Abstract
Melatonin is an indolic hormone that regulates a plethora of functions ranging from the regulation of circadian rhythms and antioxidant properties to the induction and maintenance of tumor suppressor pathways. It binds to specific receptors as well as to some cytosolic proteins, leading to several cellular signaling cascades. Recently, the involvement of melatonin in cancer insurgence and progression has clearly been demonstrated. In this review, we will first describe the structure and functions of melatonin and its receptors, and then discuss both molecular and epidemiological evidence on melatonin anticancer effects. Finally, we will shed light on potential cross-talk between melatonin signaling and the Hippo signaling pathway, along with the possible implications for cancer therapy.
Keywords: melatonin, cancer, melatonin receptors, GPCR signaling, Hippo pathway
1. Introduction
Melatonin (N-acetyl-5-methoxy tryptamine) is a pleiotropic neurohormone mainly secreted by the pineal gland and partially by other peripheral organs that are widely distributed, including in the gut, gonads, retina, and immune-competent cells [1]. Its production is tightly regulated by light/dark signals coming from the retina, following a circadian rhythm, with a peak during the night and relatively lower concentrations during the day, when the light turns off its production [2,3,4]. Melatonin peak levels are higher in new-borns and start to decline in the elderly [5].
The physiological input for pineal melatonin production starts in a subgroup of Retinal Ganglion Cells sensitive to a specific light-blue wavelength [2,3] that transmits information to the pineal gland through the retino-hypotalamic tract and induces the transcription and stabilization of N-acetyltransferase (NAT) enzyme [6,7]. This latter, together with the hydroxyindole-O-methyltransferase enzyme (HIOMT), is responsible for converting serotonin to melatonin [3,8,9]. During the day, light inhibits NAT and melatonin production [10].
Once produced, melatonin is released into the cerebrospinal fluid and capillaries and reaches all the body’s tissues, with concentrations between picomolars and nanomolars. It is metabolized by the liver and secreted in the urine, where its major metabolite, 6-sulfatoxy-melatonin (aMT6s), correlates with melatonin’s nocturnal plasma peaks [11,12,13]. Chronic exposure to artificial light at night deregulates melatonin levels, as shown in rodent models and in cohort studies of night-shift workers [14]. In addition, an inverse correlation between melatonin levels and tumor incidence has been reported in prospective nested case control studies [15,16,17,18,19,20,21,22], suggesting that supplementation with melatonin might be proposed as cancer chemopreventive treatment in human clinical studies [23,24,25].
2. Melatonin Membrane Receptors
Melatonin controls a plethora of physiological processes including regulation of sleep-wake rhythm, temperature and physiologic activities in the circadian clock, blood pressure regulation, stimulation of bone metabolism, immune function, reproductive functions, memory formation, cell differentiation and proliferation, inhibition of oxidative stress and inflammation processes [26,27,28,29,30,31,32,33,34,35,36]. All these functions employ both receptor-dependent and receptor-independent mechanisms. The two main membrane receptors, MTNR1A and MTRN1B, also known as MT1 and MT2, belong to the superfamily of G-protein coupled receptors (GPCRs), which constitute the largest family of membrane receptors with approximately 1000 members and respond to a wide variety of extracellular stimuli (hormones, neurotransmitters, or growth factors) controlling physiological processes such as cellular metabolism, secretion, cell differentiation, and growth [37]. MT1 and MT2 exist in both homo-dimeric and hetero-dimeric forms, and share high sequence homology [38]. They are expressed in several areas of the central nervous system (CNS), in the retina, the gastro-intestinal tract, arteries and immune cells [33]. They show different affinities for melatonin: MT2 has a 5-fold higher affinity than MT1, in both humans and other species [38,39,40]. MT3, a low affinity binding receptor, is a Quinone reductase 2, an enzyme that catalyzes the reduction of quinones into quinols having important implications on oxidative stress [41,42].
MT1 and MT2 Mediated Signal Transduction
Upon agonist binding, cytoplasmic heterotrimeric G proteins that are comprised of Gα, β and γ subunits dissociate from GPCR transmembrane receptors [43]. The 15 different Gα subunits are classified into four families, Gα12/13, Gαq/11, Gαi/o, and Gαs [44], which in turn act on individual effectors such as adenylate cyclase (AC), phosphodiesterase (PDE), phospholipase C (PLC), or ion channels to affect the levels of associated second messengers including 3′,5′-cyclic adenosine or guanosine monophosphate (cAMP and cGMP), inositol triphosphate (IP3), and calcium [45].
MT1 and MT2 receptors mainly associate with Gαi proteins and to a lesser extent with Gαq/11 and Gαs proteins [46,47,48,49,50,51,52,53,54,55] which can couple to multiple signal transduction cascades, either alternately, or concomitantly in the same tissue [56]. In general, the signal transduction pathways induced by melatonin receptors are cell type and tissue specific [33] leading to unique cellular responses and suggesting a potential crosstalk with other signaling pathways. For example, MT1 receptor activation by melatonin may lead to different and in some cases opposite signaling pathways, depending on which Gα protein is activated. In general, Gαi activation leads to the inhibition of the adenyl cyclase activity with consequent inhibition of cyclic AMP (cAMP) formation, inhibition of protein kinase A (PKA) activity, and reduced phosphorylation and transcriptional activity of the cAMP-responsive element binding (CREB) as well as activation of phospholipase C β [48,57,58,59,60,61,62,63,64]. Conversely, in other systems such as Cos7 fibroblasts, HEK293 and MCF7 cells, activation of Gαq and Gαs proteins coupled to MT1 receptors leads to an increase of cAMP formation. Increased intracellular cAMP in turn activates PKA and PKC, which causes the inhibition of NF-ΚB (Nuclear Factor Kappa-light-chain-enhancer of activated B cells) with consequent derepression of the oncosuppressor p27kip1 and attenuation of the androgen response in prostate cells [53,54,55,65,66,67], activation of JNK in Cos7 cells [68], and phosphorylation of ERK1/2 in HEK 293 cells [69].
3. Melatonin and Nuclear Receptors: Contrasting Evidence
In the 90’s and a few years later, some studies showed that melatonin and its analogues can bind in vitro to nuclear receptors belonging to the family of retinoid Z receptor/Retinoid Orphan Receptor alpha (RZR/RORα) [70,71,72,73,74]. These receptors are organized into the following structural domains: a N-terminal transactivating domain, a DNA-binding domain, a variable domain, and a ligand-binding domain [75]. Once activated, they bind ROR response elements (ROREs) on the chromatin (TAAA/TNTAGGTCA motif) primarily as monomers [76,77,78,79] and regulate genes involved in cell differentiation, immune response, lipid metabolism, CNS development, tumour growth and inflammation [33,71,72,73,80,81,82,83,84,85,86]. Biologically, a role for melatonin in the downregulation of 5-lipooxygenase gene through RZR/RORα receptors has been shown by Carlsberg’s group in B lymphocytes [87]. However, Carlberg’s group in 1997 retracted the report that melatonin is a direct ligand of these nuclear receptors because they could not reproduce their results. Yet, the above mentioned study suggested a positive regulation of RZR/RORα by melatonin either in transcriptional activation or in repression of target genes [70,71,72,73,87], even if a direct binding of melatonin to receptors is arguable. In 2011, the group of Lardone and coworkers showed a direct interaction between melatonin and nuclear receptors in T lymphocytes and a negative regulation of nuclear RORα levels by melatonin. Other works showed a possible negative regulation of RZR/RORα by melatonin in different experimental systems [88,89], while in models of gastric cancer melatonin has been shown to negatively regulate RZR/RORγ [90].
4. Oncoprotective Role of Melatonin: In Vitro Evidence
Epidemiological studies have suggested that melatonin decreases the risk of developing different types of cancer. Recently, the molecular mechanism by which melatonin exerts its anticancer effects has been revised [91,92]. This might occur either through downregulation of oncogenic pathways or via activation of tumor suppressor activities.
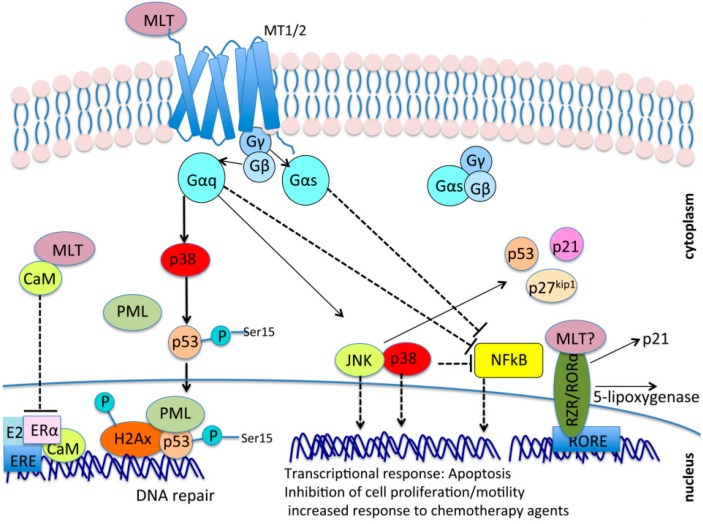
Melatonin can activate phosphorylation cascades, mediated by MEK1/2, ERK1/2, JNK and p38 MAPK, through binding to its membrane receptors MT1 and MT2 [93,94,95,96,97]. In particular, our group and others have shown that the binding of melatonin to MT1 and MT2 triggers a phosphorylation cascade, mediated in part by p38, which leads to the activation of p53 through phosphorylation of Ser15. This leads to a transient cell cycle arrest through the accumulation of tumor suppressive proteins (see Figure 1) and the induction of DNA repair mechanisms that prevent the accumulation of DNA mutations in response to DNA damage induced by chemotherapeutic agents or ionizing radiations. These events occurred both in normal and tumor cells only in the presence of intact MT1 and MT2 signaling [98,99,100].
Figure 1.
Oncosuppressive mechanisms mediated by melatonin. Melatonin (MLT) signaling has been shown to reduce the abundance and transcriptional activity of the NF-κB (nuclear factor kappa-light-chain-enhancer of activated B cells) transcription factor as well as to activate phosphorylation cascades mediated by mitogen-activated protein kinases (MAPKs) such as MEK1/2, ERK1/2, JNK, and p38. Both NF-κB inhibition and MAPKs activation in turn inhibit cell growth and motility, and promote apoptosis and DNA damage repair through mechanisms involving the accumulation of oncosuppressors such as p53, p27kip1, and p21, activation of DNA repair complexes such as P53/PML/H2AX on DNA damage sites, and transcriptional control of genes involved in the cell cycle, apoptosis, and invasiveness. Even though it is still a matter of debate, there is the possibility that melatonin can also bind to nuclear receptors RZR/ROR, controlling the transcription of RORE (ROR response Elements) on genes of the retinoic acid response, among which are several genes controlling cell cycle progression and cell growth (p21, 5-lipoxygenase, and others). Finally, melatonin can bind to the intracellular protein calmodulin (CaM) and reduce the Estrogen Receptor α (ERα) response in ER positive cells by impairing the formation of a proper E2–ERα–CaM complex on Estrogen Receptor Elements (EREs) on target genes. Arrows indicate activation, while dashed and blunt lines indicate inhibition. Activation indicates an increase in protein or activity levels, while inhibition indicates a decrease in protein or activity levels.
Melatonin also causes the reduction of the abundance and the transcriptional activity of the NF-κB (nuclear factor kappa-light-chain-enhancer of activated B cells) transcription factor, leading to reduced proliferation and metastasis as well as increased apoptosis in basal conditions or in response to chemotherapeutic agents in several models of cancer including breast cancer, prostate cancer, colon and gastric cancer, pancreatic cancer, renal carcinoma, and hepatoma [55,93,95,101,102,103,104]. Part of the inhibition of the NF-κB transcriptional activity is elicited through the activation of JNK and p38 [93]. Oncosuppressive pathways induced by melatonin were also observed in vitro in glioblastoma [105,106] and osteosarcoma [107]. It is important to mention that beside its effects on cancer cells, melatonin protects from apoptosis normal cells like spermatozoa [108], cells in the liver [109], in the nervous [110] and immune systems [84,111,112,113,114,115,116,117,118,119,120], in which melatonin counteracts aging-related diseases, and stimulates immune cells activation and proliferation, respectively. Melatonin increases the number of effector T cells and decreases the number of regulative T cells (Tregs) [119,120]. Tregs have an inhibitory effect on anti-cancer immunity and some tumor cells are able to upregulate and recruit Tregs to escape the antitumor effect of the cellular immune system [121].
In summary, melatonin promotes apoptosis in certain circumstances, for example in cancer cells and in Treg cells, while it protects normal cells from apoptosis, including cells of the immune system that actively counteract infections and tumors.
The net effect of these opposite mechanisms is the protection of the whole organism from inflammation, aging-related diseases, cancer development, and progression.
Melatonin also inhibits cancer cell migration and invasiveness by increasing the expression of cell adhesion molecules [122,123,124,125] and by reducing the expression of the RhoA kinase ROCK involved in progression and metastasization of several tumors [124,126,127].
Moreover, melatonin has been shown to inhibit the expression of stemness-related genes, [105,128,129] to inhibit stemness-related pathways [105,106] to improve the response to several anticancer therapies [102,103,130,131,132,133,134], and to inhibit angiogenesis [127,135,136,137,138,139,140,141,142,143,144,145,146]. Finally, in Androgen Receptor (AR) and Estrogen Receptor (ER) positive cells, melatonin inhibits the AR [54,65,147,148,149] and ER response [128,150,151,152,153] through different mechanisms either mediated by MT1 or independent of MT1 receptor binding.
In general, MT1 seems to play a prominent role in triggering anti-tumor cellular responses mediated by melatonin [53,54,55,154,155,156,157,158,159], although in some experimental models MT2 has been shown to be required too [160,161].
Melatonin can also counteract tumor formation through mechanisms independent of MT1 and MT2. For example, through calmodulin (CaM) binding, melatonin interferes with the transcription of Estrogen Receptor α (ERα) genes in response to estrogen (E2). The formation of a melatonin–CaM complex, in fact, impairs the formation of a proper E2–ERα–CaM complex on ERα targets [153]. Moreover, in models of colon cancer, gastric cancer [82,90,162,163], and ovarian carcinoma [164], nuclear RZR/ROR receptors were proposed to contribute to the tumor-suppressive effects of melatonin even if, as mentioned above, a direct interaction between melatonin and RZR/RORα receptors is still a matter of debate because no one has yet reproduced Carlberg et al.’s pioneering results that show a direct interaction between melatonin and nuclear receptors (Figure 1).
5. Melatonin Antioxidant Properties
Melatonin is an antioxidant, anti-inflammatory and anti-angiogenic molecule. Various oxidative reactions normally occurring in the organism, mainly in mitochondria, generate free radicals from reactive oxygen species (ROS) and reactive nitrogen species (RNS). In normal cells, these species are required for signal transduction before their elimination through endogenous antioxidant compounds and enzymes. The aberrant accumulation of reactive oxidant species can cause multiple lesions in macromolecules (nucleic acids, proteins, and lipids), leading to their damage. In cancer the aberrant activation of pathways leading to cell proliferation and invasiveness causes a hyperaccumulation of ROS and RNS. Endogenous antioxidants are not sufficient to counteract this accumulation. However, cancer cells often acquire resistance to oxidative stress and escape free radical damage. In that context, ROS accumulation in turn promotes tumor development and progression and induces increased cell proliferation, evasion of apoptosis, tissue invasion-metastasis, and angiogenesis (reviewed in [165,166]).
Melatonin counteracts the oxidative stress through multiple mechanisms [167]. It stimulates the expression and activity of antioxidative enzymes [168]. It inhibits the expression of QR2 enzyme at pharmacological concentrations that are higher than those required for MT1 and MT2 activation. Given that QR2 reduces quinones into quinols, and thereby functions as an indirect producer of ROS, it has been proposed that the inhibition of QR2 activity may in part explain the antioxidant properties of melatonin [42].
Moreover, melatonin preserves the integrity and the function of the mitochondria [169,170,171]. Through these mechanisms, melatonin prevents the genotoxic and carcinogenic effects of oxidative stress and helps to maintain cell function and survival.
6. Clinical Studies
Melatonin is involved in several physiological processes, and its deficiency (or an altered expression of its receptors) has been associated with a number of chronic diseases including several types of cancer [172,173,174,175,176]. Conversely, a number of randomized and controlled clinical trials showed that exogenously administered melatonin has, among several biological effects, anti-cancer, anti-inflammatory and antioxidant properties in different cancer types, thus improving the responses of patients to traditional therapies and reducing the side effects of the latter [23,24,25].
In the following section, we will present results from observational, translational and cohort prospective studies on the association between pre-diagnostic prolonged exposure to daylight and low melatonin serum levels and subsequent cancer development.
6.1. Circadian Disruption and Increased Light Exposure Contribute to Increased Cancer Risk
In 1991 [177], Hann and co-workers showed a reduced risk of breast cancer in blind women. Based on the observation that blind women are constantly in the dark and that melatonin production is increased during the night [178], this study suggested for the first time a possible protective role of melatonin in blind women against the risk of developing cancer. Later observations supported this hypothesis [179,180,181]. Conversely, several bodies of evidence showed that disruption of the circadian rhythm, in part as a consequence of night-shift work and light pollution at night (LAN), increases the risk of developing breast cancer [182,183,184] and prostate cancer [185]. Importantly, our group and others showed an inverse correlation between night work, circadian disruption and melatonin production suggesting a protective role of melatonin against diseases associated with circadian disruption [35].
6.2. Low Levels of Endogenous Melatonin or Altered Expression of Its Receptors Are Associated with Increased Cancer Risk
Many groups, including ours, showed that high levels of endogenous melatonin measured many years before the onset of breast cancer were associated with a reduction of breast cancer occurrence [15,16]. Other sets of evidence suggested a protective role of circulating melatonin on prostate cancer development [17].
Conversely, two recent translational studies showed a lower expression of MT1 and MT2 receptors in colon cancer tissues compared to matched normal tissues, suggesting melatonin’s protective role in colon cancer development [159,160]. A negative correlation between melatonin receptor expression and cancer has also been observed in Oral Squamous Cell Carcinoma (OSCC), where a reduced expression of MT1 is also related to the T stage of tumor [186], and in breast cancer, where a lower MT1 expression is associated with a poorer prognosis [156], together with a higher tumor grade and TNM staging [187]. Finally, in Renal Cell Carcinoma (RCC) MT1 receptor expression was found to be lower in cancer tissue compared to normal tissue [104].
7. A Possible Crosstalk between Melatonin Signaling and the Hippo Tumor Suppressor Pathway
As mentioned above, melatonin signals in part through MT1 and MT2 GPCR receptors. Recently, GPCR signaling has been shown to regulate the Hippo pathway, which controls animal organ development and growth and whose dysregulation is often involved in tumorigenesis (reviewed in [188]). Components of the Hippo pathway include membrane-associated proteins that sense cell polarity, cell density, and mechanical and metabolic cues that in turn activate a cascade of kinases with adaptor proteins whose final targets are the transcriptional coactivators YAP and TAZ. YAP/TAZ work as oncogenes in many solid cancers, where they are often upregulated or hyperactivated compared to normal tissues (reviewed in [188]).
When the Hippo cascade is on, phosphorylation of YAP and TAZ by LATS1/2 kinases results in their nuclear export, cytoplasmic retention [189,190,191,192,193,194], and degradation by the proteasome [195,196,197]. When the Hippo cascade is off, YAP/TAZ are dephosphorylated and are able to exert their nuclear function and promote transcription of oncogenes in association with oncogenic transcription factors such as TEADs, SMADs, and others [188].
Since YAP/TAZ are becoming increasingly attractive and promising therapeutic targets in cancer treatment (reviewed in [198]), much importance is being placed on the discovery and characterization of inhibitors of YAP/TAZ oncogenic function. What is melatonin’s role in this scenario? At present, no literature has been produced on this topic. However, numerous independent sets of evidence suggest a potential antagonism between melatonin signaling and YAP/TAZ oncogenic function; we will try to summarize them in the following sections.
7.1. Gαs May Be a Common Molecular Intermediate between Melatonin Signaling and GPCR/YAP/TAZ Signalng
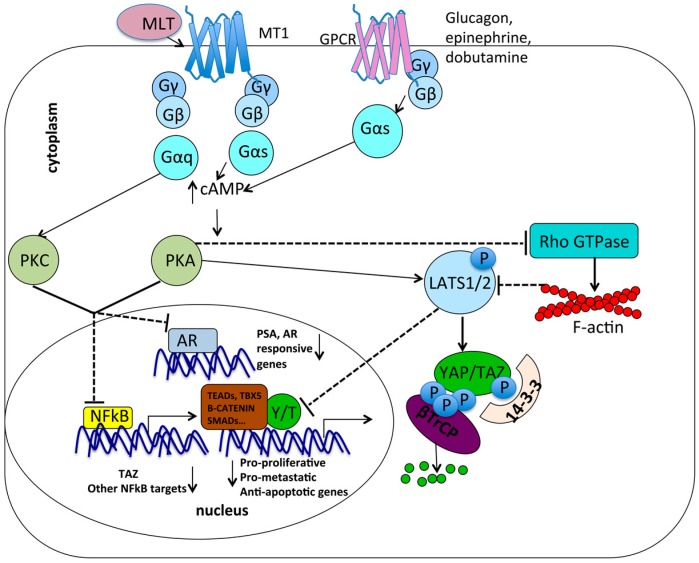
GPCR signaling regulates YAP/TAZ in response to several biochemical stimuli and YAP/TAZ can be either activated or inhibited depending on which GPCR and subsequent Gα protein is activated. For example, LPA, S1P, and thrombin activate Gαi, Gαq, and Gα12/13, which, in turn, activate YAP/TAZ by inducing their dephosphorylation mediated by Protein Phosphatase 1A (PP1A) and by repressing LATS1/2 kinase activity. This mechanism requires the Rho GTPase RhoA and its associated kinase ROCK and results in YAP/TAZ nuclear translocation [199,200,201,202,203]. In contrast, glucagon, epinephrine, and dobutamine, which transmit signal from Gαs, inhibit YAP/TAZ. One of the proposed mechanisms mediated by Gαs is an increased intracellular cAMP that leads to the activation of protein kinase A (PKA). This in turn inhibits the RhoA/ROCK signaling and stimulates LATS1/2 to phosphorylate YAP/TAZ, which are sequestered in the cytoplasm [203,204,205]. The inhibitory effect of cAMP accumulation on oncogenic YAP/TAZ is conserved in different cell lines, including breast metastatic MDA–MB-231, U2OS, MCF10A, HEK293A, and mouse embryonic fibroblasts (MEFs) [205].
Similarly, melatonin has been shown to activate Gαs proteins associated with MT1 receptors in prostate cell lines [53,54,55,65,66,67], Cos-7 cells [68], and HEK293 cells [69], as well as to increase intracellular cAMP with subsequent activation of PKA and PKC. Thus, the activation of PKA and PKC mediated by Gαs in response to different stimuli (glucagon, epinephrine, dobutamine, melatonin) may lead to inhibition of cell proliferation and invasiveness through multiple converging mechanisms, including LATS1/2 activation [203,204,205] and, as mentioned above, inhibition of NF-κB transcriptional activity and inhibition of the AR response in AR positive cells [55]. Moreover, a recent study showed that TAZ promoter is directly targeted and activated by NF-κB [206] suggesting that melatonin may potentially inhibit YAP/TAZ pro-oncogenic function either through increasing LATS1/2 activity (following PKA and PKC activation) or reducing TAZ transcription (following NF-κB inhibition) (Figure 2).
Figure 2.
Interplay between G-Protein Coupled Receptors (GPCR) signaling regulated by melatonin and GPCR signaling regulating YAP/TAZ. MT1 binding by melatonin (MLT) induces activation of associated Gαq and Gαs that leads to the accumulation of intracellular cAMP that in turn activates Protein Kinase A (PKA) and PKC. These in turn inhibit NF-κB transcriptional activity on its target promoters, including TAZ promoter. In Androgen Receptor (AR) positive cells, PKA and PKC inhibit the androgen response on AR responsive genes. In parallel, glucagon, epinephrine, and dobutamine signal through Gαs, inducing increased intracellular cAMP and activation of PKA. This in turn inhibits the RhoGTPase RhoA and activates LATS1/2 kinases, resulting in phosphorylation of YAP/TAZ, their cytoplasmic sequestration by 14-3-3 protein, their degradation mediated by βTrCP, and the impairment of their nuclear activity on pro-proliferative, pro-metastatic, and anti-apoptotic genes. ↑ indicates an increase in protein levels or activity; ↓ indicates a decrease in protein levels or activity.
7.2. Metabolic Pathways: Antagonism between Melatonin and YAP/TAZ
Beyond GPCR signaling, YAP/TAZ are also regulated by cell-cell contact, mechanical forces, and metabolic cues. These induce specific intracellular signaling affecting YAP/TAZ function through Hippo kinase cascade-dependent and independent mechanisms. Before going into more detail, some of these mechanisms may crosstalk with melatonin signaling. In general, we hypothesize an antagonism between melatonin and YAP/TAZ on multiple mechanisms involved in tumorigenesis.
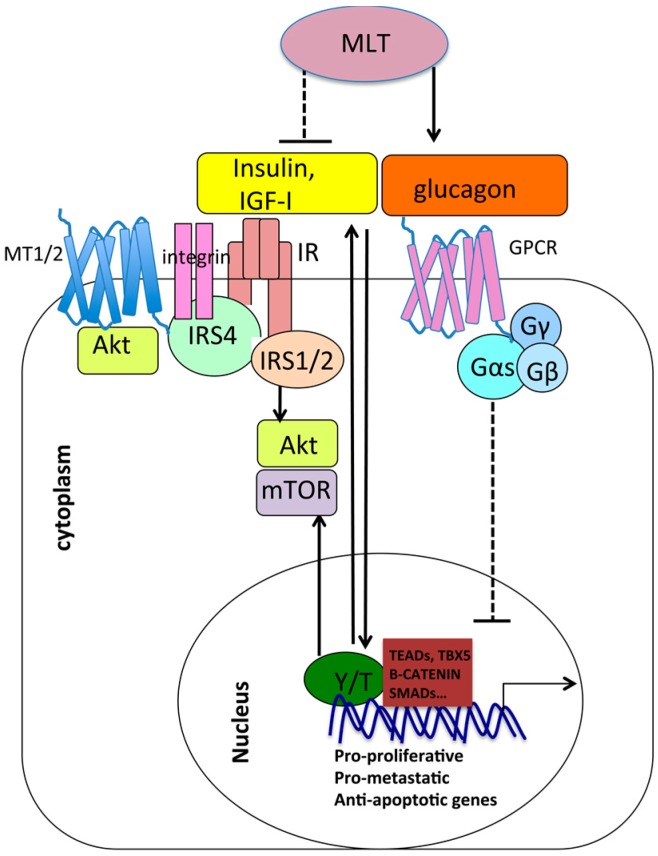
Insulin, insulin-like growth factors (IGF-I), nutrient intake, and other growth factors upregulate cellular biosynthetic pathways to sustain cellular growth and proliferation through the activation of protein kinases AKT/PI3K and mammalian target of rapamycin (mTOR) [207,208,209,210,211]. It has recently been shown that insulin and GPCR signaling engage in crosstalk and synergize to positively regulate YAP nuclear function onto YAP/TEAD target genes in pancreatic ductal adenocarcinoma (PDAC) cells via PI3K activation [212]. YAP has been shown in turn to positively regulate the insulin and the IGF-1 signaling [213] to drive IGF-2 expression, activate mTOR signaling and AKT [214,215,216], promote glucose uptake and glycolysis [217], driving growth advantage, metastatic competence, angiogenesis, and therapy resistance in various model systems. On the other hand, melatonin was shown to inhibit AKT/mTOR signaling in models of ovarian cancer [104], breast cancer [218], hepatoma [219], and melanoma [220], where AKT/mTOR are aberrantly hyperactivated and contribute to carcinogenesis [221]. Moreover, melatonin decreases insulin production from pancreatic β cells while increasing the expression and secretion of glucagon from pancreatic α cells [222]. Since glucagon is a negative regulator of YAP/TAZ nuclear function, as mentioned above, melatonin may indirectly inhibit nuclear YAP/TAZ through glucagon upregulation.
Interestingly, AKT and the Insulin Receptor Scaffold 4 (IRS4) have been shown to co-purify with MT2 receptor by Daulat and co-workers [223,224,225].
Together, this body of evidence suggests potential cross-talk between melatonin signaling, Hippo signaling, and insulin–glucagone signaling, in agreement with a growing literature that showing a reciprocal regulation between YAP/TAZ and metabolism on the one hand [226] and between melatonin and metabolism on the other [227,228] (Figure 3).
Figure 3.
Interplay between melatonin, YAP/TAZ, and metabolic pathways. Melatonin (MLT) upregulates glucagon production and downregulates insulin production and signaling. Glucagon inhibits YAP/TAZ nuclear function through Gαs signaling. Conversely, insulin and GPCR signaling synergize to positively regulate nuclear YAP onto YAP/TEAD target genes. In addition, YAP/TAZ activate AKT and mTOR, which are part of the insulin signaling. In conclusion, melatonin may inhibit YAP/TAZ nuclear function by inducing glucagon expression and decreasing insulin expression. On the other hand, YAP/TAZ positively regulate insulin signaling, and, vice versa, insulin signaling positively regulates YAP, suggesting an antagonism between melatonin function and nuclear YAP/TAZ function. Arrows indicate activation, while dashed and blunt lines indicate inhibition. The figure also shows the interaction between the insulin receptor scaffold 4 (IRS4) with insulin receptor, integrins, and MT1/2 receptors potentially linking these transmembrane proteins at the cell membrane. IR = Insulin Receptor, IRS1/2/4 = insulin receptor scaffold 1/2/4.
7.3. Mechanotransduction and Chemoresistance: Opposite Roles of Melatonin and YAP/TAZ
Mechanotransduction is a process where mechanical forces coming from the extracellular matrix (ECM) and from the cytoskeleton are transduced into cellular biochemical signals to regulate cell growth and survival. YAP/TAZ are widely recognized mechanotransducers and mechanoeffectors. They are preferentially active in the nucleus when cells are grown at low density, or on a stiff extracellular substrate, conditions where the cell–ECM contact area is larger and the cytoskeleton is subjected to a stronger mechanical stimulation (often the case of a tumor microenvironment). Conversely, YAP/TAZ effectors translocate to the cytoplasm in response to high cellular density/cell contact, or on a soft extracellular substrate, where the cell experiences lower mechanical stress [189,229,230,231,232,233,234,235,236,237]. Once activated, YAP/TAZ are able to regulate genes involved in extracellular matrix remodelling [238,239]. Matrix rigidity plays an important role in tumor development because it changes during tumorigenesis and regulates cell proliferation, stemness, and invasiveness, and also the response of cancer cells to various chemotherapy agents, through different pathways including YAP and TAZ regulation among others [240,241,242,243]. Accordingly, a role for YAP/TAZ in increasing the resistance of cancer cells to various chemotherapy agents has been extensively documented [243,244,245,246,247,248]. Conversely, melatonin treatment has been shown to partially overcome resistance to chemotherapy, suggesting a possible antagonism between melatonin and YAP/TAZ in cancer chemoresistance [24,102,103,130,131,132,133,134]. In response to mechanical stress, the stabilization of cytoskeletal F-actin fibers and the activation of RhoA–ROCK facilitate YAP/TAZ nuclear translocation, while F-actin destabilization induces YAP/TAZ phosphorylation and cytoplasmic retention. Currently, the gap between YAP/TAZ and these upstream transducers remains to be filled and it would be interesting to see what role melatonin signaling may play in this process. Some bodies of evidence suggest melatonin’s role in mechanotransduction: melatonin has been shown to regulate cytoskeletal dynamics in vitro [249,250,251] and in vivo [252,253], and to reduce the expression of the RhoA kinase ROCK [124,126,127]. Moreover, Daulat and coworkers characterized several proteins interacting with MT1 and MT2, among which is Filamin A [223,224,225], an actin-binding protein that contributes to the cross-linking of cortical actin filaments into a dynamic three-dimensional structure and is involved in mechanotransdution [254].
Akbarzadeh and co-workers’ recent work showed that ovarian cancer cells responded differently to melatonin treatment (in terms of cell proliferation, morphological changes, and stemness) depending on the composition of the extracellular matrix where they were cultured [145]. In this work, the authors showed for the first time the role played by mechanical cues in regulating the response of cells to melatonin.
7.4. Cell Contact/Polarity and RhoA/ROCK Signaling
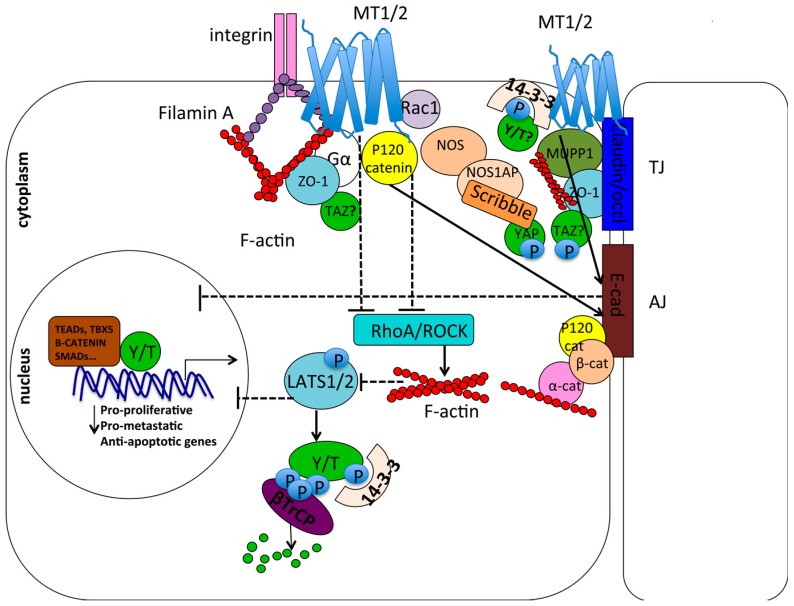
Epithelial tissues line the surface of the animal body and internal cavities. They are composed of cells oriented in the space with an apical-basal polarity. Several proteins contribute to the proper cell-cell adhesion, orientation and spatial organization within the tissue and their dysregulation can promote tumor development and metastasization [255,256,257]. In general, proteins involved in cell contact/junction and cell polarity negatively regulate YAP/TAZ nuclear function by sequestering YAP/TAZ at the apical plasma membrane, thus excluding them from the nucleus, and by interacting with and activating Hippo pathway core kinases [195,255,258,259,260,261,262,263,264,265,266,267,268,269,270,271,272]. Catenin δ1 (p120 catenin), a scaffold protein linking cytoskeletal actin fibers to adherens junctions at the plasma membrane, has been co-purified with MT1 and MT2 by Daulat and co-workers [223,224,225]. p120 has been shown to inhibit nuclear YAP and TAZ when localized at cellular junctions through inhibition of RhoA–ROCK signaling [273,274,275,276], as well as to stabilize cell adhesion cadherin complexes [277,278,279] that negatively regulate YAP/TAZ nuclear function [270,280]. Melatonin by itself reduces the migration and invasiveness of different cancer types by increasing the expression of E-cadherin and other adhesion molecules [122,123,124,125] and by reducing the expression of the RhoA kinase ROCK [124,126,127]. Rac1, a Rho GTPase that can functionally counteract RhoA [281,282], and the Ras-related GTPase Rap1 that activates Rac1 [283], have been co-purified with MT1 [223]. Together, this body of evidence suggests a possible role of melatonin and proteins associated with their receptors in the inhibition of the YAP/TAZ pro-oncogenic and metastatic function, through the inhibition of RhoA-ROCK signaling and via the stabilization of cell surface adhesion proteins [256].
Moreover, the MT1 receptor has been shown to interact with PDZ domain proteins including MUPP1 and the neuronal NO synthase (NOS) [225,284,285], while MT2 has been co-purified with 14-3-3 protein [223]. MUPP1 is concentrated at tight junctions at the apical membrane and, together with ZO-1 and other scaffold proteins, anchors the integral proteins of tight junctions to the F-actin cytoskeleton and contributes to their correct function and localization [286]. TAZ, containing a PDZ-binding motif, has been shown to interact both with ZO-1 and 14-3-3, which tether TAZ at the plasma membrane, thus inhibiting its nuclear function [189,192,193,268]. Also Gαi2, Gαo, and Gα12 have been shown to interact with ZO-1 in different systems and regulate tight junction assembly and permeability [287,288], while MUPP1 has been shown to promote Gαi coupling and signaling of the MT1 receptor [268,285]. Recently, YAP has been found in complex with the nitric oxide synthase 1 adaptor protein (NOS1AP) at cell-cell contacts together with the Scribble polarity complex [289,290], a negative regulator of YAP/TAZ pro-oncogenic function [245,291]. This interaction increases YAP phosphorylation and cytoplasmic sequestration. Interestingly, MT1 has been co-purified with the nitric oxide synthase (NOS). All these sets of evidence suggest a structural and functional role of cell polarity and cell contact proteins in the regulation of both the Hippo pathway and GPCR/MT1/MT2 signaling, which may converge in the inhibition of YAP/TAZ nuclear function. All these interactions are schematically represented in Figure 4.
Figure 4.
Interplay between melatonin signaling, cell contact-cell polarity complexes, mechanotransduction, and YAP/TAZ. Melatonin signaling inhibits RhoA/ROCK and increases the expression of cell surface adhesion molecules such as E-cadherin. This suggests that it may inhibit YAP/TAZ nuclear function, which in turn is promoted by RhoA/ROCK and inhibited by cell adhesion molecules. P120 catenin has been co-purified with MT1/MT2 receptors. When localized at the plasma membrane, it stabilizes E-cadherin at the adherens junction (AJ) while inhibiting RhoA–ROCK, thus inhibiting nuclear YAP/TAZ (Y/T). MT1/2 also co-purified with MUPP1 scaffold protein, which interacts with ZO-1 at tight junctions (TJ). Moreover, several studies showed that ZO-1 binds Gα proteins. This suggests a possible interaction with TAZ, which has been demonstrated to be sequestered at the plasma membrane through its interaction with ZO-1 at tight junctions. Moreover, YAP/TAZ may be sequestered at the plasma membrane by the 14-3-3 protein, which has been co-purified with MT1 and MT2. MT1/2 have also been co-purified with filaminA, involved in mechanotransdution, suggesting a link between melatonin receptor signaling and mechanotransduction, which has been demonstrated to regulate YAP/TAZ function and to be in turn controlled by YAP/TAZ. Finally, YAP has been co-purified with NOS1AP (nitric oxide synthase1 adaptor protein) in the complex formed with the scribble polarity proteins in proximity to cell–cell contacts. As NOS (nitric oxid syntase) has been co-purified with MT1/MT2, this again may suggest a possible indirect interaction of YAP with MT1/MT2 at the plasma membrane. In general, YAP/TAZ sequestration at the plasma membrane prevents their nuclear pro-proliferative function. Arrows indicate activation, while dashed and blunt lines indicate inhibition.
7.5. Opposite Roles of YAP/TAZ and Melatonin in Androgen–Estrogen Receptor Response and Angiogenesis
Melatonin inhibits the proliferation of Estrogen Receptor α (ERα)-positive lines more efficiently than ERα-negative lines, suggesting that part of its antiproliferative effect is mediated by the inhibition of the estrogen response. In fact, melatonin is able to inhibit the synthesis of steroids as well as interfere with the binding of the ER to its target genes [128,150,151,152,153]. Conversely, other studies showed that melatonin signaling is modulated by antiestrogens in breast and ovarian cancer cells [292]. Similarly, melatonin inhibits Androgen Receptor (AR) response in normal and malignant prostate epithelial cells [147,148,149]. On the other hand, LATS1/2 kinases have been shown to attenuate the androgen response in the prostate by inhibiting AR chromatin binding and transcriptional activity [293] as well as promoting ER degradation and reduction of its transcriptional activity in the breast [294,295], suggesting that melatonin signaling and Hippo signaling may converge to inhibit the ER and AR response.
Finally, melatonin inhibits angiogenesis by interfering with its Hif1α- and STAT3-mediated transcription of VEGF [127,135,136,137,138,139,140,141,142,143,144,145,146]. Conversely, YAP stabilizes H1F1α in response to hypoxia [296], suggesting an antagonistic role of melatonin and YAP/TAZ in angiogenesis regulation.
8. Conclusions
At present, promising preclinical and clinical studies suggest that melatonin may be a safe and valid therapy for the treatment of several types of malignancies when administered concomitantly with traditional therapies. In fact, melatonin has been shown to improve the response of patients to different therapies while reducing their toxic effects. On the other hand, preclinical studies showed that inhibitors of YAP/TAZ associated with traditional therapies reduce tumor growth as well as radio- and chemoresistance in different types of cancers [198,215,243,245,246,247,248,297]. To our knowledge, functional crosstalk between melatonin signaling and Hippo/YAP/TAZ signaling has never been previously addressed in the literature. However, several experimental observations may suggest that both the melatonin signaling and Hippo signaling pathways may intersect at different levels (GPCR signaling, AKT/PI3K signaling, and mechanotransduction) and both may potentially inhibit the oncogenic function of YAP and TAZ through many converging mechanisms. Although these potential cross-talks need extensive experimental validation, they may open up a new field of investigation with important implications for (1) a better understanding of melatonin- and YAP/TAZ-mediated pathways, which are still not completely elucidated; and (2) the potential design of novel combinatorial cancer treatments. Today, in fact, the use of pharmacological inhibitors of YAP/TAZ is still in the preclinical phase, while melatonin is used in clinic in combination with other traditional therapies. Studies in this new direction might be worth pursuing.
Acknowledgments
The work has been supported by Aboca and Associazione Aurora Tomaselli to Sabrina Strano, and by the ArceloMittal Dofasco Company to Paola Muti.
Author Contributions
Federica Lo Sardo wrote the manuscript; Paola Muti contributed to the introduction and the clinical aspects of melatonin and provided indication about the organization of the manuscript; Sabrina Strano and Giovanni Blandino supervised and corrected the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Acuna-Castroviejo D., Escames G., Venegas C., Diaz-Casado M.E., Lima-Cabello E., Lopez L.C., Rosales-Corral S., Tan D.X., Reiter R.J. Extrapineal melatonin: Sources, regulation, and potential functions. Cell. Mol. Life Sci. 2014;71:2997–3025. doi: 10.1007/s00018-014-1579-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dominguez-Solis C.A., Perez-Leon J.A. Phototransduction mediated by melanopsin in intrinsically photosensitive retinal ganglion cells. Gac. Med. Mex. 2015;151:764–776. [PubMed] [Google Scholar]
- 3.Berson D.M., Dunn F.A., Takao M. Phototransduction by retinal ganglion cells that set the circadian clock. Science. 2002;295:1070–1073. doi: 10.1126/science.1067262. [DOI] [PubMed] [Google Scholar]
- 4.Reiter R.J. The melatonin rhythm: Both a clock and a calendar. Experientia. 1993;49:654–664. doi: 10.1007/BF01923947. [DOI] [PubMed] [Google Scholar]
- 5.Hardeland R. Melatonin in aging and disease—Multiple consequences of reduced secretion, options and limits of treatment. Aging Dis. 2012;3:194–225. [PMC free article] [PubMed] [Google Scholar]
- 6.Karolczak M., Korf H.W., Stehle J.H. The rhythm and blues of gene expression in the rodent pineal gland. Endocrine. 2005;27:89–100. doi: 10.1385/ENDO:27:2:089. [DOI] [PubMed] [Google Scholar]
- 7.Klein D.C. Arylalkylamine N-acetyltransferase: “The timezyme”. J. Biol. Chem. 2007;282:4233–4237. doi: 10.1074/jbc.R600036200. [DOI] [PubMed] [Google Scholar]
- 8.Bernard M., Guerlotte J., Greve P., Grechez-Cassiau A., Iuvone M.P., Zatz M., Chong N.W., Klein D.C., Voisin P. Melatonin synthesis pathway: Circadian regulation of the genes encoding the key enzymes in the chicken pineal gland and retina. Reprod. Nutr. Dev. 1999;39:325–334. doi: 10.1051/rnd:19990305. [DOI] [PubMed] [Google Scholar]
- 9.Klein D.C., Moore R.Y. Pineal N-acetyltransferase and hydroxyindole-O-methyltransferase: Control by the retinohypothalamic tract and the suprachiasmatic nucleus. Brain Res. 1979;174:245–262. doi: 10.1016/0006-8993(79)90848-5. [DOI] [PubMed] [Google Scholar]
- 10.Gastel J.A., Roseboom P.H., Rinaldi P.A., Weller J.L., Klein D.C. Melatonin production: Proteasomal proteolysis in serotonin N-acetyltransferase regulation. Science. 1998;279:1358–1360. doi: 10.1126/science.279.5355.1358. [DOI] [PubMed] [Google Scholar]
- 11.Grof E., Grof P., Brown G.M., Arato M., Lane J. Investigations of melatonin secretion in man. Prog. Neuropsychopharmacol. Biol. Psychiatry. 1985;9:609–612. doi: 10.1016/0278-5846(85)90026-0. [DOI] [PubMed] [Google Scholar]
- 12.Graham C., Cook M.R., Kavet R., Sastre A., Smith D.K. Prediction of nocturnal plasma melatonin from morning urinary measures. J. Pineal Res. 1998;24:230–238. doi: 10.1111/j.1600-079X.1998.tb00538.x. [DOI] [PubMed] [Google Scholar]
- 13.Schernhammer E.S., Rosner B., Willett W.C., Laden F., Colditz G.A., Hankinson S.E. Epidemiology of urinary melatonin in women and its relation to other hormones and night work. Cancer Epidemiol. Biomark. Prev. 2004;13:936–943. [PubMed] [Google Scholar]
- 14.Reiter R.J., Tan D.X., Korkmaz A., Erren T.C., Piekarski C., Tamura H., Manchester L.C. Light at night, chronodisruption, melatonin suppression, and cancer risk: A review. Crit. Rev. Oncog. 2007;13:303–328. doi: 10.1615/CritRevOncog.v13.i4.30. [DOI] [PubMed] [Google Scholar]
- 15.Yang W.S., Deng Q., Fan W.Y., Wang W.Y., Wang X. Light exposure at night, sleep duration, melatonin, and breast cancer: A dose-response analysis of observational studies. Eur. J. Cancer Prev. 2014;23:269–276. doi: 10.1097/CEJ.0000000000000030. [DOI] [PubMed] [Google Scholar]
- 16.Basler M., Jetter A., Fink D., Seifert B., Kullak-Ublick G.A., Trojan A. Urinary excretion of melatonin and association with breast cancer: Meta-analysis and review of the literature. Breast Care. 2014;9:182–187. doi: 10.1159/000363426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shiu S.Y.W. Towards rational and evidence-based use of melatonin in prostate cancer prevention and treatment. J. Pineal Res. 2007;43:1–9. doi: 10.1111/j.1600-079X.2007.00451.x. [DOI] [PubMed] [Google Scholar]
- 18.Bartsch C., Bartsch H., Jain A.K., Laumas K.R., Wetterberg L. Urinary melatonin levels in human breast cancer patients. J. Neural Transm. 1981;52:281–294. doi: 10.1007/BF01256753. [DOI] [PubMed] [Google Scholar]
- 19.Tamarkin L., Danforth D., Lichter A., DeMoss E., Cohen M., Chabner B., Lippman M. Decreased nocturnal plasma melatonin peak in patients with estrogen receptor positive breast cancer. Science. 1982;216:1003–1005. doi: 10.1126/science.7079745. [DOI] [PubMed] [Google Scholar]
- 20.Schernhammer E.S., Berrino F., Krogh V., Secreto G., Micheli A., Venturelli E., Sieri S., Sempos C.T., Cavalleri A., Schunemann H.J., et al. Urinary 6-sulfatoxymelatonin levels and risk of breast cancer in postmenopausal women. J. Natl. Cancer Inst. 2008;100:898–905. doi: 10.1093/jnci/djn171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schernhammer E.S., Berrino F., Krogh V., Secreto G., Micheli A., Venturelli E., Grioni S., Sempos C.T., Cavalleri A., Schunemann H.J., et al. Urinary 6-sulphatoxymelatonin levels and risk of breast cancer in premenopausal women: The ordet cohort. Cancer Epidemiol. Biomark. Prev. 2010;19:729–737. doi: 10.1158/1055-9965.EPI-09-1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Devore E.E., Warner E.T., Eliassen A.H., Brown S.B., Beck A.H., Hankinson S.E., Schernhammer E.S. Urinary melatonin in relation to postmenopausal breast cancer risk according to melatonin 1 receptor status. Cancer Epidemiol. Biomark. Prev. 2017;26:413–419. doi: 10.1158/1055-9965.EPI-16-0630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang Y.M., Jin B.Z., Ai F., Duan C.H., Lu Y.Z., Dong T.F., Fu Q.L. The efficacy and safety of melatonin in concurrent chemotherapy or radiotherapy for solid tumors: A meta-analysis of randomized controlled trials. Cancer Chemother. Pharmacol. 2012;69:1213–1220. doi: 10.1007/s00280-012-1828-8. [DOI] [PubMed] [Google Scholar]
- 24.Seely D., Wu P., Fritz H., Kennedy D.A., Tsui T., Seely A.J., Mills E. Melatonin as adjuvant cancer care with and without chemotherapy: A systematic review and meta-analysis of randomized trials. Integr. Cancer Ther. 2012;11:293–303. doi: 10.1177/1534735411425484. [DOI] [PubMed] [Google Scholar]
- 25.Ernst E., Schmidt K., Baum M. Complementary/alternative therapies for the treatment of breast cancer. A systematic review of randomized clinical trials and a critique of current terminology. Breast J. 2006;12:526–530. doi: 10.1111/j.1524-4741.2006.00340.x. [DOI] [PubMed] [Google Scholar]
- 26.Armstrong S.M. Melatonin and circadian control in mammals. Experientia. 1989;45:932–938. doi: 10.1007/BF01953050. [DOI] [PubMed] [Google Scholar]
- 27.Comai S., Gobbi G. Unveiling the role of melatonin MT2 receptors in sleep, anxiety and other neuropsychiatric diseases: A novel target in psychopharmacology. J. Psychiatry Neurosci. 2014;39:6–21. doi: 10.1503/jpn.130009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fernando S., Rombauts L. Melatonin: Shedding light on infertility?—A review of the recent literature. J. Ovarian Res. 2014;7:98. doi: 10.1186/s13048-014-0098-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grossman E., Laudon M., Yalcin R., Zengil H., Peleg E., Sharabi Y., Kamari Y., Shen-Orr Z., Zisapel N. Melatonin reduces night blood pressure in patients with nocturnal hypertension. Am. J. Med. 2006;119:898–902. doi: 10.1016/j.amjmed.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 30.Korkmaz A., Reiter R.J., Topal T., Manchester L.C., Oter S., Tan D.X. Melatonin: An established antioxidant worthy of use in clinical trials. Mol. Med. 2009;15:43–50. doi: 10.2119/molmed.2008.00117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mathes A.M. Hepatoprotective actions of melatonin: Possible mediation by melatonin receptors. World J. Gastroenterol. 2010;16:6087–6097. doi: 10.3748/wjg.v16.i48.6087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moriya T., Horie N., Mitome M., Shinohara K. Melatonin influences the proliferative and differentiative activity of neural stem cells. J. Pineal Res. 2007;42:411–418. doi: 10.1111/j.1600-079X.2007.00435.x. [DOI] [PubMed] [Google Scholar]
- 33.Pandi-Perumal S.R., Trakht I., Srinivasan V., Spence D.W., Maestroni G.J., Zisapel N., Cardinali D.P. Physiological effects of melatonin: Role of melatonin receptors and signal transduction pathways. Prog. Neurobiol. 2008;85:335–353. doi: 10.1016/j.pneurobio.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 34.Strassman R.J., Qualls C.R., Lisansky E.J., Peake G.T. Elevated rectal temperature produced by all-night bright light is reversed by melatonin infusion in men. J. Appl. Physiol. 1991;71:2178–2182. doi: 10.1152/jappl.1991.71.6.2178. [DOI] [PubMed] [Google Scholar]
- 35.Touitou Y., Reinberg A., Touitou D. Association between light at night, melatonin secretion, sleep deprivation, and the internal clock: Health impacts and mechanisms of circadian disruption. Life Sci. 2017;173:94–106. doi: 10.1016/j.lfs.2017.02.008. [DOI] [PubMed] [Google Scholar]
- 36.Vriend J., Reiter R.J. Melatonin, bone regulation and the ubiquitin-proteasome connection: A review. Life Sci. 2016;145:152–160. doi: 10.1016/j.lfs.2015.12.031. [DOI] [PubMed] [Google Scholar]
- 37.Pavlos N.J., Friedman P.A. GPCR signaling and trafficking: The long and short of it. Trends Endocrinol. Metab. 2017;28:213–226. doi: 10.1016/j.tem.2016.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu J., Clough S.J., Hutchinson A.J., Adamah-Biassi E.B., Popovska-Gorevski M., Dubocovich M.L. MT1 and MT2 melatonin receptors: A therapeutic perspective. Annu. Rev. Pharmacol. Toxicol. 2016;56:361–383. doi: 10.1146/annurev-pharmtox-010814-124742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Legros C., Devavry S., Caignard S., Tessier C., Delagrange P., Ouvry C., Boutin J.A., Nosjean O. Melatonin MT(1) and MT(2) receptors display different molecular pharmacologies only in the G-protein coupled state. Br. J. Pharmacol. 2014;171:186–201. doi: 10.1111/bph.12457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jockers R., Delagrange P., Dubocovich M.L., Markus R.P., Renault N., Tosini G., Cecon E., Zlotos D.P. Update on melatonin receptors: Iuphar review 20. Br. J. Pharmacol. 2016;173:2702–2725. doi: 10.1111/bph.13536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nosjean O., Ferro M., Coge F., Beauverger P., Henlin J.M., Lefoulon F., Fauchere J.L., Delagrange P., Canet E., Boutin J.A. Identification of the melatonin-binding site MT3 as the quinone reductase 2. J. Biol. Chem. 2000;275:31311–31317. doi: 10.1074/jbc.M005141200. [DOI] [PubMed] [Google Scholar]
- 42.Boutin J.A. Quinone reductase 2 as a promising target of melatonin therapeutic actions. Expert Opin. Ther. Targets. 2016;20:303–317. doi: 10.1517/14728222.2016.1091882. [DOI] [PubMed] [Google Scholar]
- 43.Wettschureck N., Offermanns S. Mammalian g proteins and their cell type specific functions. Physiol. Rev. 2005;85:1159–1204. doi: 10.1152/physrev.00003.2005. [DOI] [PubMed] [Google Scholar]
- 44.Strathmann M., Wilkie T.M., Simon M.I. Diversity of the G-protein family: Sequences from five additional α subunits in the mouse. Proc. Natl. Acad. Sci. USA. 1989;86:7407–7409. doi: 10.1073/pnas.86.19.7407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Birnbaumer L. Receptor-to-effector signaling through g proteins: Roles for β γ dimers as well as α subunits. Cell. 1992;71:1069–1072. doi: 10.1016/S0092-8674(05)80056-X. [DOI] [PubMed] [Google Scholar]
- 46.Reppert S.M., Weaver D.R., Godson C. Melatonin receptors step into the light: Cloning and classification of subtypes. Trends Pharmacol. Sci. 1996;17:100–102. doi: 10.1016/0165-6147(96)10005-5. [DOI] [PubMed] [Google Scholar]
- 47.Masana M.I., Dubocovich M.L. Melatonin receptor signaling: Finding the path through the dark. Sci. STKE. 2001;2001:pe39. doi: 10.1126/stke.2001.107.pe39. [DOI] [PubMed] [Google Scholar]
- 48.Brydon L., Roka F., Petit L., de Coppet P., Tissot M., Barrett P., Morgan P.J., Nanoff C., Strosberg A.D., Jockers R. Dual signaling of human Mel1a melatonin receptors via G(i2), G(i3), and G(q/11) proteins. Mol. Endocrinol. 1999;13:2025–2038. doi: 10.1210/mend.13.12.0390. [DOI] [PubMed] [Google Scholar]
- 49.Brydon L., Petit L., de Coppet P., Barrett P., Morgan P.J., Strosberg A.D., Jockers R. Polymorphism and signalling of melatonin receptors. Reprod. Nutr. Dev. 1999;39:315–324. doi: 10.1051/rnd:19990304. [DOI] [PubMed] [Google Scholar]
- 50.Jarzynka M.J., Passey D.K., Ignatius P.F., Melan M.A., Radio N.M., Jockers R., Rasenick M.M., Brydon L., Witt-Enderby P.A. Modulation of melatonin receptors and G-protein function by microtubules. J. Pineal Res. 2006;41:324–336. doi: 10.1111/j.1600-079X.2006.00371.x. [DOI] [PubMed] [Google Scholar]
- 51.Lai L., Yuan L., Chen Q., Dong C., Mao L., Rowan B., Frasch T., Hill S.M. The Gα and Gαq proteins mediate the effects of melatonin on steroid/thyroid hormone receptor transcriptional activity and breast cancer cell proliferation. J. Pineal Res. 2008;45:476–488. doi: 10.1111/j.1600-079X.2008.00620.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.New D.C., Tsim S.T., Wong Y.H. G protein-linked effector and second messenger systems involved in melatonin signal transduction. Neurosignals. 2003;12:59–70. doi: 10.1159/000071815. [DOI] [PubMed] [Google Scholar]
- 53.Shiu S.Y.W., Pang B., Tam C.W., Yao K.M. Signal transduction of receptor-mediated antiproliferative action of melatonin on human prostate epithelial cells involves dual activation of Gα(s) and Gα(q) proteins. J. Pineal Res. 2010;49:301–311. doi: 10.1111/j.1600-079X.2010.00795.x. [DOI] [PubMed] [Google Scholar]
- 54.Tam C.W., Shiu S.Y.W. Functional interplay between melatonin receptor-mediated antiproliferative signaling and androgen receptor signaling in human prostate epithelial cells: Potential implications for therapeutic strategies against prostate cancer. J. Pineal Res. 2011;51:297–312. doi: 10.1111/j.1600-079X.2011.00890.x. [DOI] [PubMed] [Google Scholar]
- 55.Shiu S.Y., Leung W.Y., Tam C.W., Liu V.W., Yao K.M. Melatonin MT1 receptor-induced transcriptional up-regulation of p27(KIP1) in prostate cancer antiproliferation is mediated via inhibition of constitutively active nuclear factor κ B (NF-κB): Potential implications on prostate cancer chemoprevention and therapy. J. Pineal Res. 2013;54:69–79. doi: 10.1111/j.1600-079X.2012.01026.x. [DOI] [PubMed] [Google Scholar]
- 56.Hardeland R. Melatonin: Signaling mechanisms of a pleiotropic agent. Biofactors. 2009;35:183–192. doi: 10.1002/biof.23. [DOI] [PubMed] [Google Scholar]
- 57.Ho M.K., Yung L.Y., Chan J.S., Chan J.H., Wong C.S., Wong Y.H. Gα(14) links a variety of G(i)- and G(s)-coupled receptors to the stimulation of phospholipase c. Br. J. Pharmacol. 2001;132:1431–1440. doi: 10.1038/sj.bjp.0703933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McNulty S., Ross A.W., Barrett P., Hastings M.H., Morgan P.J. Melatonin regulates the phosphorylation of CREB in ovine pars tuberalis. J. Neuroendocrinol. 1994;6:523–532. doi: 10.1111/j.1365-2826.1994.tb00615.x. [DOI] [PubMed] [Google Scholar]
- 59.Niles L.P., Hashemi F. Picomolar-affinity binding and inhibition of adenylate cyclase activity by melatonin in syrian hamster hypothalamus. Cell. Mol. Neurobiol. 1990;10:553–558. doi: 10.1007/BF00712848. [DOI] [PubMed] [Google Scholar]
- 60.Morgan P.J., Barrett P., Howell H.E., Helliwell R. Melatonin receptors: Localization, molecular pharmacology and physiological significance. Neurochem. Int. 1994;24:101–146. doi: 10.1016/0197-0186(94)90100-7. [DOI] [PubMed] [Google Scholar]
- 61.Witt-Enderby P.A., MacKenzie R.S., McKeon R.M., Carroll E.A., Bordt S.L., Melan M.A. Melatonin induction of filamentous structures in non-neuronal cells that is dependent on expression of the human mt1 melatonin receptor. Cell Motil. Cytoskelet. 2000;46:28–42. doi: 10.1002/(SICI)1097-0169(200005)46:1<28::AID-CM4>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 62.Godson C., Reppert S.M. The Mel1a melatonin receptor is coupled to parallel signal transduction pathways 1. Endocrinology. 1997;138:397–404. doi: 10.1210/endo.138.1.4824. [DOI] [PubMed] [Google Scholar]
- 63.Roka F., Brydon L., Waldhoer M., Strosberg A.D., Freissmuth M., Jockers R., Nanoff C. Tight association of the human Mel(1a)-melatonin receptor and G(i): Precoupling and constitutive activity. Mol. Pharmacol. 1999;56:1014–1024. doi: 10.1124/mol.56.5.1014. [DOI] [PubMed] [Google Scholar]
- 64.Wan Q., Man H.Y., Liu F., Braunton J., Niznik H.B., Pang S.F., Brown G.M., Wang Y.T. Differential modulation of GABAA receptor function by Mel1a and Mel1b receptors. Nat. Neurosci. 1999;2:401–403. doi: 10.1038/8062. [DOI] [PubMed] [Google Scholar]
- 65.Liu V.W.S., Yau W.L., Tam C.W., Yao K.M., Shiu S.Y.W. Melatonin inhibits androgen receptor splice variant-7 (ar-v7)-induced nuclear factor-kappa b (nf-kappab) activation and nf-kappab activator-induced ar-v7 expression in prostate cancer cells: Potential implications for the use of melatonin in castration-resistant prostate cancer (crpc) therapy. Int. J. Mol. Sci. 2017;18 doi: 10.3390/ijms18061130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tam C.W., Mo C.W., Yao K.M., Shiu S.Y.W. Signaling mechanisms of melatonin in antiproliferation of hormone-refractory 22RV1 human prostate cancer cells: Implications for prostate cancer chemoprevention. J. Pineal Res. 2007;42:191–202. doi: 10.1111/j.1600-079X.2006.00406.x. [DOI] [PubMed] [Google Scholar]
- 67.Tam C.W., Chan K.W., Liu V.W.S., Pang B., Yao K.M., Shiu S.Y.W. Melatonin as a negative mitogenic hormonal regulator of human prostate epithelial cell growth: Potential mechanisms and clinical significance. J. Pineal Res. 2008;45:403–412. doi: 10.1111/j.1600-079X.2008.00608.x. [DOI] [PubMed] [Google Scholar]
- 68.Chan A.S., Lai F.P., Lo R.K., Voyno-Yasenetskaya T.A., Stanbridge E.J., Wong Y.H. Melatonin MT1 and MT2 receptors stimulate c-jun N-terminal kinase via pertussis toxin-sensitive and -insensitive G proteins. Cell Signal. 2002;14:249–257. doi: 10.1016/S0898-6568(01)00240-6. [DOI] [PubMed] [Google Scholar]
- 69.Chen L., He X., Zhang Y., Chen X., Lai X., Shao J., Shi Y., Zhou N. Melatonin receptor type 1 signals to extracellular signal-regulated kinase 1 and 2 via Gi and Gs dually coupled pathways in Hek-293 cells. Biochemistry. 2014;53:2827–2839. doi: 10.1021/bi500092e. [DOI] [PubMed] [Google Scholar]
- 70.Becker-Andre M., Wiesenberg I., Schaeren-Wiemers N., Andre E., Missbach M., Saurat J.H., Carlberg C. Pineal gland hormone melatonin binds and activates an orphan of the nuclear receptor superfamily. J. Biol. Chem. 1994;269:28531–28534. doi: 10.1074/jbc.272.26.16707. [DOI] [PubMed] [Google Scholar]
- 71.Carlberg C., Wiesenberg I. The orphan receptor family RZR/ROR, melatonin and 5-lipoxygenase: An unexpected relationship. J. Pineal Res. 1995;18:171–178. doi: 10.1111/j.1600-079X.1995.tb00157.x. [DOI] [PubMed] [Google Scholar]
- 72.Wiesenberg I., Missbach M., Kahlen J.P., Schrader M., Carlberg C. Transcriptional activation of the nuclear receptor RZR α by the pineal gland hormone melatonin and identification of CGP 52608 as a synthetic ligand. Nucleic Acids Res. 1995;23:327–333. doi: 10.1093/nar/23.3.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wiesenberg I., Missbach M., Carlberg C. The potential role of the transcription factor RZR/ROR as a mediator of nuclear melatonin signaling. Restor. Neurol. Neurosci. 1998;12:143–150. [PubMed] [Google Scholar]
- 74.Acuna-Castroviejo D., Reiter R.J., Menendez-Pelaez A., Pablos M.I., Burgos A. Characterization of high-affinity melatonin binding sites in purified cell nuclei of rat liver. J. Pineal Res. 1994;16:100–112. doi: 10.1111/j.1600-079X.1994.tb00089.x. [DOI] [PubMed] [Google Scholar]
- 75.Zhang Y., Luo X.Y., Wu D.H., Xu Y. ROR nuclear receptors: Structures, related diseases, and drug discovery. Acta Pharmacol. Sin. 2015;36:71–87. doi: 10.1038/aps.2014.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Giguere V., McBroom L.D., Flock G. Determinants of target gene specificity for RORα1: Monomeric DNA binding by an orphan nuclear receptor. Mol. Cell. Biol. 1995;15:2517–2526. doi: 10.1128/MCB.15.5.2517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Giguere V., Tini M., Flock G., Ong E., Evans R.M., Otulakowski G. Isoform-specific amino-terminal domains dictate DNA-binding properties of RORα, a novel family of orphan hormone nuclear receptors. Genes Dev. 1994;8:538–553. doi: 10.1101/gad.8.5.538. [DOI] [PubMed] [Google Scholar]
- 78.Medvedev A., Yan Z.H., Hirose T., Giguere V., Jetten A.M. Cloning of a cDNA encoding the murine orphan receptor RZR/ROR γ and characterization of its response element. Gene. 1996;181:199–206. doi: 10.1016/S0378-1119(96)00504-5. [DOI] [PubMed] [Google Scholar]
- 79.Schrader M., Danielsson C., Wiesenberg I., Carlberg C. Identification of natural monomeric response elements of the nuclear receptor RZR/ROR. They also bind coup-TF homodimers. J. Biol. Chem. 1996;271:19732–19736. doi: 10.1074/jbc.271.33.19732. [DOI] [PubMed] [Google Scholar]
- 80.Winrow C.J., Capone J.P., Rachubinski R.A. Cross-talk between orphan nuclear hormone receptor RZRα and peroxisome proliferator-activated receptor α in regulation of the peroxisomal hydratase-dehydrogenase gene. J. Biol. Chem. 1998;273:31442–31448. doi: 10.1074/jbc.273.47.31442. [DOI] [PubMed] [Google Scholar]
- 81.Karasek M., Carrillo-Vico A., Guerrero J.M., Winczyk K., Pawlikowski M. Expression of melatonin MT(1) and MT(2) receptors, and RORα(1) receptor in transplantable murine colon 38 cancer. Neuro Endocrinol. Lett. 2002;23(Suppl. 1):55–60. [PubMed] [Google Scholar]
- 82.Winczyk K., Pawlikowski M., Guerrero J.M., Karasek M. Possible involvement of the nuclear RZR/ROR-α receptor in the antitumor action of melatonin on murine colon 38 cancer. Tumour Biol. 2002;23:298–302. doi: 10.1159/000068569. [DOI] [PubMed] [Google Scholar]
- 83.Garcia-Maurino S., Pozo D., Calvo J.R., Guerrero J.M. Correlation between nuclear melatonin receptor expression and enhanced cytokine production in human lymphocytic and monocytic cell lines. J. Pineal Res. 2000;29:129–137. doi: 10.1034/j.1600-079X.2000.290301.x. [DOI] [PubMed] [Google Scholar]
- 84.Guerrero J.M., Pozo D., Garcia-Maurino S., Osuna C., Molinero P., Calvo J.R. Involvement of nuclear receptors in the enhanced IL-2 production by melatonin in jurkat cells. Ann. N. Y. Acad Sci. 2000;917:397–403. doi: 10.1111/j.1749-6632.2000.tb05404.x. [DOI] [PubMed] [Google Scholar]
- 85.Guerrero J.M., Pozo D., Garcia-Maurino S., Carrillo A., Osuna C., Molinero P., Calvo J.R. Nuclear receptors are involved in the enhanced IL-6 production by melatonin in u937 cells. Biol. Signals Recept. 2000;9:197–202. doi: 10.1159/000014639. [DOI] [PubMed] [Google Scholar]
- 86.Tang X.H., Gudas L.J. Retinoids, retinoic acid receptors, and cancer. Annu. Rev. Pathol. 2011;6:345–364. doi: 10.1146/annurev-pathol-011110-130303. [DOI] [PubMed] [Google Scholar]
- 87.Steinhilber D., Brungs M., Werz O., Wiesenberg I., Danielsson C., Kahlen J.P., Nayeri S., Schrader M., Carlberg C. The nuclear receptor for melatonin represses 5-lipoxygenase gene expression in human b lymphocytes. J. Biol. Chem. 1995;270:7037–7040. doi: 10.1074/jbc.270.13.7037. [DOI] [PubMed] [Google Scholar]
- 88.Dai J., Ram P.T., Yuan L., Spriggs L.L., Hill S.M. Transcriptional repression of RORα activity in human breast cancer cells by melatonin. Mol. Cell. Endocrinol. 2001;176:111–120. doi: 10.1016/S0303-7207(01)00449-X. [DOI] [PubMed] [Google Scholar]
- 89.Dong C., Yuan L., Dai J., Lai L., Mao L., Xiang S., Rowan B., Hill S.M. Melatonin inhibits mitogenic cross-talk between retinoic acid-related orphan receptor α (RORα) and ERα in MCF-7 human breast cancer cells. Steroids. 2010;75:944–951. doi: 10.1016/j.steroids.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 90.Wang R.X., Liu H., Xu L., Zhang H., Zhou R.X. Melatonin downregulates nuclear receptor RZR/RORγ expression causing growth-inhibitory and anti-angiogenesis activity in human gastric cancer cells in vitro and in vivo. Oncol. Lett. 2016;12:897–903. doi: 10.3892/ol.2016.4729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Reiter R.J., Rosales-Corral S.A., Tan D.X., Acuna-Castroviejo D., Qin L., Yang S.F., Xu K. Melatonin, a full service anti-cancer agent: Inhibition of initiation, progression and metastasis. Int. J. Mol. Sci. 2017;18:E843. doi: 10.3390/ijms18040843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chuffa L.G.A., Reiter R.J., Lupi Junior L.A. Melatonin as a promising agent to treat ovarian cancer: Molecular mechanisms. Carcinogenesis. 2017 doi: 10.1093/carcin/bgx054. [DOI] [PubMed] [Google Scholar]
- 93.Li W., Fan M., Chen Y., Zhao Q., Song C., Yan Y., Jin Y., Huang Z., Lin C., Wu J. Melatonin induces cell apoptosis in ags cells through the activation of jnk and p38 mapk and the suppression of nuclear factor-κB: A novel therapeutic implication for gastric cancer. Cell. Physiol. Biochem. 2015;37:2323–2338. doi: 10.1159/000438587. [DOI] [PubMed] [Google Scholar]
- 94.Kim C.H., Yoo Y.M. Melatonin induces apoptotic cell death via p53 in lncap cells. Korean J. Physiol. Pharmacol. 2010;14:365–369. doi: 10.4196/kjpp.2010.14.6.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Li W., Wu J., Li Z., Zhou Z., Zheng C., Lin L., Tan B., Huang M., Fan M. Melatonin induces cell apoptosis in mia PACA-2 cells via the suppression of nuclear factor-κB and activation of ERK and JNK: A novel therapeutic implication for pancreatic cancer. Oncol. Rep. 2016;36:2861–2867. doi: 10.3892/or.2016.5100. [DOI] [PubMed] [Google Scholar]
- 96.Cabrera J., Negrin G., Estevez F., Loro J., Reiter R.J., Quintana J. Melatonin decreases cell proliferation and induces melanogenesis in human melanoma SK-Mel-1 cells. J. Pineal Res. 2010;49:45–54. doi: 10.1111/j.1600-079X.2010.00765.x. [DOI] [PubMed] [Google Scholar]
- 97.Carbajo-Pescador S., Garcia-Palomo A., Martin-Renedo J., Piva M., Gonzalez-Gallego J., Mauriz J.L. Melatonin modulation of intracellular signaling pathways in hepatocarcinoma HEPG2 cell line: Role of the MT1 receptor. J. Pineal Res. 2011;51:463–471. doi: 10.1111/j.1600-079X.2011.00910.x. [DOI] [PubMed] [Google Scholar]
- 98.Santoro R., Marani M., Blandino G., Muti P., Strano S. Melatonin triggers p53Ser phosphorylation and prevents DNA damage accumulation. Oncogene. 2012;31:2931–2942. doi: 10.1038/onc.2011.469. [DOI] [PubMed] [Google Scholar]
- 99.Santoro R., Mori F., Marani M., Grasso G., Cambria M.A., Blandino G., Muti P., Strano S. Blockage of melatonin receptors impairs p53-mediated prevention of DNA damage accumulation. Carcinogenesis. 2013;34:1051–1061. doi: 10.1093/carcin/bgt025. [DOI] [PubMed] [Google Scholar]
- 100.Mori F., Ferraiuolo M., Santoro R., Sacconi A., Goeman F., Pallocca M., Pulito C., Korita E., Fanciulli M., Muti P., et al. Multitargeting activity of MIR-24 inhibits long-term melatonin anticancer effects. Oncotarget. 2016;7:20532–20548. doi: 10.18632/oncotarget.7978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gao Y., Xiao X., Zhang C., Yu W., Guo W., Zhang Z., Li Z., Feng X., Hao J., Zhang K., et al. Melatonin synergizes the chemotherapeutic effect of 5-fluorouracil in colon cancer by suppressing pi3k/AKT and Nf-κB/INOS signaling pathways. J. Pineal Res. 2017;62 doi: 10.1111/jpi.12380. [DOI] [PubMed] [Google Scholar]
- 102.Lu J.J., Fu L., Tang Z., Zhang C., Qin L., Wang J., Yu Z., Shi D., Xiao X., Xie F., et al. Melatonin inhibits AP-2β/HTERT, NF-κB/Cox-2 and AKT/ERK and activates caspase/cyto c signaling to enhance the antitumor activity of berberine in lung cancer cells. Oncotarget. 2016;7:2985–3001. doi: 10.18632/oncotarget.6407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ju H.Q., Li H., Tian T., Lu Y.X., Bai L., Chen L.Z., Sheng H., Mo H.Y., Zeng J.B., Deng W., et al. Melatonin overcomes gemcitabine resistance in pancreatic ductal adenocarcinoma by abrogating nuclear factor-κB activation. J. Pineal Res. 2016;60:27–38. doi: 10.1111/jpi.12285. [DOI] [PubMed] [Google Scholar]
- 104.Lin Y.W., Lee L.M., Lee W.J., Chu C.Y., Tan P., Yang Y.C., Chen W.Y., Yang S.F., Hsiao M., Chien M.H. Melatonin inhibits MMP-9 transactivation and renal cell carcinoma metastasis by suppressing AKT-MAPKS pathway and NF-κB DNA-binding activity. J. Pineal Res. 2016;60:277–290. doi: 10.1111/jpi.12308. [DOI] [PubMed] [Google Scholar]
- 105.Chen X., Hao A., Li X., Du Z., Li H., Wang H., Yang H., Fang Z. Melatonin inhibits tumorigenicity of glioblastoma stem-like cells via the AKT-EZH2-STAT3 signaling axis. J. Pineal Res. 2016;61:208–217. doi: 10.1111/jpi.12341. [DOI] [PubMed] [Google Scholar]
- 106.Zheng X., Pang B., Gu G., Gao T., Zhang R., Pang Q., Liu Q. Melatonin inhibits glioblastoma stem-like cells through suppression of EZH2-notch1 signaling axis. Int. J. Biol. Sci. 2017;13:245–253. doi: 10.7150/ijbs.16818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Liu L., Xu Y., Reiter R.J., Pan Y., Chen D., Liu Y., Pu X., Jiang L., Li Z. Inhibition of ERK1/2 signaling pathway is involved in melatonin’s antiproliferative effect on human MG-63 osteosarcoma cells. Cell. Physiol. Biochem. 2016;39:2297–2307. doi: 10.1159/000447922. [DOI] [PubMed] [Google Scholar]
- 108.Konakchieva R., Todorov P. Melatonin protects human spermatozoa from apoptosis via melatonin receptor- and extracellular signal-regulated kinase-mediated pathways. Fertil. Steril. 2011;96:e159. doi: 10.1016/j.fertnstert.2011.08.013. [DOI] [PubMed] [Google Scholar]
- 109.Molpeceres V., Mauriz J.L., Garcia-Mediavilla M.V., Gonzalez P., Barrio J.P., Gonzalez-Gallego J. Melatonin is able to reduce the apoptotic liver changes induced by aging via inhibition of the intrinsic pathway of apoptosis. J. Gerontol. A Biol. Sci. Med. Sci. 2007;62:687–695. doi: 10.1093/gerona/62.7.687. [DOI] [PubMed] [Google Scholar]
- 110.Wang X. The antiapoptotic activity of melatonin in neurodegenerative diseases. CNS Neurosci. Ther. 2009;15:345–357. doi: 10.1111/j.1755-5949.2009.00105.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ren W., Liu G., Chen S., Yin J., Wang J., Tan B., Wu G., Bazer F.W., Peng Y., Li T., et al. Melatonin signaling in T cells: Functions and applications. J. Pineal Res. 2017;62 doi: 10.1111/jpi.12394. [DOI] [PubMed] [Google Scholar]
- 112.GarciaMaurino S., GonzalezHaba M.G., Calvo J.R., RafiiElIdrissi M., SanchezMargalet V., Goberna R., Guerrero J.M. Melatonin enhances IL-2, IL-6, and IFN-γ production by human circulating CD4(+) cells—A possible nuclear receptor-mediated mechanism involving T helper type 1 lymphocytes and monocytes. J. Immunol. 1997;159:574–581. [PubMed] [Google Scholar]
- 113.Lardone P.J., Carrillo-Vico A., Naranjo M.C., de Felipe B., Vallejo A., Karasek M., Guerrero J.M. Melatonin synthesized by jurkat human leukemic T cell line is implicated in IL-2 production. J. Cell. Physiol. 2006;206:273–279. doi: 10.1002/jcp.20461. [DOI] [PubMed] [Google Scholar]
- 114.Ha E., Han E., Park H.J., Kim H.J., Hong M.S., Hong S.J., Yoon K.S., Kang I., Cho Y.H., Chung J.H., et al. Microarray analysis of transcription factor gene expression in melatonin-treated human peripheral blood mononuclear cells. J. Pineal Res. 2006;40:305–311. doi: 10.1111/j.1600-079X.2006.00317.x. [DOI] [PubMed] [Google Scholar]
- 115.Calvo J.R., Gonzalez-Yanes C., Maldonado M.D. The role of melatonin in the cells of the innate immunity: A review. J. Pineal Res. 2013;55:103–120. doi: 10.1111/jpi.12075. [DOI] [PubMed] [Google Scholar]
- 116.Lardone P.J., Carrillo-Vico A., Molinero P., Rubio A., Guerrero J.M. A novel interplay between membrane and nuclear melatonin receptors in human lymphocytes: Significance in IL-2 production. Cell. Mol. Life Sci. 2009;66:516–525. doi: 10.1007/s00018-008-8601-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Carrillo-Vico A., Lardone P.J., Alvarez-Sanchez N., Rodriguez-Rodriguez A., Guerrero J.M. Melatonin: Buffering the immune system. Int. J. Mol. Sci. 2013;14:8638–8683. doi: 10.3390/ijms14048638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Currier N.L., Sun L.Z.Y., Miller S.C. Exogenous melatonin: Quantitative enhancement in vivo of cells mediating non-specific immunity. J. Neuroimmunol. 2000;104:101–108. doi: 10.1016/S0165-5728(99)00271-4. [DOI] [PubMed] [Google Scholar]
- 119.Vigore L., Messina G., Brivio F., Fumagalli L., Rovelli F., G D.I.F., Lissoni P. Psychoneuroendocrine modulation of regulatory T lymphocyte system: In vivo and in vitro effects of the pineal immunomodulating hormone melatonin. In Vivo. 2010;24:787–789. [PubMed] [Google Scholar]
- 120.Liu H., Xu L., Wei J.E., Xie M.R., Wang S.E., Zhou R.X. Role of CD4+ CD25+ regulatory T cells in melatonin-mediated inhibition of murine gastric cancer cell growth in vivo and in vitro. Anat. Rec. 2011;294:781–788. doi: 10.1002/ar.21361. [DOI] [PubMed] [Google Scholar]
- 121.Knutson K.L., Disis M.L., Salazar L.G. CD4 regulatory T cells in human cancer pathogenesis. Cancer Immunol. Immunother. 2007;56:271–285. doi: 10.1007/s00262-006-0194-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Cos S., Fernandez R., Guezmes A., Sanchez-Barcelo E.J. Influence of melatonin on invasive and metastatic properties of MCF-7 human breast cancer cells. Cancer Res. 1998;58:4383–4390. [PubMed] [Google Scholar]
- 123.Wu S.M., Lin W.Y., Shen C.C., Pan H.C., Keh-Bin W., Chen Y.C., Jan Y.J., Lai D.W., Tang S.C., Tien H.R., et al. Melatonin set out to ER stress signaling thwarts epithelial mesenchymal transition and peritoneal dissemination via calpain-mediated c/EBPβ and NFκB cleavage. J. Pineal Res. 2016;60:142–154. doi: 10.1111/jpi.12295. [DOI] [PubMed] [Google Scholar]
- 124.Goncalves Ndo N., Colombo J., Lopes J.R., Gelaleti G.B., Moschetta M.G., Sonehara N.M., Hellmen E., Zanon Cde F., Oliani S.M., Zuccari D.A. Effect of melatonin in epithelial mesenchymal transition markers and invasive properties of breast cancer stem cells of canine and human cell lines. PLoS ONE. 2016;11:e0150407. doi: 10.1371/journal.pone.0150407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Zhou Q., Gui S., Zhou Q., Wang Y. Melatonin inhibits the migration of human lung adenocarcinoma a549 cell lines involving JNK/MAPK pathway. PLoS ONE. 2014;9:e101132. doi: 10.1371/journal.pone.0101132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Borin T.F., Arbab A.S., Gelaleti G.B., Ferreira L.C., Moschetta M.G., Jardim-Perassi B.V., Iskander A.S., Varma N.R., Shankar A., Coimbra V.B., et al. Melatonin decreases breast cancer metastasis by modulating rho-associated kinase protein-1 expression. J. Pineal Res. 2016;60:3–15. doi: 10.1111/jpi.12270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Goncalves Ndo N., Rodrigues R.V., Jardim-Perassi B.V., Moschetta M.G., Lopes J.R., Colombo J., Zuccari D.A. Molecular markers of angiogenesis and metastasis in lines of oral carcinoma after treatment with melatonin. Anticancer Agents Med. Chem. 2014;14:1302–1311. doi: 10.2174/1871520614666140812110246. [DOI] [PubMed] [Google Scholar]
- 128.Lopes J., Arnosti D., Trosko J.E., Tai M.H., Zuccari D. Melatonin decreases estrogen receptor binding to estrogen response elements sites on the OCT4 gene in human breast cancer stem cells. Genes Cancer. 2016;7:209–217. doi: 10.18632/genesandcancer.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lopes J.R., da Silva Kavagutti M., Medeiros F.A., De Campos Zuccari D.A. Evaluation of melatonin effect on human breast cancer stem cells using a three-dimensional growth method of mammospheres. Anticancer Agents Med. Chem. 2016 doi: 10.2174/1871520616666160923093229. [DOI] [PubMed] [Google Scholar]
- 130.Nooshinfar E., Bashash D., Safaroghli-Azar A., Bayati S., Rezaei-Tavirani M., Ghaffari S.H., Akbari M.E. Melatonin promotes ATO-induced apoptosis in MCF-7 cells: Proposing novel therapeutic potential for breast cancer. Biomed. Pharmacother. 2016;83:456–465. doi: 10.1016/j.biopha.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 131.Lu Y.X., Chen D.L., Wang D.S., Chen L.Z., Mo H.Y., Sheng H., Bai L., Wu Q.N., Yu H.E., Xie D., et al. Melatonin enhances sensitivity to fluorouracil in oesophageal squamous cell carcinoma through inhibition of ERK and AKT pathway. Cell Death Dis. 2016;7:e2432. doi: 10.1038/cddis.2016.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Zhelev Z., Ivanova D., Bakalova R., Aoki I., Higashi T. Synergistic cytotoxicity of melatonin and new-generation anticancer drugs against leukemia lymphocytes but not normal lymphocytes. Anticancer Res. 2017;37:149–159. doi: 10.21873/anticanres.11300. [DOI] [PubMed] [Google Scholar]
- 133.Wang Y.P., Yang Z.P. Effects of melatonin combined with cis-platinum or methotrexate on the proliferation of osteosarcoma cell line SAOS-2. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2015;37:215–220. doi: 10.3881/j.issn.1000-503X.2015.02.013. [DOI] [PubMed] [Google Scholar]
- 134.Fan L., Sun G., Ma T., Zhong F., Lei Y., Li X., Wei W. Melatonin reverses tunicamycin-induced endoplasmic reticulum stress in human hepatocellular carcinoma cells and improves cytotoxic response to doxorubicin by increasing chop and decreasing survivin. J. Pineal Res. 2013;55:184–194. doi: 10.1111/jpi.12061. [DOI] [PubMed] [Google Scholar]
- 135.Maschio-Signorini L.B., Gelaleti G.B., Moschetta M.G., Borin T.F., Jardim-Perassi B.V., Lopes J.R., Lacerda J.Z., Roela R.A., Bordin N.A., Correa L.A., et al. Melatonin regulates angiogenic and inflammatory proteins in MDA-MB-231 cell line and in co-culture with cancer-associated fibroblasts. Anticancer Agents Med. Chem. 2016;16:1474–1484. doi: 10.2174/1871520616666160422105920. [DOI] [PubMed] [Google Scholar]
- 136.Park S.Y., Jang W.J., Yi E.Y., Jang J.Y., Jung Y., Jeong J.W., Kim Y.J. Melatonin suppresses tumor angiogenesis by inhibiting Hif-1α stabilization under hypoxia. J. Pineal Res. 2010;48:178–184. doi: 10.1111/j.1600-079X.2009.00742.x. [DOI] [PubMed] [Google Scholar]
- 137.Cui P., Yu M., Peng X., Dong L., Yang Z. Melatonin prevents human pancreatic carcinoma cell PANC-1-induced human umbilical vein endothelial cell proliferation and migration by inhibiting vascular endothelial growth factor expression. J. Pineal Res. 2012;52:236–243. doi: 10.1111/j.1600-079X.2011.00933.x. [DOI] [PubMed] [Google Scholar]
- 138.Dai M., Cui P., Yu M., Han J., Li H., Xiu R. Melatonin modulates the expression of VEGF and Hif-1α induced by COCL2 in cultured cancer cells. J. Pineal Res. 2008;44:121–126. doi: 10.1111/j.1600-079X.2007.00498.x. [DOI] [PubMed] [Google Scholar]
- 139.Lv D., Cui P.L., Yao S.W., Xu Y.Q., Yang Z.X. Melatonin inhibits the expression of vascular endothelial growth factor in pancreatic cancer cells. Chin. J. Cancer Res. 2012;24:310–316. doi: 10.1007/s11670-012-0269-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Gonzalez A., Gonzalez-Gonzalez A., Alonso-Gonzalez C., Menendez-Menendez J., Martinez-Campa C., Cos S. Melatonin inhibits angiogenesis in SH-SY5Y human neuroblastoma cells by downregulation of VEGF. Oncol. Rep. 2017;37:2433–2440. doi: 10.3892/or.2017.5446. [DOI] [PubMed] [Google Scholar]
- 141.Carbajo-Pescador S., Ordonez R., Benet M., Jover R., Garcia-Palomo A., Mauriz J.L., Gonzalez-Gallego J. Inhibition of VEGF expression through blockade of Hif1α and STAT3 signalling mediates the anti-angiogenic effect of melatonin in HEPG2 liver cancer cells. Br. J. Cancer. 2013;109:83–91. doi: 10.1038/bjc.2013.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Jardim-Perassi B.V., Lourenco M.R., Doho G.M., Grigolo I.H., Gelaleti G.B., Ferreira L.C., Borin T.F., Moschetta M.G., Pires de Campos Zuccari D.A. Melatonin regulates angiogenic factors under hypoxia in breast cancer cell lines. Anticancer Agents Med. Chem. 2016;16:347–358. doi: 10.2174/1871520615666150511094201. [DOI] [PubMed] [Google Scholar]
- 143.Jardim-Perassi B.V., Arbab A.S., Ferreira L.C., Borin T.F., Varma N.R., Iskander A.S., Shankar A., Ali M.M., Pires de Campos Zuccari D.A. Effect of melatonin on tumor growth and angiogenesis in xenograft model of breast cancer. PLoS ONE. 2014;9:e85311. doi: 10.1371/journal.pone.0085311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Alvarez-Garcia V., Gonzalez A., Alonso-Gonzalez C., Martinez-Campa C., Cos S. Antiangiogenic effects of melatonin in endothelial cell cultures. Microvasc. Res. 2013;87:25–33. doi: 10.1016/j.mvr.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 145.Akbarzadeh M., Rahbarghazi R., Nabat E., Movassaghpour A.A., Shanehbandi D., Faramarzian Azimi Maragheh B., Matluobi D., Barazvan B., Kazemi M., Samadi N., et al. The impact of different extracellular matrices on melatonin effect in proliferation and stemness properties of ovarian cancer cells. Biomed. Pharmacother. 2017;87:288–295. doi: 10.1016/j.biopha.2016.12.119. [DOI] [PubMed] [Google Scholar]
- 146.Colombo J., Maciel J.M., Ferreira L.C., Silva R.F.D., Zuccari D.A. Effects of melatonin on Hif-1α and vegf expression and on the invasive properties of hepatocarcinoma cells. Oncol. Lett. 2016;12:231–237. doi: 10.3892/ol.2016.4605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Rimler A., Lupowitz Z., Zisapel N. Differential regulation by melatonin of cell growth and androgen receptor binding to the androgen response element in prostate cancer cells. Neuro Endocrinol. Lett. 2002;23(Suppl. 1):45–49. [PubMed] [Google Scholar]
- 148.Rimler A., Culig Z., Lupowitz Z., Zisapel N. Nuclear exclusion of the androgen receptor by melatonin. J. Steroid. Biochem. Mol. Biol. 2002;81:77–84. doi: 10.1016/S0960-0760(02)00050-X. [DOI] [PubMed] [Google Scholar]
- 149.Rimler A., Culig Z., Levy-Rimler G., Lupowitz Z., Klocker H., Matzkin H., Bartsch G., Zisapel N. Melatonin elicits nuclear exclusion of the human androgen receptor and attenuates its activity. Prostate. 2001;49:145–154. doi: 10.1002/pros.1129. [DOI] [PubMed] [Google Scholar]
- 150.Hill S.M., Spriggs L.L., Simon M.A., Muraoka H., Blask D.E. The growth inhibitory action of melatonin on human breast cancer cells is linked to the estrogen response system. Cancer Lett. 1992;64:249–256. doi: 10.1016/0304-3835(92)90050-6. [DOI] [PubMed] [Google Scholar]
- 151.Cos S., Sanchez-Barcelo E.J. Melatonin, experimental basis for a possible application in breast cancer prevention and treatment. Histol. Histopathol. 2000;15:637–647. doi: 10.14670/HH-15.637. [DOI] [PubMed] [Google Scholar]
- 152.Sanchez-Barcelo E.J., Cos S., Mediavilla D., Martinez-Campa C., Gonzalez A., Alonso-Gonzalez C. Melatonin-estrogen interactions in breast cancer. J. Pineal Res. 2005;38:217–222. doi: 10.1111/j.1600-079X.2004.00207.x. [DOI] [PubMed] [Google Scholar]
- 153.Del Rio B., Garcia Pedrero J.M., Martinez-Campa C., Zuazua P., Lazo P.S., Ramos S. Melatonin, an endogenous-specific inhibitor of estrogen receptor α via calmodulin. J. Biol. Chem. 2004;279:38294–38302. doi: 10.1074/jbc.M403140200. [DOI] [PubMed] [Google Scholar]
- 154.Mao L., Cheng Q., Guardiola-Lemaitre B., Schuster-Klein C., Dong C., Lai L., Hill S.M. In vitro and in vivo antitumor activity of melatonin receptor agonists. J. Pineal Res. 2010;49:210–221. doi: 10.1111/j.1600-079X.2010.00781.x. [DOI] [PubMed] [Google Scholar]
- 155.Hill S.M., Frasch T., Xiang S., Yuan L., Duplessis T., Mao L. Molecular mechanisms of melatonin anticancer effects. Integr. Cancer Ther. 2009;8:337–346. doi: 10.1177/1534735409353332. [DOI] [PubMed] [Google Scholar]
- 156.Oprea-Ilies G., Haus E., Sackett-Lundeen L., Liu Y., McLendon L., Busch R., Adams A., Cohen C. Expression of melatonin receptors in triple negative breast cancer (tnbc) in african american and caucasian women: Relation to survival. Breast Cancer Res. Treat. 2013;137:677–687. doi: 10.1007/s10549-012-2371-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Yuan L., Collins A.R., Dai J., Dubocovich M.L., Hill S.M. MT(1) Melatonin receptor overexpression enhances the growth suppressive effect of melatonin in human breast cancer cells. Mol. Cell. Endocrinol. 2002;192:147–156. doi: 10.1016/S0303-7207(02)00029-1. [DOI] [PubMed] [Google Scholar]
- 158.Collins A., Yuan L., Kiefer T.L., Cheng Q., Lai L., Hill S.M. Overexpression of the MT1 melatonin receptor in MCF-7 human breast cancer cells inhibits mammary tumor formation in nude mice. Cancer Lett. 2003;189:49–57. doi: 10.1016/S0304-3835(02)00502-5. [DOI] [PubMed] [Google Scholar]
- 159.Nemeth C., Humpeler S., Kallay E., Mesteri I., Svoboda M., Rogelsperger O., Klammer N., Thalhammer T., Ekmekcioglu C. Decreased expression of the melatonin receptor 1 in human colorectal adenocarcinomas. J. Biol. Regul. Homeost. Agents. 2011;25:531–542. [PubMed] [Google Scholar]
- 160.Leon J., Casado J., Carazo A., Sanjuan L., Mate A., Munoz de Rueda P., de la Cueva P., Quiles R., Ruiz S., Ruiz-Extremera A., et al. Gender-related invasion differences associated with mRNA expression levels of melatonin membrane receptors in colorectal cancer. Mol. Carcinog. 2012;51:608–618. doi: 10.1002/mc.20832. [DOI] [PubMed] [Google Scholar]
- 161.Kobayashi Y., Itoh M.T., Kondo H., Okuma Y., Sato S., Kanishi Y., Hamada N., Kiguchi K., Ishizuka B. Melatonin binding sites in estrogen receptor-positive cells derived from human endometrial cancer. J. Pineal Res. 2003;35:71–74. [PubMed] [Google Scholar]
- 162.Wang R.X., Liu H., Xu L., Zhang H., Zhou R.X. Involvement of nuclear receptor RZR/RORγ in melatonin-induced Hif-1α inactivation in SGC-7901 human gastric cancer cells. Oncol. Rep. 2015;34:2541–2546. doi: 10.3892/or.2015.4238. [DOI] [PubMed] [Google Scholar]
- 163.Winczyk K., Pawlikowski M., Karasek M. Melatonin and RZR/ROR receptor ligand CGP 52608 induce apoptosis in the murine colonic cancer. J. Pineal Res. 2001;31:179–182. doi: 10.1034/j.1600-079x.2001.310213.x. [DOI] [PubMed] [Google Scholar]
- 164.Petranka J., Baldwin W., Biermann J., Jayadev S., Barrett J.C., Murphy E. The oncostatic action of melatonin in an ovarian carcinoma cell line. J. Pineal Res. 1999;26:129–136. doi: 10.1111/j.1600-079X.1999.tb00574.x. [DOI] [PubMed] [Google Scholar]
- 165.Narendhirakannan R.T., Hannah M.A. Oxidative stress and skin cancer: An overview. Indian J. Clin. Biochem. 2013;28:110–115. doi: 10.1007/s12291-012-0278-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Sosa V., Moline T., Somoza R., Paciucci R., Kondoh H., ME L.L. Oxidative stress and cancer: An overview. Ageing Res. Rev. 2013;12:376–390. doi: 10.1016/j.arr.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 167.Reiter R.J., Tan D.X., Mayo J.C., Sainz R.M., Leon J., Czarnocki Z. Melatonin as an antioxidant: Biochemical mechanisms and pathophysiological implications in humans. Acta Biochim. Pol. 2003;50:1129–1146. [PubMed] [Google Scholar]
- 168.Rodriguez C., Mayo J.C., Sainz R.M., Antolin I., Herrera F., Martin V., Reiter R.J. Regulation of antioxidant enzymes: A significant role for melatonin. J. Pineal Res. 2004;36:1–9. doi: 10.1046/j.1600-079X.2003.00092.x. [DOI] [PubMed] [Google Scholar]
- 169.Ramis M.R., Esteban S., Miralles A., Tan D.X., Reiter R.J. Protective effects of melatonin and mitochondria-targeted antioxidants against oxidative stress: A review. Curr. Med. Chem. 2015;22:2690–2711. doi: 10.2174/0929867322666150619104143. [DOI] [PubMed] [Google Scholar]
- 170.Tan D.X., Manchester L.C., Qin L., Reiter R.J. Melatonin: A mitochondrial targeting molecule involving mitochondrial protection and dynamics. Int. J. Mol. Sci. 2016;17 doi: 10.3390/ijms17122124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Proietti S., Cucina A., Minini M., Bizzarri M. Melatonin, mitochondria, and the cancer cell. Cell. Mol. Life Sci. 2017 doi: 10.1007/s00018-017-2612-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Opie L.H., Lecour S. Melatonin has multiorgan effects. Eur. Heart J. Cardiovasc. Pharmacother. 2016;2:258–265. doi: 10.1093/ehjcvp/pvv037. [DOI] [PubMed] [Google Scholar]
- 173.Cardinali D.P., Hardeland R. Inflammaging, metabolic syndrome and melatonin: A call for treatment studies. Neuroendocrinology. 2017;104:382–397. doi: 10.1159/000446543. [DOI] [PubMed] [Google Scholar]
- 174.Sun H., Gusdon A.M., Qu S. Effects of melatonin on cardiovascular diseases: Progress in the past year. Curr. Opin. Lipidol. 2016;27:408–413. doi: 10.1097/MOL.0000000000000314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Quera Salva M.A., Hartley S. Mood disorders, circadian rhythms, melatonin and melatonin agonists. J. Cent. Nerv. Syst. Dis. 2012;4:15–26. doi: 10.4137/JCNSD.S4103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Zhang J.J., Meng X., Li Y., Zhou Y., Xu D.P., Li S., Li H.B. Effects of melatonin on liver injuries and diseases. Int. J. Mol. Sci. 2017;18 doi: 10.3390/ijms18040673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Hahn R.A. Profound bilateral blindness and the incidence of breast cancer. Epidemiology. 1991;2:208–210. doi: 10.1097/00001648-199105000-00008. [DOI] [PubMed] [Google Scholar]
- 178.Klerman E.B., Zeitzer J.M., Duffy J.F., Khalsa S.B., Czeisler C.A. Absence of an increase in the duration of the circadian melatonin secretory episode in totally blind human subjects. J. Clin. Endocrinol. Metab. 2001;86:3166–3170. doi: 10.1210/jc.86.7.3166. [DOI] [PubMed] [Google Scholar]
- 179.Alpert M., Carome E., Kubulins V., Hansler R. Nighttime use of special spectacles or light bulbs that block blue light may reduce the risk of cancer. Med. Hypotheses. 2009;73:324–325. doi: 10.1016/j.mehy.2009.02.027. [DOI] [PubMed] [Google Scholar]
- 180.Flynn-Evans E.E., Stevens R.G., Tabandeh H., Schernhammer E.S., Lockley S.W. Total visual blindness is protective against breast cancer. Cancer Causes Control. 2009;20:1753–1756. doi: 10.1007/s10552-009-9405-0. [DOI] [PubMed] [Google Scholar]
- 181.Kliukiene J., Tynes T., Andersen A. Risk of breast cancer among norwegian women with visual impairment. Br. J. Cancer. 2001;84:397–399. doi: 10.1054/bjoc.2000.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Blakeman V., Williams J.L., Meng Q.J., Streuli C.H. Circadian clocks and breast cancer. Breast Cancer Res. 2016;18:89. doi: 10.1186/s13058-016-0743-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Stevens R.G., Brainard G.C., Blask D.E., Lockley S.W., Motta M.E. Breast cancer and circadian disruption from electric lighting in the modern world. CA Cancer J. Clin. 2014;64:207–218. doi: 10.3322/caac.21218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.He C., Anand S.T., Ebell M.H., Vena J.E., Robb S.W. Circadian disrupting exposures and breast cancer risk: A meta-analysis. Int. Arch. Occup. Environ. Health. 2015;88:533–547. doi: 10.1007/s00420-014-0986-x. [DOI] [PubMed] [Google Scholar]
- 185.Sigurdardottir L.G., Valdimarsdottir U.A., Fall K., Rider J.R., Lockley S.W., Schernhammer E., Mucci L.A. Circadian disruption, sleep loss, and prostate cancer risk: A systematic review of epidemiologic studies. Cancer Epidemiol. Biomark. Prev. 2012;21:1002–1011. doi: 10.1158/1055-9965.EPI-12-0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Nakamura E., Kozaki K., Tsuda H., Suzuki E., Pimkhaokham A., Yamamoto G., Irie T., Tachikawa T., Amagasa T., Inazawa J., et al. Frequent silencing of a putative tumor suppressor gene melatonin receptor 1 a (MTNR1A) in oral squamous-cell carcinoma. Cancer Sci. 2008;99:1390–1400. doi: 10.1111/j.1349-7006.2008.00838.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Jablonska K., Pula B., Zemla A., Owczarek T., Wojnar A., Rys J., Ambicka A., Podhorska-Okolow M., Ugorski M., Dziegiel P. Expression of melatonin receptor mt1 in cells of human invasive ductal breast carcinoma. J. Pineal Res. 2013;54:334–345. doi: 10.1111/jpi.12032. [DOI] [PubMed] [Google Scholar]
- 188.Moroishi T., Hansen C.G., Guan K.L. The emerging roles of yap and TAZ in cancer. Nat. Rev. Cancer. 2015;15:73–79. doi: 10.1038/nrc3876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Zhao B., Wei X., Li W., Udan R.S., Yang Q., Kim J., Xie J., Ikenoue T., Yu J., Li L., et al. Inactivation of yap oncoprotein by the Hippo pathway is involved in cell contact inhibition and tissue growth control. Genes Dev. 2007;21:2747–2761. doi: 10.1101/gad.1602907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Dong J., Feldmann G., Huang J., Wu S., Zhang N., Comerford S.A., Gayyed M.F., Anders R.A., Maitra A., Pan D. Elucidation of a universal size-control mechanism in drosophila and mammals. Cell. 2007;130:1120–1133. doi: 10.1016/j.cell.2007.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Hao Y., Chun A., Cheung K., Rashidi B., Yang X. Tumor suppressor lats1 is a negative regulator of oncogene yap. J. Biol. Chem. 2008;283:5496–5509. doi: 10.1074/jbc.M709037200. [DOI] [PubMed] [Google Scholar]
- 192.Kanai F., Marignani P.A., Sarbassova D., Yagi R., Hall R.A., Donowitz M., Hisaminato A., Fujiwara T., Ito Y., Cantley L.C., et al. TAZ: A novel transcriptional co-activator regulated by interactions with 14-3-3 and PDZ domain proteins. EMBO J. 2000;19:6778–6791. doi: 10.1093/emboj/19.24.6778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Lei Q.Y., Zhang H., Zhao B., Zha Z.Y., Bai F., Pei X.H., Zhao S., Xiong Y., Guan K.L. TAZ promotes cell proliferation and epithelial-mesenchymal transition and is inhibited by the Hippo pathway. Mol. Cell. Biol. 2008;28:2426–2436. doi: 10.1128/MCB.01874-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Vassilev A., Kaneko K.J., Shu H., Zhao Y., DePamphilis M.L. TEAD/Tef Transcription factors utilize the activation domain of YAP65, a SRC/YES-associated protein localized in the cytoplasm. Genes Dev. 2001;15:1229–1241. doi: 10.1101/gad.888601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Varelas X., Samavarchi-Tehrani P., Narimatsu M., Weiss A., Cockburn K., Larsen B.G., Rossant J., Wrana J.L. The crumbs complex couples cell density sensing to Hippo-dependent control of the TGF-β-Smad pathway. Dev. Cell. 2010;19:831–844. doi: 10.1016/j.devcel.2010.11.012. [DOI] [PubMed] [Google Scholar]
- 196.Zhao B., Li L., Tumaneng K., Wang C.Y., Guan K.L. A coordinated phosphorylation by lats and CK1 regulates yap stability through SCF(β-Trcp) Genes Dev. 2010;24:72–85. doi: 10.1101/gad.1843810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Liu C.Y., Zha Z.Y., Zhou X., Zhang H., Huang W., Zhao D., Li T., Chan S.W., Lim C.J., Hong W., et al. The hippo tumor pathway promotes taz degradation by phosphorylating a phosphodegron and recruiting the SCF{β}-Trcp e3 ligase. J. Biol. Chem. 2010;285:37159–37169. doi: 10.1074/jbc.M110.152942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Zanconato F., Battilana G., Cordenonsi M., Piccolo S. YAP/TAZ as therapeutic targets in cancer. Curr. Opin. Pharmacol. 2016;29:26–33. doi: 10.1016/j.coph.2016.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Miller E., Yang J., DeRan M., Wu C., Su A.I., Bonamy G.M., Liu J., Peters E.C., Wu X. Identification of serum-derived sphingosine-1-phosphate as a small molecule regulator of yap. Chem. Biol. 2012;19:955–962. doi: 10.1016/j.chembiol.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 200.Mo J.S., Yu F.X., Gong R., Brown J.H., Guan K.L. Regulation of the Hippo-yap pathway by protease-activated receptors (pars) Genes Dev. 2012;26:2138–2143. doi: 10.1101/gad.197582.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Cai H., Xu Y. The role of LPA and YAP signaling in long-term migration of human ovarian cancer cells. Cell Commun. Signal. 2013;11:31. doi: 10.1186/1478-811X-11-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Jeong G.O., Shin S.H., Seo E.J., Kwon Y.W., Heo S.C., Kim K.H., Yoon M.S., Suh D.S., Kim J.H. Taz mediates lysophosphatidic acid-induced migration and proliferation of epithelial ovarian cancer cells. Cell. Physiol. Biochem. 2013;32:253–263. doi: 10.1159/000354434. [DOI] [PubMed] [Google Scholar]
- 203.Yu F.X., Zhao B., Panupinthu N., Jewell J.L., Lian I., Wang L.H., Zhao J., Yuan H., Tumaneng K., Li H., et al. Regulation of the hippo-yap pathway by G-protein-coupled receptor signaling. Cell. 2012;150:780–791. doi: 10.1016/j.cell.2012.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Kim M., Kim M., Lee S., Kuninaka S., Saya H., Lee H., Lee S., Lim D.S. CAMP/PKA signalling reinforces the lats-yap pathway to fully suppress yap in response to actin cytoskeletal changes. EMBO J. 2013;32:1543–1555. doi: 10.1038/emboj.2013.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Yu F.X., Zhang Y., Park H.W., Jewell J.L., Chen Q., Deng Y., Pan D., Taylor S.S., Lai Z.C., Guan K.L. Protein kinase a activates the hippo pathway to modulate cell proliferation and differentiation. Genes Dev. 2013;27:1223–1232. doi: 10.1101/gad.219402.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Cho H.H., Shin K.K., Kim Y.J., Song J.S., Kim J.M., Bae Y.C., Kim C.D., Jung J.S. NF-κB activation stimulates osteogenic differentiation of mesenchymal stem cells derived from human adipose tissue by increasing taz expression. J. Cell. Physiol. 2010;223:168–177. doi: 10.1002/jcp.22024. [DOI] [PubMed] [Google Scholar]
- 207.Brunn G.J., Hudson C.C., Sekulic A., Williams J.M., Hosoi H., Houghton P.J., Lawrence J.C., Jr., Abraham R.T. Phosphorylation of the translational repressor PHAS-i by the mammalian target of rapamycin. Science. 1997;277:99–101. doi: 10.1126/science.277.5322.99. [DOI] [PubMed] [Google Scholar]
- 208.Dennis P.B., Jaeschke A., Saitoh M., Fowler B., Kozma S.C., Thomas G. Mammalian tor: A homeostatic atp sensor. Science. 2001;294:1102–1105. doi: 10.1126/science.1063518. [DOI] [PubMed] [Google Scholar]
- 209.Shamji A.F., Nghiem P., Schreiber S.L. Integration of growth factor and nutrient signaling: Implications for cancer biology. Mol. Cell. 2003;12:271–280. doi: 10.1016/j.molcel.2003.08.016. [DOI] [PubMed] [Google Scholar]
- 210.Inoki K., Li Y., Zhu T., Wu J., Guan K.L. TSC2 is phosphorylated and inhibited by AKT and suppresses mTOR signalling. Nat. Cell Biol. 2002;4:648–657. doi: 10.1038/ncb839. [DOI] [PubMed] [Google Scholar]
- 211.Manning B.D., Tee A.R., Logsdon M.N., Blenis J., Cantley L.C. Identification of the tuberous sclerosis complex-2 tumor suppressor gene product tuberin as a target of the phosphoinositide 3-kinase/AKT pathway. Mol. Cell. 2002;10:151–162. doi: 10.1016/S1097-2765(02)00568-3. [DOI] [PubMed] [Google Scholar]
- 212.Hao F., Xu Q., Zhao Y., Stevens J.V., Young S.H., Sinnett-Smith J., Rozengurt E. Insulin receptor and gpcr crosstalk stimulates yap via PI3K and PKD in pancreatic cancer cells. Mol. Cancer Res. 2017;15:929–941. doi: 10.1158/1541-7786.MCR-17-0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Wang C., Jeong K., Jiang H., Guo W., Gu C., Lu Y., Liang J. YAP/TAZ Regulates the insulin signaling via IRS1/2 in endometrial cancer. Am. J. Cancer Res. 2016;6:996–1010. [PMC free article] [PubMed] [Google Scholar]
- 214.Tumaneng K., Schlegelmilch K., Russell R.C., Yimlamai D., Basnet H., Mahadevan N., Fitamant J., Bardeesy N., Camargo F.D., Guan K.L. Yap mediates crosstalk between the hippo and PI(3)K-TOR pathways by suppressing pten via MIR-29. Nat. Cell Biol. 2012;14:1322–1329. doi: 10.1038/ncb2615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Fernandez L.A., Squatrito M., Northcott P., Awan A., Holland E.C., Taylor M.D., Nahle Z., Kenney A.M. Oncogenic yap promotes radioresistance and genomic instability in medulloblastoma through IGF2-mediated AKT activation. Oncogene. 2012;31:1923–1937. doi: 10.1038/onc.2011.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Lin Z., Zhou P., von Gise A., Gu F., Ma Q., Chen J., Guo H., van Gorp P.R., Wang D.Z., Pu W.T. PI3KCB links hippo-yap and PI3K-AKT signaling pathways to promote cardiomyocyte proliferation and survival. Circ. Res. 2015;116:35–45. doi: 10.1161/CIRCRESAHA.115.304457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Wang W., Xiao Z.D., Li X., Aziz K.E., Gan B., Johnson R.L., Chen J. AMPK modulates hippo pathway activity to regulate energy homeostasis. Nat. Cell Biol. 2015;17:490–499. doi: 10.1038/ncb3113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Jung J.H., Sohn E.J., Shin E.A., Lee D., Kim B., Jung D.B., Kim J.H., Yun M., Lee H.J., Park Y.K., et al. Melatonin suppresses the expression of 45s preribosomal rna and upstream binding factor and enhances the antitumor activity of puromycin in MDA-MB-231 breast cancer cells. Evid. Based Complement. Alternat. Med. 2013;2013:879746. doi: 10.1155/2013/879746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Liu C., Jia Z., Zhang X., Hou J., Wang L., Hao S., Ruan X., Yu Z., Zheng Y. Involvement of melatonin in autophagy-mediated mouse hepatoma H22 cell survival. Int. Immunopharmacol. 2012;12:394–401. doi: 10.1016/j.intimp.2011.12.012. [DOI] [PubMed] [Google Scholar]
- 220.Kim H.S., Kim T.J., Yoo Y.M. Melatonin combined with endoplasmic reticulum stress induces cell death via the PI3K/AKT/mTOR pathway in B16F10 melanoma cells. PLoS ONE. 2014;9:e92627. doi: 10.1371/journal.pone.0092627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Porta C., Paglino C., Mosca A. Targeting PI3K/AKT/mTOR signaling in cancer. Front. Oncol. 2014;4:64. doi: 10.3389/fonc.2014.00064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Peschke E., Bahr I., Muhlbauer E. Melatonin and pancreatic islets: Interrelationships between melatonin, insulin and glucagon. Int. J. Mol. Sci. 2013;14:6981–7015. doi: 10.3390/ijms14046981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Daulat A.M., Maurice P., Froment C., Guillaume J.L., Broussard C., Monsarrat B., Delagrange P., Jockers R. Purification and identification of G protein-coupled receptor protein complexes under native conditions. Mol. Cell. Proteom. 2007;6:835–844. doi: 10.1074/mcp.M600298-MCP200. [DOI] [PubMed] [Google Scholar]
- 224.Daulat A.M., Maurice P., Jockers R. Recent methodological advances in the discovery of GPCR-associated protein complexes. Trends Pharmacol. Sci. 2009;30:72–78. doi: 10.1016/j.tips.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 225.Maurice P., Daulat A.M., Broussard C., Mozo J., Clary G., Hotellier F., Chafey P., Guillaume J.L., Ferry G., Boutin J.A., et al. A generic approach for the purification of signaling complexes that specifically interact with the carboxyl-terminal domain of G protein-coupled receptors. Mol. Cell. Proteom. 2008;7:1556–1569. doi: 10.1074/mcp.M700435-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Santinon G., Pocaterra A., Dupont S. Control of YAP/TAZ activity by metabolic and nutrient-sensing pathways. Trends Cell Biol. 2016;26:289–299. doi: 10.1016/j.tcb.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 227.Navarro-Alarcon M., Ruiz-Ojeda F.J., Blanca-Herrera R.M., MM A.S., Acuna-Castroviejo D., Fernandez-Vazquez G., Agil A. Melatonin and metabolic regulation: A review. Food Funct. 2014;5:2806–2832. doi: 10.1039/C4FO00317A. [DOI] [PubMed] [Google Scholar]
- 228.Cipolla-Neto J., Amaral F.G., Afeche S.C., Tan D.X., Reiter R.J. Melatonin, energy metabolism, and obesity: A review. J. Pineal Res. 2014;56:371–381. doi: 10.1111/jpi.12137. [DOI] [PubMed] [Google Scholar]
- 229.Aragona M., Panciera T., Manfrin A., Giulitti S., Michielin F., Elvassore N., Dupont S., Piccolo S. A mechanical checkpoint controls multicellular growth through YAP/TAZ regulation by actin-processing factors. Cell. 2013;154:1047–1059. doi: 10.1016/j.cell.2013.07.042. [DOI] [PubMed] [Google Scholar]
- 230.Driscoll T.P., Cosgrove B.D., Heo S.J., Shurden Z.E., Mauck R.L. Cytoskeletal to nuclear strain transfer regulates yap signaling in mesenchymal stem cells. Biophys. J. 2015;108:2783–2793. doi: 10.1016/j.bpj.2015.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Dupont S., Morsut L., Aragona M., Enzo E., Giulitti S., Cordenonsi M., Zanconato F., Le Digabel J., Forcato M., Bicciato S., et al. Role of YAP/TAZ in mechanotransduction. Nature. 2011;474:179–183. doi: 10.1038/nature10137. [DOI] [PubMed] [Google Scholar]
- 232.Wada K., Itoga K., Okano T., Yonemura S., Sasaki H. Hippo pathway regulation by cell morphology and stress fibers. Development. 2011;138:3907–3914. doi: 10.1242/dev.070987. [DOI] [PubMed] [Google Scholar]
- 233.Zhao B., Li L., Wang L., Wang C.Y., Yu J., Guan K.L. Cell detachment activates the hippo pathway via cytoskeleton reorganization to induce anoikis. Genes Dev. 2012;26:54–68. doi: 10.1101/gad.173435.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Sun Y., Yong K.M., Villa-Diaz L.G., Zhang X., Chen W., Philson R., Weng S., Xu H., Krebsbach P.H., Fu J. Hippo/YAP-mediated rigidity-dependent motor neuron differentiation of human pluripotent stem cells. Nat. Mater. 2014;13:599–604. doi: 10.1038/nmat3945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Bertero T., Oldham W.M., Cottrill K.A., Pisano S., Vanderpool R.R., Yu Q., Zhao J., Tai Y., Tang Y., Zhang Y.Y., et al. Vascular stiffness mechanoactivates YAP/TAZ-dependent glutaminolysis to drive pulmonary hypertension. J. Clin. Investig. 2016;126:3313–3335. doi: 10.1172/JCI86387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Kim N.G., Gumbiner B.M. Adhesion to fibronectin regulates hippo signaling via the FAK-SRC-PI3K pathway. J. Cell Biol. 2015;210:503–515. doi: 10.1083/jcb.201501025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Benham-Pyle B.W., Pruitt B.L., Nelson W.J. Cell adhesion. Mechanical strain induces e-cadherin-dependent yap1 and β-catenin activation to drive cell cycle entry. Science. 2015;348:1024–1027. doi: 10.1126/science.aaa4559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Bertero T., Cottrill K.A., Lu Y., Haeger C.M., Dieffenbach P., Annis S., Hale A., Bhat B., Kaimal V., Zhang Y.Y., et al. Matrix remodeling promotes pulmonary hypertension through feedback mechanoactivation of the YAP/TAZ-mir-130/301 circuit. Cell Rep. 2015;13:1016–1032. doi: 10.1016/j.celrep.2015.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Calvo F., Ege N., Grande-Garcia A., Hooper S., Jenkins R.P., Chaudhry S.I., Harrington K., Williamson P., Moeendarbary E., Charras G., et al. Mechanotransduction and yap-dependent matrix remodelling is required for the generation and maintenance of cancer-associated fibroblasts. Nat. Cell Biol. 2013;15:637–646. doi: 10.1038/ncb2756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Paszek M.J., DuFort C.C., Rossier O., Bainer R., Mouw J.K., Godula K., Hudak J.E., Lakins J.N., Wijekoon A.C., Cassereau L., et al. The cancer glycocalyx mechanically primes integrin-mediated growth and survival. Nature. 2014;511:319–325. doi: 10.1038/nature13535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Rubashkin M.G., Cassereau L., Bainer R., DuFort C.C., Yui Y., Ou G., Paszek M.J., Davidson M.W., Chen Y.Y., Weaver V.M. Force engages vinculin and promotes tumor progression by enhancing pi3k activation of phosphatidylinositol (3,4,5)-triphosphate. Cancer Res. 2014;74:4597–4611. doi: 10.1158/0008-5472.CAN-13-3698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Mouw J.K., Yui Y., Damiano L., Bainer R.O., Lakins J.N., Acerbi I., Ou G., Wijekoon A.C., Levental K.R., Gilbert P.M., et al. Tissue mechanics modulate microrna-dependent pten expression to regulate malignant progression. Nat. Med. 2014;20:360–367. doi: 10.1038/nm.3497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Lin C.H., Pelissier F.A., Zhang H., Lakins J., Weaver V.M., Park C., LaBarge M.A. Microenvironment rigidity modulates responses to the her2 receptor tyrosine kinase inhibitor lapatinib via YAP and TAZ transcription factors. Mol. Biol. Cell. 2015;26:3946–3953. doi: 10.1091/mbc.E15-07-0456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Bartucci M., Dattilo R., Moriconi C., Pagliuca A., Mottolese M., Federici G., Benedetto A.D., Todaro M., Stassi G., Sperati F., et al. TAZ is required for metastatic activity and chemoresistance of breast cancer stem cells. Oncogene. 2015;34:681–690. doi: 10.1038/onc.2014.5. [DOI] [PubMed] [Google Scholar]
- 245.Cordenonsi M., Zanconato F., Azzolin L., Forcato M., Rosato A., Frasson C., Inui M., Montagner M., Parenti A.R., Poletti A., et al. The hippo transducer TAZ confers cancer stem cell-related traits on breast cancer cells. Cell. 2011;147:759–772. doi: 10.1016/j.cell.2011.09.048. [DOI] [PubMed] [Google Scholar]
- 246.Lin L., Sabnis A.J., Chan E., Olivas V., Cade L., Pazarentzos E., Asthana S., Neel D., Yan J.J., Lu X., et al. The hippo effector yap promotes resistance to raf- and mek-targeted cancer therapies. Nat. Genet. 2015;47:250–256. doi: 10.1038/ng.3218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Lee J.E., Park H.S., Lee D., Yoo G., Kim T., Jeon H., Yeo M.K., Lee C.S., Moon J.Y., Jung S.S., et al. Hippo pathway effector yap inhibition restores the sensitivity of egfr-tki in lung adenocarcinoma having primary or acquired egfr-tki resistance. Biochem. Biophys. Res. Commun. 2016;474:154–160. doi: 10.1016/j.bbrc.2016.04.089. [DOI] [PubMed] [Google Scholar]
- 248.Cheng H., Zhang Z., Rodriguez-Barrueco R., Borczuk A., Liu H., Yu J., Silva J.M., Cheng S.K., Perez-Soler R., Halmos B. Functional genomics screen identifies yap1 as a key determinant to enhance treatment sensitivity in lung cancer cells. Oncotarget. 2016;7:28976–28988. doi: 10.18632/oncotarget.6721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Anton-Tay F., Ramirez G., Martinez I., Benitez-King G. In vitro stimulation of protein kinase c by melatonin. Neurochem. Res. 1998;23:601–606. doi: 10.1023/A:1022474402458. [DOI] [PubMed] [Google Scholar]
- 250.Benitez-King G. PKC Activation by melatonin modulates vimentin intermediate filament organization in n1e-115 cells. J. Pineal Res. 2000;29:8–14. doi: 10.1034/j.1600-079X.2000.290102.x. [DOI] [PubMed] [Google Scholar]
- 251.Benitez-King G., Hernandez M.E., Tovar R., Ramirez G. Melatonin activates PKC-α but not pkc-epsilon in n1e-115 cells. Neurochem. Int. 2001;39:95–102. doi: 10.1016/S0197-0186(01)00021-3. [DOI] [PubMed] [Google Scholar]
- 252.Koopman M.G., Koomen G.C., Krediet R.T., de Moor E.A., Hoek F.J., Arisz L. Circadian rhythm of glomerular filtration rate in normal individuals. Clin. Sci. 1989;77:105–111. doi: 10.1042/cs0770105. [DOI] [PubMed] [Google Scholar]
- 253.Richardson B.A., Studier E.H., Stallone J.N., Kennedy C.M. Effects of melatonin on water metabolism and renal function in male syrian hamsters (mesocricetus auratus) J. Pineal Res. 1992;13:49–59. doi: 10.1111/j.1600-079X.1992.tb00054.x. [DOI] [PubMed] [Google Scholar]
- 254.Lynch C.D., Sheetz M.P. Cellular mechanotransduction: Filamin a strains to regulate motility. Curr. Biol. 2011;21:R916–R918. doi: 10.1016/j.cub.2011.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Szymaniak A.D., Mahoney J.E., Cardoso W.V., Varelas X. CRUMBS3-Mediated polarity directs airway epithelial cell fate through the hippo pathway effector yap. Dev. Cell. 2015;34:283–296. doi: 10.1016/j.devcel.2015.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Elbediwy A., Vincent-Mistiaen Z.I., Thompson B.J. Yap and TAZ in epithelial stem cells: A sensor for cell polarity, mechanical forces and tissue damage. Bioessays. 2016;38:644–653. doi: 10.1002/bies.201600037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Gumbiner B.M., Kim N.G. The hippo-yap signaling pathway and contact inhibition of growth. J. Cell Sci. 2014;127:709–717. doi: 10.1242/jcs.140103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Genevet A., Wehr M.C., Brain R., Thompson B.J., Tapon N. Kibra is a regulator of the salvador/warts/hippo signaling network. Dev. Cell. 2010;18:300–308. doi: 10.1016/j.devcel.2009.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Yu J., Zheng Y., Dong J., Klusza S., Deng W.M., Pan D. Kibra functions as a tumor suppressor protein that regulates hippo signaling in conjunction with merlin and expanded. Dev. Cell. 2010;18:288–299. doi: 10.1016/j.devcel.2009.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Zhao B., Li L., Lu Q., Wang L.H., Liu C.Y., Lei Q., Guan K.L. Angiomotin is a novel hippo pathway component that inhibits yap oncoprotein. Genes Dev. 2011;25:51–63. doi: 10.1101/gad.2000111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Chen C.L., Gajewski K.M., Hamaratoglu F., Bossuyt W., Sansores-Garcia L., Tao C., Halder G. The apical-basal cell polarity determinant crumbs regulates hippo signaling in drosophila. Proc. Natl. Acad. Sci. USA. 2010;107:15810–15815. doi: 10.1073/pnas.1004060107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Gurvich N., Perna F., Farina A., Voza F., Menendez S., Hurwitz J., Nimer S.D. L3MBTL1 Polycomb protein, a candidate tumor suppressor in del(20q12) myeloid disorders, is essential for genome stability. Proc. Natl. Acad. Sci. USA. 2010;107:22552–22557. doi: 10.1073/pnas.1017092108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Ling C., Zheng Y., Yin F., Yu J., Huang J., Hong Y., Wu S., Pan D. The apical transmembrane protein crumbs functions as a tumor suppressor that regulates hippo signaling by binding to expanded. Proc. Natl. Acad. Sci. USA. 2010;107:10532–10537. doi: 10.1073/pnas.1004279107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Robinson B.S., Huang J., Hong Y., Moberg K.H. Crumbs regulates salvador/warts/hippo signaling in drosophila via the ferm-domain protein expanded. Curr. Biol. 2010;20:582–590. doi: 10.1016/j.cub.2010.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Elbediwy A., Vincent-Mistiaen Z.I., Spencer-Dene B., Stone R.K., Boeing S., Wculek S.K., Cordero J., Tan E.H., Ridgway R., Brunton V.G., et al. Integrin signalling regulates yap and TAZ to control skin homeostasis. Development. 2016;143:1674–1687. doi: 10.1242/dev.133728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Das Thakur M., Feng Y., Jagannathan R., Seppa M.J., Skeath J.B., Longmore G.D. Ajuba lim proteins are negative regulators of the hippo signaling pathway. Curr. Biol. 2010;20:657–662. doi: 10.1016/j.cub.2010.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Nguyen H.B., Babcock J.T., Wells C.D., Quilliam L.A. Lkb1 tumor suppressor regulates amp kinase/mTOR-independent cell growth and proliferation via the phosphorylation of yap. Oncogene. 2013;32:4100–4109. doi: 10.1038/onc.2012.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Remue E., Meerschaert K., Oka T., Boucherie C., Vandekerckhove J., Sudol M., Gettemans J. TAZ interacts with zonula occludens-1 and -2 proteins in a pdz-1 dependent manner. FEBS Lett. 2010;584:4175–4180. doi: 10.1016/j.febslet.2010.09.020. [DOI] [PubMed] [Google Scholar]
- 269.Oka T., Remue E., Meerschaert K., Vanloo B., Boucherie C., Gfeller D., Bader G.D., Sidhu S.S., Vandekerckhove J., Gettemans J., et al. Functional complexes between yap2 and zo-2 are pdz domain-dependent, and regulate yap2 nuclear localization and signalling. Biochem. J. 2010;432:461–472. doi: 10.1042/BJ20100870. [DOI] [PubMed] [Google Scholar]
- 270.Kim N.G., Koh E., Chen X., Gumbiner B.M. E-cadherin mediates contact inhibition of proliferation through hippo signaling-pathway components. Proc. Natl. Acad. Sci. USA. 2011;108:11930–11935. doi: 10.1073/pnas.1103345108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Schlegelmilch K., Mohseni M., Kirak O., Pruszak J., Rodriguez J.R., Zhou D., Kreger B.T., Vasioukhin V., Avruch J., Brummelkamp T.R., et al. Yap1 acts downstream of α-catenin to control epidermal proliferation. Cell. 2011;144:782–795. doi: 10.1016/j.cell.2011.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Liu X., Yang N., Figel S.A., Wilson K.E., Morrison C.D., Gelman I.H., Zhang J. Ptpn14 interacts with and negatively regulates the oncogenic function of yap. Oncogene. 2013;32:1266–1273. doi: 10.1038/onc.2012.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Anastasiadis P.Z., Moon S.Y., Thoreson M.A., Mariner D.J., Crawford H.C., Zheng Y., Reynolds A.B. Inhibition of rhoa by p120 catenin. Nat. Cell Biol. 2000;2:637–644. doi: 10.1038/35023588. [DOI] [PubMed] [Google Scholar]
- 274.Grosheva I., Shtutman M., Elbaum M., Bershadsky A.D. P120 catenin affects cell motility via modulation of activity of rho-family gtpases: A link between cell-cell contact formation and regulation of cell locomotion. J. Cell Sci. 2001;114:695–707. doi: 10.1242/jcs.114.4.695. [DOI] [PubMed] [Google Scholar]
- 275.Noren N.K., Liu B.P., Burridge K., Kreft B. P120 catenin regulates the actin cytoskeleton via rho family gtpases. J. Cell Biol. 2000;150:567–580. doi: 10.1083/jcb.150.3.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Zhu Y.T., Chen H.C., Chen S.Y., Tseng S.C. Nuclear p120 catenin unlocks mitotic block of contact-inhibited human corneal endothelial monolayers without disrupting adherent junctions. J. Cell Sci. 2012;125:3636–3648. doi: 10.1242/jcs.103267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Ireton R.C., Davis M.A., van Hengel J., Mariner D.J., Barnes K., Thoreson M.A., Anastasiadis P.Z., Matrisian L., Bundy L.M., Sealy L., et al. A novel role for p120 catenin in e-cadherin function. J. Cell Biol. 2002;159:465–476. doi: 10.1083/jcb.200205115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Davis M.A., Ireton R.C., Reynolds A.B. A core function for p120-catenin in cadherin turnover. J. Cell Biol. 2003;163:525–534. doi: 10.1083/jcb.200307111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Xiao K., Allison D.F., Buckley K.M., Kottke M.D., Vincent P.A., Faundez V., Kowalczyk A.P. Cellular levels of p120 catenin function as a set point for cadherin expression levels in microvascular endothelial cells. J. Cell Biol. 2003;163:535–545. doi: 10.1083/jcb.200306001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Yang C.C., Graves H.K., Moya I.M., Tao C., Hamaratoglu F., Gladden A.B., Halder G. Differential regulation of the hippo pathway by adherens junctions and apical-basal cell polarity modules. Proc. Natl. Acad. Sci. USA. 2015;112:1785–1790. doi: 10.1073/pnas.1420850112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Bar-Sagi D., Hall A. Ras and rho gtpases: A family reunion. Cell. 2000;103:227–238. doi: 10.1016/S0092-8674(00)00115-X. [DOI] [PubMed] [Google Scholar]
- 282.Parri M., Chiarugi P. Rac and rho gtpases in cancer cell motility control. Cell Commun. Signal. 2010;8:23. doi: 10.1186/1478-811X-8-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Arthur W.T., Quilliam L.A., Cooper J.A. Rap1 promotes cell spreading by localizing rac guanine nucleotide exchange factors. J. Cell Biol. 2004;167:111–122. doi: 10.1083/jcb.200404068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Stiffler M.A., Chen J.R., Grantcharova V.P., Lei Y., Fuchs D., Allen J.E., Zaslavskaia L.A., MacBeath G. Pdz domain binding selectivity is optimized across the mouse proteome. Science. 2007;317:364–369. doi: 10.1126/science.1144592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Guillaume J.L., Daulat A.M., Maurice P., Levoye A., Migaud M., Brydon L., Malpaux B., Borg-Capra C., Jockers R. The pdz protein mupp1 promotes gi coupling and signaling of the mt1 melatonin receptor. J. Biol. Chem. 2008;283:16762–16771. doi: 10.1074/jbc.M802069200. [DOI] [PubMed] [Google Scholar]
- 286.Hamazaki Y., Itoh M., Sasaki H., Furuse M., Tsukita S. Multi-pdz domain protein 1 (mupp1) is concentrated at tight junctions through its possible interaction with claudin-1 and junctional adhesion molecule. J. Biol. Chem. 2002;277:455–461. doi: 10.1074/jbc.M109005200. [DOI] [PubMed] [Google Scholar]
- 287.Meyer T.N., Schwesinger C., Denker B.M. Zonula occludens-1 is a scaffolding protein for signaling molecules. Gα(12) directly binds to the src homology 3 domain and regulates paracellular permeability in epithelial cells. J. Biol. Chem. 2002;277:24855–24858. doi: 10.1074/jbc.C200240200. [DOI] [PubMed] [Google Scholar]
- 288.Sabath E., Negoro H., Beaudry S., Paniagua M., Angelow S., Shah J., Grammatikakis N., Yu A.S., Denker B.M. Gα12 regulates protein interactions within the mdck cell tight junction and inhibits tight-junction assembly. J. Cell Sci. 2008;121:814–824. doi: 10.1242/jcs.014878. [DOI] [PubMed] [Google Scholar]
- 289.Clattenburg L., Wigerius M., Qi J., Rainey J.K., Rourke J.L., Muruganandan S., Sinal C.J., Fawcett J.P. Nos1ap functionally associates with yap to regulate hippo signaling. Mol. Cell. Biol. 2015;35:2265–2277. doi: 10.1128/MCB.00062-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Alzahrani F., Clattenburg L., Muruganandan S., Bullock M., MacIsaac K., Wigerius M., Williams B.A., Graham M.E., Rigby M.H., Trites J.R., et al. The hippo component yap localizes in the nucleus of human papilloma virus positive oropharyngeal squamous cell carcinoma. J. Otolaryngol. Head Neck Surg. 2017;46:15. doi: 10.1186/s40463-017-0187-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Mohseni M., Sun J., Lau A., Curtis S., Goldsmith J., Fox V.L., Wei C., Frazier M., Samson O., Wong K.K., et al. A genetic screen identifies an lkb1-mark signalling axis controlling the hippo-yap pathway. Nat. Cell Biol. 2014;16:108–117. doi: 10.1038/ncb2884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Treeck O., Haldar C., Ortmann O. Antiestrogens modulate mt1 melatonin receptor expression in breast and ovarian cancer cell lines. Oncol. Rep. 2006;15:231–235. doi: 10.3892/or.15.1.231. [DOI] [PubMed] [Google Scholar]
- 293.Powzaniuk M., McElwee-Witmer S., Vogel R.L., Hayami T., Rutledge S.J., Chen F., Harada S., Schmidt A., Rodan G.A., Freedman L.P., et al. The lats2/kpm tumor suppressor is a negative regulator of the androgen receptor. Mol. Endocrinol. 2004;18:2011–2023. doi: 10.1210/me.2004-0065. [DOI] [PubMed] [Google Scholar]
- 294.Lit L.C., Scott S., Zhang H., Stebbing J., Photiou A., Giamas G. Lats2 is a modulator of estrogen receptor α. Anticancer Res. 2013;33:53–63. [PubMed] [Google Scholar]
- 295.Britschgi A., Duss S., Kim S., Couto J.P., Brinkhaus H., Koren S., De Silva D., Mertz K.D., Kaup D., Varga Z., et al. The hippo kinases lats1 and 2 control human breast cell fate via crosstalk with ERα. Nature. 2017;541:541–545. doi: 10.1038/nature20829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Ma B., Chen Y., Chen L., Cheng H., Mu C., Li J., Gao R., Zhou C., Cao L., Liu J., et al. Hypoxia regulates hippo signalling through the siah2 ubiquitin e3 ligase. Nat. Cell Biol. 2015;17:95–103. doi: 10.1038/ncb3073. [DOI] [PubMed] [Google Scholar]
- 297.Zanconato F., Piccolo S. Eradicating tumor drug resistance at its yap-biomechanical roots. EMBO J. 2016;35:459–461. doi: 10.15252/embj.201593584. [DOI] [PMC free article] [PubMed] [Google Scholar]