Abstract
Background:
This meta-analysis aimed to evaluate the efficiency and safety of the combined adductor canal block with peri-articular infiltration versus periarticular infiltration alone for pain control after total knee arthroplasty (TKA).
Methods:
PubMed, Medline, Embase, Web of Science, and the Cochrane Library were searched to identify articles comparing the combined adductor canal block with peri-articular infiltration and periarticular infiltration alone for pain control after TKA. Main outcomes were numeric rating scale (NRS) at postoperative day (POD) 0–2 and opioid consumption. Meta-analysis was performed using Stata 11.0 software.
Results:
Four randomized controlled trial (RCTs) including 297 patients met the inclusion criteria. The present meta-analysis indicated that there were significant differences between the groups regarding NRS score at POD 0 (weighted mean difference [WMD] = −0.849, 95% confidence interval [CI]: −1.345 to −0.353, P = .001), POD 1 (WMD = −0.960, 95% CI: −1.474 to −0.446, P = .000), and POD 2 (WMD = −0.672, 95% CI: −1.163 to −0.181, P = .007) after TKA. Significant differences were found in terms of opioid consumption at POD 0 (WMD = −3.761, 95% CI: −6.192 to −1.329, P = .002), POD 1 (WMD = −4.795, 95% CI: −8.181 to −1.409, P = .006), and POD 2 (WMD = −2.867, 95% CI: −4.907 to −0.827, P = .006).
Conclusion:
Combined adductor canal block with peri-articular infiltration could significantly reduce NRS scores and opioid consumption in comparison with periarticular infiltration alone following TKA. Additionally, there is a lower incidence of nausea and vomiting in the combined groups.
Keywords: adductor canal block, meta-analysis, pain control, peri-articular infiltration, total knee arthroplasty
1. Introduction
Total knee arthroplasty (TKA) is highly effective in improving functional outcome and pain relief for patients with knee osteoarthritis.[1] With the aging population, the number of TKAs is increasing. It is estimated that more than 700 thousand TKAs are performed in the United States in 2011, and it is predicted that the numbers will continue increasing in the next few years.[2] However, the surgical procedures were associated with moderate to severe postoperative pain which affected functional recovery and the quality of life.[3] Adequate analgesia regime can contribute to early rehabilitation and less postoperative complications.[4]
Various analgesia strategies have been implemented including patient-controlled (PCA) opioid, local infiltration anesthesia, peripheral nerve block, and epidural analgesia.[5–8] The PCA opioid is associated with adverse effects, including nausea, vomiting, and respiratory depression. Patients who received epidural analgesia usually complained of urinary retention and pruritus. A peripheral nerve block has been recommended by experts for pain management in TKA. This has many advantages over PCA and epidural analgesia. Peripheral nerve block can, however, decrease the strength of musculi quadriceps femoris, increasing the risk of fall after TKA, and affecting the early mobilization.
Recently, the adductor canal block was introduced for managing pain following knee surgery.[9,10] Adductor canal block is a new technique resulting in sensory blockade that can be easily visualized, with the use of ultrasonography, at the middle third of the thigh.[11] It is a sufficient analgesic and gained popularity due to its small impact on quadriceps muscle weakness. Thus, the risk of postoperative falls was low. Additionally, it is implemented with a high overall success rate. Peri-articular infiltration with local anesthetics is considered an alternative choice for regional anesthesia.[12] The procedure can be performed without anesthetists. Its simplicity and apparent safety led it to gain popularity for pain control in orthopedic surgery. However, a short duration of action limits its clinical application. Therefore, combined adductor canal block and peri-articular infiltration may improve and prolong analgesia. There was, however, controversy surrounding whether or not the combined adductor canal block and peri-articular infiltration provide better outcomes for pain control in TKA. Thus, we conducted a meta-analysis to compare the effectiveness between the combined adductor canal block with peri-articular infiltration and periarticular infiltration for pain management in TKA.
2. Methods
This meta-analysis is perform according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines. All analyses are based on previous articles, therefore, no ethical approval are required.
2.1. Search strategy
Potentially relevant studies are identified from electronic databases including Medline (1966–2017.07), PubMed (1966–2017.07), Embase (1980–2017.07), ScienceDirect (1985–2017.07), and the Cochrane Library. The following key words are used on combination with Boolean operators AND or OR: “total knee replacement OR arthroplasty,” “adductor canal block,” “peri-articular infiltration,” and “pain control.” No restrictions are imposed on language. The bibliographies of retrieved trials and other relevant publications are cross-referenced to identify additional articles. The search process is performed as presented in Fig. 1.
Figure 1.
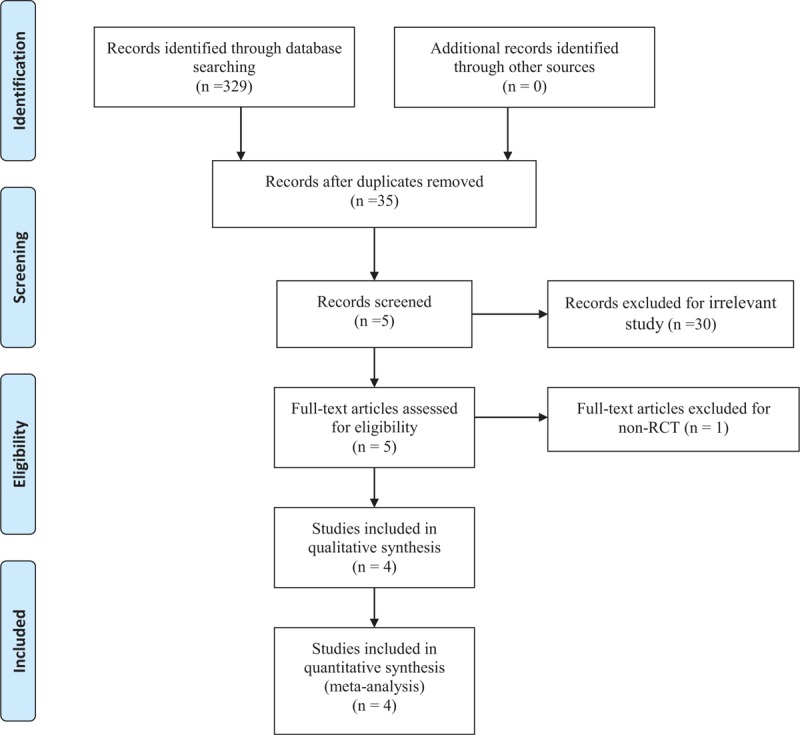
Search results and the selection procedure.
2.2. Inclusion criteria and study selection
Participants: Published literatures enrolling adult patients that with a diagnosis of end-stage of knee osteoarthritis and prepared for unilateral TKA; Interventions: The intervention group receives the combined adductor canal block by ultrasound and peri-articular infiltration for postoperative pain management; Comparisons: The control group receives peri-articular infiltration alone; Outcomes: Numeric rating scale (NRS) at rest at postoperative postoperative day (POD) 0–2, opioid consumption, length of stay, and postoperative complications such as opioid-related adverse effects; Study design: RCTs are regarded as eligible in the study. Articles would be excluded from the present meta-analysis for case reports, conference abstract, or review articles. Two reviewers independently scan the abstracts of the potential articles identified by the above searches. Subsequently, the full text of the studies that meet the inclusion criteria was screened, and a final decision is made.
2.3. Date extraction
The included studies are examined by 2 investigators and key data are extracted including first author name, samples size, published year, baseline characteristics, intervention of each groups, and other outcome parameters. The primary outcomes are NRS scores at rest and opioid consumption at different periods. The secondary outcomes are length of stay and opioid-related adverse effects.
2.4. Assessment of methodological quality
A quality assessment of each randomized trial is performed by 2 reviewers based on the Cochrane Handbook for Systematic Reviews of Interventions. Disagreement is resolved by consulting a senior reviewer. We create a “risk of bias” table that included the following elements: random sequence generation, allocation concealment, blinding, incomplete outcome data, free of selective reporting and other bias. The quality of the evidence for the main outcomes in present meta-analysis is evaluated using the recommendations assessment, development, and evaluation (GRADE) system including the following items: risk of bias, inconsistency, indirectness, imprecision and publication bias. The recommendation level of evidence is classified into the following categories: high, which means that further research is unlikely to change confidence in the effect estimate; moderate, which means that further research is likely to significantly change confidence in the effect estimate but may change the estimate; low, which means that further research is likely to significantly change confidence in the effect estimate and to change the estimate; and very low, which means that any effect estimate is uncertain.
2.5. Data analysis and statistical methods
The data are pooled using Stata 12.0 (The Cochrane Collaboration, Oxford, UK). After extracting the data from the included studies, we export the means, SDs, and sample sizes of groups into Stata 12.0 to determine the heterogeneity. Statistical heterogeneity is assessed based on the P and I2 values using the standard Chi-squared test. When I2 ≥50% or P < .1, significant heterogeneity is indicated and a random-effects model is applied for the meta-analysis. Otherwise, a fixed-effects model is used. Dichotomous outcomes (i.e., complications) are expressed as risk differences (RDs) with 95% confidence intervals (CIs). For continuous outcomes (i.e., NRS scores), standardized mean differences (SMDs), and 95% CIs are calculated.
3. Results
3.1. Search result
A total of 329 studies are identified through the initial search. By scanning the abstracts, 325 reports that do not meet inclusion criteria are excluded from the current meta-analysis. No gray studies are included. Finally, four RCTs[13–16] comprising 297 patients were determined to fulfil the inclusion criteria for our meta-analysis which contains 149 patients in combined groups and 148 patients in controls.
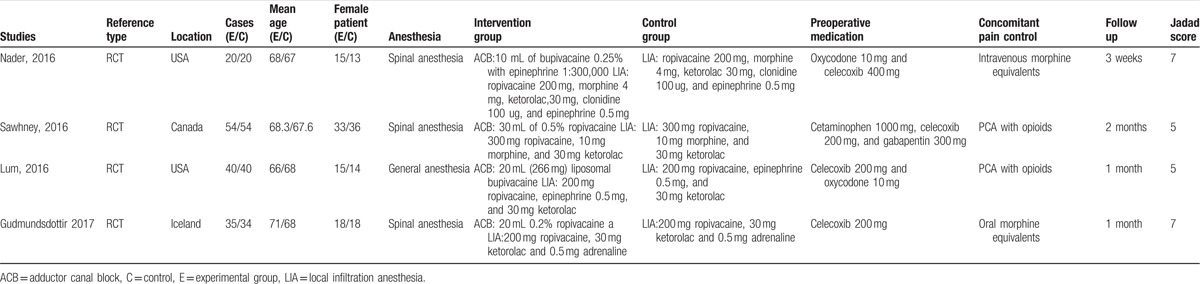
3.2. Study characteristics
Only patients with end-stage knee osteoarthritis and prepare to undergo TKA are included in our study. The sample sizes ranges from 40 to 108 patients and average age ranges from 67 to 71. In these articles, the experimental groups receive the combined adductor canal block and peri-articular infiltration and the control groups receives peri-articular infiltration alone. The characteristics of the included studies are reported in Table 1. Statistically similar baseline characteristics are observed between groups.
Table 1.
Trials characteristics.
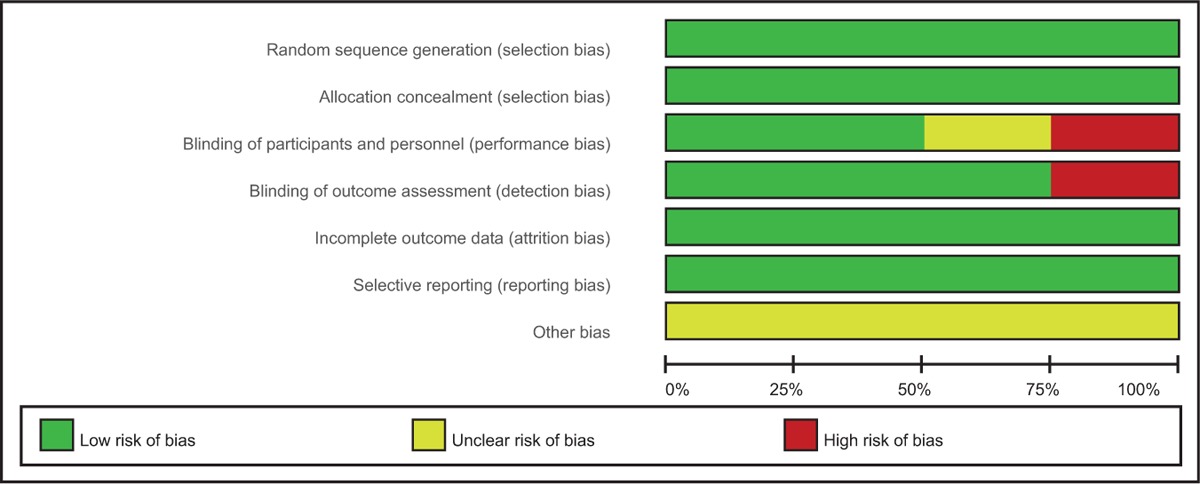
3.3. Risk of bias
The Cochrane Handbook for Systematic Review of Interventions is consulted to assess risk of bias of the RCTs. All RCTs provide clear inclusion and exclusion criteria and report their randomization methodology, describing the use of computer-generated randomization. All articles provide that allocation concealment is achieved by closed envelope. Double blinding is showed in 2 RCTs,[13,16] and 3 studies[13,14,16] attempt to blind the assessors. Low risk of bias due to incomplete outcome data or selective outcome reporting is detected. The methodological quality assessment is summarized in Table 2. Each risk of bias item is presented as the percentage across all included studies, which indicates the proportion of different levels of risk of bias for each item (Table 3).
Table 2.
Methodological quality of the randomized controlled trials.
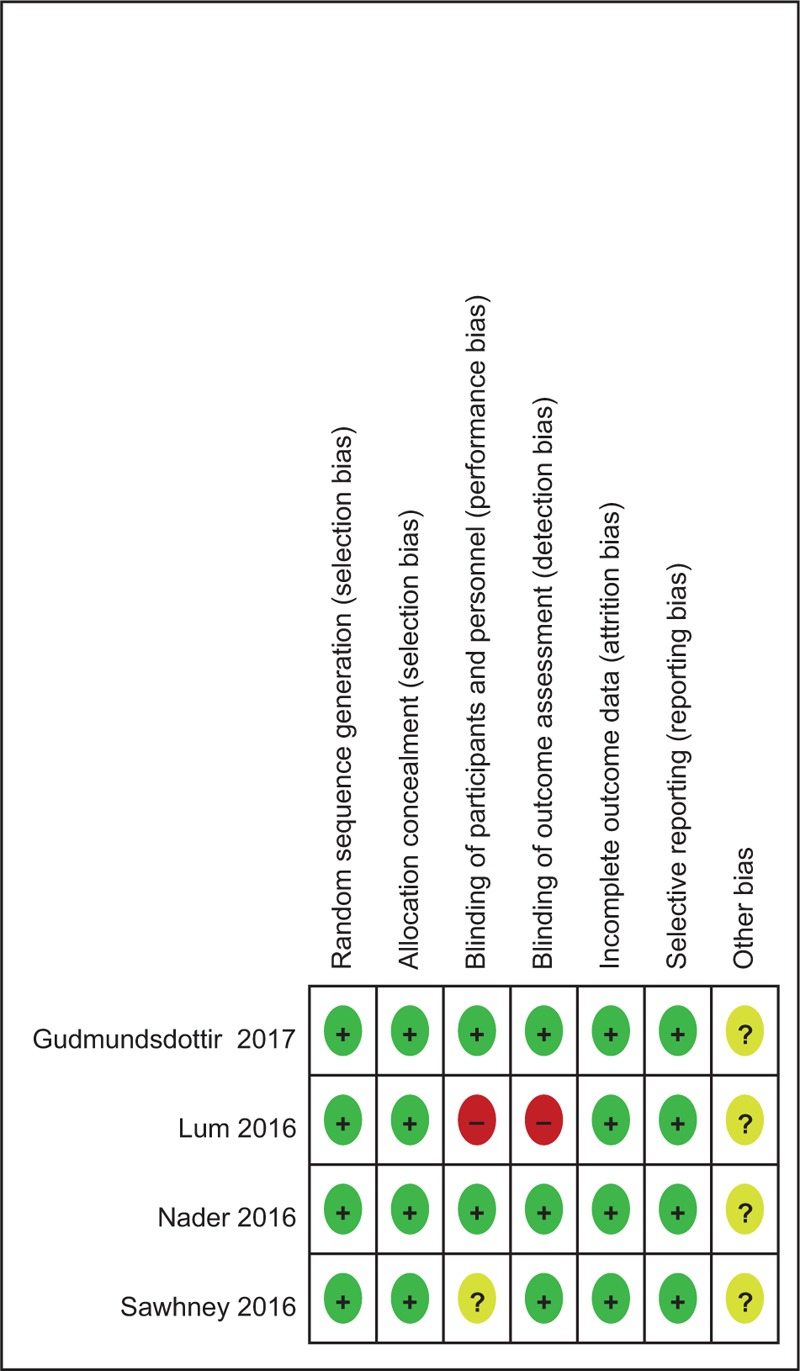
Table 3.
Risk of bias.
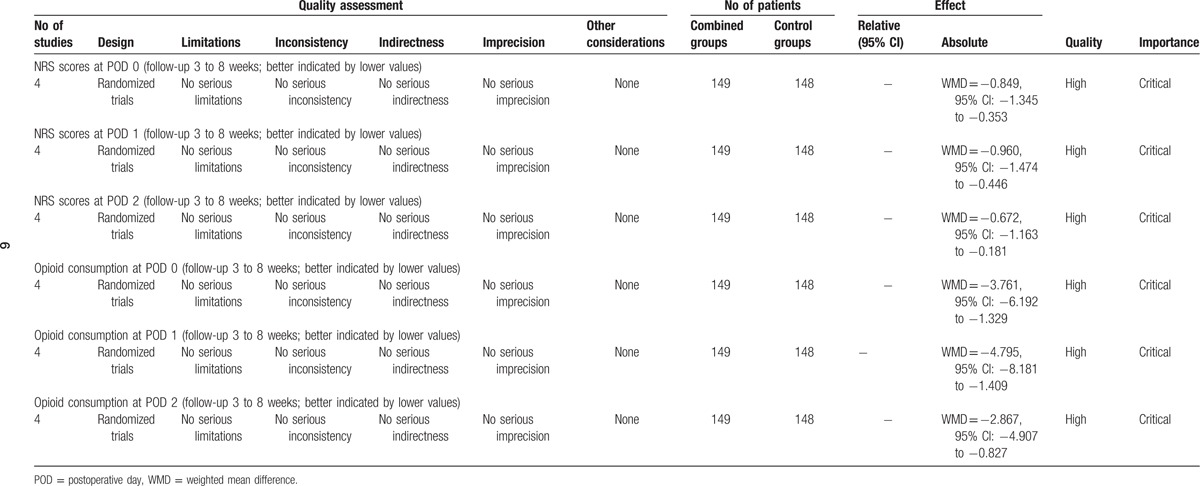
3.4. Evidence level
All outcomes in this meta-analysis are evaluated using the GRADE system. The evidence quality for most outcomes is high (Table 4) which means further research is very unlikely to change our confidence in the estimate of effect.
Table 4.
The GRADE evidence quality for main outcome.
3.5. Outcomes for meta-analysis
3.5.1. NRS scores at rest at POD 0
Four studies with 297 patients show the NRS scores at POD 0 after TKA. A fixed-effects model is used because no significant heterogeneity is found among the studies (χ2 = 2.09, df = 3, I2 = 0%, P = .553). The pooled results demonstrate that NRS scores at POD 0 is significantly higher in the control groups than in the experimental groups (weighted mean difference [WMD] = −0.849, 95% CI: −1.345 to −0.353, P = .001, power = 86%; Fig. 2).
Figure 2.
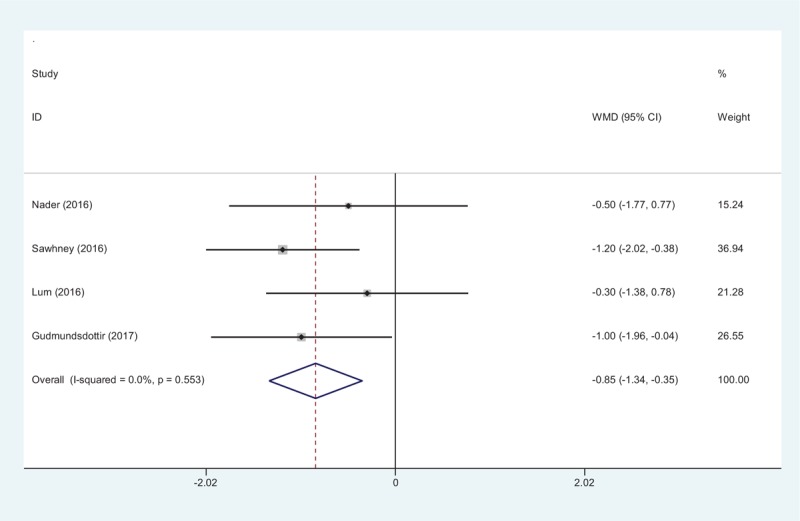
Forest plot diagram showing NRS scores at POD 0 after TKA. NRS = numeric rating scale, POD = postoperative day, TKA = total knee arthroplasty, WMD = weighted mean difference.
3.5.2. NRS scores at rest at POD 1
Four studies with 297 patients report the outcome of NRS scores at POD 1 after TKA. Significant heterogeneity is detected between groups (χ2 = 8.33, df = 3, I2 = 64.0%, P = .040). There is significant difference in NRS scores at POD 1 between groups (WMD = −0.960, 95% CI: −1.474 to −0.446, P = .000, power = 82%; Fig. 3).
Figure 3.
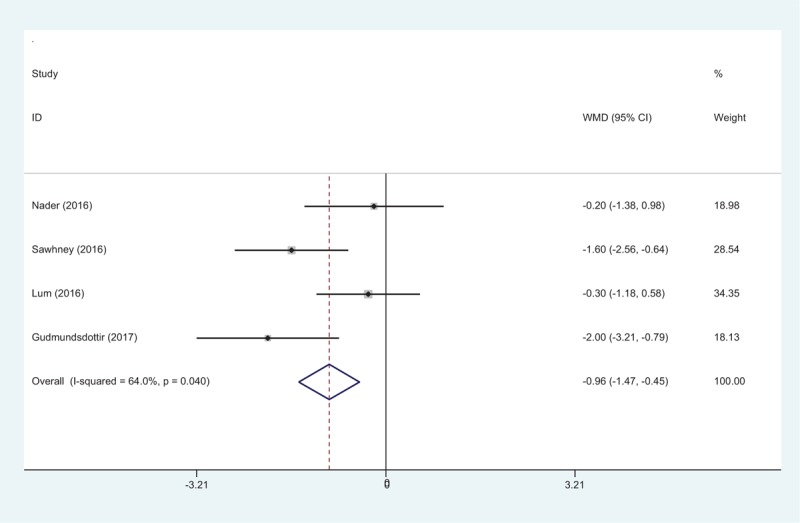
Forest plot diagram showing NRS scores at POD 1 after TKA. NRS = numeric rating scale, POD = postoperative day, TKA = total knee arthroplasty, WMD = weighted mean difference.
3.5.3. NRS scores at rest at POD 2
Four articles with 297 patients report the outcome of NRS scores at POD 2 after TKA. A fixed-effects model is used because no significant heterogeneity is found among the studies (χ2 = 2.50, df = 3, I2 = 0%, P = .475). There is significant difference in NRS scores at POD 1 between groups (WMD = −0.672, 95% CI: −1.163 to −0.181, P = .007, power = 88%; Fig. 4).
Figure 4.
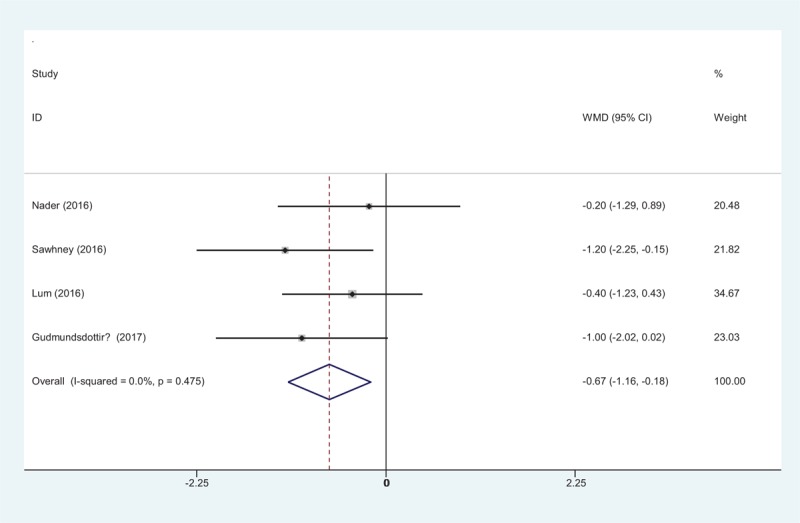
Forest plot diagram showing NRS scores at POD 2 after TKA. NRS = numeric rating scale, POD = postoperative day, TKA = total knee arthroplasty, WMD = weighted mean difference.
3.5.4. Opioid consumption at POD 0
Opioid consumption at POD 0 is reported in 4 articles. No significant heterogeneity is found among these studies (χ2 = 0.57, df = 3, I2 = 0%, P = .904) and a fixed-effects model is used. A significant difference is detected between the 2 groups (WMD = −3.761, 95% CI: −6.192 to −1.329, P = .002, power = 80%; Fig. 5).
Figure 5.
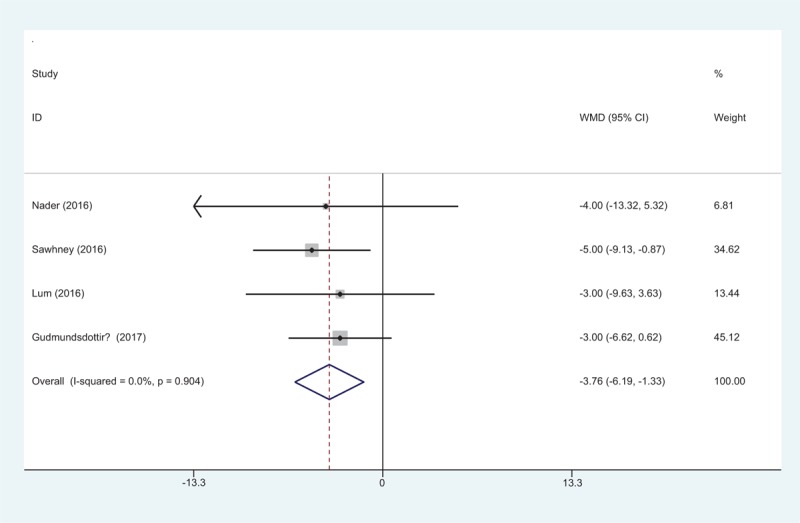
Forest plot diagram showing opioid consumption at POD 0 after TKA. POD = postoperative day, TKA = total knee arthroplasty, WMD = weighted mean difference.
3.5.5. Opioid consumption at POD 1
Four studies with 297 patients show the outcome of opioid consumption at POD 1 after TKA. A fixed-effects model because no significant heterogeneity is found (χ2 = 0.23, df = 3, I2 = 0%, P = .973). There is significant difference in opioid consumption at POD 1 between groups (WMD = −4.795, 95% CI: −8.181 to −1.409, P = .006, power = 83%; Fig. 6).
Figure 6.
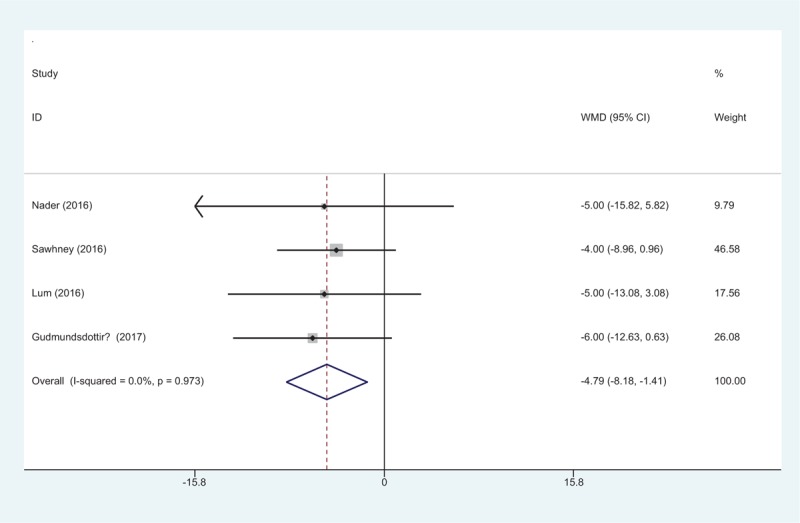
Forest plot diagram showing opioid consumption at POD 1 after TKA. POD = postoperative day, TKA = total knee arthroplasty, WMD = weighted mean difference.
3.5.6. Opioid consumption at POD 2
Four articles provide the data of opioid consumption at POD 2 after TKA. A fixed-effects model is used because no significant heterogeneity is found (χ2 = 2.46, df = 3, I2 = 0%, P = .482). There is significant difference in opioid consumption at POD 2 between groups (WMD = −2.867, 95% CI: −4.907 to −0.827, P = .006, power = 86%; Fig. 7).
Figure 7.
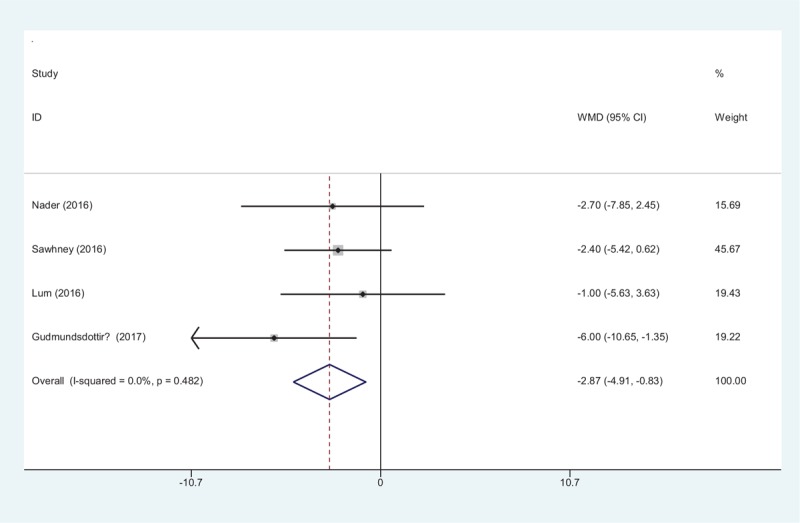
Forest plot diagram showing opioid consumption at POD 2 after TKA. POD = postoperative day, TKA = total knee arthroplasty, WMD = weighted mean difference.
3.5.7. Length of hospital stay (LOS)
Four studies report the lengths of the hospital stay for the groups. No significant difference in the LOS is observed between the 2 groups (WMD = 0.075, 95% CI: −0.020 to 0.169, P = .120, power = 88%; Fig. 8).
Figure 8.
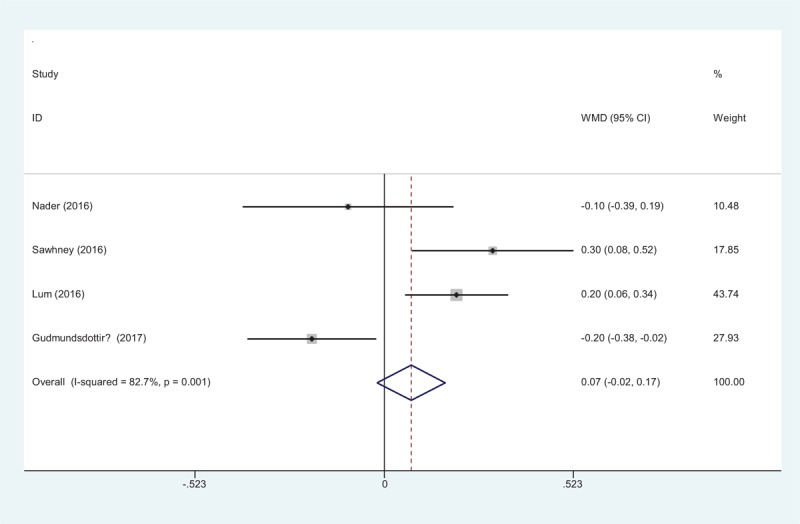
Forest plot diagram showing length of hospital stay after TKA. TKA = total knee arthroplasty, WMD = weighted mean difference.
3.5.8. Nausea
Four articles showed the postoperative complications of nausea. A fixed-effects model is used (χ2 = 0.43, df = 3, I2 = 0%, P = .935). Significant difference in the incidence of nausea is found between the 2 groups (RD = −0.121, 95% CI: −0.225 to −0.016, P = .024, power = 90%; Fig. 9).
Figure 9.
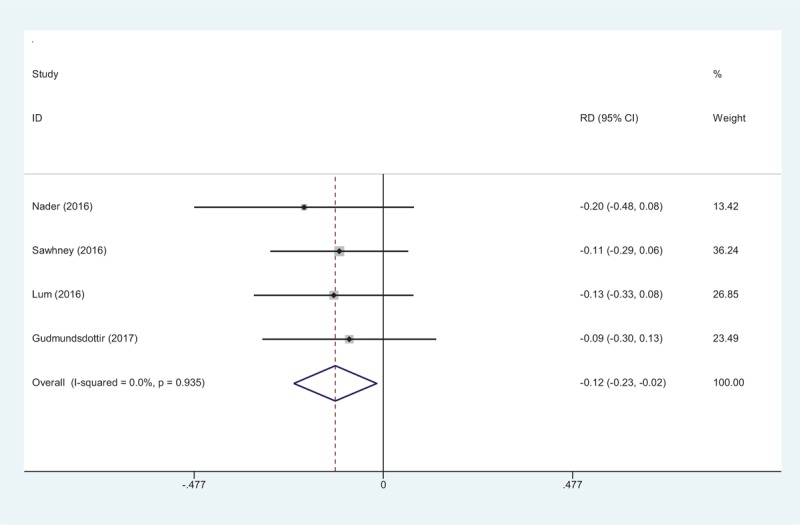
Forest plot diagram showing incidence of nausea after TKA. TKA = total knee arthroplasty.
3.5.9. Vomiting
Four studies report the postoperative complications of vomiting after TKA. A fixed-effects model is used (χ2 = 0.67, df = 3, I2 = 0%, P = .881). The pooled results demonstrate that there is an increased risk of vomiting in control groups (RD = −0.107, 95% CI: −0.203 to −0.012, P = .027, power = 91%; Fig. 10).
Figure 10.
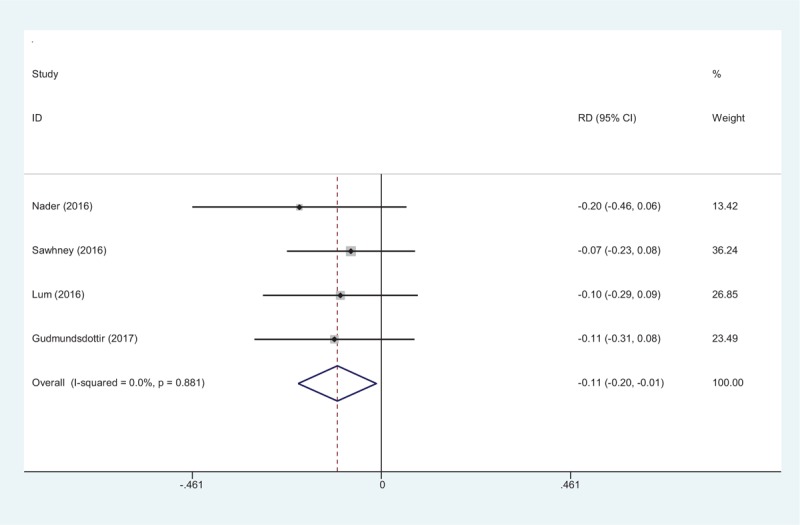
Forest plot diagram showing incidence of vomiting after TKA. TKA = total knee arthroplasty.
3.5.10. Constipation
Four articles showed the postoperative complications of constipation. A fixed-effects model is used (χ2 = 1.01, df = 3, I2 = 0%, P = .798). Significant difference in the incidence of constipation is found between the 2 groups (RD = −0.134, 95% CI: −0.231 to −0.038, P = .007, power = 90%; Fig. 11).
Figure 11.
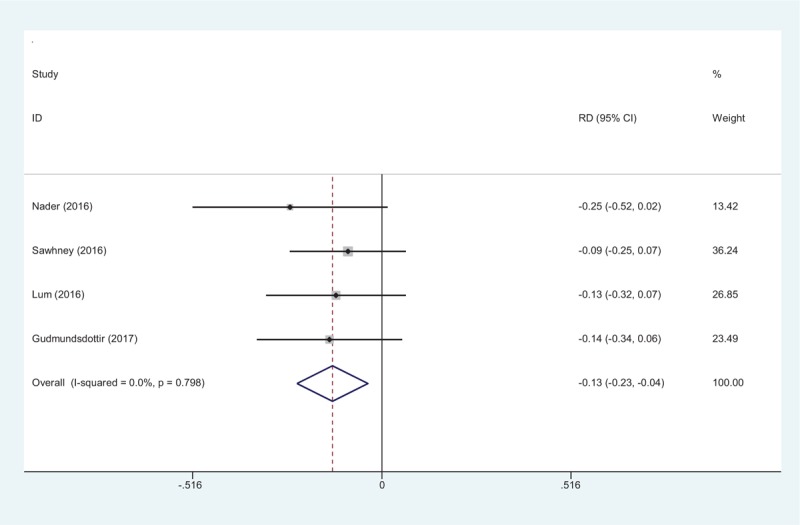
Forest plot diagram showing incidence of constipation after TKA. TKA = total knee arthroplasty.
3.5.11. Pruritus
Four studies report the pruritus for the groups. No significant difference is observed between the 2 groups (RD = −0.047, 95% CI: −0.150 to 0.056, P = .369, power = 93%; Fig. 12).
Figure 12.
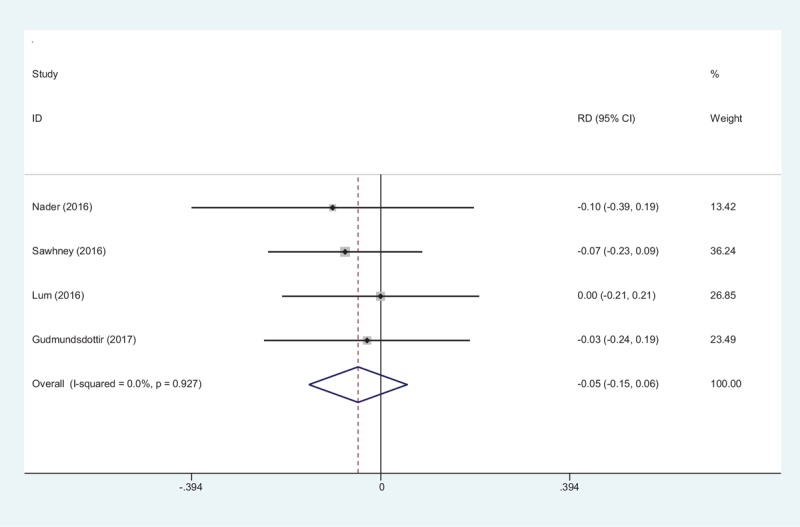
Forest plot diagram showing incidence of pruritus after TKA. TKA = total knee arthroplasty.
4. Discussion
To the best of our knowledge, this is the first meta-analysis to evaluate the efficiency and safety of the combined adductor canal block with peri-articular infiltration versus periarticular infiltration alone for pain control following TKA. The most important finding of the present meta-analysis is that the combined adductor canal block with peri-articular infiltration can significantly reduce postoperative pain scores and morphine equivalent consumption. Additionally, there is a lower risk of opioid-related adverse effects, such as nausea and vomiting in combined groups. The quality of the evidence for each outcome is high, meaning that further research is unlikely to change confidence in the effect estimate.
As the population ages, the incidence of knee osteoarthritis is increasing. TKA is an excellent surgical procedure for patients with painful arthritic knees. However, TKA is usually associated with moderate to severe postoperative pain. Postoperative pain following TKA is usually intense, and immediate postoperative opioid consumption can be high. A consensus has been reached that effective postoperative analgesia improved patient outcomes by allowing early ambulation and rehabilitation. The optimal analgesic strategy remains controversial and pain control after TKA is an interesting topic in the field of orthopedic surgery. Multimodal pain management following TKA is recommended in order to improve pain relief and reduce opioid consumption.[17,18]
Local infiltration anesthesia is widely performed and shows satisfactory outcomes for pain control following TKA. Song et al[19] reported that peri-articular injections offered improved pain control and minimal side effects in comparison to patient-controlled analgesia. Thus, peri-articular injections can replace conventional PCA for controlling postoperative pain after TKA. Yun et al[20] performed a meta-analysis from RCTs to compare the analgesia achieved with local infiltration anesthesia and femoral nerve block following TKA. They indicated that local infiltration anesthesia may be the optimal choice in pain management of TKA, as it could achieve fast pain relief and was easier to perform than femoral nerve block for patients with TKA. However, local infiltration anesthesia has been criticized by some experts due to its short-term action and inadequate provision of sufficient analgesia to the anterior aspect of the knee. Therefore, multimodal analgesia protocols are recommended to improve pain relief, decrease total perioperative morphine consumption, increase patient satisfaction, and facilitate early mobilization and discharge.
The adductor canal is an aponeurotic tunnel in the middle third of the thigh, extending from the apex of the femoral triangle to the opening in the adductor magnus, the adductor hiatus.[21] Sensory nerves dominating knee joints were located in the adductor canal. Therefore, blocking these sensory nerves could provide analgesia for patients undergoing TKA.[22] Although femoral nerve block has been recognized as the gold standard for pain control after TKA, adductor canal block has recently gained popularity because of the less block-induced motor weakness. Kim et al[23] compared adductor canal block and femoral nerve block for pain management after TKA and found that the comparative effectiveness of pain reduction and opioid consumption. More importantly, adductor canal block was confirmed to have an early sparing of the quadriceps strength with no difference in range of motion. Wang et al[24] conducted a meta-analysis from RCTs and found that adductor canal block was not inferior to femoral nerve block in regards to pain management or morphine consumption, as well as showing better knee mobility. It was superior regarding the sparing of quadriceps strength and faster knee function recovery with a decreased risk of falls. However, single-shot adductor canal blocks are still insufficient in efficacy or duration. Recent clinical trials have demonstrated that adductor canal block is effective as a rescue block when local infiltrative analgesia is insufficient for pain management and the combined adductor canal block and local infiltration anesthesia seem to be associated with further improvement in pain relief.[25] There is, however, a lack of evidence of the combined adductor canal block with peri-articular infiltration versus periarticular infiltration alone for pain control after TKA. Therefore, we performed the present meta-analysis to provide reliable evidence for orthopedists. The NRS scores at POD 0–3 are the primary outcomes assessed in our meta-analysis. The present meta-analysis indicates that the combined adductor canal block with peri-articular infiltration could significantly reduce NRS scores at rest compared with periarticular infiltration alone for pain control following TKA. Due to the limited data of the included studies, we did not analyze the pain score at movement or on weight bearing. More well-designed RCTs are needed for further study.
Additional morphine equivalent is used as a rescue to concomitant pain management. The personal control aspect of PCA and its rapid onset were preferred by patients. In the present meta-analysis, morphine equivalent consumption is considered an objective measure to assess pain. Morphine-related adverse effects including nausea, vomiting, respiratory depression, and pruritus are well known.[26,27] In addition to the side effects, drug dependence is also an important issue. Minimizing the morphine equivalent consumption is vital for early ambulation and rehabilitation. Currently, whether or not the combined adductor canal block with peri-articular infiltration could further reduce opioid consumption is seldom reported and remains controversial. Meta-analysis can combine the results from multiple studies in an effort to increase power, improve estimates of the size of the effect, and to resolve uncertainty when reports disagree. Four studies with 297 patients overall show the outcome of opioid consumption after TKA. The present meta-analysis indicates that the combined adductor canal block with peri-articular infiltration could further decrease opioid consumption for patients undergoing TKA. Considering that only four RCTs are included in our study, more RCTs with a large sample size are required for subsequent research.
Analgesia efficacy is not the only concern when assessing the analgesia of various strategies. Nausea and vomiting are common adverse effects associated with PCA. Reducing opioid consumption can subsequently decrease such complications that contribute to early ambulation and decreased medical costs. The overall incidence of nausea is 38/149 in the combined groups compared with 51/148 in control groups (P = .02). Combined adductor canal block with peri-articular infiltration could significantly reduce the incidence of postoperative complications. However, more RCTs with long term follow-up are still required.
Several potential limitations of this study should be noted. Only 5 RCTs are included, and the sample size is relatively small. Some important outcome parameters, such as range of motion are not fully described and could not be included in the meta-analysis. The methods of blinding were unclear or not described in some included studies which may influence our results. No studies performed an intent to treat analysis. Short-term follow-up may lead to the underestimation of complications. Publication bias is an inherent weakness that exists in all meta-analyses.
Despite the limitations above, this is the first meta-analysis from RCTs to evaluate the efficiency and safety of combined adductor canal block with peri-articular infiltration versus periarticular infiltration alone for pain control following TKA. Higher quality RCTs are required for further research.
5. Conclusion
Combined adductor canal block with peri-articular infiltration could significantly reduce NRS scores and opioid consumption in comparison with periarticular infiltration alone following TKA. Additionally, there is a lower incidence of nausea and vomiting in the combined groups.
Footnotes
Abbreviations: LOS= length of stay, NRS = numeric rating scale, RCT= randomized controlled trials, TKA =total knee arthroplasty.
Authors’ contributions: QJX, WWD and DFZ conceived of the design of the study. JW, CSH and YZ performed and collected the data and contributed to the design of the study. QJX finished the manuscript. All authors read and approved the final manuscript.
Funding: The Key Disciplines of Medical Science of Changning District Health Planning System (16–042).
Conflicts of Interest: The authors declare that they have no competing interests.
References
- [1].Begue T, Mebtouche N, Levante S. One-stage procedure for total knee arthroplasty in post-traumatic osteoarthritis of the knee with wound defect. Usefulness of navigation and flap surgery. Knee 2012;19:948–50. [DOI] [PubMed] [Google Scholar]
- [2].Hadzic A, Houle TT, Capdevila X, et al. Femoral nerve block for analgesia in patients having knee arthroplasty. Anesthesiology 2010;113:1014–5. [DOI] [PubMed] [Google Scholar]
- [3].Ritter MA. Postoperative pain after total knee arthroplasty. J Arthroplasty 1997;12:337–9. [DOI] [PubMed] [Google Scholar]
- [4].Li D, Tan Z, Kang P, et al. Effects of multi-site infiltration analgesia on pain management and early rehabilitation compared with femoral nerve or adductor canal block for patients undergoing total knee arthroplasty: a prospective randomized controlled trial. Int Orthop 2017;41:75–83. [DOI] [PubMed] [Google Scholar]
- [5].Ilahi OA, Davidson JP, Tullos HS. Continuous epidural analgesia using fentanyl and bupivacaine after total knee arthroplasty. Clin Orthop Relat Research 1994;44–52. [PubMed] [Google Scholar]
- [6].Lee JJ, Choi SS, Lee MK, et al. Effect of continuous psoas compartment block and intravenous patient controlled analgesia on postoperative pain control after total knee arthroplasty. Korean J Anaesthesiol 2012;62:47–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Li J, Deng X, Jiang T. Combined femoral and sciatic nerve block versus femoral and local infiltration anesthesia for pain control after total knee arthroplasty: a meta-analysis of randomized controlled trials. J Orthop Surg Res 2016;11:158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Tran J, Schwarzkopf R. Local infiltration anesthesia with steroids in total knee arthroplasty: A systematic review of randomized control trials. J Orthop 2015;12(Suppl):S44–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Hanson NA, Allen CJ, Hostetter LS, et al. Continuous ultrasound-guided adductor canal block for total knee arthroplasty: a randomized, double-blind trial. Anesth Analg 2014;118:1370–7. [DOI] [PubMed] [Google Scholar]
- [10].Mariano ER, Perlas A. Adductor canal block for total knee arthroplasty: the perfect recipe or just one ingredient? Anesthesiology 2014;120:530–2. [DOI] [PubMed] [Google Scholar]
- [11].Bendtsen TF, Moriggl B, Chan V, et al. Defining adductor canal block. Reg Anesth Pain Med 2014;39:253–4. [DOI] [PubMed] [Google Scholar]
- [12].Fenten MG, Bakker SM, Touw DJ, et al. Pharmacokinetics of 400 mg ropivacaine after periarticular local infiltration analgesia for total knee arthroplasty. Acta Anaesthesiol Scand 2017;61:338–45. [DOI] [PubMed] [Google Scholar]
- [13].Nader A, Kendall MC, Manning DW, et al. Single-dose adductor canal block with local infiltrative analgesia compared with local infiltrate analgesia after total knee arthroplasty: a randomized, double-blind, placebo-controlled trial. Reg Anesth Pain Med 2016;41:678–84. [DOI] [PubMed] [Google Scholar]
- [14].Sawhney M, Mehdian H, Kashin B, et al. Pain after unilateral total knee arthroplasty: a prospective randomized controlled trial examining the analgesic effectiveness of a combined adductor canal peripheral nerve block with periarticular infiltration versus adductor canal nerve block alone versus periarticular infiltration alone. Anesth Analg 2016;122:2040–6. [DOI] [PubMed] [Google Scholar]
- [15].Lum ZC, Lombardi AV, Hurst J, et al. Does local soft tissue infiltration with a liposomal bupivacaine cocktail have a synergistic effect when combined with single-shot adductor canal peripheral nerve block in knee arthroplasty? J Surg Orthop Adv 2016;25:222–6. [PubMed] [Google Scholar]
- [16].Gudmundsdottir S, Franklin JL. Continuous adductor canal block added to local infiltration analgesia (LIA) after total knee arthroplasty has no additional benefits on pain and ambulation on postoperative day 1 and 2 compared with LIA alone. Acta Orthop 2017;88:537–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Maheshwari AV, Blum YC, Shekhar L, et al. Multimodal pain management after total hip and knee arthroplasty at the Ranawat Orthopaedic Center. Clin Orthop Relat Res 2009;467:1418–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Tanavalee A, Thiengwittayaporn S. Multimodal pain management following minimally invasive total knee arthroplasty: an experience in 3-dose parecoxib. J Med Assoc Thai 2009;92:S11–8. [PubMed] [Google Scholar]
- [19].Song MH, Kim BH, Ahn SJ, et al. Peri-articular injections of local anaesthesia can replace patient-controlled analgesia after total knee arthroplasty: a randomised controlled study. Int Orthop 2016;40:295–9. [DOI] [PubMed] [Google Scholar]
- [20].Yun XD, Yin XL, Jiang J, et al. Local infiltration analgesia versus femoral nerve block in total knee arthroplasty: a meta-analysis. Orthop Traumatol Surg Res 2015;101:565–9. [DOI] [PubMed] [Google Scholar]
- [21].Moher D, Liberati A, Tetzlaff J, et al. The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Med 2009;3:e123–30. [PMC free article] [PubMed] [Google Scholar]
- [22].Gao F, Ma J, Sun W, et al. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: a systematic review and meta-analysis. Clin J Pain 2017;33:356–68. [DOI] [PubMed] [Google Scholar]
- [23].Kim DH, Lin Y, Goytizolo EA, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: a prospective, randomized, controlled trial. Anesthesiology 2014;120:540–50. [DOI] [PubMed] [Google Scholar]
- [24].Wang D, Yang Y, Li Q, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: a meta-analysis of randomized controlled trials. Sci Rep 2017;7:40721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Perlas A, Kirkham KR, Billing R, et al. The impact of analgesic modality on early ambulation following total knee arthroplasty. Reg Anesth Pain Med 2013;38:334–9. [DOI] [PubMed] [Google Scholar]
- [26].Bonnet MP, Mignon A, Mazoit JX, et al. Analgesic efficacy and adverse effects of epidural morphine compared to parenteral opioids after elective caesarean section: a systematic review. Eur J Pain 2010;14:894 e891–9. [DOI] [PubMed] [Google Scholar]
- [27].Tassinari D, Sartori S, Tamburini E, et al. Adverse effects of transdermal opiates treating moderate-severe cancer pain in comparison to long-acting morphine: a meta-analysis and systematic review of the literature. J Palliat Med 2008;11:492–501. [DOI] [PubMed] [Google Scholar]


