Abstract
Background
Different types of external fixators have been used for humeral lengthening with successful outcomes reported in literature. Motorized intramedullary (IM) lengthening nails have been developed as an alternative to external fixators for long bone lengthening in the lower extremity.
Questions/Purposes
This case series reports on using the new technology of IM lengthening nails for humeral lengthening. We assessed the radiological healing and functional outcomes after using the PRECICE IM nail for humeral lengthening.
Methods
This multicenter retrospective study included a total of six humeri in five patients (mean age was 20 years) that underwent lengthening with the magnetic IM PRECICE nail in two centers in the USA. The etiology was humeral growth arrest post-bone cyst (two segments), post-septic growth arrest (two segments), and multiple hereditary exostosis (bilateral segments in one patient). The outcomes measured were the length achieved, distraction index (DI; the length achieved in mm divided by the duration of lengthening in days), consolidation index (CI; number of days from surgery until consolidation divided by the length of the regenerate in cm), complications encountered, and functional outcomes (shoulder and elbow range of motion, the upper extremity functional index (UEFI), and QuickDASH functional scores).
Results
The mean follow-up period was 1.8 years (0.9 to 2.4 years). All segments achieved the goal of lengthening; the mean was 5.1 cm (4.5 to 5.8 cm). Mean DI was 0.7 mm/day (0.5 to 0.8). Mean CI was 36 days/cm (25 to 45 days/cm). No complications were observed. At the last follow-up, all patients maintained their preoperative range of motion (ROM) except one patient had reduced shoulder ROM. QuickDASH score and upper extremity functional index showed postoperative improvement compared to the preoperative scores.
Conclusion
IM lengthening nails can provide successful and safe humeral lengthening. Specifically, the PRECICE nail has accurate control over the lengthening process.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-017-9552-x) contains supplementary material, which is available to authorized users.
Keywords: humerus, intramedullary, lengthening, PRECICE nail
Introduction
Humeral deformity and shortening have both functional and esthetic implications leading to surgical intervention [22]. Different types of external fixators have been used for humeral lengthening and deformity correction and reported in the literature [6, 14, 30]. Successful outcomes after humeral lengthening have been reported using Ilizarov circular frames, monolateral fixators, and the hexapod Taylor Spatial Frame (TSF) [2, 23, 29, 37]. Circular external fixators combined with intramedullary elastic nails have been used for humeral lengthening to decrease the risk of fracture after fixator removal [30, 32]. Intramedullary (IM) lengthening devices have been developed to eliminate the need for external fixators [1, 7, 27, 31, 33]. To our knowledge, there have been only two isolated case reports that describe using fully implantable IM lengthening nails as a method for humeral lengthening [20, 36].
The aim of the current study is to evaluate the radiologic and functional outcomes as assessed by joint range of motion and functional scores (upper extremity functional index (UEFI) and QuickDASH scores), while utilizing the fully implantable magnetic PRECICE IM lengthening system (NuVasive, Irvine, USA) for IM humeral lengthening.
Patients and Methods
This current study includes patients from two specialized centers for limb lengthening and deformity correction in the USA in the period from March 2014 to August 2015. Institutional review board (IRB) approval was obtained to review the entire cohort. Retrospective chart and radiographic review were performed to capture all patients who underwent humeral lengthening with the magnetic PRECICE IM lengthening nail. There was no limitation for the inclusion criteria. A total of five patients (two males and three females) with six humeral segments were included in the final study. One humerus (case #3) was reported in a separate case report [20]. The average age was 20 years (range, 15 to 28 years). The etiology was humeral growth arrest post-bone cyst (two segments), post-septic growth arrest (two segments), and multiple hereditary exostosis (bilateral segments in one patient) (Table 1). All represented off-label uses of the device. Limb Lengthening and Reconstruction Society (LLRS) AIM Index was used to classify deformity severity in the current cohort [24].
Table 1.
Patient demographics
| Patient | Side | Age | Etiology | Rod diameter | Deformity | Length goal | LLRS AIM Index |
|---|---|---|---|---|---|---|---|
| 1 | L | 16 | MHE | 8.5 | – | 4.5 | 2 |
| R | 8.5 | – | 4.5 | 2 | |||
| 2 | R | 19 | Bone cyst/growth arrest | 8.5 | 45° ETT | 5.8 | 3 |
| 3 | R | 15 | Growth arrest | 8.5 | 15° varus, 13° apex anterior | 5 | 7 |
| 4 | L | 28 | Bone cyst growth arrest | 8.5 | 10° varus, 12° apex anterior | 5 | 7 |
| 5 | L | 27 | Septic shoulder growth arrest | 8.5 | – | 5 | 4 |
MHE multiple hereditary exostosis, ETT external tibial torsion
The outcomes measured were the amount of lengthening achieved, distraction index (DI; the length achieved in mm divided by the duration of lengthening in days), consolidation index (CI; number of days from surgery until consolidation divided by the length of the regenerate in cm), and the complications encountered. Consolidation was described as radiographic healing (continuous and not interrupted callus formation at the cortex) of three out of four cortices in both anteroposterior (medial and lateral cortices) and lateral (anterior and posterior cortices) projections. Consolidation was assessed by the senior authors. No intra- or interobserver reliability tests were done. Physician-reported functional outcome (dictated shoulder and elbow range of motion before and at last visit after lengthening) was included in the study. Also, we included the patient-reported functional outcomes before and after surgery: the UEFI [10] and QuickDASH [13] functional scores. UEFI consists of items scored on a 0 to 4 point scale where the minimum total score is 0 and the maximum is 80 points (the lower the score, the greater the disability). The QuickDASH is an alternative tool that is simpler than the original DASH score; however, both of them are valid, reliable, and responsive [5]. QuickDASH has two modules: the disability/symptom section (5 subscales with 11 items, scored 0–100 points; the higher the core, the greater the disability) and the optional high performance Sport/Art or Work section (each scored 0–20 points). We did not include the optional modules as they were not related to our study and were not consistent with our patients’ level of interest. The patients retrospectively answered the questions to report the functional status before and after humeral lengthening.
Anteroposterior (AP) and lateral radiographs were obtained for planning. Radiographic limb length and angle measurements were analyzed using the hospital’s picture archiving and communication system (PACS, efilm, Merge Healthcare Incorporated, Chicago, IL). Since there was no specific PRECICE nail for humerus lengthening at the time, off-label tibial or femoral nails were utilized. Nails (8.5 mm width × different length) were used for all segments. Identification of the osteotomy level was planned carefully to correct any deformity and to ensure that the regenerate would be within the wider and stronger female part of the nail at the end of the lengthening phase and during the consolidation phase. The bone was cut at or just below the deltoid tuberosity to avoid traction of the deltoid muscle [21].
Radial nerve exploration and decompression were indicated only if acute rotational deformity was planned as part of the surgery. Fixator-assisted nailing was utilized in segments that underwent lengthening with acute deformity correction [28].
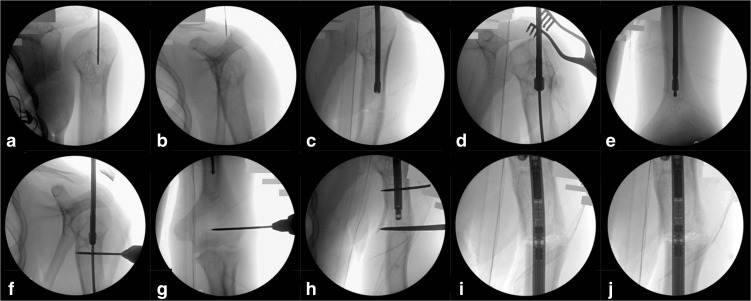
The patient was placed on the radiolucent operating table in supine position with a bump under the ipsilateral scapula. After the administration of regional anesthesia, the involved upper extremity, to include the axilla and base of the neck, was prepped and draped in a sterile fashion. The osteotomy level was identified and marked on the skin. Multiple drill holes were made to vent the IM canal at the osteotomy level through a 1-cm anterolateral incision. Next, the proximal humerus entry point was marked on the skin. A 1.8-mm wire was then percutaneously inserted at the anterolateral border of the acromion to approach the proximal humerus. Usually the starting position was on the medial side of the greater tuberosity to avoid injury to the rotator cuff insertion on the greater tuberosity. This starting position was checked under AP and lateral fluoroscopy. The wire was then driven into the center portion of the proximal humerus, and once this wire’s position was confirmed, a 3-cm incision was made around the guide wire through the skin and subcutaneous tissues. The deltoid muscle and the rotator cuff were carefully spread with a straight hemostat, an 8-mm ACL reamer was placed over the guide wire, and a starting hole was created in the humerus. The humerus was then reamed in a sequential fashion from 6 to 10.5 mm over an IM guide wire. The proximal 3 cm of the humerus was reamed to 12.5 cm as the proximal nail diameter is 10.7 mm. Once the reaming was completed, the guide wire was removed and the appropriate PRECICE nail was then obtained, inserted into the starting hole, and passed to a point just proximal to the previously drilled vent holes. The osteotomy was completed with an osteotome. The nail was advanced across the osteotomy acutely correcting the angular deformity (if present). The overall position and rotational alignment of the humerus were checked by inserting a Steinmann pin above and below the osteotomy prior to cutting the bone, to act as rotational registration markers. Proximal locking screws were inserted using the proximal locking guide. The distal locking screw insertion was performed with the perfect circle technique. If needed, repair of rotator cuff was performed. Wounds were irrigated and closed in layers. To assure proper nail function, intraoperative testing of all nails was performed by doing 1-to-2-mm acute distraction. Finally, the wounds were all sterilely dressed and the patient was placed into a shoulder arm immobilizer (Figs. 1 and 2).
Fig. 1.
a–j Operative steps. a, b Entry point identification by 1.8-mm K-wire. c Predrilled osteotomy site vents the canal, followed by opening the entry point using 8 mm rigid ACL reamer. d, e Reaming over a guide wire all through the IM canal. f, g Two Steinmann pins placed proximally and distally to control the rotation (optional). h Cutting the bone before advancing the PRECICE nail. i, j Before and after nail testing (used with permission from Sinai Hospital of Baltimore, Rubin Institute for Advanced Orthopedics).
Fig. 2.
a–c Intraoperative photos. a Entry point and while reaming the medulla. The 1-cm osteotomy wound is evident.. b Proximal and distal pins to control the rotation. c Position while introducing the IM PRECICE nail (used with permission from Sinai Hospital of Baltimore, Rubin Institute for Advanced Orthopedics).
Antibiotic prophylaxis was administered to all patients in the form of intravenous cefazoline (1 h preoperative and every 6 h for 24 h). In cases of sensitivity, we used intravenous clindamycin (1 h preoperative and every 8 h for 24 h). All patients were instructed to take calcium (1200–1500 mg/day) and vitamin D supplementation (1500–3000 IU/day) starting from the second day post-surgery.
The patients were instructed to start distraction with the external remote controller (ERC) on the seventh postoperative day at the rate of 0.25 mm three times/day. The rate was adjusted according to the regenerate quality observed during postoperative follow-up clinic visits every 2 weeks during the lengthening phase and every month during the consolidation phase. Regenerate bone quality was assessed based on qualitative evaluation of mineralization and the width of the fibrous interzone [3]. The patients were prescribed physical therapy (three to five times per week) to facilitate shoulder and elbow joint motion and to prevent joint contractures. Arm sling was allowed to be used as initially needed for comfort only. Patients were not allowed to weight bear on the arm until consolidation of three out of four cortices was observed radiographically.
Results
Five patients with six segments underwent humeral lengthening with PRECICE femoral or tibial nails. The diameter of all nails was 8.5 mm but different lengths were used for each patient. One segment underwent acute rotational deformity correction (from external to internal) with prophylactic radial nerve exploration and decompression performed during the same surgery. Another two segments underwent acute frontal plane deformity (varus; average 12.5°) and sagittal plane deformity (apex anterior; average 12.5°). For these two segments, osteotomy was performed at the apex level of the deformity. According to LLRS AIM Index, four segments were of minimal complexity, while two segments were moderately complex.
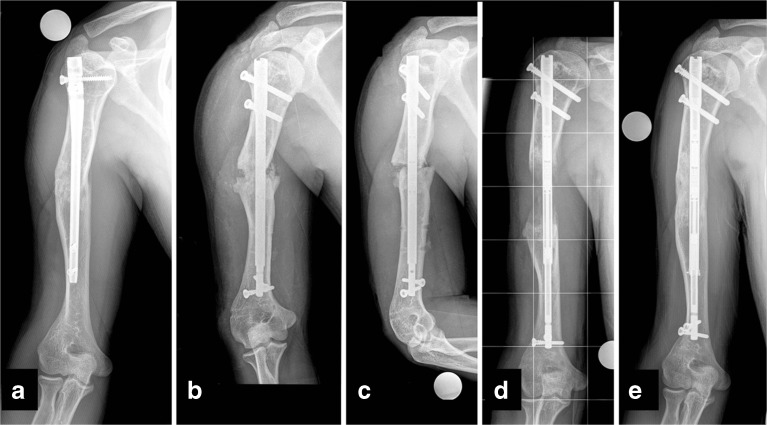
The mean follow-up period for all segments was 1.8 years (range, 0.9 to 2.4 years). All segments achieved the goal length, with a mean of 5.1 cm (range, 4.5 to 5.8 cm). The maximum stroke length allowed is 5 cm for all nails used. Two segments needed 8-mm acute distraction of the osteotomy to fit the nail; for these two, a longer latency period was used and the length achieved was 5.8 cm (Fig. 3). Regenerate distraction was completed in all segments at a mean of 78 days (range, 63 to 113 days), with a mean DI of 0.7 mm/day (range, 0.5 to 0.8 mm/day). All segments achieved full consolidation in a mean of 180 days (range, 144 to 225 days), with a mean CI of 36 days/cm (range, 24.8 to 45 days/cm). Five segments underwent elective nail removal after a mean period of 313 days (range, 273 to 368 days). No complications were observed (Tables 1 and 2).
Fig. 3.
a–e Nineteen year–old male with humeral length discrepancy of 5.8 cm (right is shorter). a Preoperative radiograph with retained IM nail to correct deformity secondary to a previous history of humeral bone cyst. b, c Anteroposterior and lateral views immediately post-removal of the trauma nail and insertion of the IM PRECICE lengthener. c After 5.8 cm lengthening. d Complete healing 9 months after surgery (used with permission from Sinai Hospital of Baltimore, Rubin Institute for Advanced Orthopedics).
Table 2.
Results
| No. | Side | Length achieved (cm) | DI (mm/day) | CI (days/cm) | QuickDASH improvement (points) | UEFI improvement (points) | Elbow forward ROM (pre/post) | Shoulder forward ROM (pre/post) | Complication |
|---|---|---|---|---|---|---|---|---|---|
| 1 | L | 4.5 | 0.6 | 35.6 | 36.3 | 40 | 120/120 | 190/120 | None |
| R | 4.5 | 0.6 | 35.6 | 56.8 | 42 | 120/140 | 190/140 | None | |
| 2 | R | 5.8 | 0.5 | 35.7 | 6.8 | 9 | 120/125 | 170/170 | None |
| 3 | R | 5.0 | 0.8 | 45.0 | 6.8 | 4 | 130/130 | 230/220 | None |
| 4 | L | 5.0 | 0.7 | 37.2 | 4.5 | -3 | 120/125 | 200/220 | None |
| 5 | L | 5.8 | 0.7 | 24.8 | 25 | 16 | 130/130 | 120/120 | None |
| Mean values (range) | 5.1 (4.5–5.8) | 0.7 (0.5–0.8) | 36 (24.8–45) | 22.7 (4.5–56.8) | 18 (−3 to 42) | – | – | – | |
DI distraction index, CI consolidation index, UEFI upper extremity function index
Preoperative mean arc of elbow motion was from −2.5° (range, 0° to −10°) extension to 125° (range, 120° to 130°) flexion. Mean shoulder abduction was 79° (range, 30° to 120°). Mean arc of shoulder motion was from 145° (range, 90° to 170°) flexion to 38° (range, 30° to 60°) extension. Mean arc of shoulder rotation was from 93° (range, 45° to 120°) internal rotation to 89° (range, 70° to 135°) external rotation.
Postoperatively, mean arc of elbow motion was from −1° (range, 0° to −5°) extension to 127° (range, 120° to 130°) flexion. Mean shoulder abduction was 83° (range, 40° to 100°). Mean arc of shoulder motion was from 120° (range, 80° to 160°) flexion to 45° (range, 30° to 60°) extension. Mean arc of shoulder rotation was from 100° (range, 90° to 120°) internal rotation to 82° (range, 70° to 90°) external rotation. Essentially, all patients at the last follow-up visit maintained their preoperative shoulder and elbow ROM. Only one patient (with complex regional pain syndrome) had significant reduction of postoperative shoulder flexion/extension ROM, compared with the preoperative status.
The QuickDASH score showed significant clinical improvement in patients’ function from a preoperative mean of 35 points (range, 9 to 64 points) to a postoperative mean of 12 points (range, 2 to 27 points). Although, the UEFI showed little improvement from a preoperative mean of 53 points (range, 29 to 75 points) to a postoperative mean of 71 points (range, 55 to 78 points).
Discussion
Upper limb lengthening surgery is much less commonly reported compared to lower limb lengthening [4]. This is partially due to the fact that upper limb discrepancies are more functionally tolerated [23, 26]. Humeral lengthening is recommended for patients with significant shortening affecting personal hygiene, daily life activity, or for cosmetic and psychological reasons [12, 18, 29]. We reported in this study our preliminary results of humeral lengthening using the magnetic IM PRECICE nail.
There are several limitations in the current study. First, it is a retrospective study presenting only six segments with humeral shortening. Second, being a multicenter study may be considered a limitation. However, that patients underwent the same plans for treatment and follow-up at both institutions. The follow-up period is relatively short. However, it was sufficient to assess healing and short-term physical and functional outcomes after using the IM lengthening nail in humeral lengthening. Finally, the study did not include intra- or interobserver reliability tests for assessing the healing of the regenerate, which may be considered a limitation.
In the current study, we used the IM PRECICE nails originally designed for lower limb lengthening. In April 2016, a PRECICE humeral compression-distraction nail was released, and we have used it once (currently <1 year follow-up).
Mean CI in the current study was 36 days/cm (range, 24.8 to 45 days/cm). This was slightly greater than reported in other studies (Table 3). However, statistical comparison was not amenable due to small cohort in the current study. In the literature, the mean humeral length achieved with Ilizarov frames ranges from 5 to 11.1 cm [15, 17, 22, 37]. Kiss et al., in their study, achieved a mean length of 6.2 cm (range, 4.5 to 10.5 cm) in 11 humeri that underwent lengthening with the Wagner external fixator [19]. Balci et al. reported a mean length achieved of 7.8 cm (6.5 to 10) in 36 achondroplastic humeri that underwent lengthening with monolateral external fixators [4]. Pawar et al. used two different monolateral external fixators to lengthen 19 humeri with a mean of 7 cm [29]. In our study, the mean length achieved was 5.1 cm, which met our initial goal (Table 3). The allowed maximum stroke length of the PRECICE nails in our study was 5 cm. Two segments had acute 8-mm intraoperative distraction to obtain the final goal of 5.8 cm. In these two segments, a longer latency time was recommended to compensate for the acute distraction gap.
Table 3.
Comparison with the literature
| Author | No. of segments | Method | Mean length achieved (cm) | CI (days/cm) | Number of complications |
|---|---|---|---|---|---|
| Current study | 6 | IM PRECICE | 5.1 | 36 | none |
| Balci et al. [4] | 36 | Monolateral fixators | 7.8 | 24.1 | 12 |
| Pawar et al. [29] | 15 | Monolateral fixators | 7 | 32 | 6 |
| McLawhorn et al. [26] | 3 | MAC system | 6.5 | 27.1 | 6 |
| Kashiwagi et al. [16] | 20 | Ilizarov | 8 | 30 | 4a |
| Hosny [15] | 16 | Hybrid | 9 | 28 | 19 |
| Cattaneo et al. [9] | 43 | Ilizarov | 9 | 27 | 19 |
CI consolidation index, MAC Multi-Axial Correction Fixation System, EBI/Biomet Trauma, Parsippany, NJ, USA
aPin-tract infection not reported
Our study demonstrated improved patient-reported functional outcomes after surgery. The QuickDASH score showed an average of 23 points improvement compared with the score before lengthening. This was comparable to the reported DASH score as a functional outcome after humeral lengthening using the monolateral external fixator, with the average of 5 points and 23 points improvement in two studies [4, 29]. UEFI showed a little improvement from a preoperative mean of 53 points to a postoperative mean of 71 points, in spite of the fact that one patient reported a little deterioration of his arm function in his UEFI post-lengthening. Few studies reported either no change or improved ROM after humeral lengthening with the external fixators [15, 16, 26, 29]. Cattaneo et al. reported permanent post-lengthening decreased elbow and shoulder ROM, manifested by joint stiffness in 7% of the cohort [8, 9]. In our study, patients maintained their ROM during the lengthening phase at pre-surgery levels. Later, during the consolidation phase, improvement in elbow and shoulder ROM (except for shoulder flexion which was limited in four segments) was observed in two segments. We were not able to compare this finding with the literature due to deficiency of data reporting timing of ROM improvement. We assume that IM nails allow for easier postoperative physiotherapy and rehabilitation that could be started immediately post-surgery, compared with external fixators. One negative is that IM nails are inserted through the rotator cuff.
We did not observe complications related to PRECICE humeral lengthening in this study. Pin-tract infection, regenerate fracture or deformity post-frame removal, radial nerve palsy, and hardware failure are all reported complications associated with humeral lengthening using external fixators [4, 8, 11, 19, 22, 25, 29, 34]. Radial nerve problems are a common complication of humeral lengthening. Sometimes they occur due to regenerate manipulation to correct iatrogenic axial deformity that occurred during lengthening [11]. Percentage of fracture regenerate post-frame removal reported in the literature ranged from 7% to 16% [4, 9, 15, 16, 29]. IM nails avoid the complications of pin-tract infection, regenerate fracture, or axial deformity post-lengthening (Table 3).
To our knowledge, this is the largest case series available reporting the use of fully implantable IM lengthening nails for humeral lengthening. Based on our preliminary results, we encourage use of the new available technology when feasible. We conclude IM lengthening nails can provide the same results and fewer complications than humeral lengthening with external fixators. Specifically, the PRECICE nail has accurate control over the lengthening process. Available nail design may limit its use to selected patients with humeri that fit certain length and size limitations. Further studies on larger cohorts and increased duration of follow-up are recommended to confirm our conclusions.
Electronic Supplementary Material
(PDF 1224 kb)
(PDF 1225 kb)
(PDF 1225 kb)
(PDF 1225 kb)
Compliance with Ethical Standards
Conflict of Interest
Ahmed I. Hammouda, MD, has declared that he has no conflict of interest. Shawn C. Standard, MD, reports grants from NuVasive Specialized Orthopedics, during the conduct of the study; personal fees from NuVasive Specialized Orthopedics and Pega Medical; grants from CS Medical Supply, Metro Prosthetics, and Stryker; grants from Baxter, DePuy Synthes, Merete Technologies, MHE Coalition, NuVasive Specialized Orthopedics, Orthofix, OrthoPediatrics, Smith & Nephew, Stryker, and Zimmer Biomet, outside the work. S. Robert Rozbruch, MD, reports personal fees from Smith and Nephew, Stryker, NuVasive, outside the work. John E. Herzenberg, MD reports grants from NuVasive Specialized Orthopedics, during the conduct of the study; personal fees from Orthofix; grants from OrthoPediatrics, NuVasive Specialized Orthopedics, Smith & Nephew, CS Medical Supply, Metro Prosthetics, and Stryker, Baxter, DePuy Synthes, Merete Technologies, MHE Coalition, NuVasive Specialized Orthopedics, Orthofix, OrthoPediatrics, Smith & Nephew, Stryker, and Zimmer Biomet, outside the work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Level IV
Study performed at Sinai Hospital of Baltimore, Baltimore, MD, USA, and Hospital for Special Surgery, New York, NY, USA.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-017-9552-x) contains supplementary material, which is available to authorized users.
References
- 1.Accadbled F, Pailhé R, Cavaignac E, Sales de Gauzy J. Bone lengthening using the Fitbone(®) motorized intramedullary nail: The first experience in France. Orthop Traumatol Surg Res. 2016. [DOI] [PubMed]
- 2.Al-Sayyad MJ. Taylor spatial frame in the treatment of upper extremity conditions. J Pediatr Orthop. 2012;32:169–178. doi: 10.1097/BPO.0b013e3182471ae4. [DOI] [PubMed] [Google Scholar]
- 3.Babatunde OM, Fragomen AT, Rozbruch SR. Noninvasive quantitative assessment of bone healing after distraction osteogenesis. HSS J. 2010;6(1):71–8. doi: 10.1007/s11420-009-9130-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balci HI, Kocaoglu M, Sen C, Eralp L, Batibay SG, Bilsel K. Bilateral humeral lengthening in achondroplasia with unilateral external fixators: is it safe and does it improve daily life? Bone Joint J. 2015;97-B(11):1577–81. doi: 10.1302/0301-620X.97B11.36037. [DOI] [PubMed] [Google Scholar]
- 5.Beaton DE, Wright JG, Katz JN, Upper Extremity Collaborative Group Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am. 2005;87(5):1038–46. doi: 10.2106/JBJS.D.02060. [DOI] [PubMed] [Google Scholar]
- 6.Belthur MV, Iobst CA, Bor N, Segev E, Eidelman M, Standard SC, Herzenberg JE. Correction of cubitus varus after pediatric supracondylar elbow fracture: alternative method using the Taylor spatial frame. J Pediatr Orthop. 2015. [DOI] [PubMed]
- 7.Black SR, Kwon MS, Cherkashin AM, Samchukov ML, Birch JG, Jo CH. Lengthening in congenital femoral deficiency: a comparison of circular external fixation and a motorized intramedullary nail. J Bone Joint Surg Am. 2015;97(17):1432–40. doi: 10.2106/JBJS.N.00932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cattaneo R, Catagni MA, Guerreschi F. Applications of the Ilizarov method in the humerus. Lengthenings and nonunions. Hand Clin. 1993;9(4):729–39. [PubMed] [Google Scholar]
- 9.Cattaneo R, Villa A, Catagni MA, Bell D. Lengthening of the humerus using the Ilizarov technique. Description of the method and report of 43 cases. Clin Orthop Relat Res. 1990;250:117–24. [PubMed] [Google Scholar]
- 10.Chesworth BM, Hamilton CB, Walton DM, Benoit M, Blake TA, Bredy H, Burns C, Chan L, Frey E, Gillies G, Gravelle T, Ho R, Holmes R, Lavallée RL, MacKinnon M, Merchant AJ, Sherman T, Spears K, Yardley D. Reliability and validity of two versions of the upper extremity functional index. Physiother Can. 2014;66(3):243–53. doi: 10.3138/ptc.2013-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dal Monte A, Andrisano A, Manfrini M, Zucchi M. Humeral lengthening in hypoplasia of the upper limb. J Pediatr Orthop. 1985;5(2):202–7. doi: 10.1097/01241398-198505020-00015. [DOI] [PubMed] [Google Scholar]
- 12.Damsin JP, Ghanem I. Upper limb lengthening. Hand Clin. 2000;16(4):685–701. [PubMed] [Google Scholar]
- 13.Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord. 2006;7:44. doi: 10.1186/1471-2474-7-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Herzenberg JE. Humeral lengthening and realignment. In, Rozbruch SR, Ilizarov S eds. Limb Lengthening and Reconstruction Surgery. New York: Informa Healthcare; 2007;ch 39:535–543.
- 15.Hosny GA. Unilateral humeral lengthening in children and adolescents. J Pediatr Orthop B. 2005;14:439–443. doi: 10.1097/01202412-200511000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Kashiwagi N, Suzuki S, Seto Y, Futami T. Bilateral humeral lengthening in achondroplasia. Clin Orthop Relat Res. 2001;391:251–257. doi: 10.1097/00003086-200110000-00029. [DOI] [PubMed] [Google Scholar]
- 17.Katz K, Goldberg I, Bahar A, Yosipovitch Z. Humeral lengthening for septic neonatal growth arrest. J Hand Surg Am. 1989;14:903–907. doi: 10.1016/S0363-5023(89)80100-5. [DOI] [PubMed] [Google Scholar]
- 18.Kim SJ, Agashe MV, Song SH, Choi HJ, Lee H, Song HR. Comparison between upper and lower limb lengthening in patients with achondroplasia: a retrospective study. J Bone Joint Surg Br. 2012;94(1):128–33. doi: 10.1302/0301-620X.94B1.27567. [DOI] [PubMed] [Google Scholar]
- 19.Kiss S, Pap K, Vízkelety T, Terebessy T, Balla M, Szoke G. The humerus is the best place for bone lengthening. Int Orthop. 2008;32(3):385–8. doi: 10.1007/s00264-007-0327-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kurtz AM, Rozbruch SR. Humerus Lengthening With the PRECICE Internal Lengthening Nail. J Pediatr Orthop. 2017 Feb 27. [DOI] [PubMed]
- 21.Lädermann A, Edwards TB, Walch G. Arm lengthening after reverse shoulder arthroplasty: a review. Int Orthop. 2014;38(5):991–1000. doi: 10.1007/s00264-013-2175-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee FY, Schoeb JS, Yu J, Christiansen BD, Dick HM. Operative lengthening of the humerus: indications, benefits, and complications. J Pediatr Orthop. 2005;25:613–616. doi: 10.1097/01.bpo.0000164868.97060.bb. [DOI] [PubMed] [Google Scholar]
- 23.Malot R, Park KW, Song SH, Kwon HN, Song HR. Role of hybrid monolateral fixators in managing humeral length and deformity correction. Acta Orthop. 2013;84(3):280–5. doi: 10.3109/17453674.2013.786636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McCarthy JJ, Iobst CA, Rozbruch SR, Sabharwal S, Eismann EA. Limb Lengthening and Reconstruction Society AIM index reliably assesses lower limb deformity. Clin Orthop Relat Res. 2013;471(2):621–7. doi: 10.1007/s11999-012-2609-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McCarthy JJ, Ranade A, Davidson RS. Pediatric deformity correction using a multiaxial correction fixator. Clin Orthop Relat Res. 2008;466:3011–3017. doi: 10.1007/s11999-008-0491-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McLawhorn AS, Sherman SL, Blyakher A, Widmann RF. Humeral lengthening and deformity correction with the multiaxial correction system. J Pediatr Orthop B. 2011;20:111–116. doi: 10.1097/BPB.0b013e328341bc87. [DOI] [PubMed] [Google Scholar]
- 27.Paley D. PRECICE intramedullary limb lengthening system. Expert Rev Med Devices. 2015;12(3):231–49. doi: 10.1586/17434440.2015.1005604. [DOI] [PubMed] [Google Scholar]
- 28.Paley D, Herzenberg JE, Bor N. Fixator-assisted nailing of femoral and tibial deformities. Techniques in Orthopaedics. 1997;12(4):260–275. doi: 10.1097/00013611-199712000-00004. [DOI] [Google Scholar]
- 29.Pawar AY, McCoy TH, Jr, Fragomen AT, Rozbruch SR. Does humeral lengthening with a monolateral frame improve function? Clin Orthop Relat Res. 2013;471:277–283. doi: 10.1007/s11999-012-2543-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Popkov D, Popkov A, Haumont T, Journeau P, Lascombes P. Flexible intramedullary nail use in limb lengthening. J Pediatr Orthop. 2010;30(8):910–8. doi: 10.1097/BPO.0b013e3181f0eaf9. [DOI] [PubMed] [Google Scholar]
- 31.Shabtai L, Specht SC, Standard SC, Herzenberg JE. Internal lengthening device for congenital femoral deficiency and fibular hemimelia. Clin Orthop Relat Res. 2014;472(12):3860–8. doi: 10.1007/s11999-014-3572-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shevtsov VI, Popkov AV, Popkov DA, Yerofeev SA, Prévot J, Lascombes P. Elastic stable intramedullary nailing in Ilizarov bone lengthening. Rev Chir Orthop Reparatrice Appar Mot. 2004;90(5):399–410. doi: 10.1016/S0035-1040(04)70166-X. [DOI] [PubMed] [Google Scholar]
- 33.Rozbruch SR, Birch JG, Dahl MT, Herzenberg JE. Motorized intramedullary nail for management of limb-length discrepancy and deformity. J Am Acad Orthop Surg. 2014;22(7):403–9. doi: 10.5435/JAAOS-22-07-403. [DOI] [PubMed] [Google Scholar]
- 34.Tellisi N, Ilizarov S, Fragomen AT, Rozbruch SR. Humeral lengthening and deformity correction in Ollier’s disease: distraction osteogenesis with a multiaxial correction frame. J Pediatr Orthop B. 2008;17:152–157. doi: 10.1097/BPB.0b013e3282f548dc. [DOI] [PubMed] [Google Scholar]
- 35.Tetsworth K, Krome J, Paley D. Lengthening and deformity correction of the upper extremity by the Ilizarov technique. Orthop Clin North Am. 1991;22(4):689–713. [PubMed] [Google Scholar]
- 36.Tiefenboeck TM, Zak L, Wozasek GE. Intramedullary magnetically actuated limb lengthening in a patient with congenital humeral limb shortening. Injury. 2016 Jul;47(7):1597-600 [DOI] [PubMed]
- 37.Yang CB, Huang SC. Humeral lengthening using the Ilizarov technique. J Formos. Med Assoc. 1997;96(4):291–4. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1225 kb)
(PDF 1225 kb)
(PDF 1225 kb)