Abstract
Although surgical outcomes of totally laparoscopic total gastrectomy (TLTG) have been reported from several centers, the effectiveness of this technique has not been conclusively established. The aim of this study was to investigate the feasibility, safety, and efficacy of TLTG for gastric cancer.
A prospectively collected and retrospectively analyzed data were used by comparing the short-term surgical outcomes of 124 patients who underwent TLTG with those of 124 patients who underwent open total gastrectomy (OTG) between March 2007 and March 2016.
The 2 groups were well matched with respect to age, sex, body mass index, ASA score, and tumor stage. There was no significant difference with regard to the operation time but TLTG showed significantly less intraoperative blood loss (115.5 ± 70.2 vs 210.5 ± 146.7 mL, P < .01). Total numbers of retrieved lymph nodes were similar in the 2 groups. Postoperatively, no significant differences were found for morbidity or mortality. The time to first flatus, initiate oral intake, and postoperative hospital stay were significantly shorter in the TLTG group than in the OTG group (3.2 ± 1.0 vs 4.1 ± 1.2 days; 4.4 ± 1.2 vs 5.6 ± 2.0 days; and 8.9 ± 3.1 vs 11.3 ± 4.5 days, respectively; P < .01).
TLTG for gastric cancer is technically safe, feasible, and minimally invasive compared with OTG. A prospective randomized trial is needed to establish the value of TLTG.
Keywords: intracorporeal anastomosis, laparoscopic gastrectomy, morbidity, stomach neoplasms
1. Introduction
Gastric cancer is one of the most commonly causes of cancer-related death worldwide.[1] Despite the rapid progress in molecular understanding of gastric cancer and development of targeted treatments, the only therapeutic option now to improve the lifetime of these patients is surgical resection. The standard surgical procedure is gastrectomy with adequate lymphadenectomy, which can now be performed laparoscopically in some specialized centers.[2] The number of patients undergoing laparoscopy-assisted gastrectomy (LAG) is rapidly increasing.[2] However, the extension of laparotomy is often necessary to obtain a better view for secure anastomosis in obese patients.[3] Furthermore, the procedure is more difficult in cases requiring transection at a more proximal site, because of the limited space even under larger auxiliary incision. Therefore, totally laparoscopic gastrectomy (TLG) has gradually increased.[4] The potential advantages of TLG include safer anastomosis under better visualization as well as a smaller scar and less pain.[5–7] However, totally laparoscopic total gastrectomy (TLTG) is performed by limited surgeons, which demands advanced expertise in the lymphadenectomy at the splenic hilum and esophagojejunostomy.[8,9] Based on our extensive laparoscopic experience obtained from performing laparoscopic pancreatic, gastric, and other operations,[10] we developed TLTG using intracorporeally stapler or hand-sewn anastomosis for middle or upper gastric cancer.[8] Here, we conducted a case-matched study to evaluate the feasibility, advantages, and drawbacks of TLTG by comparing with conventional open total gastrectomy (OTG).
2. Materials and methods
2.1. Patients
This research was approved by the Zhejiang University's Ethics Committee. Between March 2007 and March 2016, a total of 3268 patients diagnosed with gastric adenocarcinoma were treated by curative resection at Sir Run Shaw Hospital. A total of 1258 of these neoplasms were resected by laparoscopic approach and 2010 by open technique. All gastrectomy procedures were performed by experienced gastrointestinal surgeons. The indication for laparoscopic gastrectomy was gastric cancer without evidences of invasion to adjacent organs or distal metastasis. Patients were informed of the possible complications as well as advantages and disadvantages of these 2 approaches. Then, the surgical method of laparoscopic or open approach was decided by patients and their families. Written consent was obtained from every patient prior to surgery. When we retrospectively analyzed the gastric cancer database, gastrectomy other than total gastrectomy such as distal or proximal gastrectomy, wedge resection was firstly excluded. Cases of combined resection were also excluded. Then, for laparoscopic cases, all LAG cases were excluded, thus only leaving TLTG cases. Therefore, 124 cases of TLTG and 656 cases of OTG were included in this comparative study. To overcome the selection bias, we designed a matched case–control study. All data were collected by an experienced data collection assistant and analyzed by a medical statistician who matched all cases for gender, age (±5 years), American Society of Anesthesiologists Physical Status score (ASA), differentiation, and tumor-node-metastasis (TNM) stage of tumor. Finally, 248 patients (124 TLTG: 124 OTG) were identified.
We studied patient demographic information, surgical procedure, and postoperative courses. The following data were collected: age, sex, body mass index, ASA score, comorbidities, operative time, estimated blood loss, complications, hospital stay, and pathological findings. Postoperative complications were stratified according to the Clavien–Dindo classification, which defines major complications by a score ≥ 3.[11] The anastomosis-related complications included anastomotic leakage, hemorrhage, and stricture or stenosis. Pathological and clinical staging was determined based on the American Joint Committee on Cancer (the 7th edition) and the TNM classification scheme.
2.2. Surgical procedure
Under general anesthesia, the patient was placed in supine position. Lymphadenectomy was performed according to the guidelines of the Japanese Gastric Cancer Association, which included No. 8a, 9, 10, 11, and 12a in addition to D1 dissection.[12] At our institution, total gastrectomy is performed via totally laparoscopic surgery with antecolic Roux-en-Y reconstruction using following methods: type A: conventional circular stapler-anvil method; type B: trans-orally inserted anvil (OrVilTM, 25 mm; Covidien, Mansfield, MA) method; type C: linear stapler side-to-side method; type D: linear stapler delta-shaped method; and type E: hand-sewn end-to-side method. The detailed lymphadenectomy and reconstruction procedure were described in our previously published articles.[8] Open surgery was performed in the same manner as laparoscopic surgery through an upper midline incision. The anastomosis methods included stapler or sewn depending on the surgeon's habits.
2.3. Statistical analysis
Quantitative data were expressed as means ± standard deviations. The Student t test was used to compare continuous variables, whereas chi-square analysis or Fisher exact tests were used to compare categorical variables. P < .05 was considered statistically significant. All statistical analyses were performed using SPSS version 20.0 (SPSS, Inc).
3. Results
3.1. Clinicopathological characteristics
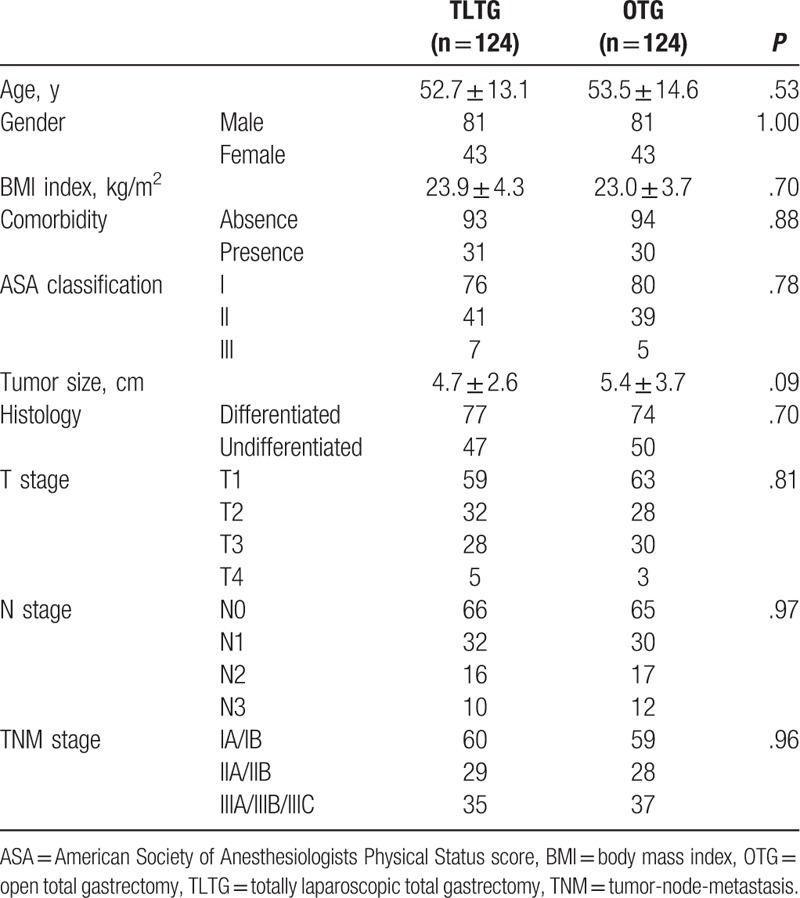
The variables including age, sex, body mass index, and TNM stage were well matched. There were 124 cases (81 males and 43 females) included in the TLTG group with a mean age of 52.7 years old. Thirty-one cases had comorbidities, 76 cases achieved ASA score I, 41 cases achieved score II, and 7 cases achieved score III. The mean tumor size of cases in TLTG was 4.7 cm, with differentiated type of 77. According to the American Joint Committee on Cancer (the 7th edition), 60 cases were diagnosed with stage I, 29 cases with stage II, and 35 cases with stage III. The clinicopathological characteristics of TLTG and OTG were summarized in Table 1.
Table 1.
Comparison of the clinicopathological characteristics.
3.2. Surgical outcomes
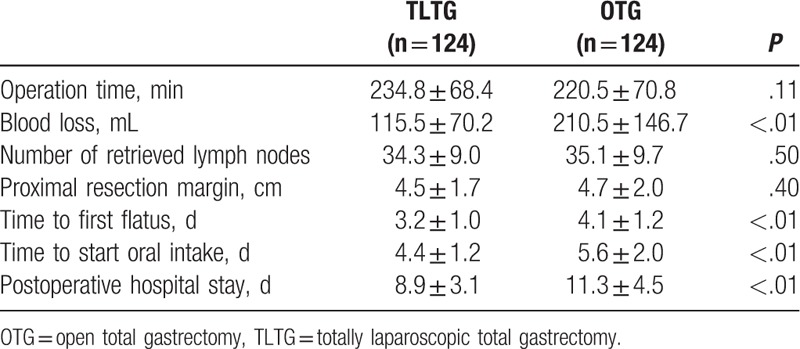
The surgical outcomes were showed in Table 2. The types of TLTG were as follow: type A (n = 14), type B (n = 28), type C (n = 22), type D (n = 10), and type E (n = 50). Compared with OTG, TLTG had similar operation time (234.8 vs 220.5 minutes, P = .11). The intraoperative blood loss was significantly less in TLTG (115.5 vs 210.5 mL, P < .01). TLTG retrieved lymph nodes no less than OTG, with similar proximal resection margin. The postoperative time to first flatus, time to first oral intake, and length of hospital stay was shorter in TLTG.
Table 2.
Comparison of surgical outcomes and postoperative recovery.
3.3. Postoperative morbidity
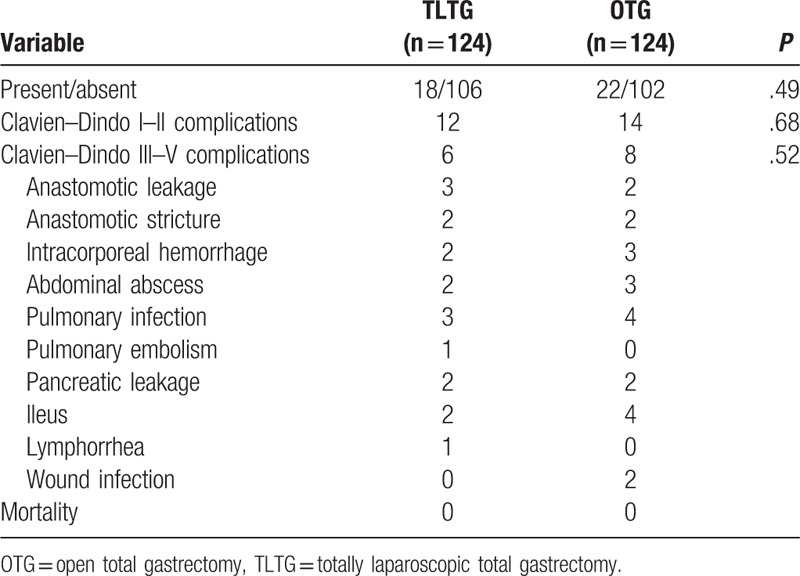
Eighteen out of 124 patients in TLTG and 22 out of 124 patients in OTG got postoperative complications, which was not statistic different between 2 groups (14.5% vs 17.7%). The anastomosis-related complications in TLTG included 3 cases of anastomotic leakage at the esophagojejunostomy site and 2 cases of stricture. These complications were controlled by conservative treatment. Morbidity related to esophagojejunostomy included 2 cases of anastomotic leakage (1 requiring surgical correction) and 2 cases of stricture (conservative treatment). There was no postoperative mortality in both groups. According to Clavien–Dindo classification, there were 6 (4.8%) major (Clavien–Dindo III or higher) postoperative complications in TLTG group, whereas 8 (6.5%) major complications in OTG group (P = .52). The detail of postoperative morbidities was summarized in Table 3.
Table 3.
Comparison of postoperative complications.
4. Discussion
Totally laparoscopic distal gastrectomy (TLDG) was a surgical method by performing distal stomach resection and gastrointestinal reconstruction totally intracorporeally,[4] which have several advantages over laparoscopy-assisted distal gastrectomy, including smaller wound, less pain, and better feasibility for safe gastrectomy.[5,7] A programme of TLG was adopted at our hospital due to its inception because we considered that it would bring about several advantages.[5] However, regarding to the laparoscopic total gastrectomy (LTG), many surgeons have preferred the “laparoscopy-assisted” type due to the high technical demand of intracorporeal esophagojejunostomy (IE), and potentially higher postoperative morbidity and mortality. In this study, we summarized our experience of TLTG and found that surgical outcomes were comparable to the conventional OTG approach.
Considering esophagojejunostomy under laparoscopy, the safety of TLTG has been a concern for many surgeons. Our results revealed that there was no significant difference in the overall postoperative complications between TLTG and OTG (14.5% vs 17.7%). When the morbidity was further analyzed, we found the anastomosis-related complications (anastomotic leakage, stenosis, and bleeding) also had no significant difference between 2 groups (4.0% vs 3.2%). The anastomotic leakage was the most frequent anastomosis-related morbidity (2.4% in TLTG) that was similar to that in OTG. However, all leakages were minor following intraabdominal abscess and treated conservatively. No patient suffered anastomotic bleeding postoperatively. In previous studies of OTG, complication rates were 17.8% after total gastrectomy alone and 39.7% after total gastrectomy with splenectomy.[13] According to a large retrospective analysis of 1185 cases of LAG, which is a relatively mature technique, from Japan,[14] the postoperative complication rate was 12.7%, in which the anastomosis-related complication rate was 5.1%. Also, Kim et al[15] retrospectively analyzed 1237 cases of LAG in Korea and found that the postoperative overall complication and anastomotic complication rates were 13.1% and 1.9%, respectively. However, 2 cases of abdominal infection were reported in the early stage of our center, while in the later stage, the incidence of abdominal infection decreased with the help of such measures as adequate gastrointestinal decompression before opening the stomach cavity and local peritoneal washing after completing anastomosis.
Given the complexity of IE, surgeons concern TLTG may prolong the operation time. However, our results showed that the operation time of TLTG was not longer than that of OTG. A stable team with a tacit cooperation plays would perform laparoscopic gastrectomy easier and faster. The reduced operative time might be related to the fact that we got substantial experience from totally laparoscopic distal gastrectomy and laparoscopy-assisted total gastrectomy. As a new technology, laparoscopic reconstruction of the gastrointestinal tract has a steep learning curve. Although its initial application takes time and energy, fast and secure laparoscopic anastomosis can be eventually achieved if the technique would be well mastered. Besides, the time to first flatus or start oral intake was earlier in TLTG than OTG, indicating a faster recovery of bowel function after TLTG.
Recently, various modified IE techniques had been reported.[8,16] However, the optimal procedure remains unclear. The conventional circular stapler has a drawback in the placement of circular anvil. The OrVilTM approach carries possible risk of pharyngeal or esophageal injury when anvil head passing the level of tracheal bifurcation, which may result in abdominal infection. Side-to-side anastomosis using linear-stapled could reduce the risk of anastomotic stenosis, because a stoma larger than 30 mm diameter can be created. However, it requires a sufficient esophageal length. For tumors near the esophagogastric junction, inserting the jaws into a short esophageal is quite difficult without proper traction by the assistant, which would adversely affect the quality of anastomosis. The limitations of mechanical approach could be overcome by the hand-sewn esophagojejunostomy. But it needs operators with rich experience in laparoscopic suture, and it may consume more time. In 2011, Kwang et al reported 6 cases of IE. In their study, the total operation time and IE time were 379.7 and 81.5 minutes, respectively.[17] Besides, they found no anastomosis-related complications and other major surgical complications in their cohorts. Facy et al[18] also reported 5 cases using unidirectional absorbable barbed sutures (V-Loc; Covidien, Mansfield, MA), in which only 1 leakage occurred in an esophagojejunostomy, which was managed with laparoscopic surgical drainage. We started performing TLTG using an anvil combined with intracorporeal purse-string suture technique in November 2007 and started using intracorporeal hand-sewn esophagojejunostomy in September 2012. In our hands, the anastomosis procedure is usually completed in 40 minutes after we mastered the skill. Although it still consumes a little longer time than the mechanical approach, it also decreased the risk of leakage and stenosis.[8]
There were several limitations of this study including retrospective, single-center design, potential for undetected selection bias, and lack of long-term follow-up results. First, because it was a retrospective study performed at a single center, case selection was inevitably affected by bias. Not exactly the same postoperative management and discharge criteria will also lead to clinical heterogeneity and a sequence of biases. Second, there must be obvious clinical homogeneity in this study due to the inherent flaws of retrospective cohort study that the baseline levels were not exactly comparable, as well as the uneven surgical skills of the different surgeons, therefore several extreme values were obtained. Third, long-term outcomes were not evaluated because of the short observation period, which is unavoidable given the relatively short history of performing TLTG for gastric cancer. Therefore, randomized controlled trials or prospective cohort studies with long-term follow-up are necessary to adequately evaluate the status of TLTG for gastric cancer.
5. Conclusion
In conclusion, our study shows that TLTG, which can achieve similar lymphadenectomy effect as OTG, is safe and feasible, and characterized by the advantage of rapid recovery. Besides, the morbidity and mortality rate was not statistically different between them. A prospective randomized study comparing long-term oncological is necessary to confirm these results.
Acknowledgments
The authors thank Hendi Maher from Australia for editing the English language.
Footnotes
Abbreviations: IE = intracorporeal esophagojejunostomy, LAG = laparoscopy-assisted gastrectomy, OTG = open total gastrectomy, TLG = totally laparoscopic gastrectomy, TLTG = totally laparoscopic total gastrectomy, TNM = tumor-node-metastasis.
Funding/support: This work was supported by the Medical and Natural Science Foundation of Zhejiang Province, China (No. 2013RCA028).
Ethics and consent to participate: The study has been reviewed and approved by the Medical Ethic Committee, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University.
The authors have no conflicts of interest to disclose.
References
- [1].Parkin DM, Bray F, Ferlay J, et al. Global cancer statistics. CA Cancer J Clin 2002;55:74–108. [DOI] [PubMed] [Google Scholar]
- [2].Strong VE. Defining the role of laparoscopic gastrectomy for gastric cancer. J Clin Oncol 2014;32:613–4. [DOI] [PubMed] [Google Scholar]
- [3].Chen K, Pan Y, Zhai ST, et al. Laparoscopic gastrectomy in obese gastric cancer patients: a comparative study with non-obese patients and evaluation of difference in laparoscopic methods. BMC Gastroenterol 2017;17:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Chen K, Xu X, Mou Y, et al. Totally laparoscopic distal gastrectomy with D2 lymphadenectomy and Billroth II gastrojejunostomy for gastric cancer: short- and medium-term results of 139 consecutive cases from a single institution. Int J Med Sci 2013;10:1462–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Chen K, Mou YP, Xu XW, et al. Comparison of short-term surgical outcomes between totally laparoscopic and laparoscopic-assisted distal gastrectomy for gastric cancer: a 10-y single-center experience with meta-analysis. J Surg Res 2015;194:367–74. [DOI] [PubMed] [Google Scholar]
- [6].Chen K, Mou YP, Xu XW, et al. Short-term surgical and long-term survival outcomes after laparoscopic distal gastrectomy with D2 lymphadenectomy for gastric cancer. BMC Gastroenterol 2014;14:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Chen K, Pan Y, Cai JQ, et al. Totally laparoscopic gastrectomy for gastric cancer: a systematic review and meta-analysis of outcomes compared with open surgery. World J Gastroenterol 2014;20:15867–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Chen K, Pan Y, Cai JQ, et al. Intracorporeal esophagojejunostomy after totally laparoscopic total gastrectomy: a single-center 7-year experience. World J Gastroenterol 2016;22:3432–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Chen K, He Y, Cai JQ, et al. Comparing the short-term outcomes of intracorporeal esophagojejunostomy with extracorporeal esophagojejunostomy after laparoscopic total gastrectomy for gastric cancer. BMC Surg 2016;16:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Chen K, Wu D, Pan Y, et al. Totally laparoscopic gastrectomy using intracorporeally stapler or hand-sewn anastomosis for gastric cancer: a single-center experience of 478 consecutive cases and outcomes. World J Surg Oncol 2016;14:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 2011;14:113–23. [DOI] [PubMed] [Google Scholar]
- [13].Kasakura Y, Fujii M, Mochizuki F, et al. Is there a benefit of pancreaticosplenectomy with gastrectomy for advanced gastric cancer? Am J Surg 2000;179:237–42. [DOI] [PubMed] [Google Scholar]
- [14].Kitano S, Shiraishi N, Uyama I, et al. A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann Surg 2007;245:68–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kim W, Song KY, Lee HJ, et al. The impact of comorbidity on surgical outcomes in laparoscopy-assisted distal gastrectomy: a retrospective analysis of multicenter results. Ann Surg 2008;248:793–9. [DOI] [PubMed] [Google Scholar]
- [16].Shim JH, Yoo HM, Oh SI, et al. Various types of intracorporeal esophagojejunostomy after laparoscopic total gastrectomy for gastric cancer. Gastric Cancer 2013;16:420–7. [DOI] [PubMed] [Google Scholar]
- [17].So KO, Park JM. Totally laparoscopic total gastrectomy using intracorporeally hand-sewn esophagojejunostomy. J Gastric Cancer 2011;11:206–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Facy O, Blasi VD, Goergen M, et al. Laparoscopic gastrointestinal anastomoses using knotless barbed sutures are safe and reproducible: a single-center experience with 201 patients. Surg Endosc 2013;27:3841–5. [DOI] [PubMed] [Google Scholar]


