Abstract
Background
In older age health needs and demand for health services utilization increase. Individual’s social relationships can play a decisive role regarding the utilization of outpatient health care services. This systematic review examines the associations of structural and functional dimensions of social relationships with outpatient health services use of older adults.
Methods
The databases PubMed, CINAHL, SocINDEX, PsycINFO, International Bibliography of the Social Sciences (IBSS), Sociological Abstracts, and Applied Social Sciences Index and Abstracts (ASSIA) were searched in February 2016. The methodological and reporting quality of the articles was assessed and the results were synthesized descriptively and systematically.
Results
Out of 1.392 hits, 36 articles (35 studies) were included in the systematic review. The methodological and reporting quality of the included articles was reasonable. Various structural and functional characteristics of social relationships were associated with the use (yes/no) and the frequency of using outpatient care among older adults. The majority of the associations between structural dimensions of social relationships and the use of physicians were positive and moderate in strength. The associations between functional dimensions of social relationships and the probability of using physician services were inconsistent and varied in strength. For the most part, social relationship variables assigned to the structural dimension were positively and weakly to moderately associated with the frequency of physician visits. Functional aspects of social relationships also tended to have positive associations with the frequency of physician utilization. The associations were weak to moderate in strength.
Conclusions
Measuring social relationships and their influence on health services use is a challenging methodological endeavor indicated by the inconclusive results. The results suggest that the outpatient care utilization behavior of older individuals being structurally and functionally integrated in social relationships is different to older adults being socially isolated or having no social support. All in all, the current status of quantitative data was insufficient. Future health services research should accentuate social ties in more detail, especially according to quality aspects of social relationships.
Background
Rapidly ageing populations generate increasing health needs and chronic conditions in Western industrial countries associated with a rising demand for health services [1]. Compared with younger cohorts, individuals within their fifties or older show more chronic illnesses and increased rates of health care use [2]. Utilization of health services is influenced by a variety of factors, e.g. predisposing, enabling and need characteristics [3]. These are constantly changing over the life course. Due to chronic conditions and physical limitations in older age need factors can expand, while levels of autonomy, mobility and social participation decrease [4]. The use of health services is embedded into a complex structure of social networks and interactions. Social relationships can be an enabling determinant of whether or not elderly individuals do consult health care services [5, 6]. Consequently, the question if social relationships buffer or foster the use of medical care has been raised within health services research [7–13]. Social relationships may be an opportunity to enable the use of health services, especially for vulnerable groups. Moreover, they can be used to support or substitute formal health services, and by that, release restricted resources in health care systems.
Following Berkman, Glass [14] social ties have an effect on individuals by providing social support, social influence, social engagement and attachment, and accessing resources and material goods. Beyond that, international studies have shown that social relationships have a substantial impact on morbidity and mortality [15–18]. In general, social relationships can be divided into structural and functional elements [15]. The degree of social network integration, a more quantitative measure, represents the structural dimension of social relationships (e.g. living arrangements, social network size, and frequency of social participation). The functional perspective is captured by received and perceived social support, and includes aspects of financial, instrumental, informational or emotional support. Through preventive care-seeking, acquisition of knowledge about potential treatments, and post-treatment recovery and rehabilitation, health service utilization behavior can be considered a health-protective action influenced by structural and functional aspects of social relationships [7]. A principal element in most health care systems is presented by outpatient health services, including primary and secondary care. Although, the first contact to health care is realized routinely through primary care services (e.g. in the US and UK), the close linkage to specialists and ambulatory health services is a ubiquitous characteristic within health care systems. By taking into account the political and scientific debate of shifting health care services from inpatient to outpatient settings, outpatient health services will be of growing importance in the future.
To date, no systematic review on this topic has been conducted. Therefore, the first aim of this systematic review was to provide an overview of studies dealing with outpatient care utilization among older adults associated with various dimensions of social relationships. The second aim was to evaluate magnitude and consistency of the associations between social ties and health services use.
Method
A systematic review on studies dealing with social relationships and the utilization of outpatient care physicians among older adults was conducted. The performance of this review was based on the PRISMA checklist [19] and a study protocol including all preliminary specifications published on PROSPERO, registration number CRD42016036004 (S1 File, S1 Table).
Search strategy and inclusion criteria
After developing the research question and performing a pilot run of literature search, seven databases were used (February 11th 2016). The databases PubMed, CINAHL, SocINDEX, PsycINFO, International Bibliography of the Social Sciences, Sociological Abstracts, and Applied Social Sciences Index and Abstracts were searched for the keywords and various synonyms “social relationships”, “utilization”, “outpatient care” and “aged” in title and abstract (S1 Text). MeSH-terms and limiters were adapted to each electronic database. In addition, references of relevant articles were searched for further matching studies.
At first, one reviewer (DB) screened the titles and abstracts of all articles identified by electronic and reference search. In a second step, two independent reviewers (DB and LI) applied a predefined set of inclusion criteria on all relevant articles by performing a full text screening. In case of disagreement between the reviewers, a third investigator (OK) was consulted and the study was discussed until consensus was accomplished.
Within the full text screening, articles had to pass five predefined inclusion criteria. Firstly, records were controlled for the criterion “peer-reviewed journal articles in German or English”. Peer-reviewed journal articles represent good scientific practice to secure quality, to foster objectivity and to provide transparency. Due to language skills and a reasonable use of resources of the reviewers, German and English articles were screened. Secondly, records were checked for three different study designs: quantitative observational 1) cross-sectional, 2) case-control and 3) cohort studies. Thirdly, full texts were inspected for the criterion “community-dwelling or noninstitutionalized individuals fifty years and older”. The rationale behind this population was to extract a reference group still active on the labor market, and to expand the number of potentially relevant studies. Compared with younger cohorts, individuals within their fifties or older show more chronic illnesses and increased rates of health care use [2]. The fourth inclusion criterion was the accounting for utilization or frequency of use of outpatient care services as the dependent or outcome variable. These measures of use are solidly established in health services research and increase the chance of comparability. Finally, studies had to include and analyze social relationship variables. To gather information on the full spectrum of social relationships including structural and functional aspects this broad term was implemented.
Data extraction and quality assessment
The data was extracted using a standardized form including information about the author, year, country, research design, study year (follow-up if applicable), sample size, response rate, age, gender, outcome, social relationship variables, and confounders in the fully adjusted model.
The quality assessment, including the methodological and reporting quality, was based on a checklist following the Newcastle-Ottawa-Scale [20] and its adaptation of Herzog, Alvarez-Pasquin [21]. The checklist included the three sections “selection”, “comparability and confounders” and “outcome”. It consisted of ten (cohort studies) respectively eight items (cross-sectional studies) which could be answered by “yes”, “no” or “unclear”. Instead of reporting a sum score, a global rating was preferred [22]. The quality of cross-sectional studies which met three or less criteria were ranked as “low”, four or five as “medium” and six or more as “high”. Cohort studies with four or less fulfilled criteria were rated as “low” quality, five to seven as “medium” and eight or more as “high”.
Analysis strategy
The results were descriptively and systematically synthesized. All associations between social relationships and utilization of physicians were extracted and categorized. Each social relationship variable was assigned to a social relationship category and dimension. For a better overview, closely related indicators were aggregated within categories (e.g., marital status or social support). Moreover, social relationship variables were classified as “structural” or “functional” [15]. The functional dimension was split into “received support” and “provided support”. To answer our two research questions, we looked comprehensively at all associations between social relationships and physician use. For the sake of clarity and presentation, we focused on the statistically significant associations in our following tables (p<0.05). Due to the heterogeneity of the included studies a meta-analysis was not performed. Instead, we decided to complement our descriptive analysis by assessing the quality of the studies and by presenting a full description of the relevant quantitative data to maximize transparency and to enable rating the certainty of the results [23]. Since use (yes/no) and frequency of practitioner visits show a distinct level of information and have different meanings, the results are reported separately.
Results
Literature search
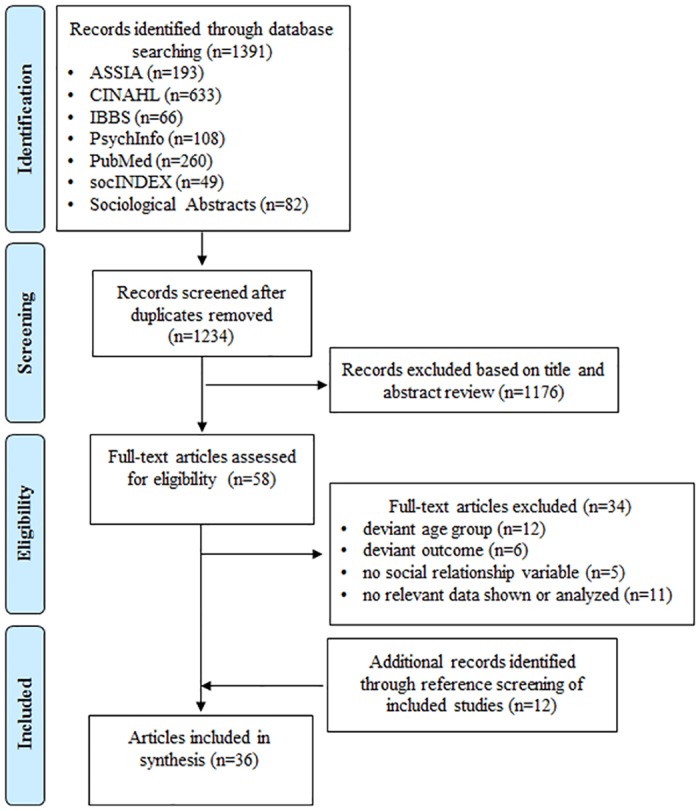
A total of 1,392 publications were identified through database search. After removing 158 duplications, 1,234 articles remained for title and abstract screening (Fig 1). 1,176 publications were excluded based on title and abstract screening. Fifty-eight full-text articles were assessed for eligibility (S3 Table). Thirty-four were eliminated due to various reasons (deviant age group, deviant outcome, no social variable, none relevant data shown or analyzed). Twelve records were identified through reference search of included articles. In the full text screening inter-rater agreement on study inclusion was 88%. In the end, thirty-six publications based on thirty-five studies were included in the review and the synthesis. Though two articles [8, 24] were based on the same study, their methodological and reporting quality was evaluated separately and their results were analyzed independently due to differing samples and data sets.
Fig 1. Flow chart of systematic literature search.
Overview of included records
The articles were published between 1981 and 2015 (Table 1). More than half of the records were from the USA (20; 55.6%). Eight articles were from Europe (22.2%), five from Asia (13.9%), two from Canada (5.6%) and one from Australia (2.8%). The sample sizes ranged from N = 40 to N = 824,952 and mean age ranged from 63 to 81 years. Two studies focused on women only [10, 25], the others had quota of women of 45% to 66%. Twenty-two studies were cross-sectional and fourteen were prospective cohort studies. Twenty-three studies analyzed the frequency of physician visits (ordinal, metric or count variables). Nine studies researched the use of physicians (yes vs. no). Four articles [12, 26–28] reported both outcomes and therefore, they were listed in the “use” and “frequency” section. The period of outpatient care use ranged from fifteen days to two years. More than half of the articles focused explicitly on GP visits [26, 29–34], primary care [35–38], ambulatory services [8, 24, 39–42], and outpatient physician visits [7, 43, 44]. The other records used more implicit terms like “physicians” [45], “doctors” [46] and “consultations” [34] in contrast to inpatient health care services (e.g. hospital days, hospital nights).
Table 1. Overview of characteristics of included studies.
| Author(s), year, country | Research design (specific population) | Study year (follow-up) | Sample size | Response rate in % | Age | Female in % | Covariates in fully adjusted model |
|---|---|---|---|---|---|---|---|
| Arling, 1985, USA [8] | cross-sectional study | 1979 | 2,051 | 87 | 60–64: 29% 65–74: 47% 75–84: 19% 85+: 5% | 59 | medical conditions, ADL impairment, psychosomatic symptoms, emotional symptoms, economic deprivation, insurance coverage, medical care source, age, education, sex, race |
| Branch et al., 1981, USA [42] | cross-sectional study | 1974 | 1,625 | 79 | 73.2 (mean) | 60 | age, gender, race, education, income, occupation, health insurance, regular physician, transportation problems, perceived health status, activities of daily living, physical activity performance, ability to climb stairs, ability to walk half a mile, health problem |
| Cafferata, 1987, USA [48] | cross-sectional study | 1977 | 4,560 | n.a. | 73.5 (mean) | 60 | race, education, chronic condition, health insurance, density of physicians, health, worry, physicians usual source of care, bed-disability days |
| Coulton & Frost, 1982, USA [41] | cohort study | 1975 (1976) | 1,834 (1,519) | n.a. | 74.2 (mean) | 65 | perceived service need, level of impairment, income, education, insurance, case management, gender, age, race, psychic stress |
| Counte & Glandon, 1991, USA [28] | cohort study (health maintenance organization members and fee-for-service clients) | 1986 (+6 months) | 402 | 74 & 44 (87 & 85) | 72.5 (mean) | 63 | health status, life stress, insurance, SES, gender |
| Crespo-Cebada & Urbanos-Garrido, 2012, Spain [26] | cross-sectional study | 2006/07 | 1,860 | n.a. | n.a. | n.a. | age, gender, longillness, symptoms, chronic diseases, limitations, depression, orientation, health, physical activity, education, job status, insurance, income, homecare |
| Dalsgaard et al., 2012, Denmark [29] | cohort study (diabetes cohort) | 2003 (2009) | 824,952 | n.a. | 55–64: 33.4% 65–79: 40.6% | 45 | sex, age, education, occupation, income |
| Eve, 1988, USA [25] | cohort study (older women cohort) | 1969 (1979) | 3,013 (1,849) | 62.9 (61.4) | 70.4 (mean) | 100 | age, education, race, head of household, retirement status, income, satisfied with way of living, able to get along on income, health insurance, metropolitan area, handicapped/disabled, health compared to others, previous use of health services |
| Ezeamama et al., 2015, USA [46] | cross-sectional study | 2010/11 | 4,562 | 80 | 50–55: 22.36% 56–60: 25.71% 61–65: 24.38% 66–70: 27.55% | 57.8 | history of loss, age, sex, education, smoking, BMI, physical activity level, US-born, fall, trouble sleeping, race, cumulative lifetime adversity, global mastery, domain-specific mastery, importance of religion, comorbidities, retirement status |
| Foreman et al., 1998, China [9] | cross-sectional study | 1998 | 350 | n.a. | 71.6 (mean) | 51.4 | gender, age, education, alcohol |
| Fritel et al., 2014, France [10] | cohort study (urinary incontinence cohort, women only) | 2000 (2008) | 2,640 (2,273) | n.a. (86) | 63 (mean) | 100 | age, parity, urinary incontinence (UI) severity at baseline, UI type, quality of life, consultation with GP in the last 12 months, neurologic disease, hypertension or cardiovascular disease |
| Gobbens & van Assen, 2012, The Netherlands [30] | cohort study | 2008 (2009, 2010) | 245 (179, 141) | 53 (73, 58) | 80.3 (mean) | 54.7 | sex, age, lifestyle, multimorbidity, physical frailty, psychological frailty, social frailty, BMI, activities, fatigue, mobility, balance, hand grip strength, depression, anxiety, coping, mental state |
| Goldsteen et al., 1992, USA [43] | cohort study | 1986 (+6 months) | 402 (346) | 59.6 (86.1) | 72.5 (mean) | 63 | age, sex, race, education, religion, health locus control, physician visits t0, desirable life events, activities, health problems, HMO, Eldercare |
| Hand et al., 2014, Canada [35] | cross-sectional study (frequent health services user) | n.a. | 40 | 44.9 | 81.3 (mean) | 55 | health status |
| Harris et al., 2004, UK [34] | cohort study | 2000 (2001) | 1,565 | 75 (92) | 65–69: 24% 70–74: 25% 75–79: 22% 80–84: 15% 85+: 14% | 62 | age, sex, practice, general health, disease score, anxiety score |
| Jordan et al., 2006, UK [31] | cohort study (knee pain cohort) | 2000 (-/+18 months) | 1,797 | 77 (100) | n.a. | n.a. | knee-related factors, general health, sex, age, education |
| Korten & Jacomb, 1998, Australia [32] | cohort study | 1990/91 (1994) | 897 (624) | 65 (85) | 76.4 (mean) | n.a. | number of current illnesses, level of pain |
| Krause, 1988, USA [11] | cohort study (stress cohort) | 1984 (+18 months) | 351 (265) | n.a. (75.5) | n.a. | n.a. | age, sex, education, physical health status |
| Levkoff et al., 1987, USA [47] | cohort study (middle-aged and aged cohorts) | n.a. | 152 | 88 (n.a.) | n.a. | n.a. | gender, education, has preventive outlook, thinks appropriate to talk to doctor about personal problems |
| Li & Chi, 2011, China [12] | cross-sectional study | 2000 | 20,255 | 98.6 | 69.1 (mean) | 47 | age, gender, education, place of residence, income, health insurance, convenience of visiting a physician, self-rated health, functional health |
| Liao et al., 2012, Taiwan [44] | cohort study (introduction of national health insurance cohort) | 1993 (1996) | 2,230 (1,504) | 90 (67.4) | 69.7–71.1 (means) | 35–62 | age, gender, education, employment status, lifestyle behaviors, ethnicity, health/chronic conditions |
| Miltiades & Wu, 2008, China & USA [49] | cross-sectional study (chinese immigrants) | 2000–03 | 597 | 88,5 & 91 | 69.7–71.8 (means) | 62.1 & 59.3 | education, traditional chinese medicine, self-rated health, depression (CES-D), chronic conditions, income, insurance, residence |
| Park, 2012, South Korea [38] | cross-sectional study | 2003 | 6,591 | 94.1 | n.a. | n.a. | age, gender, education, religion, self-perceived health status, cognitive condition, income, health insurance |
| Pourat et al., 2000, USA [39] | cross-sectional study (korean immigrants) | 1993 | 424 | n.a. | 73–75 (means) | 60 & 65 | demographics, health, functioning, income, insurance, perceptions of health/other beliefs |
| Rennemark et al., 2009, Sweden [37] | cross-sectional study (frequent health services user) | 2001–03 | 643 | 72.8 | 66 (mean) | 54.2 | age, gender, functional ability, comorbidity, education, sense of coherence, internal locus of control |
| Ryvicker et al., 2012, USA [36] | cross-sectional study | 2008 | 1,260 | 76.7 | 75.4 (mean) | 65 | supply quartile, neighborhood safety, use public transit, age, female, nonwhite, non-English speaking, education, health insurance, usual source of care, number of chronic conditions, number of ADL/IADL needs |
| Schafer, 2013, USA [7] | cross-sectional study | 2005/06 | 3,005 | 75.5 & 84 | 69.3 (mean) | 52 | sex, age, education, ethnicity, self-rated health, disease, regular place for health care, health insurance, alternative medicine |
| Schmitz et al., 1997, USA [6] | cohort study | n.a. | 226 | 55 (n.a.) | n.a. | n.a. | daily hassles, age, depression, physical health, number of health problems |
| Stoller, 1982, USA [27] | cross-sectional study | 1979 | 753 | 71 | 73.2 (mean) | 57 | symptoms, cancer effects, heart disease effects, stroke effects, worry about health, health interferes, ill in bed, health insurance, finances tight, care at MD's office, availability inconvenient, MD/population ratio, health attitudes, education, rural/urban, age, sex |
| Strain, 1990, Canada [13] | cross-sectional study | 1985 | 705 | 75 | 71 (mean) | 59 | perceived health, number of chronic conditions, functional disability, health beliefs, age, gender, education, occupation, ethnic identity, religion, income |
| Suominen-Taipale et al., 2004, Norway & Finland [33] | cross-sectional study | 1995–97 | 9,202 | 71 & 86 | 65–69: 49–57% 70–74: 43–51% | 53 & 33 | sex, age, self-rated health, education, region |
| Wan & Arling, 1983, USA [24] | cross-sectional study (functionally impaired, subsample Arling 1985) | 1979 | 772 | n.a. | 72.6 (mean) | 62.2 | age, sex, race, residential background, occupation, education, income, health insurance, regular physician, perceived service needs having been met, transportation barriers, ADL, IADL, health disorders, Mental Status Questionnaire, psychological symptoms, perceived health |
| Wan & Odell, 1981, USA [40] | cross-sectional study | 1978 | 1,182 | n.a. | 55–75: 75% 75+: 25% | 60 | sex, age, education, retired, economic dependency, ADL, IADL, depression, perceived need for service, transportation barriers, knowledge of service, health insurance coverage |
| Wolinsky & Coe, 1984, USA [45] | cross-sectional study | 1978 | 1,5899 | n.a. | 69.9 (mean) | 57 | sex, age, race, education, retired, labor force, regular source of care, telephone, income, health insurance, region, metropolitan area, limited activity, overall health, BMI |
| Wolinsky & Johnson, 1991, USA [50] | cross-sectional study | 1984 | 5,151 | n.a. | 78 (mean) | 63.2 | age, female, race, telephone, education, health worries and control, healt insurance, residentially stable, population density, social security dependent, perceived health, ADL, body limitations |
| Wolinsky et al., 1983, USA [51] | cross-sectional study | 1980 | 401 | n.a. | 74.2 (mean) | 66 | perceived health, mental orientation, ADL, IADL, sensory functions, nutritional risk, mental health, income, supplemental insurance, preventive care (MD, dentist), locus of control, sex, race, age, index of social position, nutritional knowledge |
The methodological and reporting quality of 47.2% of the records was categorized as “high”, 44.4% as “medium” and 8.3% as “low” (Table 2). Apart from criterion two (non-respondents and response rate) and criterion seven (independent assessment of outcome), the majority of the articles met the criteria of methodological and reporting quality (Table 2, S1 Fig, S2 Table). Criterion two (non-respondents and response rate) was met only by five articles [6, 12, 13, 27, 37] and criterion seven (independent assessment of outcome) by eight records [6, 29, 31, 34, 35, 37, 41, 47].
Table 2. Results of the quality assessment of the included records (+ = yes, - = no, 0 = unclear).
| Author, year | 1. repre-sentative-ness of the sample | 2. non-respon-dents & response rate | 3. sample size | 4. ascer-tainment of expo-sure | 5. validated or described instrument for exposure | 6. compara-bility and confounders | 7. indepen-dent assess-ment of outcome | 8. follow-up long enough for outcome to occur (only cohort) | 9. adequacy of follow up (only cohort) | 10. statis-tical test | Global assessment of methodological and reporting quality |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Arling, 1985 [8] | + | 0 | + | + | + | + | - | - | medium | ||
| Branch et al., 1981 [42] | + | 0 | + | + | + | + | - | + | high | ||
| Cafferata, 1987 [48] | + | 0 | + | + | + | + | - | - | medium | ||
| Coulton & Frost, 1982 [41] | + | 0 | + | + | - | + | + | + | - | + | medium |
| Counte & Glandon, 1991 [28] | 0 | 0 | + | + | + | + | - | + | - | + | medium |
| Crespo-Cebada & Urbanos-Garrido, 2012 [26] | + | 0 | + | + | + | + | - | + | high | ||
| Dalsgaard et al., 2012 [29] | + | n.a. | + | + | + | - | + | + | + | + | high |
| Eve, 1988 [25] | + | - | + | + | + | + | - | + | - | + | medium |
| Ezeamama et al., 2015 [46] | + | 0 | + | + | + | + | - | + | high | ||
| Foreman et al., 1998 [9] | - | 0 | + | + | + | + | - | + | medium | ||
| Fritel et al., 2014 [10] | 0 | - | + | + | + | + | - | + | + | + | medium |
| Gobbens & van Assen, 2012 [30] | + | - | + | + | + | + | - | + | + | + | high |
| Goldsteen et al., 1992 [43] | + | - | + | + | + | + | - | + | + | + | high |
| Hand et al., 2014 [35] | - | 0 | - | + | + | - | + | - | low | ||
| Harris et al., 2004 [34] | + | - | + | + | 0 | + | + | + | + | + | high |
| Jordan et al., 2006 [31] | + | 0 | + | + | + | + | + | + | - | - | medium |
| Korten & Jacomb, 1998 [32] | 0 | 0 | + | + | + | - | - | + | - | - | low |
| Krause, 1988 [11] | + | 0 | + | + | + | + | - | + | + | - | medium |
| Levkoff et al., 1987 [47] | + | - | - | + | + | - | + | + | - | - | medium |
| Li & Chi, 2011 [12] | + | + | + | + | + | + | - | + | high | ||
| Liao et al., 2012 [44] | + | - | + | + | + | + | - | + | + | + | high |
| Miltiades & Wu, 2008 [49] | - | - | + | + | + | + | - | + | medium | ||
| Park, 2012 [38] | 0 | - | + | + | - | + | - | - | low | ||
| Pourat et al., 2000 [39] | 0 | 0 | + | + | + | + | - | + | medium | ||
| Rennemark et al., 2009 [37] | + | + | + | + | + | + | + | + | high | ||
| Ryvicker et al., 2012 [36] | + | - | + | + | + | + | - | + | high | ||
| Schafer, 2013 [7] | + | 0 | + | + | + | + | - | + | high | ||
| Schmitz et al., 1997 [6] | - | + | + | + | + | + | + | + | + | - | high |
| Stoller, 1982 [27] | + | + | + | + | + | + | - | + | high | ||
| Strain, 1990 [13] | + | + | + | + | + | + | - | + | high | ||
| Suominen-Taipale et al., 2004 [33] | + | - | + | + | + | - | - | + | medium | ||
| Wan & Arling, 1983 [24] | 0 | 0 | + | + | + | + | - | + | medium | ||
| Wan & Odell, 1981 [40] | + | - | + | 0 | + | + | 0 | + | medium | ||
| Wolinsky & Coe, 1984 [45] | + | 0 | + | + | + | + | - | + | high | ||
| Wolinsky & Johnson, 1991 [50] | + | 0 | + | + | + | + | - | - | medium | ||
| Wolinsky et al., 1983 [51] | + | 0 | + | + | + | + | - | + | high |
Associations between social relationships and physician utilization (yes vs. no)
Fourty associations between social relationships and the use of physicians were found in thirteen articles (S4 Table). In seven articles, fourteen associations were statistically significant (Table 3). In other words, two thirds of the associations were statistically insignificant.
Table 3. Statistically significant associations between social relationship (SR) indicators and physician use (yes/no).
| No. | SR dimension | SR category | SR indicator | Author, Year | Statistics | SR coeff. (95%CI, p) |
|---|---|---|---|---|---|---|
| 1. | Structural | Marital status—single | Single (0 = married/cohabiting, 1 = single) | Suominen-Taipale et al., 2004 [33] | Odds Ratio | 0.6 (0.5–0.8, p<0.05) |
| 2. | Marital status—widowed | Widow (0 = married/cohabiting, 1 = widow) | Suominen-Taipale et al., 2004 [33] | Odds Ratio | 0.9 (0.7–1.0, p<0.05) | |
| 3. | Marital status—divorced/separated | Divorced/separated (0 = married/cohabiting, 1 = divorced/separated) | Suominen-Taipale et al., 2004 [33] | Odds Ratio | 0.7 (0.6–1.0, p<0.05) | |
| 4. | Living with others | Living with at least one child (0 = no, 1 = yes) | Li and Chi, 2011 [12] | Odds Ratio | 1.38 (1.03–1.84, p<0.05) | |
| 5. | Social network size | Social network members (0 = none, 1 = one or more) | Park, 2012 [38] | Odds Ratio | 1.28 (n.r., p<0.05) | |
| 6. | Household size | Liao et al., 2012 [44] | Random-effect probit model | -0.011 (n.r., p<0.05) | ||
| 7. | Social cohesion | Neighborhood social cohesion score (range: 5–20) | Ryvicker et al., 2012 [36] | Odds Ratio | 1.04 (1.00–1.09, p<0.05) | |
| 8. | Functional | Social support (unspecified) | Nonkin supports scale (five items) | Wolinsky and Johnson, 1991 [50] | Unst. OLS coeff. | 0.017 (n.r., p<0.05) |
| 9. | Kin supports scale (two items) | Wolinsky and Johnson, 1991 [50] | Unst. OLS coeff. | 0.034 (n.r., p<0.05) | ||
| 10. | Social support scale (0 = strong, 1 = weak) | Fritel et al., 2014 [10] | Odds Ratio | 1.4 (1.0–2.0, p<0.05) | ||
| 11. | Financial support | Receiving financial support (0 = no, 1 = yes) | Li and Chi, 2011 [12] | Odds Ratio | 0.47 (0.34–0.65, p<0.001) | |
| 12. | Health discussions with others | Discuss health with friends or close relatives (0 = no, 1 = yes) | Fritel et al., 2014 [10] | Odds Ratio | 1.5 (1.0–2.1, p<0.05) | |
| 13. | Providing financial support | Providing financial support (0 = no, 1 = yes) | Li and Chi, 2011 [12] | Odds Ratio | 0.49 (0.33–0.73, p<0.001) | |
| 14. | Providing instrumental support | Providing instrumental support (0 = no, 1 = yes) | Li and Chi, 2011 [12] | Odds Ratio | 0.73 (0.54–0.99, p<0.01) |
SR = social relationship; CI = confidence interval; p = p-value; n.r. = not reported; coeff. = coefficient; Unst. = unstandardized; OLS = ordinary least squares
Seven out of these fourteen associations included variables of the structural dimension of social ties [12, 33, 36, 38, 44]. Suominen-Taipale, Koskinen [33] found consistent and relatively strong negative associations between being single, widowed, divorced or separated and the probability of physician utilization compared to older adults who are married and cohabiting. Li and Chi [12] reported a strong positive association between living with at least one child and the physician use. Regarding the social network size, Park [38] observed a moderate positive association between having social network members and the use of physicians, while Liao, Chang [44] found a weak negative association between the household size and the probability of visiting a physician.
Seven out of fourteen associations included variables of the functional dimension of social relationships [10, 12, 50]. Wolinsky and Johnson [50] found consistently positive, but weak associations between nonkin or kin social support and physician consultations. Fritel, Panjo [10] showed a higher probability of using outpatient care doctors for older people with weak social support. Otherwise, discussing health with friends or close relatives was associated strongly and positively with using health services [10]. Li and Chi [12] analyzed specific forms of social support in their study. For older people receiving or providing financial support or providing instrumental support they observed consistent and strong negative links to the utilization of physicians [12].
Associations between social relationships and frequency of physician utilization
Ninety-two associations between social relationships and the frequency of physician use were found in twenty-eight articles (S5 Table). In seventeen articles, thirty-seven associations were statistically significant (Table 4). Consequently, more than half of the associations were statistically insignificant.
Table 4. Statistically significant associations between social relationship (SR) indicators and frequency of physician visits.
| No. | SR dimension | SR category | SR indicator | Author, Year | Statistics | SR coeff. (95%CI, p) |
|---|---|---|---|---|---|---|
| 1. | Structural | Marital status—married | Married (0 = not married, 1 = married) | Foreman et al., 1998 [9] | Weighted OLS coeff. | 20.454 (n.r., p<0.05) |
| 2. | Married (0 = no, 1 = yes) | Wolinsky and Coe, 1984 [45] | Unst. OLS coeff. | 0.091 (n.r., p<0.001) | ||
| 3. | Married (0 = otherwise, 1 = married) | Miltiades and Wu, 2008 [49] | St. OLS coeff. | 0.160 (n.r., p<0.01) | ||
| 4. | Marital status—widowed | Widowed (0 = no, 1 = yes) | Wolinsky and Coe, 1984 [45] | Unst. OLS coeff. | 0.069 (n.r., p<0.01) | |
| 5. | Living alone | Alone (0 = otherwise, 1 = lives alone) | Crespo-Cebada and Urbanos-Garrido, 2012 [26] | Count model (elasticity) | 0.0149 (n.r., p<0.1) | |
| 6. | Lives alone (0 = lives with spouse, 1 = lives alone) | Stoller, 1982 [27] | Unst. OLS coeff. | 0.07 (n.r., p<0.1) | ||
| 7. | Single (0 = cohabiting, 1 = single) | Dalsgaard et al., 2012 [29] | Rates; absolute difference | 0.4 (0.2–0.5, p<0.05) | ||
| 8. | lives alone (0 = no, 1 = yes) | Wolinsky and Coe, 1984 [45] | Unst. OLS coeff. | 0.128 (n.r., p<0.001) | ||
| 9. | Single (0 = cohabiting, 1 = single) | Dalsgaard et al., 2012 [29] | Rates; absolute difference | -0.5 (-0.7–-0.3, p<0.05) | ||
| 10. | Single (0 = cohabiting, 1 = single) | Dalsgaard et al., 2012 [29] | Rates; absolute difference | 0.0 (-0.2–0.2, p<0.05) | ||
| 11. | Single (0 = cohabiting, 1 = single) | Dalsgaard et al., 2012 [29] | Rates; absolute difference | 0.0 (-0.2–0.2, p<0.05) | ||
| 12. | Living with others | Living with children (0 = not living with children, 1 = living with children) | Foreman et al., 1998 [9] | Weighted OLS coeff. | 14.533 (n.r., p<0.05) | |
| 13. | living with at least one child (0 = no, 1 = yes) | Li and Chi, 2011 [12] | Count model coeff. | -0.06 (-0.1–-0.01, p<0.01) | ||
| 14. | lives with others (0 = lives with spouse, 1 = lives with others) | Stoller, 1982 [27] | Unst. OLS coeff. | -0.08 (n.r., p<0.05) | ||
| 15. | Living arrangement (1 = lives with others except spouse) | Cafferata, 1987 [48] | Unst. OLS coeff. | -0.9 (n.r., p<0.05) | ||
| 16. | Frequency of social interaction | Telephone contact with friends or relatives (0 = monthly or less, 1 = weekly) | Harris et al., 2004 [34] | Ordered logistic coeff. | 1.7 (1.3–2.3, p<0.001) | |
| 17. | Telephone contact with friends or relatives (0 = monthly or less, 1 = daily) | Harris et al., 2004 [34] | Ordered logistic coeff. | 1.8 (1.4–2.5, p<0.001) | ||
| 18. | Social network (two items on contact frequency, score range 1–12) | Miltiades and Wu, 2008 [49] | St. OLS coeff. | 0.219 (n.r., p<0.01) | ||
| 19. | Social network size | Social support: network (extent of subject's social network) | Korten and Jacomb, 1998 [32] | St. OLS coeff., Odds Ratio | 2.682, 14.6 (2.72–78.39, p<0.05) | |
| 20. | Social network (unspecified) | Lubben Social Network Scale: friend (revised) | Pourat et al., 2000 [39] | Exponential Betas | 1.11 (n.r., p<0.05) | |
| 21. | Lubben Social Network Scale: neighbor (revised) | Pourat et al., 2000 [39] | Exponential Betas | 0.93 (n.r., p<0.05) | ||
| 22. | Social isolation | social isolation (index of social contacts, high score = almost no contact) | Coulton and Frost, 1982 [41] | St. OLS coeff. | -0.6 (n.r., p<0.05) | |
| 23. | Functional | Social support (unspecified) | Reliable alliance social provision | Schmitz et al., 1997 [6] | St. OLS coeff. | 0.13 (n.r., p<0.05) |
| 24. | Social support (10 forms of assistance) | Arling, 1985 [8] | St. OLS coeff. | 0.14 (n.r., p<0.001) | ||
| 25. | Emotional support | filial piety (1 = not filial—4 = very filial) | Li and Chi, 2011 [12] | Count model coeff. | -0.05 (-0.08–-0.02, p<0.001) | |
| 26. | Financial support | receiving financial support (0 = no, 1 = yes) | Li and Chi, 2011 [12] | Count model coeff. | 0.05 (0.01–0.10, p<0.01) | |
| 27. | Instrumental support | Tangible support | Krause, 1988 [11] | St. OLS coeff. | 0.184 (n.r., p<0.01) | |
| 28. | Informational support | Informational support | Krause, 1988 [11] | St. OLS coeff. | 0.144 (n.r., p<0.05) | |
| 29. | Social ties & health discussions | Partner tie—very likely to discuss health (0 = no, 1 = yes) | Schafer, 2013 [7] | Unst. OLS coeff. | 1.49 (n.r., p<0.01) | |
| 30. | Partner tie—less likely to discuss health (0 = no, 1 = yes) | Schafer, 2013 [7] | Unst. OLS coeff. | 1.27 (n.r., p<0.05) | ||
| 31. | Child ties—very likely to discuss health (0 = no, 1 = yes) | Schafer, 2013 [7] | Unst. OLS coeff. | 0.34 (n.r., p<0.05) | ||
| 32. | Non-kin ties—very likely to discuss health (0 = no, 1 = yes) | Schafer, 2013 [7] | Unst. OLS coeff. | 0.37 (n.r., p<0.05) | ||
| 33. | Non-kin ties—less likely to discuss health (0 = no, 1 = yes) | Schafer, 2013 [7] | Unst. OLS coeff. | 0.27 (n.r., p<0.05) | ||
| 34. | Harmony of social interaction | Relationships with family are harmonious (0 = no, 1 = yes) | Foreman et al., 1998 [9] | Weighted OLS coeff. | -19.538 (n.r., p<0.01) | |
| 35. | Respect in social interaction | Receive as much respect from family as deserved (0 = some, little or very little respect, 1 = very much) | Pourat et al., 2000 [39] | Exponential Betas | 1.38 (n.r., p<0.05) | |
| 36. | Providing instrumental support | providing instrumental support (0 = no, 1 = yes) | Li and Chi, 2011 [12] | Count model coeff. | -0.07 (-0.12–-0.01, p<0.01) | |
| 37. | Providing financial support | Providing financial support (0 = no, 1 = yes) | Li and Chi, 2011 [12] | Count model coeff. | 0.10 (0.04–0.15, p<0.001) |
SR = social relationship; CI = confidence interval; p = p-value; n.r. = not reported; coeff. = coefficient; St. = standardized; Unst. = unstandardized; OLS = ordinary least squares
Twenty-two out of these thirty-seven associations included variables of the structural dimension of social ties. Three studies found positive associations between being married and the frequency of physician visits [9, 45, 49] and one article reported a positive association between being widowed and the frequency of physician consultations [45]. Furthermore, living alone was positively and weakly associated with a higher frequency of using outpatient health services in three records [26, 27, 45]. Dalsgaard, Vedsted [29] found no, positive and negative differences for older adults who are living alone depending on their age and gender. Living with others (e.g., child or others except spouse) was associated negatively with the frequency of utilizing physicians in three studies [12, 27, 48]. Foreman, Yu [9] reported a strong and positive association between living with children and the frequency of health services use. The size of the social network was positively and strongly associated with a higher frequency of physician visits [32]. Counting friends or neighbors amongst their social networks, older adults reported a higher number of physician consultations [39]. Coulton and Frost [41] found out that socially isolated older people showed a lower number of physician contacts than socially integrated older adults. Moreover, Harris, Cook [34] and Militades and Wu [49] observed positive associations between higher contact frequencies in social networks and the frequency of physician use.
Fifteen out of thirty-seven associations included variables of the functional dimension of social relationships. Two studies showed positive and weak associations between received social support and the frequency of physician utilization [6, 8]. Financial, instrumental or informational support was associated weakly with more physician visits [11, 12]. Emotional support was associated with less consultations [12]. Schafer [7] reported moderate to strong and positive associations between the likelihood of discussing health and the frequency of physician use taking several social ties into consideration (partner, children, non-kin). Harmonious social relationships decreased the frequency of physician visits [9] and respectful social ties increased the use rate [39].
Li and Chi [12] investigated the association between providing social support and the frequency of using physicians. Providing instrumental support was associated negatively and weakly. The provision of financial support was linked positively and weakly.
Discussion
Summary of findings
This review provides a comprehensive overview and furthers the understanding of the association between social relationships and health services use among older adults (50 years and older). The first objective of this study was to systematically review social relationships associated with the utilization of outpatient care services of older people. The second aim was to evaluate magnitude and consistency of the associations between social ties and health services use.
We included thirty-six records on thirty-five different studies reporting structural and functional dimensions of social relationships linked to the utilization of health services into our analyses. In most cases empirical evidence was insufficient and for several of the social tie variables inconsistent results were found. Taking into account the fully adjusted model, associations between use measures and social relationship variables were for the most part weak and statistically insignificant. Potentially, associations were underestimated by that strict criterion.
Overall, most of the studies focused on associations between social ties and frequency of physician use. The structural dimension of social relationships and its association with physician visits (use and frequency of use) was investigated far more often than the functional dimension. Though a substantial number of social relationship dimensions were explored until now, none of the included studies included a holistic approach of social tie measures (degree of integration, received and perceived social support) [15] and theirs links to health services utilization.
The majority of the associations between structural dimensions of social relationships and the use of physicians were positive and moderate in strength. The associations between functional dimensions of social relationships and the probability of using physician services were inconsistent and varied in strength. For the most part, social relationship variables assigned to the structural dimension were positively and weakly to moderately associated with the frequency of physician visits. Functional aspects of social relationships also tended to have positive associations with the frequency of physician utilization. The associations were weak or moderate in strength. All in all, the current status of quantitative data was insufficient to draw precise and generalizable conclusions.
Our review reveals that the link between various social relationship indicators and health care use as well as frequency of use have been investigated in few studies. This clearly indicates that further research is needed.
Limitations
Including a broad range of seven medical and sociological databases, we were able to minimize the risk of missing relevant articles. Nevertheless, the risk of publication bias is still existent. More than half of the studies (64%) were performed in North America, and therefore, findings cannot be generalized. Since the majority of included studies (61%) had cross-sectional design, conclusions concerning causal relations are not possible.
Due to the fact that ten studies did not (four studies) or did not clearly meet (six studies) the quality criterion of representativeness and thirty articles did not (twelve studies) or did not clearly report (eighteen studies) information on non-respondents and response rate, the results were moderately robust. Overall, the methodological and reporting quality of the studies was mostly categorized as medium or high (92%).
Most of the studies referred to one year of physician use. Still, the range of the utilization variable was substantial between the studies (from 15 days to two years). As the time span was quite long in some studies, and considering the older age of the interviewed individuals, risk of memory bias was existent, particularly, if the information on consultations was not compared to medical records (twenty-seven studies).
Since there were no consistent measures of predictors (social relationships) and outcome variables (use and frequency of outpatient care visits), data was analyzed systematically, but descriptively. A prerequisite of meta-analyses is a high level of accordance across the included studies regarding independent and dependent variable measures and data analysis approaches [52]. Due to the heterogeneity of the included studies (e.g. study designs, sampling procedures, data collection methods, definition of outcome and exposure variables, confounders, quality of studies, statistical analysis and reporting) a meta-analysis was not conducted. In most cases the associations were small and statistically not significant. The current status of evidence is insufficient and partly inconsistent.
Unfortunately, analyses of group-differences concerning age, gender, and chronic conditions could not conducted on the basis of the review material.
Conclusions
Social relationships can increase or decrease the probability to consult a physician, and they can influence the frequency of visits. All in all, older people who are structurally integrated by social relationships are more likely to consult a physician at all and to contact a physician more often. Functional aspects of social relationships, depending on the form of social support, can increase or decrease the probability of physician use. Older adults who are experiencing social support tend to have a higher rate of physician visits than older people without any or less support.
On the one hand, this could be read as good news, since structural and functional aspects of social relationships tend to enable the utilization of health services, and thereby potentially foster older adults’ health. Social relationships could offer informational, instrumental and emotional resources with regard to health, health care services and treatments. On the other hand, considering increasing numbers of single-person-households and an increasing risk of loneliness and social isolation in older age [53], this could be interpreted as a cause of concern, since older individuals who are not socially integrated may not find their way to health care services. The results do not include information about the adequacy of health care regarding access to health services, extent of health treatment, and quality of health care.
Social ties have an impact on the patient’s motives for a consultation and on the patient’s compliance regarding future visits for treatment, prevention or rehabilitation [54, 55]. Consequently, health care practitioners should consider information on patient’s social environments into their clinical routine. By default, physicians should assess social networks among the elderly screening for social resources or social needs of support. Furthermore, relevant stakeholders (e.g., physicians, public health institutions and health insurance companies) need to find ways to ensure that older adults can use outpatient care services regardless of their structural and functional level of social integration.
The variety of dimensions of social relationships presented in this review illustrates that utilization of outpatient health care services is a complex social process. Besides methodological challenges, the complex picture of social tie’s impact on health care utilization bases on the fact that relationships are not always of positive virtue [56, 57]. In contrary, “some of the most powerful impacts on health [and health services use] that social relationships may have, are through acts of abuse, violence, and trauma” [14]. This fact may represent a possible explanation for the inconsistent pattern of social relationships on health services use among older adults.
Furthermore, the inconclusive results demonstrate that measuring social relationships and their influence on health services use is a challenging methodological endeavor. Future health services research should accentuate social relationship variables more in detail, and not only in terms of structure and quantity, but also according to functional and quality aspects of social relationships.
The relatively low number of included studies indicates a deficit of elaborated observational studies dealing with the role of social relationships for the utilization of health services among older populations. The majority of the identified studies have a cross-sectional design investigating a number of possible social relationships of health services use. It is crucial to determine social ties for health services use more clearly and to identify causal relations, especially in the form of prospective cohort studies.
Methodologically, it can be constructive to directly connect the question of social relationships and health care utilization to the scientific debate of health care inequalities [58–62] by conducting mediator or moderator analyses to create further clarity. This may complement the identification and understanding of social inequalities in health services utilization. In the future, this can be directed into new approaches to reduce social inequalities in health services utilization and to offer needs-based access to health care and adequate levels of treatment.
Supporting information
(PDF)
(DOCX)
(DOCX)
(DOC)
(DOCX)
(XLSX)
(XLSX)
(XLSX)
Acknowledgments
DB would like to thank PD Dr. Levente Kriston and Dr. Jens Klein for their helpful methodological advice.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Beaglehole R, Irwin A, Prentice T. The World Health Report 2003: Shaping the Future. Geneva: World Health Organization, 2003. [Google Scholar]
- 2.Freid VM, Bernstein AB. Health care utilization among adults aged 55–64 years: How has it changed over the past 10 years? Hyattsville: National Center for Health Statistics, 2010. 32. [PubMed] [Google Scholar]
- 3.Andersen RM. Revisiting the Behavioral Model and Access to Medical Care: Does it Matter? J Health Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 4.Abbott P, Sapsford R. Living on the Margins: Older People, Place and Social Exclusion. Policy Studies. 2005;26(1):29–46. [Google Scholar]
- 5.Pescosolido BA. Beyond rational choice: the social dynamics of how people seek help. Am J Sociol. 1992;97(4):1096–138. [Google Scholar]
- 6.Schmitz MF, Russell DW, Cutrona CE. Perceived Social Support and Social Network Influences on Physician Utilization Among the Elderly. Research in the Sociology of Health Care. 1997;14:249–72. [Google Scholar]
- 7.Schafer MH. Discussion networks, physician visits, and non-conventional medicine: probing the relational correlates of health care utilization. Soc Sci Med. 2013;87:176–84. doi: 10.1016/j.socscimed.2013.03.031 [DOI] [PubMed] [Google Scholar]
- 8.Arling G. Interaction effects in a multivariate model of physician visits by older people. Med Care. 1985;23(4):361–71. [DOI] [PubMed] [Google Scholar]
- 9.Foreman SE, Yu LC, Barley D, Chen LW. Use of health services by Chinese elderly in Beijing. Med Care. 1998;36(8):1265–82. [DOI] [PubMed] [Google Scholar]
- 10.Fritel X, Panjo H, Varnoux N, Ringa V. The individual determinants of care-seeking among middle-aged women reporting urinary incontinence: analysis of a 2273-woman cohort. Neurourol Urodynam. 2014;33(7):1116–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krause N. Stressful life events and physician utilization. J Gerontol. 1988;43(2):S53–61. [DOI] [PubMed] [Google Scholar]
- 12.Li Y, Chi I. Correlates of physician visits among older adults in China: the effects of family support. J Aging Health. 2011;23(6):933–53. doi: 10.1177/0898264311401390 [DOI] [PubMed] [Google Scholar]
- 13.Strain LA. Physician visits by the elderly: Testing the Anderson-Newman framework. Can J Sociol. 1990;15(1):19. [Google Scholar]
- 14.Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51(6):843–57. [DOI] [PubMed] [Google Scholar]
- 15.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316 doi: 10.1371/journal.pmed.1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blazer DG. Social support and mortality in an elderly community population. Am J Epidemiol. 1982;115(5):684–94. [DOI] [PubMed] [Google Scholar]
- 17.Hemingway H, Marmot M. Evidence based cardiology: psychosocial factors in the aetiology and prognosis of coronary heart disease. Systematic review of prospective cohort studies. Bmj. 1999;318(7196):1460–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540–5. [DOI] [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097 doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses 2000 [cited 2016 July 30th]. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 21.Herzog R, Alvarez-Pasquin MJ, Diaz C, Del Barrio JL, Estrada JM, Gil A. Are healthcare workers' intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health. 2013;13:154 doi: 10.1186/1471-2458-13-154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jüni P, Altman DG, Egger M. Assessing the quality of randomized controlled trials In: Egger M, Smith GD, Altman DG, editors. Systematic reviews in Health Care Meta-Analysis in Context. London: BMJ Publishing Group; 2003. p. 87–108. [Google Scholar]
- 23.Murad MH, Mustafa RA, Schünemann HJ, Sultan S, Santesso N. Rating the certainty in evidence in the absence of a single estimate of effect. Evid Based Med. 2017:ebmed-2017-110668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wan TTH, Arling G. Differential Use of Health Services among Disabled Elderly. Res Aging. 1983;5(3):411–31. [Google Scholar]
- 25.Eve SB. A Longitudinal-Study of Use of Health-Care Services among Older Women. J Gerontol. 1988;43(2):M31–M9. [DOI] [PubMed] [Google Scholar]
- 26.Crespo-Cebada E, Urbanos-Garrido RM. Equity and equality in the use of GP services for elderly people: the Spanish case. Health Policy. 2012;104(2):193–9. doi: 10.1016/j.healthpol.2011.10.007 [DOI] [PubMed] [Google Scholar]
- 27.Stoller EP. Patterns of physician utilization by the elderly: a multivariate analysis. Med Care. 1982;20(11):1080–9. [DOI] [PubMed] [Google Scholar]
- 28.Counte MA, Glandon GL. A panel study of life stress, social support, and the health services utilization of older persons. Med Care. 1991;29(4):348–61. [DOI] [PubMed] [Google Scholar]
- 29.Dalsgaard EM, Vedsted P, Fenger-Gron M, Sandbaek A, Vestergaard M. Socioeconomic position and contact to general practice among persons with diabetes. Prim Care Diabetes. 2012;6(4):313–8. doi: 10.1016/j.pcd.2012.06.002 [DOI] [PubMed] [Google Scholar]
- 30.Gobbens RJJ, van Assen MALM. Frailty and its prediction of disability and health care utilization: The added value of interviews and physical measures following a self-report questionnaire. Arch Gerontol Geriat. 2012;55(2):369–79. [DOI] [PubMed] [Google Scholar]
- 31.Jordan K, Jinks C, Croft P. A prospective study of the consulting behaviour of older people with knee pain. Br J Gen Pract. 2006;56(525):269–76. [PMC free article] [PubMed] [Google Scholar]
- 32.Korten AE, Jacomb PA. Predictors of GP service use: a community survey of an elderly Australian sample. Australian N Z J Public Health. 1998;22(5):609. [DOI] [PubMed] [Google Scholar]
- 33.Suominen-Taipale AL, Koskinen S, Martelin T, Holmen J, Johnsen R. Differences in older adults' use of primary and specialist care services in two Nordic countries. Eur J Public Health. 2004;14(4):375–80. doi: 10.1093/eurpub/14.4.375 [DOI] [PubMed] [Google Scholar]
- 34.Harris T, Cook DG, Victor CR, Beighton C, Dewilde S, Carey IM. Linking survey data with computerised records to predict consulting by older people. Br J Gen Pract. 2004;54(509):928–31. [PMC free article] [PubMed] [Google Scholar]
- 35.Hand C, McColl MA, Birtwhistle R, Kotecha JA, Batchelor D, Barber KH. Social isolation in older adults who are frequent users of primary care services. Can Fam Physician. 2014;60(6):e322, e4–9. [PMC free article] [PubMed] [Google Scholar]
- 36.Ryvicker M, Gallo WT, Fahs MC. Environmental factors associated with primary care access among urban older adults. Soc Sci Med. 2012;75(6):914–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rennemark M, Holst G, Fagerstrom C, Halling A. Factors related to frequent usage of the primary healthcare services in old age: findings from The Swedish National Study on Aging and Care. Health Soc Care Community. 2009;17(3). [DOI] [PubMed] [Google Scholar]
- 38.Park JM. Equity of access to primary care among older adults in Incheon, South Korea. Asia-Pac J Public Health. 2012;24(6):953–60. doi: 10.1177/1010539511409392 [DOI] [PubMed] [Google Scholar]
- 39.Pourat N, Lubben J, Yu H, Wallace S. Perceptions of health and use of ambulatory care: differences between Korean and White elderly. J Aging Health. 2000;12(1):112–34. doi: 10.1177/089826430001200106 [DOI] [PubMed] [Google Scholar]
- 40.Wan TTH, Odell BG. Factors Affecting the Use of Social and Health Services Among the Elderly. Ageing Soc. 1983;1(1):95–115. [Google Scholar]
- 41.Coulton C, Frost AK. Use of Social and Health-Services by the Elderly. J Health Soc Behav. 1982;23(4):330–9. [PubMed] [Google Scholar]
- 42.Branch L, Jette A, Evashwick C, Polansky M, Rowe G, Diehr P. Toward understanding elders' health service utilization. J Community Health. 1981;7(2):80–92. [DOI] [PubMed] [Google Scholar]
- 43.Goldsteen R, Counte MA, Glandon GL, Goldsteen K. Desirable Life Events and Physician Utilization among Older American Men and Women. J Aging Stud. 1992;6(2):149–63. [Google Scholar]
- 44.Liao P-A, Chang H-H, Yang F-A. Does the Universal Health Insurance Program Affect Urban-Rural Differences in Health Service Utilization Among the Elderly? Evidence From a Longitudinal Study in Taiwan. J Rural Health. 2012;28(1):84–91. doi: 10.1111/j.1748-0361.2011.00363.x [DOI] [PubMed] [Google Scholar]
- 45.Wolinsky FD, Coe RM. Physician and Hospital Utilization among Noninstitutionalized Elderly Adults—an Analysis of the Health Interview Survey. J Gerontol. 1984;39(3):334–41. [DOI] [PubMed] [Google Scholar]
- 46.Ezeamama AE, Elkins J, Simpson C, Smith SL, Allegra JC, Miles TP. Indicators of resilience and healthcare outcomes: findings from the 2010 health and retirement survey. Qual Life Res. 2016;25(4):1007–15. doi: 10.1007/s11136-015-1144-y [DOI] [PubMed] [Google Scholar]
- 47.Levkoff SE, Cleary PD, Wetle T. Differences in Determinants of Physician Use between Aged and Middle-Aged Persons. Med Care. 1987;25(12):1148–60. [DOI] [PubMed] [Google Scholar]
- 48.Cafferata GL. Marital-Status, Living Arrangements, and the Use of Health-Services by Elderly Persons. J Gerontol. 1987;42(6):613–8. [DOI] [PubMed] [Google Scholar]
- 49.Miltiades HB, Wu B. Factors affecting physician visits in Chinese and Chinese immigrant samples. Soc Sci Med (1982). 2008;66(3):704–14. [DOI] [PubMed] [Google Scholar]
- 50.Wolinsky FD, Johnson RJ. The Use of Health-Services by Older Adults. J Gerontol. 1991;46(6):S345–S57. [DOI] [PubMed] [Google Scholar]
- 51.Wolinsky FD, Coe RM, Miller DK, Prendergast JM, Creel MJ, Chavez MN. Health-Services Utilization among the Noninstitutionalized Elderly. J Health Soc Behav. 1983;24(4):325–37. [PubMed] [Google Scholar]
- 52.Hedges LV, Olkin I. Vote-counting methods in research synthesis. Psychol Bull. 1980;88(2):359. [Google Scholar]
- 53.Laporte A, Nauenberg E, Shen L. Aging, social capital, and health care utilization in Canada. Health EconPolicy Law. 2008;3(Pt 4):393–411. [DOI] [PubMed] [Google Scholar]
- 54.Cornwell EY, Waite LJ. Social network resources and management of hypertension. J Health Soc Behav. 2012;53(2):215–31. doi: 10.1177/0022146512446832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhang AY, Siminoff LA. The role of the family in treatment decision making by patients with cancer. Oncol Nurs Forum. 2003;30(6):1022–8. doi: 10.1188/03.ONF.1022-1028 [DOI] [PubMed] [Google Scholar]
- 56.Rook K. Stressful aspects of older adults' social relationships: current theory and research In: Stephens AP, Crowther JH, Hobfoll SE, Tennenbaum DL, editors. Stress and coping in later-life families. New York: Hemisphere; 1990. p. 173–92. [Google Scholar]
- 57.von dem Knesebeck O, Dragano N, Moebus S, Jockel KH, Erbel R, Siegrist J. [Stressful experiences in social relationships and ill health]. Psychother Psych Med. 2009;59(5):186–93. [DOI] [PubMed] [Google Scholar]
- 58.Aida J, Kondo K, Kondo N, Watt RG, Sheiham A, Tsakos G. Income inequality, social capital and self-rated health and dental status in older Japanese. Soc Sci Med. 2011;73(10):1561–8. doi: 10.1016/j.socscimed.2011.09.005 [DOI] [PubMed] [Google Scholar]
- 59.Dahl E, Malmberg-Heimonen I. Social inequality and health: the role of social capital. Sociol Health Illn. 2010;32(7):1102–19. doi: 10.1111/j.1467-9566.2010.01270.x [DOI] [PubMed] [Google Scholar]
- 60.Fone D, Dunstan F, Lloyd K, Williams G, Watkins J, Palmer S. Does social cohesion modify the association between area income deprivation and mental health? A multilevel analysis. Int J Epidemiol. 2007;36(2):338–45. doi: 10.1093/ije/dym004 [DOI] [PubMed] [Google Scholar]
- 61.von dem Knesebeck O, Geyer S. Emotional support, education and self-rated health in 22 European countries. BMC Public Health. 2007;7:272 doi: 10.1186/1471-2458-7-272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Melchior M, Berkman LF, Niedhammer I, Chea M, Goldberg M. Social relations and self-reported health: a prospective analysis of the French Gazel cohort. Soc Sci Med. 2003;56(8):1817–30. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(DOCX)
(DOCX)
(DOC)
(DOCX)
(XLSX)
(XLSX)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.


