Abstract
Objective
To determine the prevalence of femoroacetabular impingement morphology (FAIM), cam- or pincer-type, by magnetic resonance imaging (MRI) in asymptomatic adolescent soccer players, and to evaluate the possible correlation between alterations on MRI and clinical examination findings.
Methods
A cross-sectional study was conducted to determine the prevalence of FAIM in asymptomatic youth soccer players aged 13–18 years. A total of 112 hips in 56 players (mean age 15.3 years) were evaluated by MRI. Images were examined by two musculoskeletal radiologists for signs of FAIM. Cam-type (impingement) deformity was diagnosed by alpha angle ≥55° or head–neck offset <7 mm. Pincer-type (impingement) deformity was diagnosed by center-edge angle (CEA) ≥35° or acetabular index ≤0°. Other MRI changes, characteristic of FAIM, were observed. Clinical examination was performed to determine the range of motion (ROM) of the hips. In addition, specific tests for anterolateral and posteroinferior impingement were performed.
Results
The prevalence of MRI findings consistent with FAIM among this young population was 84.8% (95/112). The alpha angle was ≥55° in 77.7% (87/112) of hips, while the CEA was altered in 10.7% (12/112) of hips. Qualitative MRI findings consistent with FAIM were highly prevalent, and included loss of sphericity of the femoral head (77%), osseous bump (44%), femoral neck edema (21%), and acetabular osteitis (9%). The anterior impingement test was positive in 15% of the hips evaluated.
Conclusion
Youth soccer players have a high prevalence of FAIM as diagnosed by MRI. There is no correlation between physical examination findings and MRI evidence of FAIM in this population.
Keywords: Femoroacetabular impingement, Hip joint, Soccer, Magnetic resonance imaging
Resumo
Objetivo
Determinar a prevalência da morfologia de impacto femoroacetabular (MIFA), tipo cam ou pincer, por ressonância magnética (RM) em jogadores de futebol adolescentes e assintomáticos, bem como avaliar a possível correlação entre as alterações observadas na RM e os achados do exame clínico.
Métodos
Este estudo transversal teve como objetivo determinar a prevalência de MIFA em jogadores de futebol juvenil assintomáticos, com idade entre 13 e 18 anos. Um total de 112 quadris de 56 jogadores (idade média 15,3 anos). As imagens foram examinadas por dois radiologistas musculoesqueléticos, com o objetivo de identificar sinais de MIFA. A deformidade (impacto) do tipo cam foi diagnosticada quando o ângulo alfa ≥ 55° ou desvio entre a cabeça e o colo femoral <7 mm. A deformidade (impacto) do tipo pincer foi diagnosticada quando o ângulo centro-borda (ACB) ≥ 35° ou índice acetabular ≤ 0°. Outras alterações características de MIFA foram observadas na RM. A amplitude de movimento (ADM) dos quadris foi determinada a partir de um exame clínico. Além disso, foram realizados testes específicos para impactos anterolaterais e posteroinferiores.
Resultados
A prevalência de achados de RM consistentes com MIFA nessa população foi de 84,8% (95/112). O ângulo alfa foi ≥ 55° em 77,7% (87/112) dos quadris, enquanto o ACB apresentou alterações em 10,7% (12/112) de quadris. Observou-se uma alta prevalência de achados qualitativos de RM consistentes com MIFA, incluindo perda de esfericidade da cabeça femoral (77%), elevação óssea (44%), edema femoral (21%), e osteite acetabular (9%). O teste de impacto anterior foi positivo em 15% dos quadris avaliados.
Conclusão
Os exames de RM indicaram uma alta prevalência de MIFA entre jogadores de futebol juvenil. Nesta população, não houve correlação entre os achados do exame físico e a evidência de MIFA observada na RM.
Palavras-chave: Impacto femoroacetabular, Articulação do quadril, Futebol, Ressonância magnética
Introduction
Femoroacetabular impingement (FAI) is a condition resulting from abnormal contact between the femoral head and the acetabular rim, usually caused by a change in morphology of the proximal femur and/or acetabulum.1, 2, 3, 4 Ganz et al.2 described two basic mechanisms of FAI: cam and pincer. The cam mechanism occurs in patients with a non-spherical femoral head or with a decreased offset between the head and neck of femur. The impingement area is typically located on the anterolateral portion of the femoral head–neck junction. Pincer impingement, in turn, is characterized by acetabular overcoverage caused by an excess of the anterior wall.1, 2, 4, 5
FAI may decrease the range of motion (ROM) of the hip, especially in internal rotation (IR) of the flexed hip.2, 6 FAI is described as a cause of hip pain exacerbated by physical activity, and occurs mainly in young adult patients.4, 5 Clinical symptoms usually do not appear until adulthood; however, detection of FAIM is becoming increasingly common in the pediatric population.7 Patients often develop cartilage lesions and injury to the acetabular labrum, which can progress to hip osteoarthritis (OA) if the anatomic changes are not treated or the physical activity modified.2, 8, 9, 10
Adolescent patients who practice sports often perform high-impact activities that require extreme movements of the hip, which may predispose to more frequent and more intense conflicts between the proximal femur and the acetabulum.11
Physical activity during bone growth seems to be associated with an increased risk of cam-type deformity. Siebenrock et al. suggested that cam impingement in young athletes may be related to an abnormality in the physeal plate. Studies in high-performance adolescent basketball and hockey players found a high incidence of cam type FAI.3, 12
The purpose of this study was to determine the prevalence of FAIM (both cam and pincer type) in asymptomatic youth soccer players as diagnosed by magnetic resonance imaging (MRI) findings. Patients also underwent a clinical evaluation of the hip joints to ascertain possible correlations between changes on MRI and clinical signs of FAI.
Materials and methods
Demographics
From July 2012 to July 2013, 56 athletes from a first-division Brazilian youth soccer team were selected to participate in the study. They practice soccer in competition level, training a mean of five hours per day. All athletes were aged 13–18 years and did not have any symptoms of hip pathology. The dominant side of each athlete was identified. The exclusion criteria for this study were any history of treatment for pain related to the hip joint and contraindications or intolerance to MRI.
Written informed consent was obtained from all athletes and from the parents or guardians of athletes under 18 years old. The informed consent form was approved by the local institutional review board.
Magnetic resonance imaging evaluation
MRI was performed in a 1.5-T scanner using the following parameters: panoramic T1 coronal sequences including both hips (echo times of 10–14 ms and repeat times between 400 and 600 ms) and T2 (echo times of 35–70 ms and repeat times between 2000 and 3500 ms), with a slice thickness of 5 mm and 512 × 256 line matrix with a field of view of 33–36 cm; T2 sequences focused on the hip joints, with and without fat saturation in the coronal, sagittal, and oblique axial slices, with a thickness of 4 mm and a 384 × 224 line matrix with a field of view of 22–25 cm.
Based on the radiographic appearance of the capital femoral physis on MRI, participants were stratified into those with open physeal plates and those with closed physeal plates.
Cam morphology was evaluated by measuring the alpha angle and femoral head–neck offset. The alpha angle was measured on an oblique axial sequence as described elsewhere in the literature. Participants with an alpha angle ≥55° were diagnosed with cam morphology13, 14 (Fig. 1).
Fig. 1.
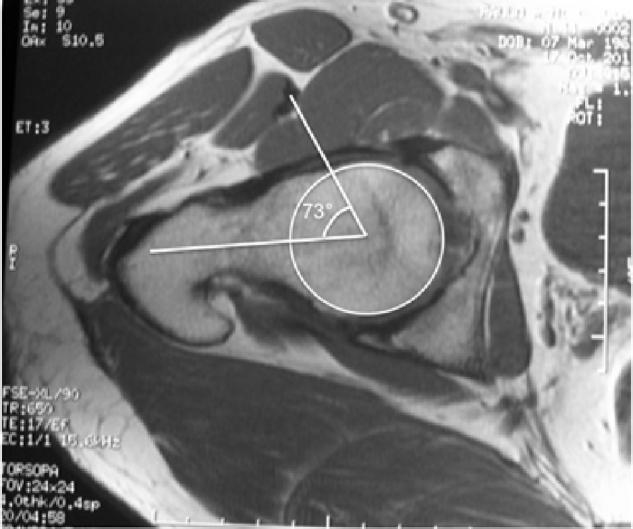
MRI of the right hip (axial oblique view) for measurement of the alpha angle. Image representative of altered alpha angle.
The femoral head–neck offset was measured by drawing a line in the center of the femoral head and neck and two parallel lines, one along the anterior cortex of the femoral neck and the other along the anterior outer part of the femoral head. The distance between the second and third lines corresponds to the head–neck offset, and, when less than 7 mm, is indicative of cam deformity15 (Fig. 2).
Fig. 2.
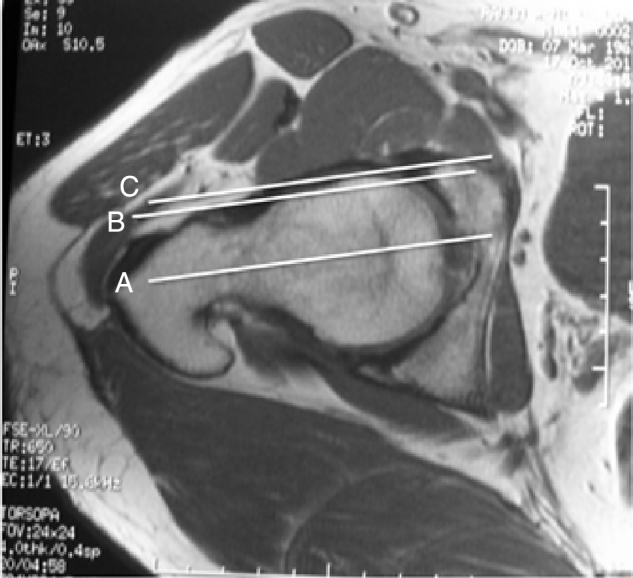
Femoral head–neck offset <7 mm indicates cam deformity.
The diagnosis of pincer morphology was established by measuring the center-edge angle (CEA), or Wiberg angle, and the acetabular index (AI), or Tönnis angle. A CEA ≥39° or AI ≤0° indicates pincer deformity. The CEA was measured on the coronal plane, between a vertical line passing through the center of the femoral head and another line drawn from the center of the femoral head to the lateral acetabular rim. The AI is defined as the angle between a horizontal line and another line connecting the medial point of the sclerotic zone of the acetabular roof and the lateral edge of the acetabulum16, 17 (Fig. 3).
Fig. 3.

CEA and the AI indicative of pincer deformity.
Other MRI alterations consistent with FAI considered by the examining radiologists were osseous bump,18 synovial pit,6, 7, 14, 19, 20, 21, 22 bone edema in the femoral neck, acetabular osteitis and lesions of the labrum and/or acetabular cartilage.
Physical examination
A physical examination of the hip was performed by an orthopedic surgeon specializing in hip surgery. ROM was measured with a manual goniometer in flexion, extension, IR, external rotation (ER), adduction, and abduction. Specific tests for anterolateral and posteroinferior impingement were also performed.
The anterior impingement test was performed with the patient in the supine position, flexing the hip 90°, with adduction and internal rotation. The test was considered positive if it elicited pain.2, 6
The posteroinferior impingement test was performed with the patient in the supine position, hanging the leg over the end of the bed while in extension and external rotation. Again, the test was considered positive if the patient reported pain.20, 23
Statistical analysis
Two independent musculoskeletal radiologists, blinded to physical examination findings, analyzed the MRI scans. Concordance between their results was assessed using the kappa index, which is considered satisfactory when >0.7. In case of discrepancy between examiners, a third, experienced radiologist conducted another evaluation.
The results were entered into a Microsoft Excel spreadsheet and exported to PASW Statistics, version 18.0, for analysis. Quantitative variables were described as means and standard deviations, and categorical variables, as absolute and relative frequencies. Prevalence was reported with 95% confidence intervals. Comparisons of continuous variables were performed using the independent samples t-test.
Results
Baseline demographics
A total of 56 male athletes (112 hips) were included in the study. No athletes were excluded. The mean age was 15.3 years, with a distribution as shown in Table 1. The right side was dominant in 80.3% (45/56) of the athletes. There was no significant difference in the prevalence of FAIM on comparison of the dominant and contralateral hips.
Table 1.
Distribution of patients by age.
| Age | n | % |
|---|---|---|
| 13 | 7 | 12.5 |
| 14 | 15 | 26.8 |
| 15 | 10 | 17.9 |
| 16 | 11 | 19.6 |
| 17 | 7 | 12.5 |
| 18 | 6 | 10.7 |
| Total | 56 | 100.0 |
MRI findings
Concordance between the findings of the two examining radiologists was satisfactory; therefore, analysis by a third radiologist was not necessary. The best inter-rater concordance was in the alpha angle, with a kappa coefficient of 0.91.
The prevalence of abnormalities characteristic of FAIM was 84.8% (95/112) (95%CI 78–91.5%). The MRI changes observed, and their respective prevalence, are described in Table 2.
Table 2.
Prevalence of MRI findings indicative of femoroacetabular impingement morphology in the sample (n = 56, 112 hips).
| MRI finding | Prevalence (%) | 95%CI |
|---|---|---|
| Loss of sphericity | 73 | 65–82 |
| Decreased head–neck offset | 57 | 48–66 |
| Alpha angle ≥55° | 77.7 | 69.8–85.5 |
| Acetabular index ≤0° | 0 | 0 |
| Wiberg angle ≥39° | 10.7 | 4.9–16.5 |
| Osseous bump | 44 | 34–53 |
| Sinovial pit | 4 | 0–7 |
| BME at head/neck junction | 21 | 14–29 |
| Labral lesion | 8 | 3–13 |
| Degenerative labral lesion | 2 | −1 to 4 |
| Acetabular osteitis | 9 | 4–14 |
| Chondral lesion | 3 | 0–6 |
BME, bone marrow edema; CI, confidence interval; MRI, magnetic resonance imaging.
Abnormal alpha angle (≥55°) was observed in 77.7% (87/112) of hips, while abnormal femoral head–neck offset (<7 mm) was seen in 57% (64/112). The alpha angle was altered in all individuals with reduced offset. The physeal plate was open in 23.2% (13/56) of athletes. There was no significant difference in the prevalence of altered alpha angle between athletes with an open physeal plate and those with a closed physeal plate.
After stratification of athletes by age, the prevalence of altered alpha angle ranged from 63.6% (7/11) in 16-year-olds 100% (6/6) in 18-year-olds. There were no significant differences in prevalence across different ages.
Areas of bone marrow edema (BME) were observed in the femoral head–neck junction of 24 hips (21%), all of which exhibited an elevated alpha angle. Acetabular labral lesions were identified in 10 hips and chondral lesions were found in three.
All hips had an AI ≥2°. A CEA >39° was seen in 10.7% (12/112) of the hips, indicating a diagnosis of pincer deformity.
Pooled analysis of MRI findings (Table 3) showed that most of the hips (76.8%) had more than one alteration suggestive of FAI, and >50% had four or more such changes.
Table 3.
Number of MRI changes found in the sample (n = 56, 112 hips).
| Number of changes | Frequency | Percentage | Cumulative percentage |
|---|---|---|---|
| 0 | 17 | 15.2 | 15.2 |
| 1 | 9 | 8.0 | 23.2 |
| 2 | 8 | 7.1 | 30.4 |
| 3 | 20 | 17.9 | 48.2 |
| 4 | 24 | 21.4 | 69.6 |
| 5 | 19 | 17.0 | 86.6 |
| 6 | 11 | 9.8 | 96.4 |
| 7 | 2 | 1.8 | 98.2 |
| 8 | 2 | 1.8 | 100.0 |
| Total | 112 | 100.0 | |
Correlation between MRI and physical examination findings
The results of ROM measurement are presented in Table 4. There was no significant association between ROM and MRI findings consistent with FAI. Concerning the posteroinferior and anterolateral impingement tests, the former was negative in all athletes, while the latter was positive in 17 hips, of which 15 showed findings suggestive of FAI on MRI scans. There was no significant difference in the prevalence of positive impingement test results between hips with and without signs of FAI. Even when an alpha angle ≥65° was considered diagnostic of cam-type impingement, there was no correlation between alpha angle and positive anterolateral impingement test. There was no correlation between MRI changes and physical examination findings.
Table 4.
Results of range of motion (ROM) tests in patients with and without MRI evidence of femoroacetabular impingement morphology.
| Variable | MRI evidence of FAIM | No MRI evidence of FAIM | p |
|---|---|---|---|
| Flexion | 127.9 ± 5.6 | 126.5 ± 7.8 | 0.48 |
| Extension | 9.9 ± 1.5 | 10.6 ± 1.7 | 0.12 |
| Adduction | 32 ± 4.5 | 31.5 ± 3.4 | 0.64 |
| Abduction | 47.4 ± 4.4 | 48.5 ± 3.8 | 0.31 |
| IR | 43 ± 11.2 | 46.8 ± 10.7 | 0.2 |
| ER | 49.3 ± 8.2 | 48.2 ± 4.6 | 0.43 |
ER, external rotation; FAI, femoroacetabular impingement; IR, internal rotation; MRI, magnetic resonance imaging.
Results expressed as mean ± standard deviation. p-values from Student's t-test for independent samples.
Discussion
Physical activity during bone growth may be associated with an increased risk of FAI deformity, which can progress to hip OA during adulthood. This is the first study to assess the prevalence of MRI changes consistent with FAIM in asymptomatic youth soccer players and analyze the potential correlation between these changes and physical examination findings.
The prevalence of MRI changes indicative of FAIM in the present sample was 84.8%. This is a higher prevalence than that reported in previous studies of soccer players.24, 25, 26 When comparing the prevalence of pathological alpha angle only (≥55°, cam-type deformity), the 77.7% rate found in the present study was higher than those reported by Gerhardt et al.25 (68%) and Johnson et al.26 (60%), both studies that evaluated adult soccer players using plain radiography. It was also higher than the 26% prevalence reported by Agricola et al. who evaluated adolescent soccer players using plain radiography, but considering the alpha angle abnormal only if >60°.24, 25, 26 This can be explained by the greater sensitivity of MRI compared to plain radiography in identifying changes that characterize FAI.27, 28, 29 The excellent concordance between the examining radiologists in measuring the alpha angle, with a kappa coefficient of 0.91, demonstrates the reproducibility of MRI for diagnosis of cam-type impingement.
MRI findings of cam deformity in the present sample were very similar to those reported in previous studies of adolescent athletes in other sports. Siebenrock et al.30 reported an 89% prevalence of cam deformity in basketball players aged 9–25 years, including after physeal closure. Philippon et al. found an alpha angle ≥55° in 75% of hockey players between the ages of 10 and 18.21
Comparing the prevalence of cam deformity in the present study with the results of Frank et al.31 in a systematic review about prevalence of FAIM in asymptomatic volunteers, it was higher than the 37–54.8% found in athletes and much higher than the 23.1% in the general population.
A high prevalence of cam-type impingement morphology in young high-level athletes corroborates the hypothesis proposed by Siebenrock et al.,12 which suggests a direct relationship between physical activity and a higher incidence of cam-type FAIM, probably due to enlargement of the physeal plate. The finding of MRI evidence of BME in the femoral head/neck junction in 21.4% of hips (24/112) in this sample is highly suggestive of stress-related changes, which suggest active FAI and probably precede the development of femoral head–neck bump deformity.
The prevalence of cam deformity was similar between athletes with open and closed physeal plates, which suggest that the cam is formed even before physeal plate growth is completed. If this lesion is caused by stress from bone impaction, the earlier it starts, the greater the potential for damage; the immature skeleton is more complacent, and can easily be remodeled by abnormal forces.
There was no correlation between dominant side and prevalence of FAIM, which suggests there is no specific activity or movement that causes FAI. Simple stress over the physis during physical activities could explain the high prevalence of cam-type impingement morphology.
The identification of two or more MRI changes indicative of FAI in 76.8% of hips, in an entirely asymptomatic sample, underlines the importance of careful assessment when recommending surgical procedures to patients in whom diagnosis is based solely on MRI findings. Monitoring of athletes could help define how many of these patients would develop symptoms and require surgery. Follow-up of the present sample would allow identification the incidence of chondral and labral lesions in youth soccer players, as well as identification of which level of sports practice intensity could be considered a risk factor for hip OA.
When athletes with signs of impingement on MRI were compared to those with normal hips, no significant differences in ROM or anterolateral and posteroinferior impingement test results were found. This suggests that, in asymptomatic youth soccer players, physical examination findings are inconclusive regarding the diagnosis of FAI. Furthermore, it suggests that MRI can reveal abnormalities consistent with FAIM before they become apparent on clinical examination.
The inverse relationship between increased prevalence of FAI and reduced IR described in the literature was not confirmed in this study, probably because the sample was asymptomatic and very young (i.e., a subclinical population).32 Any decrease in IR or ER could be important, because of the possibility of increased risk of anterior cruciate ligament rupture.33
Limitations
The limitations of this study include the lack of a control group of adolescents who did not practice physical activities at a high level. We plan to conduct a matched case–control study to evaluate the prevalence of these findings in a normal population. In addition, the age range of the athletes could have been extended down to 10 years, which would have allowed better assessment of the timing of FAIM onset, especially of cam-type FAI.
Conclusion
The youth soccer players who participated in our study had a high prevalence of abnormalities characteristic of FAIM on MRI. Physical examination findings did not correlated with MRI evidence of FAIM.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Study conducted at the Universidade Federal do Rio Grande do Sul, Faculdade de Medicina, Hospital de Clínicas de Porto Alegre (HCPA), Department of Orthopedic Surgery, Porto Alegre, RS, Brazil.
References
- 1.Clohisy J.C., Knaus E.R., Hunt D.M., Lesher J.M., Harris-Hayes M., Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467(3):638–644. doi: 10.1007/s11999-008-0680-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ganz R., Parvizi J., Beck M., Leunig M., Nötzli H., Siebenrock K.A. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 3.Ito K., Minka M.A., 2nd, Leunig M., Werlen S., Ganz R. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head–neck offset. J Bone Joint Surg Br. 2001;83(2):171–176. doi: 10.1302/0301-620x.83b2.11092. [DOI] [PubMed] [Google Scholar]
- 4.Sink E.L., Gralla J., Ryba A., Dayton M. Clinical presentation of femoroacetabular impingement in adolescents. J Pediatr Orthop. 2008;28(8):806–811. doi: 10.1097/BPO.0b013e31818e194f. [DOI] [PubMed] [Google Scholar]
- 5.Fabricant P.D., Heyworth B.E., Kelly B.T. Hip arthroscopy improves symptoms associated with FAI in selected adolescent athletes. Clin Orthop Relat Res. 2012;470(1):261–269. doi: 10.1007/s11999-011-2015-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Philippon M.J., Maxwell R.B., Johnston T.L., Schenker M., Briggs K.K. Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007;15(8):1041–1047. doi: 10.1007/s00167-007-0348-2. [DOI] [PubMed] [Google Scholar]
- 7.Philippon M.J., Yen Y.M., Briggs K.K., Kuppersmith D.A., Maxwell R.B. Early outcomes after hip arthroscopy for femoroacetabular impingement in the athletic adolescent patient: a preliminary report. J Pediatr Orthop. 2008;28(7):705–710. doi: 10.1097/BPO.0b013e318186eb2e. [DOI] [PubMed] [Google Scholar]
- 8.Beaulé P.E., Kim Y.J., Rakhra K.S., Stelzeneder D., Brown T.D. New frontiers in cartilage imaging of the hip. Instr Course Lect. 2012;61:253–262. [PubMed] [Google Scholar]
- 9.Beck M., Kalhor M., Leunig M., Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 10.Schmitz M.R., Campbell S.E., Fajardo R.S., Kadrmas W.R. Identification of acetabular labral pathological changes in asymptomatic volunteers using optimized, noncontrast 1.5-T magnetic resonance imaging. Am J Sports Med. 2012;40(6):1337–1341. doi: 10.1177/0363546512439991. [DOI] [PubMed] [Google Scholar]
- 11.Keogh M.J., Batt M.E. A review of femoroacetabular impingement in athletes. Sports Med. 2008;38(10):863–878. doi: 10.2165/00007256-200838100-00005. [DOI] [PubMed] [Google Scholar]
- 12.Siebenrock K.A., Behning A., Mamisch T.C., Schwab J.M. Growth plate alteration precedes cam-type deformity in elite basketball players. Clin Orthop Relat Res. 2013;471(4):1084–1091. doi: 10.1007/s11999-012-2740-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnston T.L., Schenker M.L., Briggs K.K., Philippon M.J. Relationship between offset angle alpha and hip chondral injury in femoroacetabular impingement. Arthroscopy. 2008;24(6):669–675. doi: 10.1016/j.arthro.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 14.Nötzli H.P., Wyss T.F., Stoecklin C.H., Schmid M.R., Treiber K., Hodler J. The contour of the femoral head–neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84(4):556–560. doi: 10.1302/0301-620x.84b4.12014. [DOI] [PubMed] [Google Scholar]
- 15.Clohisy J.C., Nunley R.M., Otto R.J., Schoenecker P.L. The frog-leg lateral radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop Relat Res. 2007;462:115–121. doi: 10.1097/BLO.0b013e3180f60b53. [DOI] [PubMed] [Google Scholar]
- 16.Kutty S., Schneider P., Faris P., Kiefer G., Frizzell B., Park R. Reliability and predictability of the centre-edge angle in the assessment of pincer femoroacetabular impingement. Int Orthop. 2012;36(3):505–510. doi: 10.1007/s00264-011-1302-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stelzeneder D., Hingsammer A., Bixby S.D., Kim Y.J. Can radiographic morphometric parameters for the hip be assessed on MRI? Clin Orthop Relat Res. 2013;471(3):989–999. doi: 10.1007/s11999-012-2654-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fritz A.T., Reddy D., Meehan J.P., Jamali A.A. Femoral neck exostosis, a manifestation of cam/pincer combined femoroacetabular impingement. Arthroscopy. 2010;26(1):121–127. doi: 10.1016/j.arthro.2009.04.076. [DOI] [PubMed] [Google Scholar]
- 19.Leunig M., Beck M., Kalhor M., Kim Y.J., Werlen S., Ganz R. Fibrocystic changes at anterosuperior femoral neck: prevalence in hips with femoroacetabular impingement. Radiology. 2005;236(1):237–246. doi: 10.1148/radiol.2361040140. [DOI] [PubMed] [Google Scholar]
- 20.Parvizi J., Leunig M., Ganz R. Femoroacetabular impingement. J Am Acad Orthop Surg. 2007;15(9):561–570. doi: 10.5435/00124635-200709000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Philippon M.J., Ho C.P., Briggs K.K., Stull J., LaPrade R.F. Prevalence of increased alpha angles as a measure of cam-type femoroacetabular impingement in youth ice hockey players. Am J Sports Med. 2013;41(6):1357–1362. doi: 10.1177/0363546513483448. [DOI] [PubMed] [Google Scholar]
- 22.Pitt M.J., Graham A.R., Shipman J.H., Birkby W. Herniation pit of the femoral neck. AJR Am J Roentgenol. 1982;138(6):1115–1121. doi: 10.2214/ajr.138.6.1115. [DOI] [PubMed] [Google Scholar]
- 23.Crawford J.R., Villar R.N. Current concepts in the management of femoroacetabular impingement. J Bone Joint Surg Br. 2005;87(11):1459–1462. doi: 10.1302/0301-620X.87B11.16821. [DOI] [PubMed] [Google Scholar]
- 24.Agricola R., Bessems J.H., Ginai A.Z., Heijboer M.P., van der Heijden R.A., Verhaar J.A. The development of Cam-type deformity in adolescent and young male soccer players. Am J Sports Med. 2012;40(5):1099–1106. doi: 10.1177/0363546512438381. [DOI] [PubMed] [Google Scholar]
- 25.Gerhardt M.B., Romero A.A., Silvers H.J., Harris D.J., Watanabe D., Mandelbaum B.R. The prevalence of radiographic hip abnormalities in elite soccer players. Am J Sports Med. 2012;40(3):584–588. doi: 10.1177/0363546511432711. [DOI] [PubMed] [Google Scholar]
- 26.Johnson A.C., Shaman M.A., Ryan T.G. Femoroacetabular impingement in former high-level youth soccer players. Am J Sports Med. 2012;40(6):1342–1346. doi: 10.1177/0363546512439287. [DOI] [PubMed] [Google Scholar]
- 27.Barton C., Salineros M.J., Rakhra K.S., Beaulé P.E. Validity of the alpha angle measurement on plain radiographs in the evaluation of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2011;469(2):464–469. doi: 10.1007/s11999-010-1624-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Masjedi M., Marquardt C.S., Drummond I.M., Harris S.J., Cobb J.P. Cam type femoro-acetabular impingement: quantifying the diagnosis using three dimensional head–neck ratios. Skeletal Radiol. 2013;42(3):329–333. doi: 10.1007/s00256-012-1459-5. [DOI] [PubMed] [Google Scholar]
- 29.Dudda M., Albers C., Mamisch T.C., Werlen S., Beck M. Do normal radiographs exclude asphericity of the femoral head–neck junction? Clin Orthop Relat Res. 2009;467(3):651–659. doi: 10.1007/s11999-008-0617-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Siebenrock K.A., Ferner F., Noble P.C., Santore R.F., Werlen S., Mamisch T.C. The cam-type deformity of the proximal femur arises in childhood in response to vigorous sporting activity. Clin Orthop Relat Res. 2011;469(11):3229–3240. doi: 10.1007/s11999-011-1945-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Frank J.M., Harris J.D., Erickson B.J., Slikker W., 3rd, Bush-Joseph C.A., Salata M.J. Prevalence of femoroacetabular impingement imaging findings in asymptomatic volunteers: a systematic review. Arthroscopy. 2015;31(6):1199–1204. doi: 10.1016/j.arthro.2014.11.042. [DOI] [PubMed] [Google Scholar]
- 32.Reichenbach S., Jüni P., Werlen S., Nüesch E., Pfirrmann C.W., Trelle S. Prevalence of cam-type deformity on hip magnetic resonance imaging in young males: a cross-sectional study. Arthritis Care Res (Hoboken) 2010;62(9):1319–1327. doi: 10.1002/acr.20198. [DOI] [PubMed] [Google Scholar]
- 33.Gomes J.L., de Castro J.V., Becker R. Decreased hip range of motion and noncontact injuries of the anterior cruciate ligament. Arthroscopy. 2008;24(9):1034–1037. doi: 10.1016/j.arthro.2008.05.012. [DOI] [PubMed] [Google Scholar]


