Abstract
Background:
Placenta increta/percreta is an increasingly common and life-threatening obstetric complication. It poses a management challenge to clinicians. The present study aimed to evaluate efficacy and safety of preoperative placement of infrarenal abdominal aorta balloon catheter (IAABC) alone or combined with Bakri tamponade for the management of cases with placenta increta/percreta.
Methods:
We retrospectively analyzed all cases with placenta increta/percreta at a tertiary referral teaching hospital in China between the year 2014 and 2017. Statistical analysis considered the individual subgroups: IAABC placed group and control group (without IAABC), and compared their maternal–fetal outcomes.
Results:
The study covered 86 cases with placenta increta. For cases in the IAABC placed group (n = 48), significant reductions were noted in maternal morbidity including estimated blood loss (EBL), EBL ≥ 2000 mL, blood products transfusions, postpartum hemorrhage, operative time, intensive care unit admission, and postoperative days (P < .05 for all). The overall rate of hysterectomy was much lower (4.2%vs 23.7%, P = .018), compared with those in the control group (n = 38). Furthermore, in the IAABC placed group, hysterectomy was avoided in a further 17 cases combined with Bakri tamponade. In the control group, 10 cases were successful in preserving uterus by Bakri tamponade. Four cases failed and needed reoperation (3 uterine arterial embolism, 1 hysterectomy). There were no differences in fetal outcomes between the 2 groups. Eighteen cases were diagnosed with placenta percreta. Almost all the cases (17/18) inevitably underwent caesarean hysterectomy. Only 1 case was treated with a combination of IAABC and Bakri tamponade, and successfully reserved uterus. No differences were observed in any other outcomes, except for a significant less mean operative time (P = .017) in cases with IAABC placed (n = 10), compared with those without IAABC (n = 8). Only 1 case had a femoral artery thrombosis directly related to IAABC placement and recovered after conservative treatment. There was no maternal or neonatal death in this study.
Conclusion:
Prophylactic insertion of IAABC alone or combined with Bakri tamponade should be safe and effective in controlling intraoperative bleeding due to placenta increta, thus hysterectomy could be avoided. It seems to be less beneficial to women with placenta percreta. Bakri tamponade can be a good choice in the management of placenta increta/percreta before more aggressive surgeries.
Keywords: occlusion, Bakri, percreta, balloon, placenta increta
1. Introduction
Morbidly adherent placenta (MAP) occurs when all or part of the placenta abnormally attaches to underlying myometrium, usually where there is an absence of decidua basalis. Depending on the depth of invasion, it is further defined as placenta accreta (placental villi are attached to the myometrium), placenta increta (villi actually invade into the myometrium), and placenta percreta (villi penetrate through the myometrium). It is becoming a common obstetric complications directly due to a dramatic and persistent increase in the rate of cesarean delivery (CD) and older maternal age at childbirth over the past 30 years. The reported incidence of MAP ranged between 0.017% and 0.9% of deliveries.[1–4] Although there was no population-based studies reported its incidence in China up to now, we believe its incidence cannot be low as the highest cesarean rate in our country.[5] Based on a recent multicentre study, the rate of CD has reached as high as 54.9%.[6] Besides, in October 2015, China's 1-child policy was replaced by a universal 2-child policy. The new policy allows all couples to have 2 children. It means that the proportion of advanced maternal age women with a history of CD would increase in the context of universal 2-child policy in China.
The management strategy for MAP is still a challenging problem in obstetric practice. As it was significantly associated with adverse maternal morbidity and mortality, indeed it has become a leading cause of intractable postpartum hemorrhage (PPH) and peripartum hysterectomy.[3,7] Prenatal diagnosis of MAP and a planned management at an appropriate tertiary care center have been proven to improve maternal and neonatal outcomes.[8]
However, when strong evidence points to the diagnosis of MAP, caesarean hysterectomy with the placenta left in situ and undisturbed is recommended as the primary treatment, particularly for women with deeper invasion (placenta increta/percreta). Thus minimizing blood loss to avoid a subsequent hysterectomy is very attractive to women with MAP who desire to preserve their fertility. For these reasons, several surgical techniques have been employed to manage intraoperative hemorrhage in cases of MAP. One of the most debated topics was the use of interventional procedures such as temporary occlusion of the internal iliac arteries (IIA), common iliac arteries (CIA), or infrarenal abdominal aorta (IAA) in women with placenta increta/percreta during caesarean section. The theory is that reduced uterine perfusion allows for effectively decreased hemorrhage and surgical complications. The efficacy of occlusion of IIA or CIA is limited by rapid recruitment of an extensive collateral system in the pelvis.[9–15]
While occlusion of the IAA can help overcome the collateral flow from the external iliac and femoral arteries, significantly decrease intraoperative hemorrhage and improve perioperative outcomes, as it gives the operator time to achieve hemostasis via over-sewing of the implantation site. Its first use as the effective treatment of MAP came in 1995 by Paull et al[16] and has been increasingly utilized since then. Bell-Thomas et al[17] in 2003, Masamoto et al[18] in 2009 and Andoh et al[19] in 2011 described the efficacy of IAABC in women with placenta percreta involving the cervix and bladder, and all 3 showed favorable outcomes. In 2010, Chou et al[20] reported a sudden and dramatic reduction in operative blood loss after the temporary cross-clamping of the IAA in a patient with placenta percreta. Although these results were promising, larger case series are needed to evaluate the safety and effectiveness of this procedure.
The Bakri tamponade is a fluid-filled tamponade balloon that is inserted into the uterine cavity to achieve control or reduction of PPH. It has been proved to be an effective adjunct in the management of PPH for placenta previa or uterine atony,[21–26] but its role in the management of MAP is uncertain.[23,25,27] To date, no studies have ever investigated Bakri tamponade for the treatment of MAP after caesarean section combined with preoperative IAABC.
Moreover, our medical center is the chief tertiary hospital providing care for the entire population in central south of China. We can afford a multidisciplinary team with expertise and experience in the management of MAP. Such center had been termed “centers of excellence” for MAP.[8]
Given this background, the aim of this study is to assess the feasibility and safety of preoperative IAABC combined with Bakri tamponade in the management of placenta increta/percreta.
2. Methods
We conducted a retrospective cohort study on all cases diagnosed with placenta increta/percreta who underwent CD between January 2014 and March 2017 at the Second Xiangya Hospital of Central South University, a tertiary referral teaching hospital in the Central south of China. Medical records of all cases during the study period were individually reviewed retrospectively. The hospital research and ethical committees at our hospital approved this study. The inclusion criteria were as follows: clinical assessment of placental invasion at surgery[28]: a diagnosis of MAP is made when the placenta is adherent to the uterus wall with heavy bleeding from implantation site after manual removing the placenta and no cleavage plane identified between the placenta and uterus. Placenta increta indicates that the placenta villi invade the uterine muscle. Placenta percreta means that the placenta villi penetrate to or through the uterine serosa. Prenatal diagnosis of placenta increta/percreta based on ultrasonography or magnetic resonance imaging assessment and confirmed at CD. Or postoperative pathologic examination from hysterectomy specimens in a few cases. Cases with placenta increta/percreta referring to our tertiary centre for surgical complications after delivery were excluded from the study. PPH was defined as amount of bleeding that exceed 1000 mL following CD. A total of 104 cases who were diagnosed as placenta increta/percreta primarily based on the medical records available at the hospital database system over the study period were enrolled in the study.
In our center, all cases with placenta increta/percreta received comprehensive counseling and were provided written informed consent before any treatment. All balloon catheter placements were performed in the angiography suite by an experienced interventional radiology team. The occlusion of IAA was performed via the percutaneous femoral arterial catheterization according to Saldinger technique. Occlusion balloon catheters were placed in IAA (Fig. 1). The proper positioning of the IAABC and the effective vascular occlusion were angiographically confirmed during the insufflation of the balloon. Once IAABC was correctly positioned, the patients were transferred from the interventional radiology suite to the operating room. After the baby was delivered and the umbilical cord clamped, temporary IAABC occlusion was implemented before placental dissection. The balloon was inflated for 5 minutes if hemostasis was secured, and the inflations were alternated with deflations of 1 to 2 minutes (Fig. 2). The endovascular instruments were removed immediately after stabilization in the postoperative recovery room, and hemostasis at the puncture sites was obtained by manual compression.
Figure 1.
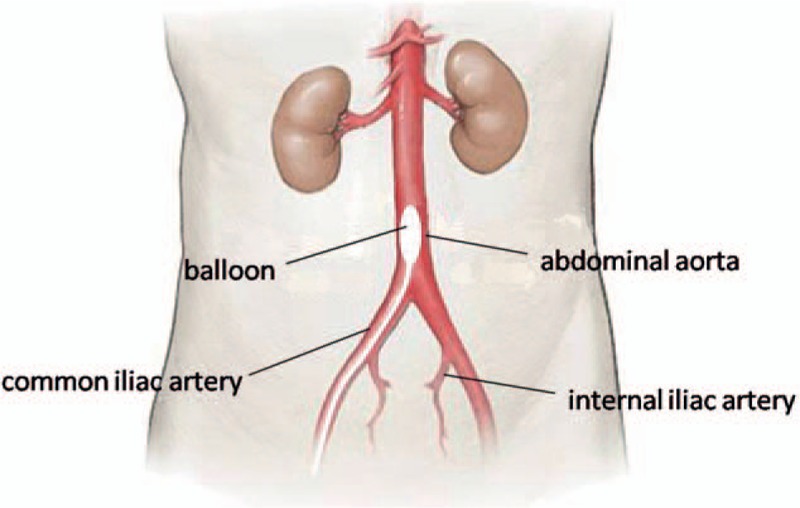
Diagram of the pelvic vascularization to show the site where the balloon is positioned.
Figure 2.
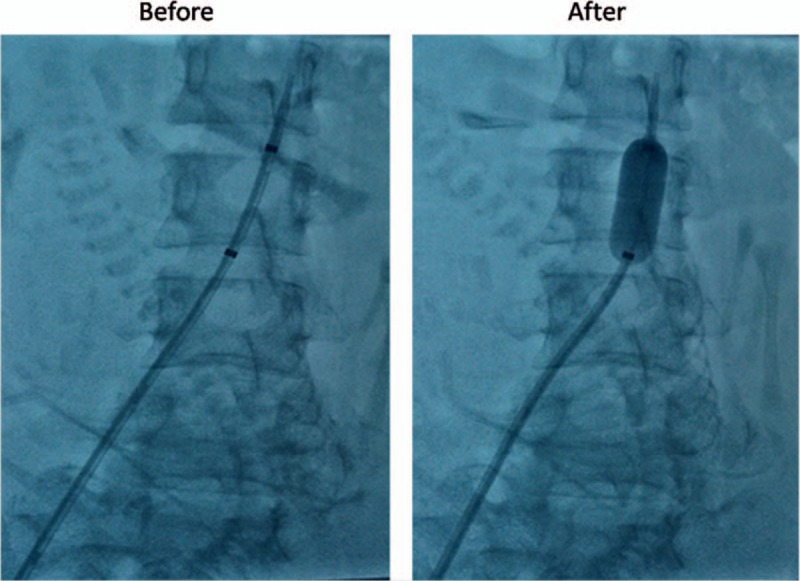
Preoperative placement of infrarenal abdominal aorta balloon catheter and contrast medium injected through the catheters confirms their correct position.
Bakri tamponade was performed in cases with PPH in one of the following situations: an uncontrolled bleeding happened after the use of uterotonic drugs or prevention of postoperative bleeding in the implantation site. The insertion of Bakri balloon was done transabdominally during CD as formerly described.[22] The distal end of the balloon shaft was passed through the cervical opening with an assistant pulling vaginally. Bakri balloon was partially filled with 100 mL of saline to keep it in proper place, then the uterine incision was closed carefully before filling the balloon completely. After the insertion of Bakri balloon, it was considered successful if the bleeding was stopped, and unsuccessful if further surgical interventions (ligation of the pelvic arteries, uterine arterial embolism (UAE), hysterectomy) were required to control bleeding.[24] In successful cases, the balloon remained in place for a maximum of 48 hours. All cases had a Foley catheter inserted into the urinary bladder monitor urine output and received broad spectrum antibiotic prophylaxis for at least 48 hours.
The cases with placenta increta/percreta were subdivided into categories based on the use of IAABC, and compared their outcomes respectively. Primary maternal outcomes included EBL (mL), blood products transfusions (BPT, U), hysterectomy, operative time (min), postoperative days (day), intensive care unit (ICU) admission, surgical complications, reoperation, or maternal death. Primary fetal outcomes included gestational age (weeks), birth weight (g), Apgar score at 1 and 5 minutes, newborn ICU (NICU) admission.
The statistical package SPSS for Windows, release 19.0 was used for data analysis. Statistical significance was calculated using the Chi-square or Fisher exact tests for differences in qualitative variables and the Student t test for differences in continuous variables, and a value of P < .05 was considered significant.
3. Results
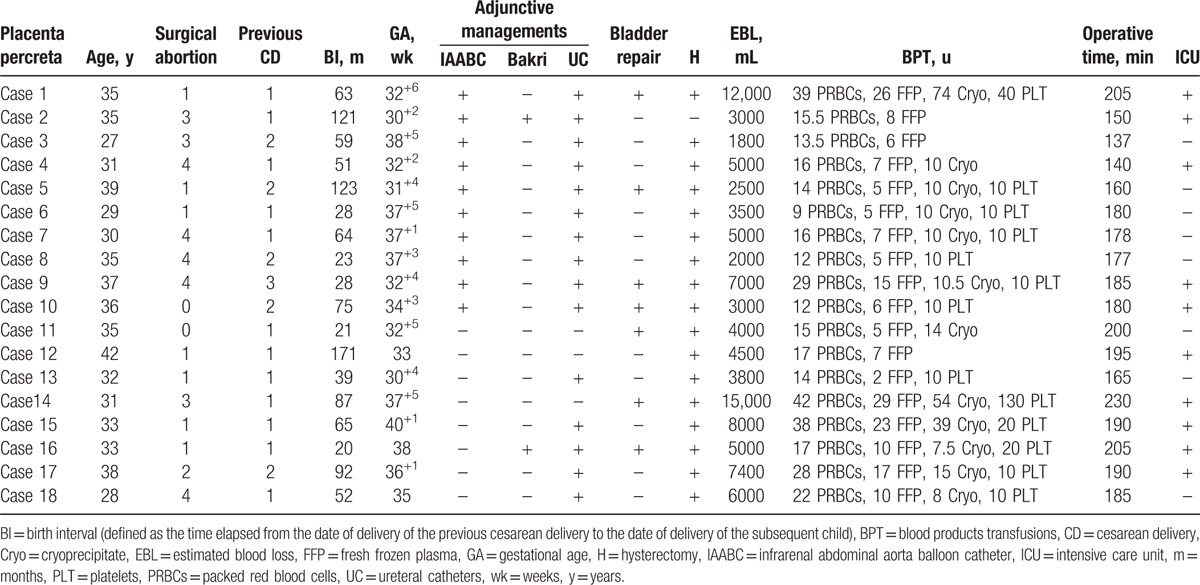
During the study period, 18 cases with placenta percreta were identified. All of them had a history of CD and combined with placenta previa. 17/18 (94.4%) of them suspected placenta percreta before delivery. Only case 15 had an intraoperative diagnosis. Table 1 summarizes the clinical characteristics and outcomes of the cases with placenta percreta. Compared with the cases without IAABC placed (n = 8), those with IAABC (n = 10) tended to have less maternal hemorrhagic morbidity. Although not significant, we did observe less mean EBL and BPT (4480 ± 3091.85 mL vs 6712.5 ± 3683.72 mL, P = .181; 49.05 ± 47.38 u vs 79.19 ± 77.49 u, P = .324, respectively). The mean operative time trended significantly less (169.2 ± 21.72 minutes vs 195 ± 18.52 minutes, P = .017). Almost all (17/18) the cases underwent caesarean hysterectomy due to massive hemorrhage. 10/18 cases admitted to the ICU after the major surgery. Their stays in the ICU ranged from 24 hours to 5 days. Nearly half of cases (7/18) required urinary bladder repair, while there were no major organ damage and no other long-term morbidity in our series of 18 cases. The Bakri balloon was inserted in case 2 and case 16. The former reserved uterus successfully, the latter was failed and eventually underwent hysterectomy. No differences in fetal outcomes were found between the cases with and without IAABC.
Table 1.
Clinical characteristics and outcomes of the cases with placenta percreta.
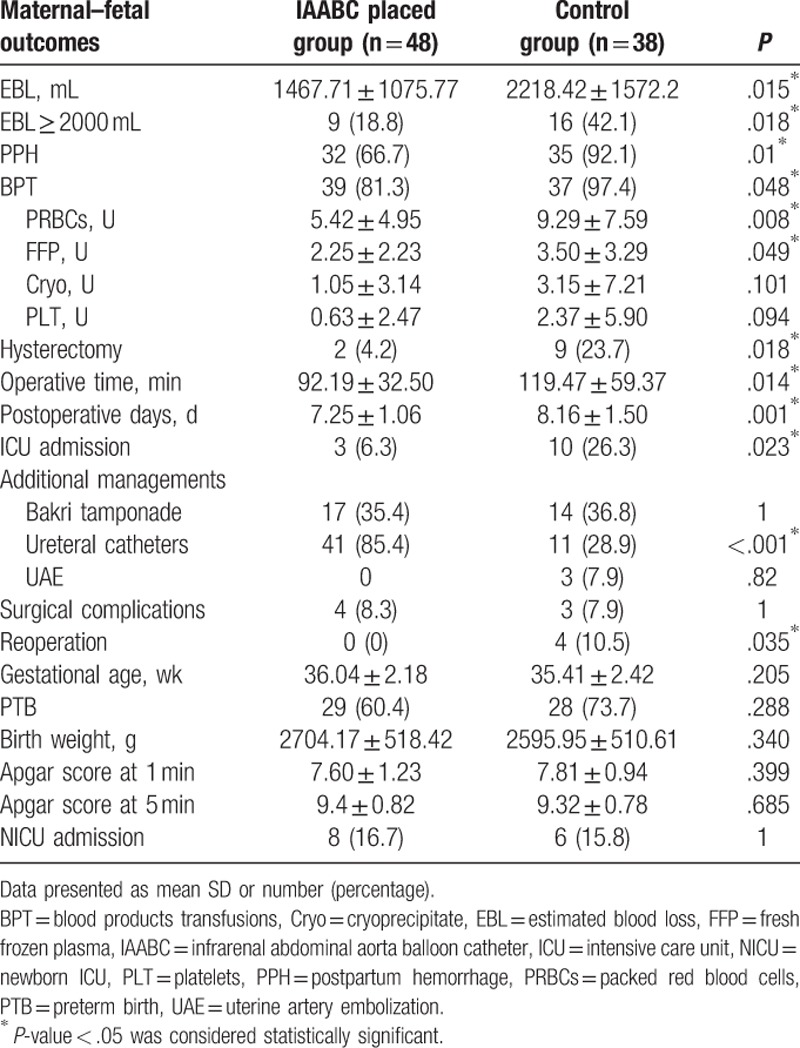
Of the 86 cases with placenta increta identified in our database, 48 cases in the IAABC placed group and 38 cases in the control group. The demographic and clinical characteristics of the 86 cases diagnosed with placenta increta are listed in Table 2. All of them presented at least one of the risk factors for MAP: previous CD, surgical abortion, or placenta previa. The demographic and obstetric characteristics of the 2 groups were similar. Preoperatively, balloon catheters were successfully placed in all cases in the IAABC placed group. The primary maternal–fetal outcomes of placenta increta are shown in Table 3. Compared with cases in the control group, cases in the IAABC placed group had less mean intraoperative EBL (1467.71 ± 1075.77 mL vs 2218.42 ± 1572.2 mL, P = .017), lower number of cases with EBL greater than 2000 mL or with PPH (18.8% vs 42.1%, P = .018; 66.7% vs 92.1%, P = .01, respectively). There was also a lower need for BPT and less amounts of packed red blood cells transfused in the IAABC placed group (81.3% vs 97.4%, P = .048; 5.42 ± 4.95 vs 9.29 ± 7.59, P = .008, respectively). No significant difference in the mean amount of cryoprecipitate or platelets was found between the 2 groups. In the IAABC placed group. Only 2 (4.2%) cases underwent hysterectomy compared with 9 (23.7%) in the control group (P = .018). Thus fewer cases were admitted to the ICU for postoperative surveillance in the IAABC placed group (6.3% vs 26.3%, P = .023). Surgical complications were not different between the 2 groups. Only 1 case had a femoral artery thrombosis specific to the IAABC and recovered after conservative treatment. The fetal outcome was similar in all respects. There was no maternal or neonatal death in this study.
Table 2.
Clinical characteristics of the cases diagnosed as placenta increta with and without IAABC.
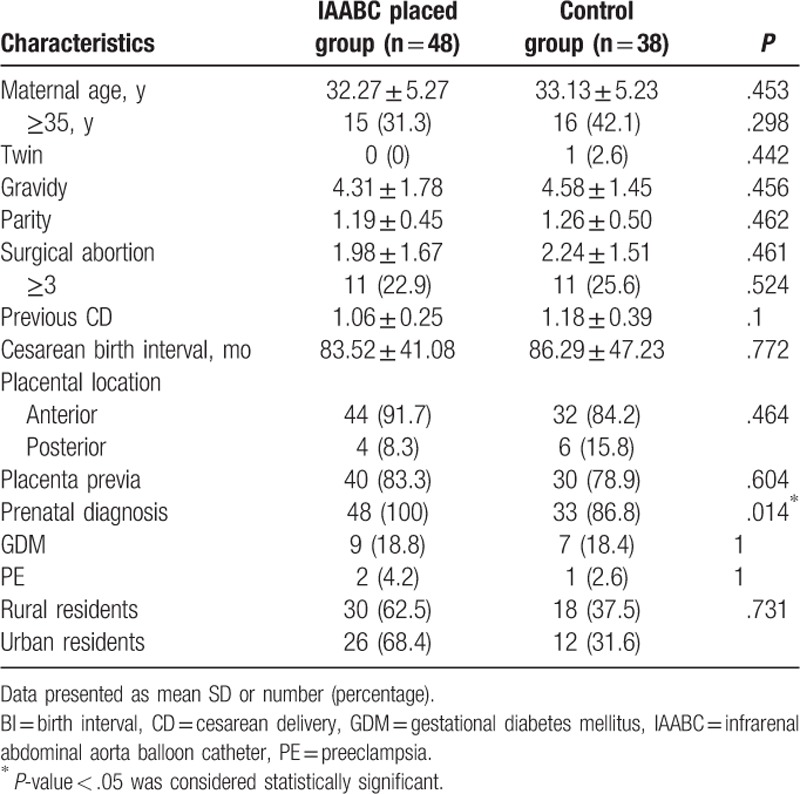
Table 3.
Primary maternal–fetal outcomes in cases diagnosed as placenta increta with and without IAABC.
The Bakri balloon was inserted in 31 cases, and was left in place within 24 hours in 28 cases (90.3%) and for 48 hours in 3 cases (9.7%). The median volume infused into the balloon was 350 mL (range 200–500 mL). In the IAABC placed group, all of 17 cases combined with Bakri tamponade were effective in avoiding hysterectomy. These cases had higher mean intraoperative EBL, compared those with IAABC alone and without hysterectomy (2176.47 ± 875.74 mL vs 843.1 ± 347.37 mL, P < .001). In the control group, 14 cases were treated with Bakri tamponade. Ten were successful,4 failed and required reoperation (3 entailed UAE, 1 needed second exploratory laparotomy and eventually underwent hysterectomy). There were no major complications directly attributable to Bakri tamponade.
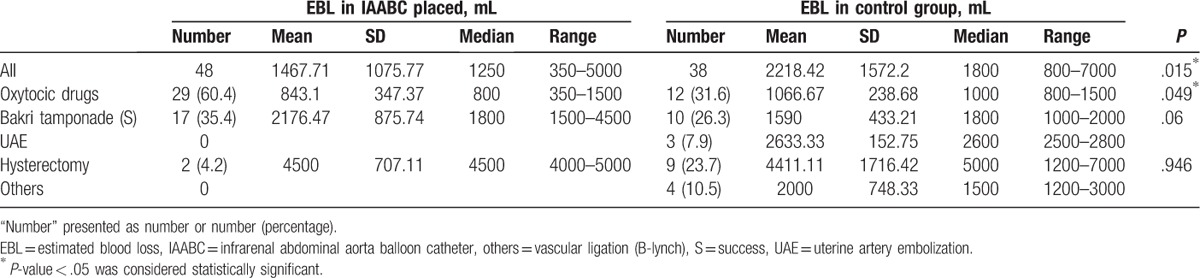
The mean EBL and management of placenta increta between the 2 groups are listed in Table 4. The number of cases using uterotonic drugs alone to control hemorrhage was lower and these cases had less mean EBL in the IAABC placed group, compared with data in the control group (60.4% vs 31.6%, P = .008; 843.1 ± 347.37 mL vs 1066.67 ± 238.68 mL, P = .049, respectively). Moreover, 4 cases in the control group needed B-lynch suture and/or vascular ligation to control bleeding.
Table 4.
Comparing EBL and management of placenta increta between IAABC placed and control group.
4. Discussion
This is the first large study to evaluate the feasibility and safety of preoperative IAABC placed alone or in combination with Bakri tamponade in the management of placenta increta/percreta. We found that maternal outcomes were improved in all respects by such procedures in the management of placenta increta. The rate of hysterectomy in the IAABC placed group was reduced to nearly one-sixth of the rate in the control group (P = .018). 60.4% of cases with placenta increta can preserve uterus by using uterotonic drugs alone in the IAABC placed group, compared with 31.6% in the control group (P = .008). Furthermore, hysterectomy was successfully avoided by a combination IAABC with Bakri tamponade in 17 cases. While these procedures were not as effective as expected in the management of placenta percreta.
Actually, some invasive and conservative approaches have been used to provide adequate hemostasis during surgery for MAP. The traditional techniques include surgical ligation of the pelvic arteries, B-lynch sutures and uterine compression sutures. The disadvantages of these surgical options include the low success rate, long time to control bleeding and increased risk of infection and surgical trauma. Now placement of occlusion balloons is becoming a popular alternative to surgical management in controlling uterine hemorrhage, although its benefits remain a subject of debate. There were particularly conflicting results when the balloons were placed in the IIA or CIA,[9–15] but the results were more consistent when placed in the IAA.[16–20] Viana et al[12] reported a randomized trial including 27 women suspected MAP, and found no benefit to hemostasis by the use of IIA balloon. The failure of IIA balloon occlusion can be largely explained by the extensive anastomoses in the pelvic vasculature. Clausen et al[10] suggested to modify employ CIA occlusion rather than IIA occlusion in women with placenta percreta because intraoperative blood loss and transfusion requirements were considerable. Then Hishikawa et al[13] found such exchange seems to be more effective for reducing blood loss during cesarean hysterectomy in a patient with placenta percreta. In contrast, in a retrospective study involving 25 women undergoing CIA balloon placement with matched controls (27 women), no significant differences were noted in EBL, postoperative hemoglobin drop and transfusion requirement.[15] Data about the IAABC occlusion in literatures indicated its potential benefits.[16–20] In fact, occluding this more proximal site would block the collateral supply from the external iliac arteries. Additionally, unlike the IIA or CIA where bilateral balloons placements are needed, the procedure of IAABC is relatively easy. The balloon can be placed rapidly because a single catheter insertion is sufficient. For cases of placenta increta, with the aid of these endovascular treatments, the overall maternal morbidity was reduced, as measured by decreased EBL, fewer PPH and BPT, lower hysterectomy rate, shorter operative time and postoperative days, and less ICU admission. Similar outcomes were achieved as these by Wu et al.[29] While Xie et al[30] found that only the EBL and decrease in hemoglobin after surgery were significantly lower in the IAA balloon group than in the control group. Multiple factors may account for the variations in efficacy. Firstly, they did not respectively analyze the outcomes of different degree of MAP as this study. Secondly, the diagnosis of MAP was mostly based on clinical criteria and lack of pathological confirmation, thus we cannot rule out the possibility that subjectively overdiagnosing influences the outcomes. Thirdly, the way intraoperative blood loss estimated and transfusion protocols also varies from one center to other. Moreover, experienced maternal–fetal medicine obstetrician and interventional radiologist are the key players in the management of women with MAP. Therefore a comparison of results from different studies is subject to inaccuracies.
It was noteworthy that 17 cases avoided hysterectomy by insertion of Bakri tamponade in the IAABC placed group. Therefore, we believe that the combination of IAABC with Bakri tamponade did appear to be more effective in preserving the uterus in the women diagnosed with placenta increta. Outcomes were also further improved by the combination of balloon occlusion and embolization of pelvic arteries for women with MAP.[31,32] But it is difficult to draw conclusions as these studies lack controls. Besides pelvic arterial embolization cannot be available promptly during the CD and it requires a radiology intervention suite. Therefore, if massive bleeding persists, caesarean hysterectomy must be performed to avoid maternal mortality. By contrast, Bakri tamponade is simple to apply and could be rapidly implemented in the operating room, which increases the chance of preserving fertility. It deserves to be one of the treatments in the hands of obstetricians who handle the massive hemorrhage of MAP.
Placenta percreta is the most serious of the abnormally invasive placentas and is associated with a significantly higher maternal morbidity. Almost all women with placenta percreta inevitably underwent caesarean hysterectomy regardless of whether IAABC occlusion was performed in our study. Our experience was that, when possible, the use of IAABC made the difficult task of completing a caesarean hysterectomy technically much easier, indeed shorter operative time were achieved in women with IAABC placed. The limited number of cases has not allowed a definite conclusion about the efficacy of this procedure in the management of placenta percreta.
In our study, we experienced only one complication related to the IAABC placement, and there was no case of maternal–fetal mortality. It benefited from accurate prenatal diagnosis followed by careful multispecialty care in our center.
One of the strengths of this study is characterized by a considerable degree of homogeneity: the same multidisciplinary team followed all the cases under consideration, and enforced the same intraoperative protocol and radiology procedure, thus reducing potential operator-dependent bias. The nature of retrospective represents limitations of this study.
5. Conclusion
Preoperative placement of IAABC is effective for reduction in operative blood loss in most women with placenta increta, thus allowing uterine conservation and future fertility. The complication rate for the placement of IAABC is low when performed by an experienced interventional radiology team. However, further studies should be done to evaluate the potential of IAABC in women with placenta percreta. Bakri tamponade can be a good choice in the management of uncontrolled bleeding due to placenta increta/percreta before more aggressive surgeries. We believe that preoperative IAABC combined with Bakri tamponade can significantly improve maternal outcomes to the greatest extent. To achieve these improvements required a close coordination of multidisciplinary team.
Footnotes
Abbreviations: BPT = blood products transfusions, CD = cesarean delivery, CIA = common iliac arteries, EBL = estimated blood loss, IAA = infrarenal abdominal aorta, IAABC = infrarenal abdominal aorta balloon catheter, ICU = intensive care unit, IIA = internal iliac arteries, MAP = morbidly adherent placenta, NICU = newborn ICU, PPH = postpartum hemorrhage, UAE = uterine arterial embolism.
The authors have no conflicts of interest to disclose.
References
- [1].Silver RM, Landon MB, Rouse DJ, et al. Maternal morbidity associated with multiple repeat Cesarean deliveries. Obstet Gynecol 2006;107:1226–32. [DOI] [PubMed] [Google Scholar]
- [2].Fitzpatrick KE, Sellers S, Spark P, et al. Incidence and risk factors for placenta accreta/increta/percreta in the UK: a national case-control study. PLoS ONE 2012;7:e52893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Mehrabadi A, Hutcheon JA, Liu S, et al. Contributionof placenta accreta to the incidence of postpartum hemorrhage and severe postpartum hemorrhage. Obstet Gynecol 2015;125:814–21. [DOI] [PubMed] [Google Scholar]
- [4].Thurn L, Lindqvist PG, Jakobsson M, et al. Abnormally invasive placenta-prevalence, risk factors and antenatal suspicion: results from a large population-based pregnancy cohort study in the Nordic countries. BJOG 2016;123:1348–55. [DOI] [PubMed] [Google Scholar]
- [5].Lumbiganon P, Laopaiboon M. Method of delivery and pregnancy outcomes in Asia: the WHO Global Survey on Maternal and Perinatal Health 2007–2008. Lancet 2010;375:490–9. [DOI] [PubMed] [Google Scholar]
- [6].Liu Y, Li G, Chen Y, et al. A descriptive analysis of the indications for caesarean section in mainland China. BMC Pregnancy Childbirth 2014;14:410–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].de la Cruz CZ, Thompson EL, O’Rourke K, et al. Cesarean section and the risk of emergency peripartum hysterectomy in high-income countries: a systematic review. Arch Gynecol Obstet 2015;292:1201–15. [DOI] [PubMed] [Google Scholar]
- [8].Silver RM, Fox KA, Barton JR, et al. Center of excellence for placenta accreta. Am J Obstet Gynecol 2015;212:561–8. [DOI] [PubMed] [Google Scholar]
- [9].Omar HR, Karlnoski R, Mangar D, et al. Staged endovascular balloon occlusion versus conventional approach for patients with abnormal placentation: a literature review. J Gynecol Surg 2012;28:247–54. [Google Scholar]
- [10].Clausen C, Stensballe J, Albrechtsen CK, et al. Balloon occlusion of the internal iliac arteries in the multidisciplinary management of placenta percreta. Acta Obstet Gynecol Scand 2013;92:386–91. [DOI] [PubMed] [Google Scholar]
- [11].Cali G, Forlani F, Giambanco L, et al. Prophylactic use of intravascular balloon catheters in women with placenta accreta, increta and percreta. Eur J Obstet Gynecol Reprod Biol 2014;179:36–41. [DOI] [PubMed] [Google Scholar]
- [12].Viana PP, Machado AP, Montenegro N. Precesarean prophylactic balloon catheters for suspected placenta accreta: a randomized controlled trial. Obstet Gynecol 2015;126:1022–8. [DOI] [PubMed] [Google Scholar]
- [13].Hishikawa K, Koshiyama M, Ueda M, et al. Exchange of intraoperative balloon occlusion of the internal iliac artery for the common iliac artery during cesarean hysterectomy in a patient with placenta percreta. Am J Case Rep 2013;14:409–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Min MC, Kung HF, Hwang JI, et al. Temporary prophylactic intravascular balloon occlusion of the common iliac arteries before cesarean hysterectomy for controlling operative blood loss in abnormal placentation. Taiwan J Obstet Gynecol 2015;54:493–8. [DOI] [PubMed] [Google Scholar]
- [15].Al-Hadethi S, Fernando S, Hughes S, et al. Does temproray bilateral balloon occlusion of the common iliac arteries reduce the need for intra-operative blood transfusion in cases of placenta accretism? J Med Imaging Radiat Oncol 2017;61:311–6. [DOI] [PubMed] [Google Scholar]
- [16].Paull JD, Smith J, William L, et al. Balloon occlusion of the abdominal aorta during caesarean hysterectomy for placenta percreta. Anaesth Intens Care 1995;23:731–4. [DOI] [PubMed] [Google Scholar]
- [17].Bell-Thomas SM, Penketh RJ, Lord RH, et al. Emergency use of a transfemoral aortic occlusion catheter to control massive haemorrhage at caesarean hysterectomy. BJOG 2003;110:1120–2. [PubMed] [Google Scholar]
- [18].Masamoto H, Uehara H, Gibo M, et al. Elective use of aortic balloon occlusion in cesarean hysterectomy for placenta previa percreta. Gynecol Obstet Invest 2009;67:92–5. [DOI] [PubMed] [Google Scholar]
- [19].Andoh S, Mitani S, Nonaka A, et al. Use of temporary aortic balloon occlusion of the abdominal aorta was useful during cesarean hysterectomy for placenta accreta. Masui 2011;60:217–9. [PubMed] [Google Scholar]
- [20].Chou MM, Ke YM, Wu HC, et al. Temporary cross-clamping of the infrarenal abdominal aorta during cesarean hysterectomy to control operative blood loss in placenta previa increta/percreta. Taiwan J Obstet Gynecol 2010;49:72–6. [DOI] [PubMed] [Google Scholar]
- [21].Nelson WL, O’Brien JM. The uterine sandwich for persistent uterine atony: combining the B-Lynch compression suture and an intrauterine Bakri balloon. Am J Obstet Gynecol 2007;196:e9–10. [DOI] [PubMed] [Google Scholar]
- [22].Diemert A, Ortmyer G, Hollwitz B, et al. The combination of intrauterine balloon tamponade and the B-Lynch procedure for the treatment of severe postpartum haemorrhage. Am J Obstet Gynecol 2012;206:65.e1–4. [DOI] [PubMed] [Google Scholar]
- [23].Vrachnis N, Iavazzo C, Salakos N, et al. Uterine tamponade balloon for the management of massive hemorrhage during cesarean section due to placenta previa/increta. Clin Exp Obstet Gynecol 2012;39:255–7. [PubMed] [Google Scholar]
- [24].Kumru P, Demirci O, Erdogdu E, et al. The Bakri balloon for the management of postpartum hemorrhage in cases with placenta previa. Eur J Obstet Gynecol Reprod Biol 2013;167:167–70. [DOI] [PubMed] [Google Scholar]
- [25].Cho HY, Yong WP, Kim YH, et al. Efficacy of intrauterine Bakri tamponade in cesarean section for placenta previa patients. PLoS ONE 2015;10:e0134282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Lo A, Marie PS, Yadav P, et al. The impact of Bakri tamponade on the rate of postpartum hysterectomy for uterine atony. J Matern Fetal Neonatal Med 2016;30:1163–6. [DOI] [PubMed] [Google Scholar]
- [27].Akdemir N, Cevrioğlu AS, Özden S, et al. Successful treatment of placenta percreta through a combinatorial treatment involving a Bakri balloon and methotrexate—a case report. Ginekol Polska 2015;86:631–4. [PubMed] [Google Scholar]
- [28].Bailit JL, Grobman W, Rice MM, et al. Morbidly adherent placenta treatments and outcomes. Obstet Gynecol 2015;125:683–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Wu Q, Liu Z, Zhao X, et al. Outcome of pregnancies after balloon occlusion of the infrarenal abdominal aorta during caesarean in 230 patients with placenta praevia accreta. Cardiovasc Intervent Radiol 2016;39:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Xie L, Wang Y, Luo FY, et al. Prophylactic use of an infrarenal abdominal aorta balloon catheter in pregnancies complicated by placenta accrete. J Obstet Gynaecol 2017;37:557–61. [DOI] [PubMed] [Google Scholar]
- [31].Sivan E, Spira M, Achiron R, et al. Prophylactic pelvic artery catheterization and embolization in women with placenta accreta: can it prevent cesarean hysterectomy? Am J Perinatol 2010;27:455–61. [DOI] [PubMed] [Google Scholar]
- [32].Wang YL, Duan XH, Han XW, et al. Comparison of temporary abdominal aortic occlusion with internal iliac artery occlusion for patients with placenta accreta—a non-randomised prospective study. Vasa 2017;46:53–7. [DOI] [PubMed] [Google Scholar]


