Abstract
Objective
To investigate the measurement properties of the Functional Test of the Hemiparetic Upper Extremity (FTHUE) and examine how its score may or may not inform design of a rehabilitation program.
Design
The FTHUE was recently used in the Interdisciplinary Comprehensive Arm Rehabilitation Evaluation Stroke (ICARE) Randomized Clinical Trial (RCT). This circumstance provided the opportunity to examine the psychometric properties of the FTHUE as it pertains to contemporary post-stroke rehabilitation and recovery models.
Setting
Outpatient rehabilitation clinic
Participants
109 participants, aged 61.2 ± 13.5 years and 46 ± 20.3 days post-stroke with resultant hemiparesis in the upper extremity
Interventions
Not applicable
Main Outcome Measures
Dimensionality was examined with confirmatory factor analysis (CFA) and person and item measures were derived with Rasch item response analysis. Therapists’ notes were also reviewed.
Results
The CFA results support unidimensionality and 16/17 items fit the Rasch model. The Rasch person separation (2.17) and item separation (4.50) indices, ability strata (3.22), person reliability (0.82) and item reliability (0.95) indicate good measurement properties. Item difficulties ranked from −6.46 to 3.43 logits, however there was a substantial ceiling effect of person measures. Post-hoc examination of therapists’ written observations indicated that the scoring criteria are not sensitive to the movement strategy used for task completion.
Conclusions
The FTHUE’s item difficulty hierarchy indicated that scores adequately distinguished the ability to perform simple vs complex motor movements of functional tasks. However, the FTHUE scoring method did not allow inclusion of the type of movement strategy used to accomplish task items. Therefore, we suggest modifications to the FTHUE that would allow it to be used for collaborative treatment planning and align well with more contemporary perspectives on treatment theory.
Keywords: Stroke, Rehabilitation, Rasch analysis
The Functional Test of the Hemiparetic Upper Extremity (FTHUE) is a performance test to measure functional limitations of upper extremity impairments consisting of 17 graded activities each scored on a pass/fail basis.1 Each item is scored as pass/fail with a “pass” defined as the ability to complete the task. The score is reported as the number of passes out of the total 17 items2,3 and/or the average time to complete items.4 A “pass” indicates that the subject successfully completes the task within the prescribed three minutes; a “fail” indicates that the participant could not complete the activity or exceeded the allowed time. The tasks are arranged so that each successive item requires a more complex motion. It takes approximately 30 minutes (or less) to administer the FTHUE and items required are mostly common objects such as a pillow, zippered shirt, sheet, and rubber bands.
The FTHUE was developed based on Brunnstrom’s recovery theory5 which is associated with traditional motor control perspectives of neurorehabilitation. The FTHUE has shown strong content validity and inter-rater reliability.6–8 Content validity was established with a stepwise regression1 and a high correlation between the Fugl-Meyer Assessment and the FTHUE.6 Interrater reliability was found to be statistically significant.6 The FTHUE has also been used as a baseline and outcome measure for stroke rehabilitation studies2 utilizing interventions such as robotics,9,10 sensory cuing,11 virtual environments,4 and action observation.3
The FTHUE has some advantages over other commonly used assessments of the hemiparetic upper extremity. The functional nature of the tasks allows the therapist and the participant to better assess functioning with everyday tasks, unlike the movements performed during the FuglMeyer Assessment.12 In addition, the FTHUE takes less time to administer than the Wolf Motor Function Test.13
The FTHUE score could be interpreted based on Brunnstrom’s Hemiplegic Record5 indicating the patient’s location along the stages of recovery.14 However, in contemporary rehabilitation practice, ideally, the score should inform design of repetitive and progressively more challenging task-practice sessions to engage behavioral and neural-cognitive motor learning processes.15 It would be advantageous if the mapping of the FTHUE to stages of recovery14 were aligned with contemporary treatment theory. For example, within the Rehabilitation Treatment Taxonomy (RTT) framework, treatment or ingredients exert forces of change on a treatment target through a known or hypothesized mechanism of action16. A treatment must contain the defined essential ingredients pertinent to the specific treatment theory and may contain other active ingredients, each of which contributes to the effects on the treatment target through the specific mechanism of action (e.g., motor learning). Within the RTT framework, the FTHUE could be used to identify the active ingredients or movement strategies needed to contribute to the aspects of functioning directly targeted for change17. To that end, there is a need to understand the relationship between the FTHUE and more contemporary treatment/recovery frameworks.
The overall purposes of this study were to explore the measurement properties of the FTHUE and determine if it could be used to inform a rehabilitation plan consistent with contemporary motor learning and treatment theories.15,17 The Interdisciplinary Comprehensive Arm Rehabilitation Evaluation (ICARE) Stroke Initiative which implemented the Accelerated Skill Acquisition Program (ASAP)18 provided an opportunity to examine the FTHUE in the context of a contemporary intervention program. ASAP is a task-oriented, principle-based approach intended to improve functional skills and is consistent with current evidence-based rehabilitation guidelines.15,18,19 The approach aims to improve upper extremity coordination during performance of meaningful tasks while reducing reach-to-grasp impairments and the need for movement compensations.
Methods
Interdisciplinary Comprehensive Arm Rehabilitation Evaluation (ICARE)
Secondary analyses were performed on data obtained from the ICARE Stroke Initiative, randomized, controlled, upper extremity rehabilitation trial assessing post-stroke arm and hand recovery.18 This study was approved by the administrative university and all participating clinical facility institutional review boards.
Inclusion and exclusion criteria
Inclusion criteria included either an ischemic or intraparenchymal hemorrhagic stroke that occurred within the previous 106 days. Participants exhibited resultant hemiparesis (weakness) in an arm or hand, had some active finger extension movement, were at least age 21, were able to communicate in English (or Spanish at one approved site), and were willing to attend outpatient therapy and all study evaluations for one year. Full inclusion/exclusion criteria are detailed elsewhere.18
Data Collection
The FTHUE was administered by trained therapists in a standardized manner during the orientation and evaluation session for 109 out of 119 participants. Data from 10 participants were not included; 9 participants did not participate in any ASAP sessions and therefore no assessments were performed, and 1 participant received ASAP treatment but the FTHUE data were missing. In the ICARE study, the FTHUE was not used as an outcome measure, but instead, it was used to provide study therapists with a baseline understanding of the participant’s capabilities in order to plan subsequent intervention sessions in collaboration with the participant. The administration of the FTHUE deviated from its standard use in that all 17 items were attempted instead of stopping the test after an item could not be completed. The sample was not designed to analyze the FTHUE as an outcome measure, but instead the ICARE data set provided a unique opportunity to elicit a critical conversation between the patient and clinician for treatment planning. The therapist also wrote qualitative notes based on his/her observation of the participant’s quality of movement/movement strategies during item performance.
Data Analysis
Demographics
Demographic differences and level of impairment (as defined by the upper extremity Fugl-Meyer assessment12) were assessed between participants with and without FTHUE data with t-tests.
Dimensionality
A 1-factor confirmatory factor analysis (CFA, M-Plus v. 6)20 weighted least-squares means and variance adjusted (WLSMV) model21 was applied to test the hypothesis that the FTHUE items measured a single construct. Adequacy of model fit was defined by the standard indices; comparative fit index (CFI) ≥ 0.95,22 Tucker Lewis index (TLI) ≥ 0.95,22 and Root Mean Square Error of Approximation (RMSEA) ≤ 0.06.21
Rasch Analysis
After factor analysis, the Dichotomous Rasch Model23 was applied (Winsteps v.3.90.224) to examine item fit, sensitivity and precision, person reliability, item reproducibility, and the person-item match.
Item fit
Acceptable model fit was defined as mean square (MnSq) values < 1.7 and concurrent standardized z score (z-std) values < 2.0.25
Sensitivity and Precision
Sensitivity was quantified with a person separation variable, which if < 2.00 implied that the assessment was not sensitive enough to differentiate high versus low performers.26 Precision was quantified using the number of statistically distinct person ability strata (according to the following equation: strata = (4* person separation index + 1)/3).26 A higher value indicated greater measurement precision. Strata ≥ 3.0 was considered adequate for the purposes of this study.
Reliability of person measures
The trustworthiness of the person-ability measures was tested with the person reliability estimate. High person reliability (≥ 0.80) suggested that there is a high probability that a high person measure reflects a high level of ability and visa-versa. In Winsteps, this value is conceptually similar to the traditional Cronbach’s alpha.27
Reliability of item difficulty measures
The item reliability value examined, with high item reliability (≥ 0.80) suggesting that the item difficulty hierarchy is reproducible.
Person-Item Match
The relationship between the sample’s ability measures and the item difficulty measures was plotted on the same linear continuum and illustrated on a Wright personitem map.28,29 The Wright map was examined for ceiling and floor effects.
Ceiling/Floor Effects
In Winsteps, people with extreme scores were dropped (casewise) during the calibrations of person and item measures. After the measures for non-extreme persons were estimated, then the extreme scores were reinstated and person-ability measures imputed using a Bayesian approach.27
Therapists’ Qualitative Comments
To gain a deeper understanding of the sample’s performance, participants who scored perfect, or near perfect, on the FTHUE were further assessed with a review of the ASAP therapists’ comments by the first author. This summary assisted in describing the lack of movement quality into generalized themes.
Results
Participants
Demographics
Table 1 describes the demographics of all of the ICARE ASAP participants. There were no statistically significant differences in age or between genders, dominant side, affected side, stroke type, or stroke location for the level of impairment (as defined by the upper extremity Fugl-Meyer assessment) for the 109 participants with FTHUE data and the total sample. There was also no statistically significant difference between the 109 participants with FTHUE data and the 10 participants without FTHUE data with respect to upper extremity FuglMeyer assessment level of impairment.
Table 1.
Participant demographics
| Total (N = 119) |
With FTHUE (N = 109) |
Without FTHUE (N = 10) |
|
|---|---|---|---|
| Gender, No. (%) | |||
| Male | 64 (53.8) | 56 (51.4) | 8 (80.0) |
| Female | 55 (46.2) | 53 (48.6) | 2 (20.0) |
| Age (Mean ± SD) | 60.9 ± 13.7 | 61.2 ± 13.5 | 58.0 ± 16.1 |
| Time since stroke to randomization (days) (Mean ± SD) | 45.2 ± 20.3 | 46.0 ± 20.3 | 37.0 ± 19.7 |
| Dominant side, No. (%) | |||
| Right | 103 (86.6) | 94 (86.2) | 9 (90.0) |
| Left | 16 (15.5) | 15 (13.8) | 1 (10.0) |
| Affected side, No. (%) | |||
| Right | 51 (42.9) | 49 (45.0) | 2 (20.0) |
| Left | 68 (57.1) | 60 (55.1) | 8 (80.0) |
| Stroke type, No. (%) | |||
| Ischemic (w/o hemorrhagic conversion) | 100 (84.0) | 90 (82.6) | 10 (100.0) |
| Ischemic (w/hemorrhagic conversion) | 3 (2.5) | 3 (2.8) | 0 (0) |
| Intraparenchymal hemorrhagic | 16 (13.5) | 16 (14.7) | 0 (0) |
| Stroke location, No. (%) | |||
| Right hemisphere | 57 (47.9) | 50 (45.9) | 7 (70.0) |
| Left hemisphere | 49 (41.2) | 47 (43.1) | 2 (20.0) |
| Brainstem | 11 (9.2) | 11 (10.1) | 0 (0) |
| Cerebellar | 0 (0) | 0 (0) | 0 (0) |
| Other | 2 (1.7) | 1 (0.9) | 1 (10.0) |
| Upper Extremity Fugl-Meyer (Mean ± SD) | 41.7 ± 9.5 | 41.4 ± 9.3 | 44.6 ± 11.0 |
Percentages may not add up to 100% due to rounding.
Dimensionality
The 1-factor model CFA yielded the following fit indices: CFI = 0.99, TLI = 0.98, and RMSEA = 0.04 indicating adequate model fit for all 17 items.
Rasch Analysis
Item Fit
Table 2 presents the item infit and outfit mean square and Z standard statistics. One item, Shirt tuck, exhibited poor infit and outfit statistics (infit MnSq = 2.50, Z std 3.50 and outfit MnSq = 9.90, Z std 3.80). Two items, Hand to lap and Associated reaction, exhibited infit and outfit statistics = 0.00 indicating that the analysis could not determine a fit value because all subjects received maximal scores on the items.
Table 2.
FTHUE Rasch Analysis (n = 109)
| Item | Item Difficulty Measure (error) | Infit MnSq (z-std) | Outfit MnSq (z-std) |
|---|---|---|---|
| Remove rubber band | 3.43 (0.30) | 1.12 (1.00) | 0.98 (0.20) |
| Screw in light bulb | 3.24 (0.30) | 0.84 (−1.20) | 0.63 (−0.60) |
| Cat’s cradle | 2.74 (0.30) | 1.03 (0.30) | 0.96 (0.10) |
| Coin into gauge | 1.05 (0.34) | 0.74 (−1.30) | 0.52 (−1.20) |
| Zip zipper | 0.92 (0.35) | 0.81 (−0.90) | 0.76 (−0.50) |
| Fold sheet | 0.90 (0.36) | 0.70 (−1.50) | 0.40 (−1.60) |
| Box to shelf | 0.51 (0.38) | 0.87 (−0.50) | 0.64 (−0.70) |
| Hold pan lid | 0.03 (0.39) | 0.89 (−0.40) | 0.61 (−.60) |
| Stabilize jar | −0.96 (0.45) | 1.20 (0.80) | 2.96 (1.70) |
| Wring rag | −1.01 (0.45) | 0.72 (−1.00) | 1.03 (0.30) |
| Blocks into box | −1.14 (0.47) | 0.68 (−1.10) | 0.23 (−0.80) |
| Shirt tuck | −1.66 (0.50) | 2.50 (3.50)* | 9.90 (3.80)* |
| Stabilize package | −1.97 (0.53) | 0.90 (−0.20) | 0.30 (−0.40) |
| Stabilize pillow | −2.85 (0.60) | 0.73 (−0.70) | 0.14 (−0.80) |
| Hold pouch | −3.24 (0.65) | 0.95 (0.00) | 0.17 (−0.70) |
| Associated reaction | −5.61 (1.92) | 0.00 (0.00) | 0.00 (0.00) |
| Hand to lap | −6.46 (1.84) | 0.00 (0.00) | 0.00 (0.00) |
Sensitivity and Precision
The person and item separation indices both exceeded 2.0 (person separation = 2.17, item separation = 4.50) thus indicating that the assessment was sensitively able to differentiate between high and low performers. The person ability indicated that the FTHUE separated the sample into 3.22 statistically distinct ability strata, thus indicating that the assessment had adequate measurement precision.
Reliability of person measures
The person reliability was high (0.82) thus supporting the trustworthiness of the person ability measures.
Reliability of item measures
The item reliability was high (0.95) thus supporting the reproducibility of the item difficulty measures.
Person-Item Match
The item difficulty measures are presented in Table 2. Items requiring undifferentiated arm motions such as Hand to lap, Associated reaction, and Hold pouch were the easiest to perform, and items requiring differentiated motor control including dexterity such as Remove rubber band, Screw in light bulb and Cat’s cradle were the most difficult to perform. There were some items that were not consistent with the item order proposed by the original FTHUE designers. For example, Stabilizing a pillow was easier than Stabilizing a package and Blocks in box was easier than Holding a pan lid. Several items exhibited similar difficulty levels; Zip zipper and Fold sheet exhibit item difficulty measures of 0.92 ± 0.35 and 0.90 ± 0.36 logits, respectively. Similarly, Wring rag and Blocks into box exhibited difficulty measures of −1.01 ± 0.45 and −1.14 ± 0.47 logits, respectively.
The person-to-item relationship is visualized on the Wright Person-Item Map shown in Figure 1. Person locations are plotted so that the person has a 50% probability of accomplishing items located at that same point on the logit scale, a > 50% probability of accomplishing items located lower on the logit scale (easy items), and a < 50% probability of accomplishing items located higher on the logit scale (difficult items).
Figure 1. Rasch Analysis Wright Person-Item Map.
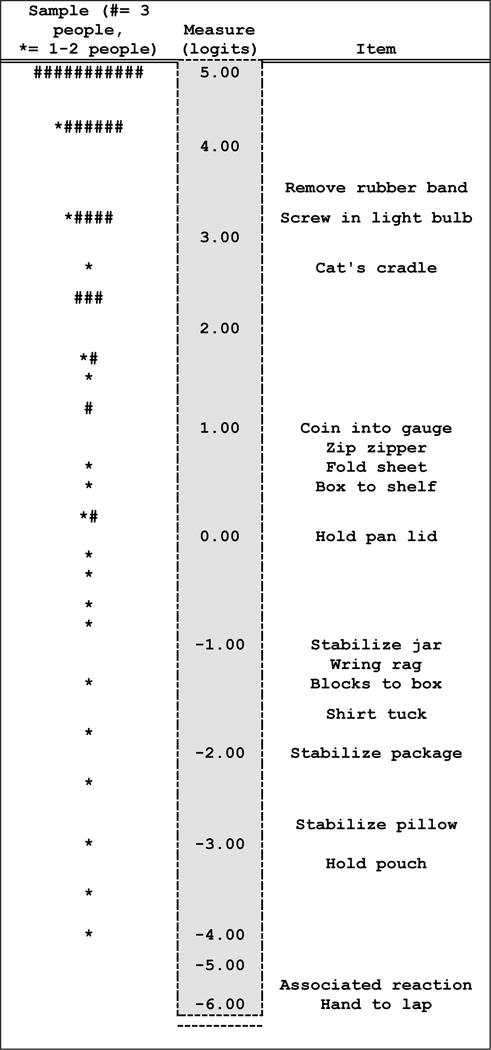
The center vertical column is the measurement metric in logit units ranging from −6.00 to 5.00. Relative to this column, people are to the left and items are to the right. People are located along the metric according to their measures of person ability so that lower ability people (low person measures) are at the bottom of the map, and higher ability people (high person measures) are at the top of the map. Each item is located along the metric according to its measure of item difficulty. The easiest items are located at the bottom of the map and the more difficult items are located at the top of the map.
Ceiling Effect
Comparing the people to the items shows that the person distribution exhibited a ceiling effect. Thirty-three people (30% of the sample) received maximal FTHUE scores of 17 points indicating that the assessment did not yield any information about the actual ability of these subjects because all FTHUE items were “too easy” for them. Mathematically, Rasch analysis does not include perfect (extreme) scores in calculations of sensitivity, precision, and reliability. However, because of this ceiling effect, we assessed how inclusion of these subjects in the analysis would impact the assessment’s measurement properties. Results show that including all data (extreme and non-extreme measures) in the analysis reduced the assessment’s sensitivity (person separation index = 1.60) precision (2.46 strata), and reliability (person reliability = 0.72,) in estimating person-ability measures, but did not impact the sensitivity and reliability of the item difficulty measures (item separation index = 3.41, item reliability = 0.92).
Therapists’ qualitative comments
Evaluator comments of the 33 participants with maximal scores were reviewed by the first author. A total of 115 comments addressed 3 themes; use of atypical movement strategies to complete the task (86% of all comments), multiple attempts required (10%), and motor planning deficits (4%). For example, regarding the item Hold pillow, an evaluator wrote “decreased shoulder adduction required shoulder compensation/elevation when manipulating pillow.” Regarding the item Coin in gauge, an evaluator wrote “Dropped the dime twice as attempting to place in the slot.” And regarding the item Cat’s cradle, an evaluator wrote “Could not problem solve which fingers to put around the string - difficulty coordinating the thumb and 5th finger to hold the string.”
Discussion
The overall purpose of this study was to explore the measurement properties of the FTHUE and determine if it could be used to inform a rehabilitation treatment plan consistent with contemporary motor learning and treatment theories. Analysis was applied to existing data obtained from participants with stroke-related mild to moderate upper extremity impairment who participated in a national multi-site randomized clinical trial. The results provide information about how the FTHUE score can be interpreted in the context of contemporary theories and suggests ways in which it could be modified.
Measurement Properties of FTHUE Items
The FTHUE items exhibited good measurement properties. Both the CFA results and Rasch fit statistics support the assessment’s unidimensionality. These findings give confidence that the FTHUE score meaningfully indicated a single construct (UE function).
Most the items fit the Rasch model’s expectations that the subjects with low ability had less successful item performance than subjects with high ability. One item, “shirt tuck” exhibited poor fit statistics suggesting that subjects demonstrated erratic responses to it, i.e., it was not always easy/hard across the sample. Perhaps this item tests a unique functional upper extremity skill such as a proximal motion (i.e., shoulder abduction/internal rotation) while the other items test a proximal-distal coordinated motion. This item could be eliminated if there was a need to shorten the assessment.
Item Difficulty Hierarchy
An advantage of Rasch analysis is that person-ability and item-difficulty measures are plotted on the same metric.23 The Wright map illustrates the person-to-item relationship, showcasing items (functional tasks) that are easy enough for people with low ability, and hard enough for people with higher ability. For example, individuals with low FTHUE scores successfully performed easy functional tasks that require use of the paretic arm as a stabilizer, while individuals with higher FTHUE scores successfully performed difficult functional tasks that require use of the paretic arm to perform individual finger movements embedded in dexterous manipulation.
The Wright map showed a gap between item 14 (“Coin in gauge”) and item 15 (“Cat’s cradle”), suggesting that some individuals exhibited more motor skill than is required to insert a coin into a gauge, but less motor skill than is required to accomplish Cat’s cradle, and these individuals will not be assessed by this measure. In other assessments, gaps in the measurement metric have been addressed by the addition of items30 and that could be done in the case of the FTHUE. Perhaps new items could be added to reflect more current real-world tasks, such as mobile phone use.
The Wright map also indicated several items having similar item difficulty calibrations. For example, items 10 (“Zip zipper”) and 11 (“Fold sheet”) exhibit nearly identical difficulty measures. Similarly, items 12 (“Blocks into box”) and 8 (“Wring rag”) exhibited difficulty measures within 1 SE of each other. This finding suggests that no additional information about the patient’s skill level is gained by using items with similar difficulty calibrations. Therefore, the assessment could be shortened by removing one of two items with similar difficulty calibrations without losing any information. Similarly, Woodbury, et al, 2007,31 used the same psychometrics to determine the dimensionality and construct validity of the Fugl-Meyer Assessment. Three reflex items were found to be disconnected from other assessment items, and when removed, the Fugl-Meyer Assessment showed a unidimensional structure.
In its original design the FTHUE was intended to locate a patient along Brunnstrom’s 6 stages of recovery to assist a therapist in understanding the outcome of a therapy program designed to reintegrate motor synergies and basic reflexes.1 However, today, post-stroke rehabilitation emphasizes behavioral re-learning, challenging practice, and improved capacity to accomplish increasingly more difficult movement tasks.15 Ideally, the FTHUE score would specify exactly where the patient is located on the measurement metric thereby clarifying which functional tasks are easy, difficult, and “just-right”.15 The FTHUE measured UE function by whether or not a task was performed but does not detail skilled behavior. A revision of the FTHUE’s scoring method could help better inform a treatment program consistent with contemporary perspectives of motor control and learning. In a similar way, Woodbury, et al, 2010,32 investigated the theoretical framework of the Wolf Motor Function Test and found that the assessment does measure a single construct related to motor learning theory. In particular, the relationship between a stroke survivor’s ability and the task difficulty is important.
Ceiling Effect
Post-hoc analysis showed that the 33 subjects with perfect FTHUE scores had an average UEFM score of 49/66, compared to the 76 subjects without perfect FTHUE scores who had an average UEFM score of 39/66. Thus, the subjects with maximal FTHUE scores had less motor impairment compared to the rest of the sample. Overall, this subsample (n = 109) exhibited mild stroke severity and demonstrated moderate33 upper extremity impairment (UEFM = 41.7), and so the ceiling effect of the FTHUE was not unexpected. However, as reported by Edwards and colleagues for a similar dataset, our sample likely experienced persistent disability, difficulty with complex activities, and reduced life satisfaction despite having mild stroke severity and moderate arm motor impairment.34 So, despite the finding of so many people with a maximum FTHUE score, they may still exhibit important functional limitations that were not detected by the FTHUE.
A review of the therapist’s qualitative comments confirmed that the FTHUE scores were not always congruent with the therapist’s observations. As the participants with perfect FTHUE scores performed each item, therapists observed and noted poor movement quality and/or altered movement strategies. Although the therapists rated successful task completion, they also noted motor impairments. Importantly, these qualitative comments were more useful for the treatment plan than the FTHUE score. Future studies should consider use of the FTHUE in treatment planning as it was for ICARE and in contrast to its use as simply an outcome measure.
For studies in which the FTHUE is used to inform a personalized treatment plan, we recommend a revision to the scoring method with the addition of an ordinal rating scale. This scale could be similar to the Wolf Motor Function Test’s Functional Ability Scale13 or the Reaching Performance Scale35 both of which utilize ordinal ratings to highlight aspects of movement quality critical to task performance.
Study Limitations
The FTHUE was administered in ICARE for the purpose to inform the therapist and patient about UE function and not as it was intended as an outcome measure. For our purposes, this is considered to be a unique opportunity for this secondary analysis, that could not otherwise have been possible. We do acknowledge that we traded this unique opportunity to assess the FTHUE in the context of the ICARE trial for the limitation on generalizability of our findings. The sample size and makeup of mostly moderately affected stroke patients does limit generalizability.
Conclusion
In a sample of moderately impaired stroke patients with relatively pure motor hemiparesis, the FTHUE was found to contain most tasks that measure the same construct of post-stroke upper extremity functional ability. The Rasch item difficulty hierarchy indicates that this sample could easily complete functional tasks requiring use of the paretic arm to hold or stabilize objects but were more challenged by functional tasks requiring dexterous individual finger movements for manipulation. Hence, the FTHUE can add some information about post-stroke functional ability and, in conjunction with other assessments, the FTHUE could aid in informing treatment decisions for patients with mild to moderate levels of motor impairment. Specifically, the FTHUE could be used as a tool to facilitate the patient-therapist collaboration pertaining to development of a personalized treatment plan to solve the movement problem.
Acknowledgments
Monica A. Nelsen, Christianne Lane, Alexander W. Dromerick
Financial support: The ICARE trial was funded jointly by the National Institutes of Health, the National Institute of Neurological Disorders and Stroke (primary), and the National Center for Medical Rehabilitation Research of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grant #U01NS056256).
Abbreviations
- ASAP
Accelerated Skill Acquisition Program
- CFA
Confirmatory Factor Analysis
- CFI
Comparative Fit Index
- FTHUE
Functional Test of the Hemiparetic Upper Extremity
- ICARE
Interdisciplinary Comprehensive Arm Rehabilitation Evaluation Stroke
- MnSq
Mean Square
- RCT
Randomized Clinical Trial
- RMSEA
Root Mean Square Error of Approximation
- TLI
Tucker Lewis Index
- WLSMV
Weighted Least-Squares Means and Variance Adjusted
- UEFM
Upper Extremity Fugl-Meyer
- z-std
standardized z score
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest: We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated AND, if applicable, we certify that all financial and material support for this research (eg, NIH or NHS grants) and work are clearly identified in the title page of the manuscript.
Trial registration: clinicaltrials.gov Identifier: NCT00871715
Contributor Information
Veronica T. Rowe, Department of Occupational Therapy, University of Central Arkansas, Conway, AR, USA.
Carolee J. Winstein, Division of Biokinesiology and Physical Therapy, Herman Ostrow School of Dentistry; Department of Neurology, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA.
Steven L. Wolf, Departments of Rehabilitation Medicine, Medicine and Cell Biology, Emory School of Medicine, VA Center on Visual and Neurocognitive Rehabilitation, Atlanta, GA, USA.
Michelle L. Woodbury, Department of Health Science and Research, Medical University of South Carolina, Charleston, SC, USA.
References
- 1.Wilson DJ, Baker LL, Craddock JA. Functional test for the hemiparetic upper extremity. AJOT. 1984;38(3):159–164. doi: 10.5014/ajot.38.3.159. [DOI] [PubMed] [Google Scholar]
- 2.Winstein CJ, Rose DK, Tan SM, Lewthwaite R, Chui HC, Azen SP. A randomized controlled comparison of upper-extremity rehabilitation strategies in acute stroke: A pilot study of immediate and long-term outcomes. Arch Phys Med Rehabil. 2004;85(4):620–628. doi: 10.1016/j.apmr.2003.06.027. [DOI] [PubMed] [Google Scholar]
- 3.Sugg K, Müller S, Winstein C, Hathorn D, Dempsey A. Does action observation training with immediate physical practice improve hemiparetic upper-limb function in chronic stroke? Neurorehabil Neural Repair. 2015;29(9):807–17. doi: 10.1177/1545968314565512. [DOI] [PubMed] [Google Scholar]
- 4.Fischer HC, Stubblefield K, Kline T, Luo X, Kenyon RV, Kamper DG. Hand rehabilitation following stroke: A pilot study of assisted finger extension training in a virtual environment. Topics in Stroke Rehabilitation. 2007;14(1):1–12. doi: 10.1310/tsr1401-1. [DOI] [PubMed] [Google Scholar]
- 5.Brunnstrom S. Movement therapy in hemiplegia. New York: Harper Rowe; 1970. [Google Scholar]
- 6.Filiatrault J, Arsenault AB, Dutil E, Bourbonnais D. Motor function and activities of daily living assessments: A study of three tests for persons with hemiplegia. The American journal of occupational therapy: official publication of the American Occupational Therapy Association. 1991;45(9):806–810. doi: 10.5014/ajot.45.9.806. [DOI] [PubMed] [Google Scholar]
- 7.Ng AKY, Leung DPK, Fong KNK. Clinical utility of the action research arm test, the wolf motor function test and the motor activity log for hemiparetic upper extremity functions after stroke: A pilot study. Hong Kong Journal of Occupational Therapy. 2008;18(1):20–27. [Google Scholar]
- 8.Wilson DJ. Assessment of the hemiparetic upper extremity: A functional test. Occup Ther Health Care. 1984;1(2):63–69. doi: 10.1080/J003v01n02_07. [DOI] [PubMed] [Google Scholar]
- 9.Hidler J, Nichols D, Pelliccio M, Brady K. Advances in the understanding and treatment of stroke impairment using robotic devices. Topics in Stroke Rehabilitation. 2005;12(2):22–35. doi: 10.1310/RYT5-62N4-CTVX-8JTE. [DOI] [PubMed] [Google Scholar]
- 10.Lambercy O, Dovat L, Yun H, et al. Effects of a robot-assisted training of grasp and pronation/supination in chronic stroke: A pilot study. Journal of NeuroEngineering and Rehabilitation. 2011;8(1) doi: 10.1186/1743-0003-8-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fong KN, Lo PC, Yu YS, et al. Effects of sensory cueing on voluntary arm use for patients with chronic stroke: A preliminary study. Arch Phys Med Rehabil. 2011;92(1):15–23. doi: 10.1016/j.apmr.2010.09.014. [DOI] [PubMed] [Google Scholar]
- 12.Fugl Meyer AR, Jaasko L, Leyman I. The post stroke hemiplegic patient. I. A method for evaluation of physical performance. Scand J Rehabil Med. 1975;7(1):13–31. [PubMed] [Google Scholar]
- 13.Wolf SL, Catlin PA, Ellis M, Archer AL, Morgan B, Piacentino A. Assessing wolf motor function test as outcome measure for research in patients after stroke. Stroke. 2001;32(7):1635–1639. doi: 10.1161/01.str.32.7.1635. [DOI] [PubMed] [Google Scholar]
- 14.Brunnstrom S. Motor testing procedures in hemiplegia: Based on sequential recovery stages. Phys Ther. 1966;46(4):357–375. doi: 10.1093/ptj/46.4.357. [DOI] [PubMed] [Google Scholar]
- 15.Winstein C, Lewthwaite R, Blanton S, Wolf L, Wishart L. Infusing motor learning research into neurorehabilitation practice: A historical perspective with case exemplar from the accelerated skill acquisition program. J Neurol Phys Ther. 2014;38(3):190–200. doi: 10.1097/NPT.0000000000000046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Whyte J, Dijkers MP, Hart T, et al. Development of a theory-driven rehabilitation treatment taxonomy: Conceptual issues. Arch Phys Med Rehabil. 2014;95(1 SUPPL) doi: 10.1016/j.apmr.2013.05.034. [DOI] [PubMed] [Google Scholar]
- 17.Hart T, Tsaousides T, Zanca JM, et al. Toward a theory-driven classification of rehabilitation treatments. Arch Phys Med Rehabil. 2014;95(1 SUPPL):S33–S44. doi: 10.1016/j.apmr.2013.05.032. [DOI] [PubMed] [Google Scholar]
- 18.Winstein C, Wolf S, Dromerick A, et al. Interdisciplinary comprehensive arm rehabilitation evaluation (ICARE): A randomized controlled trial protocol. BMC Neurology. 2013;13 doi: 10.1186/1471-2377-13-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Winstein CJ, Wolf SL, Dromerick AW, et al. Effect of a task-oriented rehabilitation program on upper extremity recovery following motor stroke the ICARE randomized clinical trial. JAMA. 2016;315(6):571–581. doi: 10.1001/jama.2016.0276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Muthen L, Muthen B. Mplus statistical analysis with latent variables user’s guide. 6th. Los Angeles, CA: Muthen & Muthen; 1998–2010. [Google Scholar]
- 21.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model. 1999;6(1):1–55. [Google Scholar]
- 22.Marsh HW, Balla JR, McDonald RP. Goodness-of-fit indexes in confirmatory factor analysis: The effect of sample size. Psychol Bull. 1988;103(3):391–410. [Google Scholar]
- 23.Wright B, Stone M. Best test design. Chicago: Mesa Press; 1979. [Google Scholar]
- 24.Linacre JM. Detecting multidimensionality: Which residual data-type works best? J Outcome Meas. 1998;2(3):266–283. [PubMed] [Google Scholar]
- 25.Wright B, Linacre J. Reasonable mean-square fit values. Rasch Measurement Transactions. 1994;8(3):370. [Google Scholar]
- 26.Fisher W. Reliability, separation, strata statistics. Rasch Measurement Transactions. 1992;6(3):238. [Google Scholar]
- 27.Linacre JM. Winsteps rasch measurement computer program. 2015 http://www.winsteps.com/winman/reliability.htm.
- 28.Wright B, Masters GN. Rating scale analysis. Chicago, Illinois: MESA Press; 1982. [Google Scholar]
- 29.Wilson M. Some notes on the term: Wright map. Rasch Measurement Transactions. 2011;25(3):1331. [Google Scholar]
- 30.Sabari JS, Woodbury M, Velozo CA. Rasch analysis of a new hierarchical scoring system for evaluating hand function on the motor assessment scale for stroke. Stroke Res Treat. 2014;2014 doi: 10.1155/2014/730298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Woodbury ML, Velozo CA, Richards LG, Duncan PW, Studenski S, Lai SM. Dimensionality and construct validity of the fugl-meyer assessment of the upper extremity. Arch Phys Med Rehabil. 2007;88(6):715–723. doi: 10.1016/j.apmr.2007.02.036. [DOI] [PubMed] [Google Scholar]
- 32.Woodbury M, Velozo CA, Thompson PA, et al. Measurement structure of the wolf motor function test: Implications for motor control theory. Neurorehabil Neural Repair. 2010;24(9):791–801. doi: 10.1177/1545968310370749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Woodbury ML, Velozo CA, Richards LG, Duncan PW. Rasch analysis staging methodology to classify upper extremity movement impairment after stroke. Arch Phys Med Rehabil. 2013;94(8):1527–1533. doi: 10.1016/j.apmr.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 34.Edwards DF, Hahn M, Baum C, Dromerick AW. The impact of mild stroke on meaningful activity and life satisfaction. Journal of Stroke and Cerebrovascular Diseases. 2006;15(4):151–157. doi: 10.1016/j.jstrokecerebrovasdis.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 35.Lèvin MF, Desrosiers J, Beauchemin D, Bergeron N, Rochette A. Development and validation of a scale for rating motor compensations used for reaching in patients with hemiparesis: The reaching performance scale. Phys Ther. 2004;84(1):8–22. [PubMed] [Google Scholar]


