Abstract
Background
Percutaneous epiphysiodesis using transphyseal screws (PETS) has been associated with implant failure, implant prominence, angular deformities, and delayed growth inhibition.
Questions/Purposes
The aim of this study was to assess the complication rate and efficacy (defined as actual growth inhibition divided by expected growth inhibition) of PETS and to identify factors associated with improved efficacy.
Methods
Patients who underwent distal femoral and/or proximal tibial PETS between January 2007 and June 2014 were identified. Complications, efficacy, and final limb-length discrepancy (LLD) were calculated using multipliers and inhibition rates based on previous growth. Associations between efficacy and screw insertion angle (SIA), body mass index, and number of threads crossing the physis were calculated.
Results
Eight-two patients (126 treated physes) were included. The mean pre-operative LLD was 27.7 mm (SD = 7.5). Following epiphysiodesis, 15 had temporary pain (18%), five had temporary effusion (6.1%), four had broken implants (4.9%), four developed mild angulation (4.9%), and three had failed epiphysiodesis requiring revision (3.7%). Thirty-one underwent screw removal (n = 31, 38%). Mean LLD at maturity was 17.3 mm (SD = 5.8 mm). Mean efficacy at the distal femur was 97% (SD = 46%), at the proximal tibia was 108% (SD = 66%) and was 103% (SD = 57%) overall. Increased screw threads across the lateral proximal tibial physis (Spearman’s correlation coefficient = 0.67; 95% CI = 0.40–0.94) and higher BMI (Spearman’s correlation coefficient = 0.55; 95% CI = 0.34–0.77) were positively associated with increased efficacy.
Conclusions
The efficacy of PETS may be more favorable than previously reported. Only 3.7% had serious complications requiring revision epiphysiodesis, lower than previous reports. Attention to sufficient screw threads across the physis may be important in optimizing PETS results.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-017-9549-5) contains supplementary material, which is available to authorized users.
Keywords: efficacy, complications, percutaneous screws, epiphysiodesis, limb length discrepancy, PETS
Introduction
Limb length discrepancy (LLD) is a common cause for referral to pediatric orthopedic surgeons. Etiologies may be congenital such as hemihypertrophy, fibular, tibial or femoral deficiencies, or developmental such as growth arrest secondary to trauma or infection [9]. Small differences in limb length often go unnoticed and are generally well-tolerated but beyond the threshold of 2 cm, discrepancies begin to alter gait and muscle physiology and may be associated with pelvic obliquity, structural and non-structural scoliosis, hip or knee pain, and knee arthritis [10, 12, 22, 25]. Predicted LLDs at maturity of less than 2 cm are not treated, while LLDs between 2 and 5 cm are typically treated with epiphysiodesis [7]. Epiphysiodesis ablates or tethers the growth plate of the long limb in skeletally immature patients with the goal of achieving an overall LLD of less than 2 cm at skeletal maturity [2, 5, 19].
Percutaneous epiphysiodesis using transphyseal screws (PETS) is a minimally invasive technique with minimal post-operative activity restrictions [14, 16, 18]. PETS for epiphysiodesis has increased since its introduction in 1998 [16]. Efficacy (actual growth inhibition divided by expected growth inhibition) has been reported at 66–79% [14, 23]. Some authors recommend treatment 6 months to 1 year before predicted optimal surgical timing to account for a hypothesized delay in growth arrest seen with this technique [14, 23]. Complications including recurvatum, valgus deformities, and need for revision surgery are not uncommon, occurring in 18% of patients in one series [14, 15]. The rate of screw removal is variable but has been reported as high as 60% [14]. Due to the development of tibial valgus angular deformity, some authors have cautioned against the use of PETS in the proximal tibia [14]. At our tertiary care orthopedic hospital, we have extensive experience with PETS and anecdotally have not found the same lack of efficacy or negative sequelae that have been reported in recent literature.
We hypothesize that within our patient population, complication rates are lower than previous reports, and the efficacy of PETS is similar to previous reports on efficacy of drill and curettage epiphysiodesis. A previous report [23] showed that a more vertical screw insertion angle was associated with improved efficacy of epiphysiodesis. Although not previously evaluated in the context of screw epiphysiodesis for LLD, the number of screw threads across the physis was found to be important in successful treatment of SCFE, screw epiphysiodesis of the proximal femoral physis [26]. Body mass index (BMI) has been hypothesized as a factor in hemi-epiphysiodesis failure [13], but has not been evaluated as a factor related to efficacy of epiphysiodesis. Based on these previous studies, we elected to evaluate these factors in the efficacy of epiphysiodesis.
The primary aim was to assess the efficacy (actual growth inhibition divided by expected growth inhibition) of PETS by calculating the expected growth inhibition and measuring pre- and post-operative LLD, providing actual growth inhibition. The second aim was to determine the proportion of patients having any form of complication or sequelae and to report the types and frequencies of these complications. The final aim was to determine through regression analysis, if efficacy was associated with screw insertion angle, the number of screw threads crossing the physis, or BMI.
Patients and Methods
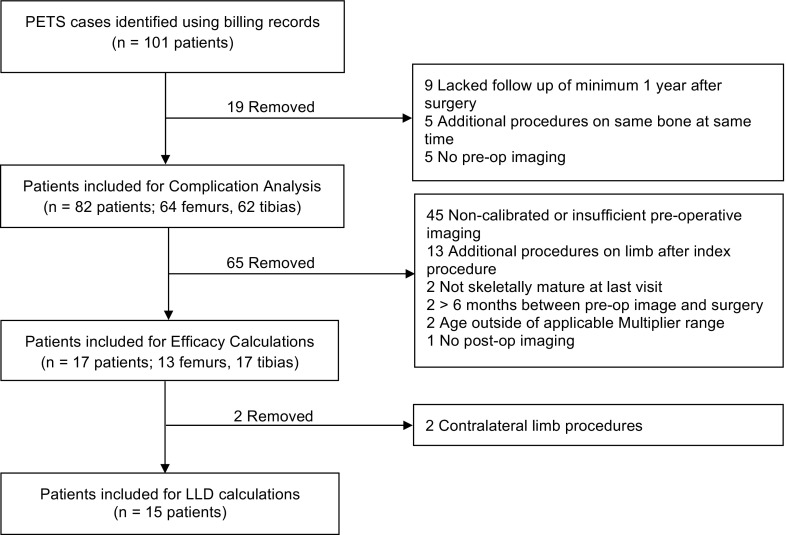
Institutional review board (IRB) approval was obtained and a search of Current Procedural Terminology Version 4 (CPT-4) billing codes was conducted to identify a consecutive series of patients who underwent distal femoral and/or proximal tibial PETS between the January 2007 and June 2014 inclusive, such that all patients would have minimum 1 year follow-up. The CPT codes used to identify patients were as follows: 27475 (arrest, epiphyseal, any method, distal femur), 27477 (arrest, epiphyseal, any method, tibia and fibula, proximal), 27479 (arrest, epiphyseal, any method, combined distal femur, proximal tibia and fibula), 27740 (arrest, epiphyseal, any method, combined, proximal and distal tibia and fibula), and 27742 (arrest, epiphyseal, any method, combined, proximal and distal tibia and fibula, and distal femur). Patients were excluded if they were lost to follow-up prior to 1 year follow-up, if they underwent concomitant ipsilateral lower extremity procedures at the time of PETS, or if pre-operative imaging was performed at an outside hospital and not available for review (Fig. 1). The surgical technique used for PETS has been previously described [16]. Stainless steel, fully threaded, cannulated, 6.5- or 7.3-mm screws were used in all cases.
Fig. 1.
Flow chart displaying excluded and included patients for each part of the analysis.
Demographic and clinical information was collected from radiographic images stored on our institution’s electronic Picture Archiving and Communications System (PACS) and electronic and paper medical records. Collected data included chronological age at the time of surgery, bone age at the time of surgery, sex, BMI, underlying diagnosis, and additional procedures performed on the ipsilateral or contralateral leg before or after PETS. Radiographic parameters were measured pre-operatively and at skeletal maturity and at every subsequent visit that imaging was obtained. Efficacy and final LLD were calculated from measurements taken pre-operatively and at skeletal maturity. Tibial length, femoral length, total leg length, mechanical lateral distal femoral angle (mLDFA), and mechanical medial proximal tibial angle (MPTA) were measured on imaging from pre-operative and post-operative visits. Measurements were made in duplicate (E.L., E.D.). Efficacy and final LLD were calculated using standard equations (Table 1), based on imaging from the pre-operative visit(s) and from imaging at skeletal maturity. Complications associated with PETS were recorded including broken implants, the need for revision surgery, and the development of an angular deformity in the coronal plane ≥5° relative to pre-operative distal femoral (mLDFA) or proximal tibial (MPTA) angles. Sequelae such as post-operative pain at the knee or surgical site and knee effusion were also recorded. The rate of screw removal was noted. Etiologies for limb length discrepancy were classified as congenital or developmental (acquired such as post-traumatic, infectious, iatrogenic, or unknown).
Table 1.
Equations for determining/calculating future growth, growth inhibition, and final limb length discrepancy based on either congenital or developmental/unknown etiologies
| Equation for congenital discrepancies | Equations for developmental/unknown discrepancies |
|---|---|
| Δm = Δ x M | Δm = Δ + i x G |
| Δm = predicted discrepancy at maturity | Δm = predicted discrepancy at maturity |
| Δ = discrepancy at a certain age (i.e. at pre-operative appointment) | Δ = discrepancy at a certain age (i.e. at pre-operative appointment) |
| M = age-specific multiplier [20] | i = growth inhibition = 1 - [(B s-B’s)/(B L-B’L)] |
| B s = short bone at time point 2 | |
| B’s = short bone at time point 1 | |
| B L = long bone at time point 2 | |
| B’L = long bone at time point 1 | |
| G = growth remaining = L(M-1) | |
| L = length of bone at specific age | |
| M = age-specific multiplier [20] |
Although complications could be assessed regardless of image calibration, the calculation of efficacy required high-quality, calibrated images so that measurements made at different time points could be accurately compared. At our institution, imaging for patients with LLD has changed over time. Plain X-ray or CT scanogram were used initially while EOS low-dose biplanar X-ray has been the standard for the last 5 years. Patients were excluded from efficacy calculations if image calibration was inadequate. Specifically, if a patient’s imaging was not obtained by a consistent modality, e.g., some studies performed with plain X-ray, and others with CT scanogram or EOS, these were excluded from efficacy calculations as magnification differences inherent with these techniques made it impossible to accurately track changes in growth over time. Some patients had pre- or post-operative imaging performed at an outside institution where images were not archived in PACS and thus not available for analysis. Patients with developmental growth disturbance require two sets of pre-operative images in order to determine their unique rate of growth inhibition, typically 6 months apart. Patients with developmental growth disturbance who did not have two sets of calibrated pre-operative imaging were also excluded. Exclusion numbers and reasons for exclusion from the efficacy calculation are reported (Fig. 1). Left hand radiographs were routinely obtained for each patient pre-operatively and skeletal age was determined based on the method described by Greulich and Pyle [11].
Expected future growth can be calculated using chronologic or bone age. As the original Paley multiplier technique was developed with chronologic age [20], and multiple previous studies on epiphysiodesis have performed calculations using chronologic age [17, 20], we selected chronologic age for this study primarily for ease of comparison to previous work. Expected bone segment length at maturity was calculated in two ways depending on the etiology of the deformity. Etiology was assessed by careful review of medical records. For patients with congenital deformities, in which the length discrepancy is proportional throughout growth, predicted LLD was calculated using the multiplier method (Table 1) and the original multiplier tables developed by Paley et al. [20]. For those with developmental etiologies, in which the length discrepancy may not remain proportional throughout growth, a different set of equations was used that required the measurement of bone segment lengths at two pre-operative time points in order to establish the unique rate of growth inhibition for each individual (Table 1). In two developmental cases, the LLD was greater than 2 cm pre-operatively but was static over time. The rate of inhibition (i) was assigned a value of zero.
Actual growth was determined using calibrated imaging from pre-operative appointments and at the time of skeletal maturity. Efficacy was calculated using the following equation where g is 0.71 for the distal femur and 0.57 for the proximal tibia [14, 20].
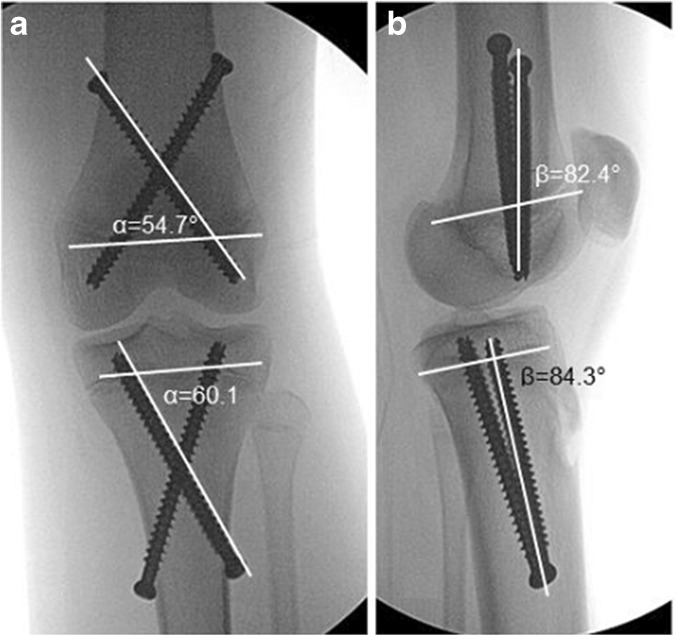
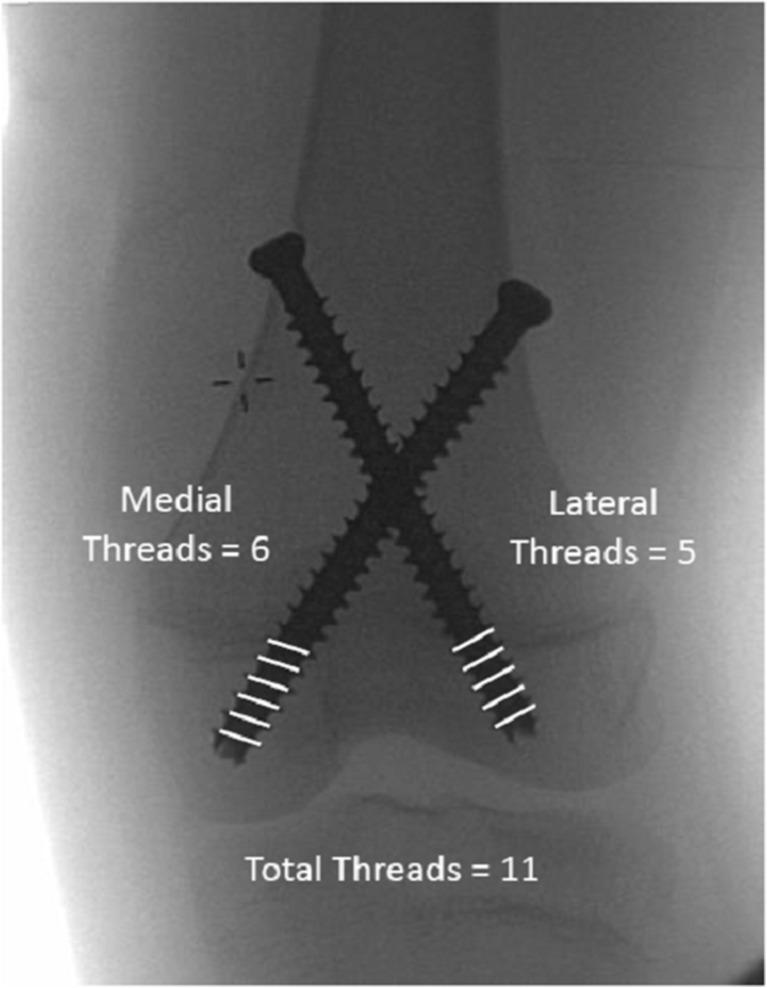
Anteroposterior view (α) and lateral view (β) screw insertion angles were measured on intraoperative fluoroscopic images to calculate an overall screw insertion angle (δ) as described by Song et al. (Fig. 2) [23]. For both the medial and lateral screws, the number of screw threads crossing the physis was counted. The total number of screw threads was calculated by adding the number of medial and lateral screw threads across the physis (Fig. 3). A non-parametric Spearman’s correlation coefficient was calculated in order to evaluate whether overall screw insertion angles (δ) of the screws crossing the lateral tibial and femoral physes, the overall insertion angles (δ) of the screws crossing the medial tibial and femoral physes, the BMI, and the thread number crossing the medial and lateral femoral and tibial physes were associated with efficacy for each bone segment.
Fig. 2.
Screw insertion angles for measurement α on the anterior-posterior view and β on the lateral view.
Fig. 3.
Technique for measurement of screw threads across the physis.
The final LLD was measured only for the subset of patients who had available calibrated images and follow-up to skeletal maturity and did not have procedures other than epiphysiodesis on the operative limb or a lengthening or other procedure on the contralateral limb (Fig. 1). LLD at maturity was reported as both a distance and as a percentage of the longer limb. Limb length correction and final LLD were measured based on calibrated hip to ankle imaging obtained pre-operatively and at the time of skeletal maturity.
Statistical analysis consisted of Spearman rank correlation coefficients as well as descriptive statistics including means with standard deviations. The level of significance was set at 0.05. All analyses were performed using Statistical Analysis Software 9.3 (SAS®, Cary, NC, USA).
Results
Eighty-two patients were included in this analysis. Sixty-four patients underwent distal femoral epiphysiodesis (21 in isolation, 43 as part of combined procedure) and 61 patients underwent proximal tibial epiphysiodesis (18 in isolation, 43 as part of combined procedure). The mean chronological age of females at the time of surgery was 12.0 years while the mean bone age was 13.2 years (Table 2). The mean chronological age of males was 13.8 years and the mean bone age was 13.9 years. The mean efficacy for the distal femur was 97% (SD = 46%), for the proximal tibia was 108% (SD = 66%), and was 103% (SD = 57%) overall (Table 3). The measurements used to calculate efficacy were pre-operative LLD, predicted LLD without treatment, and actual post-operative LLD at maturity. The mean pre-operative LLD was 27.7 mm (range 18.0–41.0 mm, SD = 7.5 mm), and the mean predicted LLD at maturity without treatment was 31.6 mm (SD = 8.8 mm). The mean LLD at skeletal maturity was 17.3 mm (SD = 5.8 mm) for a total of 14.3 mm of “prevented” LLD. The mean final LLD showed the shorter limb to be 2.1% (SD = 0.7%) shorter than the longer limb.
Table 2.
Patient demographics and etiologies
| Category | Metric |
|---|---|
| Total patients | 82 |
| Female (%) | 31 (38%) |
| Left-sided epiphysiodesis (%) | 33 (40%) |
| Mean female chronological age at time of surgery | 12.0 (SD = 1.4) |
| Mean female bone age at time of surgery | 13.2 (SD = 1.5) |
| Mean male chronological age at time of surgery | 13.8 (SD = 1.5) |
| Mean male bone age at time of surgery | 13.9 (SD = 1.3) |
| Etiology of discrepancy | |
| Congenital (%) | 38 (46%) |
| Developmental or unknown (%) | 44 (54%) |
Table 4.
Complications, sequelae, and screw removal
| Number (%) | |
|---|---|
| Expected sequelae | |
| Temporary knee pain | 15 (18%) |
| Temporary knee effusion | 5 (6.1%) |
| Complications | |
| Broken implant | 4 (4.9%) |
| Angulation change ≥5° | 4 (4.9%) |
| Revision epiphysiodesis | 3 (3.7%) |
| Total screw removal | 31 (38%) |
| Asymptomatic screw removal | 22 (27%) |
| Symptomatic screw removal | 9 (11%) |
Complications including broken implants, angulation change, and revision epiphysiodesis were observed in 4 (4.9%), 4 (4.9%), and 3 (3.7%) patients, respectively. Breakage of implants occurred at 2–3 years post-implantation. Only three patients (3.7%) experienced a failure of epiphysiodesis and required revision epiphysiodesis. Revision epiphysiodesis was performed at 3 years for two of the patients and at 1 year for the third. Short-term sequelae such as temporary effusion and knee pain occurred in 15 patients (18%) and five patients (6.1%), respectively. Typically, short-term sequelae resolved within a month of surgery. Of the 31 patients who underwent removal of implants, 22 (71%) were removed electively, in the absence of symptoms or complications (Table 4).
Table 3.
Mean efficacy for epiphysiodesis of the distal femur, proximal tibia, and overall as calculated using the patient’s bone age versus chronological age and two variations of the multiplier tables [20]
| Location | Mean efficacy (%) | Standard deviation | |
|---|---|---|---|
| Calculations based on bone age and year + month multipliers [21] | Distal femur | 102 | 22 |
| Proximal tibia | 119 | 52 | |
| Overall | 112 | 42 | |
| Calculations based on chronological age and year + month multipliers [21] | Distal femur | 109 | 27 |
| Proximal tibia | 110 | 78 | |
| Overall | 110 | 62 | |
| Calculations based on chronological age and yearly multiplier [20] | Distal femur | 97 | 46 |
| Proximal tibia | 108 | 66 | |
| Overall | 103 | 57 |
The independent effect of variables including screw insertion angle, number of screw threads crossing the physis, and BMI on overall efficacy was evaluated. The mean screw insertion angles of the screws crossing the medial physes, the lateral physes, and combined physes are reported (Table 5). The means and standard deviations for the number of screw threads crossing each physis are reported (Table 6). Increased number of screw threads across the lateral physis of the proximal tibia (Spearman’s correlation coefficient = 0.67; 95% CI = 0.40–0.94) and higher BMI (Spearman’s correlation coefficient = 0.55; 95% CI = 0.34–0.77) were positively associated with increased efficacy. The number of screw threads across the medial tibial physis, across either the lateral or medial femoral physis, and screw insertion angles were not associated with efficacy (Table 7).
Table 5.
Mean screw insertion angles
| Screw insertion angle | Femur (n = 12) Mean (SD) |
Tibia (n = 17) Mean (SD) |
|---|---|---|
| Medial screw (crosses the lateral physis) | ||
| Anteroposterior angle (α) | 50.0 (4.4) | 49.4 (6.3) |
| Lateral angle (β) | 94.7 (14.3) | 95.2 (12.8) |
| Calculated screw insertion angle (Δ) | 48.7 (5.0) | 48.5 (6.5) |
| Lateral screw (crosses the medial physis) | ||
| Anteroposterior angle (α) | 48.8 (4.5) | 51.9 (4.3) |
| Lateral angle (β) | 97.1 (7.7) | 99.3 (9.3) |
| Calculated screw insertion angle (Δ) | 48.2 (4.3) | 50.8 (4.3) |
| Mean screw insertion angle | 48.4 (3.9) | 49.6 (4.2) |
Table 6.
Mean screw threads across the physis
| Screw thread number | Femur (n = 12) Mean (SD) |
Tibia (n = 17) Mean (SD) |
|---|---|---|
| Medial physis thread number | 6.5 (1.6) | 3.9 (0.8) |
| Lateral physis thread number | 7.5 (1.1) | 3.6 (0.6) |
| Total thread number (medial + lateral) | 14.0 (1.4) | 7.5 (1.1) |
Table 7.
The association between variables of interest and efficacy
| Procedure site | Overall | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Distal femur | Proximal tibia | ||||||||
| Correlation coefficient | 95% confidence interval | Correlation coefficient | 95% confidence interval | Correlation coefficient | 95% confidence interval | ||||
| Lower CI | Upper CI | Lower CI | Upper CI | Lower CI | Upper CI | ||||
| BMI * efficacy | 0.54 | 0.16 | 0.91 | 0.61 | 0.30 | 0.92 | 0.55 | 0.34 | 0.77 |
| Medial SIA * efficacy | 0.04 | −0.56 | 0.64 | 0.32 | −0.22 | 0.85 | 0.28 | −0.09 | 0.65 |
| Lateral SIA * efficacy | 0.05 | −0.57 | 0.66 | 0.17 | −0.36 | 0.70 | 0.23 | −0.14 | 0.61 |
| # medial screw threads * efficacy | −0.12 | −0.75 | 0.51 | 0.26 | −0.31 | 0.82 | −0.02 | −0.36 | 0.32 |
| # lateral screw threads * efficacy | −0.03 | −0.64 | 0.57 | 0.67 | 0.40 | 0.94 | 0.04 | −0.37 | 0.46 |
Italic indicates statistical significance
Discussion
The primary purpose of this study was to evaluate the efficacy and rate of complications associated with PETS at a high-volume tertiary care center. Of the 82 patients (126 physes) included in this analysis, only 3 (3.7%) had failed epiphysiodesis. Post-operative knee pain and effusion were transient, mild, and expected. Mean efficacy was 103%.
Contrary to past reports, we found an efficacy of approximately 100% for both the distal femur and proximal tibia. The higher efficacy seen in our cohort may potentially be due to a difference in screw position, or some other factor. Monier et al. recently reported on variations in predicted and actual growth inhibition with screw epiphysiodesis and found that the Paley method resulted in the most accurate prediction [17]. The efficacy calculation is greatly tied to expected growth. If expected growth is under estimated, efficacy may be under estimated. In this study, we meticulously categorized patients as congenital versus developmental and only applied congenital growth equations to congenital cases, while developmental or unknown causes were treated with the developmental formulas in which two previous sets of images were used to calculate future growth and the rate of inhibition. Past studies have often referred simply to the multiplier method being used to calculate expected LLD and did not specify whether cases were treated based on congenital or developmental etiologies. Efficacy will be higher than calculated if future growth (and therefore inhibition of future growth) is greater than expected. Thus, if our population happened to be “late bloomers” with more growth remaining than typical for their age, they would have greater growth inhibition (a larger numerator), and this could potentially explain our somewhat greater efficacy.
We found that higher BMI was associated with increased efficacy. One can only hypothesize on why this may be the case. Children with elevated BMI typically have advanced bone age [6], meaning that based on chronologic age, they have less growth remaining than expected, and as such should have lower efficacy. One reasonable hypothesis is that in obese patients, the physis is more susceptible to being tethered, as it may already be struggling to grow due to excess compressive forces, the Heuter Volkmann principle [3].
Our patients experienced considerably lower rates of complications than those in previously published studies. Within our cohort, only three (3.7%, 1 distal femur, 2 proximal tibias) patients required revision surgery, and only 4 (4.9%) patients had a lateral distal femoral or medial proximal tibial angle change of 5° or greater following treatment, none of which were deemed severe enough to require treatment. Although data is limited, prior authors have noted revision rates of up to 18% and coronal plane deformities of up to 20% [14, 18]. Some of these issues may have been associated with surgical technique or screw design. The use of large diameter, stainless steel screws with careful attention to the placement of sufficient threads across the physis may have led to the lower rates of angular deformity and failure in this series.
Thirty-one patients (38%) in our cohort underwent screw removal, the majority of which were elective and not due to pain or other symptoms, much lower than other reports that describe screw removal rates of up to 60–82% [14, 23]. The difference in screw removal rates may be related to regional preferences for routine screw removal.
Prior studies on PETS reported variable complication rates and clinical outcomes [1, 9, 14, 15, 18]. The most common complications reported were angular deformity, screw failure with ongoing growth, and the need for revision surgery [1, 14, 15]. In 2012, Ilharreborde et al. reported their experience with 45 patients and showed a mean efficacy of only 66% at skeletal maturity for both the distal femur and the proximal tibia [14]. They also reported an 18% revision rate, with 7 of 8 revisions addressing failure of growth arrest in the proximal tibia and the development of valgus alignment. Song et al. published somewhat more favorable results in 2015 after reviewing 59 patients, demonstrating an efficacy of 76% for the distal femur and 79% for the proximal tibia [23]. Their analysis also described a method of quantifying a three-dimensional screw insertion angle and reported that it correlated significantly with efficacy. Unlike Song et al., we did not find a positive association between efficacy and screw insertion angle.
LLD at maturity (excluding patients with ipsilateral additional procedures or lengthening on the contralateral side) was 17.3 mm. At our center, we have traditionally aimed for a LLD of <2 cm, not zero, in order to avoid overcorrection which would cause the longer limb to become the shorter limb. We aim to preserve height as much as possible. Of the 82 patients included in this study, only four experienced a reversal of their LLD in which the long limb became the shorter following epiphysiodesis.
This study has a number of limitations. First, we acknowledge that while our rates of complications are lower than those previously reported, our cohort of 82 patients was not large enough to make broad safety recommendations. Additionally, although all 82 patients were included in the calculation of complications, a large number of our patients had to be excluded from efficacy and final LLD calculations. As many patients at our center are referred from other institutions, many lacked a full set of calibrated images due to pre-operative imaging performed at outside institutions and not catalogued at our institution. In the beginning of our study period, some patients were examined with uncalibrated plain X-rays, long cassette X-rays, or X-rays on multiple cassettes stitched together. It has been documented that length measurement error on X-rays can be as high as 4.2 cm due to parallax [8]. Even with a calibration ball or ruler, we found that parallax and magnification were unpredictable on plain X-rays and the images were not acceptable for study inclusion. At our institution CT scanogram then became the gold standard for assessing LLD, and in the past 5 years, length measurements have been performed primarily on EOS low-dose biplanar X-ray. Although patients that lacked calibrated imaging could not be included in our assessment of efficacy or LLD, they were included in our assessment of complications. A large proportion of our cohort underwent additional surgical procedures that manipulated length, excluding them from efficacy and final LLD analysis. Second, given that calibrated images were not available at standardized time points post-operatively, we were unable to assess at which post-operative time point PETS resulted in physeal growth arrest, a subject that has been a topic of previous studies [14, 23]. Third, we acknowledge that a minimum follow-up of 1 year cannot capture all potential complications; however, we believe that the majority of complications of interest (failure of epiphysiodesis) would be identified within a year of surgery.
Fourth, error can be generated based on the method used to estimate future growth and growth inhibition. For congenital cases, we used chronologic age and multipliers developed by Paley et al. [20], the same technique used in multiple previous assessments of PETS [14, 15, 17, 18], while for developmental and unknown cases we used chronologic age, multipliers, and calculated rates of inhibition from two pre-operative sets of images. In a sub-analysis we evaluated the effect of using bone age and more detailed multipliers specific to the year plus months of age [21] and found that this resulted in efficacies approximately 10% greater than using chronological age and the original multipliers. This difference highlights the importance and influence of the specific methodology for calculating expected growth, growth inhibition, and efficacy. Due to limitations inherent in growth prediction, the efficacy reported here includes some degree of error. Fifth, we acknowledge that due to undulation of the physis or X-ray projection, the reported number of screw threads across the physis may be a slight under- or overestimation of true threads across the physis.
Sixth, we assumed that for developmental cases, the rate of growth inhibition remained constant over time. In fact, in developmental cases sometimes the rate of growth inhibition actually increases over time (i.e., growth is inhibited at a certain rate, and then growth ceases entirely). If increased growth inhibition occurred over time in some developmental cases, then we may have underestimated the expected LLD, resulting in an underestimation of efficacy.
Finally, although we diligently assessed each case and assigned a congenital cause only when we felt confident of the etiology, it is possible that despite our best efforts, some cases were misclassified. If congenital formulas are applied to developmental cases, there is a risk of underestimating the expected LLD, again resulting in underestimation of efficacy. We carefully assessed each case in order to determine whether the etiology was developmental or congenital so that we could use the etiologically appropriate formula. It is not clear whether all previous studies on epiphysiodesis were similarly diligent in this respect, as typically past publications have simply referred to using the multiplier method and did not specify whether different formulas were used for congenital versus developmental cases. If this is the case, it could explain why efficacy was greater in our series than in previous publications [1, 4, 14, 24].
In conclusion, the results of this study support the high efficacy of PETS and the concept that efficacy may be influenced by both surgical techniques such as the number of screw threads across the physis and physiological parameters such as high BMI. Complications were few, while a good number of patients had expected mild pain and swelling in the weeks following surgery or went on to have screw removal. The efficacy, complication rates and cost of PETS compared to the alternative, drill, and curette technique would best be evaluated using a prospective study design in order to allow for control of both patient selection and to optimize collection of relevant data points. Further prospective studies are needed to determine the optimal timing of PETS and to more accurately define efficacy and complication rates.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
Compliance with Ethical Standards
Conflict of Interest
Emily R. Dodwell, MD, MPH, FRCSC; Matthew R. Garner, MD; Elise Bixby, BA; Eva M. Luderowski, BA; Daniel W. Green, MD; John S. Blanco, MD; and Roger F. Widmann, MD, have declared that they have no conflict of interest.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Funding
This research was funded through the Hospital for Special Surgery Pediatric Council Grant and the HSS Medical Student Summer Research Fellowship Program.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Therapeutic Level IV
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-017-9549-5) contains supplementary material, which is available to authorized users.
References
- 1.Babu LV, Evans O, Sankar A, et al. Epiphysiodesis for limb length discrepancy: a comparison of two methods. Strategies Trauma Limb Reconstr. 2014;9:1–3. doi: 10.1007/s11751-013-0180-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bowen JR, Johnson WJ (1984) Percutaneous epiphysiodesis. Clin Orthop Relat Res 170–3. [PubMed]
- 3.Bylski-Austrow DI, Wall EJ, Rupert MP, Roy DR, Crawford AH Growth plate forces in the adolescent human knee: a radiographic and mechanical study of epiphyseal staples. J Pediatr Orthop 21:817–23. [PubMed]
- 4.Campens C, Mousny M, Docquier P-L. Comparison of three surgical epiphysiodesis techniques for the treatment of lower limb length discrepancy. Acta Orthop Belg. 2010;76:226–32. [PubMed] [Google Scholar]
- 5.ST, Christian CA (1990) Techniques for epiphysiodesis about the knee. Clin Orthop Relat Res 81–5. [PubMed]
- 6.Chaumoitre K, Lamtali S, Baali A, et al. Influence of socioeconomic status and body mass index on bone age. Horm Res pædiatrics. 2010;74:129–35. doi: 10.1159/000313371. [DOI] [PubMed] [Google Scholar]
- 7.Dodwell ER, Widmann RF (2015) Percutaneous distal femoral or proximal tibial epiphysiodesis for leg length discrepancy. Oper. Tech. Pediatr. Orthop.
- 8.Escott BG, Ravi B, Weathermon AC, et al. EOS low-dose radiography: a reliable and accurate upright assessment of lower-limb lengths. J Bone Joint Surg Am. 2013;95:e1831–7. doi: 10.2106/JBJS.L.00989. [DOI] [PubMed] [Google Scholar]
- 9.Ghanem I, Karam JA, Widmann RF. Surgical epiphysiodesis indications and techniques: update. Curr Opin Pediatr. 2011;23:53–9. doi: 10.1097/MOP.0b013e32834231b3. [DOI] [PubMed] [Google Scholar]
- 10.Golightly YM, Allen KD, Renner JB, et al. Relationship of limb length inequality with radiographic knee and hip osteoarthritis. Osteoarthr Cartil. 2007;15:824–9. doi: 10.1016/j.joca.2007.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Greulich W, Pyle S. Radiographic atlas of skeletal development of the hand and wrist. 2. Redwood City, CA: Stanford University Press; 1959. [Google Scholar]
- 12.Gross RH. Leg length discrepancy: how much is too much? Orthopedics. 1978;1:307–10. doi: 10.3928/0147-7447-19780701-08. [DOI] [PubMed] [Google Scholar]
- 13.Heflin JA, Ford S, Stevens P. Guided growth for tibia vara (Blount’s disease) Medicine (Baltimore) 2016;95:e4951. doi: 10.1097/MD.0000000000004951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ilharreborde B, Gaumetou E, Souchet P, et al. Efficacy and late complications of percutaneous epiphysiodesis with transphyseal screws. J Bone Joint Surg Br. 2012;94:270–5. doi: 10.1302/0301-620X.94B2.27470. [DOI] [PubMed] [Google Scholar]
- 15.Khoury JG, Tavares JO, McConnell S, et al. Results of screw epiphysiodesis for the treatment of limb length discrepancy and angular deformity. J Pediatr Orthop. 2007;27:623–8. doi: 10.1097/BPO.0b013e318093f4f4. [DOI] [PubMed] [Google Scholar]
- 16.Métaizeau JP, Wong-Chung J, Bertrand H, et al. Percutaneous epiphysiodesis using transphyseal screws (PETS) J Pediatr Orthop. 1998;18:363–9. [PubMed] [Google Scholar]
- 17.Monier BC, Aronsson DD, Sun M. Percutaneous epiphysiodesis using transphyseal screws for limb-length discrepancies: high variability among growth predictor models. J Child Orthop. 2015;9:403–410. doi: 10.1007/s11832-015-0687-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nouth F, Kuo LA. Percutaneous epiphysiodesis using transphyseal screws (PETS): prospective case study and review. J Pediatr Orthop. 2004;24:721–5. doi: 10.1097/01241398-200411000-00023. [DOI] [PubMed] [Google Scholar]
- 19.Ogilvie JW, King K. Epiphysiodesis: two-year clinical results using a new technique. J Pediatr Orthop. 1990;10:809–11. doi: 10.1097/01241398-199011000-00021. [DOI] [PubMed] [Google Scholar]
- 20.Paley D, Bhave A, Herzenberg JE, et al. Multiplier method for predicting limb-length discrepancy. J Bone Joint Surg Am. 2000;82–A:1432–46. doi: 10.2106/00004623-200010000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Paley D. Principles of Deformity Correction. 1. Berlin, Germany: Spring; 2003. [Google Scholar]
- 22.Song KM, Halliday SE, Little DG. The effect of limb-length discrepancy on gait. J Bone Joint Surg Am. 1997;79:1690–8. doi: 10.2106/00004623-199711000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Song MH, Choi E-S, Park MS, et al. Percutaneous epiphysiodesis using transphyseal screws in the management of leg length discrepancy: optimal operation timing and techniques to avoid complications. J Pediatr Orthop. 2015;35:89–93. doi: 10.1097/BPO.0000000000000214. [DOI] [PubMed] [Google Scholar]
- 24.Song MH, Park MS, Yoo WJ, Chung CY, Choi IH, Cho TJ (2013) Effects and complications of percutaneous epiphysiodesis using transphyseal screws in the management of leg length discrepancy. Int. Fed. Paediatr. Orthop. Soc. Meet. [DOI] [PubMed]
- 25.Stanitski DF Limb-length inequality: assessment and treatment options. J Am Acad Orthop Surg 7:143–53. [DOI] [PubMed]
- 26.Upasani V, Kishan S, Oka R, et al. Biomechanical Analysis of Single Screw Fixation for Slipped Capital Femoral Epiphysis. J Pediatr Orthop. 2006;26:474–478. doi: 10.1097/01.bpo.0000217732.24041.81. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)