Abstract
Background
There are no previous whole-country studies on mental health and relationships with general health in intellectual disability populations; study results vary.
Aims
To determine the prevalence of mental health conditions and relationships with general health in a total population with and without intellectual disabilities.
Method
Ninety-four per cent completed Scotland’s Census 2011. Data on intellectual disabilities, mental health and general health were extracted, and the association between them was investigated.
Results
A total of 26 349/5 295 403 (0.5%) had intellectual disabilities. In total, 12.8% children, 23.4% adults and 27.2% older adults had mental health conditions compared with 0.3, 5.3 and 4.5% of the general population. Intellectual disabilities predicted mental health conditions; odds ratio (OR)=7.1 (95% CI 6.8–7.3). General health was substantially poorer and associated with mental health conditions; fair health OR=1.8 (95% CI 1.7–1.9), bad/very bad health OR=4.2 (95% CI 3.9–4.6).
Conclusions
These large-scale, whole-country study findings are important, given the previously stated lack of confidence in comparative prevalence results, and the need to plan services accordingly.
Declaration of interest
None.
Copyright and usage
© The Royal College of Psychiatrists 2017. This is an open access article distributed under the terms of the Creative Commons Non-Commercial, No Derivatives (CC BY-NC-ND) license.
Mental ill health is unevenly distributed across the population and appears to be more prevalent among people with intellectual disabilities compared with the general population.1,2 An adult prevalence of 22.4% has been reported excluding problem behaviours and autism or 40.9% including problem behaviours and autism;1 and a prevalence of 36% including problem behaviours has been reported in children and young people, compared with 8% in those without intellectual disabilities.2 However, most studies have limitations. Indeed, a recent National Institute for Health and Care Excellence (NICE) clinical guideline development group3 reviewed the epidemiological evidence on prevalence of mental ill health in people with intellectual disabilities compared with the general population, and concluded they were not very confident in the results, in view of the variation in quality of the studies, and the need to include administrative samples because of limited population-based cohorts. For example, the most detailed, population-based study of adults with intellectual disabilities to date included only 1023 and no direct general population comparison group,1 and the most comprehensive study of children and young people with intellectual disabilities, which did include a general population comparison group, included only 641 with intellectual disabilities, and was restricted to just those living in private households. Both studies had high recruitment uptake. Although other studies have also reported prevalence rates, they tend to be limited by non-representative samples and/or small study sizes.4,5
Poor physical health is more common among people with intellectual disabilities.6–9 People with intellectual disabilities are, therefore, at high risk of comorbid physical and mental ill health. In the general population, this combination is associated with poorer outcomes, such as premature death.10–12 Hence an improved understanding of the prevalence of mental ill health and its relationship with general health in the population with intellectual disabilities, undertaken on a large scale, is highly indicated.
This study’s aims were to (1) describe the prevalence of mental ill health in the population with intellectual disabilities compared with those without intellectual disabilities, (2) investigate the odds of intellectual disabilities on having mental ill health when adjusted for age and gender, and (3) investigate the relationship of mental and physical health in the population with intellectual disabilities.
Method
Data source
The data source was Scotland’s Census 2011. This provides statistical information on the number and characteristics of Scotland’s population and households at the census day, 27 March 2011.13 The census is undertaken every 10 years. It includes people living in communal establishments (such as care homes and student halls of residence) as well as people living in private households. In 2011, Scotland’s Census was estimated to have achieved a 94% response rate, which is close to the highest ever historic compliance rate. A coverage assessment and adjustment process was used to take account of non-response in the final Census outputs. Scotland’s Census is probably one of few country censuses that identifies people with intellectual disabilities and distinguishes these from specific learning disabilities such as dyslexia, and from autism; indeed it may be unique in this regard. Full details of the methodology and other background information on Scotland’s Census 2011 are available at: www.scotlandscensus.gov.uk/supporting-information.
The Census requires the form to be completed by the head of household or joint head of household on behalf of all occupants in private households, and the manager is responsible on behalf of all occupants in communal dwellings. It is a legal requirement to complete the Census, and the Census form clearly states this, and that a head of household not completing it or supplying false information can be fined £1000. The Census team follow up non-responders and also provide help to respond when that is needed (there was not an easy-read version), hence the high 94% completion rate.
Census variables
Intellectual disabilities, mental health condition and other conditions
People with intellectual disabilities were identified by self-/proxy-reporting on intellectual disabilities from the individual questions section; question 20: ‘Do you have any of the following conditions which have lasted, or are expected to last, at least 12 months? Tick all that apply’. There was a choice of 10 response options, which included:
deafness or partial hearing loss
blindness or partial sight loss
learning disability (e.g. Down syndrome)
learning difficulty (e.g. dyslexia)
developmental disorder (e.g. autism spectrum disorder or Asperger syndrome)
physical disability
mental health condition
long-term illness, disease or condition
other condition and
no condition.
For ‘other condition’, a prompt was included for the respondent to report the type of ‘other condition’. Importantly, the question distinguishes between intellectual disabilities (for which the term ‘learning disability’ is used in Scotland), specific learning disabilities and autism.
General health
General health status was collected through the question, ‘How is your health in general?’, with a five-point response scale as follows: (1) very good, (2) good, (3) fair, (4) bad and (5) very bad.
Procedures
Following Scottish Government approval, data from Scotland’s Census 2011 were analysed under the auspices of a collaborative research project with the National Records of Scotland at its premises in Ladywell House, Edinburgh. All resulting raw frequency tables of Census data were checked to ensure they did not breach statistical disclosure control thresholds and were published on the Scotland’s Census website, available under the Health topic at: www.scotlandscensus.gov.uk/ods-web/data-warehouse.html#additionaltab
Data analysis
We calculated the number and percentage of people with intellectual disabilities, compared with the general population. We compared gender and age structure by Pearson’s χ2 test. We calculated the number and percentage of people with intellectual disabilities reporting a mental health condition and compared this with the general population by Pearson’s χ2 test. We then used two binary logistic regressions to calculate the odds ratios (95% confidence intervals (CIs)) of intellectual disabilities referenced to no intellectual disabilities, in statistically predicting the dependent variable ‘mental health condition’, adjusted: (1) for gender and age (given the different gender and age structure in the two populations), and (2) for gender, age and general health status. Age was categorised into the following groups: 0–15, 16–24, 25–34, 35–44, 45–54, 55–64, 65–74 and 75+ years. The age group 0–15 years was the reference group for age, male was the reference gender group and good/very good health was the reference group for general health status. Next, within the population with intellectual disabilities, two binary logistic regressions were undertaken to investigate: (1) the extent to which age and gender were independent predictors of having a mental health condition, and (2) the extent to which age, gender and general health status were statistically independent predictors of having a mental health condition. The enter method was used. All analyses were conducted with SPSS version 22.
Results
Participant characteristics
Scotland’s Census 2011 includes records on 5 295 403 people; 26 349 (0.5%) with intellectual disabilities and 5 269 054 without intellectual disabilities. There were 15 149 (57.5%) males and 11 200 (42.5%) females with intellectual disabilities, compared with 2 567 444 (48.7%) males and 2 727 959 (51.8%) females without intellectual disabilities (χ2=860.5; d.f.=1; P<0.001). The population with intellectual disabilities were younger than those without, with 5234 (19.9%) aged 0–15 years, 18 660 (70.8%) aged 16–64 years and 2455 (9.3%) aged 65+ years, compared with 911 097 (17.3%) aged 0–15 years, 3 470 078 (65.9%) aged 16–64 years and 887 879 (16.9%) aged 65+ years in those without intellectual disabilities (χ2=1083.2; d.f.=2; P<0.001). The prevalence of intellectual disabilities was highest in childhood, reaching its peak by age 9 years (0.7–0.8%), being 0.5% at 25–34 years, and then progressively falling from age 55–64 years to 0.2% at age 75+ years.
The population with intellectual disabilities were significantly more likely to have physical disability (32.6% v. 6.6%; χ2=28316.0; d.f.=1; P<0.001), blindness or partial sight loss (13.1% v. 2.3%, χ2=13034.7; d.f.=1; P<0.001), deafness or partial hearing loss (12.4% v. 6.6%, χ2=1421.6; d.f.=1; P<0.001) and autism (21.7% v. 0.5%, χ2=197451.8; d.f.=1; P<0.001).
Prevalence of mental health conditions
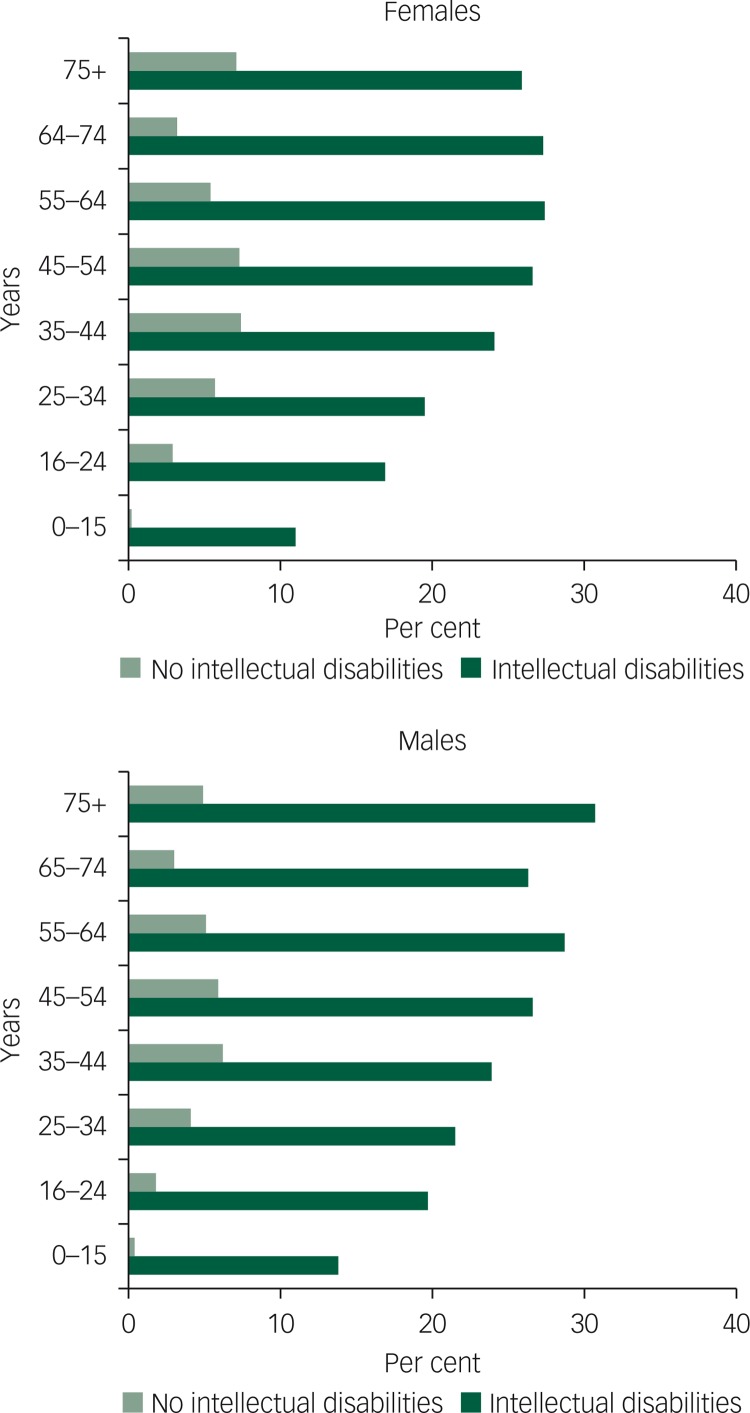
Mental health conditions were reported more often for people with, compared with people without, intellectual disabilities: 668 (12.8%) v. 2653 (0.3%) aged 0–15 years (χ2=22415.3; d.f.=1; P<0.001); 4370 (23.4%) v. 184 191 (5.3%) aged 16–64 years (χ2=11907.5; d.f.=1; P<0.001); and 668 (27.2%) v. 40 393 (4.5%) aged 65+ years (χ2=2857.7; d.f.=1; P<0.001). Table 1 and Fig. 1 show the prevalence of mental health conditions by age and gender. There are significant differences between people with and without intellectual disabilities at all ages and for both genders, most markedly so for children and young people.
Table 1. Prevalence of mental ill health in the populations with and without intellectual disabilities.
| Age group | Intellectual disabilities, n/N (%) | Other people, n/N (%) | ||||
|---|---|---|---|---|---|---|
| Male N=15 149 | Female N=11 200 | All N=26 349 | Male N=2 552 295 | Female N=2 716 759 | All N=5 269 054 | |
| 0–15 | 450/3253 (13.8) | 218/1981 (11.0) | 668/5234 (12.8) | 1739/465 853 (0.4) | 914/445 244 (0.2) | 2653/911 097 (0.3) |
| 16–24 | 492/2501 (19.7) | 281/1661 (16.9) | 773/4162 (18.6) | 5664/314 382 (1.8) | 9113/313 944 (2.9) | 14 777/628 326 (2.4) |
| 25–34 | 436/2025 (21.5) | 286/1450 (19.7) | 722/3475 (20.8) | 13 552/326 582 (4.1) | 19 330/337 270 (5.7) | 32 882/663 852 (4.9) |
| 35–44 | 529/2209 (23.9) | 398/1650 (24.1) | 927/3859 (24.0) | 22 004/355 461 (6.2) | 27 633/375 434 (7.4) | 49 637/730 895 (6.8) |
| 45–54 | 653/2456 (26.6) | 490/1845 (26.6) | 1143/4301 (26.6) | 22 723/382 061 (5.9) | 29 384/400 394 (7.3) | 52 107/782 455 (6.7) |
| 55–64 | 442/1539 (28.7) | 363/1324 (27.4) | 805/2863 (28.1) | 16 581/325 383 (5.1) | 18 207/339 167 (5.4) | 34 788/66 4550 (5.2) |
| 65–74 | 212/805 (26.3) | 208/762 (27.3) | 420/1567 (26.8) | 6776/224 557 (3.0) | 8106/255 668 (3.2) | 14 882/48 0225 (3.1) |
| 75+ | 111/361 (30.7) | 137/527 (25.9) | 248/888 (27.9) | 7741/158 016 (4.9) | 17 770/249 683 (7.1) | 25 511/407 654 (6.3) |
| All ages | 3325/15 149 (21.9) | 2381/11 200 (21.3) | 5706/26 349 (21.7) | 96 780/2 552 295 (3.8) | 130 457/2 716 759 (4.8) | 227 237/5 269 054 (4.3) |
Fig. 1. Prevalence of a mental health condition by gender and age group.
Adjusting for age and gender, given the different distributions in the two populations, intellectual disabilities had an odds ratio of 7.1 (95% CI 6.8–7.3) in statistically predicting mental health conditions (Table 2). Good/very good health, fair health had an odds ratio of 10.4 (95% CI 10.3–10.6) and bad/very bad health had an odds ratio of 25.7 (95% CI 25.4–26.0) in statistically predicting mental health conditions, when referenced against good/very good health (Table 2).
Table 2. Independent predictors of mental ill health in the whole population.
| Regression 1 | Regression 2 | |||
|---|---|---|---|---|
| Characteristic | Odds ratio | 95% CI | Odds ratio | 95% CI |
| Ability | ||||
| No intellectual disabilities (reference) | – | – | – | – |
| Intellectual disabilities | 7.058 | 6.843–7.280 | 3.187 | 3.077–3.300 |
| Gender | ||||
| Male (reference) | – | – | – | |
| Female | 1.238 | 1.227–1.248 | 1.243 | 1.232–1.255 |
| Age | ||||
| 0–15 (reference) | – | – | – | |
| 16–24 | 6.908 | 6.652–7.172 | 6.175 | 5.943–6.415 |
| 25–34 | 14.655 | 14.139–15.189 | 11.292 | 10.888–11.710 |
| 35–44 | 20.437 | 19.729–21.171 | 11.987 | 11.564–12.426 |
| 45–54 | 20.063 | 19.369–20.782 | 8.451 | 8.152–8.761 |
| 55–64 | 15.628 | 15.079–16.197 | 4.484 | 4.322–4.651 |
| 65–74 | 9.083 | 8.747–9.433 | 2.016 | 1.939–2.096 |
| 75+ | 18.456 | 17.796–19.139 | 2.979 | 2.869–3.093 |
| General health status | ||||
| Very good/good (reference) | – | |||
| Fair | 10.445 | 10.328–10.563 | ||
| Bad/very bad | 25.702 | 25.387–26.021 | ||
| Constant | 0.003 | – | 0.002 | |
Relationship between general health and mental health
Within the intellectual disabilities population, female gender reduced the likelihood of mental health conditions. Each progressive increase in age group, up to 64 years, predicted mental health conditions compared with childhood; thereafter, the odds ratio plateaued (Table 3). Fair health had an odds ratio of 1.8 (95% CI 1.7–1.9) and bad/very bad health had an odds ratio of 4.2 (95% CI 3.9–4.6) in statistically predicting mental health conditions, when referenced against good/very good health (Table 3).
Table 3. Independent predictors of mental ill health in the population with intellectual disabilities.
| Regression 1 | Regression 2 | |||
|---|---|---|---|---|
| Characteristic | Odds ratio | 95% CI | Odds ratio | 95% CI |
| Gender | ||||
| Male (reference) | – | – | – | |
| Female | 0.917 | 0.864–0.974 | 0.893 | 0.839–0.950 |
| Age | ||||
| 0–15 (reference) | – | – | – | |
| 16–24 | 1.562 | 1.396–1.748 | 1.660 | 1.479–1.863 |
| 25–34 | 1.799 | 1.603–2.019 | 1.925 | 1.710–2.166 |
| 35–44 | 2.171 | 1.945–2.423 | 2.253 | 2.014–2.522 |
| 45–54 | 2.485 | 2.236–2.763 | 2.485 | 2.230–2.770 |
| 55–64 | 2.694 | 2.401–3.023 | 2.556 | 2.271–2.876 |
| 65–74 | 2.572 | 2.220–2.902 | 2.389 | 2.072–2.753 |
| 75+ | 2.699 | 2.291–3.193 | 2.450 | 2.061–2.913 |
| General health status | ||||
| Very good/good (reference) | – | |||
| Fair | 1.783 | 1.663–1.912 | ||
| Bad/very bad | 4.210 | 3.887–4.559 | ||
| Constant | 0.151 | – | 0.092 | |
Discussion
Principle findings and interpretation
This large-scale study is the first of a whole-country population to investigate mental health and the relationship with general health in the population with intellectual disabilities at all ages, including children. It found a substantially higher prevalence of mental health conditions at all ages compared with the population without intellectual disabilities. These findings are important, given the previously stated lack of confidence as to whether people with intellectual disabilities have higher rates of mental health conditions, when excluding problem behaviours and autism.3 Few previous studies have reported mental health in comparison with the general population, and those that did had either small sample sizes or reported from general population cohort studies. The general population cohort studies are limited through being focused on mild intellectual disabilities as very few people with more severe intellectual disabilities are included in existing cohorts, and typically are restricted to private households, whereas people with intellectual disabilities are more likely to live in communal establishments than are the general population.
We found mental health conditions to be related to poorer general health status. In the whole population, this was the case for fair health compared with good/very good health and was more markedly so for people with bad/very bad health. We found the same pattern in the population with intellectual disabilities, but to a lesser extent. Contrary to the general population, however, males rather than females were more likely to have mental health conditions, highlighting the importance of specifically studying the health of people with intellectual disabilities, to provide health intelligence that is relevant to them.
The 23.4% prevalence of mental health conditions we report for adults with intellectual disabilities is very similar to the 22.4% (excluding problem behaviours and autism) reported in the previously largest study of 1023 adults who all had individual detailed assessments.1 The Census prevalence of mental health conditions also excludes autism, as autism was separately enquired about, but it did not specifically enquire about problem behaviours, so it is unclear whether or not respondents included problem behaviours within their understanding of mental health conditions. Regarding children, the previously reported rate of 36% in 641 surveyed children with intellectual disabilities did include problem behaviours.2 This is higher than the 12.8% with mental health conditions in Scotland’s Census data, which may well be accounted for by problem behaviours; the substantial difference compared with the general population is apparent in both these data-sets.
Within the population with intellectual disabilities, increasing age was associated with increasing odds of mental health conditions, until age 64 years when the odds plateaued, giving some credence to a healthy survivor effect in this population.14 As the older adults start to acquire mental health conditions related to ageing (dementia), one would expect their extent of mental health conditions to increase further. This is not observed in the data, although prevalence rates are still substantially greater than in the general population and then in the population of children with intellectual disabilities. This may be because of the premature death of people with severe/profound intellectual disabilities who have higher levels of mental health conditions, relative to people with mild intellectual disabilities.
The population with intellectual disabilities also had higher rates of physical disability, blindness or partial sight loss, deafness or partial hearing loss and autism. Despite the considerably greater burden of both mental health and physical health that we have reported in the population with intellectual disabilities, it is notable the extent to which their needs have been neglected by researchers, as shown by the limited evidence base. Clearly, more research is needed to better understand the health and healthcare needs of people with intellectual disabilities.
Strengths and limitations
This Scottish total country study is the largest and most complete population study we have identified investigating reported mental health of people with intellectual disabilities compared with people in the general population across the lifespan, and reports on general health associations with mental ill health. The advantage of Scotland’s Census data is that it covers communal establishments as well as private households, and specifically, systematically, asked about the presence of intellectual disabilities for each person, distinguishing this from specific learning disabilities and autism; lack of these features has previously been highlighted as a limitation of previous research on people with intellectual disabilities conducted with large data-sets.15 Additionally, it provides a whole-country coverage, with a 94% response. It may well be unique in having all these features and, therefore, is the strength of the study.
The ascertained prevalence of intellectual disabilities by Scotland’s Census is similar for adults (0.5%) to that reported in a recent meta-analysis of population-based studies of prevalence (4.94/1000),16 giving further credence to the ascertainment in the Census. However, we recognise that the country of study, sample population, age range, definition of intellectual disabilities and method of ascertainment can all impact on identified rate.17 Cohort effects result in prevalence varying with time, such that past and more recent studies of the same age ranges may well provide different rates.17 These factors become lost within a meta-analysis. For children and young people we found the prevalence in Scotland’s Census varied by age, in view of the time taken for identification in childhood, making comparisons with published studies difficult. Regarding proxy-reporting for presence of intellectual disabilities, limitations have been reported with young children (e.g. age 3),15 and this is apparent in Scotland’s Census data as ascertainment increases up to age 9. Adults would, of course, have been diagnosed in childhood.
We have no reason to believe the study results are not generalisable to other high-income countries.
A limitation is the lack of information on whether the responses were completed by proxies or the person with intellectual disabilities. Given the style and questions on the Census, we consider it very unlikely that people with intellectual disabilities would have been able to complete the form without help. In private households, the head of household completing the Census was most likely to be a parent of the people with intellectual disabilities, in supported living a support worker, and in communal establishments the manager. The data are, therefore, likely to be proxy-report rather than self-report for the great majority of people with intellectual disabilities. We recognise that proxy ratings could differ from self-ratings with regard to health ratings,15 but without them would have no information on people unable to self-report because of severe/profound intellectual disabilities. We note that proxy-reporting is the basis for much of the healthcare provided for people with intellectual disabilities who cannot self-report.
A further limitation is the cross-sectional design of the study. Hence, we are merely reporting associations, and causality cannot be assumed. Indeed, in the general population there is literature to suggest that mental ill health can lead to poor general ill health, and also the reverse, with poor general health leading to mental ill health.11,12 A longitudinal study would be needed to untangle the preceding and precipitating factors.
Implications
People with intellectual disabilities of all ages have substantially higher rates of mental health conditions than the rest of the population, and their mental health conditions are often associated with poor general health. Their health patterns differ from those seen in the general population.9 These conditions are often not identified or are misattributed to the persons’ learning disabilities (diagnostic overshadowing). Additionally, people with intellectual disabilities are known to experience difficulties accessing mainstream services.6,7 Globally, no country has comprehensive coverage of intellectual disability psychiatric services except the UK, and in the UK, there is increasing ‘mainstreaming’ of psychiatric care. Knowledge on intellectual disabilities and the poor general health associated with mental health is, therefore, essential for general psychiatrists and mainstream psychiatric services, as well as for carers. Without awareness of the substantial burden of mental health conditions and its co-existence with poor general health, the potential for misdiagnosis is high, and inadequate or inappropriate treatment is a risk. Health burden is also important to know for resource allocation, service planning, and to support individuals and their carers.
Clearly, given the associations we report, more research is needed to determine relationships between specific mental health problems, physical conditions and associated factors, for example, adversity, among people with intellectual disabilities, to help influence the development of appropriate interventions, and health and social care policy.
Funding
Scottish Government via the Scottish Learning Disabilities Observatory.
References
- 1.Cooper S-A, Smiley E, Morrison J, Allan L, Williamson A. Prevalence of and associations with mental ill-health in adults with intellectual disabilities. Br J Psychiatry 2007; 190: 27–35. [DOI] [PubMed] [Google Scholar]
- 2.Emerson E, Hatton C. The mental health of children and adolescents with intellectual disabilities in Britain. Br J Psychiatry 2007; 191: 493–9. [DOI] [PubMed] [Google Scholar]
- 3.National Institute for Health and Care Excellence. Mental Health Problems in People with Learning Disabilities: Prevention, Assessment and Management. NICE Clinical Guideline 54. NICE, 2016. [PubMed] [Google Scholar]
- 4.Einfeid SL, Ellis LA, Emerson E. Comorbidity if intellectual disability and mental disorder in children and adolescents: a systematic review. J Intellect Dev Disabil 2011; 36: 137–43. [DOI] [PubMed] [Google Scholar]
- 5.Buckles J, Luckasson R, Keefe E. A systematic review of the prevalence of psychiatric disorders in adults with intellectual disabilities, 2003–2010. J Ment Health Res Intellect Disabil 2013; 6: 181–207. [Google Scholar]
- 6.NHS Health Scotland. Health Needs Assessment Report. People With Learning Disabilities in Scotland. NHS Health Scotland, 2004. [Google Scholar]
- 7.Ouelette-Kuntz H, Garcin N, Lewis S. Addressing Health Disparities through Promoting Equity for Individuals with Intellectual Disabilities. Queen's University; Healthcare Equity for Intellectually Disabled Individuals Programme: Canada, 2004. [Google Scholar]
- 8.Oesburg B, Dijkstra GJ, Groothoff JW, Reijneveld SA, Jansen DE. Prevalence of chronic health conditions in children with intellectual disability: a systematic literature review. Intellect Dev Disabil 2011; 49: 59–85. [DOI] [PubMed] [Google Scholar]
- 9.Cooper S-A, McLean G, Guthrie B, McConnachie A, Mercer S, Sullivan F, et al. Multiple physical and mental health comorbidity in adults with intellectual disabilities: population-based cross-sectional analysis. BMC Fam Pract 2015: 16: 110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. Mental Health: Facing the Challenges, Building Solutions. Report from the WHO European Ministerial Conference. WHO Regional Office for Europe, 2005. [Google Scholar]
- 11.Naylor C, Parsonage M, McDaid D, Knapp M, Fosse M, Galea A. Long-term Conditions and Mental Health: The Cost of Co-morbidities. The King’s Fund, 2012. [Google Scholar]
- 12.Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, et al. No health without mental health. Lancet 2007; 370: 859–77. [DOI] [PubMed] [Google Scholar]
- 13.National Records of Scotland. 2011 Census: Digitised Boundary Data (Scotland) [computer file]. UK Data Service Census Support; (http://edina.ac.uk/census). [Google Scholar]
- 14.Moss SC. Age and functional abilities of people with a mental handicap: evidence from the Wessex mental handicap register. J Ment Defic Res 1991; 35: 430–45. [DOI] [PubMed] [Google Scholar]
- 15.Emerson E, Felce D, Stancliffe R. Issues concerning self-report data and population-based data sets involving people with intellectual disabilities. Intellect Dev Disabil 2013; 51: 333–48. [DOI] [PubMed] [Google Scholar]
- 16.Maulik PK, Mascarenhas MN, Mathers CD, Dua T, Saxena S. Prevalence of intellectual disability: a meta-analysis of population-based studies. Res Dev Disabil 2011; 32: 419–36. [DOI] [PubMed] [Google Scholar]
- 17.Cooper S-A, Henderson A, Jacobs M, Smiley E. What Are Learning Disabilities? How Common are Learning Disabilities? Scottish Learning Disabilities Observatory, 2016. (https://www.sldo.ac.uk/media/1610/what-are-learning-disabilities-how-common-are-learning-disabilities.pdf).