Abstract
Purpose
To examine nurses’ self-reported use of race in clinical evaluation.
Design
This cross-sectional study analyzed data collected from three separate studies using the Genetics and Genomics in Nursing Practice Survey, which includes items about use of race and genomic information in nursing practice. The Racial Attributes in Clinical Evaluation (RACE) scale was used to measure explicit clinical use of race among nurses from across the United States.
Methods
Multivariate regression analysis was used to examine associations between RACE score and individual-level characteristics and beliefs in 5,733 registered nurses.
Findings
Analysis revealed significant relationships between RACE score and nurses’ race and ethnicity, educational level, and views on the clinical importance of patient demographic characteristics. Asian nurses reported RACE scores 1.41 points higher than White nurses (p < .001), and Black nurses reported RACE scores 0.55 points higher than White nurses (p < .05). Compared to diploma-level nurses, the baccalaureate-level nurses reported 0.69 points higher RACE scores (p < .05), master’s-level nurses reported 1.63 points higher RACE scores (p < .001), and doctorate-level nurses reported 1.77 points higher RACE scores (p < .01). In terms of clinical importance of patient characteristics, patient race and ethnicity corresponded to a 0.54-point increase in RACE score (p < .001), patient genes to a 0.21-point increase in RACE score (p < .001), patient family history to a 0.15-point increase in RACE score (p < .01), and patient age to a 0.19-point increase in RACE score (p < .001).
Conclusions
Higher reported use of race among minority nurses may be due, in part, to differential levels of racial self-awareness. A relatively linear positive relationship between level of nursing degree nursing education and use of race suggests that a stronger foundation of knowledge about genetic ancestry, population genetics and the concept “race” and genetic ancestry may increase in clinical decision making could allow nurses to more appropriately use of race in clinical care. Integrating patient demographic characteristics into clinical decisions is an important component of nursing practice.
Clinical Relevance
Registered nurses provide care for diverse racial and ethnic patient populations and stand on the front line of clinical care, making them essential for reducing racial and ethnic disparities in healthcare delivery. Exploring registered nurses’ individual-level characteristics and clinical use of race may provide a more comprehensive understanding of specific training needs and inform nursing education and practice.
Keywords: RACE (Racial Attributes in Clinical Evaluation) Measure, clinical use of race, clinical decision making, nurses
More than 4 million healthcare professionals in the United States are nurses, making them the front line of health provision (National Council of State Boards of Nursing, 2016). Driven by the Patient Protection and Affordable Care Act of 2010, the discipline of nursing has entered a new era of clinical practice. The profession has been called upon to increase the number of baccalaureate-prepared and doctorate-prepared nurses, appropriately inform and educate the next generation of nurses, and aid in closing the health disparities gap (Fairman, Rowe, Hassmiller, & Shalala, 2011; Hassmiller, 2010; Institute of Medicine, 2010; Levin & Bateman, 2012). The growing utilization of nurses as primary care providers highlights their important role in bringing a precision medicine approach to health care (Calzone, Jenkins, Nicol, et al., 2013; Cheek, Bashore, & Brazeau, 2015).
Although precision medicine may allow a more accurate approach to patient care that moves beyond race, the complicated relationship between race and genetic ancestry continues to stir an ongoing debate around the clinical utility of race (Dankwa-Mullan, Bull, & Sy, 2015). Race is a fluid concept used to group people according to various factors, including ancestral background and social identity (Smedley & Smedley, 2012). Because race is a crude proxy for certain underlying genetic risk, it remains a commonly used indicator in disease prevention, screening, and treatment strategies.
Differential Health Treatment and Outcomes by Race and Ethnicity
Persistent health disparities are apparent in the variation of disease incidence and mortality across racial and ethnic populations (Badve et al., 2011; Kaiser Family Foundation, 2015; U.S. Cancer Statistics Working Group, 2016). For example, complex diseases such as cardiovascular disease, type 2 diabetes, and prostate and colorectal cancer have disproportionally affected certain racial and ethnic minority populations (Centers for Disease Control and Prevention-National Center for Health Statistics, 2015). A debate has risen around whether race-based screening guidelines are needed to address these disparities and to what extent race has clinical utility, particularly as a proxy for genetic ancestry.
One facet of the debate involves common practice and healthcare guidelines that specifically include the use of race as a proxy for ancestry, genetic risk, and response in diagnostic and treatment decisions. For example, a recently approved test for the Lp-PLA2 biological marker to predict risk for coronary heart disease is reported by the U.S. Food and Drug Administration (2014) to predict risk better in Black women. Additionally, there is a long history of using race in clinical decisions about the most effective type of drugs to administer (Ramamoorthy, Pacanowski, Bull, & Zhang, 2015). Given the current treatment guidelines and ongoing contention around the role of race in clinical practice, scientific discoveries that are beginning to illuminate the contributions of genomic variation and environmental factors to health outcomes for persons with complex chronic diseases hold the promise of guiding development of effective health interventions.
Nurses’ Clinical Use of Race
As research continues to clarify the contribution of social and genetic factors to racial and ethnic differences in health, disease, intervention choices, and outcomes, it is necessary to understand how healthcare providers use (i.e., collect, perceive, and interpret) race in public health practice and clinical care. Research indicates that individual background characteristics, personal beliefs, and biases influence the clinical encounter, often to the disadvantage of minority patients (Lawrence, Rasinski, Yoon, & Curlin, 2014; McKinlay, Piccolo, & Marceau, 2013; Sabin, Nosek, Greenwald, & Rivara, 2009). Research also indicates that patients receive differential treatment by race and may respond differently to treatment based on genomic profile differences (Keenan et al., 2015; Wandner et al., 2014).
There remains a dearth of literature focusing on nurses in the context of race, interpretation of genetic risk and response, and healthcare. A few studies have explored nurses’ understanding and use of genomics (Calzone, Jenkins, Culp, Bonham, & Badzek, 2013; Coleman et al., 2014), while others have focused on race and revealed low levels of cultural competency with little awareness of personal biases in nurses (Haider et al., 2015; Hirsh, Jensen, & Robinson, 2010). However, huge knowledge gaps remain about nurses’ behaviors and beliefs concerning race in clinical care. Given the importance of nursing practice and increased responsibilities of nurses in healthcare provision, our primary aim is to better understand nurses’ clinical use of race, which can affect clinical outcomes. Specifically, although patient race along with other information can help guide diagnostic and treatment decisions in certain circumstances, it can also be used inappropriately, which could adversely influence patient care (Nelson, 2002).
Methods
Eligibility
Study eligibility consisted of registered nurses (RNs) at all levels of academic preparation, role, or specialty employed at participating institutions. Licensed practical nurses and licensed vocational nurses were excluded. This was the only exclusion criterion for study participation.
Study Sample
The study sample includes 5,733 RNs across three separately recruited groups. The largest group is composed of nurses employed by Magnet® -designated hospitals participating in the Method to Integrate a New Competency (MINC) study (Calzone, Jenkins, Culp, Caskey, & Badzek, 2014). MINC included nurses from 23 American Nurses Credentialing Center–designated Magnet Recognition Program® hospitals located in 17 U.S. states. The second group was recruited by member associations of the National Coalition of Ethnic Minority Nurse Associations (NCEMNA), a national collaboration of five ethnic minority nurse associations. Four NCEMNA associations participated in this study: Asian American/Pacific Islander Nurses Association, National Association of Hispanic Nurses, National Black Nurses Association, and Philippine Nurses Association of America (Coleman et al., 2014). The third group is a sample of nurses recruited by the American Nurses Association (ANA; Calzone, Jenkins, Culp, et al., 2013).
Instrument
Data were collected in all three groups using online survey methods and convenience sampling. The survey instrument, called the Genetics and Genomics in Nursing Practice Survey (GGNPS), was developed from a tool for family practice physicians, scaled for nursing and pilot tested with a sample of RNs (Calzone et al., 2012). Instrument validation was performed using structural equation modeling (SEM), which found that the instrument items aligned well with the Rogers Diffusion of Innovations (DOI) domains (Jenkins, Steven, Kahn, & McBride, 2010; Rogers, 2003). The items used in the present study were background demographic characteristics of the nurses and the Bonham & Sellers Racial Attributes in Clinical Evaluation (RACE) scale.
The RACE scale was adapted for nurses from an eight-item RACE scale for physicians designed to measure self-reported use of patient race in clinical decision making (Bonham, Sellers, & Woolford, 2014). Bonham et al. (2014) developed the RACE scale as a tool to measure healthcare providers’ use of race in clinical care, without applying any value-laden assessment of the benefit or harm of its use. Higher RACE scores indicate greater self-reported use of race in clinical care.
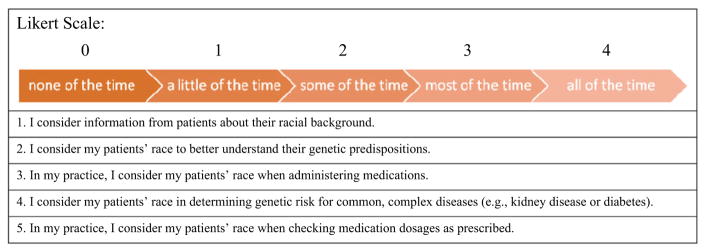
Using a portion of the total nurses’ responses (n = 577) for confirmatory factor analysis (CFA) of the 8 items, a final five-item version of the scale was developed for evaluation of nurses’ clinical use of race (Figure 1). The five-item RACE scale had a Cronbach’s alpha of .86, the loadings were all positive and statistically significant, and other measures (GFI = .99, AGFI = .95, CFI = .99, RMSEA = .08) all indicated adequate fit.
Figure 1.
Racial Attributes in Clinical Evaluation (RACE) Scale for Nurses, with score calculated as sum of responses (0–20), with higher scores signifying greater use of race in clinical practice. α = .86. Adapted from Bonham et al.’s (2014) RACE scale for physicians.
Data Collection
The GGNPS was voluntary, took 15 to 20 min, and did not collect any participant personal identifiers. Recruitment strategies varied across the three participating groups.
MINC institutions sent email announcements about the survey to their nursing staff. Some institutions employed recruitment methods such as advertising, supervisor encouragement, and intranet postings. Data were collected between July and October 2012, and the survey was open for completion 28 days at each institution (Calzone et al., 2014). Although there was no standard protocol for providing compensation, incentives were offered by some institutions when approved by their individual institutional review boards (IRBs).
Recruitment of NCEMNA study participants was done by each participating NCEMNA member association through email announcements and newsletter notifications (Coleman et al., 2014). The survey was open for completion from fall 2010 to early 2011, and a link to the survey was posted on the main NCEMNA website and each participating NCEMNA member association website. No compensation was provided for participation.
The ANA recruited study participants by posting announcements on the main ANA website (“nursing-world”) and in The American Nurse, the official publication of the ANA (Calzone, Jenkins, Culp, et al., 2013). Additionally, study announcements were sent out to ANA SmartBrief and eNewsletter subscribers. The survey was open for completion from fall 2009 to early 2010. No compensation was provided for participation.
Survey development was approved by the National Human Genome Research Institute IRB (05-HG-N196). The IRB at West Virginia University approved the MINC (H-23491) survey, and the Cedars Sinai IRB approved the NCEMNA survey (PRO00018344). The National Institutes of Health Office of Human Subjects Research Protections considered the MINC (OHSRP#11366), ANA (OHSRP#4891), and NCEMA (OHSRP#4570) surveys to be exempt pursuant to 45 CFR 46 because respondents were anonymous and there were no risks to participants.
Study Variables
The outcome variable, use of race in clinical decision making, is measured using a five-item RACE scale (see Figure 1). Items in this 0- to 20-point scale gauge level of nurses’ clinical use of race using a 0–4 rating scale, with 0 as “none of the time” and 4 as “all of the time.” This measure was adapted from the RACE scale for physicians in order to measure clinical use of race by nurses (Bonham et al., 2014). As with the original scale, higher RACE scores indicate more self-reported use of race in clinical decision making; it measures the extent of clinical use of race without placing a positive or negative label on the phenomenon itself.
Predictor variables included age, portion of work time spent with patients, nursing education level, primary nursing role, race and ethnicity, and views on clinical importance of certain patient demographics. Age was measured by subtracting participant birth year from the year in which the survey was completed by the participant. Portion of work time spent with patients was presented as a percentage-based write-in question. Nursing education level, determined by highest nursing degree attained, was measured with the following categories organized low to high: diploma nurse, associate’s, baccalaureate, master’s, and doctorate degree. Primary nursing role was broken down into five categories: patient care, administration, education, research, and other (including students). Self-identified race and ethnicity categories included American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or Pacific Islander, Hispanic or Latino, and White. However, because there were only 26 American Indian or Alaska Native participants and 39 Native Hawaiian or Pacific Islander participants, these two racial and ethnic groups were combined into one category called “Indigenous Populations.” Additionally, the racial and ethnic categories were simplified and combined into one variable with mutually exclusive categories, such that participants who identified as Hispanic or Latino were placed in that category and the other five categories are non-Hispanic in this study. The variables for opinions on clinical importance of certain patient characteristics are gender, race and ethnicity, genes, family history, and age, measured on a 1–7 Likert scale, with 1 meaning “not at all important” and 7 meaning “essential.”
Survey group was included as a covariate, with MINC, NCEMNA, and ANA respondents as three categorical groups. This variable was created specifically to show and account for between-group differences of the three nursing study subgroups.
Data Analysis
Respondents who were not RNs and those who did not answer all five RACE scale items (and therefore could not receive a valid RACE score) were excluded from data analysis (35% of respondents dropped from analysis). Before dropping these data from the final analysis, assessment showed no pattern of the missing RACE scale items, so 35% was deemed an acceptable amount of exclusion.
Once cases that met the exclusion criteria were removed from the dataset, analysis was performed using IBM® SPSS® Statistics 19.0 (SPSS, Inc., Armonk, NY, USA). After basic evaluation of descriptive frequencies and means, the relationships between variables were assessed with bivariate analyses, namely correlation and one-way analysis of variance (ANOVA). The variables were then placed in an ordinary least squares (OLS) regression model for multivariate analysis.
Results
Study Sample Description
Table 1 presents the characteristics of the 5,733 nurses in our sample. The average age in our study sample was 44 years, which is slightly younger than the national average of 50 years (Budden, Moulton, & Cimiotti, 2013). Nurses reported spending an average of 72% of their work time seeing patients, with the ANA and NCEMNA nurses averaging 52% and 53%, respectively, and MINC nurses averaging 75%. Nursing education level in the study sample shows a pattern similar to that of the national nursing workforce (i.e., relatively normal distribution curve with baccalaureate level as the mode), although the study sample has received more nursing education, with a higher percentage of baccalaureate, master’s, and doctorate degrees than the general nursing population (Budden et al., 2013). Of the nurses in the study sample, 57% were at the baccalaureate level, 17% had received master’s degrees, and 2% had their doctorates. Despite some variation in primary nursing role across the MINC, NCEMNA, and ANA survey groups, the general pattern is similar, with the highest percentage of nurses reporting patient care as the primary role and the lowest percentage of nurses reporting research as the primary role in all three groups. Of all the predictor variables, race and ethnicity varied most across survey groups, which was to be expected based on the nature of the recruiting organizations. Despite this variation, the total study sample has a racial and ethnic breakdown similar to that of the national nursing workforce, with slight oversampling of highly educated nurses and minority nurses (Budden et al., 2013).
Table 1.
Variable Means and Frequencies Across Survey Group
| Variable | ANA | NCEMNA | MINC | Total |
|---|---|---|---|---|
| Mean ± SD | ||||
|
| ||||
| RACE score | 10.3 ± 4.7 | 11.3 ± 5.3 | 8.0 ± 4.7 | 8.3 ± 4.8 |
| Age at time of survey | 52.4 ± 11.2 | 50.9 ± 11.2 | 43.7 ± 11.9 | 44.4 ± 12.1 |
| Portion of time seeing patients | 52.1 ± 38.8 | 52.5 ± 38.7 | 74.7 ± 33.5 | 72.4 ± 34.8 |
|
| ||||
| Frequency (%) | ||||
|
| ||||
| Education | ||||
| Diploma | 5 (2.0) | 4 (1.3) | 300 (6.1) | 309 (5.6) |
| Associate’s degree | 41 (16.3) | 25 (8.3) | 1009 (20.4) | 1075 (19.6) |
| Baccalaureate degree | 89 (35.5) | 107 (35.7) | 2911 (58.9) | 3107 (56.5) |
| Master’s degree | 94 (37.5) | 120 (40.0) | 693 (14.0) | 907 (16.5) |
| Doctorate degree | 22 (8.8) | 44 (14.7) | 31 (0.6) | 97 (1.8) |
| Missing | 1 | 8 | 229 | 238 |
| Nursing Role | ||||
| Administration | 18 (7.1) | 69 (22.4) | 431 (8.3) | 518 (9.0) |
| Education | 52 (20.6) | 64 (20.8) | 251 (4.9) | 367 (6.4) |
| Research | 9 (3.6) | 17 (5.5) | 67 (1.3) | 93 (1.6) |
| Patient care | 122 (48.4) | 141 (45.8) | 4002 (77.4) | 4265 (74.4) |
| Other/not specified | 51 (20.2) | 17 (5.5) | 422 (8.2) | 490 (8.5) |
| Race and ethnicity | ||||
| American Indian/Alaska Native | 4 (1.6) | 0 (0.0)a | 22 (0.5) | 26 (0.5) |
| Native Hawaiian/Pacific Islander | 2 (0.8) | 7 (2.5) | 30 (0.6) | 39 (0.7) |
| Asian | 5 (2.1) | 123 (43.5) | 357 (7.4) | 485 (9.0) |
| Black/African American | 4 (1.6) | 92 (32.5) | 315 (6.5) | 411 (7.6) |
| Hispanic/Latino | 5 (2.1) | 56 (19.8) | 221 (4.6) | 282 (5.2) |
| White | 223 (91.8) | 5 (1.8) | 3903 (80.5) | 4131 (76.9) |
| Missing | 9 | 25 | 325 | 359 |
Note. “Survey group” indicates participant recruiting organization. Percentages may not total 100% because of rounding. The sample size was N = 5,733. ANA = American Nurses Association; MINC = Magnet®-designated hospitals participating in the Method to Integrate a New Competency; NCEMNA = National Coalition of Ethnic and Minority Nurse Associations; RACE = Racial Attributes in Clinical Evaluation.
Less than 0.5% was rounded to 0.
Clinical Use of Race Analysis
As shown in Table 2, three predictors were significantly associated with RACE: higher nursing degree level, nurses’ race and ethnicity, and views on clinical importance of patient demographic information.
Table 2.
Final Regression Model Predicting Use of Race in Nurses’ Clinical Decision Making
| Predictors | ba | (95% CI)b |
|---|---|---|
| Age at time of survey | 0.011 | (−.00, .02) |
| Portion of work-time seeing patients (%) | 0.003 | (−.00, .01) |
| Education level | ||
| Entry-level diploma (Ref) | 0 | |
| Associate’s degree | 0.516 | (−.10, 1.13) |
| Baccalaureate degree | 0.686* | (.11, 1.26) |
| Master’s degree | 1.633*** | (.99, 2.28) |
| Doctorate degree | 1.770** | (.51, 3.031) |
| Primary nursing role | ||
| Patient care (Ref) | 0 | |
| Administration | 0.290 | (−.23, .87) |
| Education | −0.006 | (−.65, .64) |
| Research | 0.036 | (−.99, 1.06) |
| Race and ethnicity | ||
| White (Ref) | 0 | |
| Indigenous Populationsc | 0.364 | (−.88, 1.61) |
| Asian | 1.411*** | (.92, 1.90) |
| Black/African American | 0.554* | (.04, 1.07) |
| Hispanic/Latino | −0.152 | (−.75, .45) |
| Importance of patient demographics | ||
| Gender | 0.022 | (−.09, .13) |
| Race/ethnicity | 0.537*** | (.42, .65) |
| Genes | 0.206*** | (.09, .32) |
| Family history | 0.151** | (.04, .27) |
| Age | 0.189*** | (.10, .28) |
| Control: survey group | ||
| MINC (Ref) | 0 | |
| ANA | 0.882** | (.23, 1.53) |
| NCEMNA | 0.307 | (−.58, 1.19) |
Note. Outcome variable: RACE score. After listwise deletion, n = 4,205. Adjusted r2 = 0.199. ANA = American Nurses Association; CI = confidence interval; MINC = Magnet®-designated hospitals participating in the Method to Integrate a New Competency; NCEMNA = National Coalition of Ethnic and Minority Nurse Associations; RACE = Racial Attributes in Clinical Evaluation.
”b” shows change in RACE score for every 1-unit increase in predictor variable, or between the indicated group and reference group.
Less than 0.005 was rounded to 0.
American Indian/Alaska Native and Native Hawaiian/Pacific Islander categories were combined into Indigenous Populations category due to small n.
p < .05;
p < .01;
p < .001.
Although there was no statistically significant difference in RACE score between associate degree-level and diploma-level nurses, the baccalaureate-level nurses reported 0.69 points higher RACE scores than diploma-level nurses (p < .05), master’s-level nurses reported 1.63 points higher RACE scores than diploma-level nurses (p < .001), and doctorate-level nurses reported 1.77 points higher RACE scores than diploma-level nurses (p < .01). This relatively linear relationship between level of nursing degree and RACE score indicates that increase in education corresponds to increase in reported clinical use of race in our study sample.
Asian and Black nurses appear to be linked to higher reported RACE scores. Specifically, nurses who identified as Asian reported RACE scores 1.41 points higher than White nurses (p < .001), and those who identified as Black or African American reported RACE scores 0.55 points higher than White nurses (p < .05). Nurses in Indigenous Populations and nurses who identified as Hispanic or Latino did not have significantly different RACE scores than White nurses in this study.
The nurses’ ratings of clinical importance of patient characteristics were significant for all attributes except gender. With a one point increase in clinical importance rating as the increment, patient race and ethnicity corresponded to a 0.54-point increase in RACE score (p < .001), patient genes to a 0.21-point increase in RACE score (p < .001), patient family history to a 0.15-point increase in RACE score (p < .01), and patient age to a 0.19-point increase in RACE score (p < .001).
Our covariate, survey group, also had a significant relationship with clinical use of race. Although there was no significant difference in RACE scores for NCEMNA-and MINC-recruited nurses, ANA-recruited nurses reported RACE scores 0.88 points higher than MINC-recruited nurses (p < .01). The overall model has an adjusted r2 of 0.20, suggesting that higher nursing degree, self-identified minority racial identity, and perceived importance of various patient demographics together provide a modest explanatory power in predicting RACE score. These variables do not tell the whole story, but they provide important insights into the clinical decision-making process.
Discussion
When assessed in the bigger context of racial and ethnic health inequities, there are many implications of these findings. For highest nursing degree, the relatively linear positive relationship between education level and clinical use of race indicates that there could be differences in cultural competency and training associated with different levels of nursing education. This notion is supported by the presence of published and well-documented guidelines for cultural competency training in baccalaureate and higher degree nursing education that are not in place for associate or diploma levels (American Association of Colleges of Nursing, 2006, 2008, 2011). The linear positive relationship we found might be explained by increased depth, scope, and overall exposure to these topics in training required for baccalaureate and higher nursing degrees. Because the education for each degree comes with its own course and credit hour requirements, every additional degree earned increases exposure to and complexity of courses in population genetics, epidemiology, risk assessment, prevention, detection, symptom management, treatment strategies related to race, and other associated topics. In this case, a stronger foundation of knowledge about race and genetic ancestry in clinical decision making could allow nurses to more appropriately use race in clinical care.
Nurses who identified as Asian or Black reported more use of race in clinical decision making than nurses who identified as White. Given the sample size and potential limitations of our defined racial and ethnic groups, especially the Hispanic and Indigenous categories, we have focused on Asian, Black, and White as the primary racial and ethnic groups for interpretation of results. Generally, a significant difference in race scores was found between minority (Asian and Black) and White nurses, such that minority nurses reported higher clinical use of race than White nurses. This trend of higher reported use of race among minority nurses may be due, in part, to racial self-awareness. White nurses are not often forced to be conscious of their own race or their use of race in day-to-day life, while minorities are continuously made aware of their own race (Dottolo & Stewart, 2013; Hall & Fields, 2012; Robinson, 2014). This suggests that the lived experience of minority nurses influences their perception of race and health care in a way that makes them more inclined to be explicit about their understanding and clinical use of race (Johansson, Jones, Watkins, Haisfield-Wolfe, & Gaston-Johansson, 2011). This differential experience and awareness of White nurses and nurses of color might be reflected in the higher RACE scores of minority nurses. The difference in racial awareness and everyday experience of race, which may be a key factor in RACE score differences across racial and ethnic groups, has also been found between White and Black physicians in previous qualitative research (Bonham et al., 2009; Snipes et al., 2011).
RACE scores were also significantly associated with reported clinical importance of patient characteristics. We found that nurses who identified patient age, race and ethnicity, genes, and family history as important in clinical care had higher RACE scores. Surprisingly, patient gender was not associated with RACE scores. The significant association of RACE score with beliefs about the clinical importance of race and ethnicity is logical, and given the complicated relationships between race, genes, and family history, it is not surprising that importance ratings of all these patient demographics significantly predicted RACE score. The use of patient age, race and ethnicity, genes, and family history in clinical decision making has been documented in previous studies (Doerr, Edelman, Gabitzsch, Eng, & Teng, 2014; Hirsh, Callander, & Robinson, 2011; Musunuru et al., 2015). However, findings concerning patient gender have been less conclusive, with some studies finding no gender difference at all in clinical care (Hajjaj, Salek, Basra, & Finlay, 2010; Wandner et al., 2014). Perhaps the ambiguity of the clinical role of patient gender in previous findings, as well as the nonsignificant relationship between perceived importance of patient gender and use of race found in this study, stem from another aspect of clinical decision making such as education or other related experience.
Limitations
Our study must be interpreted within the bounds of its limitations. First, the study employed a convenience sampling method for data collection, and rates of group membership and demographic features in the study sample were not congruent with rates in the national nursing population. For example, 90% of the nurses in this study were employed by Magnet®-designated hospitals, although only 6% of all hospitals in the United States have received Magnet® designation. Nurses at these institutions may be a unique subset of the nursing population with a higher percentage prepared at baccalaureate, master’s, or doctoral levels (American Hospital Association, 2014; American Nurses Credentialing Center, 2015, February).
Second, grouping strategy for respondents’ race and ethnicity is a limitation. There was considerable variation within both the Hispanic or Latino and Indigenous Populations categories, for which potentially unlike subgroups were combined in analysis; Hispanic or Latino included all nurses who identified as such, regardless of their other additional racial and ethnic identities, and Indigenous Populations was relatively small and included nurses who identified with any of four different groups (American Indian, Alaska Native, Native Hawaiian, and Pacific Islander).
Third, it is difficult to account for social desirability bias in survey responses. Social desirability bias is especially likely to have some effect on survey studies involving sensitive subjects, like race. In an effort to avoid seeming prejudiced, consciously or unconsciously, people tend to under-report their use of race, and the effect of this bias is stronger for members of the dominant racial group (Hall & Fields, 2013; Manns-James, 2015). Relatedly, because of the discrepancy between reported conduct and actual behavior, the findings of this study only reveal factors related to the self-reported level of clinical use of race.
Conclusions and Implications
To our knowledge, this is one of the first studies to examine background characteristics of nurses related to clinical use of race and to utilize the nurses’ RACE scale. Replication of this study using a national probability sample of nurses would provide more generalizable insights into the issues addressed here. Another consideration for future studies would be inclusion of additional predictors in order to gain a more holistic understanding of the role of race in nurses’ clinical decision-making processes. Additionally, in “A Blueprint for Genomic Nursing Science,” health disparities issues are recommended as a component of any genomic nursing research (Genomic Nursing State of the Science Advisory Panel, 2013). Racial, ethnic, socioeconomic, and cultural influences on disease occurrence and response to treatment; genomic health equity (e.g., access); diseases that disproportionately affect specific groups (e.g., racial and ethnic minorities); and targeted therapeutics are specific topics for evidence development through research.
Healthcare providers are obtaining knowledge of tools to better understand complex biological, environmental, and psychosocial mechanisms relevant to clinical decision making and health outcomes (Dankwa-Mullan et al., 2015). As the precision medicine approach to health care advances, health providers’ perception and use of race in clinical decision making should change accordingly. More specifically, nursing education and clinical practice must reflect new findings and knowledge in the field of genomics to continue improving patient care (Calzone et al., 2014). Both formal academic training and continuing education efforts that include a stronger foundation regarding knowledge about use of race and genetic ancestry in clinical decision making are encouraged. This foundation will stimulate translation of the science to practice, facilitating nurses’ appropriate use of race in clinical care.
Given the important role of nurses in provision of health care, this study’s focus on clinical practice and nurses’ use of race contributes to the body of nursing research. Understanding how nurses use race in their practice provides key insights about the clinical encounter and may help inform the development of future cultural competency trainings and educational interventions.
Clinical Resources.
American Anthropological Association RACE Project: http://www.understandingrace.org/home.html
Centers for Disease Control and Prevention Fast-Stats: Health of Black or African American non-Hispanic population: http://www.cdc.gov/nchs/fastats/black-health.htm
Genetics/Genomics Competency Center (G2C2): http://g-2-c-2.org//
Institute of Medicine report brief: Unequal treatment: What health care providers need to know about racial and ethnic disparities in healthcare: https://iom.nationalacademies.org/~/media/Files/Report%20Files/2003/Unequal-Treatment-Confronting-Racial-and-Ethnic-Disparities-in-Health-Care/Disparitieshcproviders8pgFINAL.pdf
National Human Genome Research Institute: http://www.genome.gov/
Acknowledgments
The authors would like to thank the Magnet® designated hospitals that participated in the MINC study and the nursing associations (NCEMNA and ANA) that collaborated on this project. Most importantly, the authors would like to thank the thousands of RNs who participated in the study. This research was supported in part by the Intramural Research Programs of the NIH National Human Genome Research Institute, National Cancer Institute, and the West Virginia University, and the MINC project was funded by the National Council of State Boards of Nursing.
Footnotes
The opinions expressed are the authors’ own and do not reflect the policies or positions of the National Institutes of Health or the U.S. Department of Health and Human Services.
References
- American Association of Colleges of Nursing. The essentials of doctoral education for advanced nursing practice. 2006 Retrieved from http://www.aacn.nche.edu/publications/position/DNPEssentials.pdf.
- American Association of Colleges of Nursing. The essentials of baccalaureate education for professional nursing practice. 2008 Retrieved from http://www.aacn.nche.edu/education-resources/BaccEssentials08.pdf.
- American Association of Colleges of Nursing. The essentials of master’s education in nursing. 2011 Retrieved from http://www.aacn.nche.edu/education-resources/MastersEssentials11.pdf.
- American Hospital Association. December 2014 hospital update. 2014 Retrieved from http://www.ahadataviewer.com/recent-updates/December-2014-Hospital-Update/
- American Nurses Credentialing Center (Producer) Find a Magnet hospital. 2015 Feb; Retrieved from http://www.nursecredentialing.org/findamagnethospital.aspx.
- Badve S, Dabbs DJ, Schnitt SJ, Baehner FL, Decker T, Eusebi V, … Reis-Filho JS. Basal-like and triple-negative breast cancers: A critical review with an emphasis on the implications for pathologists and oncologists. Modern Pathology. 2011;24(2):157–167. doi: 10.1038/modpathol.2010.200. [DOI] [PubMed] [Google Scholar]
- Bonham VL, Sellers SL, Gallagher TH, Frank D, Odunlami AO, Price EG, Cooper LA. Physicians’ attitudes toward race, genetics, and clinical medicine. Genetics in Medicine. 2009;11(4):279–286. doi: 10.1097/GIM.0b013e318195aaf4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonham VL, Sellers SL, Woolford S. Physicians’ knowledge, beliefs, and use of race and human genetic variation: New measures and insights. BMC Health Services Research. 2014;14:456. doi: 10.1186/1472-6963-14-456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budden JZE, Moulton P, Cimiotti J. Supplement: The National Council of State Boards of Nursing and The Forum of State Nursing Workforce Centers 2013 National Workforce Survey of Registered Nurses. Journal of Nursing Regulation. 2013;4(2):S1–S72. [Google Scholar]
- Calzone KA, Culp S, Jenkins J, Caskey S, Edwards P, Fuchs MA, … Badzek L. Test/retest reliability of the genetics and genomics in nursing practice survey instrument. Journal of Nursing Measurement. 2016;24(1):54–68. doi: 10.1891/1061-3749.24.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calzone KA, Jenkins J, Culp S, Bonham VL, Badzek L. National nursing workforce survey of nursing attitudes, knowledge and practice in genomics. Personalized Medicine. 2013;10(7) doi: 10.2217/pme.13.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calzone KA, Jenkins J, Culp S, Caskey S, Badzek L. Introducing a new competency into nursing practice. Journal of Nursing Regulation. 2014;5(1):40–47. doi: 10.1016/s2155-8256(15)30098-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calzone KA, Jenkins J, Nicol N, Skirton H, Feero W, Green E. Relevance of genomics to healthcare and nursing practice. Journal of Nursing Scholarship. 2013;45(1):1–2. doi: 10.1111/j.1547-5069.2012.01464.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calzone KA, Jenkins J, Yates J, Cusack G, Wallen GR, Liewehr DJ, … McBride C. Survey of nursing integration of genomics into nursing practice. Journal of Nursing Scholarship. 2012;44(4):428–436. doi: 10.1111/j.1547-5069.2012.01475.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention/National Center for Health Statistics. Health of Black or African American non-Hispanic population. 2015 Retrieved from http://www.cdc.gov/nchs/fastats/black-health.htm.
- Cheek DJ, Bashore L, Brazeau DA. Pharmacogenomics and implications for nursing practice. Journal of Nursing Scholarship. 2015;47(6):496–504. doi: 10.1111/jnu.12168. [DOI] [PubMed] [Google Scholar]
- Coleman B, Calzone KA, Jenkins J, Paniagua C, Rivera R, Hong OS, … Bonham V. Multi-ethnic minority nurses’ knowledge and practice of genetics and genomics. Journal of Nursing Scholarship. 2014;46(4):235–244. doi: 10.1111/jnu.12083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dankwa-Mullan I, Bull J, Sy F. Precision medicine and health disparities: Advancing the science of individualizing patient care. American Journal of Public Health. 2015;105(53 Suppl 3):S368. doi: 10.2105/AJPH.2015.302755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doerr M, Edelman E, Gabitzsch E, Eng C, Teng K. Formative evaluation of clinician experience with integrating family history-based clinical decision support into clinical practice. Journal of Personalized Medicine. 2014;4:115–136. doi: 10.3390/jpm4020115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dottolo AL, Stewart AJ. “I never think about my race”: Psychological features of White racial identities. Qualitative Research in Psychology. 2013;10(1):102–117. doi: 10.1080/14780887.2011.586449. [DOI] [Google Scholar]
- Fairman JA, Rowe JW, Hassmiller S, Shalala DE. Broadening the scope of nursing practice. New England Journal of Medicine. 2011;364(3):193–196. doi: 10.1056/NEJMp1012121. [DOI] [PubMed] [Google Scholar]
- Genomic Nursing State of the Science Advisory Panel. Calzone KA, Jenkins J, Bakos AD, Cashion AK, Donaldson N, Feero WG, … Webb JA. A blueprint for genomic nursing science. Journal of Nursing Scholarship. 2013;45(1):96–104. doi: 10.1111/jnu.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haider A, Schneider E, Sriram N, Scott V, Swoboda S, Zogg C, … Cooper L. Unconscious race and class bias among registered nurses: Vignette-based study using implicit association testing. Journal of the American College of Surgeons. 2015;220:1077–1086. doi: 10.1016/j.jamcollsurg.2015.01.065. [DOI] [PubMed] [Google Scholar]
- Hajjaj FM, Salek MS, Basra MK, Finlay AY. Non-clinical influences on clinical decision-making: A major challenge to evidence-based practice. Journal of the Royal Society of Medicine. 2010;103(5):178–187. doi: 10.1258/jrsm.2010.100104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall JM, Fields B. Race and microaggression in nursing knowledge development. Advances in Nursing Science. 2012;35(1):25–38. doi: 10.1097/ANS.0b013e3182433b70. [DOI] [PubMed] [Google Scholar]
- Hall JM, Fields B. Continuing the conversation in nursing on race and racism. Nursing Outlook. 2013;61(3):164–173. doi: 10.1016/j.outlook.2012.11.006. [DOI] [PubMed] [Google Scholar]
- Hassmiller S. Nursing’s role in healthcare reform. American Nurse Today. 2010;5(9):68–69. [Google Scholar]
- Hirsh AT, Callander SB, Robinson ME. Patient demographic characteristics and facial expressions influence nurses’ assessment of mood in the context of pain: A virtual human and lens model investigation. International Journal of Nursing Studies. 2011;48(11):1330–1338. doi: 10.1016/j.ijnurstu.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsh AT, Jensen MP, Robinson ME. Evaluation of nurses’ self-insight into their pain assessment and treatment decisions. Journal of Pain. 2010;11(5):454–461. doi: 10.1016/j.jpain.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. The future of nursing: Leading change, advancing health. 2010 Retrieved from https://iom.nationalacademies.org/Reports/2010/The-Future-of-Nursing-Leading-Change-Advancing-Health.aspx.
- Jenkins JWS, Stevent N, Kahn N, McBride C. Family physicians’ likely adoption of genomic-related innovations. Case Studies in Business, Industry, and Government Statistics. 2010;3(2):70–78. [Google Scholar]
- Johansson P, Jones DE, Watkins CC, Haisfield-Wolfe ME, Gaston-Johansson F. Physicians’ and nurses’ experiences of the influence of race and ethnicity on the quality of healthcare provided to minority patients, and on their own professional careers. Journal of National Black Nurses Association. 2011;22(1):43–56. [PubMed] [Google Scholar]
- Kaiser Family Foundation. Life expectancy at birth (in years), by race/ethnicity. State Health Facts; 2015. Retrieved from http://kff.org/other/state-indicator/life-expectancy-by-re/ [Google Scholar]
- Keenan T, Moy B, Mroz EA, Ross K, Niemierko A, Rocco JW, … Bardia A. Comparison of the genomic landscape between primary breast cancer in African American versus White women and the association of racial differences with tumor recurrence. Journal of Clinical Oncology. 2015 doi: 10.1200/JCO.2015.62.2126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence RE, Rasinski KA, Yoon JD, Curlin FA. Physician race and treatment preferences for depression, anxiety, and medically unexplained symptoms. Ethnicity and Health. 2014 doi: 10.1080/13557858.2014.921893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin PJ, Bateman R. Organizing and investing to expand primary care availability with nurse practitioners. Journal of Community Health. 2012;37(2):265–269. doi: 10.1007/s10900-011-9537-5. [DOI] [PubMed] [Google Scholar]
- Manns-James L. Finding what is hidden: A method to measure implicit attitudes for nursing and health-related behaviours. Journal of Advanced Nursing. 2015;71(5):1005–1018. doi: 10.1111/jan.12626. [DOI] [PubMed] [Google Scholar]
- McKinlay J, Piccolo R, Marceau L. An additional cause of health care disparities: The variable clinical decisions of primary care doctors. Journal of Evaluation in Clinical Practice. 2013;19(4):664–673. doi: 10.1111/jep.12015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musunuru K, Hickey KT, Al-Khatib SM, Delles C, Fornage M, Fox CS, … Rosand J. Basic concepts and potential applications of genetics and genomics for cardiovascular and stroke clinicians: A scientific statement from the American Heart Association. Circulation: Cardiovascular Genetics. 2015;8(1):216–242. doi: 10.1161/HCG.0000000000000020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Council of State Boards of Nursing. The 2016 environmental scan. Journal of Nursing Regulation. 2016;6(4):4–37. [Google Scholar]
- Nelson A. Unequal treatment: Confronting racial and ethnic disparities in health care. Journal of the National Medical Association. 2002;94(8):666, 668. [PMC free article] [PubMed] [Google Scholar]
- Patient Protection and Affordable Care Act. (2010). § 3502 (2010). United States Congress.
- Ramamoorthy A, Pacanowski MA, Bull J, Zhang I. Racial/ethnic differences in drug disposition and response: Review of recently approved drugs. Clinical Pharmacology and Therapeutics. 2015;97(3):263–272. doi: 10.1002/cpt.61. [DOI] [PubMed] [Google Scholar]
- Robinson OV. Characteristics of racism and the health consequences experienced by black nursing faculty. ABNF Journal. 2014;25(4):110–115. [PubMed] [Google Scholar]
- Rogers EM. Diffusion of innovations. 5. New York, NY: The Free Press; 2003. [Google Scholar]
- Sabin JA, Nosek BA, Greenwald AG, Rivara FP. Physicians’ implicit and explicit attitudes about race by MD race, ethnicity, and gender. Journal of Health Care for the Poor and Underserved. 2009;20(3):896–913. doi: 10.1353/hpu.0.0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedley A, Smedley B. Race in North America: Origin and evolution of a worldview. 4. Boulder, CO: Westview Press; 2012. [Google Scholar]
- Snipes SA, Sellers SL, Tafawa AO, Cooper LA, Fields JC, Bonham VL. Is race medically relevant? A qualitative study of physicians’ attitudes about the role of race in treatment decision-making. BMC Health Services Research. 2011;11:183. doi: 10.1186/1472-6963-11-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Cancer Statistics Working Group. United States Cancer Statistics: 1999–2013 Incidence and Mortality Web-based Report. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; 2016. Available at: www.cdc.gov/uscs. Link to direct page is: https://nccd.cdc.gov/uscs/cancersbyraceandethnicity.aspx. [Google Scholar]
- U.S. Cancer Statistics Working Group. United States cancer statistics: 1999–2013 incidence and mortality web-based report. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; 2016. Retrieved from www.cdc.gov/uscs. [Google Scholar]
- U.S. Food and Drug Administration. FDA clears test that helps predict the risk of coronary heart disease: Study data show test predicts risk better in Black women. 2014 Retrieved from http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm426799.htm.
- Wandner LD, Heft MW, Lok BC, Hirsh AT, George SZ, Horgas AL, … Robinson ME. The impact of patients’ gender, race, and age on health care professionals’ pain management decisions: An online survey using virtual human technology. International Journal of Nursing Studies. 2014;51(5):726–733. doi: 10.1016/j.ijnurstu.2013.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]