Abstract
Physician-scientists are needed to continue the great pace of recent biomedical research and translate scientific findings to clinical applications. MD-PhD programs represent one approach to train physician-scientists. MD-PhD training started in the 1950s and expanded greatly with the development of the Medical Scientist Training Program (MSTP), launched in 1964 by the National Institute of General Medical Sciences (NIGMS) at the National Institutes of Health. MD-PhD training has been influenced by substantial changes in medical education, science, and clinical fields since its inception. In 2014, NIGMS held a 50th Anniversary MSTP Symposium to highlight the program and assess its outcomes. As of 2016, there were over 90 active MD-PhD programs in the United States, of which 45 were MSTP-supported, with a total of 988 trainee slots. Over 10,000 students have received MSTP support since 1964. The authors present data for the demographic characteristics and outcomes for 9,683 MSTP trainees over the period 1975–2014. The integration of MD and PhD training has allowed trainees to develop a rigorous foundation in research in concert with clinical training. MSTP graduates have had relative success in obtaining research grants, and some have become prominent leaders in many biomedical research fields. Many challenges remain, however, including the need to maintain rigorous scientific components in evolving medical curricula, to enhance research-oriented residency and fellowship opportunities in a widening scope of fields targeted by MSTP graduates, to achieve greater racial diversity and gender balance in the physician-scientist workforce, and to sustain subsequent research activities of physician-scientists.
Physician-scientists, who have clinical understanding coupled with the scientific skills to conduct state-of-the art research, are needed for both disease mechanism research and bench-to-bedside translation. This has dictated the development of training pathways that provide rigorous scientific training in concert with clinical training. Some physician-scientists receive their major scientific training during residency or fellowship research periods after completion of medical school. MD-PhD dual degree training, which provides scientific training earlier in the training sequence, represents another approach. Since 1964, MD-PhD training has been facilitated by Medical Scientist Training Program (MSTP) support from the National Institute of General Medical Sciences (NIGMS) of the National Institutes of Health (NIH). A meeting was held on July 17, 2014, at the NIH campus in Bethesda, MD, to recognize the 50th anniversary of the MSTP. Here, we review the development and evolution of MD-PhD training programs over the past 50 years and assesses the outcomes of MD-PhD training.
Historical Foundations of MD-PhD Training and the Launch of the Medical Scientist Training Program
Early forces driving biomedical research and the nature of physician-scientist training
The advent and evolution of MD-PhD training has been shaped by changes in medical education, science, and clinical fields over the last century. In 1910, the Flexner Report1 identified the need for medical education to incorporate scientific advances with clinical instruction. The Public Health Service Act of 1944 created the National Institutes of Health and established its responsibility for both research and research training. Dr. Vannevar Bush, Director, Office of Scientific Research and Development, produced his influential report “Science – The Endless Frontier,”2 which emphasized that scientific progress was essential for public welfare, the war against disease, and national security. Medical schools developed larger faculty sizes, including increased numbers of both MD and PhD research faculty.
The tremendous potential for translation of scientific research to impact clinical care highlighted the need to develop programs to train physician-scientists. At the same time, evolving trends in medicine and science provided new challenges for training physician-scientists. Medicine and science, and their training pathways, became increasingly sophisticated and specialized, increasing the length of training and making it harder to combine activities in multiple fields. The increasing length of specialized clinical training delayed and decreased research training opportunities for physicians. Science similarly became increasingly specialized, requiring longer periods of training to become an independent scientist.
Physician-scientist training before the MSTP era
Recognizing the importance of developing the physician-scientist workforce, the NIH initiated the Experimental Training Program in 1956–1957. This program involved summer research experiences for medical students and, at some schools, extra years for research (some included the possibility of earning an MS degree).3 In 1961, Drs. Vincent Price and Frederick Stone at NIGMS developed a second phase called the Medical Student Research Training Program. In 1956, Western Reserve University (now Case Western Reserve University) launched what, to our knowledge, was the first continuous integrated MD-PhD program, which developed in synergy with the innovative Western Reserve MD curriculum that was introduced in the 1950s.4 This curriculum introduced an integrated curricular approach and emphasized flexible, self-directed learning, which fit well with the integration of PhD training. Pre-MSTP era trainees from this program included Nobel laureates Ferid Murad and Alfred G. Gilman. During the tenure of Dr. James Shannon as NIH Director (1955–1968) NIH institutes and programs were expanded, and Dr. Shannon was directly involved in developing physician-scientist training. He supported the start of research training right after college in MD-PhD programs that would combine training in medicine and science. With growing interest at training sites across the country in the concept of MD-PhD training, the need for NIH support became apparent.
The beginning of the MSTP era
In 1964 the NIGMS launched the Medical Scientist Training Program (MSTP) to fund MD-PhD programs to train physician-scientists. The prior Medical Student Research Training Program was phased out. An NIH policy change allowed training grant support for the medical curriculum phase in the context of dual-degree integrated MD-PhD training. Dr. Vincent Price of the NIGMS was the first NIH MSTP program director and played an influential role in the early years of the MSTP. During this period, emphasis was developed on quality and rigor of science, high standards for trainees and programs, attempts to enhance science in medical education, and growing appreciation of the need for flexibility for the range of different students and training directions.
NIH awarded MSTP funding to three MD-PhD programs in 1964: Albert Einstein College of Medicine of Yeshiva University, New York University, and Northwestern University. Over the next 15 years, approximately half of the current MSTPs were established (see Supplemental Digital Appendix 1 [LWW INSERT LINK]). The addition of new programs since 1980 has resulted in a total of 45 NIH-funded MSTPs as of 2016.5 Another 455, or so, medical schools have MD-PhD programs without MSTP funding. A complete listing of MD-PhD programs is provided by the Association of American Medical Colleges (AAMC).6 Furthermore, the intramural NIH MD-PhD Partnership Training Program has been developed to engage the research and intellectual resources of the intramural NIH program with partner universities for MD-PhD training.
Evolution of MD-PhD training
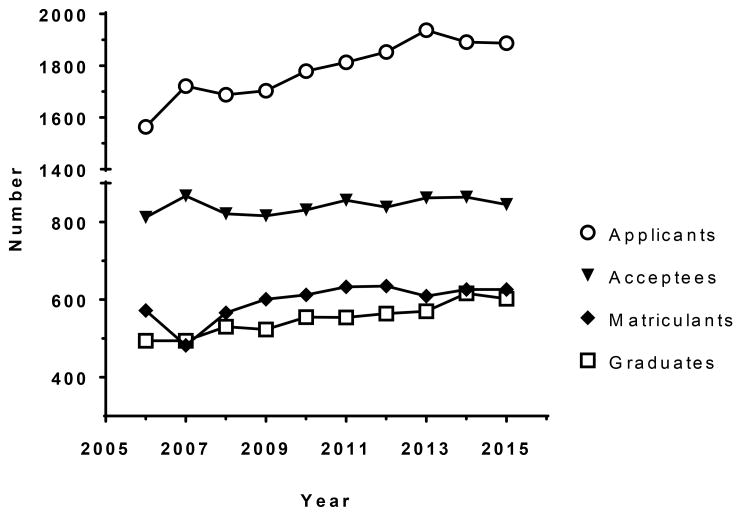
As of 2016, there are more than 5,000 MD-PhD students in training (MSTP and non-MSTP programs combined) with an average time to receive both degrees of approximately 8 years.7 In recent years, approximately 600 students annually matriculate into MD-PhD programs, and about 550 graduate each year (Figure 1). In fiscal year (FY) 2015, the MSTP-supported programs received 952 NIGMS-supported MSTP full-time training positions, and 26 additional trainees were supported by the NIH MD-PhD Partnership Training Program. The level of NIGMS support has varied from a maximum of 60–62 trainee positions for the largest programs in the early 1970s to as low as 4 slots for recently funded programs. In FY2015, the mean number of NIGMS supported MSTP slots per program was 21.2 (median 21, range 5–48). On average, MSTP trainee positions support approximately 25% of the MD-PhD student training years in MSTP-funded programs. Other training support is provided by substantial institutional commitments, as well as by other training grants, individual fellowships, and research grants during the graduate research years.
Figure 1.
Numbers of applicants, acceptees, matriculants, and graduates of MD-PhD training programs as reported by the Association of American Medical Colleges, 2006–2015.20
The organization of the MSTP at the NIH has changed over the last 50 years. The National Research Service Award (NRSA) Act of 1974 restructured all NIH training programs, including the MSTP. It established the T32 training grant support for institutional MSTP awards, and established individual NRSA fellowship grants (e.g., the F30 award that currently provides individual fellowship support for MD-PhD training). At NIH, the program directors of the MSTP have included Drs. Vincent Price (1964–1984), Lee Van Lenten (1984–1994), Bert Shapiro (1994–2010), and Peter Preusch (2011–present). These directors have provided insight, advice, and leadership for the development of the MSTP and MD-PhD training in national forums and through engagement with individual MSTPs and students.
A vibrant national MD-PhD training community has developed, particularly over the last 30 years. Since 1985, the National MD-PhD Student Conference has been organized by the University of Colorado MSTP. In 1995, the National Association of MD-PhD Programs was established, with annual meetings that were sometimes coupled with the National MD-PhD Student Conference. This organization fostered the development of best practices and shared approaches for MD-PhD training and admissions. This group developed a relationship with the Association of American Medical Colleges (AAMC), which led to the formation in 2004 of the MD-PhD Section of the AAMC Group on Graduate Research Education and Training. The AAMC MD-PhD Section has further fostered the development and dissemination of best practices for MD-PhD training. It has established the American Medical College Application Service (AMCAS) MD-PhD application, promoted the recruitment of students into MD-PhD training, developed unified “traffic rules” for admission to medical schools and MD-PhD programs (e.g. uniform expected decision dates and other admissions process rules as for MD admission practices), and improved outcomes analysis. In 2005, the American Physician Scientists Association was formed as a national organization of MD-PhD and MD students interested in careers as physician-scientists.
Evaluation and Outcomes of MD-PhD Training
Prior studies of MD-PhD training outcomes
A number of studies have assessed the outcomes of MD-PhD training7–16; here we discuss only a few prior studies. In 1998, a study by Glowinski et al8 concluded that MSTP graduates as a group have successful research careers, and their pursuit of research fellowships, later academic appointments, grants at several levels, and publications all exceeded MD-only graduates from the same institutions. Most MSTP graduates (92%) were found to have entered residency training. The study also noted a worrisome trend toward increasing time to degree (TTD) from the 1970s to the 1990s. In 2010, a study by Brass et al7 of 20 MSTP and 4 non-MSTP programs confirmed the increasing TTD and showed that the mean TTD had risen to 8.0 years. The attrition rate was about 10%. Ninety-five percent of MSTP graduates entered residencies, and 81% of alumni who had completed postgraduate training remained in academia, at research institutes, or in industry. Only 16% were in private practice. Of alumni in academia, 82% were doing research, 61% were funded, and 66% had >50% effort devoted to research. Research topics included basic, translational, and clinical research even though most trainees had done laboratory-based PhDs. MD-PhD graduates enter a wide range of clinical specialties.9 The diversity of specialties has increased in recent years (compared to the 1990s, fewer recent MD-PhD graduates have chosen internal medicine, pediatrics, pathology, or neurology, and more have selected dermatology, ophthalmology, radiation oncology, or surgical fields).7 While research opportunities exist in all clinical disciplines, the choice of clinical specialty has been associated with degree of success in the subsequent development of research careers. Brass et al reported that the percentage of graduates entering private practice was less than 20% for pathology (8%), psychiatry (12%), pediatrics (13%), neurology (13%), radiation oncology (15%), and internal medicine (16%), but over 40% for family medicine (62%), emergency medicine (46%), dermatology (44%), ophthalmology (44%), and radiology (41%).7
NIGMS data for evaluation of MSTP outcomes
NIGMS sponsored a meeting on July 17, 2014, to recognize the 50th anniversary of the MSTP. The program included physician-scientist speakers who received MSTP training (N.J. Dorsey, J. Federspiel, C.V. Harding, G.J. Lyon, L.M. McAllister-Lucas, J.C. Niles, and A. Weiss) and featured scientific presentations as well as discussion of the history and outcomes of MSTP training. The NIGMS Office of Extramural Research conducted analyses of MSTP trainees and their outcomes. Data were compiled for all trainees appointed to MSTP training grants since the creation of the NRSA-related appointment and tracking system in 1975, including NIH records for trainees who could be identified in both the trainee record and the NIH grant record system by cross-over of a unique Person ID number. Data from the National Science Foundation Survey of Earned Doctorates17 and AAMC Faculty Roster Survey18 were also included in analyses.
Over the period analyzed (1975–2014), 9,704 initial NRSA trainee appointments were made (trainees appointed at more than one institution are double counted in the total). Demographic data were retrieved for 9,683 individually identifiable trainees from the NIH grants data system Information for Management, Planning, Analysis and Coordination (IMPACI-II) Current and History Files (accessed May 21, 2014). This file reports MSTP trainees who received NRSA T32 support by race, ethnicity, gender, age, and time period for FYs 1975–2014, including independent tables for race, ethnicity, gender, and age of MSTP trainees in 4 ten-year cohorts as well as totals for the 1975–2014 time period. Data on race, ethnicity, gender, and age (totals and binned by decade) are shown in Table 1. The total number of trainees has increased during each of the past four decades, with the largest cohort (over twice the size of the 1975–1984 cohort) still largely in residency and fellowship training. This cohort will have a major impact on the physician-scientist workforce as the graduates mature in their careers.
Table 1. MSTP Trainee Demographic Characteristics, by Decade and Cumulativelya.
| Characteristic | No. (%) | ||||
|---|---|---|---|---|---|
| 1975–1984 | 1985–1994 | 1995–2004 | 2005–2014 | 1975–2014 | |
| Race | |||||
| White | 784 (51.7) | 949 (49.6) | 1,822 (63.4) | 2,068 (61.3) | 5,623 (58.1) |
| Asian | 52 (3.4) | 288 (15.0) | 568 (19.8) | 744 (22.0) | 1,652 (17.1) |
| Other coded | 13 (0.9) | 51 (2.7) | 224 (7.8) | 308 (9.1) | 596 (6.2) |
| Black | Not released | Not released | Not released | Not released | 356 (3.7) |
| Native | Not released | Not released | Not released | Not released | 29 (0.3) |
| Pacific | Not released | Not released | Not released | Not released | 19 (0.2) |
| More than one race | Not released | Not released | Not released | Not released | 192 (2.0) |
| Uncoded | 632 (41.7) | 590 (30.8) | 192 (6.7) | 28 (0.8) | 1,442 (14.9) |
| Withheld | 36 (2.4) | 37 (1.9) | 69 (2.4) | 228 (6.8) | 370 (3.8) |
| Ethnicity | |||||
| Non-Hispanic | 506 (33.4) | 659 (34.4) | 1,208 (42.0) | 2,735 (81.0) | 5,108 (52.8) |
| Hispanic | 12 (0.8) | 37 (1.9) | 128 (4.5) | 209 (6.2) | 386 (4.0) |
| Unknown | 978 (64.5) | 1,189 (62.1) | 1,494 (52.0) | 314 (9.3) | 3,975 (41.1) |
| Withheld | 21 (1.4) | 30 (1.6) | 45 (1.6) | 118 (3.5) | 214 (2.2) |
| Gender | |||||
| Male | 1,257 (82.9) | 1,414 (73.8) | 1,850 (64.3) | 2,079 (61.6) | 6,600 (68.2) |
| Female | 238 (15.7) | 468 (24.4) | 974 (33.9%) | 1,238 (36.7) | 2,918 (30.1) |
| Unknown | 22 (1.5) | 33 (1.7) | 51 (1.8%) | 59 (1.7) | 165 (1.7) |
| Age | |||||
| 18–25 | 1,141 (75.2) | 1,557 (81.3) | 2,206 (76.7%) | 2,346 (69.5) | 7,250 (74.9) |
| 26–30 | 309 (20.4) | 274 (14.3) | 548 (19.1%) | 898 (26.6) | 2,029 (21.0) |
| 31 and over | 15 (1.0) | 26 (1.4) | 72 (2.5%) | 81 (2.4) | 194 (2.0) |
| Unknown | 52 (3.4) | 58 (3.0) | 49 (1.7%) | 51 (1.5) | 210 (2.2%) |
| Total trainees | 9,683 | ||||
Abbreviation: MSTP indicates Medical Scientist Training Program.
Data from the National Institutes of Health grants data system Information for Management, Planning, Analysis and Coordination (IMPACI-II) Current and History Files, accessed May 21, 2014. Due to small sizes, numbers for individual racial groups are not reported except for the overall 1975–2014 period. “Other coded” combines data for Black/African American, Native American/Alaska Native, Native Hawaiian/Pacific Islander, and More than one race for each 10-year subset. Uncoded = no data entered. Withheld = intentionally withheld by the trainee. Unknown = uncoded or intentionally withheld.
Early cohort data on race/ethnicity is substantially incomplete because of missing information (uncoded or withheld race/ethnicity information). Reporting has improved such that only 7.6% were uncoded or withheld in 2005–2014. Both Asians and underrepresented minority groups, particularly Hispanics, have grown as a percent of the total (Table 1). The number of women appointed has grown over five-fold (238 in 1975–1984 to 1,238 in 2005–2014) and more than doubled as a percentage of the total appointments (from 15.7% in 1975–1984 to 36.7% in 2005–2014). For comparison, the percentage of women among all medical school matriculants has increased from 31.4% in 1982–198319,20 to 47.8% in 2015–2016.20,21
Table 2 presents outcomes data on two cohorts of MSTP trainees, one with their first training grant appointment in 1980–1989 and another with first appointment in 1990–1999. Assuming an 8-year time to completion of MD-PhD training,7 trainees appointed in 1980–1989 may have begun training as early as 1973 with initial appointment in their final year, or may have just begun training in 1989. Thus, most of the trainees in the first cohort would have completed their residency/fellowship training from approximately 1980 to the mid-2000s. Based on data from the National Science Foundation Survey of Earned Doctorates,17 the vast majority of this cohort completed PhD training (88.8%), somewhat higher than the completion rate for comparison groups that included non-MSTP (PhD-only) NIGMS training grant appointees and PhD-only predoctoral trainees supported by other Institutes of the NIH (Table 2). Data from the AAMC Faculty Roster Survey18 show that many in this MSTP cohort were successful in obtaining medical school faculty positions (61.9%), which is approximately three times the rate for both PhD-only comparison groups. This MSTP cohort also applied for and received mentored career development, research project grant, and R01 equivalent awards in greater numbers and percentages than the comparison groups (Table 2). Overall, 42.2% have applied for R01s and 33.6% have received awards (approximately twice the frequency of this outcome in the PhD-only comparison groups).
Table 2. Outcomes for MSTP Trainees and PhD-Only NRSA Traineesa.
| Trainee type and gender | No. trainees | No. (%)trainees who achieved various outcomes | |||||||
|---|---|---|---|---|---|---|---|---|---|
| PhD awarded | Medical school faculty | Mentored K award | Research project grant | R01 equivalent | |||||
| Applicant | Awardee | Applicant | Awardee | Applicant | Awardee | ||||
| Predoctoral trainees with initial NRSA appointments between 1980–1989 | |||||||||
| MD-PhD supported by NIGMS MSTP T32 | |||||||||
| Women | 388 | 329 | 213 | 57 | 49 | 146 | 114 | 139 | 110 |
| Men | 1,690 | 1,516 | 1,073 | 214 | 184 | 797 | 655 | 738 | 588 |
| Total | 2,078 (100) | 1,845 (88.8) | 1,286 (61.9) | 271 (13.0) | 233 (11.2) | 943 (45.4) | 769 (37.0) | 877 (42.2) | 698 (33.6) |
| PhD supported by NIGMS non-MSTP T32 | |||||||||
| Women | 3,625 | 2,905 | 545 | 28 | 22 | 704 | 543 | 588 | 459 |
| Men | 5,380 | 4,669 | 1,229 | 50 | 43 | 1,637 | 1,282 | 1,433 | 1,137 |
| Total | 9,005 (100) | 7,574 (84.1) | 1,774 (19.7) | 78 (0.9) | 65 (0.7) | 2,341 (26.0) | 1,825 (20.3) | 2,021 (22.4) | 1,596 17.7) |
| PhD supported by non-NIGMS T32 | |||||||||
| Women | 5,624 | 4,474 | 788 | 50 | 36 | 1,047 | 739 | 867 | 623 |
| Men | 5,332 | 4,539 | 1,239 | 51 | 36 | 1,408 | 1,008 | 1,187 | 872 |
| Total | 10,956 (100) | 9,013 (82.3) | 2,027 (18.5) | 101 (0.9) | 72 (0.7) | 2,455 (22.4) | 1,747 (15.9) | 2,054 (18.7) | 1,495 (13.6) |
| Predoctoral trainees with initial NRSA appointment between 1990–1999 | |||||||||
| MD-PhD supported by NIGMS MSTP T32 | |||||||||
| Women | 822 | 686 | 254 | 190 | 139 | 168 | 112 | 152 | 95 |
| Men | 2,201 | 1928 | 871 | 603 | 455 | 672 | 442 | 587 | 374 |
| Total | 3,023 (100) | 2,614 (86.5) | 1,125 (37.2) | 793 (26.2) | 594 (19.6) | 840 (27.8) | 554 (18.3) | 739 (24.4) | 469 (15.5) |
| PhD supported by NIGMS non-MSTP T32 | |||||||||
| Women | 4,824 | 3,824 | 341 | 200 | 116 | 747 | 480 | 563 | 358 |
| Men | 5,848 | 4,883 | 749 | 314 | 170 | 1,402 | 876 | 1,132 | 716 |
| Total | 10,672 (100) | 8,707 (81.6) | 1,090 (10.2) | 514 (4.8) | 286 (2.7) | 2,149 (20.1) | 1,356 (12.7) | 1,695 (15.9) | 1,074 (10.1) |
| PhD supported by non-NIGMS T32 | |||||||||
| Women | 8,166 | 6,465 | 851 | 441 | 274 | 1,667 | 970 | 1,227 | 643 |
| Men | 6,748 | 5,483 | 1,162 | 488 | 317 | 1,747 | 1,089 | 1,390 | 817 |
| Total | 14,914 (100) | 11,948 (80.1) | 2,013 (13.5) | 929 (6.2%) | 591 (4.0) | 3,414 (22.9) | 2,059 (13.8) | 2,617 (17.5) | 1,460 (9.8) |
Abbreviations: MSTP indicates Medical Scientist Training Program; NRSA, National Research Service Award Act of 1974; NIGMS, National Institute of General Medical Sciences; NIH, National Institutes of Health.
Outcomes of T32 predoctoral trainee cohorts appointed in fiscal years 1980–1989 or 1990–1999 with comparison of MSTP versus other NRSA training programs. Data were obtained from IMPAC-II Current and History files accessed May 22, 2014, and joined to a 2012 National Science Foundation Survey of Earned Doctorates file17 and the 2012 Association of American Medical Colleges Faculty Roster Survey.18 Mentored K awards include K01, K08, K22, K23, K25, K99, and R00. Research project grants include all types of individual research project awards but do not include program project or center grants (individual subproject investigator records were only captured in recent years, hence this deviation from current NIH definition of program project grants as research project grants in order to allow proper comparison between cohorts from different periods). R01 equivalents include R01, R29, R37, and DP2 awards. The follow-up period for completion of a PhD or faculty appointment was from the time of trainee appointment through 2012. The follow-up period for becoming an NIH applicant or awardee was from the time of trainee appointment through May 22, 2014. Trainees are counted in every group for which they are relevant and may be in more than one group, as groups are not mutually exclusive.
The second cohort (first training grant appointment in 1990–1999) may have started as early as 1983 or as late as 1999, and most of these trainees would have completed their residency/fellowship training from approximately 1990 to the mid-2010s. These individuals have had a shorter window of opportunity to find placements and apply for grants than the first cohort. Again, most students (86.5%) completed a PhD. Fewer (37.2%) had faculty positions as of 2014; results of a 2015 AAMC MD-PhD outcomes survey may shed additional light on academic position outcomes, but these data are not yet available. A larger number pursued and obtained mentored career development (K) awards, which presumably reflects the growth of this funding mechanism (career development awards increased from 1,029 awards in 1997 to 3,113 awards in 2014).22 Of this second cohort, 27.8% applied for an NIH research project grant, 18.3% received a research project grant, and 15.5% received an R01 equivalent award (the latter are also included in the proportion receiving a research project grant). The differences between the 1980–1989 and 1990–1999 cohorts may reflect changes in their passage down the training pipeline or the organizational structure of academia and its grant support, as well as the general increase in age of NIH principal investigators upon receipt of their first grant support. In any case, the rate at which MSTP trainees receive NIH grant awards exceeds that of PhD-only trainees on all metrics shown in Table 2, and the proportion of R01 applicants who received R01s remains high (64.0%).
Relative to the first cohort, the second cohort has a higher proportion of trainees who are women (27.2% versus 16.2%), and a higher proportion of women achieved academic positions (22.6% versus 16.5%). Women also increased as fraction of the R01 applicant pool (20.6% versus 15.8%) and R01 awardees (20.3% versus 15.8%). The fraction of applicants who received R01 support was similar for men and women.
Of great interest to each of the individual NIH institutes is the participation of former MSTP trainees in its particular research mission. Table 3 includes data on the research project applications and awards through FY2014 for all MSTP trainees with initial appointments in 1975–2014. In aggregate, the 9,683 trainees described above have submitted 19,621 research project applications and received 5,708 research project awards (including 4,227 R01 awards). This group also submitted a total of 2,212 career award applications and received 1,117 career awards. The distribution of awards among the various NIH institutes corresponds with the relative overall budgets of the institutes.23 These data demonstrate that the MSTP provides training for areas relevant to all of the institutes of the NIH. Also of interest is the type of research conducted by MSTP trainees. Table 4 provides data on the coding of awards for the involvement of animal subjects, human subjects, clinical research and clinical trials, and the use of RCDC (Research, Condition and Disease Categorization) terms. These data indicate that many MSTP graduates are involved in research that may be translational or patient-oriented and clinical (39.3% of awardees involved in research involving human subjects; 74.2% involved in research involving animal subjects).
Table 3. National Institutes of Health Research Applications and Awards for Medical Scientist Training Program Traineesa.
| Institute | Research career programs | Research project grants | R01 equivalent | |||
|---|---|---|---|---|---|---|
| Applications | Awards | Applications | Awards | Applications | Awards | |
| NIAAA: National Institute on Alcohol Abuse and Alcoholism | 9 | 4 | 108 | 34 | 69 | 21 |
| NIA: National Institute on Aging | 71 | 39 | 675 | 201 | 429 | 125 |
| NIAID of Allergy and Infectious Disease | 259 | 145 | 2,495 | 790 | 1,688 | 535 |
| NIADDK: National Institute of Arthritis, Diabetes, Digestive and Kidney Diseases [now defunct] | 4 | 1 | 23 | 9 | 16 | 5 |
| NIAMS: National Institute of Arthritis and Musculoskeletal and Skin Diseases | 109 | 54 | 711 | 192 | 520 | 139 |
| NCCAM: National Center for Complementary and Alternative Medicine | 0 | 0 | 74 | 12 | 31 | 5 |
| NCI: National Cancer Institute | 424 | 152 | 3,738 | 980 | 2,753 | 729 |
| NIDA: National Institute on Drug Abuse | 52 | 31 | 406 | 133 | 275 | 82 |
| NIDCD: National Institute on Deafness and Other Communication Disorders | 18 | 8 | 187 | 68 | 128 | 50 |
| NIDCR: National Institute of Dental and Craniofacial Research | 12 | 6 | 139 | 43 | 90 | 21 |
| NIDDK: National Institute of Diabetes and Digestive and Kidney Diseases | 203 | 128 | 1,852 | 595 | 1,446 | 444 |
| NIBIB: National Institute of Biomedical Imaging and Bioengineering | 9 | 3 | 172 | 31 | 91 | 17 |
| NIEHS: National Institute of Environmental Health Sciences | 1 | 1 | 191 | 63 | 123 | 39 |
| NEI: National Eye Institute | 47 | 33 | 571 | 215 | 472 | 187 |
| NIGMS: National Institute of General Medical Sciences | 23 | 10 | 1,350 | 463 | 1,243 | 436 |
| NICHD: National Institute of Child Health and Human Development | 57 | 34 | 689 | 152 | 476 | 101 |
| NHGRI: National Human Genome Research Institute | 2 | 1 | 139 | 45 | 73 | 30 |
| NHLBI: National Heart, Lung, and Blood Institute | 309 | 156 | 2,073 | 624 | 1,713 | 523 |
| NLM: National Library of Medicine | 5 | 1 | 58 | 23 | 49 | 19 |
| NIMHD: National Institute on Minority Health and Health Disparities | 0 | 0 | 12 | 2 | 10 | 1 |
| NIMH: National Institute of Mental Health | 172 | 88 | 1,130 | 308 | 762 | 203 |
| NINR: National Institute of Nursing Research | 0 | 0 | 23 | 6 | 16 | 5 |
| NINDS: National Institute of Neurological Disorders and Stroke | 402 | 207 | 2,191 | 649 | 1,647 | 504 |
| NCRR: National Center for Research Resources [now defunct] | 22 | 15 | 33 | 9 | 12 | 5 |
| NCATS: National Center for Advancing Translational Sciences | 0 | 0 | 10 | 5 | 0 | 0 |
| FIC: John E. Fogarty International Center | 1 | 0 | 53 | 19 | 1 | 1 |
| OD Other | 1 | 0 | 518 | 37 | 138 | 0 |
| Total | 2,212 | 1,117 | 19,621 | 5,708 | 14,271 | 4,227 |
Abbreviation: MSTP indicates Medical Scientist Training Program; NIH, National Institutes of Health.
Subsequent NIH competing applications and awards of MSTP trainees with initial appointments in fiscal years 1975–2013 (from IMPAC-II Current and History Files, trainee history accessed on May 21, 2014, and subsequent application and award activity in fiscal years 1975–2014, accessed on December 4, 2014). Award types defined as in Table 2.
Table 4. Research Types for MSTP Graduatesa.
| Type of award | No. MSTP trainees with awards | % awardees |
|---|---|---|
| Involving animal subjects | 2,032 | 74.2 |
| Involving human subjects | 1,078 | 39.3 |
| Involving both animal and human subjects | 712 | 26.0 |
| Defined as clinical using human subject exemption codes | 995 | 36.3 |
| Defined as clinical using RCDC “clinical trials” | 88 | 3.2 |
| Total number of distinct trainees with subsequent applications | n/a | n/a |
| Total number of distinct trainees with subsequent awards | 2,740 | 100.0 |
| Total number of trainees | 9,683 | n/a |
Abbreviation: MSTP indicates Medical Scientist Training Program; NIH, National Institutes f Health; NIGMS, National Institute of General Medical Sciences; RCDC, Research, Condition, and Disease Categorization process.
The Current State of MD-PhD Training and Future Challenges
Recent developments in MD-PhD training include continued innovation in MD-PhD curricula. Though MD-PhD training still includes phases focused primarily on the MD or the PhD curriculum, these curricula are more integrated than in the past. Many MSTPs now include a clerkship before the PhD phase and/or longitudinal clinical activities in the PhD phase. Challenges include the possibility that the basic science content in medical school curricula may be diminished with the introduction of new MD curricula that organize and present curricular content in new ways that may diminish the focus on scientific foundations, although this is not a necessary outcome of such curricular reforms. Any major revision of one of the constituent curricula (MD or PhD) represents challenges, as well as opportunities, for MD-PhD training. Inclusion of MD-PhD specific activities requires careful planning and institutional commitment.
Recent demographic trends in MD-PhD training
The demand for MD-PhD training as reflected in the number of applicants continues to increase (Figure 1). AAMC data shows that the MD-PhD applicant pool increased by 24% from 1,564 in 2006 to 1,936 in 2016, but the number matriculating increased by only 13% (572 to 649).20 Acceptance into MD-PhD programs has become more competitive.
Meeting the financial demands of MD-PhD training remains challenging. Whereas the number of funded MSTP institutions has increased from 41 to 45 since 2005, the number of MTSP T32 trainee positions remained relatively flat at about 900 slots until FY2015–FY2016. In some years, some programs experienced reductions in funding, and further adjustments may be needed if more MD-PhD programs are supported in the future. Meanwhile, training costs have increased, necessitating that institutions or other funding sources assume a greater proportion of the costs. This has come at a time of decreased research funding and decreased clinical revenues to medical schools and academic hospitals. At some institutions, a portion of MD-PhD training costs may be borne by the trainee.
The MD-PhD trainee pool pipeline continues to be less diverse than MD-only trainees in terms of both gender and underrepresented groups, defined by NIH as including individuals from racial and ethnic groups shown to be underrepresented in biomedical research (including Blacks or African Americans, Hispanics or Latinos, American Indians or Alaska Natives, and Native Hawaiians and other Pacific Islanders). Some of this difference in diversity may be traced to the applicant pool; AAMC data for 2015 show women as 46.8% of all MD applicants24 but only 36.2% of MD-PhD applicants.25 Similarly, in 2015, underrepresented groups were 14.2% of all MD applicants26 but only 12.2% of MD-PhD applicants.27 These numbers are likely underestimates of underrepresented groups, because applicants who report multiple races/ethnicity to the AAMC are categorized as “multiple race/ethnicity,” a category that includes both underrepresented and non-underrepresented groups, and this category is not included in the underrepresented groups numbers cited above (in 2015, multiple race/ethnicity was selected for 7% of MD applicants and 7.3% of MD-PhD applicants). Overall, these data indicate the need for more efforts to develop interest among more diverse groups and to develop diversity at earlier stages of training. Some MSTPs have developed programs to increase the diversity of the applicant pool and thus the student body.28
Challenges in physician-scientist training pathways
There are also challenges to physician-scientists at stages after completion of MD-PhD training that may contribute to attrition of trainees from the biomedical research workforce. Clinical fields have undergone increasing specialization of clinical practice with longer, more specialized training and increased ongoing training requirements (residency, fellowships, subspecialty fellowships, board requirements, CME, maintenance of certification). This has been paralleled by increasing specialization in science, accompanied by increasing needs for funding for complex technical infrastructures and staffing to perform research, as well as increasing regulatory burdens. The result has been increased duration of postgraduate training for both clinical and scientific fields. Long periods of clinical residency/fellowship training can break research momentum, just as long periods of scientific training can interrupt the development and maintenance of clinical skills. In many programs, MD-PhD training curricula have evolved to integrate clinical and research training to some degree, although certain phases focus primarily on one or the other; yet research-intensive residencies and fellowships that integrate research and clinical training are not widely available to trainees in many disciplines. Many of the challenges noted here affect both non-research clinicians and PhD scientists, but are compounded for physician-scientists. Other pressures on the physician-scientist include the lower salaries in academia relative to private practice. In addition, clinical faculty are experiencing increased pressure for clinical productivity, which decreases time available for research. Decreased grant application success rates and diminished buying power of research grants (after correction for inflation) are critical problems, particularly since the end of the NIH budget doubling period in 2003.29
Continuing need to develop the physician-scientist workforce
Despite these challenges, training future physician-scientists remains an NIH mission-critical objective. NIH director Francis Collins created the Physician-Scientist Workforce (PSW) Working Group (PSW-WG) to assess the PSW and make recommendations for how to sustain and strengthen it. The PSW-WG Report30 was presented in 2014. The working group defined physician-scientists as researchers with a medical or other professional doctoral degree (e.g., including MD only; MD-PhD dual degree; and separate MD and PhD degrees). The group found that the total number of physician-scientists has remained stable over the past few decades, while declining as percentage of the total biomedical research workforce. The report revealed that MDs and MDs with a PhD (dual degree or separate) each comprised ∼50% of the NIH grant-supported PSW. There has been a steady increase in average age at first receipt of an NIH research project grant, and the average age of the total PSW has increased steadily (both American Medical Association and NIH data show aging of physicians engaged in research, predicting future decline in the PSW as senior physician-scientists eventually retire). These trends are exacerbated by a decline in the number of new physician-scientists entering the workforce. A continued and reinforced MD-PhD training pipeline represents one solution to these challenges, given the substantial return on NIH investment in the training of physician-scientists that we documented above. Accordingly, the PSW-WG recommended continued support for MD-PhD training along with a number of other specific suggestions.30
The 2014 PSW-WG report also discussed the potential impact of constrained NIH funding on career choices of trainees as they finish MSTPs and other MD-PhD training programs. A decade of declining inflation-adjusted NIH budgets and diminishing success rates did not result in a reduced applicant pool for MD-PhD training programs (Figure 1) but may have contributed to the relative number of accepted applicants who choose not to matriculate in MD-PhD programs. It is our observation that MSTP applicants and MSTP students interviewed at MSTP site visits continue to espouse their desire for careers in academic medicine, with a large majority of their time devoted to research.
There has been evolution in the choice of clinical fields by MD-PhD trainees. More than 95% of graduates go on to complete residency training. Over the past several decades, however, there has been a shift from training in specialties that dominated the residency choices of early MSTP graduates (medicine, pathology, pediatrics, neurology and psychiatry) toward other medical specialties (e.g. radiology, radiation oncology, ophthalmology, dermatology, surgery, orthopedic surgery, neurosurgery, obstetrics and gynecology) where the opportunities for pursuing academic research careers may be less well developed.7 It remains to be seen whether this will affect the percentage of MD-PhD program graduates who remain in academia and biomedical research.
Both the 24-program study by Brass et al7 and the PSW-WG report30 found that about 65% of MSTP graduates who have completed training hold faculty positions at medical schools. Another 10–15% hold positions at NIH or in pharmaceutical/biotechnology companies.7 Thus, up to ∼80% of MSTP graduates may be pursuing careers as physician-scientists or in research related roles. Given that people enter MD-PhD programs in their early 20s and complete the entire training process in their mid- to late-30s, it is notable that four-fifths remain committed to pursuing careers as physician-scientists. Hopefully, the highly competitive prospects for obtaining grant support and the changing medical practice environment will not have too negative an impact on the current generation of trainees. This is critically important because, as noted by the PSW-WG, the NIH grant supported physician-scientist workforce has been progressively aging for several decades, but there are limits to how long the older physician-scientist can (and should) contribute to the physician-scientist workforce. An effective physician-scientist training pipeline will be important to prevent a shortage of physician-scientist researchers in the future. Therefore, continued efforts are needed to improve MD-PhD training and to address issues that arise at later stages of physician-scientist training, including the need to improve the availability of effective research-intensive residencies and fellowships in multiple fields, shorten the time to scientific independence, and increase the diversity of the physician-scientist workforce.31
Supplementary Material
Acknowledgments
The data reported here were requested through the efforts of Peter C. Preusch, program director, Medical Scientist Training Program (MSTP), National Institute of General Medical Sciences (NIGMS), who gave a preliminary account of the results at the NIGMS sponsored 50th Anniversary MSTP Symposium. He also provided valuable contributions at every stage of the development of this manuscript. Data on trainee appointments and outcomes were retrieved and analyzed by the Division of Statistical Analysis and Reporting (DSAR), Office of Planning, Analysis and Communications (OPAC), Office of Extramural Research (OER), National Institutes of Health (NIH). Thanks go to Lindsey Scott, Deepshikha RoyChowdhury, Cassandra Spears, Robert Moore, Carol Bleakley, Jennifer Sutton, Katrina Pearson, and Robin Wagner. Data on MSTP awards and slot numbers were compiled by Andrew Miklos and Paula Powell, NIGMS. The authors are grateful to Irena Tartakovsky and Hershel Alexander at the Association of American Medical Colleges (AAMC) for providing data, and recognize the work of the AAMC MD-PhD Section in developing data on MD-PhD training and outcomes. The authors thank the many colleagues who provided information and helpful comments, including Robin Lorenz, Linda Burnley, Michael Shelansky, and James Jamieson.
Funding/Support: None reported.
Other disclosures: Drs. Harding, Akabas, and Andersen are the directors of Medical Scientist Training Programs funded by NIH T32 training grants to Case Western Reserve University (T32 GM007250), Albert Einstein College of Medicine (T32 GM 007288) and Weill Cornell Medical College (T32 GM 007739). These grants provided no support for this publication. Drs. Harding, Akabas, and Andersen have additional National Institutes of Health research grants that are not related to this publication.
Footnotes
Ethical approval: Reported as not applicable.
Previous presentations: Preliminary versions of some portions of the materials in this article were presented by Drs. Clifford V. Harding and Peter C. Preusch at a meeting on July 17, 2014, National Institutes of Health, Bethesda, MD, to recognize the 50th anniversary of the MSTP.
Supplemental digital content for this article is available at [LWW INSERT LINK].
Contributor Information
Clifford V. Harding, Medical Scientist Training Program, Case Western Reserve University and University Hospitals Cleveland Medical Center, Cleveland, Ohio.
Myles H. Akabas, Medical Scientist Training Program, Albert Einstein College of Medicine, Bronx, New York.
Olaf S. Andersen, Weill Cornell Medical College, and director, Weill Cornell/Rockefeller/Sloan Kettering Tri-institutional MD-PhD Program, New York, New York.
References
- 1.Flexner A. Medical Education in the United States: A Report to the Carnegie Foundation for the Advancement of Teaching. New York, NY: Carnegie Foundation for the Advancement of Teaching; 1910. [Google Scholar]
- 2.Bush V. Science—The Endless Frontier: A Report to the President. Washington, DC: National Science Foundation; [Accessed March 25, 2017]. https://http://www.nsf.gov/od/lpa/nsf50/vbush1945.htm. [Google Scholar]
- 3.Price V. Letter from Vincent Price, reprinted (original 1979) In: Burnley L, editor. Harvard Medical School MD-PhD Program. Boston, MA: Harvard Medical School; 2004. [Google Scholar]
- 4.Williams G. Western Reserve's Experiment in Medical Education and Its Outcome. New York, NY: Oxford University Press; 1980. [Google Scholar]
- 5.National Institutes of Health. [Accessed March 25, 2017];Medical Scientist Training Program (MSTP) Institutions. 2016 https://www.nigms.nih.gov/Training/InstPredoc/Pages/PredocInst-MSTP.aspx.
- 6.Association of American Medical Colleges. [Accessed March 25, 2017];List of MD-PhD programs. 2016 https://students-residents.aamc.org/applying-medical-school/article/mdphd-degree-programs-state/
- 7.Brass LF, Akabas MH, Burnley LD, Engman DM, Wiley CA, Andersen OS. Are MD-PhD programs meeting their goals? An analysis of career choices made by graduates of 24 MD-PhD programs. Acad Med. 2010;85:692–701. doi: 10.1097/ACM.0b013e3181d3ca17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Glowinski I, Julian C, Onken J, Zimmerman C, Pion G. The Careers and Professional Activities of Graduates of the NIGMS Medical Scientist Training Program. Bethesda, MD: National Institute of General Medical Sciences and Vanderbilt University Institute for Public Policy; 1998. [Google Scholar]
- 9.Paik JC, Howard G, Lorenz RG. Postgraduate choices of graduates from medical scientist training programs, 2004–2008. JAMA. 2009;302:1271–1273. doi: 10.1001/jama.2009.1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garrison HH, Deschamps AM. NIH research funding and early career physician scientists: Continuing challenges in the 21st century. FASEB J. 2014;28:1049–1058. doi: 10.1096/fj.13-241687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Andriole DA, Jeffe DB. Predictors of full-time faculty appointment among MD-PhD program graduates: A national cohort study. Med Educ Online. 2016;21:30941. doi: 10.3402/meo.v21.30941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andriole DA, Whelan AJ, Jeffe DB. Characteristics and career intentions of the emerging MD/PhD workforce. JAMA. 2008;300:1165–1173. doi: 10.1001/jama.300.10.1165. [DOI] [PubMed] [Google Scholar]
- 13.Jeffe DB, Andriole DA. A national cohort study of MD-PhD graduates of medical schools with and without funding from the National Institute of General Medical Sciences' Medical Scientist Training Program. Acad Med. 2011;86:953–961. doi: 10.1097/ACM.0b013e31822225c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jeffe DB, Andriole DA, Wathington HD, Tai RH. The emerging physician-scientist workforce: Demographic, experiential, and attitudinal predictors of MD-PhD program enrollment. Acad Med. 2014;89:1398–1407. doi: 10.1097/ACM.0000000000000400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jeffe DB, Andriole DA, Wathington HD, Tai RH. Educational outcomes for students enrolled in MD-PhD programs at medical school matriculation, 1995-2000: a national cohort study. Acad Med. 2014;89(1):84–93. doi: 10.1097/ACM.0000000000000071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Andersen OS, O'Banion MK. Medical Scientist Training Programs: Federal funding offers support and drives innovation. Acad Med. 2010;85:1559. doi: 10.1097/ACM.0b013e3181f1195d. [DOI] [PubMed] [Google Scholar]
- 17.National Science Foundation. [Accessed March 25, 2017];Survey of Earned Doctorates. www.nsf.gov/statistics/srvydoctorates/
- 18.Association of American Medical Colleges. [Accessed March 25, 2017];Faculty Roster Survey. www.aamc.org/data/facultyroster/
- 19.Association of American Medical Colleges. [Accessed March 25, 2017];US medical school applicants and students 1982–1983 to 2011–2012. 2016 http://www.aamc.org/download/153708/data/charts1982to2012.pdf.
- 20.Association of American Medical Colleges. FACTS: Applicants, Matriculants, Enrollment, Graduates, M.D.-Ph.D., and Residency Applicants Data. [Accessed March 25, 2017];2016 http://www.aamc.org/data/facts/ [Note: The Association of American Medical Colleges' data tables are updated annually. Previous years' tables are available by request from the authors.]
- 21.Association of American Medical Colleges. [Accessed March 25, 2017];Table A-1 US Medical School Applications and Matriculants by School, State of Legal Residence, and Sex, 2016–2017. 2016 http://www.aamc.org/download/321442/data/factstablea1.pdf.
- 22.National Institutes of Health. Research Portfolio Online Reporting Tools. Funding Facts. [Accessed March 25, 2017];System report for career development awards. 2016 http://report.nih.gov/fundingfacts/fundingfacts.aspx.
- 23.National Institutes of Health. National Institutes of Health Historical Budget Requests. [Accessed March 25, 2017];2016 https://officeofbudget.od.nih.gov/history_budget_req.html.
- 24.Association of American Medical Colleges. Table A-8: Applicants to U.S. Medical Schools by Selected Combinations of Race/Ethnicity and Sex, 2013–2014 through 2016–2017. [Accessed March 25, 2017];2016 http://www.aamc.org/download/321472/data/factstablea8.pdf.
- 25.Association of American Medical Colleges. Table B-8: U.S. Medical School Applications and Matriculations by School, In-State Status, and Sex, 2016–2017. [Accessed March 25, 2017];2016 http://www.aamc.org/download/321544/data/factstableb8.pdf.
- 26.Association of American Medical Colleges. Table A-10: Applicants to U.S. Medical Schools by Race/Ethnicity and State of Legal Residence, 2016–2017. [Accessed March 25, 2017];2016 http://www.aamc.org/download/321476/data/factstablea10.pdf.
- 27.Association of American Medical Colleges. Table B-7: M.D.–Ph.D. Applicants to U.S. Medical Schools by Race/Ethnicity and State of Legal Residence, 2016–2017. [Accessed March 25, 2017];2016 http://www.aamc.org/download/321542/data/factstableb7.pdf.
- 28.Gotian R, Raymore JC, Rhooms SK, Liberman L, Anderson OS. Gateways to the laboratory: How an MD-PhD program increased the number of minority physician-scientists. Acad Med. 2016 doi: 10.1097/ACM.0000000000001478. Published ahead of print. [DOI] [PubMed] [Google Scholar]
- 29.Johnson JA, Congressional Research Service Brief history of NIH funding: Fact sheet. [Accessed March 25, 2017];2013 https://http://www.fas.org/sgp/crs/misc/R43341.pdf.
- 30.National Institutes of Health. Physician-Scientist Workforce (PSW) Working Group Report. [Accessed March 25, 2017];NIH website. http://acd.od.nih.gov/reports/PSW_Report_ACD_06042014.pdf Updated June 1, 2014.
- 31.Milewicz DM, Lorenz RG, Dermody TS, Brass LF. Rescuing the physician-scientist workforce: The time for action is now. J Clin Invest. 2015;125:3742–3747. doi: 10.1172/JCI84170. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.