injury in Europe: a systematic review of the incidence, etiology, morbidity, and mortality. Crit Care Lond Engl. 2010;14:R188. doi: 10.1186/cc9300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greenwood JE, Tee R, Jackson WL. Increasing numbers of admissions to the adult burns service at the Royal Adelaide Hospital 2001–2004. ANZ J Surg. 2007;77:358–63. doi: 10.1111/j.1445-2197.2007.04060.x. [DOI] [PubMed] [Google Scholar]
- 14.Pegg SP. Burn epidemiology in the Brisbane and Queensland area. Burns J Int Soc Burn Inj. 2005;31(Suppl 1):S27–31. doi: 10.1016/j.burns.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 15.Zayakova Y, Vajarov I, Stanev A, Nenkova N, Hristov H. Epidemiological analysis of burn patients in east Bulgaria. Burns J Int Soc Burn Inj. 2014;40:683–8. doi: 10.1016/j.burns.2013.08.016. [DOI] [PubMed] [Google Scholar]
- 16.Zhu L, Zhang Y, Liu L, Jiang J, Liu Y, Shi F, et al. Hospitalized pediatric burns in North China: a 10-year epidemiologic review. Burns J Int Soc Burn Inj. 2013;39:1004–11. doi: 10.1016/j.burns.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 17.Celko AM, Grivna M, Dánová J, Barss P. Severe childhood burns in the Czech Republic: risk factors and prevention. Bull World Health Organ. 2009;87:374–81. doi: 10.2471/BLT.08.059535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karimi H, Montevalian A, Motabar AR, Safari R, Parvas MS, Vasigh M. Epidemiology of paediatric burns in Iran. Ann Burns Fire Disasters. 2012;25:115–20. [PMC free article] [PubMed] [Google Scholar]
- 19.Harats M, Peleg K, Givon A, Kornhaber R, Goder M, Jaeger M, et al. Burns in Israel, comparative study: Demographic, etiologic and clinical trends 1997–2003 vs. 2004–2010. Burns J Int Soc Burn Inj. 2015 doi: 10.1016/j.burns.2015.05.023. [DOI] [PubMed] [Google Scholar]
- 20.Vloemans AFPM, Dokter J, van Baar ME, Nijhuis I, Beerthuizen GIJM, Nieuwenhuis MK, et al. Epidemiology of children admitted to the Dutch burn centres. Changes in referral influence admittance rates in burn centres. Burns J Int Soc Burn Inj. 2011;37:1161–7. doi: 10.1016/j.burns.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 21.Al-Shaqsi S, Al-Kashmiri A, Al-Bulushi T. Epidemiology of burns undergoing hospitalization to the National Burns Unit in the Sultanate of Oman: a 25-year review. Burns J Int Soc Burn Inj. 2013;39:1606–11. doi: 10.1016/j.burns.2013.04.012. [DOI] [PubMed] [Google Scholar]
- 22.Stylianou N, Buchan I, Dunn KW. A review of the international Burn Injury Database (iBID) for England and Wales: descriptive analysis of burn injuries 2003–2011. BMJ Open. 2015;5:e006184. doi: 10.1136/bmjopen-2014-006184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Duke J, Wood F, Semmens J, Edgar DW, Spilsbury K, Willis A, et al. Rates of hospitalisations and mortality of older adults admitted with burn injuries in Western Australian from 1983 to 2008. Australas J Ageing. 2012;31:83–9. doi: 10.1111/j.1741-6612.2011.00542.x. [DOI] [PubMed] [Google Scholar]
- 24.Duke J, Wood F, Semmens J, Edgar DW, Spilsbury K, Rea S. An assessment of burn injury hospitalisations of adolescents and young adults in Western Australia, 1983–2008. Burns J Int Soc Burn Inj. 2012;38:128–35. doi: 10.1016/j.burns.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 25.Duke J, Wood F, Semmens J, Spilsbury K, Edgar DW, Hendrie D, et al. A 26-year population-based study of burn injury hospital admissions in Western Australia. J Burn Care Res Off Publ Am Burn Assoc. 2011;32:379–86. doi: 10.1097/BCR.0b013e318219d16c. [DOI] [PubMed] [Google Scholar]
- 26.Duke J, Wood F, Semmens J, Edgar DW, Spilsbury K, Hendrie D, et al. A study of burn hospitalizations for children younger than 5 years of age: 1983–2008. Pediatrics. 2011;127:e971–977. doi: 10.1542/peds.2010-3136. [DOI] [PubMed] [Google Scholar]
- 27.Trop M, Herzog SA, Pfurtscheller K, Hoebenreich AM, Schintler MV, Stockenhuber A, et al. The past 25 years of pediatric burn treatment in Graz and important lessons been learned. An overview. Burns J Int Soc Burn Inj. 2015;41:714–20. doi: 10.1016/j.burns.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 28.Spinks A, Wasiak J, Cleland H, Beben N, Macpherson AK. Ten-year epidemiological study of pediatric burns in Canada. J Burn Care Res Off Publ Am Burn Assoc. 2008;29:482–8. doi: 10.1097/BCR.0b013e3181776ed9. [DOI] [PubMed] [Google Scholar]
- 29.Gomez M, Cartotto R, Knighton J, Smith K, Fish JS. Improved survival following thermal injury in adult patients treated at a regional burn center. J Burn Care Res Off Publ Am Burn Assoc. 2008;29:130–7. doi: 10.1097/BCR.0b013e31815f6efd. doi:1097/BCR.0b013e31815f6efd. [DOI] [PubMed] [Google Scholar]
- 30.Rojas Goldsack M, de LÁ, Saavedra Opazo R, Vicencio Pezo P, Solís Flores F. Epidemiological changes in children with burns attending clinics in a district of Santiago, Chile, over a 10 year period. Rev Chil Pediatr. 2015 doi: 10.1016/j.rchipe.2015.10.014. [DOI] [PubMed] [Google Scholar]
- 31.Cheng W, Yan-hua R, Fang-gang N, Wei-li D, Guo-an Z. Epidemiology of 1974 burn patients at a major burn center in Beijing: a nine-year study. J Burn Care Res Off Publ Am Burn Assoc. 2012;33:e228–233. doi: 10.1097/BCR.0b013e3182479b13. [DOI] [PubMed] [Google Scholar]
- 32.Hai Jun W, Jie X, Jun Z, Feng T, Hui HG. Comparable results of epidemiology of children with burns among different decades in a burn unit in JinZhou, China. Burns J Int Soc Burn Inj. 2011;37:513–20. doi: 10.1016/j.burns.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 33.Theodorou P, Xu W, Weinand C, Perbix W, Maegele M, Lefering R, et al. Incidence and treatment of burns: a twenty-year experience from a single center in Germany. Burns J Int Soc Burn Inj. 2013;39:49–54. doi: 10.1016/j.burns.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 34.Ying SY, Ho WS. An analysis of 550 hospitalized pediatric burn patients in Hong Kong. J Burn Care Rehabil. 2001;22:228–31. doi: 10.1097/00004630-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 35.Tse T, Poon CHY, Tse K-H, Tsui T-K, Ayyappan T, Burd A. Paediatric burn prevention: an epidemiological approach. Burns J Int Soc Burn Inj. 2006;32:229–34. doi: 10.1016/j.burns.2005.08.025. [DOI] [PubMed] [Google Scholar]
- 36.Akita S, Nakagawa H, Tanaka K, Hirano A. Analysis of pediatric burns in Nagasaki University from 1983 to 2002. Burns. 2005;31:1041–4. doi: 10.1016/j.burns.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 37.Orozco-Valerio M, de J, Miranda-Altamirano RA, Méndez Magaña AC, Celis A. Trends in mortality by burns in Mexico, 1979–2009. Gac Médica México. 2012;148:349–57. [PubMed] [Google Scholar]
- 38.Dokter J, Vloemans AF, Beerthuizen GIJM, van der Vlies CH, Boxma H, Breederveld R, et al. Epidemiology and trends in severe burns in the Netherlands. Burns J Int Soc Burn Inj. 2014;40:1406–14. doi: 10.1016/j.burns.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 39.Song C, Chua A. Epidemiology of burn injuries in Singapore from 1997 to 2003. Burns J Int Soc Burn Inj. 2005;31(Suppl 1):S18–26. doi: 10.1016/j.burns.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 40.Wesson HKH, Bachani AM, Mtambeka P, Schulman D, Mavengere C, Stevens KA, et al. Pediatric burn injuries in South Africa: a 15-year analysis of hospital data. Injury. 2013;44:1477–82. doi: 10.1016/j.injury.2012.12.017. [DOI] [PubMed] [Google Scholar]
- 41.Maritz D, Wallis L, Van Der Merwe E, Nel D. The aetiology of adult burns in the Western Cape, South Africa. Burns J Int Soc Burn Inj. 2012;38:120–7. doi: 10.1016/j.burns.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 42.Herbert HK, van As AB, Bachani AM, Mtambeka P, Stevens KA, Millar AJW, et al. Patterns of pediatric injury in South Africa: an analysis of hospital data between 1997 and 2006. J Trauma Acute Care Surg. 2012;73:168–74. doi: 10.1097/TA.0b013e31824d67c3. [DOI] [PubMed] [Google Scholar]
- 43.Seo DK, Kym D, Yim H, Yang HT, Cho YS, Kim JH, et al. Epidemiological trends and risk factors in major burns patients in South Korea: a 10-year experience. Burns J Int Soc Burn Inj. 2015;41:181–7. doi: 10.1016/j.burns.2014.05.004. [DOI] [PubMed] [Google Scholar]
- 44.Akerlund E, Huss FRM, Sjöberg F. Burns in Sweden: an analysis of 24,538 cases during the period 1987–2004. Burns J Int Soc Burn Inj. 2007;33:31–6. doi: 10.1016/j.burns.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 45.Fagenholz PJ, Sheridan RL, Harris NS, Pelletier AJ, Camargo CA. National study of Emergency Department visits for burn injuries, 1993 to 2004. J Burn Care Res Off Publ Am Burn Assoc. 2007;28:681–90. doi: 10.1097/BCR.0B013E318148C9AC. [DOI] [PubMed] [Google Scholar]
- 46.Saeman MR, Hodgman EI, Burris A, Wolf SE, Arnoldo BD, Kowalske KJ, et al. Epidemiology and outcomes of pediatric burns over 35 years at Parkland Hospital. Burns J Int Soc Burn Inj. 2015 doi: 10.1016/j.burns.2015.10.011. [DOI] [PubMed] [Google Scholar]
- 47.Jonsson A, Huss FRM, Svee A, Sjöberg F. Burns in Sweden: Temporal Trends 1987–2010. Ann Burns Fire Disasters. 2015:28. [PMC free article] [PubMed] [Google Scholar]
- 48.Burton KR, Sharma VK, Harrop R, Lindsay R. A population-based study of the epidemiology of acute adult burn injuries in the Calgary Health Region and factors associated with mortality and hospital length of stay from 1995 to 2004. Burns J Int Soc Burn Inj. 2009;35:572–9. doi: 10.1016/j.burns.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 49.Yongqiang F, Yibing W, Dechang W, Baohua L, Mingqing W, Ran H. Epidemiology of hospitalized burn patients in Shandong Province: 2001–2005. J Burn Care Res Off Publ Am Burn Assoc. 2007;28:468–73. doi: 10.1097/BCR.0B013E318053D28B. [DOI] [PubMed] [Google Scholar]
- 50.Ortiz-Prado E, Armijos L, Iturralde AL. A population-based study of the epidemiology of acute adult burns in Ecuador from 2005 to 2014. Burns J Int Soc Burn Inj. 2015;41:582–9. doi: 10.1016/j.burns.2014.08.012. [DOI] [PubMed] [Google Scholar]
- 51.Tung K-Y, Chen M-L, Wang H-J, Chen G-S, Peck M, Yang J, et al. A seven-year epidemiology study of 12,381 admitted burn patients in Taiwan--using the Internet registration system of the Childhood Burn Foundation. Burns J Int Soc Burn Inj. 2005;31(Suppl 1):S12–17. doi: 10.1016/j.burns.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 52.Macrino S, Slater H, Aballay A, Goldfarb IW, Caushaj PF. A three-decade review of thermal injuries among the elderly at a regional burn centre. Burns J Int Soc Burn Inj. 2008;34:509–11. doi: 10.1016/j.burns.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 53.Lentz CW, Bernal N, Faraklas I, Kahn SA, Kemalyan NA, Mian MAH. National Burn Repository 2015 Report. n.d [Google Scholar]
- 54.Hussain A, Dunn K. Burn related mortality in Greater Manchester: 11-year review of Regional Coronial Department Data. Burns J Int Soc Burn Inj. 2015;41:225–34. doi: 10.1016/j.burns.2014.10.008. [DOI] [PubMed] [Google Scholar]
- 55.Pham TN, Kramer CB, Wang J, Rivara FP, Heimbach DM, Gibran NS, et al. Epidemiology and outcomes of older adults with burn injury: an analysis of the National Burn Repository. J Burn Care Res Off Publ Am Burn Assoc. 2009;30:30–6. doi: 10.1097/BCR.0b013e3181921efc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Peck MD. Epidemiology of burns throughout the world. Part I: Distribution and risk factors. Burns J Int Soc Burn Inj. 2011;37:1087–100. doi: 10.1016/j.burns.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 57.DeKoning EP, Hakenewerth A, Platts-Mills TF, Tintinalli JE. Epidemiology of burn injuries presenting to North Carolina emergency departments in 2006–2007. Burns. 2009;35:776–82. doi: 10.1016/j.burns.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 58.WHO. Burns. WHO; 2016. [accessed May 6, 2016]. http://www.who.int/mediacentre/factsheets/fs365/en/ [Google Scholar]
- 59.Riedlinger DI, Jennings PA, Edgar DW, Harvey JG, Cleland MHJ, Wood FM, et al. Scald burns in children aged 14 and younger in Australia and New Zealand—an analysis based on the Burn Registry of Australia and New Zealand (BRANZ) Burns J Int Soc Burn Inj. 2015;41:462–8. doi: 10.1016/j.burns.2014.07.027. [DOI] [PubMed] [Google Scholar]