Abstract
For some low rectal cancer patients, ostomy (with elimination into a pouch) may be the only realistic surgical option. However, some patients have a choice between ostomy and sphincter-sparing surgery. Sphincter-sparing surgery has been preferred over ostomy because it offers preservation of normal bowel function. However, this surgery can cause incontinence and bowel dysfunction. Increasingly, it has become evident that certain patients eligible for sphincter-sparing surgery may not be well served by the surgery and construction of an ostomy may be better. No validated assessment tool or decision aid has been published to help newly diagnosed patients decide between the two surgeries, or to help physicians elicit long-term surgical outcomes. Furthermore, comparison of long-term outcomes and late effects following the two surgeries has not been synthesized. We therefore conducted a systematic review to examine this ? This systematic review summarizes controlled studies that compared long-term survivorship outcomes between these two surgical groups. Our goals are: 1) improve understanding and shared decision-making among surgeons, oncologists, primary care providers, patients, and caregivers; 2) increase the patient’s participation in the decision; (3) alert the primary care provider to patient challenges that could be addressed by provider attention and intervention; and 4) ultimately, improve patients’ long-term quality of life. This report includes discussion points for health care providers to use with their patients during initial discussions of ostomy and sphincter-sparing surgery, as well as questions to ask during follow-up examinations to ascertain any long-term challenges facing the patient.
Keywords: rectal cancer, cancer survivors, ostomy, anastomosis, patient-centered care, health communication, quality of life
Introduction
Rectal cancer occurs in 11 per 100,000 persons and is disproportionately more common in men and older persons.1 Individuals with a genetic predisposition or family history, or a personal history of colorectal polyps, or cancers of the colorectum, ovary, endometrium, or breast are also at increased risk. Low rectal cancer is variably defined, but usually occurs in the distal 6 centimeters of the rectum.2 Very low rectal cancers involve, or are very close to, the anal sphincter. The two procedures used most commonly for rectal cancer include low anterior resection with or without a temporary (“protective”) ostomy, and abdominoperineal resection with construction of a permanent ostomy. When low anterior resection is used, the part of the rectum containing the tumor is removed with preservation of the anal sphincter, and the colon is attached to the remaining part of the rectum or anal canal so that the patient retains bowel continuity. In contrast, when the cancer is growing into or is very close to the anal sphincter, the sphincter needs to be removed and a permanent ostomy needs to be constructed.3 Other clinical factors play a role in determining the type of surgery, including the bulkiness of the tumor, pre-operative anal function, smoking habits, diabetes mellitus, gender, and medications that inhibit wound healing (e.g., corticosteroids).4 Finally, some patients may be given a “temporary ostomy” with the goal of restoring bowel continuity through the anus during a second, later surgery. Bowel function may be significantly altered after sphincter-sparing surgery, and its severity largely depends on the level of the anastomosis. During 1995–2010, 73% of rectal cancer patients in the SEER population and 68% in the Veterans Administration population received sphincter-sparing surgery, while this number was 70% in the Kaiser Permanente Northern California and Northwest populations during 1990–2004;4, 5 and 67% in a northern U.K. cohort (1998–2002).6
For some patients with very low rectal cancer or other relative indications, an abdominoperineal resection may be the only realistic surgical option to treat the cancer, and it results in a permanent ostomy. However, some patients have a choice between permanent ostomy and sphincter-sparing surgery. When the probability of recurrence and survival are similar for the two surgical options, it is essential that patients have access to high-quality information so they can understand functional problems and their consequences following sphincter-sparing surgery or ostomy. Patients need information that is individualized to their circumstances so that they can make the best decision for themselves, based on their individual values and preferences.7 In addition, patient-centered information gives many patients a greater health locus of control, which has been linked to better long-term health-related quality of life (QOL).8, 9 Information, the capacity to participation in decision-making, and a degree of control over the treatment decision improves adjustment in many patients.10, 11
Impaired bowel function is a primary QOL outcome of low rectal cancer surgery.12 Impaired bowel function can affect QOL by generating pain, urgent and frequent bowel movements, incontinence, embarrassment, negative body image, poor sleep, impaired sexual function, and stigma. These symptoms can also interfere with the patient’s ability to sustain regular employment. Although not all patients experience these negative outcomes, reducing bowel symptoms and their consequent psychological and social effects should be a key goal in the decision-making for all rectal cancer procedures. Patients’ reactions to the differing consequences of ostomy and sphincter-sparing surgery, however, depend on their particular circumstances, which only they can judge. Thus, for patients who may have a choice in rectal cancer procedures, there is a need to gain an understanding of the comparative long-term patient-reported outcomes of ostomy and sphincter-sparing surgery.13
Imagining a future that has never been experienced is challenging for anyone, and rectal cancer is not often talked about. Thus, rectal cancer patients may assume that sphincter-sparing surgery is better, while living with an ostomy is worse, given general cultural notions of unpleasantness associated with ostomies and handling feces.14 With such stigma, many patients will choose sphincter-sparing surgery over ostomy, but frequently, this choice is not fully informed. Patients might not understand that impaired bowel function is common after sphincter-sparing surgery, and that many patients with ostomy adjust well to living permanently with a stoma.
Discussions regarding rectal cancer surgery are very stressful for patients and families. For the surgeon, informing patients with rectal cancer can be challenging. While a significant amount of time may be used to discuss long-term outcomes, patients may not fully synthesize information about impaired bowel function into an understanding of its long-term consequences because they are frightened and overwhelmed by the cancer diagnosis, feel a strong aversion to having a permanent ostomy, or prefer to defer decision-making to the surgeon.15 Furthermore, information provided by the surgeon might be insufficient,16, 17 fragmented and inconsistent,18 and potentially influenced by the hospital19 and the surgeon’s training.20 Some patients express regret about not having fully participated in the decision-making process about the type of surgery and have lingering doubts about whether they made the right choice.15 This regret may be particularly strong in patients who have a temporary stoma, who must adjust to life with a stoma and then adjust to functional alterations after reversal. In addition, patients who have had a temporary stoma may have experienced issues (i.e. stoma leakage, dehydration) secondary to the proximal nature of the stoma that would be less likely with a permanent ostomy, because permanent ostomies tend to be created with more distal colon. Once the ostomy approach is selected, no other options are available. With sphincter-sparing surgery, patients can elect to have an ostomy later if their bowel function is unacceptable, although the surgical procedure can be quite difficult and may be associated with other complications.21
We believe that it is essential to help patients picture how their particular life circumstances may affect long-term adjustment to ostomy and sphincter-sparing surgery. These circumstances include their frailty, comorbidity, and ability to care for themselves, gender, employment and income, lifestyle (family and social activities, recreation, and community), and social support, among others.22 This review article compares long-term patient-reported outcomes between rectal cancer patients who underwent ostomy or sphincter-sparing surgery, with or without a temporary ostomy. This article provides detailed information to help surgeons and patients discuss surgical options, and to help patients discuss their options with helpful loved ones. This report is intended to elucidate the range of factors that patients find salient about living with ostomy or sphincter-sparing surgery, and to help each patient imagine, based on other patients’ experiences, how their lives might change over the long-term. This report is focused on long-term (>5 years) patient-centered outcomes and provides a brief review of oncologic outcomes including recurrence.
Approach
We conducted a systematic review to examine the question: for the surgical treatment of rectal cancer, what are the long-term (>5 years post-surgery) patient-reported outcomes following ostomy compared with sphincter-sparing surgery? The first author implemented a search strategy, during July to December 2015, in MEDLINE. Every search included the MeSH major topic “rectal neoplasms/surgery”; in addition, searches included one of the following terms in any field: patient-centered, quality of life, stigma, body image, sexuality, participation, employment, decision aid, bowel function survey, low anterior resection syndrome, or ostomy complication. We restricted the search to English-language reports, published since January 1, 2000, of clinical trials, comparative studies, meta-analyses, multicenter studies, observational studies, pragmatic clinical trials, randomized controlled trials, reviews, and systematic reviews. The number of reports identified was 218. The first author read the title of every report to determine its relevance: 93 compared laparoscopic with open surgery, while 84 addressed other issues that were not pertinent to the comparison of sphincter-sparing surgery with ostomy or presented no original data or synthesis, and these 177 reports were removed from the review. The number of reports remaining was 41; in addition to reading these reports, we also reviewed the references they cited, obtaining and reading those that were relevant to the study question.
We focused the review on studies of long-term patient-reported outcomes (>5 years) in which it was possible to compare outcomes from sphincter-sparing surgery versus ostomy. The studies included in the review, although largely consistent in how they conceptualized long-term patient-reported outcomes, used a variety of questionnaires. These included the City of Hope Quality of Life Colorectal Cancer questionnaire, which was specifically designed for ostomies and cancer survivors with and sphincter-sparing surgery, the Functional Assessment of Cancer Therapy-Colorectal Specific Questionnaire, the European Organisation for Research and Treatment of Cancer QLQ-C30, the Short-Form 36 Version 2, the Brief Pain Inventory, and ad-hoc symptom scales.23–31
For the purpose of this report, we conceptualize patient-reported outcomes using the framework shown in Figure 1. It identifies components of QOL – physical, social, psychological and spiritual well-being – together with health-care issues, occupational and financial concerns, and concerns that are specific to having an ostomy. Each of these dimensions is set within the context of the patient’s individual characteristics, the most salient of which are frailty, comorbidity and self-care capacity, as well as gender, employment, income, lifestyle, and social support.
Figure 1.
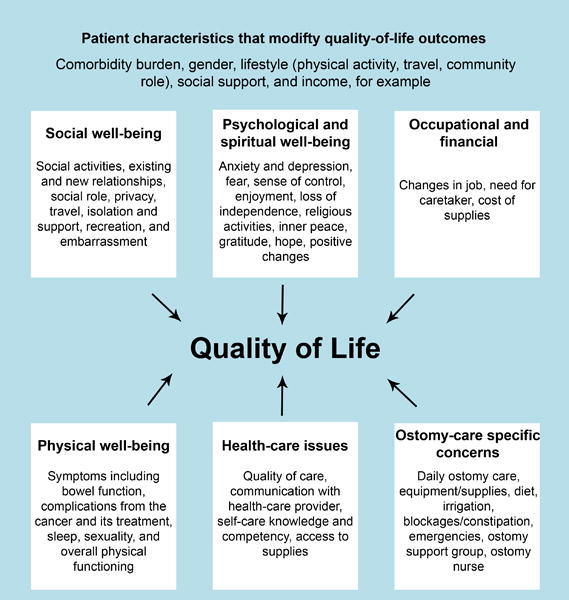
Framework
Key Predictors of Quality of Life
Immediately after their rectal cancer surgery, many patients discover that they need to undergo training, purchase equipment, and use pads and diapers to manage their bowel function. In addition, patients with an ostomy must adjust to the additional time needed for ostomy care, while persons who undergo sphincter-sparing surgery must adjust to changes in bowel function.32, 33 Patients can also experience shock, feel “not normal,” have fear and anxiety, experience less enjoyment, feel less attractive, express the inability to find meaning in life, find that they must change their daily activities, and discover that their sleep is disrupted because of ostomy malfunction or a need use the bathroom more often. These experiences are common to both ostomy and sphincter-sparing surgery.
These patients should know that over the long-term, some patients experience the same or better QOL that they had before their surgery, although other patients experience reduced QOL. It is important to keep in mind that the most important factors that determine long-term QOL are largely out of the patient’s control and are not related to the choice of ostomy vs. sphincter-sparing surgery. These factors include recurrent and metastatic colorectal cancer, radiotherapy treatment and complications, surgical complications, functional status, and comorbidities.34–41 The patient’s inherent resilience is another key factor in long-term QOL.27, 42–44 In addition, QOL can improve with time because the effects of the surgery recede, people learn how to cope, and older people simply tend to report better QOL.38, 42, 43
That being said, some patients have a choice between ostomy and sphincter-sparing surgery and want to make the choice that best enhances their long-term QOL. Studies that have compared ostomy with sphincter-sparing surgery are not entirely consistent with one another. Some studies find that the average patient with ostomy has worse overall long-term QOL than the average patient with sphincter-sparing surgery,38, 42, 45 while other studies find no differences in overall QOL,2, 41, 46–55 On the other hand, in various studies, subdomains of QOL (physical, social, psychological, or spiritual) were found to be higher or lower for ostomy compared with sphincter-sparing surgery as detailed in later sections of this report.2
Making sense of these research findings is not straightforward. First, patients with ostomy may be different from patients with sphincter-sparing surgery in important ways that affect QOL. Differences can include pre-existing health problems, the aggressiveness of the tumor, the use of chemotherapy and radiation therapy, and post-operative complications.13, 37, 50–55 These factors reduce QOL regardless of choice of surgery. Second, outcomes after sphincter-sparing surgery are heterogeneous. Patients with low rectal cancers (≤6 cm from the anus) will be more likely to have part of their anal sphincter removed and thus will be more likely to have worse bowel function than those whose cancers are higher up in the rectum.12 Finally, applying information from a research study to an individual patient is challenging because no patient is average, with many factors affecting the individual’s long-term bowel function and QOL. For example, men and women differ in their response to rectal cancer surgery, as do those with comorbidities, with greater or less social support, or who depend on others for personal care.12, 42, 47, 56–60
Notwithstanding these challenges in interpreting the research evidence, the existing studies have brought forth some important insights, and these insights are helpful to the patient who is facing the choice between ostomy and sphincter-sparing surgery. In the following sections, we review specific challenges that rectal cancer survivors face and how these challenges are influenced by the choice of surgery.
Comparison of Bowel Function
Ostomy patients empty their bowels into an external ostomy pouch. For patients with an ostomy, bowel function is assessed through the frequency, convenience, and privacy of pouch changes, dealing with gas and odor from the pouch, and changes in diet and activity to increase control over the rate and timing of pouch fills.25, 26 When an ostomy pouch is emptied, it needs to be rinsed out before disposal or reattachment to the stoma. This means having a source of water convenient to the toilet, which is frequently not the case in public restrooms. Some ostomy patients experience reduced QOL because their bowel function is no longer controllable or private. They feel embarrassed in social settings when their ostomy pouch “burbles” or smells, or because the pouch fills suddenly and needs to be emptied or “burped”.42, 61
Patients with sphincter-sparing surgery empty their bowels through their anus. Bowel function is impaired especially for those patients whose rectal cancer is low in the rectum, likely due to alterations in the anatomy of the colon, pelvic floor and anal sphincter. Poor function is likely compounded because of scarring after radiation.17, 41, 62–65 For patients with sphincter-sparing surgery, bowel function is assessed by measuring how often patients cannot get to the toilet in time, soil undergarments, use pads or diapers, have gas, diarrhea and loose stools, and change diet and activities to improve bowel control.66, 67 This collection of bowel symptoms affecting patients with sphincter-sparing surgery has been termed “low anterior resection syndrome,” or LARS.68–74 Bowel movements may be urgent, frequent, and clustered. Compared to ostomy patients, those with sphincter-sparing surgery have more pain, diarrhea, and constipation.46, 53 In addition, some patients with sphincter-sparing surgery have reduced control over their bowel function.68 For example, in one study, 45% reported occasional incontinence, while 16% reported complete incontinence.38 Other studies have reported liquid or solid fecal incontinence in 30% of patients and nocturnal incontinence in 53% of patients,46 indicating a high prevalence of bowel symptoms associated with sphincter-sparing surgery for low-rectal cancer.75–78 Poor bowel control reduces QOL79–82 primarily through embarrassment and social well-being, rather than physical well-being,42 and it can cause pain.
Comparison of Psychological Effects
Ostomy patients report feelings of embarrassment, stigma, and poor body image.14, 37, 45, 51, 53, 61, 83–90 Embarrassment stems from leakage, gas, and odor related to the ostomy pouch. Younger patients (under 70 years) and persons without a partner express higher levels of embarrassment. Embarrassment is related to anxiety and depression, more difficulty with meeting new people, dissatisfaction with appearance, interference with relationships and intimacy, greater feelings of isolation, and difficulty looking at the ostomy. One study noted that ostomy affected psychological health more strongly in women than men.42 Among patients with sphincter-sparing surgery, social function and role functioning are higher in persons without bowel symptoms.69, 81
Comparison of Social Well-Being
Participating in social activities such as work, interacting with family and friends, recreation, religious gatherings, and community service is important to most people, including cancer patients. The ability to continue participating in these activities is a key predictor of QOL among rectal cancer patients. It is more important than bowel function or whether the patient had an ostomy or sphincter-sparing surgery.14, 42
For patients with low rectal cancer and sphincter-sparing surgery, the ability to participate in activities is largely determined by bowel function.14 In addition, ostomy patients may restrict their social participation because of embarrassment.14 However, one study that was focused only on low rectal tumors (within 6 cm of the anal verge) found that patients with an ostomy had better social functioning than patients with sphincter-sparing surgery.46 Lower participation in activities is related to lower QOL.(McMullen, submitted)
Most rectal cancer patients are beyond retirement age and may not be concerned about their ability to work for pay. Other patients may need to work full- or part-time, and many older individuals get satisfaction from volunteering. Patients with ostomy, and possibly those patients with poor bowel function related to sphincter-sparing surgery, may face barriers to working and volunteering and may experience reduced support from their employers and coworkers.91
Comparison of Other Effects
Medical complications
In the days and weeks following surgery, the most common complication of surgery to create an ostomy is perineal wound failure that potentially requires extensive wound care; wound failure occurs in 25 to 35% of patients.92 The most common complication of sphincter-sparing surgery is anastomotic leak, which creates the potential that fecal matter will pass into the abdominal cavity and cause a serious infection. .93–95 It has become common in recent years to use a temporary ostomy to avoid serious intra-abdominal infections related to anastomotic leaks, which has lowered the risk of anastomotic leak from approximately 24% to approximately 10%.96–98 In addition, over the long term, as many as 10% of ostomy patients and 3% of patients with sphincter-sparing surgery experience urinary retention and intestinal obstruction.68
Sleep
In studies that compared ostomy with sphincter-sparing surgery, patients with ostomy reported greater sleep disturbance.44, 46
Intimacy and sexual functioning
Some rectal cancer survivors report challenges with intimacy and sexuality.38, 47, 51, 52, 66,99–102
The effect of rectal cancer on sexual activity appears to be different in men and women. As many as 40% of men report lower sexual activity after rectal cancer surgery, and as many as 50% reported new erectile dysfunction, although the role of radiation therapy and type of cancer surgery have not been clearly evaluated.41, 47, 101, 102 Three studies reported greater sexual difficulties after ostomy compared with sphincter-sparing surgery,38, 51, 62, 82 while others found no differences,40, 46, 83 and one found better sexual function in those with ostomy.53 In these studies, patients who had ostomy more often had low rectal tumors, while patients who had sphincter-sparing surgery more often had tumors that were higher in the rectum, so that the location of the tumor and effects of radiation make these results particularly difficult to compare.
In two studies, women who had had rectal cancer reported more challenges with sexuality and intimacy than men,38, 101 while one study found no difference.40 Radiation treatment and changes to the vagina and surrounding tissues can cause intercourse to become painful. Other women report that changes in sexuality resulting from rectal cancer were not problematic; for these women, lower sexual activity was appreciated as a life passage related to getting older.101
Comparison of Recurrence Rates
Observational studies have compared the risk of recurrence in cohorts of patients who received sphincter-sparing surgery versus ostomy, but these studies are not comparable, because patients were not randomized to one surgery or the other.104 Consequently, factors that influenced the choice of surgery might well have resulted in differences in oncologic outcomes. These factors include the bulkiness and aggressiveness of the tumor and the tumor’s response to neo-adjuvant therapy. That being said, 5-year local recurrence rates on the order of 5% have been achieved following each of these surgical approaches.104, 105
Choosing Ostomy or Sphincter-Sparing Surgery
We are not aware of any validated tool or evidence-based resource to assist with the decision to undergo ostomy or sphincter-sparing surgery. A decision aid has been described that focuses on three aspects of ostomy (not having bowel movements “in the usual way”, the inconvenience of stoma care, and the risk of long-term stoma complications) and three aspects of anastomosis (potential unpredictability of bowel function, fecal incontinence, and risk of rehospitalization).106 However, the tool does not go in depth into the other themes we discuss in this report and has not been evaluated. Therefore, for the purpose of summarizing the information in this report, we have created a list of topics, relevant to initial treatment decision-making, that may be useful to health providers when helping patients newly diagnosed with rectal cancer choose between the two surgical options (Box 1). This list is not formally used at our institutions and has not been systematically assessed. We have encountered patients who find ostomy to be so stigmatizing that they accepted a hypothetical level of bowel function to avoid the ostomy. Nonetheless, informing patients by individualizing the research evidence to their circumstances may improve decision making and the setting of realistic expectations. Further research into decision support tools is paramount to both patients and physicians.
Box 1. Discussion Guide: Initial Treatment Decision-Making – Key Information and Discussion Topics.
Informational. Many important factors that determine long-term well-being are not primarily related to the choice of ostomy vs. sphincter-sparing surgery. These factors include the size and extent of the tumor, whether the patient needs radiotherapy, complications, and the patient’s underlying functional status and comorbidities.
- Informational. Ostomy patients empty their bowels into an external ostomy pouch, while patients with sphincter-sparing surgery empty their bowels through their anus. Each surgery has its own problems.
- Patients with an ostomy may need to empty their pouch frequently and at unexpected times, this may be inconvenient and they may not have the privacy they need. In addition, they must deal with gas and odor and the need to change their diet and activities to increase control over pouch fills. Some patients with ostomy feel embarrassed in social settings when their ostomy pouch “burbles” or smells, or because the pouch fills suddenly and needs to be emptied. When an ostomy pouch is emptied, it may need to be rinsed out before disposal or reattachment to the stoma. Ostomy patients typically carry “ostomy kits” that include bottles of water for washing out their pouches. In addition, some patients with ostomy feel disgust with the way they look.
- Some patients with sphincter-sparing surgery may not get to the toilet in time. They may soil their undergarments, or need to use pads or diapers. Some patients have diarrhea and loose stools, and need to change their diet and activities to improve bowel control. Some patients with sphincter-sparing surgery have more pain than patients with ostomy.
Discussion Topic. How important is it to you that your body looks the same after your surgery? Patients who want to look the same might do better with sphincter-sparing surgery.
Discussion Point. As you get older, you might need help taking care of your bowel function. This help is different for ostomy and sphincter-sparing surgery. Is there someone you could depend on to help you? How do you feel about needing this kind of help?
- Discussion Topic. In some patients, but not all, impaired bowel function affects favored activities. What activities are most important to you and how would they be affected if you had an ostomy or sphincter-sparing surgery? These activities might be affected by the appearance of your body, access to a bathroom, the need for privacy in public bathrooms, or embarrassment you might feel with gas or incontinence.
Check the activities that are most important to you Specify the activity (e.g., gardening) How would this activity be affected by ostomy? How would this activity be affected by sphincter-spring surgery? [ ] Activities I do by myself [ ] Interactions with family and friends [ ] Recreation/sports [ ] Religious activities [ ] Volunteering/community service [ ] Work [ ] Sex and intimacy
Survivorship Care
Patients with ostomies have described their initial healthcare experiences of learning how to live with an ostomy, including initial guidance about ostomy self-care following the surgery, teaching “failures,” home visits, peer education, and accessing the internet and ostomy association newsletters. Specialized nurses have been trained to enhance the functioning of patients with ostomies, and ostomy patients report the need for continued access to these nurses to manage persistent symptoms.15 Persistent ostomy-related issues include skin problems at the ostomy site, clothing restrictions and adaptations, dietary concerns, change in body weight and its effect on ostomy care, issues related to ostomy equipment and daily self-care, late complications such as hernias, continued adjustments to ostomy over the life course, and the need to pay for ostomy supplies.14, 32, 95, 107–109
Special health care needs for patients with sphincter-sparing surgery have not been adequately described, but include skin problems from frequent wiping, the use of pads or diapers, dietary adjustments, lifestyle adjustments, and travel restrictions.68, 110 Few, if any, training programs for nurses or other health care providers exist to enhance functioning in patients with sphincter-sparing surgery,111, 112 and interventions primarily involve strategies to increase the strength of the pelvic floor, such as Kegel exercises, biofeedback, and sacral nerve stimulation.33, 113–117
A critical role of the primary care provider is to refer patients who have poor bowel function after sphincter-sparing surgery to experienced providers who can offer various activity-based, pharmacologic, and dietary interventions. In addition, the primary care provider should consider surgical referral to discuss conversion to an ostomy, although the procedure can be difficult and has the potential for complications. Box 2 is a clinical assessment tool for gauging long-term bowel function among rectal cancer survivors; it was adapted from the validated Memorial Sloan Kettering Cancer Center (MSKCC) Bowel Function Instrument,59 where it has been in use for 10 years as a research tool and for 2 years as a clinical assessment tool. A similar instrument, the Low Anterior Resection Syndrome Score, was developed and validated in Denmark and has been translated to English.69–71
Box 2. Clinical Assessment Tool for Long-Term Follow-up of Bowel Function.
| If ostomy | If sphincter-sparing surgery | |
| 1. | How many times each day do you empty your pouch? | How many times each day do you have a bowel movement? |
| 2. | How often does your pouch leak? | How often do you get to the toilet too late? |
| 3. | Do you have problems with gas or odor? | How often do you use a pad or diaper? |
| 4. | Do you have abdominal pain or obstruction? | Do you have abdominal pain or obstruction? |
| 5. | Can you eat and drink the foods you want? | Can you eat and drink the foods you want? |
| 6. | Are you satisfied with your appearance? | [Not applicable] |
| 7. | Does your ostomy get in the way of doing the things you like to do? | Does your bowel function get in the way of doing the things you like to do? |
| … working | … working | |
| … interacting with friends and family | … interacting with friends and family | |
| … traveling | … traveling | |
| … participating in religious activities | … participating in religious activities | |
| … participating in community service/volunteer work | … participating in community service/volunteer work | |
| … participating in recreation and sports | … participating in recreation and sports | |
| 8. | Are you satisfied with your sexual and intimate activity? | Are you satisfied with your sexual and intimate activity? |
| 9. | Does your ostomy affect your sleep? | Does your bowel function affect your sleep? |
| 10. | Do you feel embarrassed by your ostomy? | Do you feel embarrassed by your bowel function? |
| 11. | Are you having any problems with the skin around your ostomy? | Are you having any problems with the skin around your anus? |
| 12. | Do you need help with your ostomy, and do you get the help you need? | Do you need help with your bowel function, and do you get the help you need? |
| 13. | Are you having any other problems with your ostomy? | Are you having any other problems with your rectal cancer surgery? |
| 14. | If persistent problems: Would you like to talk to an ostomy nurse? | If persistent problems: Would you like to talk to a surgeon about options for improving control over your bowel function? |
Conclusions and Future Directions
The topics included in this review are appropriate for doctor-patient discussions in advance of surgery and for following patients over their life course, to assure the best possible outcomes that can be obtained. Both sphincter-sparing surgery and rectal excision with ostomy are effective surgical approaches to low rectal cancer. Although sphincter-sparing surgery is clearly perceived as the preferred option for patients, it may not always be appropriate given a patient’s preferences and circumstances. Decisions about rectal cancer surgery may not be optimal without an informed discussion using the existing evidence about the comparative long-term consequences of the two approaches, and without eliciting patients’ preferences and circumstances.118 Information offers the patient the potential to anticipate their future challenges, to increase their internal health locus of control, to learn from patients who have gone before them, and ultimately to improve coping.
Current unmet needs of rectal cancer survivors are broadly similar to those of many cancer survivors.119 Research into bowel function and long-term patient-reported outcomes is more extensive for ostomy than for sphincter-sparing surgery. Furthermore, the outcomes after sphincter preserving surgery are so varied and it is difficult for surgeons to predict and/or preoperatively describe the expected bowel function to patients. Supportive interventions that focus on sphincter-sparing surgery are lacking, even though there are many more patients with sphincter-sparing surgery than permanent ostomy. In addition, many studies have compared ostomy patients with low rectal tumors to patients with higher tumors who did not receive an ostomy, so that the comparison between the two surgeries may be confounded.
Box 3. Resources.
For Ostomy and Sphincter-Sparing Surgery
National Cancer Institute Rectal Cancer Treatment (PDQ®): http://www.cancer.gov/types/colorectal/patient/rectal-treatment-pdq
American Cancer Society Colorectal Cancer Survivorship Care Guidelines: http://www.cancer.org/cancer/news/news/acs-releases-long-term-care-guidelines-for-colon-and-rectal-cancer-survivors
Reeves, C. MD Anderson Cancer Center. Colorectal Cancer Survivorship, Late Effects of Surgery: http://www3.mdanderson.org/streams/FullVideoPlayer.cfm?xml=cfg%2FPOE-Survivorship-Late-Effects-Reeves–cfg
For Ostomy
International Ostomy Association: http://www.ostomyinternational.org/
Ostomy Association of America: http://www.ostomy.org/Home.html
Wound, Ostomy, and Continence Nurses Society: http://www.wocn.org/
Meet an OstoMate: http://www.meetanostomate.org/phpBB2/viewtopic.php?t=186
For Sphincter-Sparing Surgery
Memorial Sloan Kettering Cancer Center, Managing Bowel Function After Your Low Anterior Resection: https://www.mskcc.org/cancer-care/patient-education/managing-bowel-function-after-your-low-anterior-resection
LARS questionnaire. Juul T, Ahlberg M, Biondo S, et al. International validation of the low anterior resection syndrome score. Ann Surg. 2014;259:728-34. PMID 23598379.
Acknowledgments
Funding: This research was made possible by Grant Number R01 CA106912, HRQOL in Colorectal Cancer Survivors with Stomas, from the National Cancer Institute, National Institutes of Health in collaboration with resources and the use of facilities provided at the Southern Arizona VA Health Care System, Tucson, Arizona and Kaiser Permanente.
Footnotes
Conflict of interest: Dr. Herrinton received support from MedImmune; this support did not pose a conflict of interest for this manuscript.
Contributor Information
Lisa J. Herrinton, Division of Research, Kaiser Permanente Northern California.
Andrea Altschuler, Division of Research, Kaiser Permanente Northern California.
Carmit K. McMullen, Center for Health Research, Kaiser Permanente Northwest.
Joanna E. Bulkley, Center for Health Research, Kaiser Permanente Northwest.
Mark C. Hornbrook, Center for Health Research, Kaiser Permanente Northwest.
Virginia Sun, Division of Nursing Research and Education, Department of Population Sciences, City of Hope, Duarte, California.
Christopher S. Wendel, Arizona Center on Aging, University of Arizona College of Medicine.
Marcia Grant, Division of Nursing Research and Education, Department of Population Sciences, City of Hope, Duarte, California.
Carol M. Baldwin, College of Nursing & Health Innovation, Arizona State University, Phoenix, AZ.
Wendy Demark-Wahnefried, Nutrition Sciences, University of Alabama at Birmingham.
Larissa K.F. Temple, Memorial Sloan Kettering Cancer Center, New York, New York.
Robert S. Krouse, Southern Arizona Veterans Affairs Health Care System and University of Arizona College of Medicine, Tucson, Arizona.
References
- 1.Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2012. National Cancer Institute; Bethesda, MD: Available from URL: http://seer.cancer.gov/csr/1975_2012/. [accessed Apr 15, 2015]. Available from URL: http://seer.cancer.gov/csr/1975_2012/browse_csr.php?sectionSEL=6&pageSEL=sect_06_table.08.html. [accessed September 9, 2015] [Google Scholar]
- 2.Pachler J, Wille-Jorgensen P. Quality of life after rectal resection for cancer, with or without permanent colostomy. Cochrane Database Syst Rev. 2012;12:CD004323. doi: 10.1002/14651858.CD004323.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Cancer Institute. Rectal Cancer Treatment (PDQ®) Available from URL: http://www.cancer.gov/types/colorectal/patient/rectal-treatment-pdq. [accessed September 9, 2015]
- 4.Mohammed S, Anaya DA, Awad SS, et al. Sphincter preservation rates after radical resection for rectal cancer in the United States veteran population: opportunity for improvement in early disease. Ann Surg Oncol. 2015;22:216–23. doi: 10.1245/s10434-014-4101-z. [DOI] [PubMed] [Google Scholar]
- 5.Chongpison Y, Hornbrook MC, Harris RB, et al. Self-reported depression and perceived financial burden among long-term rectal cancer survivors. Psychooncology. 2015 Sep 14; doi: 10.1002/pon.3957. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Borowski DW, Kelly SB, Bradburn DM, et al. Northern Region Colorectal Cancer Audit Group Impact of surgeon volume and specialization on short-term outcomes in colorectal cancer surgery. Br J Surg. 2007 Jul;94(7):880–9. doi: 10.1002/bjs.5721. [DOI] [PubMed] [Google Scholar]
- 7.Mulsow J, Winter DC. Sphincter preservation for distal rectal cancer–a goal worth achieving at all costs? World J Gastroenterol. 2011;17(7):855–61. doi: 10.3748/wjg.v17.i7.855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Asadi-Lari M, Tamburini M, Gray D. Patients’ needs, satisfaction, and health related quality of life: towards a comprehensive model. Health Qual Life Outcomes. 2004;2:32. doi: 10.1186/1477-7525-2-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kulpa M, Kosowicz M, Stypuła-Ciuba BJ, et al. Anxiety and depression, cognitive coping strategies, and health locus of control in patients with digestive system cancer. Prz Gastroenterol. 2014;9:329–35. doi: 10.5114/pg.2014.47895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perez S, Néron S, Benc R, et al. The meaning and experience of patients undergoing rectal high-dose-rate brachytherapy. Cancer Nurs. 2015 doi: 10.1097/NCC.0000000000000246. [DOI] [PubMed] [Google Scholar]
- 11.O’Connor G, Coates V, O’Neill S. Randomised controlled trial of a tailored information pack for patients undergoing surgery and treatment for rectal cancer. Eur J Oncol Nurs. 2014 Apr;18(2):183–91. doi: 10.1016/j.ejon.2013.10.011. [DOI] [PubMed] [Google Scholar]
- 12.Hendren S, Abdelsattar Z. Sphincter-preserving surgery for rectal cancer: a controversial measure of quality. Ann Surg Oncol. 2015;22:9–10. doi: 10.1245/s10434-014-4104-9. [DOI] [PubMed] [Google Scholar]
- 13.Russell MM, Ganz PA, Lopa S, et al. Comparative effectiveness of sphincter-sparing surgery versus abdominoperineal resection in rectal cancer: patient-reported outcomes in National Surgical Adjuvant Breast and Bowel Project randomized trial R-04. Ann Surg. 2015;261:144–8. doi: 10.1097/SLA.0000000000000594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McMullen CK, Hornbrook MC, Grant M, et al. The greatest challenges reported by long-term colorectal cancer survivors with stomas. J Support Oncol. 2008;6(4):175–82. [PubMed] [Google Scholar]
- 15.Sun V, Grant M, McMullen CK, et al. From diagnosis through survivorship: health-care experiences of colorectal cancer survivors with ostomies. Support Care Cancer. 2014;22(6):1563–70. doi: 10.1007/s00520-014-2118-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Snijders HS, Kunneman M, Bonsing BA, et al. Preoperative risk information and patient involvement in surgical treatment for rectal and sigmoid cancer. Colorectal Dis. 2014;16(2):O43–9. doi: 10.1111/codi.12481. [DOI] [PubMed] [Google Scholar]
- 17.Scheer AS, O’Connor AM, Chan BP, et al. The myth of informed consent in rectal cancer surgery: what do patients retain? Dis Colon Rectum. 2012;55(9):970–5. doi: 10.1097/DCR.0b013e31825f2479. [DOI] [PubMed] [Google Scholar]
- 18.Van Mossel C, Leitz L, Scott S, et al. Information needs across the colorectal cancer care continuum: scoping the literature. Eur J Cancer Care (Engl) 2012;21(3):296–320. doi: 10.1111/j.1365-2354.2012.01340.x. [DOI] [PubMed] [Google Scholar]
- 19.Dodgion CM, Neville BA, Lipsitz SR, et al. Hospital variation in sphincter preservation for elderly rectal cancer patients. J Surg Res. 2014;191(1):161–8. doi: 10.1016/j.jss.2014.03.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Augestad KM, Lindsetmo RO, Stulberg JJ, et al. System-based factors influencing intraoperative decision-making in rectal cancer by surgeons: an international assessment. Colorectal Dis. 2012;14(10):e679–88. doi: 10.1111/j.1463-1318.2012.03093.x. [DOI] [PubMed] [Google Scholar]
- 21.Genser L, Manceau G, Karoui M, et al. Postoperative and long-term outcomes after redo surgery for failed colorectal or coloanal anastomosis: retrospective analysis of 50 patients and review of the literature. Dis Colon Rectum. 2013;56:747–55. doi: 10.1097/DCR.0b013e3182853c44. [DOI] [PubMed] [Google Scholar]
- 22.Jansen L, Koch L, Brenner H, et al. Quality of life among long-term (≥5 years) colorectal cancer survivors–systematic review. Eur J Cancer. 2010;46(16):2879–88. doi: 10.1016/j.ejca.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 23.Mohler MJ, Coons SJ, Hornbrook MC, et al. The health-related quality of life in long-term colorectal cancer survivors study: objectives, methods and patient sample. Curr Med Res Opin. 2008;24(7):2059–70. doi: 10.1185/03007990802118360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krouse RS, Mohler MJ, Wendel CS, et al. The VA Ostomy Health-Related Quality of Life Study: objectives, methods, and patient sample. Curr Med Res Opin. 2006;22(4):781–91. doi: 10.1185/030079906X96380. [DOI] [PubMed] [Google Scholar]
- 25.Grant M, Ferrell B, Dean G, et al. Revision and psychometric testing of the City of Hope Quality of Life-Ostomy Questionnaire. Qual Life Res. 2004;13(8):1445–57. doi: 10.1023/B:QURE.0000040784.65830.9f. [DOI] [PubMed] [Google Scholar]
- 26.Wendel CS, Grant M, Herrinton L, et al. Reliability and validity of a survey to measure bowel function and quality of life in long-term rectal cancer survivors. Qual Life Res. 2014;23(10):2831–40. doi: 10.1007/s11136-014-0724-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Popek S, Grant M, Gemmill R, et al. Overcoming challenges: life with an ostomy. Am J Surg. 2010;200(5):640–5. doi: 10.1016/j.amjsurg.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 28.Bakas T, McLennon SM, Carpenter JS, et al. Systematic review of health-related quality of life models. Health Qual Life Outcomes. 2012;10:134. doi: 10.1186/1477-7525-10-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harji DP, Griffiths B, Velikova G, et al. Systematic review of health-related quality of life issues in locally recurrent rectal cancer. J Surg Oncol. 2015;111:431–8. doi: 10.1002/jso.23832. [DOI] [PubMed] [Google Scholar]
- 30.Maslyankov S, Penchev D, Todorov G, et al. A meta-analysis of quality of life, estimated by questionnaires of the European Organization for Research and Treatment of Cancer (EORTC) after Rectal Cancer Surgery. Chirurgia (Bucur) 2015;110:356–61. [PubMed] [Google Scholar]
- 31.Thaysen HV, Jess P, Laurberg S. Health-related quality of life after surgery for primary advanced rectal cancer and recurrent rectal cancer: a review. Colorectal Dis. 2012 Jul;14(7):797–803. doi: 10.1111/j.1463-1318.2011.02668.x. [DOI] [PubMed] [Google Scholar]
- 32.Sun V, Grant M, McMullen CK, et al. Surviving colorectal cancer: long-term, persistent ostomy-specific concerns and adaptations. J Wound Ostomy Continence Nurs. 2013;40(1):61–72. doi: 10.1097/WON.0b013e3182750143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sloots K, Barlett L. Practical strategies for treatment postsurgical bowel dysfunction. J Wound Ostomy Continence Nurs. 2009;36:522–7. doi: 10.1097/WON.0b013e3181b35e95. [DOI] [PubMed] [Google Scholar]
- 34.Parc Y, Zutshi M, Zalinski S, et al. Preoperative radiotherapy is associated with worse functional results after coloanal anastomosis for rectal cancer. Dis Colon Rectum. 2009 Dec;52(12):2004–14. doi: 10.1007/DCR.0b013e3181beb4d8. [DOI] [PubMed] [Google Scholar]
- 35.Lundby L, Krogh K, Jensen VJ, et al. Long-term anorectal dysfunction after postoperative radiotherapy for rectal cancer. Dis Colon Rectum. 2005 Jul;48(7):1343–9. doi: 10.1007/s10350-005-0049-1. [DOI] [PubMed] [Google Scholar]
- 36.Jain S, McGory ML, Ko CY, et al. Comorbidities play a larger role in predicting health-related quality of life compared to having an ostomy. Am J Surg. 2007;194(6):774–9. doi: 10.1016/j.amjsurg.2007.08.020. [DOI] [PubMed] [Google Scholar]
- 37.Hornbrook MC, Wendel CS, Coons SJ, et al. Complications among colorectal cancer survivors: SF-6D preference-weighted quality of life scores. Med Care. 2011;49(3):321–6. doi: 10.1097/MLR.0b013e31820194c8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Downing A, Morris EJ, Richards M, et al. Health-related quality of life after colorectal cancer in England: a patient-reported outcomes study of individuals 12 to 36 months after diagnosis. J Clin Oncol. 2015;33(6):616–24. doi: 10.1200/JCO.2014.56.6539. [DOI] [PubMed] [Google Scholar]
- 39.Finlayson E, Zhao S, Varma MG. Outcomes after rectal cancer surgery in elderly nursing home residents. Dis Colon Rectum. 2012;55(12):1229–35. doi: 10.1097/DCR.0b013e318267bfe3. [DOI] [PubMed] [Google Scholar]
- 40.Peng J, Shi D, Goodman KA, et al. Early results of quality of life for curatively treated rectal cancers in Chinese patients with EORTC QLQ-CR29. Radiat Oncol. 2011;6:93. doi: 10.1186/1748-717X-6-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Knowles G, Haigh R, McLean C, et al. Long term effect of surgery and radiotherapy for colorectal cancer on defecatory function and quality of life. Eur J Oncol Nurs. 2013;17(5):570–7. doi: 10.1016/j.ejon.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 42.Krouse RS, Herrinton LJ, Grant M, et al. Health-related quality of life among long-term rectal cancer survivors with an ostomy: manifestations by sex. J Clin Oncol. 2009;27(28):4664–70. doi: 10.1200/JCO.2008.20.9502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bulkley J, McMullen CK, Hornbrook MC, et al. Spiritual well-being in long-term colorectal cancer survivors with ostomies. Psycho-oncology. 2013;22(11):2513–21. doi: 10.1002/pon.3318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Baldwin CM, Grant M, Wendel C, et al. Gender differences in sleep disruption and fatigue on quality of life among persons with ostomies. J Clin Sleep Med. 2009;5(4):335–43. [PMC free article] [PubMed] [Google Scholar]
- 45.Hoerske C, Weber K, Goehl J, et al. Long-term outcomes and quality of life after rectal carcinoma surgery. Br J Surg. 2010;97(8):1295–303. doi: 10.1002/bjs.7105. [DOI] [PubMed] [Google Scholar]
- 46.How P, Stelzner S, Branagan G, et al. Comparative quality of life in patients following abdominoperineal excision and low anterior resection for low rectal cancer. Dis Colon Rectum. 2012;55(4):400–6. doi: 10.1097/DCR.0b013e3182444fd1. [DOI] [PubMed] [Google Scholar]
- 47.Guren MG, Eriksen MT, Wiig JN, et al. Abdominoperineal resection does not decrease quality of life in patients with low rectal cancer. Clinics (Sao Paulo) 2011;66:1035–40. doi: 10.1590/S1807-59322011000600019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Reshef A, Lavery I, Kiran RP. Factors associated with oncologic outcomes after abdominoperineal resection compared with restorative resection for low rectal cancer: patient- and tumor-related or technical factors only? Dis Colon Rectum. 2012;55:51–8. doi: 10.1097/DCR.0b013e3182351c1f. [DOI] [PubMed] [Google Scholar]
- 49.Omidvari S, Hamedi SH, Mohammadianpanah M, et al. Comparison of abdominoperineal resection and low anterior resection in lower and middle rectal cancer. J Egypt Natl Canc Inst. 2013;25:151–60. doi: 10.1016/j.jnci.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 50.de Campos-Lobato LF, Alves-Ferreira PC, Lavery IC, et al. Abdominoperineal resection does not decrease quality of life in patients with low rectal cancer. Clinics (Sao Paulo) 2011;66:1035–40. doi: 10.1590/S1807-59322011000600019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fucini C, Gattai R, Urena C, et al. Quality of life among five-year survivors after treatment for very low rectal cancer with or without a permanent abdominal stoma. Ann Surg Oncol. 2008;15:1099–106. doi: 10.1245/s10434-007-9748-2. [DOI] [PubMed] [Google Scholar]
- 52.Chuwa EW, Seow-Choen F. Outcomes for abdominoperineal resections are not worse than those of anterior resections. Dis Colon Rectum. 2006;49:41–49. doi: 10.1007/s10350-005-0227-1. [DOI] [PubMed] [Google Scholar]
- 53.Kasparek MS, Hassan I, Cima RR, Larson DR, et al. Quality of life after coloanal anastomosis and abdominoperineal resection for distal rectal cancers: sphincter preservation vs quality of life. Colorectal Dis. 2011;13:872–7. doi: 10.1111/j.1463-1318.2010.02347.x. [DOI] [PubMed] [Google Scholar]
- 54.Bossema ER, Seuntiëns MW, Marijnen CA, et al. The relation between illness cognitions and quality of life in people with and without a stoma following rectal cancer treatment. Psychooncology. 2011;20:428–34. doi: 10.1002/pon.1758. [DOI] [PubMed] [Google Scholar]
- 55.Cornish JA, Tilney HS, Heriot AG, et al. A meta-analysis of quality of life for abdominoperineal excision of rectum versus anterior resection for rectal cancer. Ann Surg Oncol. 2007;14:2056–68. doi: 10.1245/s10434-007-9402-z. [DOI] [PubMed] [Google Scholar]
- 56.Grant M, McMullen CK, Altschuler A, et al. Gender differences in quality of life among long-term colorectal cancer survivors with ostomies. Oncol Nurs Forum. 2011;38(5):587–96. doi: 10.1188/11.ONF.587-596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Altschuler A, Ramirez M, Grant M, et al. The influence of husbands’ or male partners’ support on women’s psychosocial adjustment to having an ostomy resulting from colorectal cancer. J Wound Ostomy Continence Nurs. 2009;36(3):299–305. doi: 10.1097/WON.0b013e3181a1a1dc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McMullen CK, Schneider J, Altschuler A, et al. Caregivers as healthcare managers: health management activities, needs, and caregiving relationships for colorectal cancer survivors with ostomies. Support Care Cancer. 2014;22(9):2401–8. doi: 10.1007/s00520-014-2194-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schmidt CE, Bestmann B, Küchler T, et al. Gender differences in quality of life of patients with rectal cancer. A five-year prospective study. World J Surg. 2005;29:1630–41. doi: 10.1007/s00268-005-0067-0. [DOI] [PubMed] [Google Scholar]
- 60.Feddern ML, Jensen TS, Laurberg S. Chronic pain in the pelvic area or lower extremities after rectal cancer treatment and its impact on quality of life: a population-based cross-sectional study. Pain. 2015;156:1765–71. doi: 10.1097/j.pain.0000000000000237. [DOI] [PubMed] [Google Scholar]
- 61.Mitchell KA, Rawl SM, Schmidt CM, et al. Demographic, clinical, and quality of life variables related to embarrassment in veterans living with an intestinal stoma. J Wound Ostomy Continence Nurs. 2007;34(5):524–32. doi: 10.1097/01.WON.0000290732.15947.9e. [DOI] [PubMed] [Google Scholar]
- 62.Konanz J, Herrle F, Weiss C, et al. Quality of life of patients after low anterior, intersphincteric, and abdominoperineal resection for rectal cancer–a matched-pair analysis. Int J Colorectal Dis. 2013;28(5):679–88. doi: 10.1007/s00384-013-1683-z. [DOI] [PubMed] [Google Scholar]
- 63.Ekkarat P, Boonpipattanapong T, Tantiphlachiva K, Sangkhathat S. Factors determining low anterior resection syndrome after rectal cancer resection: A study in Thai patients. Asian J Surg. 2015 doi: 10.1016/j.asjsur.2015.07.003. pii: S1015-9584(15)00086-X. [DOI] [PubMed] [Google Scholar]
- 64.Kasparek MS, Hassan I, Cima RR, Larson DR, Gullerud RE, Wolff BG. Long-term quality of life and sexual and urinary function after abdominoperineal resection for distal rectal cancer. Dis Colon Rectum. 2012;55:147–54. doi: 10.1097/DCR.0b013e31823d2606. [DOI] [PubMed] [Google Scholar]
- 65.Lange MM, den Dulk M, Bossema ER, et al. Cooperative Clinical Investigators of the Dutch Total Mesorectal Excision Trial Risk factors for faecal incontinence after rectal cancer treatment. Br J Surg. 2007;94:1278–84. doi: 10.1002/bjs.5819. [DOI] [PubMed] [Google Scholar]
- 66.Temple LK, Bacik J, Savatta SG, et al. The development of a validated instrument to evaluate bowel function after sphincter-preserving surgery for rectal cancer. Dis Colon Rectum. 2005;48(7):1353–65. doi: 10.1007/s10350-004-0942-z. [DOI] [PubMed] [Google Scholar]
- 67.Chen TY, Emmertsen KJ, Laurberg S. What are the best questionnaires to capture anorectal function after surgery in rectal cancer? Curr Colorectal Cancer Rep. 2015;11:37–43. doi: 10.1007/s11888-014-0217-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Desnoo L, Faithfull S. A qualitative study of anterior resection syndrome: the experiences of cancer survivors who have undergone resection surgery. Eur J Cancer Care (Engl) 2006;15:244–51. doi: 10.1111/j.1365-2354.2005.00647.x. [DOI] [PubMed] [Google Scholar]
- 69.Emmertsen KJ, Laurberg S. Low anterior resection syndrome score: development and validation of a symptom-based scoring system for bowel dysfunction after low anterior resection for rectal cancer. Ann Surg. 2012;255:922–8. doi: 10.1097/SLA.0b013e31824f1c21. [DOI] [PubMed] [Google Scholar]
- 70.Juul T, Battersby NJ, Christensen P, et al. for the UK LARS Study Group Validation of the English Translation of the Low Anterior Resection Syndrome Score (The LARS score) Colorectal Dis. 2015;21 doi: 10.1111/codi.12952. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 71.Juul T, Ahlberg M, Biondo S, et al. International validation of the low anterior resection syndrome score. Ann Surg. 2014;259:728–34. doi: 10.1097/SLA.0b013e31828fac0b. [DOI] [PubMed] [Google Scholar]
- 72.Bryant CL, Lunniss PJ, Knowles CH, et al. Anterior resection syndrome. Lancet Oncol. 2012;13:e403–8. doi: 10.1016/S1470-2045(12)70236-X. [DOI] [PubMed] [Google Scholar]
- 73.Pucciani F. A review on functional results of sphincter-saving surgery for rectal cancer: the anterior resection syndrome. Updates Surg. 2013;65:257–63. doi: 10.1007/s13304-013-0220-5. [DOI] [PubMed] [Google Scholar]
- 74.Ziv Y, Zbar A, Bar-Shavit Y, Igov I. Low anterior resection syndrome (LARS): cause and effect and reconstructive considerations. Tech Coloproctol. 2013;17:151–62. doi: 10.1007/s10151-012-0909-3. [DOI] [PubMed] [Google Scholar]
- 75.Bregendahl S, Emmertsen KJ, Lous J, Laurberg S. Bowel dysfunction after low anterior resection with and without neoadjuvant therapy for rectal cancer: a population-based cross-sectional study. Colorectal Dis. 2013;15:1130–9. doi: 10.1111/codi.12244. [DOI] [PubMed] [Google Scholar]
- 76.Lai X, Wong FK, Ching SS. Review of bowel dysfunction of rectal cancer patients during the first five years after sphincter-preserving surgery: a population in need of nursing attention. Eur J Oncol Nurs. 2013;17:681–92. doi: 10.1016/j.ejon.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 77.Maris A, Penninckx F, Devreese AM, et al. Persisting anorectal dysfunction after rectal cancer surgery. Colorectal Dis. 2013;15:e672–9. doi: 10.1111/codi.12291. [DOI] [PubMed] [Google Scholar]
- 78.Wells CI, Vather R, Chu MJ, et al. Anterior resection syndrome–a risk factor analysis. J Gastrointest Surg. 2015;19:350–9. doi: 10.1007/s11605-014-2679-x. [DOI] [PubMed] [Google Scholar]
- 79.Chen TY, Wiltink LM, Nout RA, et al. Bowel function 14 years after preoperative short-course radiotherapy and total mesorectal excision for rectal cancer: report of a multicenter randomized trial. Clin Colorectal Cancer. 2015;14:106–14. doi: 10.1016/j.clcc.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 80.Juul T, Ahlberg M, Biondo S, et al. Low anterior resection syndrome and quality of life: an international multicenter study. Dis Colon Rectum. 2014;57:585–91. doi: 10.1097/DCR.0000000000000116. [DOI] [PubMed] [Google Scholar]
- 81.Emmertsen KJ, Laurberg S, Rectal Cancer Function Study Group Impact of bowel dysfunction on quality of life after sphincter-preserving resection for rectal cancer. Br J Surg. 2013;100:1377–87. doi: 10.1002/bjs.9223. [DOI] [PubMed] [Google Scholar]
- 82.Digennaro R, Tondo M, Cuccia F, et al. Coloanal anastomosis or abdominoperineal resection for very low rectal cancer: what will benefit, the surgeon’s pride or the patient’s quality of life? Int J Colorectal Dis. 2013;28:949–57. doi: 10.1007/s00384-012-1629-x. [DOI] [PubMed] [Google Scholar]
- 83.Reese JB, Finan PH, Haythornthwaite JA, et al. Gastrointestinal ostomies and sexual outcomes: a comparison of colorectal cancer patients by ostomy status. Support Care Cancer. 2014;22(2):461–8. doi: 10.1007/s00520-013-1998-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Phelan SM, Griffin JM, Jackson GL, et al. Stigma, perceived blame, self-blame, and depressive symptoms in men with colorectal cancer. Psycho-oncology. 2013;22(1):65–73. doi: 10.1002/pon.2048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bossema ER, Seuntiëns MW, Marijnen CA, et al. The relation between illness cognitions and quality of life in people with and without a stoma following rectal cancer treatment. Psychooncology. 2011;20:428–34. doi: 10.1002/pon.1758. [DOI] [PubMed] [Google Scholar]
- 86.Taylor C, Morgan L. Quality of life following reversal of temporary stoma after rectal cancer treatment. Eur J Oncol Nurs. 2011;15:59–66. doi: 10.1016/j.ejon.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 87.Varpe P, Huhtinen H, Rantala A, et al. Quality of life after surgery for rectal cancer with special reference to pelvic floor dysfunction. Colorectal Dis. 2011;13:399–405. doi: 10.1111/j.1463-1318.2009.02165.x. [DOI] [PubMed] [Google Scholar]
- 88.Yau T, Watkins D, Cunningham D, et al. Longitudinal assessment of quality of life in rectal cancer patients with or without stomas following primary resection. Dis Colon Rectum. 2009;52:669–77. doi: 10.1007/DCR.0b013e31819eb970. [DOI] [PubMed] [Google Scholar]
- 89.Pucciarelli S, Del Bianco P, Toppan P, et al. Health-related quality of life outcomes in disease-free survivors of mid-low rectal cancer after curative surgery. Ann Surg Oncol. 2008;15:1846–54. doi: 10.1245/s10434-008-9923-0. [DOI] [PubMed] [Google Scholar]
- 90.Schmidt CE, Bestmann B, Küchler T, et al. Prospective evaluation of quality of life of patients receiving either abdominoperineal resection or sphincter-preserving procedure for rectal cancer. Ann Surg Oncol. 2005;12:117–23. doi: 10.1245/ASO.2005.12.036. [DOI] [PubMed] [Google Scholar]
- 91.van den Brink M, van den Hout WB, Kievit J, et al. The impact of diagnosis and treatment of rectal cancer on paid and unpaid labor. Dis Colon Rectum. 2005;48:1875–82. doi: 10.1007/s10350-005-0120-y. [DOI] [PubMed] [Google Scholar]
- 92.Hawkins AT, Berger DL, Shellito PC, et al. Wound dehiscence after abdominoperineal resection for low rectal cancer is associated with decreased survival. Dis Colon Rectum. 2014;57:143–50. doi: 10.1097/DCR.0000000000000027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bakker IS, Snijders HS, Wouters MW, et al. High complication rate after low anterior resection for mid and high rectal cancer; results of a population-based study. Eur J Surg Oncol. 2014;40:692–8. doi: 10.1016/j.ejso.2014.02.234. [DOI] [PubMed] [Google Scholar]
- 94.Snijders HS, Bakker IS, Dekker JW, et al. High 1-year complication rate after anterior resection for rectal cancer. J Gastrointest Surg. 2014;18:831–8. doi: 10.1007/s11605-013-2381-4. [DOI] [PubMed] [Google Scholar]
- 95.Liu L, Herrinton LJ, Hornbrook MC, et al. Early and late complications among long-term colorectal cancer survivors with ostomy or anastomosis. Dis Colon Rectum. 2010;53(2):200–12. doi: 10.1007/DCR.0b013e3181bdc408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tan WS, Tang CL, Shi L, Eu KW. Meta-analysis of defunctioning stomas in low anterior resection for rectal cancer. Br J Surg. 2009;96:462–72. doi: 10.1002/bjs.6594. [DOI] [PubMed] [Google Scholar]
- 97.Chen J, Wang DR, Yu HF, et al. Defunctioning stoma in low anterior resection for rectal cancer: a meta- analysis of five recent studies. Hepatogastroenterology. 2012;59:1828–31. doi: 10.5754/hge11786. [DOI] [PubMed] [Google Scholar]
- 98.Matthiessen P, Hallböök O, Rutegård J, et al. Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer: a randomized multicenter trial. Ann Surg. 2007;246:207–14. doi: 10.1097/SLA.0b013e3180603024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Manderson L. Boundary breaches: the body, sex and sexuality after stoma surgery. Soc Sci Med. 2005;61(2):405–15. doi: 10.1016/j.socscimed.2004.11.051. [DOI] [PubMed] [Google Scholar]
- 100.Symms MR, Rawl SM, Grant M, et al. Sexual health and quality of life among male veterans with intestinal ostomies. Clin Nurse Spec. 2008;22(1):30–40. doi: 10.1097/01.NUR.0000304181.36568.a7. [DOI] [PubMed] [Google Scholar]
- 101.Ramirez M, McMullen C, Grant M, et al. Figuring out sex in a reconfigured body: experiences of female colorectal cancer survivors with ostomies. Women Health. 2009;49(8):608–24. doi: 10.1080/03630240903496093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ho VP, Lee Y, Stein SL, Temple LK. Sexual function after treatment for rectal cancer: a review. Dis Colon Rectum. 2011;54:113–25. doi: 10.1007/DCR.0b013e3181fb7b82. [DOI] [PubMed] [Google Scholar]
- 103.Lange MM, Marijnen CA, Maas CP, et al. Risk factors for sexual dysfunction after rectal cancer treatment. Eur J Cancer. 2009;45(9):1578–88. doi: 10.1016/j.ejca.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 104.Silberfein EJ, Kattepogu KM, Hu CY, Skibber JM, et al. Long-term survival and recurrence outcomes following surgery for distal rectal cancer. Ann Surg Oncol. 2010;17:2863–9. doi: 10.1245/s10434-010-1119-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Mulsow J, Winter DC. Sphincter preservation for distal rectal cancer–a goal worth achieving at all costs? World J Gastroenterol. 2011;17:855–61. doi: 10.3748/wjg.v17.i7.855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Boushey Wu R, Potter R, Stacey BD. The evaluation of a rectal cancer decision aid and the factors influencing its implementation in clinical practice. BMC Surg. 2014;14:16. doi: 10.1186/1471-2482-14-16. Available from URL: http://www.biomedcentral.com/1471-2482/14/16/additional. [accessed September 9, 2015] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Grant M, McMullen CK, Altschuler A, et al. Irrigation practices in long-term survivors of colorectal cancer with colostomies. Clin J Oncol Nurs. 2012;16(5):514–9. doi: 10.1188/12.CJON.514-519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Coons SJ, Chongpison Y, Wendel CS, et al. Overall quality of life and difficulty paying for ostomy supplies in the Veterans Affairs ostomy health-related quality of life study: an exploratory analysis. Med Care. 2007;45(9):891–5. doi: 10.1097/MLR.0b013e318074ce9b. [DOI] [PubMed] [Google Scholar]
- 109.Lundy JJ, Coons SJ, Wendel C, et al. Exploring household income as a predictor of psychological well-being among long-term colorectal cancer survivors. Qual Life Res. 2009;18(2):157–61. doi: 10.1007/s11136-008-9432-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Jorge JM, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum. 1993;36:77–97. doi: 10.1007/BF02050307. [DOI] [PubMed] [Google Scholar]
- 111.Chaudhri S, Brown L, Hassan I, et al. Preoperative intensive, community-based vs. traditional stoma education: A randomized, controlled trial. Dis Colon Rectum. 2005;48:504–9. doi: 10.1007/s10350-004-0897-0. [DOI] [PubMed] [Google Scholar]
- 112.Colwell JC, Gray M. Does preoperative teaching and stoma site marking affect surgical outcomes in patients undergoing ostomy surgery? J Wound Ostomy Continence Nurs. 2007;34(5):492–496. doi: 10.1097/01.WON.0000290726.08323.a6. [DOI] [PubMed] [Google Scholar]
- 113.Ramage L, Qiu S, Kontovounisios C, et al. A systematic review of sacral nerve stimulation for low anterior resection syndrome. Colorectal Dis. 2015;17:762–71. doi: 10.1111/codi.12968. [DOI] [PubMed] [Google Scholar]
- 114.Visser WS, Te Riele WW, Boerma D, et al. Pelvic floor rehabilitation to improve functional outcome after a low anterior resection: a systematic review. Ann Coloproctol. 2014;30:109–14. doi: 10.3393/ac.2014.30.3.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kuo LJ, Lin YC, Lai CH, et al. Improvement of fecal incontinence and quality of life by electrical stimulation and biofeedback for patients with low rectal cancer after intersphincteric resection. Arch Phys Med Rehabil. 2015;96:1442–7. doi: 10.1016/j.apmr.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 116.Laforest A, Bretagnol F, Mouazan AS, et al. Functional disorders after rectal cancer resection: does a rehabilitation programme improve anal continence and quality of life? Colorectal Dis. 2012;14:1231–7. doi: 10.1111/j.1463-1318.2012.02956.x. [DOI] [PubMed] [Google Scholar]
- 117.Schwandner O. Sacral neuromodulation for fecal incontinence and “low anterior resection syndrome” following neoadjuvant therapy for rectal cancer. Int J Colorectal Dis. 2013;28:665–9. doi: 10.1007/s00384-013-1687-8. [DOI] [PubMed] [Google Scholar]
- 118.Chen TY, Emmertsen KJ, Laurberg S. Bowel dysfunction after rectal cancer treatment: a study comparing the specialist’s versus patient’s perspective. BMJ Open. 2014;4:e003374. doi: 10.1136/bmjopen-2013-003374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Burg MA, Adorno G, Lopen EDS, et al. Current unmet needs of cancer survivors: analysis of open-ended responses to the American Cancer Society Study of Cancer Survivors II. Cancer. 2015;121:623–30. doi: 10.1002/cncr.28951. [DOI] [PubMed] [Google Scholar]


