Abstract
The association of visual agnosia and prosopagnosia with cerebral metastasis is very rare. The presence of symmetric and bilateral cerebral metastases of melanoma is also uncommon.We report the case of a 34 year-old man who was admitted to hospital with seizures and a three-month history of headache, with blurred vision during the past month. A previous history of melanoma resection was obtained. CT of the skull showed bilateral heterogeneous hypodense lesions in the occipito-temporal regions, with a ring pattern of contrast enhancement. Surgical resection of both metastatic lesions was performed after which the patient developed visual agnosia and prosopagnosia. On follow-up, he showed partial recovery of visual agnosia, while prosopagnosia was still evident. The relevance of this case is the rare presentation of metastatic malignant melanoma affecting homologous occipito-temporal areas associated with prosopagnosia and associative visual agnosia.
Keywords: prosopagnosia, visual agnosia, metastasis, melanoma
Abstract
A associação de agnosia visual e prosopagnosia com metástase cerebral são muito raras. A presença de lesões metastáticas de melanoma, simétricas e bilaterais, também é incomum. Nós descrevemos o caso de um homem de 34 anos que foi admitido no hospital com convulsões e uma história de cefaléia há três meses, com dificuldade visual no último mês. História pregressa revelava ressecção de melanoma. TC de crânio evidenciou lesões hipodensas, heterogêneas, bilaterais nas regiões occipito-temporais, com captação de contraste anelar. A ressecção cirúrgica de ambas as metástases cerebrais foi realizada e o paciente desenvolveu agnosia visual e prosopagnosia após o procedimento. Na evolução houve melhora parcial da agnosia visual enquanto a prosopagnosia ainda estava evidente. A relevância deste caso consiste na apresentação rara de melanoma maligno metastático afetando as áreas occipito-temporais homólogas associada com prosopagnosia e agnosia visual associativa.
Keywords: prosopagnosia, agnosia visual, metastase, melanoma
Visual agnosia is defined as a disorder of the visual process leading to dysfunction in perception and/or recognition of objects, faces (prosopagnosia), letters (alexia) or colors (achromatopsia), either in isolation or combination1-4.
Prosopagnosia was defined by Bodamer in 1947, although it had been known since the XIX century, according to a description by Quaglino, Hughlings Jackson and Charcot. It is associated with bilateral lesions in the fusiform gyrus, although unilateral lesions involving the right fusiform gyrus have also been described5.
Ischemic lesions are the most frequent causes, but focal atrophy, congenital disorders and tumors can also be associated with prosopagnosia1.
Brain metastases are the most frequently encountered intracranial tumors. Malignant melanoma is the third most frequently encountered histologic type of brain metastasis. Occipital lobe lesions represent 5.5% of brain metastasis5,6. Association with prosopagnosia has previously been described in only one patient7.
Case report
A 34 year-old man, a professional cook, with an educational level of four years, presented a clinical history of headache, nausea and vomiting in the past three months. He also complained of a visual disorder described as a “reading difficulty” in the last month.
The patient was admitted to the emergency room because of a tonic-clonic seizure the day before. On examination, the patient was confused and somnolent, but arousable, with reactive pupils and no motor deficits.
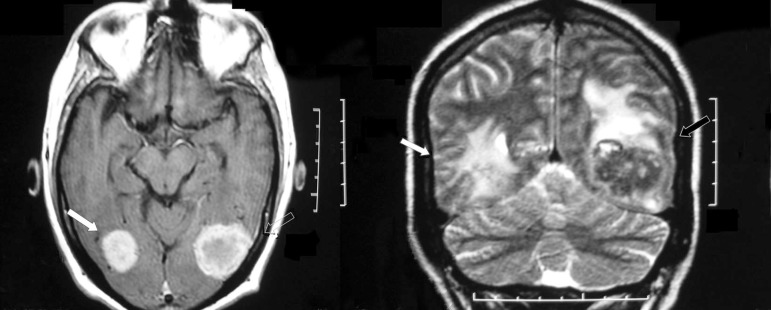
The magnetic resonance imaging (MRI) showed bilateral occipito-temporal lesions suggestive of brain metastasis. These lesions, involved the medial and inferior occipital gyrus bilaterally, the left fusiform and lingual gyrus and part of the right fusiform gyrus (Figure 1). Eight years before, the patient had undergone partial resection of a malignant melanoma in the nose, without further treatment.
Figure 1.
Preoperative MRI: arrows showing bilateral occipito-temporal metastasis with contrast enhancement.
Subsequently, he was submitted to a neurosurgical procedure involving total metastasis resection through occipital craniectomy. A ZEISS 588 microscope was used to access both lesions. Following surgery, the patient was admitted to the critical care unit.
After surgery, the patient had no motor, sensory or coordination deficits, but presented associative visual agnosia for colors, objects, faces and letters.
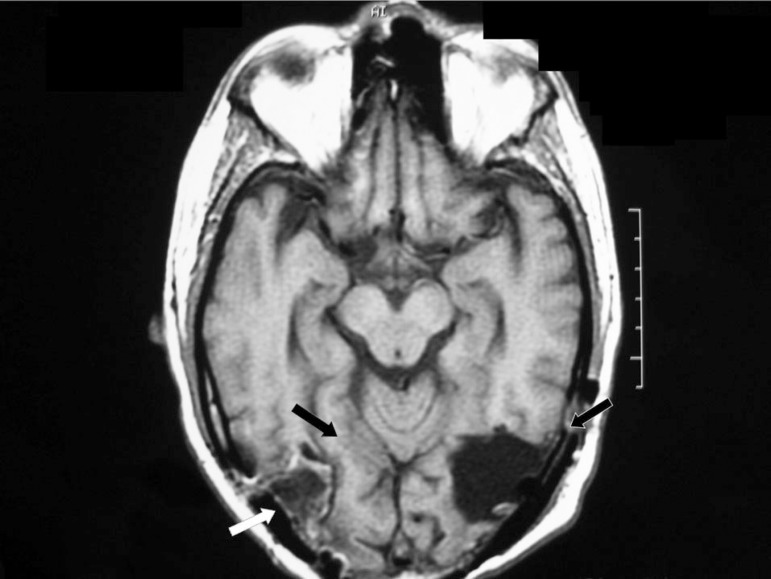
Upon hospital discharge, he underwent whole-head radiotherapy with 30 Gy, followed by chemotherapy using dacarbazine. On follow-up the MRI was repeated, showing no signs of residual brain metastasis (Figure 2).
Figure 2.
Postoperative MRI: To the right, white arrows showing involvement of inferior and occipital gyrus, with black arrows showing relative preservation of the right fusiform gyrus. To the left the black arrows show involvement of inferior and medial occipital gyrus and fusiform.
The patient was re-evaluated at the outpatient unit 30 days after surgery. He complained of difficulties in recognizing faces.
On neurological examination, he scored 21 out of 30 points on the Mini Mental State Examination (MMSE). No motor, sensory or coordination deficits were recorded. The examination of the cranial nerves was unremarkable. Visual recognition deficits were still evident, albeit improved since surgery. Neuropsychological testing three months after surgery confirmed visual recognition deficits, more markedly for faces and colors (Table 1).
Table 1.
Neuropsychological testing: face and color discrimination.
| Test | Patient | |
|---|---|---|
| Visual function | Thematic figure | Severe difficulty in describing picture parts |
| Raven progressive matrices | Color series: 16/36 (10thpercentile) | |
| Face recognition | Familiar faces (12 stimuli): no recognition; | |
| Famous faces (4 stimuli): recognition of one face (after prompt) |
Table 2 shows impaired performance in other neuropsychological tests.
Table 2.
Neuropsychological testing: attention, executive functions, memory, language and visuospatial skills.
| Visuospatial skills | Block design (WAIS) | Severe impairment |
| Rey-Osterrieth complex figure | Severe impairment | |
| Attention | Trail making test | Unable to perform test |
| Stroop test | Unable to recognize colors | |
| Planning | Chapuis labyrinth | Mild impairment |
| Wisconsin card sorting test | Number of errors = 32/64 | |
| Number of categories = 01/03 | ||
| Numbers of perseveration errors = 15 | ||
| Memory | Wechsler memory scale- | Logical memory (immediate recall) = normal |
| review (WMS-R) | Visual reproduction (immediate recall) = 21/41 (4thpercentile) | |
| Delayed recall | ||
| Logical memory = normal | ||
| Visual reproduction =10/41 (1stpercentile) | ||
| Rey-Osterrieth complex figure | Delayed recall = 06/36 (moderate impairment ) | |
| Language | Verbal fluency | Semantic category (animals): normal performance |
| Phonemic category (FA.S): normal performance | ||
| Boston naming test | 10/60 |
The patient died nine months after surgery due to multiple metastases (liver, spleen, skin and bones).
Discussion
The pattern of distribution of the lesions involving, bilaterally and almost symmetrically, the medial and inferior occipital gyrus, the left fusiform and lingual gyrus and part of the right fusiform gyrus is unusual, especially for brain metastasis. These areas play a critical role in visual recognition of objects, faces, colors and letters and are known as the “what system” of the central visual processing1.
Deficits presented soon after surgery were more obvious, probably due to brain swelling, surgical manipulation and brain resection, characterizing a clinical picture of associative visual agnosia. The patient underwent neuropsychological testing approximately three months postoperatively (Tables 1 and 2) which revealed below-average scores in almost all cognitive domains, except episodic memory and verbal fluency.Visual agnosia had become more prominent and might have influenced performance in the other tests. Recognition for faces and colors was more affected than for objects.
Prosopagnosia was initially associated with bilateral occipito-temporal lesions, most of them being ischemic1-3. Right fusiform gyrus lesions are also described in association to prosopagnosia5,9. Degenerative, vascular, traumatic and congenital lesions are possible etiologies1, but a metastatic lesion has been described in one case8.
Achromatopsy is also associated with occipito-temporal lesions, mainly on the right side. In the majority of cases it has a favorable outcome, except when the lesion is more posteriorly located, the case in our patient4.
In this patient, the right fusiform gyrus involvement was partial, but the medial and inferior occipital gyri were also involved. This pattern of anatomical distribution of the lesions probably disrupted the visual processing network for face recognition, as described by Rossion10.
The relevance of the present case is justified not only because of the rarity of prosopagnosia due to brain metastasis, but also to the relative preservation of the right fusiform gyrus, indicating the importance of other areas in the visual process related to face recognition.
References
- 1.Damasio AR, Tranel D, Rizzo M. Disorders of complex visual processing. In: Mesulam MM, editor. Principles of behavioral and cognitive neurology. 2th ed. New York: Oxford University; 2000. pp. 332–372. [Google Scholar]
- 2.Farah MJ, Feinberg TE. Visual object agnosia. Behavioral Neurology and Neuropsychology. New York: Mc Graw- Hill; 1997. pp. 239–244. [Google Scholar]
- 3.De Renzi E. Prosopagnosia. In: Farah MJ, Feinberg TE, editors. Behavioral Neurology and Neuropsychology. Bew York: Mc Graw Hill; 1997. pp. 245–255. [Google Scholar]
- 4.De Renzi E. Disorders of visual recognition. Semin Neurol. 2000;20:479–485. doi: 10.1055/s-2000-13181. [DOI] [PubMed] [Google Scholar]
- 5.De Renzi E, Perani D, Carlesimo GA, Silveri MC, Fazio F. Prosopagnosia can be associated with damage confined to the right hemisphere--an MRI and PET study and a review of the literature. Neuropsychologia. 1994;32:893–902. doi: 10.1016/0028-3932(94)90041-8. [DOI] [PubMed] [Google Scholar]
- 6.Klos KJ, O'Neill BP. Brain metastases. Neurologist. 2004;10:31–46. doi: 10.1097/01.nrl.0000106922.83090.71. [DOI] [PubMed] [Google Scholar]
- 7.Delattre JY, Krol G, Thaler HT. Distribution of brain metastases. Arch Neurol. 1988;45:741–744. doi: 10.1001/archneur.1988.00520310047016. [DOI] [PubMed] [Google Scholar]
- 8.Seron X, Mataigne F, Coyette F, Rectem D, Bruyer R, Laterre EC. A case of metamorphopsia restricted to faces and different familiar objects. Rev Neurol. 1995;151:691–698. [PubMed] [Google Scholar]
- 9.Yamamot T, Wada Y. Selective impairment of facial recognition due to a haematoma restricted to the right fusiform and lateral occipital region. J Neurol Neurosurg Psychiatr. 2001;71:254–257. doi: 10.1136/jnnp.71.2.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rossion B, Caldara R, Seghier M, Schuller AM, Lazeyras F, Mayer E. A network of occipito-temporal face-sensitive areas besides the right middle fusiform gyrus is necessary for normal face processing. Brain. 2003;126:2381–2395. doi: 10.1093/brain/awg241. [DOI] [PubMed] [Google Scholar]