Abstract
Background
The direct costs associated with menopausal and postmenopausal symptoms (hereafter “menopausal symptoms”) may include the costs of physician and emergency department visits, medications, laboratory testing, and the management of side effects. However, much remains unknown about the costs related to menopausal symptoms, including how they compare with the costs of other diseases that are common among menopausal women.
Objective
To compare the economic burden of menopausal symptoms with other select prevalent chronic conditions among a nationally representative sample of US menopausal women aged 45 to 65 years.
Methods
Women aged 45 to 65 years who have not had a hysterectomy and who participated in the 2010–2012 Medical Expenditure Panel Survey Household Component were included in the analysis. We estimated the direct costs of care associated with the management of menopausal symptoms and compared them with the direct costs of care for other indications, including osteoporosis, influenza, disorders of lipid metabolism, essential hypertension, mood disorders, esophageal disorders, headache, osteoarthritis, urinary tract infections, asthma, glaucoma, anxiety disorder, diabetes, chronic obstructive pulmonary disease/bronchiectasis, and cataract. Regression analyses were used to estimate the differences in direct costs, which included total expenditures and charges for inpatient, outpatient, and emergency department visits.
Results
The annual per-patient direct cost of menopausal symptoms was $248 in 2010–2012 dollars. Based on the modeled costs, menopausal symptoms were associated with significantly higher annual costs than osteoporosis, disorders of lipid metabolism, and esophageal disorders; and these annual costs were comparable to those of influenza, asthma, anxiety disorder, essential hypertension, and headache. The direct costs associated with the management of menopausal symptoms were significantly lower than the direct costs associated with osteoarthritis, mood disorders, chronic obstructive pulmonary disease/bronchiectasis, urinary tract infections, diabetes, glaucoma, and cataract.
Conclusion
The direct costs of care for menopausal symptoms are substantial and are similar to or greater than the direct healthcare costs associated with a number of medical conditions often requiring medical attention in menopausal women.
Keywords: direct cost of care, healthcare costs, hysterectomy, Medical Expenditure Panel Survey data, menopause
More than 6 million women in the United States experience menopausal and postmenopausal symptoms (hereafter “menopausal symptoms”) annually.1 Vasomotor symptoms (VMS; eg, hot flushes and night sweats) occur in approximately 56% to 88% of women in the United States during and/or after the menopausal transition,2–4 lasting for a median of approximately 7 to 10 years.5,6 Although VMS may be infrequent and/or mild in some patients, 24% of women with hot flushes experience them daily (and often multiple times daily), and 20% experience night sweats every night.4 The genitourinary symptoms of menopause may include vaginal dryness, itching, pain with intercourse, tissue fragility, decreased elasticity and vaginal rugae, increased vaginal pH and parabasal cells, as well as urinary urgency or frequency, and recurrent urinary tract infections (UTIs).7 A total of 45% of postmenopausal US women experience vulvar-vaginal symptoms,8 which can be progressive and may not resolve without treatment.9 Menopausal symptoms significantly reduce mental and physical quality-of-life scores, negatively affect personal and intimate relationships, decrease occupational productivity, and impair daily activities.10,11 According to a recent analysis, the adverse psychological impact of moderately and severely bothersome menopausal symptoms on general well-being is comparable to that experienced with housing insecurity (ie, lack of confidence about continuing to afford one's current living accommodation).12 This illustrates the importance of evaluating the burden of menopausal symptoms on individual women, their families, and society.
KEY POINTS
-
▸
Menopausal and postmenopausal symptoms (hereafter “menopausal symptoms”) are costly and negatively affect quality-of-life issues, personal and intimate relationships, and productivity.
-
▸
This retrospective study assessed the direct costs of care associated with menopausal symptoms versus the direct costs of care of 15 other health conditions in women aged 45–65 years who have not had a hysterectomy.
-
▸
The mean annual per-patient direct cost of menopausal symptoms was $248, excluding the cost of prescription medications.
-
▸
The mean annual per-patient direct costs of the comparator conditions ranged from $26 for osteoporosis to $3440 for cataract.
-
▸
The direct cost of care for menopausal symptoms was significantly higher than the costs associated with osteoporosis, lipid metabolism disorders, and esophageal disorders.
-
▸
Treating moderate-to-severe vasomotor symptoms with hormone therapy may be cost-effective in younger menopausal women.
Women with bothersome menopausal symptoms often seek healthcare intervention for these symptoms. In a cross-section US population–based survey of 4402 women aged 40 to 65 years, approximately 60% said they had consulted a healthcare provider regarding menopausal symptoms, and the proportion who had sought such care increased with age.13 A majority (61.4%) of the women who participated in the survey reported using some type of treatment for menopausal symptoms (ie, hormone therapy or complementary/alternative therapy), and approximately 60% of the overall survey population reported lifetime use of hormone therapy.13 Treatment with hormone therapy completely resolved the symptoms in only a small proportion of patients (VMS, 21.3%; vaginal symptoms, 11.8%); no data were collected on whether treatment reduced the severity of symptoms,13 which may be a more clinically important outcome.
These figures likely represent conservative estimates of the affected number of women, because it is probable that some women either do not seek help from a healthcare professional for menopausal problems,14 or they mention only some of their symptoms (eg, VMS, sleeping difficulties), but not others, to their healthcare providers, possibly because of embarrassment or confusion about their available treatment options.15
Menopausal symptoms impose an increased economic burden on women and society, reflecting the direct costs of physician and emergency department visits, prescription and over-the-counter medications, laboratory analyses, and the management of medication side effects.16,17 In one analysis, the total health expenditures for menopausal symptoms were estimated at $3 billion annually in the United States.1 In another analysis, the annual direct costs of VMSs were estimated at $1346 per person, and the annual indirect costs, primarily resulting from absenteeism, were estimated at $770 per person.17 Other indirect costs may include the loss of productivity at work (ie, presenteeism) or at home, increased energy use for air conditioning and laundry, and hygiene-related personal costs.16 In another analysis comparing women who had no menopausal symptoms with those who did, the women with menopausal symptoms had $1343 higher overall direct costs, $457 higher prescription drug costs, $48 more sick leave costs, 0.27 more sick leave days annually, lower hourly productivity rates by 2 units of work, and lower annual productivity rates by 2600 units of work.18
Much remains unknown about the direct and indirect costs of healthcare for managing menopausal symptoms, including how the costs compare with those of other diseases that are prevalent among the menopausal population. Because menopausal symptoms are often transient and are perceived to be part of a natural biologic process, it is possible that clinicians manage these symptoms less aggressively than other medical conditions, which may ultimately limit the costs of care relative to other conditions.
Although economic data regarding various other common conditions are available, comparisons of costs between studies are difficult, because available studies differ with regard to the populations enrolled, methodologies used, symptom severity, and time period conducted. To address this gap, this current study was performed to assess the economic burden of managing patients with menopausal symptoms relative to other chronic conditions that are prevalent among a nationally representative sample of US women of menopausal age (45–65 years).
Methods
The Household Component of the Medical Expenditure Panel Survey (MEPS-HC) is an annual survey of the civilian, noninstitutionalized US population that is sponsored by the Agency for Healthcare Research and Quality.19 The MEPS-HC collects data regarding the health services that Americans use and how often they use them, the costs of these services, and the method by which health services are paid, as well as the cost and scope of health insurance available to Americans.20
The MEPS-HC samples individuals from a nationally representative subsample of households that participated in the previous year's National Health Interview Survey, to form a nationally representative cohort.19,20 Data relating to demographics, health conditions, healthcare utilization and costs, and health insurance status are collected per household and per individual, and are supplemented by data from the individuals' medical providers.20 MEPS-HC uses an overlapping panel design, such that a new panel of sample households is selected annually, and each panel contributes data via 5 rounds of interviews conducted over a 2.5-year period.19 For these analyses, we extracted and pooled data from the 2010, 2011, and 2012 MEPS-HC databases, which at the time of this study were the 3 most recent years with cost data available.21
Based on expert clinical opinion (of one of the authors), 28 conditions common to menopausal women were selected from the full set of MEPS Clinical Classification Code (CCC) classifications. Of the initial 28 conditions selected by the clinical expert, 8 conditions were excluded because of an insufficient number of patients in the MEPS data set to permit analysis. Five other conditions were excluded, because they were acute conditions that were deemed to be poorly comparable to menopausal symptoms, which are of longer duration, and/or because they were known to be extremely costly to treat (eg, cancer) relative to the costs of the other conditions and therefore would not contribute meaningfully to the cost continuum.
Study Population
The principal subgroup of the study population consisted of women aged 45 to 65 years who have not had a hysterectomy and had self-reported menopausal symptoms (MEPS CCC 173) as a reason for a prescription drug claim or a medical event. We also identified women aged 45 to 65 years who have not had a hysterectomy and had any of the following 15 comparator conditions listed as a self-reported medical condition, the only reason for a particular prescription drug claim, or as any reason for a medical event, including osteoporosis (CCC 206), influenza (CCC 123), disorders of lipid metabolism (CCC 53), essential hypertension (CCC 98), mood disorders (bipolar and depressive disorders; CCC 657), esophageal disorders (including, among others, esophageal varices, hemorrhage, and reflux; CCC 138), headache (including migraine; CCC 84), osteoarthritis (CCC 203), UTI (CCC 159), asthma (CCC 128), glaucoma (CCC 88), anxiety disorder (CCC 651), diabetes mellitus (with complications, CCC 50; without complications, CCC 49), chronic obstructive pulmonary disease (COPD) and bronchiectasis (CCC 127), and cataract (CCC 86). Each of these categories encompasses multiple International Classification of Diseases, Ninth Revision, Clinical Modification codes (see Appendix Table at www.AHDBonline.com).
These comparators were included solely to place the relative magnitude of the costs of treatment of menopausal symptoms into perspective along a continuum of direct costs. Comparators were chosen as being representative of a range of conditions that often affect menopausal women.
Women were included if they had ≥1 of the comparator conditions and/or menopausal symptoms and contributed CCC-specific cost data for each applicable category. The analysis population was limited to women who had experienced natural menopause (ie, they had not had a hysterectomy), because hysterectomized women with surgically induced menopause might have different underlying comorbid conditions (eg, increased rate of urinary incontinence22) and other factors driving healthcare costs that could potentially confound the analysis.
Statistical Analyses
The sociodemographic characteristics, including age, race/ethnicity, insurance status, highest level of education attained at the time of the survey, and household income as a percent of the federal poverty line, were extracted from the MEPS full-year consolidated data file (HC-121), summarized descriptively as means and/or percentages, and used as covariates in the modeling of direct costs. Women who were missing any of these covariates were excluded from the descriptive statistics and the modeled analyses.
We calculated the direct healthcare utilization costs associated with the treatment of menopausal symptoms and each of the 15 comparator conditions from MEPS data in 2010, 2011, and 2012 US dollars, without adjustments for inflation. In addition, we averaged the direct costs, including expenditures and charges associated with inpatient medical events, outpatient care, emergency department visits, and office-based provider visits, to assess descriptively the mean and range of the direct per-patient costs per condition. Only costs associated with the conditions of interest were included. However, because the primary condition associated with each visit is not identified in the MEPS database, the costs reflect the total costs of each office visit that included a code for menopausal symptoms or the comparator conditions rather than costs attributable to a particular diagnosis.
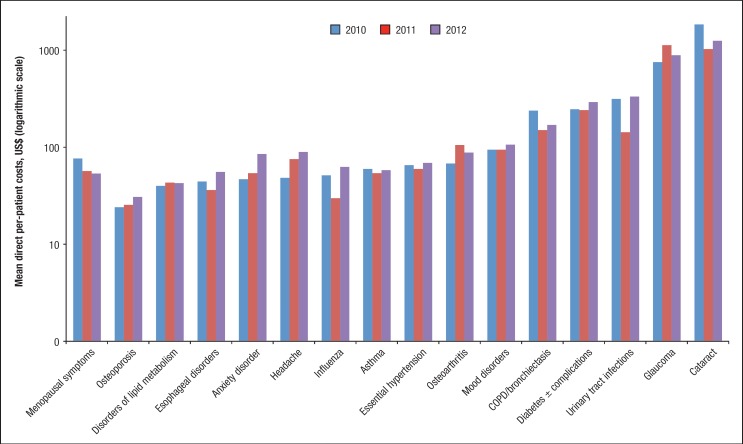
Because pharmaceutical treatment paradigms across these conditions are not comparable, and MEPS 2010–2012 data did not provide an account of nonprescription drug use, the costs associated with prescription and nonprescription medications were not included in our direct-cost calculation. In addition, no indirect costs were included in the calculation, because MEPS does not collect such data. For the sensitivity analysis, we reviewed the cost data for the 3 individual years, which were similar (Figure 1). This was determined to support pooling of the cost data for the primary analysis.
Figure 1. Sensitivity Analysis: Direct Per-Patient Costs of Menopausal Symptoms and Select Comparators for 2010–2012 (Modeled Costs).
We compared the direct costs of the 15 selected comparator conditions with the direct costs of menopausal symptoms using a (natural) log-linear regression model. In this model, $1 was added to the direct costs of every person to allow log-transformation to be applied to persons with zero cost. Log-transformed direct cost was used as the outcome, and the condition (ie, menopausal symptoms and each comparator condition) as a predictor adjusting for age, race/ethnicity, insurance status, income, and education.
All covariates were represented by categorical variables to avoid imposing a linear relationship between the outcome and the predictors. Based on this model, the differences in the least square means were estimated over the balanced population.
We calculated the predicted dollar cost differences using a simple lognormal regression analysis with back-transformation of the estimated least square means, as , where Єi represents a random error component following a Gaussian distribution mean 0 and constant variance σ2. The addition of $1 to the original cost sets the log-transformed cost to $0 when the original cost is $0. If costs are log-normally distributed, then the average cost on the untransformed scale is a function of the mean and the variance on the transformed scale, and the predicted mean cost on the original scale is
Results
Cost data were available in the 2010, 2011, and 2012 MEPS databases from 401 women with menopausal symptoms, 1370 with diabetes, 2525 with lipid metabolism disorders, 856 with headache, 164 with cataract, 148 with glaucoma, 3515 with essential hypertension, 578 with influenza, 697 with COPD/bronchiectasis, 869 with asthma, 822 with esophageal disorders, 484 with UTIs, 927 with osteoarthritis, 1105 with osteoporosis, 1231 with anxiety disorders, and 1491 with mood disorders (see Appendix Figure at www.AHDBonline.com).
Table 1 provides demographic data for the women included in the modeled analysis. Compared with women who had one of the comparator conditions, women with menopausal symptoms were more likely to be white and to have health insurance, a higher level of education, and a higher household income level; in addition, women with menopausal symptoms had a lower proportion at the upper end of the age range (61–65 years) compared with all comparators except headache. Any variations among groups with regard to age, ethnicity/race, insurance status, education level, and income were subsequently adjusted for in the analyses.
Table 1.
| Patient characteristic |
Menopausal symptoms (N = 383) |
Diabetesc (N = 1292) |
Disorders of lipid metabolism (N = 2398) |
Headache (N = 806) |
Cataract (N = 158) |
Glaucoma (N = 143) |
Essential hypertension (N = 3313) |
Influenza (N = 515) |
| Age, yrs, mean (SD) | 53.6 (5.2) | 55.8 (5.9) | 56.1 (5.8) | 52.8 (5.6) | 59.6 (5.4) | 57.0 (5.7) | 55.3 (6.0) | 54.3 (5.8) |
| 45–50, % | 30.3 | 24.0 | 21.3 | 41.2 | 8.9 | 17.5 | 26.5 | 30.7 |
| 51–55, % | 37.1 | 22.2 | 22.7 | 26.4 | 11.4 | 21.7 | 23.7 | 27.0 |
| 56–60, % | 20.4 | 27.2 | 28.6 | 20.7 | 21.5 | 28.0 | 25.1 | 23.7 |
| 61–65, % | 12.3 | 26.6 | 27.4 | 11.7 | 58.2 | 32.9 | 24.6 | 18.6 |
| Race/ethnicity, % | ||||||||
| White | 68.7 | 31.9 | 46.1 | 52.9 | 53.8 | 42.7 | 37.5 | 56.9 |
| Black | 12.3 | 25.7 | 19.7 | 16.0 | 23.4 | 28.0 | 29.6 | 11.3 |
| Asian | 3.1 | 6.8 | 7.7 | 6.0 | 7.6 | 9.8 | 7.3 | 6.2 |
| Hispanic | 14.9 | 32.4 | 24.5 | 23.9 | 12.7 | 18.9 | 23.5 | 23.1 |
| Other | 1 | 3.2 | 2 | 1.2 | 2.5 | 0.7 | 2.0 | 2.5 |
| Insured, % | 82.2 | 72.5 | 77.7 | 79.7 | 86.1 | 76.2 | 73.6 | 73.6 |
| Education, mean, yrs (SD) | 13.9 (2.7) | 11.5 (4.0) | 12.3 (3.8) | 13.0 (3.5) | 13.2 (3.6) | 12.8 (3.9) | 12.2 (3.7) | 13.1 (3.7) |
| Less than high school, % | 6 | 30.7 | 22.9 | 17.9 | 19.0 | 20.3 | 23.4 | 15.3 |
| GED/high school diploma, % | 48 | 46.4 | 46.2 | 41.6 | 36.1 | 37.8 | 47.9 | 43.9 |
| Bachelor's, % | 23 | 11.2 | 15.4 | 19.5 | 25.9 | 13.3 | 14.4 | 22.1 |
| Master's or above, % | 23 | 11.8 | 15.6 | 21.5 | 19.0 | 28.7 | 14.4 | 19.0 |
| Income, US$, mean (SD) | 37,804 (36,401) | 23,314 (27,235) | 28,296 (31,691) | 32,754 (34,409) | 34,839 (37,652) | 29,068 (32,387) | 26,370 (28,242) | 32,929 (32,549) |
| Relative to federal poverty level, % | ||||||||
| <100 | 11 | 24.7 | 20.4 | 16.3 | 22.8 | 25.9 | 20.6 | 12.8 |
| 100 to <125 | 2.6 | 7.2 | 5.2 | 4.2 | 5.1 | 5.6 | 6.5 | 2.9 |
| 125 to <200 | 11.5 | 16.6 | 15.3 | 15.3 | 9.5 | 14.0 | 16.4 | 16.9 |
| 200 to <400 | 26.9 | 29.1 | 28.0 | 30.6 | 21.5 | 23.8 | 28.9 | 28.0 |
| ≥400 | 48 | 22.4 | 31.1 | 33.6 | 41.1 | 30.8 | 27.6 | 39.4 |
|
COPD and bronchiectasis (N = 667) |
Asthma (N = 820) |
Esophageal disorders (N = 786) |
UTIs (N = 453) |
Osteoarthritis (N = 884) |
Osteoporosis (N = 1051) |
Anxiety disorders (N = 1170) |
Mood disorders (N = 1431) |
|
| Age, yrs, mean (SD) | 55.0 (5.8) | 54.4 (5.7) | 55.2 (6.0) | 53.9 (6.0) | 56.6 (5.6) | 56.8 (5.6) | 54.0 (5.8) | 53.9 (5.6) |
| 45–50, % | 26.5 | 30.7 | 27.2 | 34.7 | 18.4 | 17.3 | 32.8 | 32.0 |
| 51–55, % | 25.6 | 25.9 | 22.5 | 23.6 | 22.5 | 21.6 | 28.0 | 29.3 |
| 56–60, % | 27.4 | 25.7 | 27.0 | 26.3 | 28.2 | 28.8 | 22.5 | 24.0 |
| 61–65, % | 20.4 | 17.7 | 23.3 | 15.5 | 30.9 | 32.3 | 16.7 | 14.7 |
| Race/ethnicity, % | ||||||||
| White | 59.4 | 49.6 | 57.4 | 56.5 | 57.5 | 57.8 | 62.1 | 58.8 |
| Black | 16.9 | 19.0 | 21.8 | 14.1 | 19.5 | 17.0 | 12.1 | 15.2 |
| Asian | 1.8 | 6.1 | 3.4 | 3.1 | 3.1 | 5.0 | 2.6 | 3.1 |
| Hispanic | 18.3 | 21.1 | 15.0 | 24.1 | 17.2 | 17.7 | 20.9 | 20.5 |
| Other | 3.6 | 4.1 | 2.4 | 2.2 | 2.8 | 2.5 | 2.4 | 2.4 |
| Insured, % | 77.2 | 78.5 | 86.0 | 79.7 | 78.7 | 80.1 | 77.6 | 77.4 |
| Education, mean (SD), yrs | 12.9 (3.0) | 12.9 (3.3) | 12.7 (3.1) | 12.9 (4.0) | 13.2 (3.1) | 13.2 (3.2) | 13.1 (3.2) | 12.7 (3.3) |
| Less than high school, % | 15.9 | 20.7 | 19.7 | 18.8 | 14.6 | 14.7 | 16.7 | 20.0 |
| GED/high school diploma, % | 51.0 | 44.8 | 49.0 | 43.0 | 47.4 | 45.1 | 46.4 | 47.9 |
| Bachelor's, % | 18.1 | 16.8 | 13.1 | 19.2 | 18.8 | 20.4 | 19.0 | 15.9 |
| Master's or above, % | 15.4 | 17.9 | 18.6 | 19.2 | 19.5 | 20.0 | 18.0 | 16.3 |
| Income, US$, mean (SD) | 26,702 (28,170) | 27,775 (32,983) | 29,361 (33,727) | 32,756 (33,132) | 29,578 (34,147) | 30,564 (34,117) | 31,056 (34,631) | 27,378 (30,950) |
| Relative to federal poverty level, % | ||||||||
| <100 | 21.4 | 26.0 | 25.6 | 14.1 | 19.7 | 18.1 | 21.4 | 27.1 |
| 100 to <125 | 5.8 | 4.9 | 5.7 | 4.2 | 4.8 | 4.4 | 5.0 | 5.2 |
| 125 to <200 | 15.3 | 16.1 | 12.1 | 14.1 | 15.4 | 15.9 | 14.5 | 13.3 |
| 200 to <400 | 29.1 | 25.0 | 25.1 | 29.8 | 27.0 | 26.4 | 26.8 | 26.6 |
| ≥400 | 28.3 | 28.0 | 31.6 | 37.7 | 33.1 | 35.3 | 32.2 | 27.9 |
NOTE: The study included women aged 45 to 65 years who had not had a hysterectomy and had menopausal symptoms or any of 15 comparator conditions and participated in the 2010, 2011, and/or 2012 MEPS-HC (descriptive statistics, pooled).
Data shown here are for women who were included in the modeled data analysis; some women who contributed direct cost data (see Appendix Table at www.AHDBonline.com) were excluded from the analysis if any of the covariate data were missing.
Percentages may not total 100 because of rounding.
Diabetes with/without complications, combined.
COPD indicates chronic obstructive pulmonary disease; GED, General Educational Development; MEPS-HC, Medical Expenditure Panel Survey Household Component; SD, standard deviation; UTIs, urinary tract infections.
Direct Healthcare Costs (Descriptive Statistics)
Excluding the costs of prescription medications, the mean annual per-patient direct cost of treating menopausal symptoms was $248. The mean annual per-patient direct costs of the comparator conditions ranged from $26 for osteoporosis to $3440 for cataract (Table 2).
Table 2.
Per-Patient Direct Costs of Menopausal Symptoms and 15 Comparator Conditions
| Mean (SD), median (range) annual direct per-patient costs, US$a | |||||
|---|---|---|---|---|---|
| Condition | Inpatient visits | Outpatient visits | Emergency department visits | Office-based medical provider visits | Total |
| Menopausal symptoms (N = 401) | 0 (0) 0 (0–0) | 74 (720) 0 (0–8919) |
20 (320) 0 (0–6046) |
153 (581) 0 (0–6480) |
248 (1021) 0 (0–9575) |
| Diabetes ± complications (N = 1370) | 370 (5983) 0 (0–130,809) |
95 (1017) 0 (0–22,577) |
61 (965) 0 (0–31,382) |
1249 (17,130) 0 (0–441,684) |
1776 (18,671) 0 (0–446,231) |
| Disorders of lipid metabolism (N = 2525) | 4 (203) 0 (0–10,214) |
11 (249) 0 (0–11,289) |
0 (0) 0 (0–0) |
76 (665) 0 (0–28,236) |
91 (739) 0 (0–28,236) |
| Headache (N = 856) | 122 (2904) 0 (0–81,839) |
50 (467) 0 (0–5862) |
158 (1308) 0 (0–21,138) |
156 (772) 0 (0–11,905) |
486 (3737) 0 (0–97,932) |
| Cataract (N = 164) | 155 (1984) 0 (0–25,401) |
1287 (5237) 0 (0–40,308) |
0 (0) 0 (0–0) |
1998 (5671) 96 (0–46,632) |
3440 (7779) 186 (0–46,632) |
| Glaucoma (N = 148) | 0 (0) 0 (0–0) |
215 (1910) 0 (0–21,208) |
0 (0) 0 (0–0) |
671 (1367) 199 (0–10,105) |
885 (2400) 199 (0–22,542) |
| Essential hypertension (N = 3515) | 52 (1236) 0 (0–46,719) |
14 (306) 0 (0–13,616) |
77 (940) 0 (0–25,635) |
109 (609) 0 (0–20,586) |
252 (1976) 0 (0–63,516) |
| Influenza (N = 578) | 0 (0) 0 (0–0) |
5 (78) 0 (0–1425) |
26 (331) 0 (0–4973) |
55 (233) 0 (0–2659) |
86 (417) 0 (0–4973) |
| COPD/bronchiectasis (N = 697) | 2110 (32,116) 0 (0–642,742) |
53 (528) 0 (0–10,657) |
113 (630) 0 (0–6624) |
337 (3118) 0 (0–78,150) |
2614 (32,395) 0 (0–646,045) |
| Asthma (N = 869) | 213 (2765) 0 (0–42,549) |
57 (1227) 0 (0–35,487) |
202 (1999) 0 (0–36,541) |
137 (1182) 0 (0–32,012) |
607 (4038) 0 (0–51,095) |
| Esophageal disorders (N = 822) | 88 (2176) 0 (0–61,481) |
170 (1928) 0 (0–43,106) |
89 (917) 0 (0–16,580) |
169 (1252) 0 (0–24,762) |
516 (3328) 0 (0–61,481) |
| Urinary tract infections (N = 484) | 59 (950) 0 (0–18,177) |
14 (192) 0 (0–3960) |
207 (1156) 0 (0–13,122) |
310 (1796) 0 (0–32,326) |
591 (2357) 0 (0–32,326) |
| Osteoarthritis (N = 927) | 475 (6098) 0 (0–93,794) |
115 (1391) 0 (0–28,880) |
31 (477) 0 (0–9767) |
382 (1956) 0 (0–40,187) |
1002 (6863) 0 (0–104,853) |
| Osteoporosis (N = 1105) | 0 (0) 0 (0–0) |
5 (96) 0 (0–2382) |
0 (0) 0 (0–0) |
20 (173) 0 (0–2832) |
26 (219) 0 (0–4474) |
| Anxiety disorder (N = 1231) | 288 (3768) 0 (0–77,249) |
5 (141) 0 (0–4788) |
63 (681) 0 (0–12,849) |
264 (2294) 0 (0–68,898) |
620 (4506) 0 (0–77,249) |
| Mood disorder (N = 1491) | 173 (3090) 0 (0–105,118) |
72 (1339) 0 (0–42,330) |
18 (366) 0 (0–12,197) |
452 (2037) 0 (0–36,753) |
714 (4399) 0 (0–125,423) |
NOTE: The costs were of women aged 45 to 65 years who had not had a hysterectomy and who participated in the 2010, 2011, and/or 2012 MEPS-HC (descriptive statistics, pooled).
Costs are rounded to the nearest dollar.
COPD indicates chronic obstructive pulmonary disease; MEPS-HC, Medical Expenditure Panel Survey Household Component; SD, standard deviation.
Office-based medical provider visits accounted for a majority (62%) of the costs of menopausal symptoms. The same was true for most conditions, although the costs of COPD/bronchiectasis, osteoarthritis, and anxiety disorder were more heavily driven by inpatient visits; the cost of esophageal disorders was driven by a combination of outpatient and office visits; and the costs of headache and asthma were more closely distributed between inpatient, office, and emergency department visits (Table 2).
Estimated Healthcare Cost Differences
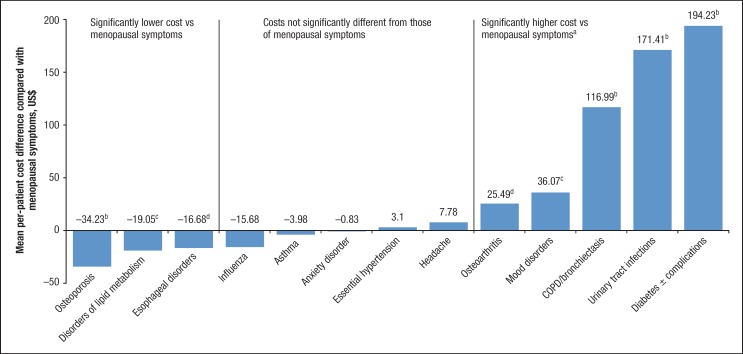
In the model-based results, the estimated mean annual per-patient direct cost of care for menopausal symptoms ($75) was significantly higher than those for osteoporosis ($24), lipid metabolism disorders ($39), and esophageal disorders ($44) in women aged 45 to 65 years (Figure 2). The cost of menopausal symptoms was relatively similar to those of influenza ($50), asthma ($59), anxiety disorder ($46), essential hypertension ($64), and headache ($48) in this population. The conditions associated with significantly higher costs than menopausal symptoms included osteoarthritis ($67), mood disorders ($93), COPD/bronchiectasis ($234), UTI ($309), diabetes ($242), glaucoma ($740), and cataract ($1807; Figure 2).
Figure 2. Estimated Differences in Mean Per-Patient Direct Costs Among US Women with Menopausal Symptoms versus Other Conditions.
Discussion
In this population-based representative sample of US women of menopausal age, the estimated per-patient healthcare expenditures (excluding medication costs) attributable to the management of menopausal symptoms were higher than those associated with osteoporosis, lipid metabolism disorders, and esophageal disorders among women aged 45 to 65 years, controlling for age, race/ethnicity, insurance status, household income, and education. The costs of treating menopausal symptoms were comparable to those of several other prevalent diseases selected for comparison, including influenza, asthma, anxiety disorder, essential hypertension, and headache in this population.
These findings demonstrate that menopausal symptoms, which are known to be associated with considerable decrements in quality of life,16 are also associated with a substantial economic burden relative to other conditions often occurring in the menopausal population. The direct costs of management of menopausal symptoms were largely attributable to office-based medical provider visits, proving that many women consider menopausal symptoms bothersome enough to seek medical attention. This claim is also supported by other analyses.13
The annual direct per-person costs of menopausal symptoms (excluding prescription drug costs) in our analysis ($248) are conservative compared with the costs reported in a recent analysis by Sarrel and colleagues ($423).17 They compared VMS-specific and overall healthcare costs, including prescription drug costs, among 252,273 women who had VMS that were untreated during the 6 months before screening versus the same number of women without VMS. Women in the non-VMS group were matched based on beneficiary status, hysterectomy status, and menopause-related diagnoses, as well as by propensity scores that were determined based on age, region, payer type, employer industry, and year of index date.17
Sarrel and colleagues compiled cost data for a 12-month period beginning from the first VMS diagnosis in the VMS group and a randomly chosen index date in the non-VMS group using insurance claims from the 1999 to 2011 OptumHealth Reporting and Insights Database.17 Women in the VMS group had $1346 higher all-cause annual direct costs and $423 higher annual VMS-specific direct costs than the non-VMS group. The main driver of VMS-related costs was again outpatient visits ($395 higher for women with VMS vs women without VMS) followed by pharmacy costs ($33 higher for women with VMS).17
Although the costs in our analysis are lower than those of Sarrel and colleagues, our findings nonetheless confirmed, using a different claims database, their finding that untreated VMS are potentially costly; our analysis also adds comparative costs for other common conditions. The lower costs found in our analysis compared with those of Sarrel and colleagues may be attributable to differences in the populations studied and the claims databases used, and that we did not include prescription drug claims. (However, given that pharmacy costs were only $33 in their analysis,17 those costs do not account for the entire difference between their results and ours.) The costs in our analysis are expressed in 2010, 2011, and 2012 US dollars without adjustment; in their analysis, all costs were expressed in 2011 US dollars.
A previous study based on the 2000–2002 MEPS database evaluated incremental costs for women with and without various female-specific conditions, including menopausal symptoms, gynecologic disorders, pregnancy-related conditions, female cancers, and benign breast disease, among girls and women aged ≥14 years.1 The results of that study demonstrated that female-specific conditions and disorders substantially increased healthcare utilization and total health expenditures across the life span compared with women without these conditions who were similar in terms of age, race, education, income, and number of chronic conditions.1 Our study extends these findings by comparing healthcare utilization costs associated with the management of menopausal symptoms—which Kjerulff and colleagues found to be most prevalent among middle-aged and older women1—with other specific chronic health conditions among women in this same age-group.
Given the exclusion of prescription and over-the-counter drug costs, our findings may represent a conservative estimate of the total direct costs for all of the conditions studied, including menopausal symptoms. If prescription drug costs had been included, they may have altered the placement of menopause and some of the comparators within the cost continuum. Prescription drugs, which may be underutilized in the treatment of menopausal symptoms, accounted for only 7.8% of the total VMS-specific costs in an analysis by Sarrel and colleagues.23 By contrast, an analysis of medical claims data among women aged 50 to 64 years showed that prescription drugs accounted for $1410 (22.5%) of the $6259 average annual direct costs (in 2000 US dollars) for osteoporosis.24
Osteoarthritis is associated with an excess annual per-patient cost of $10,941, of which medication accounts for $968 (in 2009 US dollars; 8.8%) in women and men of all ages.25 The direct cost associated with major depressive disorder is $2366 per patient (in 2012 US dollars) for men and women aged 18 to 64 years, of which prescription drugs account for approximately $955 (40.4%).26 The annual per-patient medication cost for glaucoma in women is approximately $635 in 2009 US dollars.27 The annual costs of diabetes medications (among women and men) are approximately $148 to $597.28
By comparison, a separate analysis of the costs of medications for VMS reported annual costs of approximately $47 to $591 for oral estrogens, $358 to $658 for transdermal estrogens, and $73 to $1194 for nonhormonal prescription therapies.29 It is possible that better management of some of the comparator conditions via the use of prescription medications accounts for the lower medical costs of these conditions relative to menopausal symptoms in our study.
Despite the sizable direct medical costs of menopausal symptoms, treatment is potentially cost-effective in younger menopausal women. According to the North American Menopause Society (NAMS), the benefits of treating moderate-to-severe VMS with hormone therapy “outweigh the risks for most healthy, symptomatic women aged younger than 60 years or within 10 years of the final menstrual period.”30
Estimates from a computer-based cost-effectiveness model suggested that the use of hormone therapy for 15 years starting at age 50 years resulted in a gain of 1.49 (standard deviation [SD], 0.24) quality-adjusted life-years (QALYs) at a cost (in 2006 US dollars) of $2438 per QALY gained.31 In this population, hormone therapy was considered “a highly cost-effective strategy for improving quality-adjusted life.” By contrast, when hormone therapy initiation was delayed until age 65 years (which is not a strategy recommended by the NAMS),30,32 there was a net loss in QALYs for the first 9 years before the QALYs increased, resulting in a net gain of only 0.11 (SD, 0.23) QALYs at year 15, at a cost of $27,953 per QALY.
The strengths of our analysis include the large number of participants who contributed cost data and that the sample is nationally representative. Another strength is that age, race/ethnicity, insurance status, household income, and education were adjusted for in the statistical model. The between-group variations in such demographic characteristics may be expected in an observational study, because the subjects are not randomly assigned to the study groups as they are in randomized, placebo-controlled trials. However, the adjustments made in our model allowed the estimation of mean costs in a balanced population.
Limitations
The objective of our analysis was to place menopausal symptoms in the context of well-known conditions frequently identified as economically burdensome in this population. It is possible that had we chosen different comparator groups, we would have found the costs of menopausal symptoms to be comparable to additional major conditions. Although our choice of comparator conditions was not exhaustive, the chosen conditions allowed us to provide comparisons with a spectrum of conditions meaningful for patients and physicians alike.
The costs in the current analysis were determined for women aged 45 to 65 years. The costs of some of the comparators may be higher or lower in older or younger women, but the purpose of our analysis was to compare the costs of conditions across a comparably aged population that is most likely to be affected by menopausal symptoms.
Another limitation was a lack of inclusion of prescription drug costs and indirect costs. Menopausal women are typically of working age, and menopausal symptoms have been associated with increased absenteeism and decreased work productivity.18 The costs of work impairment corresponded to the severity of VMS.10 Women may also incur out-of-pocket costs for nonprescription or alternative therapies for menopausal symptoms, which are not reflected in the current analysis. It is unknown how indirect costs and nonprescription drug costs compare for menopause and other common conditions.
Conclusions
Menopause is usually a natural change, and menopausal symptoms are often transient, but they can be long in duration (median of 7–10 years, and potentially lifelong for some women) and are often sufficiently bothersome to prompt women to seek medical intervention. This analysis showed that the annual direct healthcare costs of menopausal symptoms, excluding prescription drug costs, are similar to or greater than the annual direct costs associated with conditions generally understood to require medical attention, including osteoporosis, disorders of lipid metabolism, esophageal disorders, influenza, asthma, anxiety disorders, essential hypertension, and headache, including migraine.
However, comparison with published literature suggests that some of these other conditions are associated with a much higher share of prescription drug costs. A greater use of prescription treatments for those conditions may account for their better management and lower medical costs than for menopausal symptoms.
Future studies should further evaluate whether the treatment of bothersome menopausal symptoms is cost-effective from a societal perspective and whether it reduces indirect costs and improves health-related quality of life. Although there are costs incurred from treating menopausal symptoms, not treating them may prove even more costly.
Acknowledgments
We wish to thank former Pfizer colleagues Arthi Chandran, MS, MPH, for her contribution to the conceptual design and preliminary analyses, and Dan Escudero for his contribution to the development of the manuscript. Lauren Cerruto and Diane M. Sloan, PharmD, provided medical writing support.
This research was supported by the National Institute of Mental Health of the National Institutes of Health under award number T32MH019733. The content is solely the responsibility of the authors and does not necessarily represent the views of the National Institutes of Health.
Source of Funding
This study was sponsored by Pfizer, Inc.
Author Disclosure Statement
Dr Assaf, Mr Bushmakin, and Ms Moffatt are employees and stockholders of Pfizer; Dr Joyce was a paid Fellow with Pfizer through Brown University during the study and is currently a consultant for Precision Health Economics; Dr Louie was an employee and stockholder of Pfizer during the study; Mr Flores was a paid Fellow with Pfizer through Brown University during the manuscript preparation.
Contributor Information
Annlouise R. Assaf, Senior Director, Pfizer Medical, Pfizer, and Adjunct Professor, Brown University, Providence, RI.
Andrew G. Bushmakin, Director of Biostatistics, GIP, Pfizer.
Nina Joyce, Research Fellow, Department of Health Care Policy, Harvard Medical School, Boston, MA.
Michael J. Louie, Senior Medical Director, Women's Health, Pfizer, during the study.
Michael Flores, Predoctoral Fellow, Brown University.
Margaret Moffatt, Manager, Women's Health, Pfizer.
References
- 1. Kjerulff KH, Frick KD, Rhoades JA, Hollenbeak CS. The cost of being a woman: a national study of health care utilization and expenditures for female-specific conditions. Womens Health Issues. 2007; 17:13–21. [DOI] [PubMed] [Google Scholar]
- 2. Gold EB, Colvin A, Avis N, et al. Longitudinal analysis of the association between vasomotor symptoms and race/ethnicity across the menopausal transition: Study of Women's Health Across the Nation. Am J Public Health. 2006; 96:1226–1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Freeman EW, Sammel MD, Sanders RJ. Risk of long-term hot flashes after natural menopause: evidence from the Penn Ovarian Aging Study cohort. Menopause. 2014; 21:924–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Williams RE, Kalilani L, DiBenedetti DB, et al. Frequency and severity of vasomotor symptoms among peri- and postmenopausal women in the United States. Climacteric. 2008; 11:32–43. [DOI] [PubMed] [Google Scholar]
- 5. Avis NE, Crawford SL, Greendale G, et al; for the Study of Women's Health Across the Nation. Duration of menopausal vasomotor symptoms over the menopause transition. JAMA Intern Med. 2015; 175:531–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Freeman EW, Sammel MD, Lin H, et al. Duration of menopausal hot flushes and associated risk factors. Obstet Gynecol. 2011; 117:1095–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Portman DJ, Gass ML; for the Vulvovaginal Atrophy Terminology Consensus Conference Panel. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women's Sexual Health and the North American Menopause Society. Menopause. 2014; 21:1063–1068. [DOI] [PubMed] [Google Scholar]
- 8. Santoro N, Komi J. Prevalence and impact of vaginal symptoms among postmenopausal women. J Sex Med. 2009; 6:2133–2142. [DOI] [PubMed] [Google Scholar]
- 9. Gass ML, Bachman GA, Goldstein SR, et al; for the North American Menopause Society 2013 Symptomatic Vulvovaginal Atrophy Advisory Panel. Management of symptomatic vulvovaginal atrophy: 2013 position statement of The North American Menopause Society. Menopause. 2013; 20:888–902; quiz 903–904. [DOI] [PubMed] [Google Scholar]
- 10. Whiteley J, DiBonaventura MD, Wagner JS, et al. The impact of menopausal symptoms on quality of life, productivity, and economic outcomes. J Womens Health (Larchmt). 2013; 22:983–990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Simon JA, Nappi RE, Kingsberg SA, et al. Clarifying Vaginal Atrophy's Impact on Sex and Relationships (CLOSER) survey: emotional and physical impact of vaginal discomfort on North American postmenopausal women and their partners. Menopause. 2014; 21:137–142. [DOI] [PubMed] [Google Scholar]
- 12. Gartoulla P, Bell RJ, Worsley R, Davis SR. Moderate-severely bothersome vasomotor symptoms are associated with lowered psychological general wellbeing in women at midlife. Maturitas. 2015; 81:487–492. [DOI] [PubMed] [Google Scholar]
- 13. Williams RE, Kalilani L, DiBenedetti DB, et al. Healthcare seeking and treatment for menopausal symptoms in the United States. Maturitas. 2007; 58:348–358. [DOI] [PubMed] [Google Scholar]
- 14. Schonberg MA, Wee CC. Menopausal symptom management and prevention counseling after the Women's Health Initiative among women seen in an internal medicine practice. J Womens Health (Larchmt). 2005; 14:507–514. [DOI] [PubMed] [Google Scholar]
- 15. Cumming GP, Herald J, Moncur R, et al. Women's attitudes to hormone replacement therapy, alternative therapy and sexual health: a web-based survey. Menopause Int. 2007; 13:79–83. [DOI] [PubMed] [Google Scholar]
- 16. Utian WH. Psychosocial and socioeconomic burden of vasomotor symptoms in menopause: a comprehensive review. Health Qual Life Outcomes. 2005; 3:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sarrel P, Portman D, Lefebvre P, et al. Incremental direct and indirect costs of untreated vasomotor symptoms. Menopause. 2015; 22:260–266. [DOI] [PubMed] [Google Scholar]
- 18. Kleinman NL, Rohrbacker NJ, Bushmakin AG, et al. Direct and indirect costs of women diagnosed with menopause symptoms. J Occup Environ Med. 2013; 55:465–470. [DOI] [PubMed] [Google Scholar]
- 19. Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey: MEPS-HC panel design and data collection process. http://meps.ahrq.gov/mepsweb/survey_comp/hc_data_collection.jsp. Accessed July 17, 2015.
- 20. Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey: survey background. http://meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp. Accessed April 1, 2014.
- 21. Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey: MEPS-HC sample sizes. http://meps.ahrq.gov/mepsweb/survey_comp/hc_sample_size.jsp?prfricon=yes. Accessed April 1, 2014.
- 22. Brown JS, Sawaya G, Thom DH, Grady D. Hysterectomy and urinary incontinence: a systematic review. Lancet. 2000; 356:535–539. [DOI] [PubMed] [Google Scholar]
- 23. Sarrel P, Lefebvre P, Lafeuille MH, et al. Incremental direct and indirect cost of untreated vasomotor symptoms (VMS). Menopause. 2013; 20: Abstract S-23. [DOI] [PubMed] [Google Scholar]
- 24. Sasser AC, Rousculp MD, Birnbaum HG, et al. Economic burden of osteoporosis, breast cancer, and cardiovascular disease among postmenopausal women in an employed population. Womens Health Issues. 2005; 15:97–108. [DOI] [PubMed] [Google Scholar]
- 25. Le TK, Montejano LB, Cao Z, et al. Health care costs in US patients with and without a diagnosis of osteoarthritis. J Pain Res. 2012; 5:23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Greenberg PE, Fournier AA, Sisitsky T, et al. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry. 2015; 76:155–162. [DOI] [PubMed] [Google Scholar]
- 27. Lam BL, Zheng DD, Davila EP, et al. Trends in glaucoma medication expenditure: Medical Expenditure Panel Survey 2001–2006. Arch Ophthalmol. 2011; 129:1345–1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zhuo X, Zhang P, Hoerger TJ. Lifetime direct medical costs of treating type 2 diabetes and diabetic complications. Am J Prev Med. 2013; 45:253–261. [DOI] [PubMed] [Google Scholar]
- 29. Williams-Frame A, Carpenter JS. Costs of hormonal and nonhormonal prescription medications for hot flashes. Womens Health (Lond). 2009; 5:497–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Shifren JL, Gass ML; for the NAMS Recommendations for Clinical Care of Midlife Women Working Group. The North American Menopause Society recommendations for clinical care of midlife women. Menopause. 2014; 21:1038–1062. [DOI] [PubMed] [Google Scholar]
- 31. Salpeter SR, Buckley NS, Liu H, Salpeter EE. The cost-effectiveness of hormone therapy in younger and older postmenopausal women. Am J Med. 2009; 122:42–52.e2. [DOI] [PubMed] [Google Scholar]
- 32. North American Menopause Society. The North American Menopause Society statement on continuing use of systemic hormone therapy after age 65. Menopause. 2015; 22:693. [DOI] [PubMed] [Google Scholar]