Abstract
Aggressive behaviour is the most disturbing and distressing behaviour displayed by elderly people. The prevalence of aggressive behaviour is around 50% among psychogeriatric patients.
OBJECTIVE
This study sought to analyze the psychometric properties and diagnostic accuracy of the French version of the Rating Scale for Aggressive Behaviour in the Elderly (F-RAGE).
METHODS
The F-RAGE was administered to 79 patients hospitalized in a geriatric psychiatry department. A psychiatrist, who was blind to the subjects' RAGE scores, performed the diagnosis for aggressivity based on global clinical impression. The F-RAGE and MMSE were applied by a trained researcher blind to subjects' clinical diagnoses while the Cohen-Mansfield Agitation Inventory and Neuropsychiatric Inventory were administered by medical and nursing staff. Internal consistency, reliability, cut-off points, sensitivity and specificity for F-RAGE were estimated.
RESULTS
F-RAGE showed satisfactory validity and reliability measurements. Regarding reliability, Cronbach's α coefficient was satisfactory with a value of 0.758. For diagnostic accuracy, a cut-off point of 8 points (sensitivity=74.19%; specificity=97.98%) and area under curve of 0.960 were estimated to distinguish between aggressive patients and control subjects.
DISCUSSION
F-RAGE showed acceptable psychometric properties, supported by evidence of validity and reliability for its use in the diagnosis of aggressive behaviour in elderly.
Keywords: aggressive behaviour, psychogeriatric, RAGE, CMAI, NPI
Abstract
O comportamento agressivo é o comportamento mais perturbador e angustiante que possa ser apresentado pelos idosos. A prevalência de comportamento agressivo é cerca de 50% entre os pacientes psicogeriátricos.
OBJETIVO
Analisar as propriedades psicométricas e acurácia diagnóstica da versão francesa da Escala de Avaliação do Comportamento Agressivo em Idosos (F-RAGE).
MÉTODOS
A F-RAGE foi administrada a 79 pacientes internados no departamento de psiquiatria geriátrica. Um psiquiatra que era cego às pontuações F-RAGE dos sujeitos realizou o diagnóstico de DSM-IV com base na impressão clínica global. O F-RAGE e MMSE foram realizados por um pesquisador treinado cego ao diagnóstico clínico dos sujeitos e o Inventário de agitação de Cohen-Mansfield e o Inventário Neuropsiquiátrico pela equipe médica e de enfermagem. Consistência interna, pontos de corte, sensibilidade e especificidade para F-RAGE foram estimados.
RESULTADOS
F-RAGE mostrou validade satisfatória e medidas de confiabilidade. Em relação à confiabilidade, coeficiente α de Cronbach foi satisfatória com um valor de 0,758. Para maior precisão de diagnóstico, um ponto de corte de 8 pontos (sensibilidade=74,2%, especificidade=98,0%) e área sob a curva de 0,960 foram estimados para distinguir entre os pacientes agressivos e controles.
DISCUSSÃO
F-RAGE mostrou propriedades psicométricas aceitáveis, apoiados por evidências de validade e confiabilidade para sua utilização no diagnóstico do comportamento agressivo em idosos.
INTRODUCTION
Aggressive behaviour (AB) is the most disturbing and distressing behaviour displayed by older patients in long-term care facilities or in psychogeriatric units. Patel and Hope1 defined AB as an overt act, involving the delivery of noxious stimuli to (but not necessarily aimed at) another object, organism or self, which is clearly not accidental. It affects older patients themselves and their informal and formal caregivers. It can also lead to increased health care costs. Family members and friends are affected by aggressive behaviours in long-term care facilities. They can be embarrassed by these disruptive behaviours and can reduce the frequency of their visits.2 Some individual and environmental factors are implicated in the triggering of AB. Dementia is the leading cause of disruptive behaviours and Alzheimer's disease accounts for 60%-80% of such cases in the elderly.3 Male gender and being in the younger strata of the older adult population are individual factors associated with AB. Psychiatric diseases such as depression, schizophrenia, anxiety, hallucination and delusion have also been linked to AB.2,5
The prevalence of AB varies widely from 7% to 91% in long-term care facilities4 and it is estimated to average 50% in psychogeriatric facilities.5,6 Patel and Hope found nearly half the sample was at least mildly aggressive over a 3-day period. Rabinset al.7 reported a prevalence of 47% in a psychogeriatric ward. In an institution, Zimmeret al.8 found that 22.6% of residents had serious behavioral problems. Two-thirds of these patients were diagnosed as suffering from dementia. Prevalence of AB is more significant among community-based patients with dementia. Between 20% and 50% of families of patients with Alzheimer's disease reported AB. Ryden9 reported a prevalence of verbal aggression of 49%, physical aggression of 46% and sexual aggression of 17%.
Several tools are used for the assessment of behavioural symptoms, but most of these scales are not specific for one behavioural disorder such as aggression. In addition, they were initially developed for the assessment of behavioural problems in dementia whereas they are not adapted for the measure of these disorders in patients with other psychiatric problems. The Rating Scale for Aggressive Behaviour in the Elderly (RAGE) is a rating scale specifically developed for the assessment of aggressive behaviour in institutionalized or hospitalized elderly1. This scale takes into account different dimensions of aggression: verbal and physical aggressions. It has the advantage of being used for different diseases found in psychogeriatric departments, not just for dementia. This study sought to analyze the psychometric properties and diagnostic accuracy of the French version of the Rating Scale for Aggressive Behaviour in the Elderly (F-RAGE) among patients hospitalized in psychogeriatric departments, and compares the diagnostic performances of the F-RAGE to that of the Cohen-Mansfield Agitation Inventory (CMAI).10,11
MATERIALS AND METHODS
Subjects. The study was carried out at the Hospital Center Esquirol in 2013 and included participants of both sexes, aged 65 or older, who were hospitalized for at least seven days. Of the 170 patients hospitalized during the inclusion period, only 79 (46.5% of the total population) were enrolled. Patients with acute somatic illness or who presented incapacity to communicate were not included in this study. Patients who were included gave their informed consent (or proxy consent for patients with severe cognitive impairment (MMSE<15)) and underwent a standardized assessment that included taking of a detailed socio-demographic history, and assessments of neuropsychiatric symptoms, aggressive behaviour and cognition. The protocol was approved by the regional board of medical research ethics.
Assessment. Aggressive behaviour – The gold standard was the diagnosis based on the expertise and global clinical impression of the psychiatrist's blind assessment of other aggressive behaviour scales such as the F-RAGE, the CMAI or the NPI. Based on this expertise, the psychiatrist overseeing the patient stated whether the patient had exhibited verbal or physical aggressive behaviour.
Two instruments were chosen for assessment of aggressive behaviours:
– The French version of the Rating Scale for Aggressive Behaviour (F-RAGE)1, for measuring aggressive behaviour in psychogeriatric inpatients. It is designed to be completed by the staff, who are asked to specify the types of aggressive behavior observed in patients under their care for 3 days. The original version of the RAGE was a 21-item scale. Seventeen items concerned specific kinds of aggressive behaviour. Three items enquired about the consequences of the aggressive behaviour, and the final item asked the rater to provide an overall assessment of aggressive behaviour. Each item was rated on a four-point scale based on frequency ranging from 0 (never) to 3 (always). The RAGE was translated into French and back-translated into English with satisfactory pilot testing. The required time for completing the F-RAGE was only about five minutes.
– The French version of the Cohen-Mansfield Agitation Inventory (CMAI)12, for comparing the diagnostic performance of the CMAI with the F-RAGE. It is widely used in psychogeriatric units; it measures 29 disruptive behaviors in four dimensions: physical aggression, nonphysical aggression, aggressive verbal and non-verbal aggressive behaviour. In this study, we focused only on two dimensions: physical aggression and aggressive verbal behaviour.
Cognitive status – Overall cognitive function was assessed using the Mini-Mental State Examination (MMSE),13 a brief 30-point questionnaire test used to screen for cognitive impairment.
Neuropsychiatric symptoms – The Neuropsychiatric Inventory (NPI)14 is a useful tool for rating the major neuropsychiatric symptoms observed in dementia such as delusion, hallucinations, anxiety, depression, aggressive behaviour/agitation, sleep disorders, eating disorders, apathy, disinhibition, euphoria, aberrant motor activity and irritability.
Procedures. This study was conducted in three steps. The first step was the inclusion visit with the psychiatrist who, blind to the subjects' different scores, performed the diagnosis of aggressive behaviour. The last two steps correspond to administration of different rating scales. These last steps were carried out independently and blinded. The order of administration of different rating scale was not pre-defined. Only the assessment of cognitive function was systematically carried out at the inclusion visit. The F-RAGE and MMSE were performed by a trained researcher from the staff team, whereas the NPI was applied by physicians. The CMAI was administered by nursing staff.
Statistical analysis. Socio-demographic characteristics of participants were described by frequencies and percentages for qualitative variables and by means and standard deviation for continuous variables. To compare the two groups (aggressive patients and non-aggressive behaviours) on continuous data (age and MMSE, CMAI, F-RAGE, NPI scores), Student's t test was used, whereas qualitative variables (sex, marital status) were compared using the Chi-square test. Cronbach's α and split-half correlation coefficients were calculated for internal consistency analysis. For the validity analysis, the mean F-RAGE scores of aggressive and non-aggressive groups were compared using Student's t test. The diagnostic performance was assessed by reference to two standard criteria: sensitivity, specificity. This graphic representation allows definition of these performances and choice of optimal cut-off. To compare diagnostic performances between the Cohen-Mansfield Agitation Inventory (CMAI) and the French version of the Rating Scale for Aggressive Behaviour in the Elderly (F-RAGE), areas under curves were compared using the Hanley and McNeil's method. Items were factor analyzed using principal component extraction and orthogonally rotated using Varimax rotation. Following this significant analysis, the items which did not correlate with at least one other variable at a value greater than 0.5, were dropped from the analysis. Factors with eigenvalues >1 were extracted. To compare the diagnostic performances between the two tests, we applied the Hanley and McNeil's method. All analyses were performed using SPSS for Windows 20.0 and ROC analysis conducted with MedCalc® 12.7.0. Level of significance was 0.05 for all analyses.
RESULTS
Sample characteristics. The sample comprised 79 patients with a mean age of 83.3±6.8(66-94) years. The average MMSE score was 17.9±7.1(2-30) (Table 1) and 36 subjects had been diagnosed as suffering from dementia according to DSM-IV-TR. Thirty-one patients were aggressive according to the psychiatrist global clinical impression. The sex ratio (male/female) was 0.58 (29 men and 50 women). All patients could read and write. Fifty patients lived alone or in nursing homes. Among the reasons for hospitalization, 35 were for affective symptoms, 31 were for behaviour disturbances (apathy, agitation, disinhibition), 9 were for psychotic disturbances and 4 were for other reasons (cognitive impairment, bipolar disorders). The score for the Cohen-Mansfield Agitation Inventory (CMAI) total population was 46.2±22.2 (28-148), for the French version of the Rating Scale for Aggressive Behaviour in the Elderly (F-RAGE) score was 9.3±13.1(0-9) and for the Neuropsychiatric Inventory (NPI) the score was 16.4±11.6(0-49) (Table 1).
Table 1.
Socio-demographic characteristics of aggressive and non-aggressive subjects.
| Study populationN=79 | Aggressive subjectsn=31 | Non-aggressive subjectsn=48 | Significancep | |
|---|---|---|---|---|
| Mean age | 82.7±8.7 | 80.2±11.2 | 84.4±6.2 | 0.1 |
| Sex (% female) | 50 (63.3) | 14 (45.2) | 36 (75.0) | 0.01 |
| Marital status (% living alone) | 50 (63.3) | 15 (48.4) | 35 (72.9) | 0.028 |
| MMSE mean±SD | 17.9±7.1 | 15.13±7.8 | 19.7±5.9 | 0.009 |
| CMAI mean±SD | 46.2±22.1 | 63.3±25.8 | 35.2±8.5 | <0.001 |
| F-RAGE mean±SD | 9.3±13.1 | 21.7±12.9 | 1.2±3.1 | <0.001 |
| NPI mean±SD | 16.4±11.6 | 22.1±10.9 | 12.8±10.7 | <0.001 |
MMSE: Mini-Mental State Examination; CMAI: Cohen-Mansfield Agitation Inventory, F RAGE: French version of Rating Scale for Aggressive Behaviour in the Elderly, NPI: Neuropsychiatric Inventory, SD: Standard Deviation.
Comparison of aggressive and non-aggressive patients. The population was divided into two groups on the basis of the psychiatrist's global clinical impression. The proportion of females (p=0.010) and of patients living alone (p=0.028) was significantly higher in the group of non-aggressive patients. According to the NPI, affective symptoms were more frequent in non-aggressive group (p=0.001) while behaviour disorders were more frequent in the aggressive group (p=0.010). There was no significant difference in the proportion of dementia between the two groups. MMSE score was significantly higher in the non-aggressive group (p=0.009). There were significant differences in scores for the following NPI dimensions: irritability, aggressive behaviour, anxiety, disinhibition, and aberrant motor activity (Table 2).
Table 2.
Clinical characteristics of aggressive and non-aggressive subjects.
| Mean score±SD | Study populationn=79 | Aggressive subjectsn=31 | Non-aggressive subjectsn=48 | Significancep | |
|---|---|---|---|---|---|
| Neuropsychiatric Inventory | Hallucinations | 1.0±2.4 | 1.9±3.4 | 0.4±1.1 | 0.09 |
| Delusions | 1.7±3.2 | 1.8±3.6 | 1.6±3.0 | 0.7 | |
| Aggression/agitation | 2.7±4.0 | 6.7±3.9 | 0.2±0.7 | <0.001 | |
| Depression/dysphoria | 2.9±3.8 | 2.3±3.8 | 3.3±3.9 | 0.19 | |
| Anxiety | 1.7±2.6 | 0.7±1.4 | 2.4±3.0 | 0.004 | |
| Euphoria | 0.3±1.5 | 0.1±0.4 | 0.4±1.9 | 0.53 | |
| Apathy | 1.2±3.0 | 1.4±3.6 | 1.1±2.6 | 0.7 | |
| Disinhibition | 0.7±2.2 | 1.5±3.3 | 0.2±0.6 | 0.01 | |
| Irritability | 0.9±2.1 | 2.2±3.0 | 0.1±0.5 | 0.03 | |
| Aberrant motor activity | 1.0±2.6 | 1.8±3.6 | 0.5±1.6 | <0.001 | |
| Sleep disorders | 1.3±2.5 | 0.9±1.7 | 1.5±2.9 | 0.44 | |
| Eating disorders | 1.2±2.6 | 1.0±2.1 | 1.3±2.9 | 0.71 | |
| Total score | 16.4±11.6 | 22.1±10.9 | 12.8±10.7 | <0.001 | |
| CMAI | Non-aggressive physical behaviour | 21.8±11.8 | 29.9±14.6 | 16.9±5.6 | <0.001 |
| Non-aggressive verbal behaviour | 6.9±4.1 | 8.5±4.6 | 5.9±3.3 | 0.003 | |
| Aggressive physical behaviour | 12.2±7.9 | 17.1±11.0 | 9.1±0.9 | <0.001 | |
| Aggressive verbal behaviour | 5.4±3.8 | 8.4±3.9 | 3.5±2.0 | <0.001 | |
| Total Score of aggression | 17.7±10.7 | 25.5±13.7 | 12.6±2.3 | <0.001 | |
| Total Score | 46.2±22.1 | 63.3±25.8 | 35.2±8.5 | <0.001 | |
| F-RAGE | Total Score | 9.3±3.1 | 21.7±12.9 | 1.2±3.1 | <0.001 |
CMAI: Cohen-Mansfield Agitation Inventory, F-RAGE: French version of the Rating Scale for Aggressive Behaviour in the Elderly; SD: Standard deviation.
Selection of items. In order to optimize the Cronbach's α reliability index, we decided to eliminate items 12 and 21 in agreement with psychiatrists. Question 12 of the F-RAGE was also dropped because of its redundancy with the question 17. Question 21 was deleted because it summarizes the global measure of aggressive behaviour. Logically the total rating score should determine the presence of aggressive behaviour and the magnitude of this behaviour disorder. The principal component analysis was applied in order to delete those items which did not have a correlation coefficient greater than 0.5. Subsequently, item 1 was deleted for this reason. Finally, we kept a construct of 18 items. Its total score was 52 whereas the original version of the RAGE was 61.
Factor structure. Five factors with eigenvalue >1 were extracted and these accounted for 75.1% of the variance. Factor I accounted for 31.4% and reflected mainly physical aggression, factor II accounted for 16.4% and corresponded to verbal aggression, factor III accounted for 11.1%, reflecting self-destruction, factor IV accounted for 8.5% and reflected the possible consequence of aggressive behaviour. Factor V accounted for 7.7% and related to antisocial acts (Table 3).
Table 3.
Factor analysis of items of the RAGE after Varimax rotation.
| Items | FactorI | Factor II | Factor III | Factor IV | Factor V |
|---|---|---|---|---|---|
| Item 15 | 0.947 | ||||
| Item 14 | 0.919 | ||||
| Item 11 | 0.895 | ||||
| Item 16 | 0.768 | ||||
| Item 5 | 0.561 | ||||
| Item 7 | 0.837 | ||||
| Item 9 | 0.727 | ||||
| Item 3 | 0.720 | ||||
| Item 8 | 0.681 | ||||
| Item 6 | 0.613 | ||||
| Item 10 | 0.889 | ||||
| Item 13 | 0.850 | ||||
| Item 18 | 0.784 | ||||
| Item 19 | 0.715 | ||||
| Item 17 | 0.708 | ||||
| Item 20 | 0.678 | ||||
| Item 2 | 0.553 | ||||
| Item 4 | 0.865 | ||||
| Item 1 | 0.457 | ||||
| Eigenvalue | 5.974 | 3.108 | 2.106 | 1.616 | 1.462 |
| Percentage of variance | 31.4 | 16.4 | 11.1 | 8.5 | 7.7 |
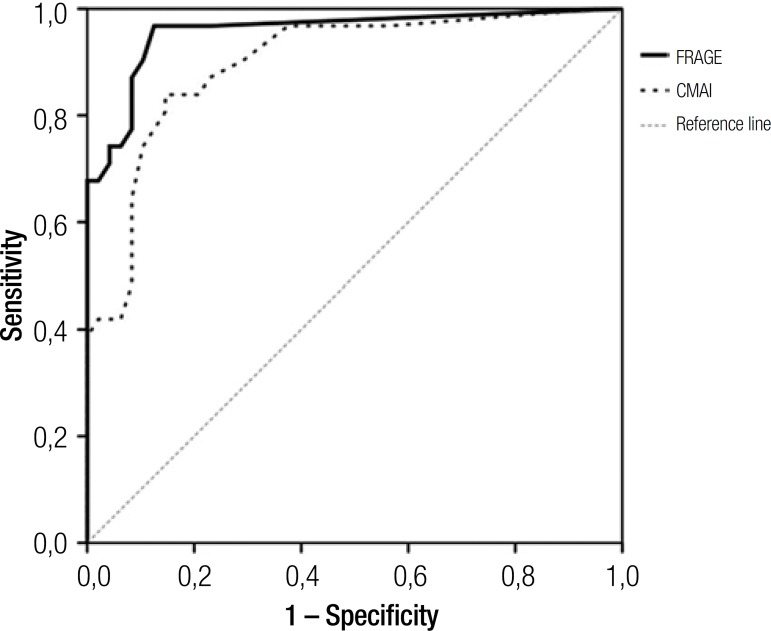
Determination of RAGE diagnostic performance. Cronbach's α was 0.76 and the split-half correlation coefficient was 0.74. Validity analysis showed that the aggressive group had a significantly higher mean F-RAGE total score than the group without aggression (21.7±2.3v 1.2±0.5, P<0.001). The highest sum of sensitivity and specificity values, 172.1, was obtained for the cut-off score of 8/9. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for cut-off scores between 1 and 40 are shown in Table 4. The ROC curve also showed that the 8/9 provided the best results, since they were very close to each other, with 8/9 being closest to the upper left of the graph. The area under the curve (AUC) value was 0.96±0.03(95% CI 0.89 to 0.99; P<0.001). A sensitivity value of 74.2 95% CI (55.4-88.1) and a specificity of 97.9 95% CI (88.5-99.9) were determined. In this population, the prevalence of aggressive behaviour was 39.2%. We found a positive predictive value of 95.8% 95% CI (78.3-99.9) and a negative predictive value of 85.6 95% CI (73.5-93.6) .The final test of the French version of the Rating Scale for Aggressive Behaviour in the Elderly (RAGE) is illustrated by the receiver operating characteristic curve depicted in Figure 1.
Table 4.
Discrimination between aggressive (n=31) and non-aggressive (n=48) groups.
| Cut-off | Sensitivity | 95% CI | Specificity | 95% CI | PPV | 95% CI | NPV | 95% CI |
|---|---|---|---|---|---|---|---|---|
| 0 | 100.0 | 88.8-100.0 | 0.0 | 0.0-7.4 | 39.0 | 28.2-50.6 | ||
| 0/1 | 96.8 | 83.3-99.9 | 75.1 | 62.7-88.0 | 73.0 | 56.6-85.8 | 97.4 | 86.2-99.9 |
| 1/3 | 93.6 | 78.6-99.2 | 89.6 | 77.3-96.5 | 85.2 | 68.5-95.1 | 95.6 | 84.9-99.5 |
| 3/4 | 90.3 | 74.2-98.0 | 89.6 | 77.3-96.5 | 84.7 | 67.6-94.9 | 93.5 | 82.2-98.7 |
| 4/5 | 77.4 | 58.9-90.4 | 91.7 | 80.0-97.7 | 85.6 | 66.8-96.0 | 86.4 | 73.9-94.4 |
| 5/6 | 74.2 | 55.4-88.1 | 91.7 | 80.0-97.7 | 85.1 | 65.7-95.9 | 84.7 | 72.1-93.2 |
| 6/7 | 74.2 | 55.4-88.1 | 93.8 | 82.8-98.7 | 88.4 | 69.2-97.6 | 85.0 | 72.6-93.3 |
| 7/8 | 74.2 | 55.4-88.1 | 95.8 | 85.7-99.5 | 91.9 | 73.4-99.1 | 85.3 | 73.0-93.5 |
| 8/9 | 74.2 | 55.4- 88.1 | 97.9 | 88.9- 99.9 | 95.8 | 78.3- 99.9 | 85.6 | 73.5- 93.6 |
| 9/10 | 71.0 | 52.0-85.8 | 97.9 | 88.9-99.9 | 95.6 | 77.4-99.9 | 84.1 | 71.8-92.5 |
| 10/11 | 71.0 | 52.0-85.8 | 100.0 | 92.6-100.0 | 100 | 83.9-100.0 | 84.3 | 72.3-92.6 |
| 11/12 | 64.5 | 45.4-80.8 | 100.0 | 92.6-100.0 | 100 | 82.4-100.0 | 81.5 | 69.3-90.4 |
| 12/13 | 61.3 | 42.2-78.2 | 100.0 | 92.6-100.0 | 100 | 81.5-100.0 | 80.2 | 67.9-89.3 |
| 13/14 | 54.8 | 36.0-72.7 | 100.0 | 92.6-100.0 | 100 | 79.4-100.0 | 77.6 | 65.2-87.2 |
| 15/17 | 45.2 | 27.3-64.0 | 100.0 | 92.6-100.0 | 100 | 75.3-100.0 | 74.0 | 61.7-84.1 |
| 19/20 | 41.9 | 24.5-60.9 | 100.0 | 92.6-100.0 | 100 | 73.5-100.0 | 72.9 | 60.6-83.1 |
| 10/11 | 38.7 | 21.8-57.8 | 100.0 | 92.6-100.0 | 100 | 71.5-100.0 | 71.8 | 59.5-82.2 |
| 22/25 | 32.3 | 16.7-51.4 | 100.0 | 92.6-100.0 | 100 | 66.4-100.0 | 69.8 | 57.5-80.3 |
| 25/26 | 25.8 | 11.9-44.6 | 100.0 | 92.6-100.0 | 100 | 59.0-100.0 | 67.8 | 55.7-78.4 |
| 13/14 | 22.6 | 9.6-41.1 | 100.0 | 92.6-100.0 | 100 | 54.1-100.0 | 66.9 | 54.8-77.5 |
| 14/15 | 19.4 | 7.5-37.5 | 100.0 | 92.6-100.0 | 100 | 47.8-100.0 | 66 | 54.0-76.7 |
| 30/31 | 16.1 | 5.5-33.7 | 100.0 | 92.6-100.0 | 100 | 39.8-100.0 | 65.1 | 53.1-75.8 |
| 31/38 | 6.5 | 0.8-21.4 | 100.0 | 92.6-100.0 | 100 | 2.5-100.0 | 62.6 | 50.8-73.3 |
| 38/39 | 3.2 | 0.08-16.7 | 100.0 | 92.6-100.0 | 100 | 0.0-100.0 | 61.8 | 50.1-72.6 |
| 39/40 | 0.0 | 0.0-11.2 | 100.0 | 92.6-100.0 | 61 | 49.4-71.8 |
CI: confidence interval. NPV: negative predictive value. PPV: positive predictive value. cut-off calculated on 18 items.
Figure 1.
Receiver operating characteristic (ROC) analysis: comparison of the French version of the Rating Scale for Aggressive Behaviour in the Elderly (F-RAGE) and the Cohen-Mansfield Agitation Inventory (CMAI) with diagnosis of aggression by psychiatrist clinical diagnosis.
Comparison of F-RAGE versus cmAi diagnostic performance. To compare F-RAGE with CMAI performance, areas under curve of two graphic representations were used. The area under curve of CMAI was 0.894±0.040(95% CI 0.81 to 0.95). The difference in areas was 0.058±0.042(CI 95%: –0.024; 0.142) but this difference was not significant (p=0.166). The two tests are illustrated by the Receiver Operating Characteristics presented in Figure 1.
DISCUSSION
Our results suggested that the French version of the RAGE (F-RAGE) is a valid instrument for measuring aggressive behaviour (AB) in French elderly. The F-RAGE is a useful tool for rating these behavioral disorders in psychogeriatric demented and non-demented inpatients and can be easily used by nursing staff in routine procedures. Moreover, completing the questionnaire takes only around ten minutes.
In this sample, aggressive inpatients were more likely to be of male gender and have greater cognitive decline than non-aggressive inpatients. Aggressive inpatients also more often had other behavioral or psychological disorders compared to nonaggressive subjects. All these socio-demographic characteristics and clinical results are consistent with other international studies.15-17 Aggressive behaviour was reported in 39% of inpatients. This prevalence is lower than those reported in the literature.5-B7 Several studies found that nearly half of the samples exhibited aggression. These differences could be due to the variability of tools used, the definition used for aggressive behaviour, and the percentage of demented patients. In fact, dementia is a common etiology of aggressive behaviours in the elderly.18-20 In the present study, 46% of inpatients suffered from dementia. However, this percentage is lower than the rate found for example in nursing homes or long-term care facilities.2,21-23
In our study, we chose the clinical diagnosis established by psychiatrists, in consultation with the health care team of the psychogeriatric ward, as the gold standard. This observational method for the diagnosis of these disorders is frequently used in the international literature.24,25
In the original version of the RAGE, the Cronbach's α was 0.89. We found a satisfactory value (0.758) which exceeded the permitted acceptability threshold in the scientific community.26 During the validation of the Chinese version of the RAGE, Lamet al.6 found a coefficient of 0.74. These results are in accordance with those for F-RAGE. The diagnostic performance of the French version of the RAGE was evaluated by sensitivity (74%), specificity (98%), and positive and negative predictive values (96% and 86%, respectively). For the F-RAGE, we chose a cutoff ≥8 because it demonstrated the combination of the highest sensitivity and specificity for this version. In the original and the Chinese version of the RAGE, there is no mention of any level of specificity or sensitivity based on the overall score or specific score for each dimension of aggression.1,6
We observed no significant difference in diagnostic performance between the F-RAGE and the CMAI. Although this result was not significant, it is clear that the F-RAGE measures more dimensions of aggressive behaviour than the CMAI which primarily evaluates agitation. The F-RAGE is thus more adapted to take account of all dimensions of aggression in elderly. The small size of our sample and the high Pearson r correlation between these two scales (r=0.73)1 might explain why we did not observe a significant difference, but this was not the main objective of this study.
The management of AB in the elderly may require physical and pharmacological approaches such as medications which are associated with several adverse effects.27-31 Moreover, these approaches, when used in a non-rational way, can harm the individual's dignity and leave the patient prone to damaging side effects, and even the risk of abuse.32 Neuroleptics are often used to control physical and verbal aggressions whereas benzodiazepines are more often employed to reduce verbal aggressive behaviour.4,33,34 Physical restraint is used in an attempt to control aggressive or other risky behaviors. This approach can lead to serious adverse effects for patient health, such as loss of autonomy and self-esteem, and worsening of AB or disruptive behaviour.35-39 Another significant finding is that professional carers experience considerable stress, negative feelings and burnout as a result of being the victims of AB in institutions.40-44 Consequently, having a valid instrument for identifying aggression is very important both for the health care team and patients.
According to the principal component analysis, the F-RAGE is composed of five dimensions of AB as the original scale: physical aggressive behaviour, verbal aggressive behaviour, antisocial acts, self-harming and consequences of aggressive behaviour. Self-harming is the main reason for use of physical restraint in institutions or in psychogeriatric wards.36,39 The antisocial dimension is relevant to study because it produces frustration, emotional distress, increasing absenteeism and burn-out of carers and leads to violence against patients by carers. Finally, consequences of aggressive behavior are a dimension which leads to use of drugs in order to reduce these behavioral disorders. Identifying these different dimensions allows more suitable management for each type of aggressive behaviour in institutions or care units. Our study provides the validation of the French version of the RAGE. However, further studies are needed to verify the inter-rater and test-retest reliabilities of this French version.
Acknowledgements
The authors wish to thank the study patients and the staff of the psychogeriatric center Jean Marie Leger for their contributions, and Alexandra Foucher for all their logistical support. B. Calvet received financial sponsorship from the Médéric Alzheimer Foundation.
Footnotes
Disclosure: The authors report no conflicts of interest.
description of Authors' Roles. The paper was jointly conceived and written by A. Barry, A. Prado-Jean, B. Calvet and J.P. Clément. A. Barry contributed to data collection. A. Prado-Jean and M. Druet-Cabanac contributed to the statistical design of the study and to data analysis.
REFERENCES
- 1.Patel V, Hope RA. A rating scale for aggressive behaviour in the elderly—the RAGE. Psychol Med. 1992;22:211–221. doi: 10.1017/s0033291700032876. [DOI] [PubMed] [Google Scholar]
- 2.Voyer P, Verreault R, Azizah GM, Desrosiers J, Champoux N, Bédard A. Prevalence of physical and verbal aggressive behaviours and associated factors among older adults in long-term care facilities. BMC Geriatr. 2005;5:13. doi: 10.1186/1471-2318-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berg G, Edwards DF, Danzinger WL, Berg L. Longitudinal change in three brief assessments of SDAT. J Am Geriatr Soc. 1987;35:205–212. doi: 10.1111/j.1532-5415.1987.tb02310.x. [DOI] [PubMed] [Google Scholar]
- 4.Talerico KA, Evans LK, Strumpf NE. Mental health correlates of aggression in nursing home residents with dementia. Gerontologist. 2002;42:169–177. doi: 10.1093/geront/42.2.169. [DOI] [PubMed] [Google Scholar]
- 5.Patel V, Hope T. Aggressive behavior in elderly people with dementia: A review. Int J Geriatr Psychiatry. 1993;8:457–472. [Google Scholar]
- 6.Lam LCW, Chui HF, NG J. Aggressive behaviour in the Chinese elderly- validation of the Chinese version of the rating scale for aggressive behaviour in the elderly (RAGE) in hospital and nursing home settings. Int J Geriatr Psychiatry. 1997;12:678–681. doi: 10.1002/(sici)1099-1166(199706)12:6<678::aid-gps610>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 7.Rabins PV, Mace NL, Lucas MJ. The impact of dementia on the family. JAMA. 1982;248:333–335. [PubMed] [Google Scholar]
- 8.Zimmer JG, Watson N, Treat A. Behavioral problems among patients in skilled nursing facilities. Am J Public Health. 1984;74:1118–1121. doi: 10.2105/ajph.74.10.1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ryden MB. Aggressive behavior in persons with dementia who live in the community. Alzheimer Dis Assoc Disord. 1988;2:342–355. doi: 10.1097/00002093-198802040-00003. [DOI] [PubMed] [Google Scholar]
- 10.Cohen-Mansfield J, Billig N. Agitated behaviors in the elderly. J Am Geriatr Soc. 1986;34:711–721. doi: 10.1111/j.1532-5415.1986.tb04302.x. [DOI] [PubMed] [Google Scholar]
- 11.Cohen-Mansfield J, Marx MS, Rosenthal AS. A description of agitation in a nursing home. J Gerontol Med Sci. 1989;44:M77–M84. doi: 10.1093/geronj/44.3.m77. [DOI] [PubMed] [Google Scholar]
- 12.Micas M, Ousset PJ, Vellas B. Évaluation des troubles du comportement. Présentation de léchelle de Cohen-Mansfield. La Revue Française de Psychiatrie et de Psychologie. Médicale. 1997:151–154. [Google Scholar]
- 13.Folstein MF, Folstein SE, McHugh PR. ”Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 14.Cumming JL, Mega MS, Gray K, Rosemberg -Thompson S, Gornbein T. The Neuropsychiatric Inventory: comprehensive assessement of psychopathology in dementia. Neurology. 1994;44:2308–2314. doi: 10.1212/wnl.44.12.2308. [DOI] [PubMed] [Google Scholar]
- 15.Salzman C, Jeste DV, Meyer RE, et al. Elderly patients with dementia-related symptoms of severe agitation and aggression: consensus statement on treatment options, clinical trials methodology, and policy. J Clin Psychiatry. 2008;69:889–898. doi: 10.4088/jcp.v69n0602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zuidema SU, de Jonghe JF, Verhey FR, Koopmans RT. Predictors of neuropsychiatric symptoms in nursing home patients: influence of gender and dementia severity. Int J Geriatr Psychiatry. 2009;24:1079–1086. doi: 10.1002/gps.2225. [DOI] [PubMed] [Google Scholar]
- 17.Margari F, Sicolo M, Spinelli L, et al. Aggressive behavior, cognitive impairment, and depressive symptoms in elderly subjects. Neuropsychiatr Dis Treat. 2012;8:347–353. doi: 10.2147/NDT.S33745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brodaty H, Low LF. Aggression in the elderly. J Clin Psychiatry. 2003;64(Suppl 4):36–43. [PubMed] [Google Scholar]
- 19.Zeller A, Hahn S, Needham I, Kok G, Dassen T, Halfens RJ. Aggressive behavior of nursing home residents toward caregivers: a systematic literature review. Geriatr Nurs. 2009;30:174–187. doi: 10.1016/j.gerinurse.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 20.Cornaggia CM, Beghi M, Pavone F, Barale F. Aggression in psychiatry wards: a systematic review. Psychiatry Res. 2011;189:10–20. doi: 10.1016/j.psychres.2010.12.024. [DOI] [PubMed] [Google Scholar]
- 21.Brodaty H, Draper B, Saab D, et al. Psychosis, depression and behavioural disturbances in Sydney nursing home residents: prevalence and predictors. Int J Geriatr Psychiatry. 2001;16:504–512. doi: 10.1002/gps.382. [DOI] [PubMed] [Google Scholar]
- 22.Teresi J, Morris J, Mattis S, Reisberg B. Cognitive impairment among SCU and non-SCU residents in the United States: Estimates from the National Institutes on Aging collaborative studies of dementia special care units for Alzheimer's disease. Res Pract Alzheimers Dis. 2001;4:117–138. [Google Scholar]
- 23.Rosen T, Pillemer K, Lachs M. Resident-to-Resident Aggression in Long-Term Care Facilities: An Understudied Problem. Aggress Violent Behav. 2008;13:77–87. doi: 10.1016/j.avb.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gothelf D, Apter A, van Praag HM. Measurement of aggression in psychiatric patients. Psychiatry Res. 1997;71:83–95. doi: 10.1016/s0165-1781(97)00047-4. [DOI] [PubMed] [Google Scholar]
- 25.Suris A, Lind L, Emmett G, Borman PD, Kashner M, Barratt ES. Measures of aggressive behavior: overview of clinical and research instruments. Aggress Violent Behav. 2004;9:165–227. [Google Scholar]
- 26.Nunnally JC, Bernstein I. Psychometric theory. 2nd edition. New York: McGraw-Hill; 1978. 736p [Google Scholar]
- 27.Burton LC, Rovner BW, German PS, Brant LJ, Clark RD. Neuroleptic use and behavioral disturbance in nursing homes: a 1-year study. Int Psychogeriatr. 1995;7:535–545. doi: 10.1017/s1041610295002274. [DOI] [PubMed] [Google Scholar]
- 28.Devanand DP, Marder K, Michaels KS, et al. A randomized, placebo-controlled dose-comparison trial of haloperidol for psychosis and disruptive behaviors in Alzheimer's disease. Am J Psychiatry. 1998;155:1512–1520. doi: 10.1176/ajp.155.11.1512. [DOI] [PubMed] [Google Scholar]
- 29.Shah AK. Violence and psychogeriatric inpatients with dementia. Int J Psychogeriatr. 1992;7:39–44. [Google Scholar]
- 30.Brodaty H, Ames D, Snowdon J, et al. A randomized placebo-controlled trial of risperidone for the treatment of aggression, agitation, and psychosis of dementia. J Clin Psychiatry. 2003;64:134–143. doi: 10.4088/jcp.v64n0205. [DOI] [PubMed] [Google Scholar]
- 31.Haute Autorité de la Santé . Maladie d'Alzheimer et maladies apparentées: prise en charge des troubles du comportement perturbateurs. 2009. http://www.has-sante.fr [Google Scholar]
- 32.Pulsford D, Duxbury J. Aggressive behaviour by people with dementia in residential care settings: a review. J Psychiatr Ment Health Nurs. 2006;13:611–618. doi: 10.1111/j.1365-2850.2006.00964.x. [DOI] [PubMed] [Google Scholar]
- 33.Draper B, Snowdon J, Meares S, et al. Case-controlled study of nursing home residents referred for treatment of vocally disruptive behavior. Int Psychogeriatr. 2000;12:333–344. doi: 10.1017/s1041610200006438. [DOI] [PubMed] [Google Scholar]
- 34.Sourial R, McCusker J, Cole M, Abrahamowicz M. Agitation in demented patients in an acute care hospital: prevalence, disruptiveness, and staff burden. Int Psychogeriatr. 2001;13:183–197. doi: 10.1017/s1041610201007578. [DOI] [PubMed] [Google Scholar]
- 35.Meddaugh DI. Reactance. Understanding aggressive behavior in long-term care. J Psychosoc Nurs Ment Health Serv. 1990;28:28–33. doi: 10.3928/0279-3695-19900401-09. [DOI] [PubMed] [Google Scholar]
- 36.Tinetti ME, Liu WL, Marottoli RA, Ginter SF. Mechanical restraint use among residents of skilled nursing facilities. Prevalence, patterns, and predictors. JAMA. 1991;265:468–471. [PubMed] [Google Scholar]
- 37.Fogarty JS. Reactance theory and patient noncompliance. Soc Sci Med. 1997;45:1277–1288. doi: 10.1016/s0277-9536(97)00055-5. [DOI] [PubMed] [Google Scholar]
- 38.Ryden MB, Feldt KS, Oh HL, et al. Relationships between aggressive behavior in cognitively impaired nursing home residents and use of restraints, psychoactive drugs, and secured units. Arch Psychiatr Nurs. 1999;13:170–178. doi: 10.1016/s0883-9417(99)80003-x. [DOI] [PubMed] [Google Scholar]
- 39.Laurin D, Voyer P, Verreault R, Durand PJ. Physical restraint use among nursing home residents: A comparison of two data collection methods. BMC Nurs. 2004;3:5. doi: 10.1186/1472-6955-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gates D, Fitzwater E, Mayer U. Violence against caregivers in nursing homes: expected, tolerated and accepted. J Gerontol Nurs. 1999;25:12–21. doi: 10.3928/0098-9134-19990401-05. [DOI] [PubMed] [Google Scholar]
- 41.Rodney V. Nurse stress associated with aggression in people with dementia: its relationship to hardiness, cognitive appraisal and coping. J Adv Nurs. 2000;31:172–80. doi: 10.1046/j.1365-2648.2000.01247.x. [DOI] [PubMed] [Google Scholar]
- 42.Evers W, Tomic W, Brouwers A. Aggressive behaviour and burnout among staff of homes for the elderly. Int J Ment Health Nurs. 2002;11:2–9. doi: 10.1046/j.1440-0979.2002.00219.x. [DOI] [PubMed] [Google Scholar]
- 43.Astrom S, Karlsson S, Bucht Get, et al. Staff's experience of the management of violent inci dents in elderly care. Scand J Caring Sci. 2004;18:410–416. doi: 10.1111/j.1471-6712.2004.00301.x. [DOI] [PubMed] [Google Scholar]
- 44.Jansen GJ, Dassen TW, Groot Jebbink G. Staff attitudes towards aggression in health care: a review of the literature. J Psychiatr Ment Health Nurs. 2005;12:3–13. doi: 10.1111/j.1365-2850.2004.00772.x. [DOI] [PubMed] [Google Scholar]