Abstract
Background:
Several studies have revealed that high shock index (SI) is a risk factor for acute myocardial infarction (AMI) patients. These studies do not give a systematic review in this issue. Therefore, we conducted a systematic review and meta-analysis to determine the effect of high SI on the prognosis of AMI patients.
Methods:
We did a systematic search of PubMed, Embase, and the Cochrane Library, using various combinations of keywords such as “shock index,” “shock-index,” “acute myocardial infarction,” “ST elevation myocardial infarction,” “non-ST segment elevation myocardial infarction,” “STEMI,” “NSTEMI,” “AMI,” and “MI” for eligible studies published up to December 23, 2016. The 3 primary outcomes for this analysis were all-cause in-hospital mortality, short-term adverse outcomes, and long-term adverse outcomes.
Results:
Database searches retrieved 226 citations. Finally, 8 studies enrolling 20,404 patients were eventually included in the analysis. High SI was associated with an increased in-hospital mortality (pooled RR = 10.96, 95% CI: 2.00–59.94, P = .01). Adverse outcomes were significantly higher in the high SI group compared to the low SI group (pooled RR = 1.93, 95% CI: 1.10–3.39, P = .02; I2 = 95%). Individuals with high SI had an increased risk of long-term adverse outcomes (pooled RR = 2.31, 95% CI: 1.90–2.81, P < .001) compared to low SI.
Conclusion:
High SI may increase the in-hospital mortality, short-term, and long-term adverse outcomes in AMI patients.
Keywords: acute myocardial infarction, prognosis, meta-analysis, shock index
1. Introduction
The concept of shock index (SI), defined as the ratio of heart rate to systolic blood pressure, has been coined by Allgower and Burri.[1] It has been originally used to evaluate the degree of hypovolemia in hemorrhagic and infectious shock states.[1]
Then SI has been widely used for predicting outcomes in other critically ill patients, for example, those with severe sepsis[2,3] and pulmonary embolism.[4,5]
Recently several studies have revealed that high SI is a risk factor for acute myocardial infarction (AMI) patients, particularly for the ST elevated myocardial infarction patients.[6–13] Huang and his colleagues explored that patients with SI ≥0.7 had a 2.2-fold increased risk of 7-day all-cause mortality and 1.9-fold increased risk of 30-day all-cause mortality.[7] Another study has demonstrated that admission SI ≥0.66 were identified as an independent predictor of major adverse cardiac events (MACEs) with a cumulative hazard ratio for 5-year MACEs of 2.14.[10] Elevated SI has also been shown as a risk factor of in-hospital mortality in patients undergoing primary percutaneous coronary intervention (PCI).[8]
Although more and more studies have revealed the prognostic value of elevated SI in the AMI patients, the quality of the studies vary widely.[6,7,10,11,13] Up to now, there has been no systematic review to evaluate the relationship between elevated SI and the in-hospital, short-term, and long-term adverse outcome, respectively. Therefore, we conducted a systematic review and meta-analysis of clinical trials to determine the effect of high SI on the prognosis of AMI patients.
2. Material and methods
This systematic review and meta-analysis were performed according to the guidelines set forth in Preferred Reporting Items for Systematic Reviews and Meta-Analyses.[14] The ethical approval was not necessary because the meta-analysis was based on data from previously published studies.
2.1. Search strategy
We searched scientific literature databases for trials assessing the prognostic value of SI in patients with AMI. We did a systematic search of PubMed, Embase, and the Cochrane Library, using various combinations of keywords such as “shock index,” “shock-index,” “acute myocardial infarction,” “ST elevation myocardial infarction,” “non-ST segment elevation myocardial infarction,” “STEMI,” “NSTEMI,” “AMI,” and “MI” for eligible studies published up to April 10, 2017 (see Fig. 1 for detailed search strategy). English language was considered for inclusion; no other languages were allowed. The search was conducted by 2 independent researchers (XZ and ZW).
Figure 1.
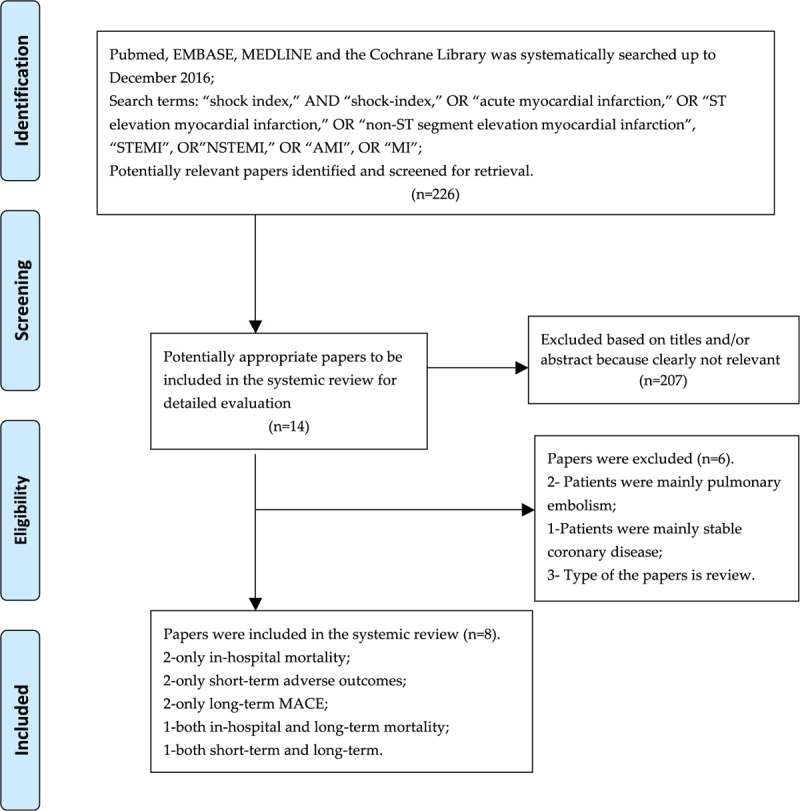
Flow of chart.
2.2. Selection criteria
We included clinical trials to investigate the relationship between the prognostic value of SI and acute coronary infarction. Inclusion criteria for studies were adult patients with AMI, with SI accessed as a risk factor. We excluded studies which were only available in the abstract and number of patients less than 100 patients. We also excluded that patients whose heart rate or systolic blood pressure were not recorded correctly.
Relevant studies identified by the search strategy were reviewed by the title and abstract, and excluded if they were not relevant to the research target by 3 investigators (XZ, ZW, and ZW). According to inclusion and exclusion criteria, the potentially eligible studies were then retrieved in the full text. If the potential studies exhibited divergence, then a fourth investigator (ZS) made the final decision. Citations of retrieved full text were also discreetly screened for other eligible studies.
2.3. Data extraction
Three independent investigators (XZ, ZW, and ZW) sorted and extracted information about details of the publications (ie, authors, year of publication), study design, sample size, inclusion/exclusion criteria, demographics (patients’ age and gender), and SI-related information (ie, heart rate, systolic blood pressure, the value of SI and SI categories). And outcome definitions, events were collected and collated, mainly all-cause mortality or major adverse cardiovascular events. Discrepancies were resolved by consensus between the study investigators, if necessary, after discussing with authors.
2.4. Outcomes
The 3 primary outcomes for this analysis were all-cause in-hospital mortality, short-term adverse outcomes, and long-term adverse outcomes.
The high SIs included in the systemic review and meta-analysis were defined as the highest categories of SI and the others as low SI. If the included studies have evaluated the adjusted confounding factors, the adjusted hazard risks or odds ratios should be given priority to be extracted.
2.5. Statistical analysis
All the potential references for this systemic review and meta-analysis were managed by the EndNote software. All the analyses were performed using Review Manager (RevMan version 5.3; Cochrane Collaboration, Oxford, UK). We used the Cochrane Handbook for methodological guidance. The unadjusted and multivariable-adjusted risk estimates for categorical (high versus low categories) outcome data (odds ratios, hazard risks, and 95% confidence intervals [CIs]) were transformed logarithmically in each study.
Relative risks (RRs) were used to pool outcomes with a 2-sided significance level of 5%. Multivariate-adjusted outcome data (expressed as RRs and 95% CIs) were used for analysis. We logarithmically transformed these values in each study and calculated the corresponding SEs. The statistical analysis used the inverse variance approach to combine log RRs and SEs. We assessed heterogeneity with the I2 test, and the studies were pooled using fixed-effects models with low heterogeneity (I2 < 50%).[15] Otherwise, a random-effects model was used. Publication bias was assessed by inspecting funnel plots for each outcome in which the log (RR) was plotted against SE. Sensitivity analyses were conducted in which the pooled RR was recalculated by omitting 1 study at a time. However, the sensitivity analyses were also performed by the use of fixed-effects models compared with random-effects models. Newcastle-Ottawa Scale (NOS) was used to assess the quality of included studies.[16]
3. Results
Three hundred twenty-six citations were retrieved by database searches and reference screening. Most papers were excluded based on titles and/or abstract because clearly not relevant or duplicated. Fourteen potentially appropriate papers were included for the full text review. According to the inclusion criteria, 8 studies enrolling 20,404 patients were eventually included in the systemic review and meta-analysis. Of the 8 studies, 2 showed only in-hospital mortality,[6,13] 2 reported only short-term adverse outcomes,[7,9] 2 assessed only long-term MACE,[10,12] 1 evaluated both in-hospital and long-term mortality,[8] and 1 measured both short-term and long-term mortality.[11] Therefore, there were 3, 3, and 4 studies for the analyses of in-hospital mortality, short-term, and long-term adverse outcomes, respectively.
3.1. Description of included studies and quality assessment
The baselines of study characteristics are summarized in Table 1. Average age across all studies is over 60 years. All of the studies involved males (range, 64.00%–82.50%), with a follow-up period ranging from 7 days to 5 years. Six studies just focused on the population of STEMI patients. Seven studies reported the cardiac shock patients, ranged from 0.63% to 14.91%. Most of the studies classified cut-off point of SI around 0.7 based on ROC or previous studies presented. The potential confounding adjusted factors differed across studies.
Table 1.
Study and participant summary characteristics.
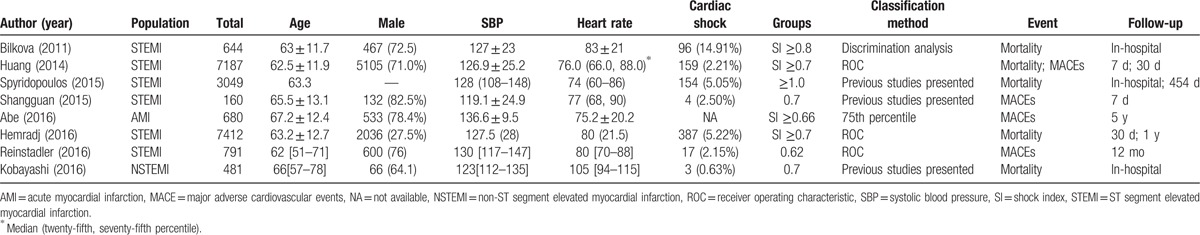
Study quality, as Table 2 specified, was relatively high. Based on the NOS quality assessment, 4 studies were defined as high quality (1 study scored 8 and 4 studies scored 7), and the other 3 studies were defined as moderate quality (3 studies scored 6).
Table 2.
Assessment of study quality.
3.2. Quantitative data synthesis
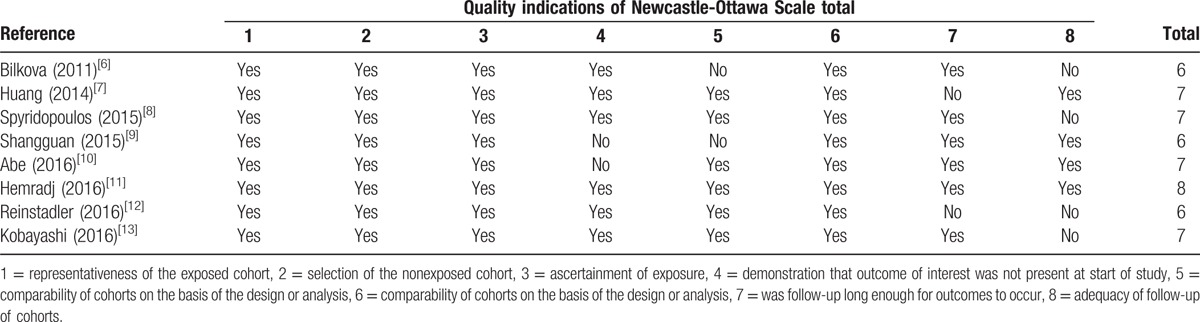
3.2.1. High SI and in-hospital mortality
The analysis pooled data for in-hospital mortality for 4174 patients from 3 studies.[6,8,13] Data sets were heterogeneous (I2 = 77%); therefore, random-effects models were used for this analyses. Overall, high SI was associated with an increased in-hospital mortality after multivariate adjustment (pooled RR = 10.96, 95% CI: 2.00–59.94, P = .01) (Fig. 2). However, the cut-off points of SI were divergence, ranged from 0.7 to 1.0.
Figure 2.
The relationship between in-hospital mortality and high SI. SI = shock index.
3.2.2. High SI and short-term adverse outcomes
Three studies evaluated the influence of high SI on the prognosis in 14,759 STEMI patients.[7,9,11] Adverse outcomes (all-cause mortality or MACE) were significantly higher in the high SI group compared with the low SI group (pooled RR = 1.93, 95% CI: 1.10–3.39, P = .02; I2 = 95%) (Fig. 3). Fortunately, in the 3 included studies, threshold of high SI were all defined as more than 0.7.
Figure 3.
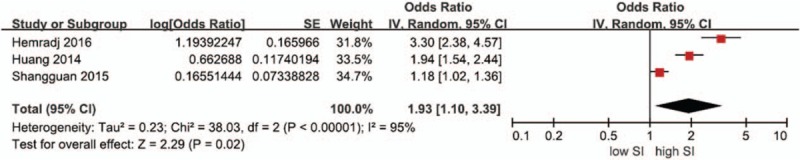
The relationship between short-term adverse outcomes and high SI. SI = shock index.
3.2.3. High SI and long-term adverse outcomes
The analysis pooled data on long-term adverse outcomes for 11,932 participants from 4 studies.[8,10–12] The Figure 4 forest plot presents the association between elevated SI and long-term adverse outcomes compared with low SI (Fig. 4). A statistical heterogeneity (I2 = 0%) was observed, so the fixed-effect model was performed. The meta-analysis of the 4 studies revealed that individuals with high SI had an increased risk of long-term adverse outcomes (pooled RR = 2.31, 95% CI: 1.90–2.81, P < .001) compared with low SI.
Figure 4.
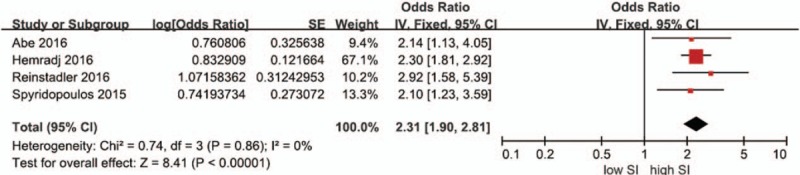
The relationship between long-term adverse outcomes and high SI. SI = shock index.
3.3. Heterogeneity among included studies
Due to the differences in the cut-point of SI and duration of follow-up and the small number of events of some studies, we could not explore the sources of heterogeneity with subgroup analysis or meta-regression.
3.4. Publication bias and funnel plots
Owing to the small number of included studies on the influence of SI on adverse outcomes of patients with AMI, with a maximum of 4 studies investigating high SI and long-term adverse outcomes, the graphical or statistical assessment of publication bias was not sensitive. The funnel plots showed each comparison outcomes (Fig. 5).
Figure 5.
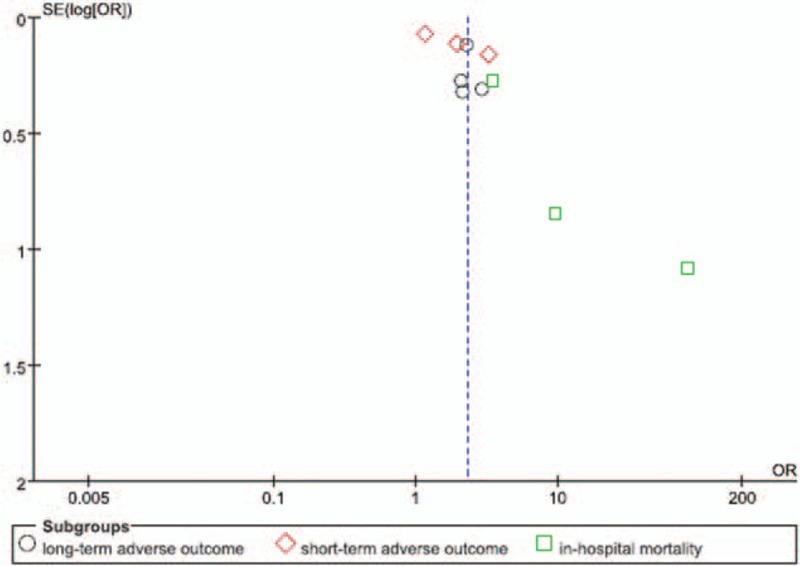
The funnel plots showed each comparison outcomes.
3.5. Sensitivity analyses
Two methods were used to perform the sensitivity analyses and found that the primary results were not influenced by the use of fixed-effects models compared with random-effects models and recalculation by omitting 1 study at a time.
4. Discussion
In this systemic review and meta-analysis including 8 studies for more than 20,000 AMI patients, we demonstrated high SI as a risk factor for AMI patients, despite in-hospital mortality, short-term or long-term adverse outcomes. In most of the included studies, the cut-off of SI was around 0.7.
SI ratio of 2 important hemodynamics parameters, is increasingly been recognized as a crucial risk factor for cardiovascular disease, such as pulmonary embolism[4] and AMI.[8,9,12,13] Recently more and more studies have focused the prognostic value of SI for the AMI patients. However, there are no systematic reviews to evaluate the SI as a risk factor. Our systematic review and meta-analysis is the first one to include 3 categories of adverse outcomes, in-hospital mortality, short-term, and long-term adverse cardiovascular outcomes, respectively.
For the sake of quantitative analysis or the clinical practices, the SI was divided in 2 parts, high or low SI, based on what previous studies reported or receiver operating characteristic (ROC) curve. AMI patients with high SI had a 10.96-fold increased risk of in-hospital mortality, 1.93-fold increased risk of short-term adverse outcomes, and 2.31-fold increase risk of long-term adverse outcomes. Therefore, we should not just focus on the heart rate and systolic blood pressure, as SI may also provide additional values for the AMI patients.
Cardiogenic shock has previously been demonstrated as a strong and independent predictor of both short-term and long-term mortality in patients with AMI.[17] Although the prognosis of AMI has been improved, the prognosis of cardiogenic shock is still poor.[18] SI, a sample algorithm, has been shown to be more sensitive than cardiogenic shock.[11] The sensitive value of SI may help detect the pre-shock AMI patients earlier to improve the prognosis.
In this systematic review, the threshold of SI is around 0.7 in 7 out of 8 studies, mostly based on ROC curve. This may reveal that the cut-off should be defined as 0.7 in the future clinical practice and research studies.
Up to now, only 1 study has shown the relationship between modified SI and the prognosis of AMI, which has revealed modified SI may be more accurate than SI.[9] In the future, more studies should pay attention to the modified SI.
The reason why SI is associated with the adverse outcomes in patients with AMI remains to be elucidated. However, several possible interpretations may be performed. In the setting of AMI, a series of neurohumoral reactions are aroused, of which sympathetic nerve activation is the most significant.[19] Therefore, blood pressure and heart rate level after AMI may reflect the integrated hemodynamics status and neuroendocrine system.[7]
Moreover, SI is a relatively objective indicator independently of systolic blood pressure and heart rate in the state of pain and anxiety,[20] which cause a concurrent increase of heart rate and systolic blood pressure.
5. Study limitations
There are several potential limitations to the present systematic review and meta-analysis. First, given the lack of prospective trial data, further prospective trials are needed to verify these findings in this population. Second, there was significant heterogeneity among the included 8 studies for the analysis relationship between in-hospital mortality or short-term adverse outcomes and high SI. However, we could not identify the sources of heterogeneity as a result of the limited number of included studies for each outcome. Third, the included studies do not have the same criteria for high SI, which may have substantial detrimental effect on the explanation of the pooled results. Fortunately, most of the included studies have defined high SI around 0.7.
6. Conclusion
Our systematic review and meta-analysis reveals that high SI may increase the in-hospital mortality, short-term, and long-term adverse outcomes in AMI patients. In the future, we should not only focus on heart rate and systolic blood pressure, but also pay special attention on ratio of the 2 parameters for the AMI patients, which may be more accurate and sensitive.
Footnotes
Abbreviations: AMI = acute myocardial infarction, CI = confidence interval, MACEs = major adverse cardiac events, RR = relative risk, SI = shock index.
The authors declare that they have no conflicts of interests.
References
- [1].Allgower M, Burri C. Shock index. Dtsch Med Wochenschr 1967;92:1947–50. [DOI] [PubMed] [Google Scholar]
- [2].Rousseaux J, Grandbastien B, Dorkenoo A, et al. Prognostic value of shock index in children with septic shock. Pediatr Emerg Care 2013;29:1055–9. [DOI] [PubMed] [Google Scholar]
- [3].Yussof SJ, Zakaria MI, Mohamed FL, et al. Value of Shock Index in prognosticating the short-term outcome of death for patients presenting with severe sepsis and septic shock in the emergency department. Med J Malaysia 2012;67:406–11. [PubMed] [Google Scholar]
- [4].Toosi MS, Merlino JD, Leeper KV. Prognostic value of the shock index along with transthoracic echocardiography in risk stratification of patients with acute pulmonary embolism. Am J Cardiol 2008;101:700–5. [DOI] [PubMed] [Google Scholar]
- [5].Otero R, Trujillo-Santos J, Cayuela A, et al. Haemodynamically unstable pulmonary embolism in the RIETE Registry: systolic blood pressure or shock index? Eur Respir J 2007;30:1111–6. [DOI] [PubMed] [Google Scholar]
- [6].Bilkova D, Motovska Z, Widimsky P, et al. Shock index: a simple clinical parameter for quick mortality risk assessment in acute myocardial infarction. Can J Cardiol 2011;27:739–42. [DOI] [PubMed] [Google Scholar]
- [7].Huang B, Yang Y, Zhu J, et al. Usefulness of the admission shock index for predicting short-term outcomes in patients with ST-segment elevation myocardial infarction. Am J Cardiol 2014;114:1315–21. [DOI] [PubMed] [Google Scholar]
- [8].Spyridopoulos I, Noman A, Ahmed JM, et al. Shock-index as a novel predictor of long-term outcome following primary percutaneous coronary intervention. Eur Heart J Acute Cardiovasc Care 2015;4:270–7. [DOI] [PubMed] [Google Scholar]
- [9].Shangguan Q, Xu JS, Su H, et al. Modified shock index is a predictor for 7-day outcomes in patients with STEMI. Am J Emerg Med 2015;33:1072–5. [DOI] [PubMed] [Google Scholar]
- [10].Abe N, Miura T, Miyashita Y, et al. Long-term prognostic implications of the admission shock index in patients with acute myocardial infarction who received percutaneous coronary intervention. Angiology 2016;68:339–45. [DOI] [PubMed] [Google Scholar]
- [11].Hemradj VV, Ottervanger JP, de Boer MJ, et al. Shock index more sensitive than cardiogenic shock in ST-elevation myocardial infarction treated by primary percutaneous coronary intervention. Circ J 2016;81:199–205. [DOI] [PubMed] [Google Scholar]
- [12].Reinstadler SJ, Fuernau G, Eitel C, et al. Shock index as a predictor of myocardial damage and clinical outcome in ST-elevation myocardial infarction. Circ J 2016;80:924–30. [DOI] [PubMed] [Google Scholar]
- [13].Kobayashi A, Misumida N, Luger D, et al. Shock Index as a predictor for In-hospital mortality in patients with non-ST-segment elevation myocardial infarction. Cardiovasc Revasc Med 2016;17:225–8. [DOI] [PubMed] [Google Scholar]
- [14].Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 2009;151:W65–94. [DOI] [PubMed] [Google Scholar]
- [15].Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Margulis AV, Pladevall M, Riera-Guardia N, et al. Quality assessment of observational studies in a drug-safety systematic review, comparison of two tools: the Newcastle-Ottawa Scale and the RTI item bank. Clin Epidemiol 2014;6:359–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Hochman JS. Cardiogenic shock complicating acute myocardial infarction: expanding the paradigm. Circulation 2003;107:2998–3002. [DOI] [PubMed] [Google Scholar]
- [18].Subramaniam S, Rutman M. Cardiogenic shock. Pediatr Rev 2015;36:225–6. [DOI] [PubMed] [Google Scholar]
- [19].Graham LN, Smith PA, Stoker JB, et al. Sympathetic neural hyperactivity and its normalization following unstable angina and acute myocardial infarction. Clin Sci 2004;106:605–11. [DOI] [PubMed] [Google Scholar]
- [20].Keller AS, Kirkland LL, Rajasekaran SY, et al. Unplanned transfers to the intensive care unit: the role of the shock index. J Hosp Med 2010;5:460–5. [DOI] [PubMed] [Google Scholar]


