Abstract
Mammalian target of rapamycin (mTOR) is the core component of two complexes, mTORC1 and mTORC2. mTORC1 is inhibited by rapamycin and analogues. mTORC2 is impeded only in some cell types by prolonged exposure to these compounds. mTOR activation is linked to tubular cell proliferation in animal models and human autosomal dominant polycystic kidney disease (ADPKD). mTOR inhibitors impede cell proliferation and cyst growth in polycystic kidney disease (PKD) models. After renal transplantation, two small retrospective studies suggested that mTOR was more effective than calcineurin inhibitor-based immunosuppression in limiting kidney and/or liver enlargement. By inhibiting vascular remodeling, angiogenesis, and fibrogenesis, mTOR inhibitors may attenuate nephroangiosclerosis, cyst growth, and interstitial fibrosis. Thus, they may benefit ADPKD at multiple levels. However, mTOR inhibition is not without risks and side effects, mostly dose-dependent. Under certain conditions, mTOR inhibition interferes with adaptive increases in renal proliferation necessary for recovery from injury. They restrict Akt activation, nitric oxide synthesis, and endothelial cell survival (downstream from mTORC2) and potentially increase the risk for glomerular and peritubular capillary loss, vasospasm, and hypertension. They impair podocyte integrity pathways and may predispose to glomerular injury. Administration of mTOR inhibitors is discontinued because of side effects in up to 40% of transplant recipients. Currently, treatment with mTOR inhibitors should not be recommended to treat ADPKD. Results of ongoing studies must be awaited and patients informed accordingly. If effective, lower dosages than those used to prevent rejection would minimize side effects. Combination therapy with other effective drugs could improve tolerability and results.
Careful clinical observations have been key to the identification of the genes mutated in autosomal dominant polycystic kidney disease (ADPKD) and tuberous sclerosis complex (TSC), the function of the gene products, and mammalian target of rapamycin (mTOR) signaling as an important player in the pathogenesis of ADPKD and hamartomatous diseases. ADPKD, a potentially lethal monogenic disorder with an estimated prevalence of 1:400 to 1:1000, is characterized by the development of cysts in the kidneys, liver, seminal vesicles, pancreas, and arachnoid membrane; intracranial aneurysms and dolichoectasias; aortic root dilation and aneurysms; mitral valve prolapse; and abdominal wall hernias (1). TSC, an autosomal dominant disease with a prevalence of 1:6000 to 1:10,000, is characterized by multiple brain, retina, skin, kidney, heart, and lung hamartomas (2). A Portuguese family segregating a chromosome 16:22 translocation with ADPKD and TSC helped to identify the TSC2 and PKD1 genes immediately adjacent to each other on chromosome 16 (3,4). The cloning of PKD1 and subsequently PKD2, genes that encode polycystin-1 and polycystin-2, led to the identification of a new subfamily of transient receptor potential channels (5). The cloning of TSC1 and TSC2, genes that encode hamartin and tuberin, made possible studies of Tsc1 and Tsc2 homologues in Drosophila and the subsequent identification of the hamartin-tuberin heterodimer as a GTPase-activating protein for Rheb (Ras homolog enriched in brain), linking growth factor, nutrient, and energy sensing signals to mTOR and mTOR-dependent targets (6). The description of a contiguous gene syndrome characterized by early onset of severe polycystic kidney disease (PKD) in patients with deletions involving PKD1 and TSC2 suggested that polycystin-1 and tuberin function in a common pathway (7). A better understanding of the molecular mechanisms laid out the foundation for the development of potentially effective therapies (8). The purpose of this review is to critically analyze the potential benefits and risks of mTOR inhibitors to treat ADPKD, TSC, and other hamartomatous diseases.
Overview of mTOR Signaling and Inhibitors
mTOR is a serine/threonine kinase of the phosphoinositide 3-kinase (PI3K)-related kinase family identified as the mammalian target of rapamycin (sirolimus). Rapamycin is a fungal metabolite found to have potent growth-inhibitory and immunosuppressant properties (9,10).
mTOR is the core component of two distinct complexes only partially characterized: complex 1 (mTORC1) and complex 2 (mTORC2) (9). In addition to mTOR, both complexes contain the small adaptor GβL but differ in the composition of additional adaptors. In particular, the presence of the Rictor protein in the complex characterizes mTORC2, whereas the Raptor protein defines mTORC1 (Figure 1, A and B) (10–12). mTOR can be specifically inhibited by rapamycin only when it is in mTORC1, leading to the initial definition of mTORC1 as “rapamycin sensitive” and of mTORC2 as “rapamycin insensitive” (12), although subsequent studies demonstrated that the mTORC2 assembly can be inhibited in long-term treatments with rapamycin in some cell types (13).
Figure 1.
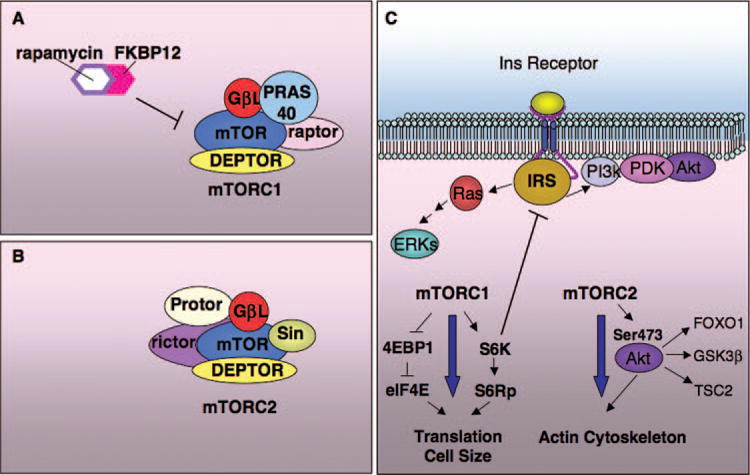
Schematic overview of the mTOR complexes, mTORC1 and mTORC2, and of the feedback loop. (A) The rapamycin-sensitive mTORC1 comprises, in addition to the mTOR kinase, raptor, GβL, PRAS40, and DEPTOR. (B) mTORC2 contains Rictor, GβL, Protor, Sin, and DEPTOR. (C) mTORC1 regulates translation, cell size, and the cell cycle, as well as autophagy and cellular metabolism. mTORC2 regulates the cellular cytoskeleton. In addition, mTORC2 is the kinase responsible for phosphorylation of Akt in Ser473. Activation of mTORC1 results in regulation of a negative feedback loop through which S6K inhibits the insulin receptor signaling by phosphorylating and inducing degradation of the adaptor IRS. As a consequence, activation of mTORC1 downregulates PI3k/Akt and the ERKs, whereas inhibition of mTORC1 upregulates both cascades.
The functions and downstream biologic effects of the two complexes are also different. mTORC1 is involved in regulating cell cycle progression, translational control, and cellular energy responses (11), whereas mTORC2 has been recently identified as the kinase responsible for phosphorylating Akt (or protein kinase B) in Ser-473 and plays a role in regulating the actin cytoskeleton (12,14).
mTORC1 is activated in response to an elevated GTP-bound form of Rheb, a small GTPase of the Ras superfamily, through an unclear mechanism (15). The guanine nucleotide exchange factor inducing Rheb’s active state was recently identified in Drosophila (16), whereas the GTPase-activating protein (GAP) inducing its inactive state is tuberin, the TSC2 gene product (17). The mechanisms regulating the complex TSC1/TSC2 have been the focus of intense investigations, leading to the identification of several cascades that regulate the GAP activity of TSC2, and consequently Rheb/mTORC1 (Figure 2). Tuberin can be phosphorylated in numerous phosphosites (18). Several kinases have been reported to phosphorylate tuberin; some of them lead to inhibition of its GAP activity, ultimately resulting in upregulation of mTORC1, including Akt (19), p90RSK (20), and the extracellular-related kinases (ERKs) (21), whereas others lead to enhanced GAP activity, ultimately resulting in downregulation of mTORC1, including 5′-AMP-activated protein kinase (AMPK) (22), GSK3β (23), and the hypoxia-induced molecule REDD1 (24).
Figure 2.
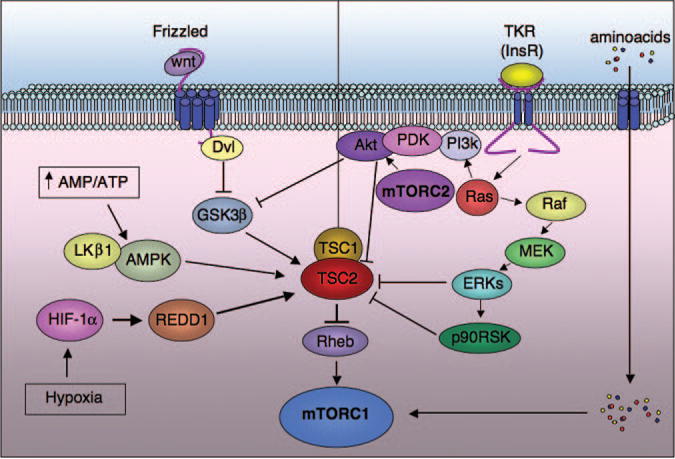
Overview of the cascades converging on regulation of the TSC2 gene product tuberin. Downstream of the tyrosine kinase receptor (TKR) signaling, Akt, ERK, and p90RSK can all phosphorylate different residues of TSC2, resulting in inhibition of its GAP activity toward Rheb (right diagram). As a result, activation of TKRs results in activation of the mTORC1 cascade. Amino acids can also activate mTORC1 downstream of the TSC1/TSC2 complex by acting directly on mTORC1. In contrast, REDD1, AMPK, and GSK3β act as energy or hypoxia sensors and are able to potently inhibit the mTORC1 cascade by enhancing the TSC1/TSC2 activity toward Rheb (left diagram). Wnts can activate the mTORC1 complex by inhibiting GSK3β.
The two effectors of mTORC1 that are better characterized are the ribosomal S6 kinases (SK6; p70S6K1 and p70S6K2) and the eukaryotic initiation factor 4 binding proteins 1 and 2 (4E-BP1 and 4E-BP2) (9,10). S6K is activated by phosphorylation at several sites, but the one with highest sensitivity to rapamycin and thus believed to be a direct target of mTORC1 is threonine 389 (25). Upon activation, S6K phosphorylates subunit 6 of ribosomal protein, leading to a general activation of translation through an unclear and still highly debated mechanism (9,10). Phosphorylation of 4E-BP instead leads to dissociation from eukaryotic initiation factor 4E, which is released, allowing the formation of translation initiation complexes (9,10). Thus, both branches of the downstream effectors of mTORC1 regulate translation and growth (size) of cells (Figure 1C).
In addition to acting on subunit 6 of ribosomal protein, S6K was recently found to regulate a feedback loop toward the PDGF receptor and the insulin receptor substrate (IRS) (26,27). Upon phosphorylation in Ser/Thr, IRS undergoes degradation (28), thus attenuating the response to insulin and the activation of PI3K/Akt and Ras/ERKs (29,30). As a result of this effect, a feedback loop is initiated whereby activation of mTORC1 results in activation of S6K, which in turn downregulates the IRS, PI3K/Akt, and Ras/ERKs, thus diminishing their effect on the TSC1/TSC2 complex and ultimately restoring the basal activity of mTORC1. Because of these feedback loops, constitutive inhibition of mTORC1 ultimately results in upregulation of PI3K/Akt and Ras/ERK pathways (29,30). It is important to consider this when designing therapeutic approaches through the inhibition of mTORC1.
As outlined above, mTOR was identified as the target of rapamycin and subsequently shown to be specifically inhibited by this metabolite. Rapamycin and its subsequent derivatives CCI-779 (temsirolimus), RAD001 (everolimus), and AP23573 (deforolimus) all share a similar chemical structure and comprise a binding site for the intracellular immunophilin FKBP12 (31). Interaction with FKBP12 is an absolute requirement for rapamycin and its derivatives to bind to and inhibit mTOR (31). Whereas the mechanism of action for all of these drugs is similar, the different chemical composition renders the rapamycin derivatives soluble in water, allowing for intravenous or oral administration (31). All of these molecules are specific for inhibition of mTOR only when it is associated with mTORC1. In certain cases, this might represent a problem, because inhibition of mTORC1 leads to upregulation of tumorigenic cascades (e.g., PI3K/Akt and Ras/ERKs) as highlighted above. Although long-term treatment with rapamycin was reported to downregulate mTORC2, this effect appears to be cell-type-dependent (13). Therefore, treatment with rapamycin will be effective and safe mostly in tissues (cancers or cystic tissues) in which mTORC2 is inhibited in long-term treatments. A new generation of drugs directed against the mTOR catalytic site is being developed that might be effective on mTORC1 and mTORC2 (32). These drugs will be preferable in cases where the feedback loops are insensitive to long-term treatment with rapamycin. Alternatively, combination therapies might be used to bypass this problem (33,34).
Dysregulation of mTOR Signaling in Hamartoma Syndromes
Hamartomas are a benign, histologically defined subtype of tumors with relatively normal differentiation but disorganized tissue architecture. Hamartomas can present as incidental findings in the general population or clinically defined familial syndromes with variable expressivity involving one or more body sites. Positional cloning of Mendelian hamartoma syndromes has identified at least seven disease genes (TSC1, TSC2, PTEN, STK11, FLCN, PKD1, and NF1) that encode components of multiple signaling pathways that converge at the mTORC1 complex (Figure 3, Table 1). Although an autosomal dominant inheritance underlies all of these syndromes, a “2-hit” cellular recessive mechanism has been shown in many but not all of the associated hamartomas, suggesting that the disease genes function as tumor suppressors (35,36). Interestingly, some but not all of these mTOR-dysregulated hamartoma syndromes are associated with an increased risk of cancer (35,37,38).
Figure 3.
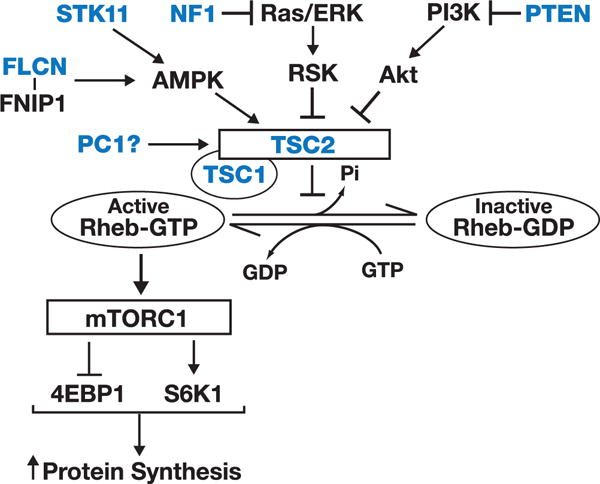
Multiple signaling (AMPK, Ras/ERK, PIK3) pathways converge at the TSC1-TSC2 complex to regulate the rapamycin-sensitive mTORC1 activity, protein synthesis, and cell growth. Mutations of at least seven (blue) disease genes associated with Mendelian hamartoma syndromes have been linked to mTORC1 activation (see text for more details), providing a rationale for the potential therapeutic use of mTOR inhibitors in these disorders. 4EBP1, initiation factor 4E binding protein; FNIP1, folliculin-interacting protein 1; NF1, neurofibromin 1; PTEN, phosphatase and tensin homolog; RSK, p90 S6K 1; STK11, serine/threonine kinase 11 (also known as LKB1); TSC1, hamartin; TSC2, tuberin.
Table 1.
| Gene | Protein | Protein Function | Disease | Clinical Features |
|---|---|---|---|---|
| TSC1 | Hamartin (TSC1) | Binding partner for TSC2 | Tuberous sclerosis | Hamartomas in skin, central nervous system, and heart; renal cysts and angiomyolipomas; lymphangiomyomatosis |
| TSC2 | Tuberin (TSC2) | Rheb GAP | Tuberous sclerosis | Same as above |
| PTEN | PTEN | 3′-phosphoinositide phosphatase | PTEN-hamartoma tumor syndromes | Hamartomas in multiple organs, lentigines, macrocephaly, hemihypertrophy, increased risk of breast and thyroid cancer |
| STK11 | STK11 | AMPK-dependent regulator of TSC2 | Peutz-Jeghers syndrome | Hamartomas in GI tract, lentigines, increased risk of GI and non-GI carcinomas |
| FLCN | Folliculin (FLCN) | AMPK-dependent regulator of TSC2 | BHD syndrome | Hamartomas in multiple organs (including hair follicles), lung cysts (spontaneous pneumothorax), increased risk of renal carcinomas |
| PKD1 | Polycystin 1 (PC1) | Regulator of TSC2? | Autosomal dominant polycystic kidney disease | Renal and extrarenal cysts, cardiac valvular and vascular defects (including intracranial arterial aneurysms), hernias, colonic diverticulosis |
| NF1 | Neurofibromin 1 (NF1) | RAS GAP | Neurofibromatosis | Neurocutaneous hamartomas, endocrine tumors, increased risk of malignant peripheral nerve tumors, sarcomas, myeloid leukemia |
GI, gastrointestinal; PTEN, phosphatase and tensin homolog (PTEN-hamartoma tumor syndromes include Cowden disease, Bannayan-Riley-Ruvalcaba syndrome, Proteus syndrome, and Lhermitte-Duclos syndrome); STK11, serine/threonine kinase 11 (also known as LKB1).
Figure 3 shows the components of the key signaling pathways that converge at the rapamycin-sensitive mTORC1 and how disease mutations affecting some of the upstream regulatory proteins can lead to mTOR activation. In this regard, the most extensively characterized example is TSC (35,39). The TSC1-TSC2 protein complex serves as a node that integrates cues from growth factors, nutrients, and other external signals to regulate mTORC1 activity. Loss-of-function TSC1 or TSC2 mutations are associated with increased Rheb-GTP levels and aberrant activation of mTORC1 in various TSC-associated hamartomas (39,40). Growth factor stimulation and increased Akt activity, after receptor tyrosine kinase activation, provide a major upstream negative regulatory signal to TSC2. Loss-of-function mutations of phosphatase and tensin homolog, a lipid phosphatase that negatively regulates Akt, have been documented in several closely related clinical syndromes linked to aberrant mTOR activation (41,42). Similarly, growth factors that lead to RAS activation can also provide an upstream negative regulatory signal to TSC2 through the mitogen-activated protein kinase (ERK/RSK) cascade. Loss-of-function mutations of neurofibromin, which negatively regulates RAS, can cause aberrant mTOR activation in neurofibromatosis (43). By contrast, cellular energy depletion (low AMP) is sensed by AMPK and provides a positive regulatory signal to TSC2. Loss-of-function mutations of STK11 (LKB1), which release TSC2 activation by AMPK, cause Peutz-Jeghers syndrome and aberrant mTOR activation (44). Likewise, through a complex, incompletely understood interaction between folliculin (FLCN), FLCN-interacting protein 1, and AMPK, loss-of-function mutations of FLCN, the product of a gene that is mutated in Birt-Hogg-Dubé (BHD) syndrome, have also been shown to cause aberrant mTOR activation (45,46). More recently, aberrant mTOR activation has been implicated in playing a pathogenic role in ADPKD (see later section) (47).
The documentation of aberrant mTOR activation in the above hamartoma syndromes provides a strong rationale for testing the therapeutic efficacy of mTOR inhibitors in these disorders. Indeed, a recently completed nonrandomized, open-label study of 20 patients with TSC showed that a 12-month treatment with rapamycin reduced the mean volume of renal angiomyolipomas by approximately 50% compared with the baseline value and improved the lung function of 14 of the same patients who also have lymphangioleiomyomatosis. However, the renal and pulmonary treatment benefits tended to reverse in most patients after discontinuation of rapamycin for 1 year (48). Despite these exciting initiatives, a better understanding of the pathobiology of mTOR signaling in the above hamartoma syndromes is needed if the therapeutic potential of mTOR inhibitors in these disorders is to be fully exploited. For example, what are the molecular bases for the distinct phenotypic differences and tissue specificities in these disorders? Does mTORC2 play a role in their pathobiology (37)? Is ciliary dysfunction involved in their pathogenesis (38)? Why is there an increased risk for cancer in some but not all of these disorders (Table 1)? Several groups have begun to address this latter question by suggesting that hyperactive mTOR signaling activates crucial negative feedback mechanisms through S6K (Figure 3) (27,49) or PDGF receptor-mediated (26) downregulation of IRS, PI3K, and Akt activities. This may explain why the risk of cancer is not increased in ADPKD, but is increased in phosphatase and tensin homolog-associated hamartoma syndromes. However, this negative feedback mechanism should also operate in neurofibromatosis, Peutz-Jeghers, and BHD syndromes, all of which are associated with an increased risk of cancer (43,44,46).
mTOR Signaling in PKD
The earliest suggestion for a role of mTOR in PKD came from the observation that many TSC patients develop renal cysts. The PKD1 and TSC2 genes were found to lie immediately adjacent to each other on chromosome 16 (3,50) in a tail-to-tail orientation, and this gene proximity is highly conserved from humans to fish (51), suggesting that the gene products may be functionally linked or that their expression may at least be coregulated. In approximately 2% to 3% of TSC patients, a contiguous germline deletion that affects TSC2 and PKD1 leads to much earlier onset and more severe PKD than mutations in the individual genes (7). Thus, the gene products may function in a common pathway, and the severe cystic phenotype in patients with a combined TSC2 and PKD1 mutation may be due to gene dosage that affects two components of the same pathway.
Components of the mTOR pathway (mTOR, S6K, and S6) were found to be aberrantly phosphorylated in epithelial cells of a subset of renal cysts in human ADPKD, autosomal recessive PKD, and PKD mouse models (38,47,52,53). The observation that some but not all of the cysts exhibit signs of mTOR activation suggests that this pathway may only be active during certain stages of cyst development or that other signaling pathways may be required for full mTOR activation. It is currently unclear if mTOR activation is sufficient to induce cyst formation because renal cysts are observed in only 32% of TSC patients and in most cases the cystic disease is relatively mild (54). These observations suggest that mTOR activation may be important, but not sufficient, for cyst growth. However, several groups independently found that rapamycin reduced renal cyst growth in rodent models of PKD (see below).
The mechanism for mTOR activation in ADPKD must ultimately be due to a direct or indirect mechanistic link to the polycystins. The identification of a binding interaction between the cytoplasmic tail of PC1 and tuberin (47) supports a model in which PC1 normally suppresses mTOR activity by its interaction with tuberin (47,55,56). Recently, Pkd1−/− mouse embryonic fibroblasts were shown to have increased cell size and phosphorylation levels of S6K, S6, and 4EBP1, consistent with activation of mTORC1 (57). Conversely, PC1 overexpression reduced ERK activation and S6KThr389, S6, and 4EBP1 phosphorylation, despite strong Akt activation. Additional studies using MDCK cells expressing dominant negative or constitutionally active Akt or MEK constructs confirmed that PC1 downregulates cell size and mTORC1 activation by affecting the ERK-mediated phosphorylation of tuberin at S664. Clinical studies have demonstrated high levels of constitutively active ERK in TSC-associated lesions that lack loss of heterozygosity in the TSC genes and in TSC2+/− cell lines (58), which suggests a positive feedback loop, with ERK activation not only upstream but also downstream of TSC/mTOR.
Currently, the role of Akt in mTOR regulation and cell proliferation in PKD remains unclear. In normal renal cells, Akt phosphorylates an inhibitory site on B-Raf, preventing cAMP activation of the B-Raf/MEK/ERK signaling pathway and cell proliferation (59–61). In cultured cells from human ADPKD cysts, Akt activity is reduced, and cAMP activates B-Raf signaling to the MEK/ERK pathway and cell proliferation (60). On the other hand, phosphorylated Akt (p-Akt) was found to be elevated in mitotic cells in Cy/+ kidneys (62). The reason for the discrepancy in basal Akt activity between cultured human ADPKD cells and cyst cells of Cy/+ kidneys in vivo is unclear. It is possible that Akt may modulate mTORC1 activity independent of its inhibitory effect on B-Raf.
mTOR is active in renal epithelial cells in developing, postnatal kidneys of mice, but markers such as P-mTOR and P-S6 become almost undetectable in adult kidneys (46) (Shillingford and Weimbs, unpublished results). This, and the finding that high-level rapamycin treatment had no apparent structural or functional effects on the healthy, adult mouse or rat kidney (47,63,64), suggests that mTOR activity is not needed for normal renal function. By contrast, increased cell proliferation, fibrosis, and cellular hypertrophy after renal injury (e.g., ischemia/reperfusion and ureteral obstruction) and during compensatory hypertrophy after unilateral nephrectomy are largely inhibited by rapamycin treatment (64–67). These studies suggest that activation of the mTOR pathway is an essential, but normally dormant, component of the response to renal injury (64–67). It has been suggested that the changes leading to renal cyst growth in PKD represent the aberrant activation of a renal repair pathway (55,56). Given that the PKD rodent models that exhibit activated mTOR and/or respond to mTOR inhibition involve a wide variety of affected proteins (Table 2), it has been suggested that all of these proteins (and likely many more) function in pathways that eventually converge on the mTOR pathway (55,56). Such a convergent pathway represents a highly attractive therapeutic target.
Table 2.
Summary of mTOR activation and sensitivity to mTOR inhibition in polycystic kidney rodent models
| Rodent Model | Affected Protein | mTOR Activation in Kidneys? | Drug Treatment | Effective? | Reference |
|---|---|---|---|---|---|
| Han:SPRD rat (Cy/+ rat) | SamCystin (mutant protein) | Yes | SRL (0.2 mg/kg/d, IP) | Yes | Tao et al. (69) |
| SRL (2 mg/kg/d, oral) | Yes | Wahl et al. (70) | |||
| EVL (3 mg/kg/d, oral) | Yes | Wu et al. (72) | |||
| SRL (0.2 mg/kg/d, IP) | Yes (long term) | Zafar et al. (73) | |||
| SRL (2 mg/kg/d, oral) | Yes | Zhang et al. (71) | |||
| Pkd1 mouse model | Polycystin-1 (conditional, knockout) | Yes | SRL (5 mg/kg/d, IP) | Yes | Shillingford et al. (80) |
| Pkd2 mouse model | Polycystin-2 | Yes (liver) | SRL (1.5 mg/kg/d, IP) | Yes (liver) | Spirli et al. (81) |
| MAL-transgenic mouse | MAL/VIP17 (overexpression) | Yes | ND | ND | Shillingford et al. (47) |
| orpk-rescue mouse | Polaris (re-expression of Polaris in hypomorphic mutant) | Yes | SRL (5 mg/kg/d, IP) | Yes | Shillingford et al. (47) |
| bpk mouse | Bicaudal-C (mutant protein) | ND | SRL (5 mg/kg/d, IP) | Yes | Shillingford et al. (47) |
| SRL (1.67 mg/kg/d, IP) | Yes | ||||
| pcy mouse | Nephrocystin-3 | Yes | SRL (3 mg/kg/d, oral) | Yes (late phase) | Gattone et al. (76) |
| ND | SRL (5 mg/kg/d, IP) | Yes | Reichardt (77) | ||
| Folliculin KO mouse | FLCN (kidney-specific, conditional KO) | Yes | SRL (2 mg/kg/d, IP) | Yes | Baba et al. (46) |
EVL, everolimus; IP, intraperitoneal; KO, knockout; ND, not determined; SRL, sirolimus.
Efficacy of mTOR Inhibitors in PKD Rodent Models
In all PKD rodent models tested so far, treatment with mTOR inhibitors has proven effective in inhibiting cyst growth and kidney enlargement and preserving renal function (Table 2). In the Cy/+ rat, a mutation in Anks6 (formally Pkdr1) that encodes for SamCystin, a novel protein with no known function, causes slowly progressive cystic disease (68). Administration of 0.2 mg/kg per d rapamycin by intraperitoneal injection for 5 weeks (69), or 2 mg/kg per d orally for 8 to 12 weeks (70,71), reduced PKD progression and preserved renal function (69,70). Everolimus, a rapamycin analogue, proved equally effective in the Cy/+ rat (72). Long-term rapamycin treatment from 1 to 12 months resulted in a normalization of kidney volume, renal function, blood pressure, and heart weight (73).
The orpk-rescue mouse arose from alterations of the gene encoding for Polaris, a protein involved in ciliogenesis and intraflagellar transport, leading to slowly progressing PKD (74). Treatment with rapamycin for 1 month (5 mg/kg per d, intraperitoneally) resulted not only in inhibition of renal growth but significant regression of already enlarged kidneys, as determined by magnetic resonance imaging (47). This was likely due to the observed induction of apoptosis, specifically in cystlining cells. In the same study, the effect of rapamycin was tested in the bpk mouse, a rapidly progressive PKD model caused by a mutation in bicaudal-C, an RNA-binding protein of no known function in mammals. Rapamycin treatment for 2 weeks (1.67 or 5 mg/kg per d, intraperitoneally) was highly effective in slowing renal and cyst growth and preserving renal function (47).
The pcy gene in mice is orthologous to the NPHP3 gene in humans; mutation in human NPHP3 causes adolescent nephronophthisis (75). Phosphorylated S6K was slightly elevated at 4 weeks, moderately increased at 12 weeks, and markedly increased at 30 weeks of age, whereas phosphorylated ERK was uniformly increased at all ages (76). Administration of pellets releasing rapamycin from 20 to 30 weeks of age to male pcy mice at a rate of 3 mg/kg per d prevented further renal cystic enlargement and deterioration of renal function (76). However, treatment between 6 and 12 weeks of age was without detectable effect, suggesting that mTOR activation may be less important at early stages of cystic disease in this animal model (76). Rapamycin was also protective in female pcy mice treated from 18 to 28 weeks of age (77).
Recently, rapamycin was tested in a cystic mouse model generated by a kidney-specific knockout of BHD, a gene that encodes FLCN (46). FLCN is the protein affected in BHD syndrome (78) and has been implicated in the regulation of the AMPK/mTOR pathway, although its exact function is unclear (79). These mice exhibit rapidly progressing PKD and die from renal failure by 3 weeks (46). Rapamycin treatment (2 mg/kg per d, intraperitoneally) reduced renal growth and nearly doubled the life span of the mice (46).
Finally, mTOR inhibitors have been recently tested in animal models orthologous to human ADPKD. Rapamycin treatment (5 mg/kg per d, intraperitoneally) was highly effective in a newly developed mouse model in which the Pkd1 gene was inactivated in a mosaic fashion (80). Rapamycin treatment resulted in strong inhibition of renal cyst growth, partial reversal of the cystic phenotype in already enlarged kidneys, and preservation of renal function. Rapamycin (1.5 mg/kg per d, intraperitoneally) significantly reduced the liver/body weight ratio, liver cyst volume, and pericystic microvascular density in a conditional Pkd2 knockout mouse (81). In both studies, rapamycin reduced the rates of cell proliferation while enhancing the rates of apoptosis. These would suggest that mTOR inhibition may also be effective in human ADPKD.
Preclinical studies summarized in Table 2 indicate that mTOR inhibition may provide a potential clinical approach to slow the progression of PKD; however, several limitations to these studies should be considered. The doses of rapamycin or everolimus used in rodent studies exceed the dose commonly used for immunosuppression in patients. In rodents, high doses of mTOR inhibitors appear to be well tolerated with no adverse effects. Small reductions in body weight have been reported in some studies (69,71,73) but not others (76,82). Rapamycin at 3 mg/kg per d (intraperitoneally) was needed to achieve complete suppression of S6 phosphorylation in the brain of an epilepsy mouse model with conditional inactivation of the TSC1 gene (82). To our knowledge, the dose of mTOR inhibitor required to adequately suppress mTOR in target organs, including PKD kidneys, in humans is unknown.
Retrospective Clinical Studies of mTOR in ADPKD
Some ADPKD patients who undergo renal transplantation receive rapamycin for immune suppression. This has led to the fortuitous circumstance in which some ADPKD patients with their native polycystic kidney still in place have been treated with rapamycin. It was reported in a small retrospective study that the total renal volumes decreased by approximately 25% during an average period of 2 years in transplanted ADPKD patients who were treated with rapamycin, whereas no significant change was found in the nonrapamycin control group (47). In a subsequent larger study, a similar trend was observed, but the difference from the control group did not achieve statistical significance (83). However, there was a significant reduction in the total liver volumes, whereas the liver volumes increased in the control group (83). These results are encouraging because they suggest that the dose of rapamycin required for immunosuppression may be sufficient to suppress mTOR activity and the growth of liver and kidney cysts. An important caveat in these studies is that the kidneys of these patients represent highly cystic end-stage kidneys in which little, if any, normal renal tissue remains.
mTOR, Fibrosis Chronic Kidney Disease, and Animal Models of Noncystic Renal Disease
mTOR signaling is important in the regulation of intrinsic renal cell, T cell, and B cell proliferation and function. Therefore, it is not surprising that activation of mTOR has been implicated in the progression of chronic kidney disease (CKD), a common pathology of glomerulosclerosis and tubulointerstitial fibrosis initiated by many diverse causes of renal injury. mTOR inhibition can be beneficial or deleterious depending on the nature and severity of the underlying renal injury, timing of treatment in relation to the onset of disease, and dose of mTOR inhibitor.
Akt and/or mTOR are activated or play a role in nonimmunologic models of CKD, such as 5/6 nephrectomy (84,85), chronic ischemic nephropathy (86–88), unilateral ureteral obstruction (89,90), type I (streptozotocin-induced) (85,91–93) and type II (db/db mice and Zucker rat) (94,95) diabetic nephropathy, protein overload (96), and adriamycin- and puromycin-induced nephropathies. In all of these cases, administration of rapamycin inhibited the development and progression of the disease at least in part by inhibiting inflammation (87) and the expression of fibrosis-associated genes such as TGF-β (67,86,97). Of note is that whereas mTOR inhibition early after renal mass reduction caused further reduction in renal function (84), late treatment was protective (84). Similarly, mTOR inhibition delayed recovery from renal ischemia reperfusion injury in mice (98,99) and rats (64,100,101) and aggravated protein ovesrload nephropathy (96), whereas it had a beneficial effect on chronic ischemic nephropathy induced by ischemia-reperfusion injury. These observations indicate that mTOR inhibition may interfere with adaptive increases in renal proliferation that are necessary for recovery from injury but inhibit potentially deleterious aspects of injury repair such as development of inflammation and fibrosis.
Interestingly, Rangan and Coombes (102) found that mTOR inhibition attenuates the renal enlargement in adriamycin nephropathy and the fibrosis without reducing proteinuria in rats, whereas Lui et al. (103) found that rapamycin given at the time adriamycin nephritis was induced or started 1 week after induction was effective in reducing the proteinuria, interstitial inflammation, and collagen expression. Everolimus pretreatment in puromycin aminonucleoside nephrosis similarly ameliorated the puromycin aminonucleoside-induced proteinuria and mononuclear leukocyte infiltration in mice (104). The attenuation of adriamycin- and puromycin-induced nephropathies contrasts with other reports that mTOR inhibitors impair pathways essential for podocyte integrity and predispose to glomerular injury (see below) (105,106).
The mTOR pathway also affects the development and progression of immunologically mediated forms of CKD, such as membranous glomerulopathy (passive and active forms of Heymann nephritis) (65,107), mesangiocapillary anti-Thy-1 nephritis (108,109), lupus (105–107,110,111), and antiglomerular basement membrane GN (112). Whereas mTOR inhibitors usually exert beneficial effects consistent with their immunosuppressive and anti-inflammatory actions, they can be detrimental under certain conditions because of downregulation of vascular endothelial growth factor (VEGF). For example, administration of high-dose everolimus to rats early after “full-dose” anti-Thy-1 antiserum inhibits endothelial cell (EC) proliferation and increases apoptosis, crescent formation, glomerulosclerosis, and mortality, whereas low-dose everolimus or treatment of a less severe lesion (“reduced dose” anti-Thy-1 model) is relatively safe, and late treatment (after the acute proliferative phase) inhibits glomerular hypertrophy, glomerulosclerosis, proteinuria, and interstitial fibrosis and improves renal function (108,109). On the other hand, rapamycin significantly reduces B and T cell responses and protects from GN when administered early in the autologous phase of antiglomerular basement membrane GN, but it worsens GN by disturbing the EC/VEGF system in the kidney once disease is established (112).
Role of mTOR in Vascular Remodeling and Angiogenesis in ADPKD
The polycystins are strongly expressed in endothelial and vascular smooth muscle cells (VSMCs) (113–116). VSMCs from Pkd1+/− or Pkd2+/− mice exhibit an exaggerated contractile response to phenylephrine associated with lesser cytosolic calcium rise (117,118). ECs from Pkd1 null mice lacking polycystin-1 in primary cilia cannot modulate calcium signaling and nitric oxide synthesis in response to fluid shear (119). Endothelium-dependent vasorelaxation is reduced in ADPKD (120). Therefore, it is not surprising that vascular pathology constitutes a prominent component of this disease. This includes renal (vascular remodeling, rarefaction, angiogenesis) and extrarenal [arterial aneurysms, dolichoectasias, and dissections (121), and possibly an increased risk for cerebral vasospasm (122) and atherosclerosis (123)] vascular pathologies.
The renal vasculature in ADPKD is characterized by small artery and arteriolar sclerosis, rarefaction, and angiogenesis at relatively early stages of the disease (121,124–128). These are not distinct, but are interrelated processes. Sustained vasoconstriction and increased blood pressure induce arterial/arteriolar hyperplasia and sclerosis, rarefaction, and focal ischemia (129). Ischemia through hypoxia-inducible transcription factors upregulates VEGF and other growth factors that stimulate angiogenesis (130). VEGF, normally expressed in tubular epithelia, is overexpressed in cyst epithelial cells (128,131). Inflammatory mediators in cyst fluids may contribute to the upregulation of VEGF (132), which in a paracrine fashion further stimulates angiogenesis and further cyst growth (131).
The PI3K/Akt/mTOR signaling pathway plays an important role in the vascular smooth muscle changes that occur in ADPKD. VSMC plasticity is important for pathologic responses such as intimal hyperplasia and atherosclerosis (133). These require dedifferentiation of VSMCs from a contractile to a proliferative, migratory, synthetic phenotype. Activation of mTOR effector S6K1, feedback inhibition of IRS-1, and inhibition of Akt2 mediate this phenotypic switch (134). Rapamycin blocks this pathway, promotes the differentiated contractile phenotype, inhibits VSMC migration and proliferation, and attenuates intimal hyperplasia. Consistent with these effects, inhibition of mTOR markedly reduces transplant vasculopathy in recipients of cardiac (118) and renal transplants (135) and the incidence of restenosis, although improving coronary artery physiology after rapamycin-eluting stents (136–139). Therefore, mTOR inhibitors have the potential of attenuating the renal vascular remodeling and possibly early development of atherosclerosis associated with ADPKD.
Both mTORC complexes and Akt signaling play a key role in angiogenesis (140–143). mTORC1 activates EC proliferation. mTORC2 directly phosphorylates Akt and promotes EC survival (13,144). Akt activates endothelial nitric oxide synthase by direct phosphorylation (145). Akt1, rather than Akt2, is required for acute permeability response to VEGF and angiogenesis in a hind-limb ischemia model (146). Contrary to VSMCs, where Akt is only partially inhibited after prolonged treatment with mTOR inhibitors, Akt is strongly inhibited in ECs after exposure to rapamycin for 24 hours (140). These effects on ECs and VSMCs may contribute to the increased risk of late coronary artery thrombosis and peri-stent coronary aneurysms with rapamycin-eluting stents (140,147–150).
Angiogenesis is required for tumor growth, and the antineoplastic action of mTOR inhibitors is due at least in part to their antiangiogenic properties (151,152). Capillary sprouting and development of a rich vascular network around the cysts ensures that the proliferation of epithelial cells is matched by an adequate supply of blood and nutrients (127). Therefore, mTOR inhibition has the potential of preventing cyst expansion by its antiangiogenic effect (127). However, the results of antiangiogenic strategies targeting VEGF in PKD have been mixed. Treatment of Han:SPRD Cy/+ rats with ribozymes inhibiting mRNA expression of VEGF receptors 1 or 2 blunted cystogenesis and improved renal function (131). Administration of the VEGF receptor inhibitor SU-5416 to Pkd2WS25/− mice was protective against the development of cystic disease in the liver, but not in the kidney (153). On the other hand, treatment of developing CD-1 mice with antibodies against VEGF receptor 2 promoted renal cyst growth (154).
Strategies targeting angiogenesis in ADPKD raise additional concerns. Apoptotic EC loss in peritubular capillaries is associated with interstitial fibrosis (155–157). By further inducing EC apoptosis, such strategies could potentially accelerate the development of interstitial fibrosis, a prominent feature in polycystic kidneys (124), and hasten the decline in kidney function. EC and VSMC apoptosis may be important in the pathogenesis of arterial aneurysms and dissections, well recognized extrarenal manifestations of ADPKD. However, to date, no association between administration of mTOR inhibitors and aneurysmal rupture or arterial dissection has been reported. By their effects on nitric oxide production and VSMC contractility, mTOR inhibitors could enhance the development of hypertension or vasospastic complications. Although hypertension has been reported to be less common in mTOR than in calcineurin inhibitor-treated patients, a recent study has shown an equivalent development of hypertension in rats treated with mTOR or calcineurin inhibitors (158). Hypertension, proteinuria, and acute kidney injury are recognized adverse effects of anti-VEGF therapy (159).
Risk/Benefit Considerations for mTOR Inhibition Therapy: Lessons Learned from Organ Transplantation and Treatment of Glomerulopathies
mTOR inhibitors have gained a proper place in the present-day immunosuppressive armamentarium in renal transplantation (160–162). However, significant adverse events lead to discontinuation of mTOR inhibitors in between 7% and 37% of patients, with discontinuation reported to be directly related to exposure to sirolimus and tacrolimus (7.8% and 2.2%, respectively) (163,164). Nonrenal-related side effects are listed in Table 3. These, along with a mild to moderate nephrotoxic potential (see below), need to be kept in mind when considering the use of mTOR inhibitors for nontransplant and nonmalignant medical disorders such as ADPKD.
Table 3.
| Side Effect | Frequency |
|---|---|
| Hypertriglyceridemia | High |
| Hypercholesterolemia | High |
| Mucositis (mouth ulcers, diarrhea) | High |
| Folliculitis, acne, dermatitis | High |
| Anemia, leukopenia, thrombocytopenia | Moderate |
| Impaired wound healing | Moderate |
| Arthralgias | Moderate |
| Insulin resistance | Moderate |
| Liver enzyme elevations | Low |
| Decreased testosterone and spermatogenesis | Low |
| Eyelid or leg edema | Low |
| Angioedema | Rare |
| Lymphedema | Rare |
| Interstitial pneumonitis | Rare |
| Thrombotic microangiopathy | Rare |
The mTOR inhibitor-induced dyslipidemia may result in part from a decrease in catabolism of apolipoprotein (apo)B100-containing lipoproteins, possibly because of downregulation of LDL receptors (165,166). This hyperlipidemic effect should be weighed against the potential antiatherogenic effects of these drugs. Administration of everolimus to LDL receptor-deficient (LDLR−/−) mice markedly reduced the extent of atherosclerosis despite a 40% increase of plasma cholesterol (167). Although administration of rapamycin to transplant recipients increases cholesterol and triglyceride levels by 17 and 59 mg/dl (at a dose of 2 mg/d) or by 30 and 103 mg/dl (at a dose of 5 mg/d), respectively, compared with patients receiving placebo or azathioprine, and the Framingham risk model predicts that a 17-mg/dl elevation in cholesterol would increase the incidence of coronary heart disease by 1.5 new cases per 1000 persons per year and coronary heart disease death by 0.7 events per 1000 persons per year (168), no increase in the 4-year risk of cardiovascular events was detected in rapamycin-treated patients in a single-center study (169).
Of particular concern is their potential nephrotoxicity. In transplant patients, mTOR inhibitors cause delayed renal allograft function and increase the nephrotoxicity of calcineurin inhibitors. On the other hand, conversion from calcineurin to mTOR inhibitor-based immunosuppressive regimens offers the opportunity to improve renal function (170). The probability of benefit from this conversion diminishes with time from transplant, impairment of renal function, and severity of proteinuria (170,171). A large, multicenter, prospective, randomized, open-label rapamycin renal conversion trial (CONVERT) randomly assigned (2:1) 830 maintenance renal allograft recipients (stratified by baseline GFR; 20 to 40 versus >40 ml/min) to undergo conversion or to continue receiving calcineurin inhibitor-based therapy (172). Enrollment in the group with baseline GFR of 20 to 40 ml/min was discontinued because of a higher incidence of safety end points in the rapamycin conversion arm (16.7% versus 0%). In the patients with baseline GFR >40 ml/min and urine protein to creatinine ratio ≤0.11, a modest improvement in GFR was noted at 12 and 24 months. De novo proteinuria occurred as an unexpected finding after sirolimus conversion, and worsening proteinuria was associated with sclerotic glomeruli at baseline (172). A smaller study assessed outcomes by the magnitude of proteinuria at conversion (≤300, 301 to 3500, or >3500 mg/d). Increasing degree of proteinuria at baseline was associated with increased levels of creatinine 6 months later (173). Similar observations have been made in cardiac and pulmonary transplant patients (174,175).
The electrophoretic pattern, response to angiotensin-converting enzyme inhibitors, and demonstration of normal tubular endocytosis of albumin indicate that the proteinuria associated with the administration of mTOR inhibitors is of glomerular origin (176–178). Development of or increase in proteinuria after switching from a calcineurin to an mTOR inhibitor may in part be due to a renal hemodynamic effect (105). Nevertheless, a large body of evidence indicates that mTOR inhibitors are, at least in part, directly responsible. Development or increase in proteinuria has been observed in patients switched to rapamycin from an azathioprine-based regimen (179), in kidney transplant recipients treated de novo with mTOR inhibitors compared with control groups receiving calcineurin inhibitor-based (180–182) or mycophenolate-based (183) immunosuppressive regimens, and rarely in liver transplant recipients (184). In a few patients, proteinuria was in the nephrotic range and remitted after withdrawal of the drug (185). Prolonged rapamycin treatment of cultured human podocytes reduces the expression of total mTOR, mTORC1 activation, Rictor, mTORC2 formation, and Akt phosphorylation; downregulates nephrin, TRPC6, Nck, WT-1, and VEGF; and inhibits cell adhesion and motility (105,106).
There is limited information on the use of mTOR inhibitors in nontransplanted patients with underlying renal disease. Administration of rapamycin to patients with focal segmental glomerulosclerosis or proteinuric primary glomerulopathies has been associated with effects ranging from worsening of proteinuria and/or acute kidney injury (186,187) to partial or complete remission of the proteinuria in some patients (188). Proteinuria (1 to 7 g/d) or microalbuminuria developed in 3 and 5 of 62 type I diabetes mellitus patients, respectively, who underwent islet transplantation; in all patients, the proteinuria or microalbuminuria resolved after discontinuation of rapamycin (189). Proteinuria in ADPKD is usually low grade (<1 g/d) and associated with higher disease severity and worse prognosis (190–192). Currently, there is no information on whether administration of mTOR inhibitors to patients with ADPKD might increase proteinuria or negatively affect renal function, although it appeared to be safe in an animal model of PKD (76,193). Therefore, close monitoring of proteinuria and renal function is essential in clinical trials of mTOR inhibition in ADPKD, particularly in patients with more advanced stages of the disease.
Strategies for a Clinical Trial Design Using mTOR Inhibitors in ADPKD
Data from various longitudinal ADPKD cohort studies have demonstrated that cyst volume growth represents an exponential expansion process (194–196). These studies have also impressively shown that the GFR decline occurs only late in the disease, at a time when the kidney has already been irreversibly damaged by the relentlessly progressing cyst growth. The process of glomerular hyperfiltration might explain this dissociation between the steadily progressing cyst growth and the late GFR decline. The tardy decline of GFR is often accelerated, leading to ESRD within only a few years.
Therefore, the cyst volume growth rate represents a more suitable study end point than GFR decline, because the effect of a drug on cyst growth can be precisely monitored by repetitive magnetic resonance imaging or computed tomography scanning with subsequent volumetry of the kidneys and/or the cysts. GFR decline is a late phenomenon, and it might be difficult to obtain a therapeutic benefit with mTOR inhibitors at this later stage. This is also illustrated by another genetic disease, namely Fabry disease, which is a lysosomal storage disease for which it has been shown that late treatment with recombinant α-galactosidase enzyme replacement in proteinuric patients with impaired GFR has little or no effect (197). ADPKD and Fabry disease require establishment of treatment that is early and lifelong to be effective. Health authorities must be convinced to use cyst volume growth retardation as a meaningful clinical end point because it is likely that it will also retard or even prevent the occurrence of ESRD. It can also be expected that drugs that reduce cyst volume growth will have an effect on other ADPKD-related morbidities, including delayed development of hypertension or less cyst bleeding.
ADPKD is a slowly progressing disease, requiring a long treatment time to detect meaningful effects of mTOR inhibitors on cyst volume growth retardation. Volume changes can reliably be detected in a short interval of 6 months (195); however, because approximately 10% to 20% of patients display volume regression within 6 months (because of the spontaneous rupture of cysts) (195), a much longer observation time is recommended. The dosage of the mTOR inhibitors must also be adapted to the specific side effect profile of these drugs. Mucositis, infections, hyperlipidemia, anemia, and thrombocytopenia are the most common, and the severity of these side effects depends on the dosage and the achieved trough levels. Therefore, for a lifelong treatment, it would be desirable to use a lower dosage than what is used for prevention of transplant rejection.
Currently, there is detailed information on the design of four ongoing clinical trials using mTOR inhibitors in patients with ADPKD (198,199). The data from these studies are summarized in Table 4. Several other additional small trials have been reported at scientific meetings, some of which have been published in abstract form (data not shown). A small pilot study of rapamycin (1 mg/d orally for 6 months) has recently reported promising results, but extraordinarily high rates of renal enlargement, particularly in the control group, were observed (200).
Table 4.
Currently active clinical trials using mTOR inhibitors in ADPKD
| Study Name | Trial Number | Sponsor | Study Drug |
Study Design | Treatment Duration (months) |
Eligibility (age in years; GFR in ml/ min/1.73 m2) |
Patient Number |
Primary End Point | Completion Date |
|---|---|---|---|---|---|---|---|---|---|
| SUISSE ADPKD (202) | NCT00346918 | University of Zürich, Zürich, Switzerland | SRL | Single-left, open-label, randomized | 24 | Age 18 to 40; GFR >70 | 100 | Percent TKV change, MRI | June 2010 |
| SIRENA study (203) | NCT00491517 | Mario Negri Institute, Bergamo, Italy | SRL | Single-left, open-label, randomized, crossover | 6 | Age 18 to 80; GFR >40 | 16 | TKV change, CT | December 2009 |
| Sirolimus for ADPKD (204) | NCT00286156 | The Cleveland Clinic, Cleveland, Ohio, United States | SRL | Single-left, open-label, randomized, dose comparison | 12 | Age ≥18; I: GFR ≥60, II GFR: 25 to 59 | 30 | Iothalamate GFR change (secondary end point, TKV/TLV, CT) | – |
| Everolimus in ADPKD (205) | NCT00414440 | Novartis Pharmaceuticals, Basel, Switzerland | EVL | Multileft, placebo-controlled, randomized | 24 | Age 18 to 65; GFR 30 to 89 | 400 | TKV change, MRI | December 2009 |
CT, computed tomography; MRI, magnetic resonance imaging; TKV, total kidney volume; TLV, total liver volume.
Three of the four trials use kidney (cyst) volume change as the primary end point. The patient numbers and dosing ranges are quite different in the four trials. The SUISSE ADPKD study enrolled 100 patients and is using rapamycin at 2 mg/d for 18 months. A larger German study enrolled 400 patients and is using everolimus for 2 years at a higher dose. The Cleveland Clinic and the Bergamo studies involve a smaller patient population with a dose-finding strategy.
Definitive data from these four clinical trials will be available in 2010. Certainly, if an important beneficial effect of mTOR inhibitors is found, more detailed dosing strategies targeting early, intermediate, and late stages of the disease need to be tested in additional trials. In the case that only a moderate positive effect is found, future trials could seek to establish whether combination therapy of mTOR inhibitors, which primarily target cell proliferation, with drugs targeting fluid secretion, would improve therapeutic results.
Currently, it is too early to recommend that patients with ADPKD start treatment with mTOR inhibitors. The results of the ongoing studies must be awaited, and patients must be informed accordingly.
Acknowledgments
This manuscript resulted from a meeting held in Montréal, Canada, October 11 to 12, 2008. The authors had total responsibility for the content and writing of the manuscript. The meeting was funded by Wyeth Pharmaceuticals [makers of Rapamune (sirolimus)], which was acquired by Pfizer, Inc., in October 2009. MediMedia Educational Group, LLC, provided support for the meeting. Each author, with the exception of Drs. Qi Qian and Vicente E. Torres, received an honorarium from Wyeth Pharmaceuticals.
Disclosures
Dr. Vicente Torres has had research and is an investigator in clinical trials funded by Otsuka and Novartis Pharmaceuticals. Dr. Arlene Chapman has served as a consultant for Otsuka and Novartis Pharmaceuticals. Dr. Vincent Gattone has served as a consultant for Hoffmann-La Roche, has performed studies funded by Amgen and Genzyme, and has a patent licensed by Otsuka Pharmaceuticals. Dr. York Pei has served as a consultant to Novartis, Plexxikon, Roche, and Wyeth Pharmaceuticals. Dr. Qi Qian is principal investigator for an ADPKD study (Wyeth # 0468E6-4517). Dr. Darren P. Wallace is a consultant for Plexxikon, Inc. Dr. Rudolf P. Wüthrich has served as an advisory board member for Novartis and Wyeth Pharmaceuticals and has received grant support from Wyeth Pharmaceuticals for research in the field of ADPKD.
References
- 1.Torres VE, Harris PC, Pirson Y. Autosomal dominant polycystic kidney disease. Lancet. 2007;369:1287–1301. doi: 10.1016/S0140-6736(07)60601-1. [DOI] [PubMed] [Google Scholar]
- 2.Roach ES, Gomez MR, Northrup H. Tuberous sclerosis complex consensus conference: Revised clinical diagnostic criteria. J Child Neurol. 1998;13:624–628. doi: 10.1177/088307389801301206. [DOI] [PubMed] [Google Scholar]
- 3.European Chromosome 16 Tuberous Sclerosis Consortium. Identification and characterization of the tuberous sclerosis gene on chromosome 16. Cell. 1993;75:1305–1315. doi: 10.1016/0092-8674(93)90618-z. [DOI] [PubMed] [Google Scholar]
- 4.The European Polycystic Kidney Disease Consortium. The polycystic kidney disease 1 gene encodes a 14 kb transcript and lies within a duplicated region on chromosome 16. Cell. 1994;78:725. [PubMed] [Google Scholar]
- 5.Venkatachalam K, Montell C. TRP channels. Annu Rev Biochem. 2007;76:387–417. doi: 10.1146/annurev.biochem.75.103004.142819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li Y, Corradetti MN, Inoki K, Guan KL. TSC2: Filling the GAP in the mTOR signaling pathway. Trends Biochem Sci. 2004;29:32–38. doi: 10.1016/j.tibs.2003.11.007. [DOI] [PubMed] [Google Scholar]
- 7.Brook-Carter PT, Peral B, Ward CJ, Thompson P, Hughes J, Maheshwar MM, Nellist M, Gamble V, Harris PC, Sampson JR. Deletion of the TSC2 and PKD1 genes associated with severe infantile polycystic kidney disease—A contiguous gene syndrome. Nat Genet. 1994;8:328–332. doi: 10.1038/ng1294-328. [DOI] [PubMed] [Google Scholar]
- 8.Torres VE, Harris PC. Autosomal dominant polycystic kidney disease: The last 3 years. Kidney Int. 2009;76:149–168. doi: 10.1038/ki.2009.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wullschleger S, Loewith R, Hall MN. TOR signaling in growth and metabolism. Cell. 2006;124:471–484. doi: 10.1016/j.cell.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 10.Huang J, Manning BD. The TSC1-TSC2 complex: A molecular switchboard controlling cell growth. Biochem J. 2008;412:179–190. doi: 10.1042/BJ20080281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim DH, Sarbassov DD, Ali SM, King JE, Latek RR, Erdjument-Bromage H, Tempst P, Sabatini DM. mTOR interacts with raptor to form a nutrient-sensitive complex that signals to the cell growth machinery. Cell. 2002;110:163–175. doi: 10.1016/s0092-8674(02)00808-5. [DOI] [PubMed] [Google Scholar]
- 12.Sarbassov DD, Ali SM, Kim DH, Guertin DA, Latek RR, Erdjument-Bromage H, Tempst P, Sabatini DM. Rictor, a novel binding partner of mTOR, defines a rapamycin-insensitive and raptor-independent pathway that regulates the cytoskeleton. Curr Biol. 2004;14:1296–1302. doi: 10.1016/j.cub.2004.06.054. [DOI] [PubMed] [Google Scholar]
- 13.Sarbassov DD, Ali SM, Sengupta S, Sheen JH, Hsu PP, Bagley AF, Markhard AL, Sabatini DM. Prolonged rapamycin treatment inhibits mTORC2 assembly and Akt/PKB. Mol Cell. 2006;22:159–168. doi: 10.1016/j.molcel.2006.03.029. [DOI] [PubMed] [Google Scholar]
- 14.Sarbassov DD, Guertin DA, Ali SM, Sabatini DM. Phosphorylation and regulation of Akt/PKB by the Rictor-mTOR complex. Science. 2005;307:1098–1101. doi: 10.1126/science.1106148. [DOI] [PubMed] [Google Scholar]
- 15.Saucedo LJ, Gao X, Chiarelli DA, Li L, Pan D, Edgar BA. Rheb promotes cell growth as a component of the insulin/TOR signaling network. Nat Cell Biol. 2003;5:566–571. doi: 10.1038/ncb996. [DOI] [PubMed] [Google Scholar]
- 16.Hsu YC, Chern JJ, Cai Y, Liu M, Choi KW. Drosophila TCTP is essential for growth and proliferation through regulation of dRheb GTPase. Nature. 2007;445:785–788. doi: 10.1038/nature05528. [DOI] [PubMed] [Google Scholar]
- 17.Tee AR, Manning BD, Roux PP, Cantley LC, Blenis J. Tuberous sclerosis complex gene products, Tuberin and Hamartin, control mTOR signaling by acting as a GTPase-activating protein complex toward Rheb. Curr Biol. 2003;13:1259–1268. doi: 10.1016/s0960-9822(03)00506-2. [DOI] [PubMed] [Google Scholar]
- 18.Ballif BA, Roux PP, Gerber SA, MacKeigan JP, Blenis J, Gygi SP. Quantitative phosphorylation profiling of the ERK/p90 ribosomal S6 kinase-signaling cassette and its targets, the tuberous sclerosis tumor suppressors. Proc Natl Acad Sci U S A. 2005;102:667–672. doi: 10.1073/pnas.0409143102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Manning BD, Tee AR, Logsdon MN, Blenis J, Cantley LC. Identification of the tuberous sclerosis complex-2 tumor suppressor gene product tuberin as a target of the phosphoinositide 3-kinase/akt pathway. Mol Cell. 2002;10:151–162. doi: 10.1016/s1097-2765(02)00568-3. [DOI] [PubMed] [Google Scholar]
- 20.Roux PP, Ballif BA, Anjum R, Gygi SP, Blenis J. Tumor-promoting phorbol esters and activated Ras inactivate the tuberous sclerosis tumor suppressor complex via p90 ribosomal S6 kinase. Proc Natl Acad Sci U S A. 2004;101:13489–13494. doi: 10.1073/pnas.0405659101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ma L, Chen Z, Erdjument-Bromage H, Tempst P, Pandolfi PP. Phosphorylation and functional inactivation of TSC2 by Erk implications for tuberous sclerosis and cancer pathogenesis. Cell. 2005;121:179–193. doi: 10.1016/j.cell.2005.02.031. [DOI] [PubMed] [Google Scholar]
- 22.Inoki K, Zhu T, Guan KL. TSC2 mediates cellular energy response to control cell growth and survival. Cell. 2003;115:577–590. doi: 10.1016/s0092-8674(03)00929-2. [DOI] [PubMed] [Google Scholar]
- 23.Inoki K, Ouyang H, Zhu T, Lindvall C, Wang Y, Zhang X, Yang Q, Bennett C, Harada Y, Stankunas K, Wang CY, He X, MacDougald OA, You M, Williams BO, Guan KL. TSC2 integrates Wnt and energy signals via a coordinated phosphorylation by AMPK and GSK3 to regulate cell growth. Cell. 2006;126:955–968. doi: 10.1016/j.cell.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 24.Brugarolas J, Lei K, Hurley RL, Manning BD, Reiling JH, Hafen E, Witters LA, Ellisen LW, Kaelin WG., Jr Regulation of mTOR function in response to hypoxia by REDD1 and the TSC1/TSC2 tumor suppressor complex. Genes Dev. 2004;18:2893–2904. doi: 10.1101/gad.1256804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pearson RB, Dennis PB, Han JW, Williamson NA, Kozma SC, Wettenhall RE, Thomas G. The principal target of rapamycin-induced p70s6k inactivation is a novel phosphorylation site within a conserved hydrophobic domain. EMBO J. 1995;14:5279–5287. doi: 10.1002/j.1460-2075.1995.tb00212.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang H, Bajraszewski N, Wu E, Wang H, Moseman AP, Dabora SL, Griffin JD, Kwiatkowski DJ. PDGFRs are critical for PI3K/Akt activation and negatively regulated by mTOR. J Clin Invest. 2007;117:730–738. doi: 10.1172/JCI28984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shah OJ, Wang Z, Hunter T. Inappropriate activation of the TSC/Rheb/mTOR/S6K cassette induces IRS1/2 depletion, insulin resistance, and cell survival deficiencies. Curr Biol. 2004;14:1650–1656. doi: 10.1016/j.cub.2004.08.026. [DOI] [PubMed] [Google Scholar]
- 28.Shah OJ, Hunter T. Turnover of the active fraction of IRS1 involves raptor-mTOR- and S6K1-dependent serine phosphorylation in cell culture models of tuberous sclerosis. Mol Cell Biol. 2006;26:6425–6434. doi: 10.1128/MCB.01254-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Manning BD, Logsdon MN, Lipovsky AI, Abbott D, Kwiatkowski DJ, Cantley LC. Feedback inhibition of Akt signaling limits the growth of tumors lacking Tsc2. Genes Dev. 2005;19:1773–1778. doi: 10.1101/gad.1314605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carracedo A, Ma L, Teruya-Feldstein J, Rojo F, Salmena L, Alimonti A, Egia A, Sasaki AT, Thomas G, Kozma SC, Papa A, Nardella C, Cantley LC, Baselga J, Pandolfi PP. Inhibition of mTORC1 leads to MAPK pathway activation through a PI3K-dependent feedback loop in human cancer. J Clin Invest. 2008;118:3065–3074. doi: 10.1172/JCI34739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Faivre S, Kroemer G, Raymond E. Current development of mTOR inhibitors as anticancer agents. Nat Rev Drug Discov. 2006;5:671–688. doi: 10.1038/nrd2062. [DOI] [PubMed] [Google Scholar]
- 32.Choo AY, Yoon SO, Kim SG, Roux PP, Blenis J. Rapamycin differentially inhibits S6Ks and 4E-BP1 to mediate cell-type-specific repression of mRNA translation. Proc Natl Acad Sci U S A. 2008;105:17414–17419. doi: 10.1073/pnas.0809136105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Serra V, Markman B, Scaltriti M, Eichhorn PJ, Valero V, Guzman M, Botero ML, Llonch E, Atzori F, Di CS, Maira M, Garcia-Echeverria C, Parra JL, Arribas J, Baselga J. NVP-BEZ235, a dual PI3K/mTOR inhibitor, prevents PI3K signaling and inhibits the growth of cancer cells with activating PI3K mutations. Cancer Res. 2008;68:8022–8030. doi: 10.1158/0008-5472.CAN-08-1385. [DOI] [PubMed] [Google Scholar]
- 34.Molhoek KR, Brautigan DL, Slingluff CL., Jr Synergistic inhibition of human melanoma proliferation by combination treatment with B-Raf inhibitor BAY43-9006 and mTOR inhibitor rapamycin. J Transl Med. 2005;3:39. doi: 10.1186/1479-5876-3-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Inoki K, Corradetti MN, Guan KL. Dysregulation of the TSC-mTOR pathway in human disease. Nat Genet. 2005;37:19–24. doi: 10.1038/ng1494. [DOI] [PubMed] [Google Scholar]
- 36.Rosner M, Hanneder M, Siegel N, Valli A, Fuchs C, Hengstschlager M. The mTOR pathway and its role in human genetic diseases. Mutat Res. 2008;659:284–292. doi: 10.1016/j.mrrev.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 37.Rosner M, Hengstschlager M. Cytoplasmic and nuclear distribution of the protein complexes mTORC1 and mTORC2: Rapamycin triggers dephosphorylation and delocalization of the mTORC2 components Rictor and sin1. Hum Mol Genet. 2008;17:2934–2948. doi: 10.1093/hmg/ddn192. [DOI] [PubMed] [Google Scholar]
- 38.Hartman TR, Liu D, Zilfou JT, Robb V, Morrison T, Watnick T, Henske EP. The tuberous sclerosis proteins regulate formation of the primary cilium via a rapamycin-insensitive and polycystin 1-independent pathway. Hum Mol Genet. 2009;18:151–163. doi: 10.1093/hmg/ddn325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Crino PB, Nathanson KL, Henske EP. The tuberous sclerosis complex. N Engl J Med. 2006;355:1345–1356. doi: 10.1056/NEJMra055323. [DOI] [PubMed] [Google Scholar]
- 40.Kwiatkowski DJ, Manning BD. Tuberous sclerosis: A GAP at the crossroads of multiple signaling pathways. Hum Mol Genet. 2005;14:R251–R258. doi: 10.1093/hmg/ddi260. [DOI] [PubMed] [Google Scholar]
- 41.Eng C. PTEN: One gene, many syndromes. Hum Mutat. 2003;22:183–198. doi: 10.1002/humu.10257. [DOI] [PubMed] [Google Scholar]
- 42.Lachlan KL, Lucassen AM, Bunyan D, Temple IK. Cowden syndrome and Bannayan Riley Ruvalcaba syndrome represent one condition with variable expression and age-related penetrance: Results of a clinical study of PTEN mutation carriers. J Med Genet. 2007;44:579–585. doi: 10.1136/jmg.2007.049981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McClatchey AI. Neurofibromatosis. Annu Rev Pathol. 2007;2:191–216. doi: 10.1146/annurev.pathol.2.010506.091940. [DOI] [PubMed] [Google Scholar]
- 44.Corradetti MN, Inoki K, Bardeesy N, DePinho RA, Guan KL. Regulation of the TSC pathway by LKB1: Evidence of a molecular link between tuberous sclerosis complex and Peutz-Jeghers syndrome. Genes Dev. 2004;18:1533–1538. doi: 10.1101/gad.1199104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Baba M, Hong SB, Sharma N, Warren MB, Nickerson ML, Iwamatsu A, Esposito D, Gillette WK, Hopkins RF, III, Hartley JL, Furihata M, Oishi S, Zhen W, Burke TR, Jr, Linehan WM, Schmidt LS, Zbar B. Folliculin encoded by the BHD gene interacts with a binding protein, FNIP1, and AMPK, and is involved in AMPK and mTOR signaling. Proc Natl Acad Sci U S A. 2006;103:15552–15557. doi: 10.1073/pnas.0603781103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Baba M, Furihata M, Hong SB, Tessarollo L, Haines DC, Southon E, Patel V, Igarashi P, Alvord WG, Leighty R, Yao M, Bernardo M, Ileva L, Choyke P, Warren MB, Zbar B, Linehan WM, Schmidt LS. Kidney-targeted Birt-Hogg-Dube gene inactivation in a mouse model: Erk1/2 and Akt-mTOR activation, cell hyperproliferation, and polycystic kidneys. J Natl Cancer Inst. 2008;100:140–154. doi: 10.1093/jnci/djm288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shillingford JM, Murcia NS, Larson CH, Low SH, Hedgepeth R, Brown N, Flask CA, Novick AC, Goldfarb DA, Kramer-Zucker A, Walz G, Piontek KB, Germino GG, Weimbs T. The mTOR pathway is regulated by polycystin-1, and its inhibition reverses renal cystogenesis in polycystic kidney disease. Proc Natl Acad Sci U S A. 2006;103:54665471. doi: 10.1073/pnas.0509694103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bissler JJ, McCormack FX, Young LR, Elwing JM, Chuck G, Leonard JM, Schmithorst VJ, Laor T, Brody AS, Bean J, Salisbury S, Franz DN. Sirolimus for angiomyolipoma in tuberous sclerosis complex or lymphangioleiomyomatosis. N Engl J Med. 2008;358:140–151. doi: 10.1056/NEJMoa063564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Harrington LS, Findlay GM, Gray A, Tolkacheva T, Wigfield S, Rebholz H, Barnett J, Leslie NR, Cheng S, Shepherd PR, Gout I, Downes CP, Lamb RF. The TSC1-2 tumor suppressor controls insulin-PI3K signaling via regulation of IRS proteins. J Cell Biol. 2004;166:213–223. doi: 10.1083/jcb.200403069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.The European Polycystic Kidney Disease Consortium. The polycystic kidney disease 1 gene encodes a 14 kb transcript and lies within a duplicated region on chromosome 16. Cell. 1994;77:881–894. doi: 10.1016/0092-8674(94)90137-6. [DOI] [PubMed] [Google Scholar]
- 51.Sandford R, Sgotto B, Burn T, Brenner S. The tuberin (TSC2), autosomal dominant polycystic kidney disease (PKD1), and somatostatin type V receptor (SSTR5) genes form a synteny group in the Fugu genome. Genomics. 1996;38:84–86. doi: 10.1006/geno.1996.0596. [DOI] [PubMed] [Google Scholar]
- 52.Bonnet CS, Aldred M, von Ruhland C, Harris R, Sandford R, Cheadle JP. Defects in cell polarity underlie TSC and ADPKD-associated cystogenesis. Hum Mol Genet. 2009;18:2166–2176. doi: 10.1093/hmg/ddp149. [DOI] [PubMed] [Google Scholar]
- 53.Fischer DC, Jacoby U, Pape L, Ward CJ, Kuwertz-Broeking E, Renken C, Nizze H, Querfeld U, Rudolph B, Mueller-Wiefel DE, Bergmann C, Haffner D. Activation of the AKT/mTOR pathway in autosomal recessive polycystic kidney disease (ARPKD) Nephrol Dial Transplant. 2009;24:1819–1827. doi: 10.1093/ndt/gfn744. [DOI] [PubMed] [Google Scholar]
- 54.Cook JA, Oliver K, Mueller RF, Sampson J. A cross sectional study of renal involvement in tuberous sclerosis. J Med Genet. 1996;33:480–484. doi: 10.1136/jmg.33.6.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Weimbs T. Polycystic kidney disease and renal injury repair: Common pathways, fluid flow, and the function of polycystin-1. Am J Physiol Renal Physiol. 2007;293:F1423–F1432. doi: 10.1152/ajprenal.00275.2007. [DOI] [PubMed] [Google Scholar]
- 56.Weimbs T. Regulation of mTOR by polycystin-1: Is polycystic kidney disease a case of futile repair? Cell Cycle. 2006;5:2425–2429. doi: 10.4161/cc.5.21.3408. [DOI] [PubMed] [Google Scholar]
- 57.Distefano G, Boca M, Rowe I, Wodarczyk C, Ma L, Piontek KB, Germino GG, Pandolfi PP, Boletta A. Polycystin-1 regulates extracellular signal-regulated kinase-dependent phosphorylation of tuberin to control cell size through mTOR and its downstream effectors S6K and 4EBP1. Mol Cell Biol. 2009;29:2359–2371. doi: 10.1128/MCB.01259-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Govindarajan B, Mizesko MC, Miller MS, Onda H, Nunnelley M, Casper K, Brat D, Cohen C, Arbiser JL. Tuberous sclerosis-associated neoplasms express activated p42/44 mitogen-activated protein (MAP) kinase, and inhibition of MAP kinase signaling results in decreased in vivo tumor growth. Clin Cancer Res. 2003;9:3469–3475. [PubMed] [Google Scholar]
- 59.Yamaguchi T, Wallace DP, Magenheimer BS, Hempson SJ, Grantham JJ, Calvet JP. Calcium restriction allows cAMP activation of the B-Raf/ERK pathway, switching cells to a cAMP-dependent growth-stimulated phenotype. J Biol Chem. 2004;279:40419–40430. doi: 10.1074/jbc.M405079200. [DOI] [PubMed] [Google Scholar]
- 60.Yamaguchi T, Hempson SJ, Reif GA, Hedge AM, Wallace DP. Calcium restores a normal proliferation phenotype in human polycystic kidney disease epithelial cells. J Am Soc Nephrol. 2006;17:178–187. doi: 10.1681/ASN.2005060645. [DOI] [PubMed] [Google Scholar]
- 61.Guan KL, Figueroa C, Brtva TR, Zhu T, Taylor J, Barber TD, Vojtek AB. Negative regulation of the serine/threonine kinase B-Raf by Akt. J Biol Chem. 2000;275:27354–27359. doi: 10.1074/jbc.M004371200. [DOI] [PubMed] [Google Scholar]
- 62.Wahl PR, Le Hir M, Vogetseder A, Arcaro A, Starke A, Waeckerle-Men Y, Serra AL, Wuthrich RP. Mitotic activation of Akt signaling pathway in Han:SPRD rats with polycystic kidney disease. Nephrology (Carlton) 2007;12:357–363. doi: 10.1111/j.1440-1797.2007.00811.x. [DOI] [PubMed] [Google Scholar]
- 63.DiJoseph JF, Sharma RN, Chang JY. The effect of rapamycin on kidney function in the Sprague-Dawley rat. Transplantation. 1992;53:507–513. doi: 10.1097/00007890-199203000-00002. [DOI] [PubMed] [Google Scholar]
- 64.Lieberthal W, Fuhro R, Andry CC, Rennke H, Abernathy VE, Koh JS, Valeri R, Levine JS. Rapamycin impairs recovery from acute renal failure: Role of cell-cycle arrest and apoptosis of tubular cells. Am J Physiol Renal Physiol. 2001;281:F693–F706. doi: 10.1152/ajprenal.2001.281.4.F693. [DOI] [PubMed] [Google Scholar]
- 65.Bonegio RG, Fuhro R, Wang Z, Valeri CR, Andry C, Salant DJ, Lieberthal W. Rapamycin ameliorates proteinuria-associated tubulointerstitial inflammation and fibrosis in experimental membranous nephropathy. J Am Soc Nephrol. 2005;16:2063–2072. doi: 10.1681/ASN.2004030180. [DOI] [PubMed] [Google Scholar]
- 66.Chen JK, Chen J, Neilson EG, Harris RC. Role of mammalian target of rapamycin signaling in compensatory renal hypertrophy. J Am Soc Nephrol. 2005;16:1384–1391. doi: 10.1681/ASN.2004100894. [DOI] [PubMed] [Google Scholar]
- 67.Wu MJ, Wen MC, Chiu YT, Chiou YY, Shu KH, Tang MJ. Rapamycin attenuates unilateral ureteral obstruction-induced renal fibrosis. Kidney Int. 2006;69:2029–2036. doi: 10.1038/sj.ki.5000161. [DOI] [PubMed] [Google Scholar]
- 68.Brown JH, Bihoreau MT, Hoffmann S, Kranzlin B, Tychinskaya I, Obermuller N, Podlich D, Boehn SN, Kaisaki PJ, Megel N, Danoy P, Copley RR, Broxholme J, Witzgall R, Lathrop M, Gretz N, Gauguier D. Missense mutation in sterile alpha motif of novel protein SamCystin is associated with polycystic kidney disease in (Cy/+) rat. J Am Soc Nephrol. 2005;16:3517–3526. doi: 10.1681/ASN.2005060601. [DOI] [PubMed] [Google Scholar]
- 69.Tao Y, Kim J, Schrier RW, Edelstein CL. Rapamycin markedly slows disease progression in a rat model of polycystic kidney disease. J Am Soc Nephrol. 2005;16:46–51. doi: 10.1681/ASN.2004080660. [DOI] [PubMed] [Google Scholar]
- 70.Wahl PR, Serra AL, Le HM, Molle KD, Hall MN, Wuthrich RP. Inhibition of mTOR with sirolimus slows disease progression in Han:SPRD rats with autosomal dominant polycystic kidney disease (ADPKD) Nephrol Dial Transplant. 2006;21:598–604. doi: 10.1093/ndt/gfi181. [DOI] [PubMed] [Google Scholar]
- 71.Zhang T, Wang L, Xiong X, Mao Z, Wang L, Mei C. Mycophenolate mofetil versus rapamycin in Han:SPRD rats with polycystic kidney disease. Biol Res. 2009;42:437–444. [PubMed] [Google Scholar]
- 72.Wu M, Wahl PR, Le HM, Wackerle-Men Y, Wuthrich RP, Serra AL. Everolimus retards cyst growth and preserves kidney function in a rodent model for polycystic kidney disease. Kidney Blood Press Res. 2007;30:253–259. doi: 10.1159/000104818. [DOI] [PubMed] [Google Scholar]
- 73.Zafar I, Belibi FA, He Z, Edelstein CL. Long-term rapamycin therapy in the Han:SPRD rat model of polycystic kidney disease (PKD) Nephrol Dial Transplant. 2009;24:2349–2353. doi: 10.1093/ndt/gfp129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Brown NE, Murcia NS. Delayed cystogenesis and increased ciliogenesis associated with the re-expression of polaris in Tg737 mutant mice. Kidney Int. 2003;63:1220–1229. doi: 10.1046/j.1523-1755.2003.00863.x. [DOI] [PubMed] [Google Scholar]
- 75.Olbrich H, Fliegauf M, Hoefele J, Kispert A, Otto E, Volz A, Wolf MT, Sasmaz G, Trauer U, Reinhardt R, Sudbrak R, Antignac C, Gretz N, Walz G, Schermer B, Benzing T, Hildebrandt F, Omran H. Mutations in a novel gene, NPHP3, cause adolescent nephronophthisis, tapeto-retinal degeneration and hepatic fibrosis. Nat Genet. 2003;34:455–459. doi: 10.1038/ng1216. [DOI] [PubMed] [Google Scholar]
- 76.Gattone VH, Sinders RM, Hornberger TA, Robling AG. Late progression of renal pathology and cyst enlargement is reduced by rapamycin in a mouse model of nephronophthisis. Kidney Int. 2009;76:178–182. doi: 10.1038/ki.2009.147. [DOI] [PubMed] [Google Scholar]
- 77.Reichardt W, Romaker D, Becker A, Buechert M, Walz G, von Elverfeldt D. Monitoring kidney and renal cyst volumes applying MR approaches on a rapamycin treated mouse model of ADPKD. MAGMA. 2009;22:143–149. doi: 10.1007/s10334-008-0158-7. [DOI] [PubMed] [Google Scholar]
- 78.Nickerson ML, Warren MB, Toro JR, Matrosova V, Glenn G, Turner ML, Duray P, Merino M, Choyke P, Pavlovich CP, Sharma N, Walther M, Munroe D, Hill R, Maher E, Greenberg C, Lerman MI, Linehan WM, Zbar B, Schmidt LS. Mutations in a novel gene lead to kidney tumors, lung wall defects, and benign tumors of the hair follicle in patients with the Birt-Hogg-Dubé syndrome. Cancer Cell. 2002;2:157–164. doi: 10.1016/s1535-6108(02)00104-6. [DOI] [PubMed] [Google Scholar]
- 79.Hasumi H, Baba M, Hong SB, Hasumi Y, Huang Y, Yao M, Valera VA, Linehan WM, Schmidt LS. Identification and characterization of a novel folliculin-interacting protein FNIP2. Gene. 2008;415:60–67. doi: 10.1016/j.gene.2008.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Shillingford JM, Piontek KB, Germino GG, Weimbs T. Rapamycin ameliorates PKD resulting from conditional inactivation of pkd1. J Am Soc Nephrol. 2010;21:489–497. doi: 10.1681/ASN.2009040421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Spirli C, Okolicsanyi S, Fiorotto R, Fabris L, Cadamuro M, Lecchi S, Tian X, Somlo S, Strazzabosco M. Mammalian target of rapamycin regulates vascular endothelial growth factor-dependent liver cyst growth in polycystin-2-defective mice. Hepatology. 2009;51:1–11. doi: 10.1002/hep.23511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zeng LH, Xu L, Gutmann DH, Wong M. Rapamycin prevents epilepsy in a mouse model of tuberous sclerosis complex. Ann Neurol. 2008;63:444–453. doi: 10.1002/ana.21331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Qian Q, Du H, King BF, Kumar S, Dean PG, Cosio FG, Torres VE. Sirolimus reduces polycystic liver volume in ADPKD patients. J Am Soc Nephrol. 2008;19:631–638. doi: 10.1681/ASN.2007050626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Vogelbacher R, Wittmann S, Braun A, Daniel C, Hugo C. The mTOR inhibitor everolimus induces proteinuria and renal deterioration in the remnant kidney model in the rat. Transplantation. 2007;84:1492–1499. doi: 10.1097/01.tp.0000282866.92367.99. [DOI] [PubMed] [Google Scholar]
- 85.Sakaguchi M, Isono M, Isshiki K, Sugimoto T, Koya D, Kashiwagi A. Inhibition of mTOR signaling with rapamycin attenuates renal hypertrophy in the early diabetic mice. Biochem Biophys Res Commun. 2006;340:296–301. doi: 10.1016/j.bbrc.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 86.Jain S, Bicknell GR, Whiting PH, Nicholson ML. Rapamycin reduces expression of fibrosis-associated genes in an experimental model of renal ischaemia reperfusion injury. Transplant Proc. 2001;33:556–558. doi: 10.1016/s0041-1345(00)02141-2. [DOI] [PubMed] [Google Scholar]
- 87.Yang B, Jain S, Pawluczyk IZ, Imtiaz S, Bowley L, Ashra SY, Nicholson ML. Inflammation and caspase activation in long-term renal ischemia/reperfusion injury and immunosuppression in rats. Kidney Int. 2005;68:2050–2067. doi: 10.1111/j.1523-1755.2005.00662.x. [DOI] [PubMed] [Google Scholar]
- 88.Yang B, Jain S, Ashra SY, Furness PN, Nicholson ML. Apoptosis and caspase-3 in long-term renal ischemia/reperfusion injury in rats and divergent effects of immunosuppressants. Transplantation. 2006;81:1442–1450. doi: 10.1097/01.tp.0000209412.77312.69. [DOI] [PubMed] [Google Scholar]
- 89.Damiao MJ, Bertocchi AP, Monteiro RM, Goncalves GM, Cenedeze MA, Feitoza CQ, Marques GD, Giannocco G, Mazzali M, Teixeira VP, Dos Reis MA, Pacheco-Silva A, Camara NO. The effects of rapamycin in the progression of renal fibrosis. Transplant Proc. 2007;39:457–459. doi: 10.1016/j.transproceed.2007.01.031. [DOI] [PubMed] [Google Scholar]
- 90.Schaefer L, Tsalastra W, Babelova A, Baliova M, Minnerup J, Sorokin L, Grone HJ, Reinhardt DP, Pfeilschifter J, Iozzo RV, Schaefer RM. Decorin-mediated regulation of fibrillin-1 in the kidney involves the insulin-like growth factor-I receptor and mammalian target of rapamycin. Am J Pathol. 2007;170:301–315. doi: 10.2353/ajpath.2007.060497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lloberas N, Cruzado JM, Franquesa M, Herrero-Fresneda I, Torras J, Alperovich G, Rama I, Vidal A, Grinyo JM. Mammalian target of rapamycin pathway blockade slows progression of diabetic kidney disease in rats. J Am Soc Nephrol. 2006;17:1395–1404. doi: 10.1681/ASN.2005050549. [DOI] [PubMed] [Google Scholar]
- 92.Wittmann S, Daniel C, Stief A, Vogelbacher R, Amann K, Hugo C. Long-term treatment of sirolimus but not cyclosporine ameliorates diabetic nephropathy in the rat. Transplantation. 2009;87:1290–1299. doi: 10.1097/TP.0b013e3181a192bd. [DOI] [PubMed] [Google Scholar]
- 93.Yang Y, Wang J, Qin L, Shou Z, Zhao J, Wang H, Chen Y, Chen J. Rapamycin prevents early steps of the development of diabetic nephropathy in rats. Am J Nephrol. 2007;27:495–502. doi: 10.1159/000106782. [DOI] [PubMed] [Google Scholar]
- 94.Zdychova J, Kazdova L, Pelikanova T, Lindsley JN, Anderson S, Komers R. Renal activity of Akt kinase in obese Zucker rats. Exp Biol Med (Maywood) 2008;233:1231–1241. doi: 10.3181/0801-RM-29. [DOI] [PubMed] [Google Scholar]
- 95.Sataranatarajan K, Mariappan MM, Lee MJ, Feliers D, Choudhury GG, Barnes JL, Kasinath BS. Regulation of elongation phase of mRNA translation in diabetic nephropathy: Amelioration by rapamycin. Am J Pathol. 2007;171:1733–1742. doi: 10.2353/ajpath.2007.070412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Coombes JD, Mreich E, Liddle C, Rangan GK. Rapamycin worsens renal function and intratubular cast formation in protein overload nephropathy. Kidney Int. 2005;68:2599–2607. doi: 10.1111/j.1523-1755.2005.00732.x. [DOI] [PubMed] [Google Scholar]
- 97.Das F, Ghosh-Choudhury N, Mahimainathan L, Venkatesan B, Feliers D, Riley DJ, Kasinath BS, Choudhury GG. Raptor-Rictor axis in TGFβ-induced protein synthesis. Cell Signal. 2008;20:409–423. doi: 10.1016/j.cellsig.2007.10.027. [DOI] [PubMed] [Google Scholar]
- 98.Goncalves GM, Cenedeze MA, Feitoza CQ, de Paula CB, Marques GD, Pinheiro HS, de Paula Antunes Teixeira V, Antônia dos RM, Pacheco-Silva A, Câmara NO. The role of immunosuppressive drugs in aggravating renal ischemia and reperfusion injury. Transplant Proc. 2007;39:417–420. doi: 10.1016/j.transproceed.2007.01.027. [DOI] [PubMed] [Google Scholar]
- 99.Lui SL, Chan KW, Tsang R, Yung S, Lai KN, Chan TM. Effect of rapamycin on renal ischemia-reperfusion injury in mice. Transpl Int. 2006;19:834–839. doi: 10.1111/j.1432-2277.2006.00361.x. [DOI] [PubMed] [Google Scholar]
- 100.Fuller TF, Freise CE, Serkova N, Niemann CU, Olson JL, Feng S. Sirolimus delays recovery of rat kidney transplants after ischemia-reperfusion injury. Transplantation. 2003;76:1594–1599. doi: 10.1097/01.TP.0000095897.38634.30. [DOI] [PubMed] [Google Scholar]
- 101.Lieberthal W, Fuhro R, Andry C, Patel V, Levine JS. Rapamycin delays but does not prevent recovery from acute renal failure: Role of acquired tubular resistance. Transplantation. 2006;82:17–22. doi: 10.1097/01.tp.0000225772.22757.5e. [DOI] [PubMed] [Google Scholar]
- 102.Rangan GK, Coombes JD. Renoprotective effects of sirolimus in non-immune initiated focal segmental glomerulosclerosis. Nephrol Dial Transplant. 2007;22:2175–2182. doi: 10.1093/ndt/gfm191. [DOI] [PubMed] [Google Scholar]
- 103.Lui SL, Tsang R, Chan KW, Zhang F, Tam S, Yung S, Chan TM. Rapamycin attenuates the severity of murine adriamycin nephropathy. Am J Nephrol. 2009;29:342–352. doi: 10.1159/000166599. [DOI] [PubMed] [Google Scholar]
- 104.Daniel C, Ziswiler R, Frey B, Pfister M, Marti HP. Proinflammatory effects in experimental mesangial proliferative glomerulonephritis of the immunosuppressive agent SDZ RAD, a rapamycin derivative. Exp Nephrol. 2000;8:52–62. doi: 10.1159/000020648. [DOI] [PubMed] [Google Scholar]
- 105.Vollenbroker B, George B, Wolfgart M, Saleem MA, Pavenstadt H, Weide T. mTOR regulates expression of slit diaphragm proteins and cytoskeleton structure in podocytes. Am J Physiol Renal Physiol. 2009;296:F418–F426. doi: 10.1152/ajprenal.90319.2008. [DOI] [PubMed] [Google Scholar]
- 106.Letavernier E, Bruneval P, Vandermeersch S, Perez J, Mandet C, Belair MF, Haymann JP, Legendre C, Baud L. Sirolimus interacts with pathways essential for podocyte integrity. Nephrol Dial Transplant. 2009;24:630–638. doi: 10.1093/ndt/gfn574. [DOI] [PubMed] [Google Scholar]
- 107.Naumovic R, Jovovic D, Basta-Jovanovic G, Miloradovic Z, Mihailovic-Stanojevic N, Aleksic T, Jovanovic D. Effects of rapamycin on active Heymann nephritis. Am J Nephrol. 2007;27:379–389. doi: 10.1159/000103918. [DOI] [PubMed] [Google Scholar]
- 108.Daniel C, Renders L, Amann K, Schulze-Lohoff E, Hauser IA, Hugo C. Mechanisms of everolimus-induced glomerulosclerosis after glomerular injury in the rat. Am J Transplant. 2005;5:2849–2861. doi: 10.1111/j.1600-6143.2005.01120.x. [DOI] [PubMed] [Google Scholar]
- 109.Wittmann S, Daniel C, Braun A, Vogelbacher R, Shimizu F, Kawachi H, Hugo C. The mTOR inhibitor everolimus attenuates the time course of chronic anti-Thy1 nephritis in the rat. Nephron Exp Nephrol. 2008;108:e45–e56. doi: 10.1159/000116112. [DOI] [PubMed] [Google Scholar]
- 110.Warner LM, Adams LM, Sehgal SN. Rapamycin prolongs survival and arrests pathophysiologic changes in murine systemic lupus erythematosus. Arthritis Rheum. 1994;37:289–297. doi: 10.1002/art.1780370219. [DOI] [PubMed] [Google Scholar]
- 111.Ramos-Barrón A, Piñera-Haces C, Gómez-Alamillo C, Santiuste-Torcida I, Ruiz JC, Buelta-Carrillo L, Merino R, de Francisco AL, Arias M. Prevention of murine lupus disease in (NZBxNZW)F1 mice by sirolimus treatment. Lupus. 2007;16:775–781. doi: 10.1177/0961203307081401. [DOI] [PubMed] [Google Scholar]
- 112.Hochegger K, Jansky GL, Soleiman A, Wolf AM, Tagwerker A, Seger C, Griesmacher A, Mayer G, Rosenkranz AR. Differential effects of rapamycin in anti-GBM glomerulonephritis. J Am Soc Nephrol. 2008;19:1520–1529. doi: 10.1681/ASN.2007121375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Griffin MD, Torres VE, Grande JP, Kumar R. Vascular expression of polycystin. J Am Soc Nephrol. 1997;8:616–626. doi: 10.1681/ASN.V84616. [DOI] [PubMed] [Google Scholar]
- 114.Torres VE, Cai Y, Chen X, Wu GQ, Geng L, Cleghorn KA, Johnson CM, Somlo S. Vascular expression of polycystin-2. J Am Soc Nephrol. 2001;12:1–9. doi: 10.1681/ASN.V1211. [DOI] [PubMed] [Google Scholar]
- 115.Ibraghimov-Beskrovnaya O, Dackowski WR, Foggensteiner L, Coleman N, Thiru S, Petry LR, Burn TC, Connors TD, Van RT, Bradley J, Qian F, Onuchic LF, Watnick TJ, Piontek K, Hakim RM, Landes GM, Germino GG, Sandford R, Klinger KW. Polycystin: In vitro synthesis, in vivo tissue expression, and subcellular localization identifies a large membrane-associated protein. Proc Natl Acad Sci U S A. 1997;94:6397–6402. doi: 10.1073/pnas.94.12.6397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Qian Q, Li M, Cai Y, Ward CJ, Somlo S, Harris PC, Torres VE. Analysis of the polycystins in aortic vascular smooth muscle cells. J Am Soc Nephrol. 2003;14:2280–2287. doi: 10.1097/01.asn.0000080185.38113.a3. [DOI] [PubMed] [Google Scholar]
- 117.Morel N, Vandenberg G, Ahrabi AK, Caron N, Desjardins F, Balligand JL, Horie S, Devuyst O. PKD1 haploinsufficiency is associated with altered vascular reactivity and abnormal calcium signaling in the mouse aorta. Pflugers Arch. 2009;457:845–856. doi: 10.1007/s00424-008-0561-y. [DOI] [PubMed] [Google Scholar]
- 118.Raichlin E, Bae JH, Khalpey Z, Edwards BS, Kremers WK, Clavell AL, Rodeheffer RJ, Frantz RP, Rihal C, Lerman A, Kushwaha SS. Conversion to sirolimus as primary immunosuppression attenuates the progression of allograft vasculopathy after cardiac transplantation. Circulation. 2007;116:2726–2733. doi: 10.1161/CIRCULATIONAHA.107.692996. [DOI] [PubMed] [Google Scholar]
- 119.Abou Alaiwi WA, Takahashi M, Mell BR, Jones TJ, Ratnam S, Kolb RJ, Nauli SM. Ciliary polycystin-2 is a mechanosensitive calcium channel involved in nitric oxide signaling cascades. Circ Res. 2009;104:860–869. doi: 10.1161/CIRCRESAHA.108.192765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wang D, Iversen J, Wilcox CS, Strandgaard S. Endothelial dysfunction and reduced nitric oxide in resistance arteries in autosomal-dominant polycystic kidney disease. Kidney Int. 2003;64:1381–1388. doi: 10.1046/j.1523-1755.2003.00236.x. [DOI] [PubMed] [Google Scholar]
- 121.Ritter SA, Baehr G. The arterial supply of the congenital polycystic kidney and its relation to the clinical picture. J Urol. 1929;21:583–592. [Google Scholar]
- 122.Chapman AB, Rubinstein D, Hughes R, Stears JC, Earnest MP, Johnson AM, Gabow PA, Kaehny WD. Intracranial aneurysms in autosomal dominant polycystic kidney disease. N Engl J Med. 1992;327:916–920. doi: 10.1056/NEJM199209243271303. [DOI] [PubMed] [Google Scholar]
- 123.Turkmen K, Oflaz H, Uslu B, Cimen AO, Elitok A, Kasikcioglu E, Alisir S, Tufan F, Namli S, Uysal M, Ecder T. Coronary flow velocity reserve and carotid intima media thickness in patients with autosomal dominant polycystic kidney disease: From impaired tubules to impaired carotid and coronary arteries. Clin J Am Soc Nephrol. 2008;3:986–991. doi: 10.2215/CJN.02330607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zeier M, Fehrenbach P, Geberth S, Mohring K, Waldherr R, Ritz E. Renal histology in polycystic kidney disease with incipient and advanced renal failure. Kidney Int. 1992;42:1259–1265. doi: 10.1038/ki.1992.413. [DOI] [PubMed] [Google Scholar]
- 125.Schacht FW. Hypertension in cases of polycystic kidney. Arch Intern Med. 1931;47:500–509. [Google Scholar]
- 126.Ettinger A, Kahn PC, Wise HM., Jr The importance of selective renal angiography in the diagnosis of polycystic disease. J Urol. 1969;102:156–161. doi: 10.1016/s0022-5347(17)62101-3. [DOI] [PubMed] [Google Scholar]
- 127.Wei W, Popov V, Walocha JA, Wen J, Bello-Reuss E. Evidence of angiogenesis and microvascular regression in autosomal-dominant polycystic kidney disease kidneys: A corrosion cast study. Kidney Int. 2006;70:1261–1268. doi: 10.1038/sj.ki.5001725. [DOI] [PubMed] [Google Scholar]
- 128.Bello-Reuss E, Holubec K, Rajaraman S. Angiogenesis in autosomal-dominant polycystic kidney disease. Kidney Int. 2001;60:37–45. doi: 10.1046/j.1523-1755.2001.00768.x. [DOI] [PubMed] [Google Scholar]
- 129.Martinez-Lemus LA, Hill MA, Meininger GA. The plastic nature of the vascular wall: a continuum of remodeling events contributing to control of arteriolar diameter and structure. Physiology (Bethesda) 2009;24:45–57. doi: 10.1152/physiol.00029.2008. [DOI] [PubMed] [Google Scholar]
- 130.Humar R, Kiefer FN, Berns H, Resink TJ, Battegay EJ. Hypoxia enhances vascular cell proliferation and angiogenesis in vitro via rapamycin (mTOR)-dependent signaling. FASEB J. 2002;16:771–780. doi: 10.1096/fj.01-0658com. [DOI] [PubMed] [Google Scholar]
- 131.Tao Y, Kim J, Yin Y, Zafar I, Falk S, He Z, Faubel S, Schrier RW, Edelstein CL. VEGF receptor inhibition slows the progression of polycystic kidney disease. Kidney Int. 2007;72:1358–1366. doi: 10.1038/sj.ki.5002550. [DOI] [PubMed] [Google Scholar]
- 132.Angelo LS, Kurzrock R. Vascular endothelial growth factor and its relationship to inflammatory mediators. Clin Cancer Res. 2007;13:2825–2830. doi: 10.1158/1078-0432.CCR-06-2416. [DOI] [PubMed] [Google Scholar]
- 133.Rzucidlo EM, Martin KA, Powell RJ. Regulation of vascular smooth muscle cell differentiation. J Vasc Surg. 2007;45(Suppl A):A25–A32. doi: 10.1016/j.jvs.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 134.Martin KA, Merenick BL, Ding M, Fetalvero KM, Rzucidlo EM, Kozul CD, Brown DJ, Chiu HY, Shyu M, Drapeau BL, Wagner RJ, Powell RJ. Rapamycin promotes vascular smooth muscle cell differentiation through insulin receptor substrate-1/phosphatidylinositol 3-kinase/Akt2 feedback signaling. J Biol Chem. 2007;282:36112–36120. doi: 10.1074/jbc.M703914200. [DOI] [PubMed] [Google Scholar]
- 135.Jindra PT, Jin YP, Rozengurt E, Reed EF. HLA class I antibody-mediated endothelial cell proliferation via the mTOR pathway. J Immunol. 2008;180:2357–2366. doi: 10.4049/jimmunol.180.4.2357. [DOI] [PubMed] [Google Scholar]
- 136.Mourani PM, Garl PJ, Wenzlau JM, Carpenter TC, Stenmark KR, Weiser-Evans MC. Unique, highly proliferative growth phenotype expressed by embryonic and neointimal smooth muscle cells is driven by constitutive Akt, mTOR, and p70S6K signaling and is actively repressed by PTEN. Circulation. 2004;109:1299–1306. doi: 10.1161/01.CIR.0000118462.22970.BE. [DOI] [PubMed] [Google Scholar]
- 137.Tang Z, Wang Y, Fan Y, Zhu Y, Chien S, Wang N. Suppression of c-Cbl tyrosine phosphorylation inhibits neointimal formation in balloon-injured rat arteries. Circulation. 2008;118:764–772. doi: 10.1161/CIRCULATIONAHA.107.761932. [DOI] [PubMed] [Google Scholar]
- 138.Sousa JE, Costa MA, Abizaid A, Feres F, Seixas AC, Tanajura LF, Mattos LA, Falotico R, Jaeger J, Popma JJ, Serruys PW, Sousa AG. Four-year angiographic and intravascular ultrasound follow-up of patients treated with sirolimuseluting stents. Circulation. 2005;111:2326–2329. doi: 10.1161/01.CIR.0000164271.01172.1A. [DOI] [PubMed] [Google Scholar]
- 139.Sinha SS, Pham MX, Vagelos RH, Perlroth MG, Hunt SA, Lee DP, Valantine HA, Yeung AC, Fearon WF. Effect of rapamycin therapy on coronary artery physiology early after cardiac transplantation. Am Heart J. 2008;155:889.e1–e6. doi: 10.1016/j.ahj.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 140.Barilli A, Visigalli R, Sala R, Gazzola GC, Parolari A, Tremoli E, Bonomini S, Simon A, Closs EI, Dall’Asta V, Bussolati O. In human endothelial cells rapamycin causes mTORC2 inhibition and impairs cell viability and function. Cardiovasc Res. 2008;78:563–571. doi: 10.1093/cvr/cvn024. [DOI] [PubMed] [Google Scholar]
- 141.Dada S, Demartines N, Dormond O. mTORC2 regulates PGE2-mediated endothelial cell survival and migration. Biochem Biophys Res Commun. 2008;372:875–879. doi: 10.1016/j.bbrc.2008.05.154. [DOI] [PubMed] [Google Scholar]
- 142.Li W, Petrimpol M, Molle KD, Hall MN, Battegay EJ, Humar R. Hypoxia-induced endothelial proliferation requires both mTORC1 and mTORC2. Circ Res. 2007;100:79–87. doi: 10.1161/01.RES.0000253094.03023.3f. [DOI] [PubMed] [Google Scholar]
- 143.Xue Q, Nagy JA, Manseau EJ, Phung TL, Dvorak HF, Benjamin LE. Rapamycin inhibition of the Akt/mTOR pathway blocks select stages of VEGF-A164-driven angiogenesis, in part by blocking S6Kinase. Arterioscler Thromb Vasc Biol. 2009;29:1172–1178. doi: 10.1161/ATVBAHA.109.185918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Dormond O, Madsen JC, Briscoe DM. The effects of mTOR-Akt interactions on anti-apoptotic signaling in vascular endothelial cells. J Biol Chem. 2007;282:23679–23686. doi: 10.1074/jbc.M700563200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Fulton D, Gratton JP, McCabe TJ, Fontana J, Fujio Y, Walsh K, Franke TF, Papapetropoulos A, Sessa WC. Regulation of endothelium-derived nitric oxide production by the protein kinase Akt. Nature. 1999;399:597–601. doi: 10.1038/21218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Ackah E, Yu J, Zoellner S, Iwakiri Y, Skurk C, Shibata R, Ouchi N, Easton RM, Galasso G, Birnbaum MJ, Walsh K, Sessa WC. Akt1/protein kinase Balpha is critical for ischemic and VEGF-mediated angiogenesis. J Clin Invest. 2005;115:2119–2127. doi: 10.1172/JCI24726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Bavry AA, Chiu JH, Jefferson BK, Karha J, Bhatt DL, Ellis SG, Whitlow PL. Development of coronary aneurysm after drug-eluting stent implantation. Ann Intern Med. 2007;146:230–232. doi: 10.7326/0003-4819-146-3-200702060-00146. [DOI] [PubMed] [Google Scholar]
- 148.Iakovou I, Schmidt T, Bonizzoni E, Ge L, Sangiorgi GM, Stankovic G, Airoldi F, Chieffo A, Montorfano M, Carlino M, Michev I, Corvaja N, Briguori C, Gerckens U, Grube E, Colombo A. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 2005;293:2126–2130. doi: 10.1001/jama.293.17.2126. [DOI] [PubMed] [Google Scholar]
- 149.Lee SE, John SH, Lim JH, Rhew JY. Very late stent thrombosis associated with multiple stent fractures and peristent aneurysm formation after sirolimus-eluting stent implantation. Circ J. 2008;72:1201–1204. doi: 10.1253/circj.72.1201. [DOI] [PubMed] [Google Scholar]
- 150.Kotani J, Awata M, Nanto S, Uematsu M, Oshima F, Minamiguchi H, Mintz GS, Nagata S. Incomplete neointimal coverage of sirolimus-eluting stents: Angioscopic findings. J Am Coll Cardiol. 2006;47:2108–2111. doi: 10.1016/j.jacc.2005.11.092. [DOI] [PubMed] [Google Scholar]
- 151.Guba M, von Breitenbuch P, Steinbauer M, Koehl G, Flegel S, Hornung M, Bruns CJ, Zuelke C, Farkas S, Anthuber M, Jauch KW, Geissler EK. Rapamycin inhibits primary and metastatic tumor growth by antiangiogenesis: Involvement of vascular endothelial growth factor. Nat Med. 2002;8:128–135. doi: 10.1038/nm0202-128. [DOI] [PubMed] [Google Scholar]
- 152.Fujishita T, Aoki K, Lane HA, Aoki M, Taketo MM. Inhibition of the mTORC1 pathway suppresses intestinal polyp formation and reduces mortality in ApcDelta716 mice. Proc Natl Acad Sci U S A. 2008;105:13544–13549. doi: 10.1073/pnas.0800041105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Amura CR, Brodsky KS, Groff R, Gattone VH, Voelkel NF, Doctor RB. VEGF receptor inhibition blocks liver cyst growth in pkd2(WS25/−) mice. Am J Physiol Cell Physiol. 2007;293:C419–C428. doi: 10.1152/ajpcell.00038.2007. [DOI] [PubMed] [Google Scholar]
- 154.Grath-Morrow S, Cho C, Molls R, Burne-Taney M, Haas M, Hicklin DJ, Tuder R, Rabb H. VEGF receptor 2 blockade leads to renal cyst formation in mice. Kidney Int. 2006;69:1741–1748. doi: 10.1038/sj.ki.5000314. [DOI] [PubMed] [Google Scholar]
- 155.Kang DH, Hughes J, Mazzali M, Schreiner GF, Johnson RJ. Impaired angiogenesis in the remnant kidney model: II. Vascular endothelial growth factor administration reduces renal fibrosis and stabilizes renal function. J Am Soc Nephrol. 2001;12:1448–1457. doi: 10.1681/ASN.V1271448. [DOI] [PubMed] [Google Scholar]
- 156.Kang DH, Johnson RJ. Vascular endothelial growth factor: A new player in the pathogenesis of renal fibrosis. Curr Opin Nephrol Hypertens. 2003;12:43–49. doi: 10.1097/00041552-200301000-00008. [DOI] [PubMed] [Google Scholar]
- 157.Fine LG, Norman JT. Chronic hypoxia as a mechanism of progression of chronic kidney diseases: From hypothesis to novel therapeutics. Kidney Int. 2008;74:867–872. doi: 10.1038/ki.2008.350. [DOI] [PubMed] [Google Scholar]
- 158.Reis F, Parada B, Teixeira de Lemos, Garrido P, Dias A, Piloto N, Baptista S, Sereno J, Eufrásio P, Costa E, Rocha-Pereira P, Santos-Silva A, Figueiredo A, Mota A, Teixeira F. Hypertension induced by immunosuppressive drugs: A comparative analysis between sirolimus and cyclosporine. Transplant Proc. 2009;41:868–873. doi: 10.1016/j.transproceed.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 159.Gurevich F, Perazella MA. Renal effects of anti-angiogenesis therapy: Update for the internist. Am J Med. 2009;122:322–328. doi: 10.1016/j.amjmed.2008.11.025. [DOI] [PubMed] [Google Scholar]
- 160.Augustine JJ, Bodziak KA, Hricik DE. Use of sirolimus in solid organ transplantation. Drugs. 2007;67:369–391. doi: 10.2165/00003495-200767030-00004. [DOI] [PubMed] [Google Scholar]
- 161.Dunn C, Croom KF. Everolimus: A review of its use in renal and cardiac transplantation. Drugs. 2006;66:547–570. doi: 10.2165/00003495-200666040-00009. [DOI] [PubMed] [Google Scholar]
- 162.Flechner SM. Sirolimus in kidney transplantation indications and practical guidelines: De novo sirolimus-based therapy without calcineurin inhibitors. Transplantation. 2009;87(Suppl 8):S1–S6. doi: 10.1097/TP.0b013e3181a059a1. [DOI] [PubMed] [Google Scholar]
- 163.Ekberg H, Tedesco-Silva H, Demirbas A, Vitko S, Nashan B, Gurkan A, Margreiter R, Hugo C, Grinyo JM, Frei U, Vanrenterghem Y, Daloze P, Halloran PF. Reduced exposure to calcineurin inhibitors in renal transplantation. N Engl J Med. 2007;357:2562–2575. doi: 10.1056/NEJMoa067411. [DOI] [PubMed] [Google Scholar]
- 164.Larson TS, Dean PG, Stegall MD, Griffin MD, Textor SC, Schwab TR, Gloor JM, Cosio FG, Lund WJ, Kremers WK, Nyberg SL, Ishitani MB, Prieto M, Velosa JA. Complete avoidance of calcineurin inhibitors in renal transplantation: A randomized trial comparing sirolimus and tacrolimus. Am J Transplant. 2006;6:514–522. doi: 10.1111/j.1600-6143.2005.01177.x. [DOI] [PubMed] [Google Scholar]
- 165.Kasiske BL, de Mattos A, Flechner SM, Gallon L, Meier-Kriesche HU, Weir MR, Wilkinson A. Mammalian target of rapamycin inhibitor dyslipidemia in kidney transplant recipients. Am J Transplant. 2008;8:1384–1392. doi: 10.1111/j.1600-6143.2008.02272.x. [DOI] [PubMed] [Google Scholar]
- 166.Hoogeveen RC, Ballantyne CM, Pownall HJ, Opekun AR, Hachey DL, Jaffe JS, Oppermann S, Kahan BD, Morrisett JD. Effect of sirolimus on the metabolism of apoB100-containing lipoproteins in renal transplant patients. Transplantation. 2001;72:1244–1250. doi: 10.1097/00007890-200110150-00011. [DOI] [PubMed] [Google Scholar]
- 167.Mueller MA, Beutner F, Teupser D, Ceglarek U, Thiery J. Prevention of atherosclerosis by the mTOR inhibitor everolimus in LDLR−/− mice despite severe hypercholesterolemia. Atherosclerosis. 2008;198:39–48. doi: 10.1016/j.atherosclerosis.2007.09.019. [DOI] [PubMed] [Google Scholar]
- 168.Blum CB. Effects of sirolimus on lipids in renal allograft recipients: An analysis using the Framingham risk model. Am J Transplant. 2002;2:551–559. doi: 10.1034/j.1600-6143.2002.20610.x. [DOI] [PubMed] [Google Scholar]
- 169.Chueh S-C, Kahan BD. Dyslipidemia in renal transplant recipients treated with a sirolimus and cyclosporine-based immunosuppressive regimen: Incidence, risk factors, progression, and prognosis. Transplantation. 2003;76:375–382. doi: 10.1097/01.TP.0000074310.40484.94. [DOI] [PubMed] [Google Scholar]
- 170.Mulay AV, Cockfield S, Stryker R, Fergusson D, Knoll GA. Conversion from calcineurin inhibitors to sirolimus for chronic renal allograft dysfunction: A systematic review of the evidence. Transplantation. 2006;82:1153–1162. doi: 10.1097/01.tp.0000237101.58974.43. [DOI] [PubMed] [Google Scholar]
- 171.Wali RK, Weir MR. Chronic allograft dysfunction: Can we use mammalian target of rapamycin inhibitors to replace calcineurin inhibitors to preserve graft function? Curr Opin Organ Transplant. 2008;13:614–621. doi: 10.1097/MOT.0b013e3283193bad. [DOI] [PubMed] [Google Scholar]
- 172.Schena FP, Pascoe MD, Alberu J, del Carmen Rial M, Oberbauer R, Brennan DC, Campistol JM, Racusen L, Polinsky MS, Goldberg-Alberts R, Li H, Scarola J, Neylan JF, for the Sirolimus CONVERT Trial Study Group Conversion from calcineurin inhibitors to sirolimus maintenance therapy in renal allograft recipients: 24-month efficacy and safety results from the CONVERT trial. Transplantation. 2009;87:233–242. doi: 10.1097/TP.0b013e3181927a41. [DOI] [PubMed] [Google Scholar]
- 173.Ruiz JC, Campistol JM, Sanchez-Fructuoso A, Rivera C, Oliver J, Ramos D, Campos B, Arias M, Diekmann F. Increase of proteinuria after conversion from calcineurin inhibitor to sirolimus-based treatment in kidney transplant patients with chronic allograft dysfunction. Nephrol Dial Transplant. 2006;21:3252–3257. doi: 10.1093/ndt/gfl447. [DOI] [PubMed] [Google Scholar]
- 174.Aliabadi D, Kammerstatter G, Seebacher G, Rodler S, Wolner E, Grimm M, Pohanka E, Zuckermann A. Development of proteinuria after switch to sirolimus based immunosuppression in long term cardiac transplant patients. Am J Transplant. 2008;8:854–861. doi: 10.1111/j.1600-6143.2007.02142.x. [DOI] [PubMed] [Google Scholar]
- 175.Stephany BR, Boumitri M, Budev M, Alao B, Poggio ED. Absence of proteinuria predicts improvement in renal function after conversion to sirolimus-based immunosuppressive regimens in lung transplant survivors with chronic kidney disease. J Heart Lung Transplant. 2009;28:564–571. doi: 10.1016/j.healun.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 176.Mreich E, Coombes JD, Rangan GK. Sirolimus does not reduce receptor-mediated endocytosis of albumin in proximal tubule cells. Transplantation. 2007;83:105–107. doi: 10.1097/01.tp.0000240055.49572.07. [DOI] [PubMed] [Google Scholar]
- 177.Letavernier E, Pe’raldi M-N, Pariente A, Morelon E, Legendre C. Proteinuria following a switch from calcineurin inhibitors to sirolimus. Transplantation. 2005;80:1198–1203. doi: 10.1097/01.tp.0000185200.17589.74. [DOI] [PubMed] [Google Scholar]
- 178.Letavernier E, Legendre C. mToR inhibitors-induced proteinuria: Mechanisms, significance, and management. Transplant Rev (Orlando) 2008;22:125–130. doi: 10.1016/j.trre.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 179.van den Akker JM, Wetzels JF, Hoitsma AJ. Proteinuria following conversion from azathioprine to sirolimus in renal transplant recipients. Kidney Int. 2006;70:1355–1357. doi: 10.1038/sj.ki.5001792. [DOI] [PubMed] [Google Scholar]
- 180.Lebranchu Y, Etienne I, Topance O, Westeel PF, Legendre C, de Ligny BH, Le Meur Y, Moulin B, Touchard G, Deteix P, Villemain F, Le Pogamp P, Noel C, Idier I. Preliminary results of a randomized trial comparing sirolimus (SRL) vs cyclosporine (CsA) in 150 transplant recipients receiving a cadaveric renal graft. Transplantation. 2004;78:463. [Google Scholar]
- 181.Stephany BR, Augustine JJ, Krishnamurthi V, Goldfarb DA, Flechner SM, Braun WE, Hricik DE, Dennis VW, Poggio ED. Differences in proteinuria and graft function in de novo sirolimus-based vs. calcineurin inhibitor-based immunosuppression in live donor kidney transplantation. Transplantation. 2006;82:368–374. doi: 10.1097/01.tp.0000228921.43200.f7. [DOI] [PubMed] [Google Scholar]
- 182.Buchler M, Caillard S, Barbier S, Thervet E, Toupance O, Mazouz H, Hurault de Ligny B, Le Meur Y, Thierry A, Villemain F, Heng AE, Moulin B, Morin MP, Noel C, Lebranchu Y. Sirolimus versus cyclosporine in kidney recipients receiving thymoglobulin, mycophenolate mofetil and a 6-month course of steroids. Am J Transplant. 2007;7:2522–2531. doi: 10.1111/j.1600-6143.2007.01976.x. [DOI] [PubMed] [Google Scholar]
- 183.Diekmann F, Gutierrez-Dalmau A, Lopez S, Cofan F, Esforzado N, Ricart MJ, Rossich E, Saval N, Torregrosa JV, Oppenheimer F, Campistol JM. Influence of sirolimus on proteinuria in de novo kidney transplantation with expanded criteria donors: Comparison of two CNI-free protocols. Nephrol Dial Transplant. 2007;22:2316–2321. doi: 10.1093/ndt/gfm181. [DOI] [PubMed] [Google Scholar]
- 184.Neau-Cransac M, Moreau K, Deminiere C, Merville P, Saric J. Decrease in sirolimus-induced proteinuria after switch to everolimus in a liver transplant recipient with diabetic nephropathy. Transpl Int. 2009;22:586–587. doi: 10.1111/j.1432-2277.2008.00811.x. [DOI] [PubMed] [Google Scholar]
- 185.Letavernier E, Bruneval P, Mandet C, Van Huyen JP, Peraldi MN, Helal I, Noel LH, Legendre C. High sirolimus levels may induce focal segmental glomerulosclerosis de novo. Clin J Am Soc Nephrol. 2007;2:326–333. doi: 10.2215/CJN.03751106. [DOI] [PubMed] [Google Scholar]
- 186.Fervenza FC, Fitzpatrick PM, Mertz J, Erickson SB, Liggett S, Popham S, Wochos DN, Synhavsky A, Hippler S, Larson TS, Bagniewski SM, Velosa JA. Acute rapamycin nephrotoxicity in native kidneys of patients with chronic glomerulopathies. Nephrol Dial Transplant. 2004;19:1288–1292. doi: 10.1093/ndt/gfh079. [DOI] [PubMed] [Google Scholar]
- 187.Rangan GK. Sirolimus-associated proteinuria and renal dysfunction. Drug Saf. 2006;29:1153–1161. doi: 10.2165/00002018-200629120-00006. [DOI] [PubMed] [Google Scholar]
- 188.Tumlin JA, Miller D, Near M, Selvaraj S, Hennigar R, Guasch A. A prospective, open-label trial of sirolimus in the treatment of focal segmental glomerulosclerosis. Clin J Am Soc Nephrol. 2006;1:109–116. doi: 10.2215/CJN.00120605. [DOI] [PubMed] [Google Scholar]
- 189.Senior PA, Paty BW, Cockfield SM, Ryan EA, Shapiro AM. Proteinuria developing after clinical islet transplantation resolves with sirolimus withdrawal and increased tacrolimus dosing. Am J Transplant. 2005;5:2318–2323. doi: 10.1111/j.1600-6143.2005.01013.x. [DOI] [PubMed] [Google Scholar]
- 190.Chapman AB, Johnson AM, Gabow PA, Schrier RW. Overt proteinuria and microalbuminuria in autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 1994;5:1349–1354. doi: 10.1681/ASN.V561349. [DOI] [PubMed] [Google Scholar]
- 191.Sharp C, Johnson A, Gabow P. Factors relating to urinary protein excretion in children with autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 1998;9:1908–1914. doi: 10.1681/ASN.V9101908. [DOI] [PubMed] [Google Scholar]
- 192.Torres VE. Hypertension, proteinuria, and progression of autosomal dominant polycystic kidney disease: Where do we go from here? Am J Kidney Dis. 2000;35:547–550. doi: 10.1016/s0272-6386(00)70213-7. [DOI] [PubMed] [Google Scholar]
- 193.Serra AL, Kistler AD, Poster D, Krauer F, Senn O, Raina S, Pavik I, Rentsch K, Regeniter A, Weishaupt D, Wüthrich RP. Safety and tolerability of sirolimus treatment in patients with autosomal dominant polycystic kidney disease. Nephrol Dial Transplant. 2009;24:3334–3342. doi: 10.1093/ndt/gfp280. [DOI] [PubMed] [Google Scholar]
- 194.Grantham JJ, Torres VE, Chapman AB, Guay-Woodford LM, Bae KT, King BF, Jr, Wetzel LH, Baumgarten DA, Kenney PJ, Harris PC, Klahr S, Bennett WM, Hirschman GN, Meyers CM, Zhang X, Zhu F, Miller JP. Volume progression in polycystic kidney disease. N Engl J Med. 2006;354:2122–2130. doi: 10.1056/NEJMoa054341. [DOI] [PubMed] [Google Scholar]
- 195.Kistler AD, Poster D, Krauer F, Weishaupt D, Raina S, Senn O, Binet I, Spanaus K, Wuthrich RP, Serra AL. Increases in kidney volume in autosomal dominant polycystic kidney disease can be detected within 6 months. Kidney Int. 2009;75:235–241. doi: 10.1038/ki.2008.558. [DOI] [PubMed] [Google Scholar]
- 196.Franz KA, Reubi FC. Rate of functional deterioration in polycystic kidney disease. Kidney Int. 1983;23:526–529. doi: 10.1038/ki.1983.51. [DOI] [PubMed] [Google Scholar]
- 197.Banikazemi M, Bultas J, Waldek S, Wilcox WR, Whitley CB, McDonald M, Finkel R, Packman S, Bichet DG, Warnock DG, Desnick RJ. Agalsidase-beta therapy for advanced Fabry disease: A randomized trial. Ann Intern Med. 2007;146:77–86. doi: 10.7326/0003-4819-146-2-200701160-00148. [DOI] [PubMed] [Google Scholar]
- 198.Serra AL, Kistler AD, Poster D, Struker M, Wuthrich RP, Weishaupt D, Tschirch F. Clinical proof-of-concept trial to assess the therapeutic effect of sirolimus in patients with autosomal dominant polycystic kidney disease: SUISSE ADPKD study. BMC Nephrol. 2007;8:13. doi: 10.1186/1471-2369-8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Walz G. Therapeutic approaches in autosomal dominant polycystic kidney disease (ADPKD): Is there light at the end of the tunnel? Nephrol Dial Transplant. 2006;21:1752–1757. doi: 10.1093/ndt/gfl246. [DOI] [PubMed] [Google Scholar]
- 200.Soliman AR, Ismail E, Zamil S, Lotfy A. Sirolimus therapy for patients with adult polycystic kidney disease: A pilot study. Transplant Proc. 2009;41:3639–3641. doi: 10.1016/j.transproceed.2009.05.032. [DOI] [PubMed] [Google Scholar]
- 201.Stallone G, Infante B, Grandaliano G, Gesualdo L. Management of side effects of sirolimus therapy. Transplantation. 2009;87(Suppl 8):S23–S26. doi: 10.1097/TP.0b013e3181a05b7a. [DOI] [PubMed] [Google Scholar]
- 202.Sirolimus (Rapamune®) for autosomal dominant polycystic kidney disease (ADPKD) Bethesda, MD: National Institutes of Health; 2008. Available online at http://clinicaltrials.gov/ct2/show/NCT00346918. Accessed December 17, 2008. [Google Scholar]
- 203.Sirolimus treatment in patients with autosomal dominant polycystic kidney disease: Renal efficacy and safety (SIRENA) Bethesda, MD: National Institutes of Health; 2007. Available online at http://clinicaltrials.gov/ct2/show/NCT00491517. Accessed December 18, 2009. [Google Scholar]
- 204.Pilot study of rapamycin as treatment for autosomal dominant polycystic kidney disease (ADPKD) Bethesda, MD: National Institutes of Health; 2006. Available online at http://clinicaltrials.gov/ct2/show/NCT00286156. Accessed November 18, 2009. [Google Scholar]
- 205.Efficacy, safety and tolerability of everolimus in preventing end-stage renal disease in patients with autosomal dominant polycystic kidney disease. Bethesda, MD: National Institutes of Health; 2008. Available online at http://clinicaltrials.gov/ct2/show/NCT00414440?term=NCT00414440. Accessed November 18, 2009. [Google Scholar]


