Abstract
Acculturation represents an important construct for elucidating the determinants and consequences of health disparities in minority populations. However, the processes and mechanisms underlying acculturation’s effects on health are largely undetermined and warrant further study. We integrate concepts from anthropology and statistics to describe the role of sociocultural context as a putative modifier of the relationship between acculturation and health. Sociocultural context may influence the extent to which exposure to host culture leads to internalization of host cultural orientation, and may influence the extent to which acculturation leads to stress and adoption of unhealthy behaviors. We focus on specific aspects of sociocultural context: (1) neighborhood ethno-cultural composition; (2) discrimination; (3) discrepancy between origin and host environments; (4) discrepancy between heritage and host cultures; (5) origin group, host group, and individual attitudes towards assimilation; (6) variation in targets of assimilation within host community; (7) public policy and resources; (8) migration selection bias. We review and synthesize evidence for these moderation effects among first- and later-generation immigrants, refugees, and indigenous populations. Furthermore, we propose best-practices data-collection and statistical-analysis methods for this purpose, in order to improve our understanding of the complex, multilevel aspects of the relationship between acculturation and health.
Keywords: acculturation, minority health, health disparities, sociocultural context, effect moderation, statistical interaction
INTRODUCTION
In our increasingly globalized world, interaction between cultures is more common than ever before. Cultural contact can lead to sharing of beliefs, values, and practices between formerly culturally distinct groups. For the individual exposed to another (often majority) culture, changes in the individual’s beliefs, values, and practices may occur (Berry 1997, 2005). These group-level and individual-level phenomena have been referred to as “acculturation,” a construct with its origins in the field of anthropology (Boas 1888; Herskovits 1937; Redfield, Linton, and Herskovits 1936) and subsequently extrapolated for use in a wide range of disciplines, particularly psychology (Berry 2002), epidemiology (Henry and Cassel 1969), and public health (Abraído-Lanza et al. 2006). Here, we define acculturation as changes in beliefs, values, identity, or behaviors such as language, customs, diet, or social relationships that occur in minority-culture individuals (immigrant or indigenous) as a result of prolonged contact with the majority culture. Acculturation is a dynamic, multifaceted process that unfolds over time, and can manifest in various trajectories of change—or “strategies” (Berry 1997)—that may or may not involve increasing orientation towards majority-group culture. In addition, we use the term “trajectories” to highlight the temporal process of acculturative change, and “strategies” to highlight the different paths acculturative change may take. Lastly, we use the term “host” to refer to the majority group, which may be indigenous or colonizing, and may be defined based on any combination of culture, ethnicity, religion, and heritage.
Acculturation at both the population and individual level is believed to shape patterns of minority health and disease risk. Anthropology provides an important theoretical framework for addressing these issues, drawing concepts, methods, and data from sociocultural, biological, medical, and psychological subfields. The study of the relationship between acculturation and health naturally lends itself to the anthropological agenda of examining the interplay between culture, community, and individual embodiment.
Both acculturation and health are multifaceted, dynamic, complex constructs that have been assessed in various ways. Despite heterogeneity in the definition of each of these constructs, a large number of studies have reported associations between various indices of acculturation and health among minority populations (see Lara et al. 2005; Sanou et al. 2013; Suinn 2010). While the complexity of which aspects of acculturation are related to which aspects of health is itself worthy of review, here we simply call attention to the vast number of studies in this area in order to emphasize the immense public, academic, and policymaker interest in understanding the interconnection between these two complex constructs.
Findings across the large and growing literature on acculturation and health vary in terms of the direction and magnitude of effects (Abraído-Lanza, Echeverría, and Flórez 2016), often with contradictory results. For example, among Chinese Americans, acculturation has been associated with higher (Chen, Guarnaccia, and Chung 2003), lower (Hwang et al. 2005), and no differences (Mak and Zane 2004) in rates of depression. Among Hispanic Americans, acculturation has been associated with higher (Heilemann et al. 2004), lower (Yonkers et al. 2001), and no difference (Kuo et al. 2004) in rates of postpartum depression, and acculturation is paradoxically associated with both rates of obesity and more physical exercise (see Pérez-Escamilla and Putnik 2007).
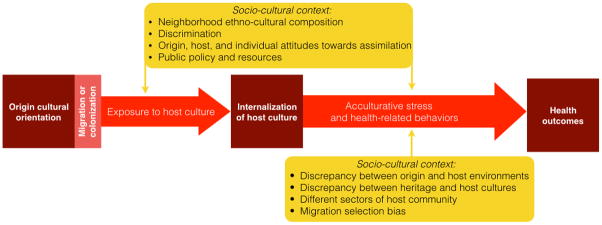
We suggest that one important reason for these discrepancies is likely related to the effects of other variables that may moderate the nature of the relationship between acculturation and health. Given the broad relevance of this topic to social science and public health, alongside the multitude of public resources that have been dedicated to investigating the relationship between acculturation and health (e.g., National Institutes of Health 2016a, 2016b), it is crucial that the conventional methodology is improved. A fundamental aspect of the way cultural exposure, acculturation, and health interact is that these constructs are embedded within a sociocultural context, which modifies the relationships of interest. As such, our model is based on the premise that the relationship between acculturation and health is not monotonic but conditional in nature. In other words, acculturation’s effect on health is a function of one or more other variables. We emphasize that the concept of effect modification (moderation) is distinct from that of mediation (elucidation of factors that describe the causal pathway) (Figure 1) (Hayes 2013), and that a moderator may alter the directionality and/or strength of a relationship (Figure 2). We argue that sociocultural context may change the extent to which exposure to host culture leads to internalization of host cultural orientation, and also change the extent to which acculturation causes stress and unhealthy behaviors (Figure 2). Here, we focus on eight key aspects of sociocultural context: (1) neighborhood ethnocultural composition, (2) discrimination, (3) discrepancy between origin and host environments, (4) discrepancy between heritage and host cultures, (5) origin group, host group, and individual attitudes towards assimilation, (6) variation in targets of assimilation within host community, (7) public policy and resources, and (8) migration selection bias (Figure 3). We discuss evidence for these factors as effect modifiers, drawing examples from first- and later-generation immigrants, refugees, and indigenous populations. We also provide suggestions for research methodology for data collection protocols, and detailed statistical analysis techniques and considerations.
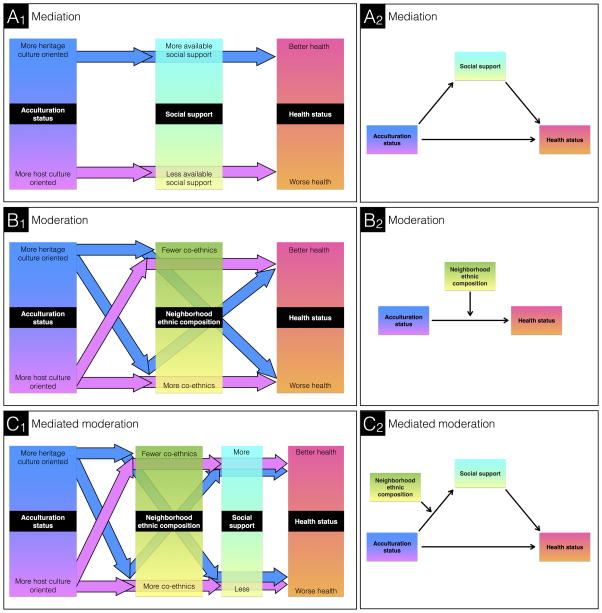
Figure 1.
Modeling indirect effects. These panels present a hypothetical example of a study in which the effect of acculturation status upon health varies as a function of neighborhood ethnic composition, and the effect of neighborhood ethnic composition on health is transmitted via social support. A1, B1, and C1 panel diagrams explicate what mediation and moderation models practically mean, with arrows representing binary conceptualization of variables. Color gradients reflect the continuous nature of each variable. A2, B2, and C2 panels present conceptual diagrams of indirect effects in the tradition of statistics. In A2 and C2, the arrows directly linking predictor and outcome indicate that the mediating variable does not necessarily account for the entirety of the main effect. Altogether, these diagrams reveal the importance of considering the many complex interactions involved in the relationship between acculturation and health. For example, previous authors have asserted that for certain immigrant groups, heritage-culture orientation may be associated with health benefits due to more available social support (A). If this correlation is attributable to the communalistic values in the heritage culture, then the relationship may vary as a function of the neighborhood proportion of coethnics (C). A heritage culture oriented individual who resides in an ethnic enclave may exhibit health benefits due to high availability of social support that offsets the detriments of poverty, compared to a heritage culture oriented individual who resides in a neighborhood dominated by the majority ethnocultural group (B).
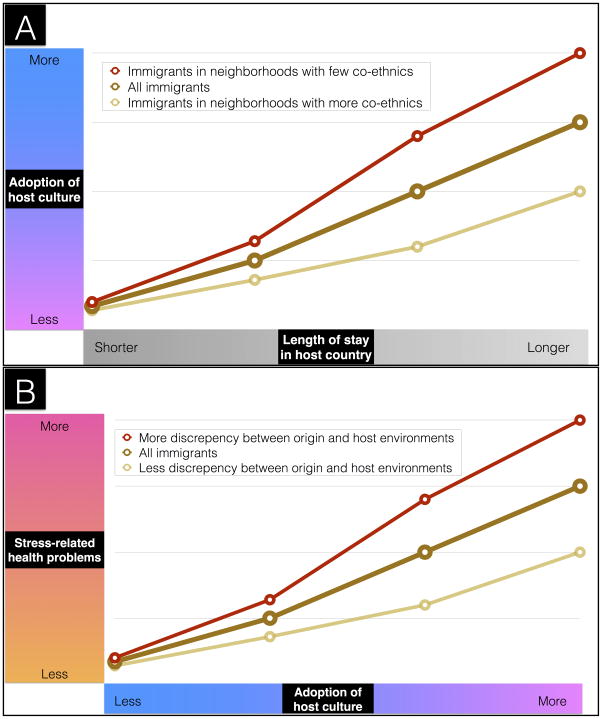
Figure 2.
Sociocultural context moderates relationships between (A) exposure and adoption of host culture, and (B) acculturation and health
Figure 3.
Diagram of how acculturation can influence health. A minority-culture individual’s exposure to the majority (“host”) culture may lead to the individual’s internalization of the host group’s cultural orientation. Host cultural orientation (and the process of adoption of host cultural orientation) may induce psychosocial stress and/or promote adoption of unhealthy behaviors, and thereby negatively affect the individual’s health. Both of these processes (the extent to which exposure to host culture leads to internalization of host culture; the extent to which acculturation causes stress and unhealthy behavior) are potentially modified by sociocultural context. In other words, firstly, the relationship between exposure and adoption of host culture may be moderated by sociocultural context, and secondly, the relationship between acculturation and stress/unhealthy behavior may be moderated by sociocultural context. We emphasize eight aspects of sociocultural context: (1) neighborhood ethnocultural composition; (2) discrimination; (3) discrepancy between origin and host environments; (4) discrepancy between heritage and host cultures; (5) origin group, host group, and individual attitudes towards assimilation; (6) variation in targets of assimilation within host community; (7) public policy and resources; (8) migration selection bias.
SOCIOCULTURAL CONTEXT OF ACCULTURATION
The context in which acculturation occurs may modify its effect on health (Figure 2). Here, we describe eight aspects of sociocultural context that we posit are potentially important effect modifiers (Figure 3). For each, we describe anthropological conceptual underpinnings, concrete recommendations for operationalization, and examples of relevant studies.
NEIGHBORHOOD ETHNOCULTURAL COMPOSITION
The field of sociocultural anthropology highlights the importance of contemplating individual persons as embedded within communities and cultures, and considering the interactive, reciprocal relationship between individual and community (Sökefeld 1999). The type of neighborhood in which an individual resides may affect her/his process of acculturation (Alegria 2009; Lara et al. 2005; Wandersman and Nation 1998). Neighborhood characteristics can facilitate different acculturation trajectories (Castro, Kellison, et al. 2010; Castro, Marsiglia, et al. 2010; Schwartz et al. 2006). This concept has been previously referred to as “cultural congruity,” described as the difference in cultural orientation between an individual and her/his surrounding community (Bhugra and Arya 2005). For example, among Hispanic immigrants to the United States, whether they reside in locales dominated by Anglo or Hispanic individuals is an issue that has attracted attention (Lopez-Class, Castro, and Ramirez 2011). In some ethnic enclaves, the origin culture is so preserved that Hispanic immigrants, particularly those who immigrate as adults, “can function in their day-to-day lives without interacting with, let alone acquiring the practices, values, or identifications of the receiving society” (Schwartz et al. 2010, 9), and “go about their daily business as though they were still in their countries of origin (Cano et al. 2016, 262). Among Russian immigrants to the United States, residing in a Russian-immigrant neighborhood has been associated with greater retention of Russian identity and behavior (Miller et al. 2009; Vinokurov, Birman, and Trickett 2000), although findings were inconsistent for explaining the degree to which host culture was espoused (Miller et al. 2009).
These observations that neighborhood ethnic composition predicts differences in acculturation trajectories are consistent with the premise that, among migrant populations, neighborhood ethnic composition is a moderator of the relationship between duration of residence and acculturation (Figure 3). This hypothesis posits for a unit of time spent living in the host country, the amount of host culture adopted may be less for individuals in neighborhoods with more coethnic residents compared with individuals residing in neighborhoods with fewer coethnic residents (Figure 2). The amount of heritage culture retained may be more for those in neighborhoods with more coethnic residents and less for those residing in neighborhoods with fewer coethnic residents. In sum, the degree to which an individual retains heritage culture or adopts host culture may be contingent on neighborhood context.
Neighborhood context may affect not only the relationship between cultural exposure and internalization but also the relationship between acculturation and health (Figure 1). Previous studies have demonstrated that neighborhood ethnic composition modifies acculturation’s effect upon health-related behavior among Hispanic American adults (Kimbro 2009), upon antisocial behavior among Hispanic American adolescents (Eamon and Mulder 2005), and upon self-esteem among Chinese Americans (Schnittker 2002). For example, Park et al. (2008) found in a cohort of Hispanic Americans, the relationship between nativity and body mass index (BMI) varied as a function of neighborhood linguistic isolation. These latter authors employed an efficacious multilevel analytic approach in which individuals were nested within neighborhoods, which were nested within districts. We highlight the multilevel approach to demonstrate the utility of this analytic technique for revealing patterns of moderation, especially for investigating how the correlation between variances for two traits measured at the individual level (i.e., nativity and BMI) may be modified by a grouping or group-level variable (i.e., neighborhood).
There are several ethnocultural features of the surrounding neighborhood that could explain its moderating effect on acculturation’s relationship to health. Firstly, lacking the ability to speak the host-country language could affect health-related behaviors, access to health care, and quality of health care in a context in which the host language is necessary, but this barrier may be absent in a bilingual or origin-language-dominant community (Castro, Shaibi, and Boehm-Smith 2009; González, Haan, and Hinton 2001). Individuals who do not speak the host language may choose to engage in fewer health-care-seeking behaviors compared to host-language speakers, in order to avoid social or psychological discomfort (Bhattacharya 2004), or may face structural or practical impediments to access. In the United States, non-English speakers are less likely than English speakers to have a regular source of medical care or use preventative services (Flores 2006). As for the quality of care, a report by a refugee resettlement program in New England described how language barriers between health-care providers and patients were problematic when a patient’s condition required physicians to ask probing questions to ascertain the nature of the problem. Instances of miscommunication with physicians led to a non-English-speaking family being administered the same set of shots twice, and to a surgical patient believing that her kidney had been removed when in reality it was her gallbladder (Stewart et al. 2005). A study conducted in Ontario, Canada, reported that linguistic minorities—French, Arabic, and Urdu speakers—had better access to physicians with matching language-specific capabilities if they resided in neighborhoods with higher concentrations of cospeakers (Bell et al. 2013). Linguistic-minority individuals who did not reside in such neighborhoods exhibited difficulties in accessing language-specific health care, demonstrating the moderating effect of neighborhood on health-care access. Altogether, these examples serve to demonstrate how language barriers in health-care settings may detrimentally affect health for non-host-language speaking individuals.
Secondly, neighborhood ethnocultural composition may influence health patterns through social-support availability and social cohesion (Figure 2). For example, ethnic enclaves may be characterized by community-wide closeness (Gallo et al. 2009). Stronger ties with coethnics have been associated with better self-rated health among Hispanic immigrants (Kimbro, Gorman, and Schachter 2012). Among former Soviet Union refugees in the United States, coethnic social support was associated with better mental health (Birman et al. 2014). Hispanics may find support and familiarity in barrio communities (Pérez-Escamilla and Putnik 2007; Riosmena, Wong, and Palloni 2012), where health benefits have been observed for first-generation (Cagney, Browning, and Wallace 2007) and second-generation Hispanics (Lee and Ferraro 2007). “Barrio advantages” have been observed for rates of mortality (Eschbach et al. 2004), cancer (Eschbach, Mahnken, and Goodwin 2005), depression (Ostir et al. 2003), and overall health (Patel et al. 2003). Incorporating into the more individualistic and nuclear family social structure of Anglo America may induce stress due to loss of supportive community and extended family. A study of Hispanics in Los Angeles found that the relationship between nativity and self-rated health was moderated by perceived cohesion in the neighborhood environment (Bjornstrom and Kuhl 2014). A useful tool for quantitatively assessing neighborhood coethnic social support is the neighborhood subscale from the Social Support Microsystems Scales (Seidman et al. 1995), initially validated in black, white, and Latino US adolescents, but also utilized in other contexts (Birman et al. 2014). Notably, the impact of the migration-induced loss of social support among minority individuals living in host-culture communities may be partially mitigated by internet-based social media. A study of Polish and Filipino immigrants residing in Ireland found that consistent, low-level social media monitoring along with active messaging of family and friends in origin countries maintained social links and created a virtual experience of community (Komito 2011). Further research is needed to investigate whether social media plays a buffering role in the relationship between migration-induced loss of social community and poor mental health.
Finally, discordance between desired and actual neighborhood contexts may be a source of stress. Counter to preferences, individuals may reside in host-culture neighborhoods (e.g., due to occupational constraints) or minority enclaves (e.g., due to financial constraints or family obligations). Both situations could translate into increased stress and the development of stress-related diseases.
There are two methodological options for characterizing neighborhood ethnocultural composition. Researchers could refer to census-tract information or other public surveys in order to objectively measure neighborhood demographics (Gee 2002). Alternatively, new instruments could be developed to assess subjective experiences and interpretations of neighborhood ethnocultural composition, for instance, by asking respondents about their perception of the nativity, ethnicity, linguistic, or cultural composition of the local community.
DISCRIMINATION
Minority individuals may experience discrimination by majority individuals and institutions. Some environments impose larger amounts of discrimination than others; thus different contexts produce differential exposure to discrimination. The ways in which cultural barriers, such as interpersonal or institutionalized discrimination, can impact population health has emerged as an important area of research in the field of medical anthropology (Winkelman 2008). We contribute to this growing body of research by pointing out how the amount of discrimination encountered in a community may moderate the extent to which host cultures are internalized, and may alter the ways acculturation affects health.
Discrimination can moderate the relationship between cultural exposure and cultural adoption. Discrimination against minority individuals may enhance incentives to abandon heritage cultural behaviors in order to gain access and acceptance into the host community. However, the opposite effect may also occur, with greater discrimination discouraging acculturation by creating an inhospitable atmosphere that does not invite minority individuals to seek participation in the majority culture. Consistent with the latter prediction, among Iranian refugees in the Netherlands, perceived discrimination was associated with greater maintenance of Iranian cultural orientation, and perceived acceptance of immigrants in Dutch society was associated with greater Dutch cultural orientation (Te Lindert et al. 2008).
The severity and prevalence of discrimination in the surrounding community can also exert a moderating effect on how cultural orientation affects health. Myriad evidence supports the likelihood that discrimination instigates chronic and/or sustained activation of stress physiology, including elevated blood pressure, heart rate, cortisol, which over time negatively impacts health (Pascoe and Smart Richman 2009). Exposure to racism and other forms of discrimination has been robustly associated with unhealthy behaviors and poor mental and physical health (Krieger 1999; Paradies 2006).
Communities may vary in amount of discrimination exposure as a function of the proportion of coethnic residents or overall ethnic diversity of the community. Specifically, reduced interaction with other ethnicities may incidentally decrease discrimination experience. Low degrees of discrimination due to decreased interaction with other ethnicities have been hypothesized to contribute to barrio health advantages among Hispanic Americans (Cagney, Browning, and Wallace 2007; Eschbach et al. 2004, Eschbach, Mahnken, and Goodwin 2005; Lee and Ferraro 2007; Ostir et al. 2003; Patel et al. 2003).
Other factors may shape amount of discrimination exposure. Low-acculturated individuals may experience more stress when residing in communities with more discriminatory attitudes or greater degrees of institutional discrimination than their equivalently acculturated counterparts residing in communities with less discrimination, regardless of the ethnicity of the discriminators. As an example of discrimination exposure not corresponding to proportion of coethnic neighbors, Bosnian refugee adolescents encountered more discrimination if they were internally displaced or resettled in Croatia, compared to those who were resettled in Austria, and greater perceived discrimination was associated with worse mental health and self-reported overall health (Sujoldžić et al. 2006). For a further example, Chinese Americans exhibited an association between poor health and discrimination both at the institutional level (e.g., neighborhood home-mortgage discrimination) and interpersonal level, and this relationship was not influenced by neighborhood percentages of Chinese residents (Gee 2002). Because chronic stress is a contributor to poor health, discrimination norms in a community could modify the relationship between acculturation and health.
Discrimination may exert a differential influence on health depending on the target individual’s age. Studies in psychological anthropology suggest that adolescence is an example of a life phase of exceptional vulnerability to the detrimental effects of discrimination on psychological health and well-being (Korbin and Anderson-Fye 2011). Adolescence is a critical phase of neurocognitive development and mental-illness emergence, alongside primary relationships transitioning from family to peer, and societal role culturally transitioning to adulthood. These factors coalesce to make minority adolescents both more likely to encounter, and more sensitive to the effects of, discrimination (Weisner 2011).
Several instruments have been developed to measure discrimination (see Bastos et al. 2010). Depending on the scientific question, validated instruments are available to measure a variety to aspects of discrimination, based on target identity (e.g., race/ethnicity [McNeilly et al. 1995], age [Furunes and Mykletun 2010]), severity (e.g., everyday discrimination [Williams et al. 1997] or major experiences of discrimination [Williams et al. 2008]), and temporality (e.g., frequency, recency, lifetime experiences [Landrine and Klonoff 1996]). Several instruments contain subscales for dimensions that may be key to certain studies, such as institutional, individual, overt, and covert discrimination (McNeilly et al. 1995); blatant and subtle discrimination (Pettigrew and Meertens 1995); and social exclusion, stigmatization, discrimination at work/school, and threat/harassment (Brondolo et al. 2011).
DISCREPANCY BETWEEN ORIGIN AND HOST ENVIRONMENTS
Biological anthropologists have investigated and demonstrated how the mismatch between current environment and environment of origin, both personally and historically, can negatively impact health (Bateson et al. 2004; Candib 2007). For migrants, the degree of distance and difference between their lives in the origin environment compared to host environment can affect the acculturation experience (Lopez-Class, Castro, and Ramirez 2011) and modify its impact on health (Organista, Organista, and Kurasaki 2003; Palinkas and Pickwell 1995; Salant and Lauderdale 2003) (Figure 2). Differences may include population density, social stratification, urbanization, socioeconomic conditions, and religiosity. Lee et al. (2013) further point out potential differences between the origin and host environments of the status of women and underrepresented populations, legal systems, and forms of government, although they discuss these factors with regards to cultural distance (which we address in the next section) rather than the structural context in which culture is embedded. Cabassa (2003) offers a list of factors that may be relevant when contrasting experiences in origin and host countries for Hispanic immigrants. The degree of difference between origin and host environments is a function of variation in the premigration setting as well as the postmigration setting.
One of the routes by which acculturation can causally influence health is psychosocial stress, which induces stress-related health problems, such as cardiovascular disease, depression, and gastrointestinal problems. Acculturation induces more psychosocial stress when there is a greater discrepancy between origin and host environments, due to the greater challenges involved in learning and familiarizing oneself with new systems and ways of life (Berry and Annis 1974). For this reason, we argue that the degree to which an individual adopts host culture may be associated with more stress-related health problems for individuals with a greater discrepancy between their origin and host environments, compared with peers with less discrepancy (Figure 2). In this way, origin-host environment discrepancy may interact with host-culture adoption to enhance the relationship between host-culture adoption and stress-related health problems. While no study known to the authors has specifically investigated the moderating effect of environmental discrepancy between origin and host environments on the relationship between acculturation and health, we point out indirect evidence for this possibility and encourage further study. For example, among immigrants to the United Kingdom, obesity risk was positively associated with later-generation status among Indian, Bangladeshi, Black Caribbean, Irish, and Chinese groups, while obesity was negatively associated with later generation status among Pakistani and black African groups, and these differences were not explained by health behaviors or socioeconomic factors (Smith, Kelly, and Nazroo 2012). The different valences of relationships between generation status (a proxy for acculturation) and obesity (an aspect of health) depending on national origin are consistent with the possibility that different degrees of difference between origin and host environments moderates the relationship between acculturation and health.
Depending on the hypothesis being tested, future studies may benefit from assessing key aspects of origin and host environments using national or available survey data, or by developing new instruments to measure subjective experiences and interpretation of discrepancy.
DISCREPANCY BETWEEN HERITAGE AND HOST CULTURES
For any minority-heritage individual, regardless of nativity, the discrepancy between their heritage and host cultures can be assessed. In the case of migrants, the heritage culture refers to the culture of their place of origin. Examples of aspects of culture that may differ between two groups include language, religion, work norms, competitiveness, individualism and collectivism (Chirkov, Lynch, and Niwa 2005), and concepts of masculinity and femininity (Berry 2002; Lee et al. 2013). These discrepancies may explain why individuals from certain origins tend to exhibit more stress or social difficulties in the acculturation process than individuals from other origins (Babiker, Cox, and Miller 1980; Ward and Kennedy 1992; Ward and Searle 1991; Zlobina et al. 2006).
The discrepancy between origin and host cultures varies as a function of cultural starting conditions from which an individual begins to assimilate, as well as the culture of the receiving society. For understanding starting conditions, the concept of the “acculturation intercept” is relevant (Castro 2013; Castro, Marsiglia, et al. 2010). Lopez-Class, Castro, and Ramirez (2011) adapted the acculturation intercept concept from Castro, Marsiglia, et al.’s (2010) statistical model. Mathematically, for two related variables, an intercept is the value of one variable at the point of origin for the other variable. Thus, among migrants, the acculturation intercept is the acculturation status at the time of migration. This concept is important because acculturation likely exerts its effects on health through novel exposure to the host group’s lifestyle, culture, and environments. Therefore, premigration media and personal exposure to the host country and interaction with host-culture individuals should be considered (De La Rosa, Vega, and Radisch 2000). Popular methodologies have been criticized as “ahistorical” in the lack of attention to premigration exposures to host culture (Tardif-Williams and Fisher 2009). Furthermore, second- and later-generation individuals would likely have cultural-orientation starting points that are already relatively “acculturated” when compared with first-generation individuals.
The discrepancy between heritage and host cultures may behave as an effect modifier, with greater discrepancy enhancing the association between acculturation and adverse health due to the greater challenges involved in transitioning to a vastly different cultural identity and set of behaviors. Evidence supporting this possibility comes from the study of stress psychology. For example, among Amerindian indigenous groups, the degree of difference between heritage and colonizing cultures has been correlated with the magnitude of acculturative stress experienced by members of those groups (Berry and Annis 1974). In addition, among North African immigrants to Spain (Zlobina et al. 2006) and foreign exchange students in Russia (Suanet and Van de Vijver 2009), greater degree of perceived cultural discrepancy between home and host countries has been negatively associated with psychological adjustment.
There are three methodological options for characterizing cultural distance traversed. The first option is for investigators to directly ask respondents about participants’ perceptions of cultural discrepancy (Galchenko and Van de Vijver 2007; Suanet and Van de Vijver 2009; Ward and Searle 1991; Zlobina et al. 2006). The second option is for investigators to determine cultural discrepancy based on population-level rather than individual-level data (Berry and Annis 1974). Thirdly, we suggest that investigators could collect information about each respondent’s perceptions of their origin and host cultures.
ORIGIN GROUP, HOST GROUP, AND INDIVIDUAL ATTITUDES TOWARDS ASSIMILATION
Acculturation can be modeled as the orthogonally unfolding processes of acquisition/avoidance of host culture and retention/loss of heritage culture, with several possible trajectories including biculturalism, alienation from both cultures, or preferential orientation towards one culture (Berry 1997). Assimilation is a specific type of acculturation strategy characterized by acquisition of host culture alongside loss of heritage culture (Berry 2005). Whether assimilation is considered favorably or unfavorably by the origin community, host community, and individual undergoing acculturation may modify both the extent to which exposure to host culture leads to internalization of host cultural identity, as well as the extent to which adoption of host cultural identity leads to poor health (Figure 3).
Firstly, attitudes towards assimilation can modify the extent to which exposure to host culture leads to internalization of host cultural identity. For a unit of time spent living in the host country, the amount of host culture adopted may be less if assimilation is discouraged, and more if assimilation is encouraged. In a study in which Berry’s four acculturation strategies (Berry 1992; Berry et al. 1989) were assessed, Turkish and Moroccan immigrants to the Netherlands most positively regarded integration, followed by assimilation, separation, and marginalization strategies, while the majority-culture Dutch group most positively regarded Turkish and Moroccan immigrants enacting assimilation, followed by integration, marginalization, and separation strategies (Van Oudenhoven, Prins, and Buunk 1998). The Turkish and Moroccan immigrant group exhibited a distribution of acculturation strategies that mirrored their origin (and not host) group’s order of preferred strategies, suggesting that in this circumstance, acculturation strategies may be more influenced by origin than host-group attitudes. In addition, regardless of group attitudes, extent of host-culture adoption may be less for individuals who personally stigmatize assimilation, and more for individuals who personally embrace the idea of assimilation. Further research should investigate how personal attitudes towards different acculturation strategies influences individuals’ trajectories of cultural change.
Whether assimilation is encouraged or discouraged by the origin group, host group, or individual attitudes can alter the way in which acculturation affects health. As described above, one of the routes by which acculturation influences health is psychosocial stress, which can cause stress-related health problems. In fact, acculturative stress (Berry et al. 1987), or the negative psychological impact of negotiating between heritage and host cultures, has been described as the predominant explanation for acculturation’s association with poor physical (Finch et al. 2001) and mental (D’Anna-Hernandez, Aleman, and Flores 2015; Sirin et al. 2013) health. However, there is substantial variation in the extent to which acculturation leads to acculturative stress, which we suggest may be a function of personal and community attitudes towards assimilation. Community attitudes can affect the way individuals are treated based on their acculturation strategies, can become internalized to alter individuals’ acculturation strategies, and can become internalized to alter how individuals feel about their own acculturation strategies, interacting with individuals’ community-independent feelings about their own acculturation strategies. For example, the receiving group’s resistance to minority integration may alter acculturation trajectories (e.g., Hispanics in the United States [Hunt, Schneider, and Comer 2004; Pantin et al. 2004]) or induce unhealthy responses to acculturation, such as social isolation (Bourhis et al. 1997). Alternatively, pressure from peers within Amerindian communities to acculturate may enhance acculturative stress rather than relieve it (Berry and Annis 1974).
A small number of studies have operationalized appraisal of community or individual attitudes towards acculturation strategies, and none have explicitly investigated how those attitudes shape acculturation trajectories or modify the relationship between acculturation and health. One strategy that has been employed is to present respondents with a vignette to read, which describes different acculturation strategies, and assess their evaluation of the vignette (Kosic, Mannetti, and Lackland Sam 2005; Van Oudenhoven, Prins, and Buunk 1998). Others have directly questioned respondents about their opinion regarding acculturation strategies (Sommerlad and Berry 1970). Another strategy is exemplified by the Multidimensional Acculturative Stress Inventory with the subscales “Pressure to Acculturate” and “Pressure Against Acculturation” (Rodriguez et al. 2002).
HOST CULTURE HETEROGENEITY
In sociology, the concept of “segmented assimilation” describes the process by which second-generation individuals can become assimilated into various tiers of the social hierarchy, with the majority of scholarship focused on assimilation into disadvantaged, countercultural communities, such as street gangs or drug culture (Portes 2007; Zhou 1997). Segmented assimilation theory has been discussed mostly with respect to economic development, social mobility, and ethnic identity (Neckerman, Carter, and Lee 1999; Rumbaut 1994; Waters et al. 2010) rather than health, but this theory highlights the importance of considering the context in which acculturation occurs. Instruments that assess assimilation into the dominant tier of the majority culture will not accurately capture the experience of an individual who assimilates into a different sector of the majority culture. The composite structure of the host society must be understood in order for researchers to decide how they will measure assimilation towards host culture.
The variation in host-society sectors could exert a moderating effect on the relationship between acculturation and health (Figure 3). For minority individuals who take the acculturation strategy of assimilation, those embedded in a disadvantaged or deprived host community may exhibit health detriments the more acculturated they become, while those embedded in an advantaged or healthy host community may exhibit health benefits associated with acculturation. Among Korean immigrants to the United States, the relationship between acculturation and health was moderated by educational attainment, such that acculturation was associated with poorer self-rated health and health behaviors among less-educated immigrants, and more favorable health and health behaviors among highly educated immigrants (Ra, Cho, and Hummer 2013), exemplifying how acculturation can promote either better or worse health depending on whether the individual is embedded in advantaged or disadvantaged sectors of a host society.
PUBLIC POLICY AND RESOURCES
The relationship between time exposed to host culture and internalization of host culture may be partly dependent on public policies and resources, such as school busing, language education, affirmative action in schools and workplaces, antidiscrimination employment and housing laws, and neighborhood integration policies (Bisin et al. 2016). For example, local school programs that promote effective acquisition of host language can result in more rapid adoption of host cultural orientation among immigrant students. Education policies that promote instruction or materials in local indigenous languages, such as the Bolivian National Education Reform of 1994 that introduced thirty indigenous languages into school curricula and materials, can result in maintenance of heritage cultural orientation (Hornberger 1998). Among elderly immigrants from the former Soviet Union to the US, those residing in public housing projects exhibited more American cultural orientation for both identity and behaviors compared with those residing in nonpublic housing ethnic enclaves (Vinokurov and Trickett 2015).
The ways in which acculturation affects health may also be modified by public policy and resources. Firstly, public policies and resources directly related to healthcare may alter the relationship between acculturation status and health status for groups of individuals, such as public investment in healthcare resources in underserved minority communities, cultural skills and sensitivity of health professionals, and language services in healthcare settings. For example, significantly more adverse events in US hospitals occur with non-English-speaking patients (Divi et al. 2007). Title VI of the Federal Civil Rights Act of 1964 requires that healthcare providers receiving federal funding provide equal access for non-English-speaking patients at no extra cost to patients, usually implemented by providing language assistance (Snowden et al. 2011). Policies requiring healthcare access equity for minority-language speakers are associated with improvements in health among less-acculturated minority individuals (Timmins 2002), moderating the association between acculturation status and health status. State-mandated implementation of language services may diminish the moderating effect of ethnocultural composition of a neighborhood on health outcomes described above.
Secondly, public policies and resources that are not directly related to healthcare may affect the relationship between acculturation and health by shaping minority rights, participation of minorities in the political process to advocate for their needs, and community degrees of racism, discrimination, and multicultural attitudes. For example, the goal of the 1998 Canadian Multiculturalism Act was removal of discriminatory barriers to immigrant and indigenous minority participation in Canadian life (Gagnon 2002). A better understanding of how acculturation, context, and biology interact to affect health in immigrant and indigenous groups would enable more effective public policy interventions aimed at improving health and well-being in these disadvantaged populations.
IMPACT OF MIGRATION BIAS
The relationship between acculturation and health may vary as a function of population subset. Because population division is inherent to migration, it is imperative to determine how biases in migration patterns may confound the relationship between acculturation and health. Firstly, biases in migration patterns may lend false support to the credence that acculturation causes poor health. The “healthy migrant” hypothesis suggests that healthier individuals are more likely to relocate than less healthy individuals. “Salmon bias” suggests that migrants who develop poor health in the receiving country are disproportionately likely to return to their origin country (Abraído-Lanza et al. 1999; Turra and Elo 2008). Selection bias for healthy migrants and salmon bias for unhealthy migrants could cause the immigrant population to be healthier than the host population, a pattern that could be incorrectly attributed to the health benefits of cultural traditionalism, or could obscure the health problems that emerge in migrant populations over time. However, evidence suggests only very weak (Rubalcava et al. 2008; Turra and Elo 2008) or nonexistent (Abraído-Lanza et al. 1999; Pablos-Méndez 1994) healthy migrant and salmon biases among Hispanic immigrants.
Secondly and alternatively, biases in migration patterns may lend false support to the idea that acculturation causes health benefits. The healthy migrant hypothesis has been called into question because of the counter effect of inflated population-size numbers. National census data may fail to exclude from population counts immigrants who return to their origin country, thereby creating the impression that poor health outcomes are at a lower frequency in the population (Weitoft et al. 1999). Seasonal or cyclic migration may also contribute to the inaccuracy of population counts (Turra and Elo 2008). Furthermore, for intranational migration patterns, the healthy migrant effect is relevant for interpreting outcomes in both the nonmigrating and migrating subpopulations. It has been observed among Native Americans that health influences acculturation trajectories, reversing the typical paradigm of acculturation affecting health. Healthy Native American individuals are more likely to migrate to urban regions within the United States for employment opportunities, compared to their unhealthy counterparts (Kunitz 2014). Thus, comparisons of urban (high acculturation) and rural (low acculturation) Native Americans suggest that acculturation confers health benefits when, in fact, the health gradient plays a large role in shaping acculturation trajectories.
In summary, we urge researchers to include measurements of sociocultural context in studies of the relationship between acculturation and health, in order to assess potential effect modification. For certain constructs, such as discrepancy between origin and host environments, no validated measures exist yet. Our purpose in raising these points and creating this conceptual model is to encourage development of new instruments that can subsequently be tested. For other constructs described in this paper, such as discrimination, we point to validated instruments and previously employed methods for assessment. Below, we discuss techniques for integrating moderator variables into study design, methods, and statistical analysis.
QUANTITATIVE METHODOLOGY
Here we describe quantitative methods for researchers to investigate sociocultural moderators of the relationship between acculturation and health. Effect modification refers to moderating factors in the causal relationship between two entities, and when data behave according to this pattern it is referred to as “statistical interaction.” Statistical interaction may be additive, multiplicative, or both, depending on whether the predictor’s relationship with the moderator is most accurately measured as a scale or ratio (VanderWeele and Knol 2014).
Certain statistical precautions are necessary for moderation analysis—that is, in designing and interpreting models of statistical interaction. We describe four issues with crucial relevance to investigations of sociocultural context as a moderator of the relationship between acculturation and health. Firstly, the causal sequencing of the model should be theoretically justified before conducting statistical testing of moderation. The determination of (1) whether cultural orientation’s effect on health varies as a function of sociocultural context versus (2) whether sociocultural context’s effect on health varies as a function of cultural orientation is most accurately determined by theoretical rationale, rather than by comparing the two statistical moderation models (Carte and Russell 2003; Landis and Dunlap 2000). Investigators who justify the existence of a moderating effect based solely on statistical results may be testing the wrong question.
Secondly, the study by Park et al. (2008) described above employed the common but problematic technique of dichotomizing the moderator (in this case, linguistic isolation), which we highlight to exemplify the pitfall of this procedure. Typically, this technique of binning data into categories of “low” and “high” is used to facilitate simpler types of statistical analyses, or results that are easier to interpret (Hayes 2009; Rucker, McShane, and Preacher 2015). However, slicing a continuum into artificial groups has been widely reported by computational scientists to generate spurious correlations and other kinds of misleading results (Hayes 2009; Kuss 2013; MacCallum et al. 2002). We urge investigators to evaluate interactive relationships using continuous variables (Maxwell and Delaney 1993), or alternatively, create groups by empirically determining whether there is a point in the moderator continuum at which the effect of the predictor upon the outcome changes (Hamaker, Grasman, and Kamphuis 2010).
Thirdly, the issue of how to describe the magnitude of moderating effects has particular challenges for sociocultural moderator variables. The numerical expression of change in the main effect based on one unit of change in the moderator variable will vary based on the scale on which the moderator variable is measured. For social and cultural variables, such as discrimination, cultural discrepancy, or group attitudes, quantitative measures are based on arbitrary scales. Therefore, changing the arbitrary scale on which the moderator is measured alters the observed magnitude of influence on the main effect. This challenge can be addressed by reporting the change in the regression model R2 value that results from including the interaction term, rather than the interaction term’s beta value (Carte and Russell 2003).
Fourthly, many previous authors have suggested mediators by which acculturation may influence health, such as through behavioral changes (Birman and Taylor-Ritzler 2007; Gonzales et al. 2006; Shen and Takeuchi 2001; Unger et al. 2000). We emphasize that those mediators play a different role than moderators in modeling the relationship between acculturation and health. The two concepts (mediation and moderation) are compatible and equip the model with distinct pieces of information (Figure 1). For the relationships between acculturation and health, acculturation and the mediator, or the mediator and health, any of these may vary as a function of yet another factor (moderator). Any path in a mediation model can be moderated, which is mathematically described as a conditional indirect effect (Figure 1). Rather than a piecemeal approach in which individual mediation paths and moderators are explored in different studies, the statistical gold standard of accuracy involves creating an integrated process model that quantifies conditional direct and indirect effects together (Hayes 2013). Optimal accuracy can be obtained by modeling the process as a whole. We encourage investigators to create more complex statistical models that take into account both mediators and moderators of the relationship between acculturation and health in order to capture the complexity of the actual lived experience.
CONCLUSION
In sum, sufficient evidence suggests that the process of acculturation proceeds differently contingent on sociocontextual factors, and thus the impacts of acculturation on health are expected to vary in response to those factors. The purpose of this paper is therefore to provide a methodological intervention and argue that the possibility that acculturation’s effect on health varies as a function of sociocultural context should be explored more widely and deeply than has been done. To this end, more effectual (and in some cases, new) methods are needed to measure neighborhood ethnocultural composition, discrimination, discrepancy between origin and host environments, discrepancy between heritage and host cultures, origin group, host group, and individual attitudes towards assimilation, variation in targets of assimilation within host community, public resources, and migration bias. Instruments capturing these constructs should be utilized in statistical models to test moderation of the degree to which exposure to host culture results in internalization of the host culture or loss of heritage culture, and the degree to which host/heritage cultural orientations are associated with health outcomes. Statistical models testing moderating effects should establish causal ordering before conducting statistical analysis, and quantify constructs and report the magnitude of moderating effects as accurately as possible.
Moreover, while sociocultural context is the focus of this paper, other sources of variation also play important roles in the relationship between acculturation and health. In addition to the sociocultural effect moderators described here, other factors and traits may further moderate the relationships in the causal pathway between cultural exposure and health outcomes. For instance, individuals vary in psychobiological stress reactivity, sensitivity and coping in response to psychosocial stressors, and propensity for mental and physical ailments. Furthermore, while this paper focuses on the construct of sociocultural context, rigorous scrutiny also should be applied to the conceptualization, component selection, and assessment procedures for acculturation and health. To fully understand the role of acculturation in population epidemiology, both sociocultural and other issues should be considered as effect modifiers, and all constructs should be measured and analyzed in the most appropriate, accurate way possible.
Deducing the mechanisms and processes by which acculturation affects health is critical for forecasting and preparing for worldwide changes in health and disease burden, particularly because contact between cultures continues to accelerate due to urbanization, globalization (Wike and Kohut 2008), and the growing issue of refugee displacement (United Nations 2015). Given the vulnerability and sociopolitical disenfranchisement of undocumented immigrants (Chavez 2012) and refugees (United Nations 2016), as well as growing health crises among indigenous communities (Stephens et al. 2005), investing in the health of minority populations has never been as crucial as it is today. The inherently multidisciplinary field of anthropology provides an important perspective for informing public policy related to minority health by highlighting the interacting effects of biology, behavior, psychology, community, and culture in a global, scientific perspective.
Acknowledgments
This research was supported by the National Institutes of Health (NIH), with Molly Fox’s effort supported by grant K01 DK-105110 to Molly Fox.; Pathik D. Wadhwa’s effort was supported, in part, by grants R01 MD-010738 and R01 HD-060628 to Pathik D. Wadhwa; and Zaneta M. Thayer’s effort was supported, in part, by grant P20 MD-006871. The authors thank the editors and anonymous reviewers at American Anthropologist for their generous engagement with this manuscript and insightful feedback.
REFERENCES CITED
- Abraído-Lanza Ana F, Armbrister Adria N, Flórez Karen R, Aguirre Alejandra N. Toward a Theory-Driven Model of Acculturation in Public Health Research. American Journal of Public Health. 2006;96(8):1342–46. doi: 10.2105/AJPH.2005.064980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraído-Lanza Ana F, Dohrenwend Bruce P, Ng-Mak Daisy S, Blake Turner J. The Latino Mortality Paradox: A Test of the ‘salmon bias’ and Healthy Migrant Hypotheses. American Journal of Public Health. 1999;89(10):1543–48. doi: 10.2105/ajph.89.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraído-Lanza Ana F, Echeverría Sandra E, Flórez Karen R. Latino Immigrants, Acculturation, and Health: Promising New Directions in Research. Annual Review of Public Health. 2016;37(1):219–36. doi: 10.1146/annurev-publhealth-032315-021545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria Margarita. The Challenge of Acculturation Measures: What Are We Missing? A Commentary on Thomson & Hoffman-Goetz. Social Science & Medicine. 2009;69(7):996–98. doi: 10.1016/j.socscimed.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babiker Isam E, Cox John L, Miller Patrick M. The measurement of cultural distance and its relationship to medical consultations, symptomatology and examination performance of overseas students at Edinburgh University. Social Psychiatry. 1980;15(3):109–16. [Google Scholar]
- Bastos Joao Luiz, Celeste Roger Keller, Faerstein Eduardo, Barros Aluisio JD. Racial Discrimination and Health: A Systematic Review of Scales With a Focus on Their Psychometric Properties. Social Science & Medicine. 2010;70(7):1091–99. doi: 10.1016/j.socscimed.2009.12.020. [DOI] [PubMed] [Google Scholar]
- Bateson Patrick, Barker David, Clutton-Brock Timothy, Deb Debal, D’Udine Bruno, Foley Robert A, Gluckman Peter, Godfrey Keith, Kirkwood Tom, Lahr Marta Mirazon, McNamara John, Metcalfe Neil B, Monaghan Patricia, Spencer Hamish G, Sultan Sonia E. Developmental Plasticity and Human Health. Nature. 2004;430(6998):419–21. doi: 10.1038/nature02725. [DOI] [PubMed] [Google Scholar]
- Bell Scott, Wilson Kathi, Bissonnette Laura, Shah Tayyab. Access to Primary Health Care: Does Neighborhood of Residence Matter? Annals of the Association of American Geographers. 2013;103(1):85–105. [Google Scholar]
- Berry John W. Acculturation and Adaptation in a New Society. International Migration. 1992;30(S1):69–85. [Google Scholar]
- Berry John W. Immigration, Acculturation, and Adaptation. Applied Psychology. 1997;46(1):5–34. [Google Scholar]
- Berry John W. Cross-Cultural Psychology: Research and Applications. Cambridge: Cambridge University Press; 2002. [Google Scholar]
- Berry John W. Acculturation: Living Successfully in Two Cultures. International Journal of Intercultural Relations. 2005;29(6):697–712. [Google Scholar]
- Berry John W, Annis Robert C. Acculturative Stress: The Role of Ecology, Culture and Differentiation. Journal of Cross-Cultural Psychology. 1974;5(4):382–406. [Google Scholar]
- Berry John W, Kim Uichol, Minde Thomas, Mok Doris. Comparative Studies of Acculturative Stress. International Migration Review. 1987;21(3):491–511. [Google Scholar]
- Berry John W, Kim Uichol, Power Steven, Young Marta, Bujaki Merridee. Acculturation Attitudes in Plural Societies. Applied Psychology. 1989;38(2):185–206. [Google Scholar]
- Bhattacharya Gauri. Health Care Seeking for HIV/AIDS among South Asians in the United States. Health & Social Work. 2004;29(2):106–15. doi: 10.1093/hsw/29.2.106. [DOI] [PubMed] [Google Scholar]
- Bhugra Dinesh, Arya Pradeep. Ethnic Density, Cultural Congruity and Mental Illness in Migrants. International Review of Psychiatry. 2005;17(2):133–37. doi: 10.1080/09540260500049984. [DOI] [PubMed] [Google Scholar]
- Birman Dina, Simon Corrina D, Chan Wing Yi, Tran Nellie. A Life Domains Perspective on Acculturation and Psychological Adjustment: A Study of Refugees from the Former Soviet Union. American Journal of Community Psychology. 2014;53(1/2):60–72. doi: 10.1007/s10464-013-9614-2. [DOI] [PubMed] [Google Scholar]
- Birman Dina, Taylor-Ritzler Tina. Acculturation and Psychological Distress among Adolescent Immigrants from the Former Soviet Union: Exploring the Mediating Effect of Family Relationships. Cultural Diversity and Ethnic Minority Psychology. 2007;13(4):337. doi: 10.1037/1099-9809.13.4.337. [DOI] [PubMed] [Google Scholar]
- Bisin Alberto, Patacchini Eleonora, Verdier Thierry, Zenou Yves. Bend It Like Beckham: Ethnic Identity and Integration. European Economic Review. 2016;90:146–64. [Google Scholar]
- Bjornstrom Eileen ES, Kuhl Danielle C. A Different Look at the Epidemiological Paradox: Self-Rated Health, Perceived Social Cohesion, and Neighborhood Immigrant Context. Social Science & Medicine. 2014;120:118–25. doi: 10.1016/j.socscimed.2014.09.015. [DOI] [PubMed] [Google Scholar]
- Boas F. The Aims of Ethnology. In: Boas Franz., editor. Race, Language, and Culture. New York: Macmillan; 1888. pp. 628–38. [Google Scholar]
- Bourhis Richard Y, Moise Lena Celine, Perreault Stephane, Senecal Sacha. Towards An Interactive Acculturation Model: A Social Psychological Approach. International Journal of Psychology. 1997;32(6):369–86. [Google Scholar]
- Brondolo Elizabeth, Hausmann Leslie RM, Jhalani Juhee, Pencille Melissa, Atencio-Bacayon Jennifer, Kumar Asha, Kwok Jasmin, Ullah Jahanara, Roth Alan, Chen Daniel, Crupi Robert, Schwartz Joseph. Dimensions of Perceived Racism and Self-Reported Health: Examination of Racial/Ethnic Differences and Potential Mediators. Annals of Behavioral Medicine. 2011;42(1):14–28. doi: 10.1007/s12160-011-9265-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabassa Leopoldo J. Measuring Acculturation: Where We Are and Where We Need to Go. Hispanic Journal of Behavioral Sciences. 2003;25(2):127–46. [Google Scholar]
- Cagney Kathleen A, Browning Christopher R, Wallace Danielle M. The Latino Paradox in Neighborhood Context: The Case of Asthma and Other Respiratory Conditions. American Journal of Public Health. 2007;97(5):919–25. doi: 10.2105/AJPH.2005.071472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Candib Lucy M. Obesity and Diabetes in Vulnerable Populations: Reflection on Proximal and Distal Causes. The Annals of Family Medicine. 2007;5(6):547–56. doi: 10.1370/afm.754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cano Miguel Ángel, Schwartz Seth J, Castillo Linda G, Unger Jennifer B, Huang Shi, Zamboanga Byron L, Romero Andrea J, Lorenzo-Blanco Elma I, Córdova David, Des Rosiers Sabrina E. Health Risk Behaviors and Depressive Symptoms among Hispanic Adolescents: Examining Acculturation Discrepancies and Family Functioning. Journal of Family Psychology. 2016;30(2):254. doi: 10.1037/fam0000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carte Traci A, Russell Craig J. In Pursuit of Moderation: Nine Common Errors and Their Solutions. Management Information Systems Quarterly. 2003;27(3):479–501. [Google Scholar]
- Castro Felipe Gonzalez. Emerging Hispanic Health Paradoxes. American Journal of Public Health. 2013;103(9):1541. doi: 10.2105/AJPH.2013.301529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro Felipe González, Kellison Joshua G, Boyd Stephen J, Kopak Albert. A Methodology for Conducting Integrative Mixed Methods Research and Data Analyses. Journal of Mixed Methods Research. 2010;4(4):342–60. doi: 10.1177/1558689810382916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro Felipe González, Marsiglia Flavio F, Kulis Stephen, Kellison Joshua G. Lifetime Segmented Assimilation Trajectories and Health Outcomes in Latino and Other Community Residents. American Journal of Public Health. 2010;100(4):669. doi: 10.2105/AJPH.2009.167999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro Felipe González, Shaibi Gabriel Q, Boehm-Smith Edna. Ecodevelopmental Contexts for Preventing Type 2 Diabetes in Latino and Other Racial/Ethnic Minority Populations. Journal of Behavioral Medicine. 2009;32(1):89–105. doi: 10.1007/s10865-008-9194-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavez Leo. Shadowed Lives: Undocumented Immigrants in American Society. 2. Belmont, CA: Cengage Learning; 2012. [Google Scholar]
- Chen Hongtu, Guarnaccia Peter J, Chung Henry. Self-Attention as a Mediator of Cultural Influences on Depression. International Journal of Social Psychiatry. 2003;49(3):192–203. doi: 10.1177/00207640030493005. [DOI] [PubMed] [Google Scholar]
- Chirkov Valery I, Lynch Martin, Niwa Sora. Application of the Scenario Questionnaire of Horizontal and Vertical Individualism and Collectivism to the Assessment of Cultural Distance and Cultural Fit. International Journal of Intercultural Relations. 2005;29(4):469–490. [Google Scholar]
- D’Anna-Hernandez Kimberly L, Aleman Brenda, Flores Ana-Mercedes. Acculturative Stress Negatively Impacts Maternal Depressive Symptoms in Mexican-American Women During Pregnancy. Journal of Affective Disorders. 2015;176:35–42. doi: 10.1016/j.jad.2015.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De La Rosa Mario, Vega Rodolfo, Radisch Matthew A. The Role of Acculturation in the Substance Abuse Behavior of African-American and Latino Adolescents: Advances, Issues, and Recommendations. Journal of Psychoactive Drugs. 2000;32(1):33–42. doi: 10.1080/02791072.2000.10400210. [DOI] [PubMed] [Google Scholar]
- Divi Chandrika, Koss Richard G, Schmaltz Stephen P, Loeb Jerod M. Language Proficiency and Adverse Events in US Hospitals: A Pilot Study. International Journal for Quality in Health Care. 2007;19(2):60–67. doi: 10.1093/intqhc/mzl069. [DOI] [PubMed] [Google Scholar]
- Eamon Mary Keegan, Mulder Cray. Predicting Antisocial Behavior among Latino Young Adolescents: An Ecological Systems Analysis. American Journal of Orthopsychiatry. 2005;75(1):117–27. doi: 10.1037/0002-9432.75.1.117. [DOI] [PubMed] [Google Scholar]
- Eschbach Karl, Mahnken Jonathan D, Goodwin James S. Neighborhood Composition and Incidence of Cancer Among Hispanics in the United States. Cancer. 2005;103(5):1036–44. doi: 10.1002/cncr.20885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eschbach Karl, Ostir Glenn V, Patel Kushang V, Markides Kyriakos S, Goodwin James S. Neighborhood Context snd Mortality among Older Mexican Americans: Is There a Barrio Advantage? Journal Information. 2004;94(10):1807–12. doi: 10.2105/ajph.94.10.1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch Brian Karl, Hummer Robert A, Kol Bohdan, Vega William A. The Role of Discrimination and Acculturative Stress in the Physical Health of Mexican-Origin Adults. Hispanic Journal of Behavioral Sciences. 2001;23(4):399–429. [Google Scholar]
- Flores Glenn. Language Barriers to Health Care in the United States. New England Journal of Medicine. 2006;355(3):229–31. doi: 10.1056/NEJMp058316. [DOI] [PubMed] [Google Scholar]
- Furunes Trude, Mykletun Reidar J. Age Discrimination in the Workplace: Validation of the Nordic Age Discrimination Scale (NADS) Scandinavian Journal of Psychology. 2010;51(1):23–30. doi: 10.1111/j.1467-9450.2009.00738.x. [DOI] [PubMed] [Google Scholar]
- Gagnon AJ. Royal Commission on the Future of Health Care in Canada (Romanow Commission) Ottawa: Health Canada; 2002. The Responsiveness of the Canadian Health Care System Towards Newcomers. [Google Scholar]
- Galchenko Irina, Van De Vijver Fons JR. The Role of Perceived Cultural Distance in the Acculturation of Exchange Students in Russia. International Journal of Intercultural Relations. 2007;31(2):181–97. [Google Scholar]
- Gallo Linda C, Penedo Frank J, De Los Monteros Karla Espinosa, Arguelles William. Resiliency in the Face of Disadvantage: Do Hispanic Cultural Characteristics Protect Health Outcomes? Journal of Personality. 2009;77(6):1707–46. doi: 10.1111/j.1467-6494.2009.00598.x. [DOI] [PubMed] [Google Scholar]
- Gee Gilbert C. A Multilevel Analysis of the Relationship Between Institutional and Individual Racial Discrimination and Health Status. American Journal of Public Health. 2002;92(4):615–23. doi: 10.2105/ajph.92.4.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzales Nancy A, Deardorff Julianna, Formoso Diana, Barr Alicia, Barrera Manuel. Family Mediators of the Relation Between Acculturation and Adolescent Mental Health. Family Relations. 2006;55(3):318–30. [Google Scholar]
- González Hector M, Haan Mary N, Hinton Ladson. Acculturation and the Prevalence of Depression in Older Mexican Americans: Baseline Results of the Sacramento Area Latino Study on Aging. Journal of the American Geriatrics Society. 2001;49(7):948–53. doi: 10.1046/j.1532-5415.2001.49186.x. [DOI] [PubMed] [Google Scholar]
- Hamaker Ellen L, Grasman Raoul PPP, Kamphuis Jan Henk. Regime-Switching Models to Study Psychological Process. In: Molenaar PCM, Newell KM, editors. Individual Pathways of Change: Statistical Models for Analyzing Learning and Development. Washington, DC: American Psychological Association; 2010. pp. 155–168. [Google Scholar]
- Hayes Andrew F. Statistical Methods for Communication Science. New York: Routledge; 2009. [Google Scholar]
- Hayes Andrew F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York: Guilford Press; 2013. [Google Scholar]
- Heilemann Marysue, Frutos Lisa, Lee Kathyrn, Kury Felix Salvador. Protective Strength Factors, Resources, and Risks in Relation yo Depressive Symptoms among Childbearing Women of Mexican Descent. Health Care for Women International. 2004;25(1):88–106. doi: 10.1080/07399330490253265. [DOI] [PubMed] [Google Scholar]
- Henry James P, Cassel John C. Psychosocial Factors in Essential Hypertension Recent Epidemiologic and Animal Experimental Evidence. American Journal of Epidemiology. 1969;90(3):171–200. doi: 10.1093/oxfordjournals.aje.a121062. [DOI] [PubMed] [Google Scholar]
- Herskovits Melville J. The Significance of the Study of Acculturation for Anthropology. American Anthropologist. 1937;39(2):259–64. [Google Scholar]
- Hornberger Nancy H. Language Policy, Language Education, Language Rights: Indigenous, Immigrant, and International Perspectives. Language in Society. 1998;27(4):439–58. [Google Scholar]
- Hunt Linda M, Schneider Suzanne, Comer Brendon. Should ‘Acculturation’ Be a Variable in Health Research? A Critical Review of Research on US Hispanics. Social Science & Medicine. 2004;59(5):973–86. doi: 10.1016/j.socscimed.2003.12.009. [DOI] [PubMed] [Google Scholar]
- Hwang Wei-Chin, Chun Chi-Ah, Takeuchi David T, Myers Hector F, Siddarth Prabha. Age of First Onset Major Depression in Chinese Americans. Cultural Diversity and Ethnic Minority Psychology. 2005;11(1):16–27. doi: 10.1037/1099-9809.11.1.16. [DOI] [PubMed] [Google Scholar]
- Kimbro Rachel Tolbert. Acculturation in Context: Gender, Age at Migration, Neighborhood Ethnicity, and Health Behaviors. Social Science Quarterly. 2009;90(5):1145–66. [Google Scholar]
- Kimbro Rachel Tolbert, Gorman Bridget K, Schachter Ariela. Acculturation and Self-Rated Health among Latino and Asian Immigrants to the United States. Social Problems. 2012;59(3):341–63. [Google Scholar]
- Komito Lee. Social Media and Migration: Virtual Community 2.0. Journal of the American Society For Information Science And Technology. 2011;62(6):1075–86. [Google Scholar]
- Korbin Jill E, Anderson-Fye Eileen P. Adolescence Matters: Practice- and Policy-Relevant Research and Engagement in Psychological Anthropology. Ethos. 2011;39(4):415–25. [Google Scholar]
- Kosic Ankica, Mannetti Lucia, Sam David Lackland. The Role of Majority Attitudes Towards Out-Group in the Perception of the Acculturation Strategies of Immigrants. International Journal of Intercultural Relations. 2005;29(3):273–88. [Google Scholar]
- Krieger Nancy. Embodying Inequality: A Review of Concepts, Measures, and Methods for Studying Health Consequences of Discrimination. International Journal of Health Services. 1999;29(2):295–352. doi: 10.2190/M11W-VWXE-KQM9-G97Q. [DOI] [PubMed] [Google Scholar]
- Kunitz SJ, Veazie M, Henderson JA. Historical Trends and Regional Differences in All-Cause and Amenable Mortality among American Indians and Alaska Natives Since 1950. American Journal Of Public Health. 2014;104(S3):S268–77. doi: 10.2105/AJPH.2013.301684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo Wen-Hung, Wilson Tracey E, Holman Susan, Fuentes-Afflick Elena, O’Sullivan Mary Jo, Minkoff Howard. Depressive Symptoms in the Immediate Postpartum Period among Hispanic Women Iin Three US Cities. Journal of Immigrant Health. 2004;6(4):145–53. doi: 10.1023/B:JOIH.0000045252.10412.fa. [DOI] [PubMed] [Google Scholar]
- Kuss Oliver. The Danger of Dichotomizing Continuous Variables: A Visualization. Teaching Statistics. 2013;35(2):78–79. [Google Scholar]
- Landis Ronald S, Dunlap William P. Moderated Multiple Regression Tests are Criterion Specific. Organizational Research Methods. 2000;3(3):254–66. [Google Scholar]
- Landrine Hope, Klonoff Elizabeth A. The Schedule of Racist Events: A Measure of Racial Discrimination and a Study of Its Negative Physical and Mental Health Consequences. Journal Of Black Psychology. 1996;22(2):144–68. [Google Scholar]
- Lara Marielena, Gamboa Cristina, Iya Kahramanian M, Morales Leo S, Hayes Bautista David E. Acculturation and Latino Health in the United States: A Review of the Literature and Its Sociopolitical Context. Annual Review of Public Health. 2005;26:367–97. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Min-Ah, Ferraro Kenneth F. Neighborhood Residential Segregation and Physical Health among Hispanic Americans: Good, Bad, or Benign? Journal of Health and Social Behavior. 2007;48(2):131–48. doi: 10.1177/002214650704800203. [DOI] [PubMed] [Google Scholar]
- Lee Sunmin, Chen Lu, He Xin, Miller Matthew J, Juon Hee-Soon. A Cluster Analytic Examination of Acculturation and Health Status among Asian Americans in the Washington DC Metropolitan Area, United States. Social Science & Medicine. 2013;96:17–23. doi: 10.1016/j.socscimed.2013.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Class Maria, Castro Felipe González, Ramirez Amelie G. Conceptions of Acculturation: A Review and Statement of Critical Issues. Social Science & Medicine. 2011;72(9):1555–62. doi: 10.1016/j.socscimed.2011.03.011. [DOI] [PubMed] [Google Scholar]
- Maccallum Robert C, Zhang Shaobo, Preacher Kristopher J, Rucker Derek D. On the Practice of Dichotomization of Quantitative Variables. Psychological Methods. 2002;7(1):19–40. doi: 10.1037/1082-989x.7.1.19. [DOI] [PubMed] [Google Scholar]
- Mak Winnie WS, Zane Nolan WS. The Phenomenon of Somatization among Community Chinese Americans. Social Psychiatry and Psychiatric Epidemiology. 2004;39(12):967–74. doi: 10.1007/s00127-004-0827-4. [DOI] [PubMed] [Google Scholar]
- Maxwell Scott E, Delaney Harold D. Bivariate Median Splits and Spurious Statistical Significance. Psychological Bulletin. 1993;113(1):181–90. [Google Scholar]
- Mcneilly Maya D, Anderson Norman B, Armstead Cheryl A, Clark Rodney, Corbett Marcella, Robinson Elwood L, Pieper Carl F, Lepisto Eva M. The Perceived Racism Scale: A Multidimensional Assessment of the Experience of White Racism among African Americans. Ethnicity & Disease. 1995;6(1/2):154–66. [PubMed] [Google Scholar]
- Miller Arlene Michaels, Birman Dina, Zenk Shannon, Wang Edward, Sorokin Olga, Connor Jorgia. Neighborhood Immigrant Concentration, Acculturation, and Cultural Alienation in Former Soviet Immigrant Women. Journal of Community Psychology. 2009;37(1):88–105. doi: 10.1002/jcop.20272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health. Addressing Health Disparities through Effective Interventions among Immigrant Populations (R01) Funding Opportunity Announcement (FOA) 2016a PA-17-043. [Google Scholar]
- National Institutes of Health. Addressing the Etiology of Health Disparities and Health Advantages among Immigrant Populations (R01) Funding Opportunity Announcement (FOA) 2016b PA-17-041. [Google Scholar]
- Neckerman Kathryn M, Carter Prudence, Lee Jennifer. Segmented Assimilation and Minority Cultures of Mobility. Ethnic and Racial Studies. 1999;22(6):945–65. [Google Scholar]
- Organista Pamela Balls, Organista Kurt C, Kurasaki Karen. The Relationship Between Acculturation and Ethnic Minority Health. Washington DC: American Psychological Association; 2003. [Google Scholar]
- Ostir Glenn V, Eschbach Karl, Markides Kyriakos S, Goodwin James S. Neighbourhood Composition and Depressive Symptoms among Older Mexican Americans. Journal Of Epidemiology and Community Health. 2003;57(12):987–92. doi: 10.1136/jech.57.12.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pablos-Méndez A. Letter to the Editor. Journal of the American Medical Association. 1994;271:1237–38. [Google Scholar]
- Palinkas Lawrence A, Pickwell Sheila M. Acculturation as a Risk Factor for Chronic Disease among Cambodian Refugees in the United States. Social Science & Medicine. 1995;40(12):1643–53. doi: 10.1016/0277-9536(94)00344-s. [DOI] [PubMed] [Google Scholar]
- Pantin Hilda, Schwartz Seth J, Sullivan Summer, Prado Guillermo, Szapocznik José. Ecodevelopmental HIV Prevention Programs for Hispanic Adolescents. American Journal of Orthopsychiatry. 2004;74(4):545–58. doi: 10.1037/0002-9432.74.4.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paradies Yin. A Systematic Review of Empirical Research on Self-Reported Racism and Health. International Journal of Epidemiology. 2006;35(4):888–901. doi: 10.1093/ije/dyl056. [DOI] [PubMed] [Google Scholar]
- Park Yoosun, Neckerman Kathryn M, Quinn James, Weiss Christopher, Rundle Andrew. Place of Birth, Duration of Residence, Neighborhood Immigrant Composition and Body Mass Index in New York City. International Journal of Behavioral Nutrition and Physical Activity. 2008;5(1):19. doi: 10.1186/1479-5868-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe Elizabeth A, Richman Laura Smart. Perceived Discrimination and Health: A Meta-Analytic Review. Psychological Bulletin. 2009;135(4):531–54. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel Kushang V, Eschbach Karl, Rudkin Laura L, Kristen Peek M, Markides Kyriakos S. Neighborhood Context and Self-Rated Health in Older Mexican Americans. Annals of Epidemiology. 2003;13(9):620–28. doi: 10.1016/S1047-2797(03)00060-7. [DOI] [PubMed] [Google Scholar]
- Pérez-Escamilla Rafael, Putnik Predrag. The Role of Acculturation in Nutrition, Lifestyle, and Incidence of Type 2 Diabetes among Latinos. The Journal Of Nutrition. 2007;137(4):860–70. doi: 10.1093/jn/137.4.860. [DOI] [PubMed] [Google Scholar]
- Pettigrew Thomas F, Meertens Roel W. Subtle and Blatant Prejudice in Western Europe. European Journal of Social Psychology. 1995;25(1):57–75. [Google Scholar]
- Portes Alejandro. Migration, Development, and Segmented Assimilation: A Conceptual Review of the Evidence. The Annals of the American Academy of Political and Social Science. 2007;610(1):73–97. [Google Scholar]
- Ra Chaelin Karen, Cho Youngtae, Hummer Robert A. Is Acculturation Always Adverse To Korean Immigrant Health in the United States? Journal of Immigrant and Minority Health. 2013;15:510–16. doi: 10.1007/s10903-012-9723-2. [DOI] [PubMed] [Google Scholar]
- Redfield Robert, Linton Ralph, Herskovits Melville J. Memorandum for the Study of Acculturation. American Anthropologist. 1936;38(1):149–52. [Google Scholar]
- Riosmena Fernando, Wong Rebeca, Palloni Alberto. Migration Selection, Protection, and Acculturation in Health: A Binational Perspective on Older Adults. Demography. 2012;50(3):1–26. doi: 10.1007/s13524-012-0178-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez Norma, Myers Hector F, Mira Consuelo Bingham, Flores Thomas, Garcia-Hernandez Loretta. Development of the Multidimensional Acculturative Stress Inventory for Adults of Mexican Origin. Psychological Assessment. 2002;14(4):451–61. [PubMed] [Google Scholar]
- Rubalcava Luis N, Teruel Graciela M, Thomas Duncan, Goldman Noreen. The Healthy Migrant Effect: New Findings from the Mexican Family Life Survey. Journal Information. 2008;98(1):78–84. doi: 10.2105/AJPH.2006.098418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rucker Derek D, Mcshane Blakeley B, Preacher Kristopher J. A Researcher’s Guide to Regression, Discretization, and Median Splits of Continuous Variables. Journal of Consumer Psychology. 2015;25(4):666–78. [Google Scholar]
- Rumbaut Ruben G. The Crucible Within: Ethnic Identity, Self-Esteem, and Segmented Assimilation among Children of Immigrants. International Migration Review. 1994;28(4):748–94. [Google Scholar]
- Salant Talya, Lauderdale Diane S. Measuring Culture: A Critical Review of Acculturation and Health in Asian Immigrant Populations. Social Science & Medicine. 2003;57(1):71–90. doi: 10.1016/s0277-9536(02)00300-3. [DOI] [PubMed] [Google Scholar]
- Sanou Dia, O’Reilly Erin, Ngnie-Teta Ismael, Batal Malek, Mondain Nathalie, Andrew Caroline, Newbold Brucek, Bourgeault Ivyl. Acculturation and Nutritional Health of Immigrants in Canada: A Scoping Review. Journal of Immigrant and Minority Health. 2013;15(2):1–11. doi: 10.1007/s10903-013-9823-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnittker Jason. Acculturation in Context: The Self-Esteem of Chinese Immigrants. Social Psychology Quarterly. 2002;65(1):56–76. [Google Scholar]
- Schwartz Seth J, Pantin Hilda, Sullivan Summer, Prado Guillermo, Szapocznik José. Nativity and Years in the Receiving Culture as Markers of Acculturation in Ethnic Enclaves. Journal of Cross-Cultural Psychology. 2006;37(3):345–53. doi: 10.1177/0022022106286928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz Seth J, Unger Jennifer B, Zamboanga Byron L, Szapocznik José. Rethinking the Concept of Acculturation: Implications for Theory and Research. American Psychologist. 2010;65(4):237–51. doi: 10.1037/a0019330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidman Edward, Allen Larue, Lawrence Aber J, Mitchell Christina, Feinman Joanna, Yoshikawa Hirokazu, Comtois Katherine Anne, Golz Judith, Miller Robin L, Ortiz-Torres Blanca. Development snd Validation of Adolescent-Perceived Microsystem Scales: Social Support, Daily Hassles, and Involvement. American Journal of Community Psychology. 1995;23(3):355–88. doi: 10.1007/BF02506949. [DOI] [PubMed] [Google Scholar]
- Shen Biing-Jiun, Takeuchi David T. A Structural Model of Acculturation and Mental Health Status among Chinese Americans. American Journal of Community Psychology. 2001;29(3):387–418. doi: 10.1023/A:1010338413293. [DOI] [PubMed] [Google Scholar]
- Sirin Selcuk R, Ryce Patrice, Gupta Taveeshi, Rogers-Sirin Lauren. The Role of Acculturative Stress on Mental Health Symptoms for Immigrant Adolescents: A Longitudinal Investigation. Developmental Psychology. 2013;49(4):736–49. doi: 10.1037/a0028398. [DOI] [PubMed] [Google Scholar]
- Smith NR, Kelly YJ, Nazroo JY. The Effects of Acculturation on Obesity Rates in Ethnic Minorities in England: Evidence from the Health Survey for England. European Journal of Public Health. 2012;22(4):508–13. doi: 10.1093/eurpub/ckr070. [DOI] [PubMed] [Google Scholar]
- Snowden Lonnie R, Masland Mary C, Peng Carol J, Lou Christine Wei-Mien, Wallace Neal T. Limited English Proficient Asian Americans: Threshold Language Policy and Access to Mental Health Treatment. Social Science & Medicine. 2011;72(2):230–37. doi: 10.1016/j.socscimed.2010.10.027. [DOI] [PubMed] [Google Scholar]
- Sökefeld Martin. Debating Self, Identity, and Culture in Anthropology. Current Anthropology. 1999;40(4):417–48. [Google Scholar]
- Sommerlad Elizabeth A, Berry John W. The Role of Ethnic Identification in Distinguishing Between Attitudes Towards Assimilation and Integration of a Minority Racial Group. Human Relations. 1970;23(1):23–29. [Google Scholar]
- Stephens Carolyn, Nettleton Clive, Porter John, Willis Ruth, Clark Stephanie. Indigenous Peoples’ Health—Why Are They Behind Everyone, Everywhere? The Lancet. 2005;366(9479):10–13. doi: 10.1016/S0140-6736(05)66801-8. [DOI] [PubMed] [Google Scholar]
- Stewart Andrew T, Chaplain Sylvia F, Epaphras Antony J, Gormley Patricia M, Killam Cheryl L, Metoyer Marie, Orr Gregory W, Rodriguez Ray R, Ruiz-Mingote Lina, Ali-Salaam Jibril, Taylor Patricia. Language and Access to Health Care: Easing Barriers n New Hampshire. Concord: New Hampshire Advisory Committee to the U.S. Commission on Civil Rights; 2005. [Google Scholar]
- Suanet Irina, Van De Vijver Fons JR. Perceived Cultural Distance and Acculturation among Exchange Students in Russia. Journal of Community & Applied Social Psychology. 2009;19(3):182–97. [Google Scholar]
- Suinn Richard M. Reviewing Acculturation and Asian Americans: How Acculturation Affects Health, Adjustment, School Achievement, and Counseling. Asian American Journal of Psychology. 2010;1(1):5–17. [Google Scholar]
- Sujoldžić Anita, Peternel Lana, Kulenović Tarik, Terzić Rifet. Social Determinants of Health: A Comparative Study of Bosnian Adolescents in Different Cultural Contexts. Collegium Antropologicum. 2006;30(4):703–11. [PubMed] [Google Scholar]
- Tardif-Williams Christine Yvette, Fisher Lianne. Clarifying the Link Between Acculturation Experiences and Parent-Child Relationships among Families in Cultural Transition: The Promise of Contemporary Critiques of Acculturation Psychology. International Journal of Intercultural Relations. 2009;33(2):150–61. [Google Scholar]
- Te Lindert Annet, Korzilius Hubert, Van De Vijver Fons JR, Kroon Sjaak, Arends-Tóth Judit. Perceived Discrimination and Acculturation among Iranian Refugees in the Netherlands. International Journal of Intercultural Relations. 2008;32(6):578–88. [Google Scholar]
- Timmins Caraway L. The Impact of Language Barriers on the Health Care of Latinos in the United States: A Review of the Literature and Guidelines for Practice. The Journal of Midwifery & Women’s Health. 2002;47(2):80–96. doi: 10.1016/s1526-9523(02)00218-0. [DOI] [PubMed] [Google Scholar]
- Turra Cassio M, Elo Irma T. The Impact of Salmon Bias on the Hispanic Mortality Advantage: New Evidence from Social Security Data. Population Research and Policy Review. 2008;27(5):515–30. doi: 10.1007/s11113-008-9087-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unger JB, Cruz TB, Rohrbach LA, Ribisl KM, Baezconde-Garbanati L, Chen X, Trinidad DR, Johnson CA. English Language Use as a Risk Factor for Smoking Initiation among Hispanic and Asian American Adolescents: Evidence for Mediation by Tobacco-Related Beliefs and Social Norms. Health Psychology. 2000;19(5):403–10. doi: 10.1037//0278-6133.19.5.403. [DOI] [PubMed] [Google Scholar]
- United Nations. Worldwide Displacement Hits All-Time High as War and Persecution Increase. Office Of The United Nations High Commissioner For Refugees. 2015 Jun 18; http://www.unhcr.org/558193896.html.
- United Nations. Public Health. Office Of The United Nations High Commissioner For Refugees. 2016 http://www.unhcr.org/pages/49c3646cdd.html.
- Van Oudenhoven Jan Pieter, Prins Karin S, Buunk Bram P. Attitudes of Minority and Majority Members Towards Adaptation of Immigrants. European Journal of Social Psychology. 1998;28(6):995–1013. [Google Scholar]
- Vanderweele Tyler J, Knol Mirjam J. A Tutorial on Interaction. Epidemiologic Methods. 2014;3(1):33–72. [Google Scholar]
- Vinokurov Andrey, Birman Dina, Trickett Edison. Psychological and Acculturation Correlates of Work Status among Soviet Jewish Refugees in the United States. International Migration Review. 2000;34(2):538–59. [Google Scholar]
- Vinokurov Andrey, Trickett Edison J. Ethnic Clusters in Public Housing and Independent Living Oof Elderly Immigrants from the Former Soviet Union. Journal of Cross-Cultural Gerontology. 2015;30(4):353–76. doi: 10.1007/s10823-015-9271-z. [DOI] [PubMed] [Google Scholar]
- Wandersman Abraham, Nation Maury. Urban Neighborhoods and Mental Health: Psychological Contributions to Understanding Toxicity, Resilience, and Interventions. American Psychologist. 1998;53(6):648–49. [PubMed] [Google Scholar]
- Ward Colleen, Kennedy Antony. Locus of Control, Mood Disturbance, and Social Difficulty During Cross-Cultural Transitions. International Journal of Intercultural Relations. 1992;16(2):175–94. [Google Scholar]
- Ward Colleen, Searle Wendy. The Impact of Value Discrepancies and Cultural Identity on Psychological and Sociocultural Adjustment of Sojourners. International Journal of Intercultural Relations. 1991;15(2):209–24. [Google Scholar]
- Waters Mary C, Tran Van C, Kasinitz Philip, Mollenkopf John H. Segmented Assimilation Revisited: Types of Acculturation and Socioeconomic Mobility in Young Adulthood. Ethnic and Racial Studies. 2010;33(7):1168–93. doi: 10.1080/01419871003624076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisner Thomas S. ‘If You Work in This Country You Should Not Be Poor, and Your Kids Should Be Doing Better’: Bringing Mixed Methods and Theory in Psychological Anthropology to Improve Research in Policy and Practice. Ethos. 2011;39(4):455–76. [Google Scholar]
- Weitoft G Ringbäck, Gullberg Anders, Hjern Anders, Rosén Måns. Mortality Statistics in Immigrant Research: Method for Adjusting Underestimation of Mortality. International Journal of Epidemiology. 1999;28(4):756–63. doi: 10.1093/ije/28.4.756. [DOI] [PubMed] [Google Scholar]
- Wike Richard, Kohut Andrew. Assessing Globalization. Harvard International Review. 2008 Jul 8; http://hir.harvard.edu/pew-research-center-assessing-globalization/
- Williams David R, Gonzalez Hector M, Williams Stacey, Mohammed Selina A, Moomal Hashim, Stein Dan J. Perceived Discrimination, Race snd Health in South Africa. Social Science & Medicine. 2008;67(3):441–52. doi: 10.1016/j.socscimed.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams David R, Yu Yan, Jackson James S, Anderson Norman B. Racial Differences in Physical and Mental Health Socio-Economic Status, Stress and Discrimination. Journal of Health Psychology. 1997;2(3):335–51. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Winkelman Michael. Culture and Health: Applying Medical Anthropology. San Francisco, CA: John Wiley & Sons; 2008. [Google Scholar]
- Yonkers Kimberly A, Ramin Susan M, John Rush A, Navarrete Carlos A, Carmody Thomas, March Dana, Heartwell Stephen F, Leveno Kenneth J. Onset and Persistence of Postpartum Depression in an Inner-City Maternal Health Clinic System. American Journal of Psychiatry. 2001;158(11):1856–63. doi: 10.1176/appi.ajp.158.11.1856. [DOI] [PubMed] [Google Scholar]
- Zhou Min. Segmented Assimilation: Issues, Controversies, and Recent Research on the New Second Generation. International Migration Review. 1997;31(4):975–1008. [PubMed] [Google Scholar]
- Zlobina Anna, Basabe Nekane, Paez Dario, Furnham Adrian. Sociocultural Adjustment of Immigrants: Universal and Group-Specific Predictors. International Journal of Intercultural Relations. 2006;30(2):195–211. [Google Scholar]