Sir,
A 43-year-old male patient presented with generalized pruritic, erythematous to violaceous plaques and hypopigmented scaly ill-defined patches. The patient was treated for psoriasis for the past 20 years, by various doctors in tertiary centers, with topical steroid, methotrexate, cyclosporine, and phototherapy without much control. His condition remained overall uncontrolled and progressive. He was started on subcutaneous injections of etanercept (Enbrel™) 5 years back, and was discontinued after 3 months, as there was no improvement in Psoriasis Area and Severity Index score.
The patient's condition further worsened, and he developed multiple new plaques in the past 6 months. He sought treatment from another hospital in Southern India and was prescribed secukinumab (Injection Scapho™) loading dose (five injections at weekly interval). After the fifth injection of secukinumab, the patient showed no improvement.
After this development, he came to our hospital for the second opinion of whether he should be continuing the injection.
On examination, we noticed that he had many erythematous to violaceous plaques and nodular lesions in face, trunk, and extremities, some of which showed signs of crusting in the center [Figure 1]. He also had scaly ill-defined patches spread over the trunk and extremities; on careful history taking, it was revealed that these scaly patches were there for more than 25 years, and his plaque developed much later.
Figure 1.

Psoriasiform plaques in the trunk and extremities
We asked the patient to stop secukinumab injections for the time being and asked for the routine blood counts and serology, which was within normal limit. We did a 4 mm skin punch biopsy from the plaque, and on hematoxylin and eosin staining, the histopathology revealed epidermotropism with atypical lymphocytes in clusters throughout the epidermis [Figure 2a and b]. Immunohistochemistry revealed clonal proliferation of CD2, CD3, and CD5 positive and CD20 and CD7 negative lymphocytes in epidermis and superficial dermis [Figure 3a–e]. Fludeoxyglucose whole-body positron emission tomography/computed tomography scans revealed bilateral involvement of axillary, external iliac, and inguinal lymph node. Peripheral blood smear, however, failed to detect any atypical T-lymphocyte. We diagnosed the case as cutaneous T-cell lymphoma (CTCL), and currently, the patient is undergoing chemotherapy in a tertiary cancer hospital.
Figure 2.
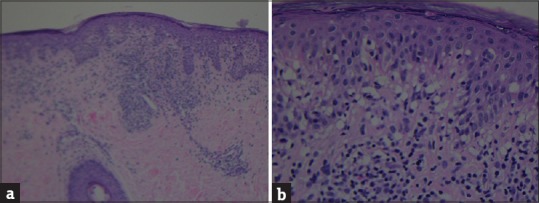
Histopathology with hematoxylin and eosin stain (a) Photomicrograph ×10 showing epidermotropism with atypical lymphocytes in clusters throughout the epidermis. (b) Photomicrograph ×40 showing epidermotropism with atypical lymphocytes in clusters throughout the epidermis
Figure 3.
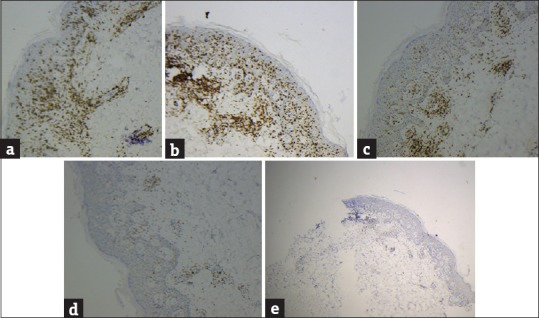
(a) Immunocytochemistry shows CD2-positive cells in the epidermis and dermis. (b) Immunocytochemistry shows CD3-positive cells in the epidermis and dermis. (c) Immunocytochemistry shows CD5-positive cells in the epidermis and dermis. (d) Immunocytochemistry shows CD7-negative cells. (e) Immunocytochemistry shows CD20-negative cells
We report this case to draw attention to this unusual situation when more than one biologics were used in a patient with a provisional diagnosis of psoriasis. CTCL can be a great mimicker of many diseases including psoriasis. Many dermatologists treated the patient with multiple immunosuppressives and immunomodulators, and a battery of tests was conducted. However, somehow, no one considered doing a biopsy even after repeated failure of systemic therapies including biologics.
CTCL can mimic psoriasis in different stages as it may produce psoriasiform plaques[1] or acquired palmoplantar keratoderma[2] and erythroderma.[3] Moreover, even histopathologically, early CTCL may be difficult to be differentiated from psoriasiform dermatitis.[4]
CTCL has been described in patients of psoriasis;[5] especially, there can be a sudden onset of cutaneous lymphoma, after initiation of immunosuppressives.[6] Systemic hepatosplenic T-cell lymphoma was also reported with immunomodulators and biologics in a patient with Crohn's disease.[7] It is reported in literature that there is a definite risk of developing lymphoma in the patients of psoriasis.[8] There was a suggestion of genetic linkage in the pathogenesis of psoriasis and CTCL.[9]
Hence, we conclude that CTCL can not only be masquerading as psoriasis both clinically and histopathologically but also there can be some causal linkage. CTCL was reported in patients of psoriasis who were treated with biologicals such as etanercept[10] and efalizumab.[11] Keeping in mind the above discussion and the context of our patient, we strongly suggest that a biopsy for histopathology should be considered in cases of recalcitrant psoriasis, especially before starting biological therapy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Jinno N, Yamana Y, Kawashima M, Tsunemi Y. Mycosis fungoides with psoriasiform lesions. J Dermatol. 2015;42:227–9. doi: 10.1111/1346-8138.12749. [DOI] [PubMed] [Google Scholar]
- 2.Kim J, Foster R, Lam M, Kumarasinghe SP. Mycosis fungoides: An important differential diagnosis for acquired palmoplantar keratoderma. Australas J Dermatol. 2015;56:49–51. doi: 10.1111/ajd.12155. [DOI] [PubMed] [Google Scholar]
- 3.Dubrey SW, Rosser G, Patel K, Whittaker SJ. Erythroderma is not all psoriasis: A case of Sézary syndrome. Br J Hosp Med (Lond) 2014;75:50–1. doi: 10.12968/hmed.2014.75.1.50. [DOI] [PubMed] [Google Scholar]
- 4.Reddy K, Bhawan J. Histologic mimickers of mycosis fungoides: A review. J Cutan Pathol. 2007;34:519–25. doi: 10.1111/j.1600-0560.2006.00662.x. [DOI] [PubMed] [Google Scholar]
- 5.Punchak M, Farahmand A, Turegano MM, Lazarus ME. Cutaneous T-cell lymphoma in a patient with psoriasis. Am J Med Sci. 2017;353:193. doi: 10.1016/j.amjms.2016.05.028. [DOI] [PubMed] [Google Scholar]
- 6.Quéreux G, Renaut JJ, Peuvrel L, Knol AC, Brocard A, Dréno B. Sudden onset of an aggressive cutaneous lymphoma in a young patient with psoriasis: Role of immunosuppressants. Acta Derm Venereol. 2010;90:616–20. doi: 10.2340/00015555-0978. [DOI] [PubMed] [Google Scholar]
- 7.Thayu M, Markowitz JE, Mamula P, Russo PA, Muinos WI, Baldassano RN. Hepatosplenic T-cell lymphoma in an adolescent patient after immunomodulator and biologic therapy for Crohn disease. J Pediatr Gastroenterol Nutr. 2005;40:220–2. doi: 10.1097/00005176-200502000-00026. [DOI] [PubMed] [Google Scholar]
- 8.Gelfand JM, Shin DB, Neimann AL, Wang X, Margolis DJ, Troxel AB. The risk of lymphoma in patients with psoriasis. J Invest Dermatol. 2006;126:2194–201. doi: 10.1038/sj.jid.5700410. [DOI] [PubMed] [Google Scholar]
- 9.Elder JT. What can psoriasis teach us about the genetic basis of cutaneous T-cell lymphoma? Clin Lymphoma Myeloma Leuk. 2010;10(Suppl 2):S70–3. doi: 10.3816/CLML.2010.s.011. [DOI] [PubMed] [Google Scholar]
- 10.Lafaille P, Bouffard D, Provost N. Exacerbation of undiagnosed mycosis fungoides during treatment with etanercept. Arch Dermatol. 2009;145:94–5. doi: 10.1001/archdermatol.2008.526. [DOI] [PubMed] [Google Scholar]
- 11.Hernandez C, Worobec SM, Gaitonde SS, Kiripolsky ML, Aquino K. Progression of undiagnosed cutaneous T-cell lymphoma during efalizumab therapy. Arch Dermatol. 2009;145:92–4. doi: 10.1001/archdermatol.2008.530. [DOI] [PubMed] [Google Scholar]


