Abstract
Objectives
1. To assess the long-term effectiveness of a comprehensive cardiac rehabilitation programme on quality of life and survival in patients with a large spectrum of cardiovascular diseases (myocardial infarction, acute coronary syndrome, percutaneous transluminal coronary angioplasty and coronary artery bypass grafting). 2. To establish the degree of correlation between expected improvement of health-related quality of life and improvement in physical function attributable to rehabilitation in the intervention group, in comparison with similar changes in the conventional care group.
Design
Randomized, controlled, parallel-group design (intervention/conventional care).
Setting
Akershus County, southeast of Oslo City, Norway.
Participants
500 patients, men and women, aged 40-85 years, who have sustained at least one of the above-mentioned cardiovascular diseases.
Interventions
8 weeks of supervised, structured physical training of three periods of 20 min per week, targeting a heart rate of 60-70% of the individual's maximum; home-based physical exercise training with the same basic schedule as in the supervised period; quantification of patients' compliance with the exercise programme by the use of wristwatches, information stored in the watch memory being retrieved once a month during the 3-year follow-up period; and life-style modification with an emphasis on the cessation of smoking and on healthy nutrition and weight control.
Keywords: cardiac, intervention, rehabilitation, risk factors
Introduction
Post-infarct rehabilitation, a process of restoring physical and psychological fitness, has become increasingly employed in hospitals both in the USA and Europe during the past three decades, primarily as a vehicle of secondary prevention with the ultimate goal of reducing long-term mortality. However, rehabilitation programmes from the 1960s were particularly focused on psychologically based therapy and exercise training, with a gradual shift during the 1990s to programmes of comprehensive rehabilitation in the context of randomized, controlled trials [1,2,3,4].
The clinical benefits of cardiac rehabilitation are clear, as demonstrated by several reports and meta-analyses [5,6,7,8]. The benefits included decreased mortality, improved quality of life, and possibly lower costs because of lower rates of rehospitalization.
Important components of rehabilitative programming for coronary patients include progressive physical activity, education of patient and family, and psychosocial and vocational counselling. Conventionally, rehabilitation is incorporated into traditional care during hospitalization for myocardial infarction (MI), coronary bypass surgery or angioplasty; it involves the patient's family and social environment as a support system, and continues in the office of the patient's physician and/or in a variety of community facilities. Initiation and coordination of rehabilitative efforts fall within the responsibility of both hospital doctors (usually cardiologists) and the primary care physician. The multifactorial nature of morbidity after acute myocardial infarction (AMI) indicates the need for and relevance of a multifactorial approach and the contribution of a multidisciplinary team.
In spite of improvements in the quality of previous cardiac rehabilitation trials and the encouraging conclusions of meta-analysis that indicate a reduction of about 20% in total and cardiovascular mortality, there are still controversies on the overall effectiveness of rehabilitation generally [9,10,11]. Several factors have contributed to this situation, which in practice translates into a poor external validity for many of the trials reported in the past 20 years.
Many uncontrolled observations making unjustifiable claims probably reflect nothing more than the natural resolution of morbidity after MI. Small trials, as many trials are in the field of cardiac rehabilitation, are prone to bias towards exaggeration, with the consequent risk of false positive findings.
Among the drawbacks encountered in most of the trials is the use of highly selected patients or volunteers in specialist centres and very restrictive inclusion criteria (eg the exclusion of patients with associated co-morbidities) [12]. Most trials included only patients aged less than 65 years, yet more than 40% of MI patients are more than 65 years old [13,14,15]. Patients older than 70 years account for one-third to one-half of patients with AMI admitted to hospital. The application of trial results to clinical practice is hampered by the fact that such patients, although accounting for up to half of the cases of MI and having a disproportionately high mortality, are significantly under-represented in clinical trials.
Most trials have included only men (eg the WHO trial [7]), yet about 30% of MI patients are women [16,17].
The overall heterogeneity of the rehabilitation trials performed so far, mainly generated by the employment of exclusive designs, impairs their external validity. Generalization of the conclusions beyond the groups studied is therefore not possible. This, in turn, makes the effectiveness of rehabilitation in all potentially eligible patients questionable, because it is largely untested.
Study design
The CORE Study is designed as a pragmatic (effectiveness) trial meant to evaluate an intervention with already proven efficacy [secondary prevention of coronary heart disease (CHD)], but with special emphasis on the assessment of quality of life (five different domains) and on the quantification of patients' long-term compliance with regular physical exercise. The intervention is offered to a heterogeneous group of people under ordinary clinical circumstances, covering a wide age range, for both sexes and with heterogeneous characteristics (co-morbidities).
Through the specific nature of the primary and secondary objectives, the trial is a combination of qualitative and quantitative research, targeting both soft and hard measures of outcome.
To ensure a rigorous methodological approach, considerable effort has been dedicated to developing appropriate strategies for screening, recruitment and assessment [18,19].
The CORE study will be a randomized, controlled, single centre trial, driven by the Medical Department of the Akershus Central Hospital in Oslo, Norway.
Subjects are being recruited from a population of about 300,000 inhabitants of Akershus County during a 12-month period starting in April 2000. Men and women between 40 and 85 years old with at least one of the inclusion criteria [AMI, stabilized acute coronary syndrome (ACS), percutaneous transluminal coronary angioplasty (PTCA) or coronary artery bypass grafting (CABG)] will be screened for participation in the study.
The follow-up period will continue until the last randomized patient has been followed up for 36 months. Patients not randomized because of scheduled coronary angiography, scheduled PTCA or CABG or who necessitated one of these alternatives after being randomized will be approached and checked or rechecked for eligibility within 6 weeks of the invasive investigation, or alternatively after a PTCA or CABG.
Co-morbidities such as hypertension, heart failure and diabetes will not be exclusion criteria in themselves; however, a certain degree of severity of these conditions, as stipulated in the exclusion criteria, might exclude a particular patient from being randomized.
Study objectives
The primary objective is to assess patients' quality of life in the light of their health-related experiences after having sustained an AMI/ACS or PTCA/CABG and to establish the extent of correlation of quality of life with improvement in physical function attributable to rehabilitation.
The secondary objectives are to study total and cardiovascular mortality, morbidity and recurrence rates of coronary events throughout a 3-year follow-up period, and to determine the efficacy and feasibility of a comprehensive rehabilitation programme encompassing home-based long-term follow-up with the aim of preserving continuity of care.
Eligibility criteria
Inclusion criteria
1. Males and females aged 40-85 years.
2. Unequivocal hospital-verified, definite AMI less than 3 months ago defined by either unequivocal ECG evidence of a new MI with or without typical history, or a typical rise and fall in biochemical markers of myocardial damage, where the maximal value reached is greater than twice the upper limit of the hospital reference range, with either a typical history and/or new ECG changes indicating myocardial ischaemia.
3. Patients with a recent ACS (that is, established CHD with a stabilized condition after a recent unstable episode) defined by either a changed pattern of angina or chest pain at rest or on minimal exertion or emotion (two 5-min episodes or one episode lasting more than 10 min) in addition to evidence of underlying coronary artery disease (at least one of the following): ECG (ST segment depression, T wave inversion or transient ST elevation); enzyme elevation [troponine I or T, creatine kinase (CK) or CK-MB]; evidence of coronary artery disease on angiography or perfusion scanning.
4. PTCA patients (more than 4 weeks after a PTCA).
5. CABG patients (more than 4 weeks after a CABG).
6. Ambulatory patients who have signed a declaration of consent.
Exclusion criteria
1. Unstable angina pectoris.
2. Scheduled angiography.
3. Clinically significant heart failure (peripheral oedema, rales over two-thirds of the chest, pulmonary congestion on chest X-ray, cardiothoracic ratio more than 0.5, ejection fraction less than 35%).
4. Severe hypertension (systolic blood pressure more than 200 mmHg and/or diastolic blood pressure more than 105 mmHg) despite treatment to decrease blood pressure.
5. Symptoms of orthostatic hypotension or a supine systolic blood pressure of 90 mmHg or lower.
6. Severe arrhythmias persisting after the acute phase of the AMI (frequent premature ventricular beats, grade III-IV of the Lown classification, atrial flutter, partial or complete atrioventricular block).
7. Psychoneurotic disorders (depression or/and anxiety).
8. Severe obstructive airway disease with permanent respiratory insufficiency [interfering with performance in the exercise tolerance test (ETT)].
9. Uncontrolled diabetic mellitus (HbA1C more than 9).
10. Severe orthopaedic disability (interfering with ETT performance).
11. Serum creatinine more than double the local upper normal limit (in the context of known renal disease).
12. Alanine amino-transferase or aspartate amino-transferase more than three times the local upper limit (in the context of known liver disease).
13. Presence of any condition that limits life expectancy (eg cancer or haematological diseases).
14. Problems expected with compliance or follow-up.
15. Participation in another trial or study during the past 30 days.
16. Stroke with severe physical disability (interfering with ETT performance).
Ethics and informed consent
The final protocol was approved by an independent Institutional Review Board affiliated to the University of Oslo.
Written consent is obtained from patients after the study objectives, design, scope of the intervention, and risks and benefits have been explained carefully. Risks are described as related to the ETT with a cycle ergometer and partly to the physical training itself. Exercise testing has documented safety when appropriate guidelines are followed [20], and risks of injury and/or sudden cardiac death during physical training can be minimized with medical evaluation, risk stratification, supervision and education [21]. Emergency equipment and trained personnel will be available to deal with unusual situations that might arise [22,23,24].
Sample size and statistical analysis
Prospective international registries (OASIS registry [25] and PRAIS UK registry [26]) indicate rates of death or MI of about 10-12% at 6 months. On the basis of further literature reviews, an overall mean proportion of survival rate for all subjects enrolled in the study after 3 years of follow-up would be about 80%.
A desired 10% improvement in the survival of patients in the intervention group, with 80% power and 0.05% significance level, will require 250 subjects per group and 500 subjects in total [27].
An 'intention to treat' analysis is to be strictly applied, subjects withdrawn will be followed up for endpoints and attention will be paid to appropriate handling of missing information (sensitivity analysis).
Pearson's correlation coefficient will be calculated for the QLMI (quality of life after MI) scores between groups and for QLMI scores and patients' improvement in physical activity as quantified through the ETT.
The responsiveness of the questionnaire will be evaluated by calculating the ratio between the change in subjects' score between the baseline and the 12-month, 24-month and 36-month visits and the pooled standard deviation of change during this period.
The χ2 test and independent-samples t test respectively will be used for comparing proportions and means of targeted parameters, with 0.05 as the level of statistical significance and a 95% confidence interval around point estimates.
Subgroup analysis will be performed for the three age groups: 40-65 years, 66-75 years and 76-85 years.
Randomization
After having ascertained the patient's eligibility and willingness to participate in the study and after written consent has been given, randomization takes place with allocation to the intervention (I) or the conventional care (CC) group [28,29,30]. The particular allocation and its consequences for the long-term follow-up are clearly explained to each patient.
Separate randomization sheets are generated by a computer program for the two main groups (I and CC) and for three age subgroups. The pseudorandom number generator is a linear congruent algorithm of Park and Miller with Bays-Durham shuffling. It has a period of over 2 ×109 [31].
The process of randomization will be concealed.
Risk stratification, follow-up and investigation schedule
During hospitalization, risk stratification is performed in all patients with the aim of selecting the high-risk individuals at this early stage and deciding on the need for invasive investigation, eventually leading to PTCA or CABG.
Before discharge from the hospital, patients assigned to both the I and CC groups will be exposed to a standardized programme developed for addressing the knowledge and skills of cardiac assessment, drug use and adherence as well as for facilitating behaviour change in relation to lifestyle and modification of risk factors.
After discharge, an outpatient ETT is scheduled to be performed on every patient within 6 weeks, with the aim of assessing their baseline physical capacity.
Follow-up visits after the first ETT are scheduled for both groups (I and CC) at 6-month intervals for an average period of 3 years (Fig. 1). However, a prolonged period for follow-up visits may be decided upon, on the basis of several objective factors emerging with time (accrual rate, losses to follow-up, overall patient compliance, or rate of major endpoint). Parameters checked at different visits are indicated in the investigation schedule (Table 1).
Figure 1.
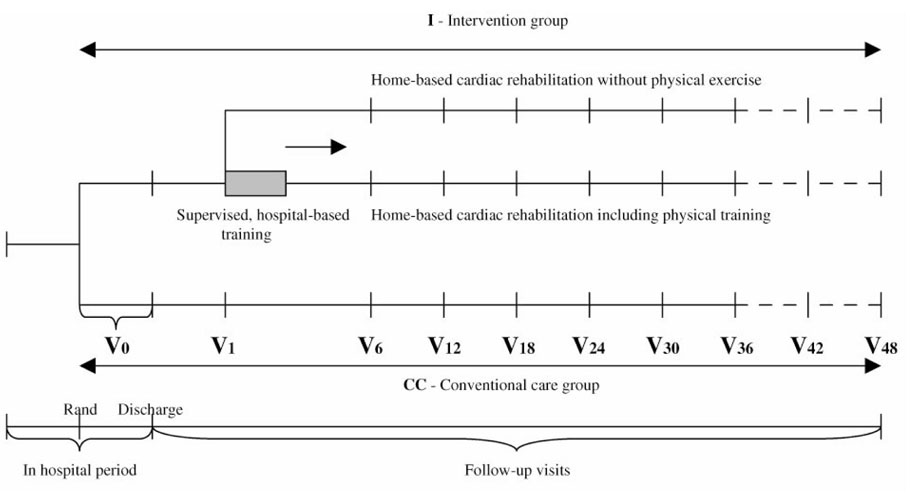
Study design.
Table 1.
Investigation schedule
| Investigation | V0 | V1 | V6 | V12 | V18 | V24 | V30 | V36 | V42* | V48* |
| History | × | |||||||||
| Clinical examination | × | × | × | × | × | × | ||||
| QLMI questionnaire | A | B | B | B† | B | B† | B | B† | B | B† |
| Blood pressure | × | × | × | × | × | × | × | × | × | |
| ECG | × | × | × | × | × | × | ||||
| Laboratory tests | × | × | × | × | × | × | ||||
| Smoking + S-cotinine | × | × | × | × | × | × | × | × | × | × |
| Exercise level | × | × | × | × | × | × | × | × | ||
| Nutrition + BMI | × | × | × | × | × | × | × | × | × | |
| Alcohol status | × | × | × | × | × | × | × | × | × | × |
| ETT | ×†× | × | × | |||||||
| Medication | × | × | × | × | × | × | × | × | × | × |
| Adverse events | × | × | × | × | × | × | × | × | × | × |
*If applicable. †Patient's evaluation questionnaire. ‡ETT at the start and the end of 8 weeks of supervised exercise training.V0-V48, visits at 6-month intervals; BMI, basal metabolic index.
Intervention programme
Patients in the I group will be targeted for a structured secondary prevention programme under the supervision of a team of workers who will use the knowledge, skills, techniques and services of a variety of medical consultants, healthcare personnel and community resources to implement rehabilitation in a wide spectrum of patients with CHD (AMI, ACS, PTCA and CABG) and to establish continuity in the provision of care. The ultimate goal is an improvement in the quality of life and survival in all these patients, regardless of age or associated co-morbidities.
A patient education curriculum has been designed as a standardized programme developed for the modification of secondary risk factor through structured counselling of the particular patient and his or her closest family member. The following topics will be focused on: nutrition, smoking and alcohol habits, behaviour modification, social and familial support and compliance with the drug regimen [32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51]. Special teaching classes on these topics will be given repeatedly during the 8 weeks after the first ETT, in parallel with a physical training programme given during the same period.
Brief counselling will be offered individually at the 6-month visits.
Special consideration has been given to targeting a programme of systematic physical training tailored to each individual, on the basis of the results of an initial ETT performed 6 weeks after an acute event. The programme consists of 8 weeks of supervised outpatient physical training. At the end of this programme a new ETT will quantify any improvement in the patient's physical condition (total work capacity at the end of the trial [W], absolute oxygen consumption [VO2], relative energy expenditure in metabolic equivalents [1 MET = 3.5 kcal/min] and the rate-pressure product). A structured physical training programme will be tailored for each individual in the form of a home-based exercise programme. Compliance with the programme and the results attained will be quantified by the use of a wristwatch given to every patient in the intervention group [52,53,54,55,56]. In the interval between two visits, the patients in the I group will be asked to come to the outpatient clinic every fourth week (five times between two 6-month visits). During these short visits lasting 10-15 min, the information stored in the wristwatch will be printed out and documented on the case report form.
A final ETT will be performed on subjects allocated to both groups (I and CC) at the end of the trial and compared with the results of the baseline ETT. (A detailed description of the ETT protocol, the 8-week supervised programme and the home-based exercise training programme will be reported elsewhere.)
Assessment of quality of life
Measurement of the quality of life has evolved as the endpoint of choice and the ultimate goal of rehabilitation programmes after MI [57,58,59]. Although survival, return to previous employment or comfortable retirement are paramount issues for patients having sustained one of the four pathological entities focused on, there are other concerns dealing with the quality of life such as the persistence of symptoms, the ability to perform appropriate activities at different stages of the illness and the ability to care for oneself. Such issues reflect the quality of life in terms of personal satisfaction and a sense of well-being.
The disease-specific QLMI questionnaire developed by N Oldridge and G Guyatt [60] has been tested in the context of a randomized rehabilitation trial and has been shown to have a high degree of reliability in measuring changes in health-related quality of life over time while being more responsive than other questionnaires employed so far. We decided on the use of a modified version of the QLMI questionnaire with new items covering the patient's period before admission to hospital, and 10 items omitted from the original version.
The following domains are covered in the questionnaire: pre-hospital period (three questions), symptom domain (five questions), restriction domain (two questions), confidence domain (three questions), self-esteem domain (three questions) and emotion domain (three questions). There are seven graded answers to each question (one to seven points per question), leading to a final score assessed at randomization and after 1, 2 and 3 years of follow-up.
Conclusions
The CORE Study is a randomized, controlled, parallel-group, single-centre trial to investigate the benefits of a systematically implemented comprehensive rehabilitation programme, with its main focus on quality of life and survival in patients with large spectrum of CHDs. Important features include:
1. targeting patients with AMI, stabilized ACS, PTCA and CABG;
2. planning the enrolment of a large number of women;
3. broad age range (40-85 years);
4. concealed randomization;
5. recruitment of sufficient patients to provide adequate statistical power to detect effects of small size;
6. provision of an individually tailored yet standardized, well-defined programme for both physical exercise and change of risk factors for CHD;
7. monitoring of patient safety and data integrity by an independent data and safety monitoring board;
8. ascertainment of primary and secondary endpoint and planned intention-to-treat analysis completely and in an unbiased manner.
References
- Cundey PE, Frank MJ. Cardiac rehabilitation and secondary prevention after a myocardial event. Clin Cardiol. 1995;18:547–553. doi: 10.1002/clc.4960181003. [DOI] [PubMed] [Google Scholar]
- Moher M. Evidence of effectiveness of interventions for secondary prevention and treatment of coronary heart disease in primary care Cambridge: Anglia and Oxford Regional Health Authority; 1995.
- Campbell NC, Thain J, Deans HG. Secondary prevention in coronary heart disease: baseline survey of provision in general practice. Br Med J. 1998;316:1430–1434. doi: 10.1136/bmj.316.7142.1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lonn EM, Yusuf S. Evidence based cardiology: emerging approaches in preventing cardiovascular disease. Br Med J. 1999;318:1337–1341. doi: 10.1136/bmj.318.7194.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor GT, Buring JE, Yusuf S, Goldhaber SZ, Olmstead EM, Paffenbarger RX, Jr, Hennekens CH. An overview of randomized trials of rehabilitation with exercise after myocardial infarction. Circulation. 1989;80:2234–2244. doi: 10.1161/01.cir.80.2.234. [DOI] [PubMed] [Google Scholar]
- Horgan J, Bethel H, Carson P, Davidson C, Julian D, Mayou RA, Nagle R. Working party report on cardiac rehabilitation. Br Med J. 1992;67:412–416. doi: 10.1136/hrt.67.5.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organisation Rehabilitation and comprehensive secondary prevention after acute myocardial infarction (EURO Report 1984) Copenhagen: WHO; 1983.
- West R, Pitt B, Desmond J, Pocock S. Clinical Trials in Cardiology London: WB Company Ltd; 1997.
- ISFC Councils on Atherosclerosis, Clinical Cardiology, Epidemiology and Prevention, and Rehabilitation Joint recommendations on secondary prevention for persons with clinical coronary heart disease. Heartbeat. 1984;1:1–8. [Google Scholar]
- Study Group of the European Society of Atherosclerosis Strategy for the prevention of coronary heart disease. Eur Heart J. 1987;8:77–88. [PubMed] [Google Scholar]
- ASPIRE Steering Group A British Cardiac Society survey of the potential for secondary prevention of coronary heart disease. Heart. 1996;75:334–342. doi: 10.1136/hrt.75.4.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeBusk RF, Houston Miller N, Superko R. A case-management system for coronary risk factor modification after acute myocardial infarction. Ann Intern Med. 1994;120:721–729. doi: 10.7326/0003-4819-120-9-199405010-00001. [DOI] [PubMed] [Google Scholar]
- US Department for Health and Human Services Expenditures for the medical care of elderly people living in the community throughout 1980 Washington, DC: US Department of Health and Human Services; 1983 [Health Care Financing Administration Data Report no 4] 1983.
- US Department for Health and Human Services Summary: National Hospital Discharge Survey, Advance Data no 95 (PHS) Washington, DC: US Government Printing Office; 1983 [Publication no 84-1205] 1983.
- Lavie CJ, Milani RV, Litman AB. Benefits of cardiac rehabilitation and exercise training in secondary coronary prevention in the elderly. J Am Coll Cardiol. 1993;22:678–683. doi: 10.1016/0735-1097(93)90176-2. [DOI] [PubMed] [Google Scholar]
- Maeland JG, Mavik OE. Use of health services after myocardial infarction. Scand J Soc Med. 1989;17:93–102. doi: 10.1177/140349488901700114. [DOI] [PubMed] [Google Scholar]
- Sanne H. Exercise tolerance and physical training of non-selected patients after myocardial infarction. Acta Med Scand. 1973;551 (Suppl):1–124. [PubMed] [Google Scholar]
- Bradley F, Morgan S, Smith H. Preventive care for patients following myocardial infarction. Fam Pract. 1997;14:220–226. doi: 10.1093/fampra/14.3.220. [DOI] [PubMed] [Google Scholar]
- Patton M. Qualitative evaluation and research methods Newbury Park, California: Sage; 1999.
- Rochmis P, Blackburn H. Exercise tests: A survey of procedures, safety and litigation experience in approximately 170,000 tests. J Am Med Ass. 1971;217:1061. doi: 10.1001/jama.217.8.1061. [DOI] [PubMed] [Google Scholar]
- Fletcher GF, Balady G, Blair SN, Blumenthal J, Caspersen C, Chaitman B, Epstein S, Sivarjan Froelicher ES, Froelicher VF, Pina IL, Pollock ML. Statement on exercise: benefits and recommendations for physical activity programs for all Americans. Circulation. 1996;94:857–862. doi: 10.1161/01.cir.94.4.857. [DOI] [PubMed] [Google Scholar]
- Pollock ML, Evans WJ. Resistance training for health. The President's Council on Physical fitness and Sports Research Digest, series 2, no 8; December. 1996.
- Sandvik L, Erikssen J, Thaulow E, Erikssen G, Mundal R, Rodahl K. Physical fitness as a predictor of mortality among healthy, middle-aged Norwegian men. N Engl J Med. 1993;328:533–537. doi: 10.1056/NEJM199302253280803. [DOI] [PubMed] [Google Scholar]
- Pollock ML, Carroll JF, Graves JE, Leggett SH, Braith RW, Limacher M, Hagberg JM. Injuries and adherence to walk/jog and resistance training programs in the elderly. Med Sci Sports Exerc. 1991;23:1194–1200. [PubMed] [Google Scholar]
- Yusuf S, Flather M, Pogue , Hunt D, Varigos J, Piegas L, Avezum A, Anderson J, Keltai M, Budaj A, Fox K, Ceremuzynski L. Variations between countries in invasive cardiac procedures and outcomes in patients with suspected unstable angina or myocardial infarction without initial ST elevation. Lancet. 1998;352:507–514. doi: 10.1016/S0140-6736(97)11162-X. [DOI] [PubMed] [Google Scholar]
- Collinson J, Flather MD, Fox KAA, Findlay I, Rodrigues E, Dooley P, Ludman P, Adgey J, Bowker TJ, Matuu R. Clinical outcomes, risk stratification and practice patterns of unstable angina and myocardial infarction without ST elevation: prospective registry of acute ischaemic syndrome in the UK. Eur Heart J. 2000;21:1450–1457. doi: 10.1053/euhj.1999.1995. [DOI] [PubMed] [Google Scholar]
- Dawson-Saunders B, Trapp RG. Basic and Clinical Biostatistics, edn 2 Norwalk, Connecticut: Appleton and Lange; 1994.
- Lachin JM. Properties of simple randomization in clinical trials. Controlled Clin Trials. 1988;9:312. doi: 10.1016/0197-2456(88)90046-3. [DOI] [PubMed] [Google Scholar]
- Lachim JM, Matts JP, Wei LJ. Randomization in clinical trials: conclusions and recommendations. Controlled Clin Trials. 1988;9:365–374. doi: 10.1016/0197-2456(88)90049-9. [DOI] [PubMed] [Google Scholar]
- Pocock S, Simon R. Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Biometrics. 1975;31:103–115. [PubMed] [Google Scholar]
- Press WH. Numerical Recipes in C Cambridge: Cambridge University Press; 1992. p. 280.
- Bradley F, Wiles R, Kinmonth AL. Development and evaluation of complex interventions in health service research: case study of the Southampton heart integrated care project (SHIP). Br Med J. 1999;319:711–715. doi: 10.1136/bmj.318.7185.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51:390–395. doi: 10.1037//0022-006X.51.3.390. [DOI] [PubMed] [Google Scholar]
- Cupples ME, McKnight A. Randomized controlled trial of health promotion in general practice for patients at high cardiovascular risk. Br Med J. 1994;309:993–996. doi: 10.1136/bmj.309.6960.993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- South Tyneside Patient Satisfaction Workshop Who should give lifestyle advice in general practice and what factors influence attendance at health promotion clinics? Br Gen Pract. 1999;31:1009–1104. [PMC free article] [PubMed] [Google Scholar]
- Yusuf S. Randomized controlled trials in cardiovascular disease: past achievements, future challenges. Br Med J. 1999;3119:564–568. doi: 10.1136/bmj.319.7209.564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walden CE, Retzlaf BM, Buck BL. Lipoprotein lipid response to the National Cholesterol Education Program Step II Diet by hypercholesterolemic and combined hyperlipidemic women and men. Arterioscler Thromb Vasc Biol. 1997;17:375–382. doi: 10.1161/01.atv.17.2.375. [DOI] [PubMed] [Google Scholar]
- Summary of the second report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. J Am Med Ass. 1993;269:3015–3023. doi: 10.1001/jama.269.23.3015. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services Reducing the Health Consequences of Smoking: 25 Years of Progress A Report of the Surgeon General Washington, DC: Office on Smoking and Health; 1989 [US Department of Health and Human Services publication CDC 89-8411] 1989.
- Krupski WC. The peripheral vascular consequences of smoking. Ann Vasc Surg. 1991;5:291–304. doi: 10.1007/BF02329389. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services The Health Benefits of Smoking Cessation A Report of the Surgeon General Washington, DC: Office on Smoking and Health; 1990 [US Department of Health and Human Services publication CDC 90-8416] 1990.
- Timmreck TC, Randolph JF. Smoking cessation: clinical steps to improve compliance. Geriatrics. 1993;48:63–70. [PubMed] [Google Scholar]
- Rose G, Colwell L. Randomized controlled trial of anti-smoking advice: final results. J Epidemiol Community Health. 1992;46:65–77. doi: 10.1136/jech.46.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly LE, Mulcahy R, Graham IM, Hickey N. Long-term effect on mortality of stopping smoking after unstable angina and myocardial infarction. Br Med J. 1963;287:324–326. doi: 10.1136/bmj.287.6388.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Clemente CC, Prochaska JO, Fairhurst SK, Velicer WF, Velasues MM, Rossi JS. The process of smoking cessation: an analysis of precontemplation, contemplation and preparation stages of change. J Consult Clin Psychol. 1991;59:295–304. doi: 10.1037//0022-006X.59.2.295. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51:390–395. doi: 10.1037//0022-006X.51.3.390. [DOI] [PubMed] [Google Scholar]
- Lando HA. A factorial analysis of pregnation, aversion, and maintenance in the elements of smoking. Addict Behav. 1982;7:143–154. doi: 10.1016/0306-4603(82)90039-9. [DOI] [PubMed] [Google Scholar]
- Nett LM. The physician's role in smoking cessation. A present and future agenda. Chest. 1990;97 (Suppl):28–32. [PubMed] [Google Scholar]
- Kararck TW, Lichtenstein E. Program adherence and coping strategies as predictors of success in a smoking treatment program. Health Psychol. 1988;7:557–574. doi: 10.1037//0278-6133.7.6.557. [DOI] [PubMed] [Google Scholar]
- Frank E, Winkleby MA, Altman DG, Rockhill B, Fortmann SP. Predictors of physicians' smoking cessation advice. J Am Med Ass. 1991;266:3139–3144. doi: 10.1001/jama.266.22.3139. [DOI] [PubMed] [Google Scholar]
- Kottke TE, Battista RN, DeFriese GH, Brekke ML. Attributes of successful smoking cessation interventions in medical practice: a meta-analysis of 39 controlled trials. J Am Med Ass. 1988;259:2883–2889. doi: 10.1001/jama.259.19.2883. [DOI] [PubMed] [Google Scholar]
- Subcommittee on Exercise/Rehabilitation Standards for supervised cardiovascular exercise maintenance programs. Circulation. 1980;62:669A–672A. [PubMed] [Google Scholar]
- Astrand PO, Rodahl K. Textbook of work physiology New York, McGraw-Hill; 1970. pp. 613–627.
- Mitchell JH, Blomquist G. Maximal oxygen uptake. New Engl J Med. 1971;284:1018–1022. doi: 10.1056/NEJM197105062841809. [DOI] [PubMed] [Google Scholar]
- Cortes CW, Findley TW, Cavalieri T. Analyses of Predicted and Actual Metabolic Equivalents in the Frail Older Adult with Chronic Disease. Greenville, NC: East Carolina University; http://www.css.edu/users/tboone2/asep/jan13.htm.
- Golding L, Myers C, Sinning W. The Y's way to physical fitness: the complete guide to fitness testing and instruction IL: Human Kinetics; 1989.
- Borg G. In Psychophysical Judgement and the Process of Perception Edited by Geisler HG, Petzold P Berlin: VEB Deutscher Verlag Wissenschaften; 1982. pp. 25–34.
- Heller RF, Knapp JC, Valenti LA. Secondary prevention after acute myocardial infarction. Am J Cardiol. 1993;72:759–762. doi: 10.1016/0002-9149(93)91058-p. [DOI] [PubMed] [Google Scholar]
- Lim L, Valenti L, Knapp J. A self-administered quality-of-life questionnaire after acute myocardial infarction. J Clin Epidemiol. 1993;46:1249–1256. doi: 10.1016/0895-4356(93)90089-j. [DOI] [PubMed] [Google Scholar]
- Oldridge N, Guyatt G, Jones N, Crowe J, Singer J, Feeny D, McKelvie R, Runions J, Streiner D, Torrance G. Effects on quality of life with comprehensive rehabilitation after acute myocardial infarction. Am J Cardiol. 1991;67:1084–1089. doi: 10.1016/0002-9149(91)90870-q. [DOI] [PubMed] [Google Scholar]