Abstract
BACKGROUND AND OBJECTIVES:
Given the nature of FMR1 gene expansions, most biological mothers, and often multiple other family members of children with fragile X syndrome (FXS), will have a premutation, which may increase individual and family vulnerabilities. This article summarizes important gaps in knowledge and notes potential implications for pediatric providers with regard to developmental and medical risks for children and adolescents with an FMR1 premutation, including possible implications into adulthood.
METHODS:
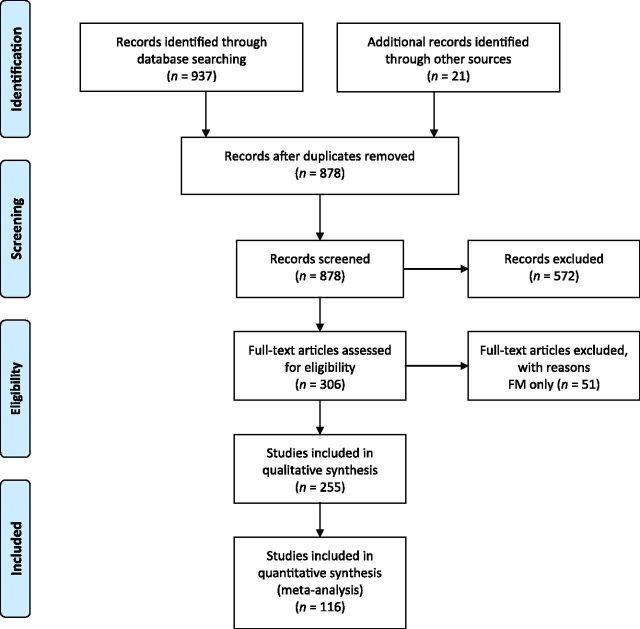
A structured electronic literature search was conducted on FMR1 pre- and full mutations, yielding a total of 306 articles examined. Of these, 116 focused primarily on the premutation and are included in this review.
RESULTS:
Based on the literature review, 5 topic areas are discussed: genetics and epidemiology; phenotypic characteristics of individuals with the premutation; implications for carrier parents of children with FXS; implications for the extended family; and implications for pediatricians.
CONCLUSIONS:
Although the premutation phenotype is typically less severe in clinical presentation than in FXS, premutation carriers are much more common and are therefore more likely to be seen in a typical pediatric practice. In addition, there is a wide range of medical, cognitive/developmental, and psychiatric associated features that individuals with a premutation are at increased risk for having, which underscores the importance of awareness on the part of pediatricians in identifying and monitoring premutation carriers and recognizing the impact this identification may have on family members.
Once thought to only be affected by an increased risk for having offspring with fragile X syndrome (FXS), individuals with a premutation (PM, “carriers”) are now known to be at increased risk for several health concerns. Most research to date on PM carriers has focused on adults, primarily due to identification of 2 later-onset fragile X–associated disorders (FXADs), fragile X–associated tremor ataxia syndrome (FXTAS) and fragile X–associated primary ovarian insufficiency (FXPOI). After the discovery of the link between these FXADs and the PM, additional research has elucidated several other medical (eg, hypertension and thyroid disease), emotional (eg, anxiety), and cognitive (eg, executive function) challenges, which may occur at a greater frequency among a subset of carriers.1–5 Although interest in the PM phenotype has increased substantially over the last decade as these issues have become more apparent, studies on children remain limited due to a lack of early identification or biased samples who were clinically referred. The goal of this review is to highlight recent findings and gaps in the knowledge base regarding developmental, psychiatric, and medical features of the PM phenotype, as well as the familial impact of FMR1 mutations.
Methods
The methods for obtaining articles for the literature review, including inclusion and exclusion criteria for articles on both pre- and full mutations, are described in detail in the article by Raspa et al in this supplement (Public Health Literature Review of Fragile X Syndrome). Of the 306 articles retained from the larger review, 51 were excluded because the content focused exclusively on the full mutation of FXS. A total of 116 articles that were specific to the PM are cited in this article (Fig 1). Results are organized into 5 sections: (1) genetics and epidemiology, (2) phenotypic characteristics of individuals with the premutation, (3) implications for carrier parents of children with FXS, (4) implications for the extended family, and (5) implications for pediatricians.
FIGURE 1.
Articles included in the literature review. Adapted from Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009; 6(7):e1000097.
Results
Genetics and Epidemiology of the FMR1 Premutation
FMR1 mutations refer to an expansion of a trinucleotide repeat (CGG) on the 5′ untranslated region of the FMR1 gene. The normal CGG range of repeats is 6 to 44. Those with 45 to 54 CGG repeats are considered to be intermediate or “gray zone,” and those with 55 to 200 repeats have the premutation, which is unstable and expands when inherited. If the inherited expansion reaches >200 CGG repeats, it is considered a full mutation, also known as FXS. FMR1 mutations are now considered to result in a spectrum of phenotypic involvement, the most severe of which is FXS, but with implications for individuals with a broad range of expanded CGG repeats.
Research on the molecular pathways leading to increased risks for individuals with a PM is still in its infancy, although expanding research using animal models (primarily mice engineered to carry the premutation) has elucidated cognitive, motor, and molecular abnormalities.6,7 In general, the larger the number of CGG repeats, the lower the level of the fragile X mental retardation protein (FMRP),8,9 which is essential for normal brain development. Also, with an increasing number of CGG repeats, there is elevation in FMR1 messenger RNA, which may result in reduced neuronal function and central nervous system dysregulation.10–13 Currently, there is active research on several core mechanisms, such as RNA toxicity, polyglycine-containing FMRP, lowered FMRP, and additive copy number variant (CNV) genetic abnormalities that may be associated with an increased risk for medical or emotional problems.14–17
The PM status of the FMR1 gene is more prevalent than the full mutation status. Several recent population studies (with large sample sizes) have yielded reliable prevalence estimates ranging between 1 in 148 and 1 in 204 for females and between 1 in 290 and 1 in 468 for males.18–22 Thus, although it may not be known unless there is a child with FXS diagnosed in the family, pediatricians have a high likelihood of encountering children and family members with a PM. Increased pediatrician knowledge about potential PM issues could potentially improve identification, as well as promote prevention and early treatment options for symptomatic carriers.
Phenotypic Characteristics of Individuals With a Premutation
Developmental Profile
Developmental involvement in PM carriers was first reported in 199418 among carrier boys who presented with developmental problems (eg, autism, intellectual deficits) for which they were clinically referred. In a retrospective case series study of clinically referred children, Renda et al19 found that a high percentage of children with expanded CGG repeats had some type of neurodevelopmental diagnosis. Similarly, Bailey et al20 found a higher rate of developmental disabilities reported by parents of children with the PM compared with noncarrier children. Several case studies23–25 have reported developmental delays in carriers with lower levels of FMRP. However, there is a significant difference in the developmental profile of carriers who were clinically referred, like the cases described above, compared with carriers identified through cascade testing through a family member with FXS. Farzin et al21 found that patients with the PM who presented clinically have more developmental problems than those identified by cascade testing or controls without the PM from the same families. In this study, only those who were clinically referred demonstrated significantly lower IQ scores and increased autism symptoms compared with controls.
In contrast, Myers et al22 found overall intact cognitive and developmental profiles in a study of 14 children with a PM who were not clinically referred. Similarly, for adults with the PM without a diagnosis of FXTAS, overall cognitive abilities are generally unaffected26 whereas for individuals with FXTAS, overall cognition declines with age.27 However, a few studies have documented lower verbal IQ scores among women with a PM compared with female controls28,29 and males with a PM.30 In addition, there may be increased difficulties in specific domains of cognition, especially in executive function (EF),26,31,32 numeric reasoning and spatial-temporal processing,33 language,34,35 working memory,36 and arithmetic.29,37 In one of the few published studies of infants with the PM,38 visual processing deficits were found in 14 babies identified through newborn screening relative to noncarrier controls. The PM infants were as likely as infants with FXS or those with Down syndrome to have visual processing deficits, despite having overall higher developmental scores. These challenges may be very early markers of later EF challenges. These deficits reported in human PM studies parallel findings of locomotor, spatial learning and processing, memory, anxiety, and reaching deficits found in the PM mice.7,39,40
In summary, we do not have a clear picture of developmental outcomes for individuals with a PM. The adult literature would suggest some cognitive challenges beyond what would be expected as a result of normal aging, but the developmental trajectory of FXTAS may confound the generalizability of results suggesting cognitive decline. In children and adolescents, there are several reports suggesting a higher than expected rate of developmental disabilities in PM carriers, but many of these studies are based on clinically referred children, again limiting the generalizability of the findings. More natural history studies of children with a PM are needed to identify relative risks and potential biomarkers associated with those risks.
Psychiatric Profile
Comorbid anxiety, attention-deficit/hyperactivity disorder (ADHD), and autism spectrum disorders (ASD) are the most commonly reported psychiatric conditions for both individuals with PM and those with FXS. In a national parent-report survey, children with a PM were reported to have significantly more attention problems than non-PM children matched on sex, age, and family income, excluding any matches with siblings.20 Similarly, Hunter et al41 found that adult female carriers had significantly more symptoms of inattention and memory than noncarrier controls. In a follow-up study, Hunter et al42 found that the FMR1 CGG repeat accounted for ∼5% of the variance in ADHD symptoms, whereas other genes accounted for ∼50% of the residual variance, suggesting that the PM acts with other genes to influence the severity of ADHD symptoms.
Given that many individuals with FXS are also diagnosed with ASD, several studies have examined the rates and severity of autism in individuals with a PM. One study found an increased rate of ASD in PM siblings of an individual with FXS compared with noncarrier siblings.21 In a large survey of families, 19% of males and 1% of females with the PM had a diagnosis of ASD.20 Similarly, in a direct-screening study, 14% of boys and 5% of girls with the PM were found to have ASD.43 This is an elevated risk relative to the general population, where just over 2% of males and <1% of females have ASD.44 Even among carriers who do not meet criteria for ASD, elevated autismlike symptoms have been reported. For example, increased rates of social aloofness45 and a rigid perfectionism46 have been described among carrier women. Behavioral features of the broad autism phenotype, including pragmatic language problems, have been found in women with a PM,34 suggesting a possible link between FMR1 and autism-related phenotypes. As with developmental profiles, higher rates of psychiatric problems, such as ASD and ADHD, have been found in children with the PM who were clinically referred compared with those with the PM who were not clinically referred and controls.21,47
Adults with a PM may be at higher risk for mood and anxiety disorders.48–52 Recent studies found a relationship between the number of CGG repeats and the prevalence50 and severity51 of depressive symptoms. The prevalence of major depressive disorder is high for women with a PM relative to the national average, with a higher than expected rate of first major depressive disorder episodes occurring before the birth of a child with FXS.52 Other mood disorders (eg, dysthymia and bipolar disorder) are not higher in carriers compared with controls.53 Although not studied extensively in children or adolescents with the PM, Bailey et al54 reported that depression may occur at a higher frequency among younger individuals with a PM compared with a matched sample of noncarriers. Anxiety symptoms, including social avoidance, interpersonal sensitivity, shyness, and eye contact avoidance, are also common in PM carriers, with up to 41% reporting a lifetime diagnosis of an anxiety disorder.45 Social phobia and panic disorder are the most commonly reported anxiety disorders.45,52 Schizotypal personality traits may also be more common among PM carriers.45,55 In addition, several case studies have noted the presence of psychotic illnesses.56–58 However, given the low rate of psychosis in the general population, its challenging to study the relative risk for PM carriers.
Psychiatric issues have been studied more extensively in adults with a PM, although many of these studies are confounded by the high percentage of participants who were also parents of children with FXS and therefore likely impacted by increased caregiver stress. Emerging evidence suggests that there is an increased risk for some psychiatric vulnerabilities, especially anxiety, attention regulation, and autism features in individuals with a PM, which may develop in childhood or adolescence.
Medical Profile
Little is known about relative medical risks, other than seizures, for children or adolescents with a PM. However, several medical problems occur more frequently in adult PM carriers than in noncarriers, and there may be early signs of these issues apparent in adolescence. Brief descriptions of some of these health risks are included below, with typical age of onset reported where known.
Seizures
Seizures have been reported at a higher rate among children with a PM who also display autistic features.47 Subsequent work on the rat model of early-life seizures has demonstrated that seizures shift FMRP away from the dendritic spine and into the cell body of the neuron.59 Because seizures can worsen autism features in any genetic or idiopathic cause of autism in patients,60 it is important to recognize seizures early and treat them appropriately.
FXPOI
FXPOI is associated with premature ovarian failure, cessation of menses before age 40 years, and other indicators of early ovarian aging or dysfunction.61 Approximately 20% of carriers will be diagnosed with FXPOI.62 Even among women with the PM that do not have a diagnosis of FXPOI, several hormonal changes have been documented, including decreased levels of anti-Müllerian hormone; increased levels of follicle-stimulating hormone62–67; irregular, shorter, or skipped cycles; subfertility66,68; and hot flashes.69 PM carriers, on average, reach menopause 5 years earlier than the general population of women.63,70,71 Increased risk for earlier menopause has been associated with mid-range CGG repeats (80–100).62,63,68,72–74
Although girls with PM typically begin menses around the same age as their noncarrier peers,64,65 they have an increased risk for irregular periods, especially if they have mid-range CGG lengths.62 These females are also more likely to have difficulties with fertility and may experience other estrogen-related health concerns, such as lower bone mineral density and osteoporosis.75 About 3% of adolescents with the PM are expected to have some difficulties with menstruation, and <1% may experience cessation of menses during adolescence.76 The increased risk for FXPOI and other reproductive challenges have important implications for adolescent and young adult females as they make decisions regarding their reproductive future. These potential reproductive challenges, along with their genetic risk for passing on a fully expanded FMR1 gene, increase the importance of early discussions with girls regarding their PM status. De Caro et al76 provide guidelines for genetic counselors and other medical professionals in providing information and support for adolescent PM carriers.
FXTAS
Although not a condition thought to affect younger PM carriers, FXTAS is the most well-described FXAD associated with a PM.77 The core features of FXTAS are cerebellar gait ataxia and action tremor. Other symptoms include parkinsonism, cognitive decline (especially in EF), peripheral neuropathy, and autonomic dysfunction.78 FXTAS occurs in ∼40% of male carriers and 8% to 16% of female carriers.79,80 Clear signs of FXTAS typically begin at ∼60 years of age, although there are rare cases that begin earlier.1 Rates of FXTAS increase with age; >75% of men with PM >80 years of age display signs of FXTAS. Pediatricians should be aware of the risk of FXTAS within families of children with FXS or a PM and note that carrier parents may be at increased risk for stress related to caring for their own aging parent with FXTAS.
Other Health Risks
There is a subset of boys with the PM who present with some of the physical characteristics seen in FXS, including large ears, high arched palate, flat feet, and macroorchidism.24 Other medical concerns in adults include thyroid problems,4,81,82 fibromyalgia,82–84 migraines or similar headaches,69,85 hypertension,81,86 sleep issues,87,88 neuropathy,69,70,79–81,89–91 and vestibular complaints (eg, unbalanced, disequilibrium).69,70,80,92 These symptoms are seen in carriers with or without FXTAS and often start in young adulthood, particularly hypertension, migraines, or hypothyroidism. Studies that compare symptoms in carrier parents with noncarrier parents caring for children with similar developmental disabilities are needed to sort out the relative contribution of stressful parenting and the genetic risk for these symptoms.93
Knowledge of Carrier Status
Not all children will know about or fully understand their PM status, and pediatricians may be called on to assist parents and other caregivers regarding when and how to inform children or adolescents about their carrier status. In an interview study of attitudes about the timing of carrier testing, parents indicated their primary concern was that their children know and understand their carrier status before becoming sexually active.94 Parents were also concerned about having the appropriate information and ability to support their child in adjusting to their carrier status. Three papers describe results from a longitudinal study of women at risk for the PM before and after finding out their status.95–97 The women who found out they were carriers over the course of this study experienced some initial negative emotions and reported concerns primarily with the impact on their future marriage and motherhood. These women were more likely to endorse early childhood (0–9 years) as the preferred age to be told about carrier status, more so than those who were noncarriers and more so than the age they endorsed before knowing their own status. The primary reason for desiring this information earlier was to provide time to adjust and cope. Ultimately, when parents choose to tell their children about their genetic status is a family decision; however, pediatricians may play a role in helping children and adolescents with a PM understand and cope with their diagnosis.
Carrier Parents of Children With FXS
In addition to being aware of possible risks for their patients with a PM, pediatricians should also be aware that, unless adopted, all of their patients with FXS will have a mother who is herself affected by the PM or FXS (the majority will have a PM). Several studies have examined the impact of raising a child with FXS on maternal health. In general, carrier mothers have elevated rates of stress, depression, anger, and anxiety, with nearly half scoring in the clinically significant range in at least 1 of these areas.54 Carrier mothers also have higher lifetime occurrence rates of mood and some anxiety disorders (eg, agoraphobia and panic disorder) compared with national samples of women.52,98 Based on a survey of 508 FXS families in 2011, one-third of mothers reported having seen a professional to treat depression, anxiety, or stress in the last year, and one-quarter reported taking prescription medication for these symptoms.52,99 Stress is reported to be higher in families of children with FXS than those of children with Down syndrome,100,101 which may be a result of increased child behavioral problems in FXS.54,102–104
A more complex picture of stress in mothers with a PM has emerged in recent work. Mothers at higher genetic risk (eg, those with a lower activation ratio of PM versus normal cells) had lower levels of cortisol the day after their child had multiple episodes of behavior problems than mothers at lower levels of genetic risk.105 Another study of the same sample found that mothers who had between 90 and 105 CGG repeats and experienced above-average numbers of negative life events (eg, death of a friend or family member and financial or health problems) in the previous year had more depressive symptoms, higher anxiety, and lower morning cortisol levels compared with those with higher or lower repeat lengths. The opposite pattern was true for mothers with mid-range CGG repeats who experienced below-average numbers of negative life events. These mothers had the lowest levels of depressive symptoms and anxiety and had typical cortisol awakening levels.106 These studies illustrate how environmental conditions can regulate the stress response in PM carriers.
In contrast to these negative outcomes, mothers of children with FXS have relatively high levels of hope and optimism.54 Compared with other groups, carrier mothers had levels of positive affect equivalent to mothers of typically developing children69 but lower levels of well-being compared with mothers of a child with Down syndrome.100 Hope was also shown to be a strong predictor of quality of life.104 Higher levels of social support and maintaining a social life may reduce potentially negative child and family factors on quality of life and well-being.107
Carrier mothers have elevated rates of adverse physical health symptoms, including a higher proportion of days with headaches, backaches, muscle soreness, fatigue, or hot flashes compared with mothers of children without disabilities.69
Implications for the Extended Family
The impact on the extended family is an important consideration for a heritable condition, such as FXS. In a recent pilot study of cascade testing as a result of newborn screening for FXS, Sorensen et al108 reported on 27 extended family members who were identified as having an FMR1 mutation resulting from the identification of 14 newborns. This finding highlights the potential challenges for immediate family members regarding communication with extended relatives (ie, ethical implications of providing versus withholding information). Anxiety may be expected to be heightened as a result of receiving any medically relevant news. For inherited conditions, this anxiety may be multiplied as family members consider the impact for multiple loved ones throughout a family system. For example, the parents of a newly diagnosed child may need to consider the possible impact of an FMR1 expansion on not only the child and carrier parent, but also the possibility of a grandparent developing FXTAS, as well as the reproductive impact for siblings, aunts, or cousins.109 Future reproductive decisions will also be impacted. In qualitative interview studies of reproductive decisions made by carrier mothers,110,111 the majority (77%) had decided not to have more biological children because of the 50% risk of passing on the mutation to their child. The impact of an FMR1 mutation can reach many family members, and this “family spillover” of consequences is an important reality for pediatricians to consider in their support of the family system.
Implications for Pediatricians
As primary care physicians, pediatricians are in a unique position to support children, their parents, and extended family members regarding both PM and FXS problems. Boys with the PM are at higher risk than the general population for ADHD, anxiety, and social deficits21,47 and these problems usually require an evaluation and often multimodality treatment, such as medication and counseling. Seizures can occur in 8% to 13% of carriers,47 and other medical problems, such as hypertension, migraines, immune-mediated, and endocrine problems, generally develop in adulthood, but could potentially arise in adolescent carriers. Therefore, pediatricians should be alert to the increased risk for these problems in their patients.
Pediatricians will encounter carrier children because the PM is common in the general population; however, the majority of individuals with the PM will not know they are carriers. For this reason, pediatricians are on the front line when it comes to identifying the spectrum of problems that can arise in PM carriers. Although most of the carriers that they will see will not have overt developmental problems, there are a significant number of children who will have challenges, and there may be an increased risk of susceptibility to stressful situations for all carriers, regardless of their clinical involvement. Even among those without medical or neurocognitive concerns, it will be important to emphasize general guidance regarding staying healthy to decrease risk,112 as well as encouraging stress reduction and positive coping mechanisms to promote resilience.
Pediatricians may want to review the whole family tree of children with FXS or a PM, because these pedigrees often have extensive involvement.109 Pediatricians can help increase awareness of and support families in receiving services, such as referrals for genetic testing and counseling, behavioral therapies, psychological counseling, psychopharmacology, and educational interventions. This support includes services for a clinically referred child, as well as other affected family members. For instance, pediatricians can provide encouragement for the mother to receive treatment for the anxiety or depression that she may be experiencing, which could have a significant impact on the environment and mental health of her children. Pediatricians can also guide the family in genetic testing of other family members and facilitate or order fragile X DNA testing and assist with managing insurance concerns.
Conclusions
Several important questions remain unanswered with regards to the FMR1 PM. These questions form the basis for future research directions.
What is the true prevalence and severity of symptoms and comorbid conditions associated with PM status? Although the prevalence of the FMR1 PM is now better understood, the penetrance and range of severity of associated symptoms is not as well known, nor is the developmental trajectory of associated features. This is especially true outside of the documented conditions of FXPOI and FXTAS. Several medical, psychiatric, and cognitive features have been noted to possibly or likely be related to the PM,5 but are in need of more empirical documentation. This information is needed to better describe the public health burden of the PM.
What mechanistic factors can be used to predict who is at the greatest risk for which outcomes? An important question for researchers is why some individuals with a PM develop cognitive, emotional, and medical conditions whereas others do not. There is some evidence that the higher the number of CGG repeats is within the PM range, the earlier the onset of FXTAS, the greater the level of RNA toxicity and the lower the level of FMRP, which in itself can lead to developmental problems.8,9,14 This association requires additional investigation, including possible mediating or protective factors. Identification of preventive measures could enable public health programs to make large strides in improving outcomes for the PM population. Another cause of clinical involvement in PM carriers is the presence of an additional genetic abnormality or a CNV. Because the PM itself can lead to oxidative stress and early cell death in culture,113 the addition of a CNV or other genetic lesion may have an additive effect with the PM, whereas by itself it may or may not have a clinical phenotype.114 There is clearly a spectrum of affectedness, but it is unclear what mechanisms contribute to this spectrum.
To what extent do environmental factors play a role in outcomes? In addition to molecular mechanisms, it also remains unclear as to whether the risks for known conditions (eg, FXPOI and FXTAS) and associated features develop due to cumulative genetic risk, a genetic susceptibility to stress, exposure to stress, or some other genetic or environmental influence. Although some findings regarding the impact of the PM on children can be extrapolated from studies of adults, there is a significant need for more studies focusing on younger individuals. Studies examining the medical, developmental, and emotional trajectories of younger individuals with the PM are currently underway and should shed light on the development of these conditions. The potential differential susceptibility to stress for individuals with a PM93 is another important area for future investigation, especially the potential consequences for cumulative stress for children and adolescents with it.
What treatments or environmental modifications could prevent or reduce the severity of symptoms? From a molecular viewpoint, there is oxidative stress and mitochondrial dysfunction in the cells of PM carriers both with and without FXTAS.10,115,116 Because of these problems, recommendations have been made for the use of antioxidants, healthy eating, and regular exercise to enhance mitochondrial function, increase serotonin levels, and promote neurogenesis.112 There is limited research on treatment studies for the learning, emotional, and stress problems seen in some carriers, and the impact of multiple family members with FMR1 mutations on the family system is not clear. Studies addressing these issues could provide needed information to guide treatment of carriers with clinical problems.
Acknowledgments
We thank Don Bailey who reviewed earlier drafts of the manuscript. We thank the individuals with the premutation and their families for teaching us what we know.
Glossary
- ADHD
attention-deficit/hyperactivity disorder
- ASD
autism spectrum disorder
- CNV
copy number variant
- EF
executive function
- FMRP
fragile X mental retardation protein
- FXAD
fragile X–associated disorder
- FXPOI
fragile X–associated primary ovarian insufficiency
- FXS
fragile X syndrome
- FXTAS
fragile X–associated tremor ataxia syndrome
- PM
premutation
Footnotes
Dr Wheeler conceptualized and designed the study, conducted the literature review, and drafted the initial manuscript; Dr Raspa conceptualized and designed the study, conducted the literature review, and reviewed and revised the manuscript; Dr Hagerman reviewed and revised the manuscript, and contributed clinical knowledge to the Implications for Pediatricians section; Dr Mailick reviewed and revised the manuscript; Dr Riley conceptualized and designed the study and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
FUNDING: This literature review was supported by Centers for Disease Control and Prevention (CDC) contract 200-2007-22644-0013. The manuscript development was supported by the CDC, the National Institute of Child Health and Human Development, National Institutes of Health (grants HD 036071 and HD03110), and RTI International. The findings and conclusions in this publication are those of the authors and do not necessarily represent the views of CDC. Funded by the National Institutes of Health (NIH).
References
- 1.Hagerman R, Hagerman P. Advances in clinical and molecular understanding of the FMR1 premutation and fragile X-associated tremor/ataxia syndrome. Lancet Neurol. 2013;12(8):786–798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crum-Bailey JM, Dennison DH, Weiner WJ, Hawley JS. The neurology and corresponding genetics of fragile X disorders: insights into the genetics of neurodegeneration. Future Neurol. 2013;8(2):225–235 [Google Scholar]
- 3.Kraan CM, Hocking DR, Bradshaw JL, et al. Neurobehavioural evidence for the involvement of the FMR1 gene in female carriers of fragile X syndrome. Neurosci Biobehav Rev. 2013;37(3):522–547 [DOI] [PubMed] [Google Scholar]
- 4.Rodriguez-Revenga L, Madrigal I, Pagonabarraga J, et al. Penetrance of FMR1 premutation associated pathologies in fragile X syndrome families. Eur J Hum Genet. 2009;17(10):1359–1362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wheeler AC, Bailey DB Jr, Berry-Kravis E, et al. Associated features in females with an FMR1 premutation. J Neurodev Disord. 2014;6(1):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hunsaker MR. Neurocognitive endophenotypes in CGG KI and Fmr1 KO mouse models of Fragile X-Associated disorders: an analysis of the state of the field. F1000 Res. 2013;2:287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berman RF, Buijsen RA, Usdin K, et al. Mouse models of the fragile X premutation and fragile X-associated tremor/ataxia syndrome. J Neurodev Disord. 2014;6(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ludwig AL, Espinal GM, Pretto DI, et al. CNS expression of murine fragile X protein (FMRP) as a function of CGG-repeat size. Hum Mol Genet. 2014;23(12):3228–3238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pretto DI, Mendoza-Morales G, Lo J, et al. CGG allele size somatic mosaicism and methylation in FMR1 premutation alleles. J Med Genet. 2014;51(5):309–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cao Z, Hulsizer S, Tassone F, et al. Clustered burst firing in FMR1 premutation hippocampal neurons: amelioration with allopregnanolone. Hum Mol Genet. 2012;21(13):2923–2935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sellier C, Rau F, Liu Y, et al. Sam68 sequestration and partial loss of function are associated with splicing alterations in FXTAS patients. EMBO J. 2010;29(7):1248–1261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sellier C, Freyermuth F, Tabet R, et al. Sequestration of DROSHA and DGCR8 by expanded CGG RNA repeats alters microRNA processing in fragile X-associated tremor/ataxia syndrome. Cell Rep. 2013;3(3):869–880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen E, Sharma MR, Shi X, Agrawal RK, Joseph S. Fragile X mental retardation protein regulates translation by binding directly to the ribosome. Mol Cell. 2014;54(3):407–417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hagerman P. Fragile X-associated tremor/ataxia syndrome (FXTAS): pathology and mechanisms. Acta Neuropathol. 2013;126(1):1–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lozano R, Summers S, Lozano C, et al. Association between macroorchidism and intelligence in FMR1 premutation carriers. Am J Med Genet A. 2014;164A(9):2206–2211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sellier C, Usdin K, Pastori C, Peschansky VJ, Tassone F, Charlet-Berguerand N. The multiple molecular facets of fragile X-associated tremor/ataxia syndrome. J Neurodev Disord. 2014;6(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Todd PK, Oh SY, Krans A, et al. CGG repeat-associated translation mediates neurodegeneration in fragile X tremor ataxia syndrome. Neuron. 2013;78(3):440–455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hagerman R, O’Connor R, Staley L. Mild clinical involvement in two males with a large FMR1 premutation. Am J Hum Genet. 1994;55(CONF-941009--) [Google Scholar]
- 19.Renda MM, Voigt RG, Babovic-Vuksanovic D, et al. Neurodevelopmental disabilities in children with intermediate and premutation range fragile X cytosine-guanine-guanine expansions. J Child Neurol. 2014;29(3):326–330 [DOI] [PubMed] [Google Scholar]
- 20.Bailey DB Jr, Raspa M, Olmsted M, Holiday DB. Co-occurring conditions associated with FMR1 gene variations: findings from a national parent survey. Am J Med Genet A. 2008;146A(16):2060–2069 [DOI] [PubMed] [Google Scholar]
- 21.Farzin F, Perry H, Hessl D, et al. Autism spectrum disorders and attention-deficit/hyperactivity disorder in boys with the fragile X premutation. J Dev Behav Pediatr. 2006;27(Suppl 2):S137–S144 [DOI] [PubMed] [Google Scholar]
- 22.Myers GF, Mazzocco MM, Maddalena A, Reiss AL. No widespread psychological effect of the fragile X premutation in childhood: evidence from a preliminary controlled study. J Dev Behav Pediatr. 2001;22(6):353–359 [DOI] [PubMed] [Google Scholar]
- 23.Tassone F, Hagerman RJ, Taylor AK, et al. Clinical involvement and protein expression in individuals with the FMR1 premutation. Am J Med Genet. 2000;91(2):144–152 [DOI] [PubMed] [Google Scholar]
- 24.Aziz M, Stathopulu E, Callias M, et al. Clinical features of boys with fragile X premutations and intermediate alleles. Am J Med Genet B Neuropsychiatr Genet. 2003;121B(1):119–127 [DOI] [PubMed] [Google Scholar]
- 25.Goodlin-Jones BL, Tassone F, Gane LW, Hagerman RJ. Autistic spectrum disorder and the fragile X premutation. J Dev Behav Pediatr. 2004;25(6):392–398 [DOI] [PubMed] [Google Scholar]
- 26.Loesch DZ, Bui QM, Grigsby J, et al. Effect of the fragile X status categories and the fragile X mental retardation protein levels on executive functioning in males and females with fragile X. Neuropsychology. 2003;17(4):646–657 [DOI] [PubMed] [Google Scholar]
- 27.Adams PE, Adams JS, Nguyen DV, et al. Psychological symptoms correlate with reduced hippocampal volume in fragile X premutation carriers. Am J Med Genet B Neuropsychiatr Genet. 2010;153B(3):775–785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Allen EG, Sherman S, Abramowitz A, et al. Examination of the effect of the polymorphic CGG repeat in the FMR1 gene on cognitive performance. Behav Genet. 2005;35(4):435–445 [DOI] [PubMed] [Google Scholar]
- 29.Franke P, Leboyer M, Hardt J, et al. Neuropsychological profiles of FMR-1 premutation and full-mutation carrier females. Psychiatry Res. 1999;87(2–3):223–231 [DOI] [PubMed] [Google Scholar]
- 30.Adams JS, Adams PE, Nguyen D, et al. Volumetric brain changes in females with fragile X-associated tremor/ataxia syndrome (FXTAS). Neurology. 2007;69(9):851–859 [DOI] [PubMed] [Google Scholar]
- 31.Grigsby J, Brega AG, Engle K, et al. Cognitive profile of fragile X premutation carriers with and without fragile X-associated tremor/ataxia syndrome. Neuropsychology. 2008;22(1):48–60 [DOI] [PubMed] [Google Scholar]
- 32.Grigsby J, Cornish K, Hocking D, et al. The cognitive neuropsychological phenotype of carriers of the FMR1 premutation. J Neurodev Disord. 2014;6(1):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goodrich-Hunsaker NJ, Wong LM, McLennan Y, et al. Adult female fragile X premutation carriers exhibit age- and CGG repeat length-related impairments on an attentionally based enumeration task. Front Hum Neurosci. 2011;5:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Losh M, Klusek J, Martin GE, Sideris J, Parlier M, Piven J. Defining genetically meaningful language and personality traits in relatives of individuals with fragile X syndrome and relatives of individuals with autism. Am J Med Genet B Neuropsychiatr Genet. 2012;159B(6):660–668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sterling AM, Mailick M, Greenberg J, Warren SF, Brady N. Language dysfluencies in females with the FMR1 premutation. Brain Cogn. 2013;82(1):84–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cornish KM, Li L, Kogan CS, et al. Age-dependent cognitive changes in carriers of the fragile X syndrome. Cortex. 2008;44(6):628–636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lachiewicz AM, Dawson DV, Spiridigliozzi GA, McConkie-Rosell A. Arithmetic difficulties in females with the fragile X premutation. Am J Med Genet A. 2006;140(7):665–672 [DOI] [PubMed] [Google Scholar]
- 38.Gallego PK, Burris JL, Rivera SM. Visual motion processing deficits in infants with the fragile X premutation. J Neurodev Disord. 2014;6(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hunsaker MR, Goodrich-Hunsaker NJ, Willemsen R, Berman RF. Temporal ordering deficits in female CGG KI mice heterozygous for the fragile X premutation. Behav Brain Res. 2010;213(2):263–268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Van Dam D, Errijgers V, Kooy RF, et al. Cognitive decline, neuromotor and behavioural disturbances in a mouse model for fragile-X-associated tremor/ataxia syndrome (FXTAS). Behav Brain Res. 2005;162(2):233–239 [DOI] [PubMed] [Google Scholar]
- 41.Hunter JE, Allen EG, Abramowitz A, et al. No evidence for a difference in neuropsychological profile among carriers and noncarriers of the FMR1 premutation in adults under the age of 50. Am J Hum Genet. 2008;83(6):692–702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hunter JE, Epstein MP, Tinker SW, Abramowitz A, Sherman SL. The FMR1 premutation and attention-deficit hyperactivity disorder (ADHD): evidence for a complex inheritance. Behav Genet. 2012;42(3):415–422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Clifford S, Dissanayake C, Bui QM, Huggins R, Taylor AK, Loesch DZ. Autism spectrum phenotype in males and females with fragile X full mutation and premutation. J Autism Dev Disord. 2007;37(4):738–747 [DOI] [PubMed] [Google Scholar]
- 44.Developmental Disabilities Monitoring Network Surveillance Year 2010 Principal Investigators; Centers for Disease Control and Prevention . Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2010. MMWR Surveill Summ. 2014;63(2):1–21 [PubMed] [Google Scholar]
- 45.Franke P, Leboyer M, Gänsicke M, et al. Genotype-phenotype relationship in female carriers of the premutation and full mutation of FMR-1. Psychiatry Res. 1998;80(2):113–127 [DOI] [PubMed] [Google Scholar]
- 46.Hessl D, Rivera SM, Reiss AL. The neuroanatomy and neuroendocrinology of fragile X syndrome. Ment Retard Dev Disabil Res Rev. 2004;10(1):17–24 [DOI] [PubMed] [Google Scholar]
- 47.Chonchaiya W, Au J, Schneider A, et al. Increased prevalence of seizures in boys who were probands with the FMR1 premutation and co-morbid autism spectrum disorder. Hum Genet. 2012;131(4):581–589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Reiss AL, Freund L, Abrams MT, Boehm C, Kazazian H. Neurobehavioral effects of the fragile X premutation in adult women: a controlled study. Am J Hum Genet. 1993;52(5):884–894 [PMC free article] [PubMed] [Google Scholar]
- 49.Sobesky WE, Pennington BF, Porter D, Hull CE, Hagerman RJ. Emotional and neurocognitive deficits in fragile X. Am J Med Genet. 1994;51(4):378–385 [DOI] [PubMed] [Google Scholar]
- 50.Johnston C, Eliez S, Dyer-Friedman J, et al. Neurobehavioral phenotype in carriers of the fragile X premutation. Am J Med Genet. 2001;103(4):314–319 [PubMed] [Google Scholar]
- 51.Hunter JE, Allen EG, Abramowitz A, et al. Investigation of phenotypes associated with mood and anxiety among male and female fragile X premutation carriers. Behav Genet. 2008;38(5):493–502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Roberts JE, Bailey DB Jr, Mankowski J, et al. Mood and anxiety disorders in females with the FMR1 premutation. Am J Med Genet B Neuropsychiatr Genet. 2009;150B(1):130–139 [DOI] [PubMed] [Google Scholar]
- 53.Bourgeois JA, Coffey SM, Rivera SM, et al. A review of fragile X premutation disorders: expanding the psychiatric perspective. J Clin Psychiatry. 2009;70(6):852–862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bailey DB Jr, Sideris J, Roberts J, Hatton D. Child and genetic variables associated with maternal adaptation to fragile X syndrome: a multidimensional analysis. Am J Med Genet A. 2008;146A(6):720–729 [DOI] [PubMed] [Google Scholar]
- 55.Thompson NM, Rogeness GA, McClure E, Clayton R, Johnson C. Influence of depression on cognitive functioning in Fragile X females. Psychiatry Res. 1996;64(2):97–104 [DOI] [PubMed] [Google Scholar]
- 56.Ashworth A, Abusaad I, Walsh C, et al. Linkage analysis of the fragile X gene FMR-1 and schizophrenia: no evidence for linkage but report of a family with schizophrenia and an unstable triplet repeat. Psychiatr Genet. 1996;6(2):81–86 [DOI] [PubMed] [Google Scholar]
- 57.Al-Semaan Y, Malla AK, Lazosky A. Schizoaffective disorder in a fragile-X carrier. Aust N Z J Psychiatry. 1999;33(3):436–440 [DOI] [PubMed] [Google Scholar]
- 58.Khin NA, Tarleton J, Raghu B, Park SK. Clinical description of an adult male with psychosis who showed FMR1 gene methylation mosaicism. Am J Med Genet. 1998;81(3):222–224 [DOI] [PubMed] [Google Scholar]
- 59.Bernard PB, Castano AM, O’Leary H, Simpson K, Browning MD, Benke TA. Phosphorylation of FMRP and alterations of FMRP complex underlie enhanced mLTD in adult rats triggered by early life seizures. Neurobiol Dis. 2013;59:1–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.van Eeghen AM, Pulsifer MB, Merker VL, et al. Understanding relationships between autism, intelligence, and epilepsy: a cross-disorder approach. Dev Med Child Neurol. 2013;55(2):146–153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sullivan SD, Welt C, Sherman S. FMR1 and the continuum of primary ovarian insufficiency. Semin Reprod Med. 2011;29(4):299–307 [DOI] [PubMed] [Google Scholar]
- 62.Spath MA, Feuth TB, Allen EG, et al. Intra-individual stability over time of standardized anti-Mullerian hormone in FMR1 premutation carriers. Hum Reprod. 2011;26(8):2185–2191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sullivan AK, Marcus M, Epstein MP, et al. Association of FMR1 repeat size with ovarian dysfunction. Hum Reprod. 2005;20(2):402–412 [DOI] [PubMed] [Google Scholar]
- 64.Murray A, Ennis S, MacSwiney F, Webb J, Morton NE. Reproductive and menstrual history of females with fragile X expansions. Eur J Hum Genet. 2000;8(4):247–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hundscheid RD, Braat DD, Kiemeney LA, Smits AP, Thomas CM. Increased serum FSH in female fragile X premutation carriers with either regular menstrual cycles or on oral contraceptives. Hum Reprod. 2001;16(3):457–462 [DOI] [PubMed] [Google Scholar]
- 66.Welt CK. Primary ovarian insufficiency: a more accurate term for premature ovarian failure. Clin Endocrinol (Oxf). 2008;68(4):499–509 [DOI] [PubMed] [Google Scholar]
- 67.Rohr J, Allen EG, Charen K, et al. Anti-Mullerian hormone indicates early ovarian decline in fragile X mental retardation (FMR1) premutation carriers: a preliminary study. Hum Reprod. 2008;23(5):1220–1225 [DOI] [PubMed] [Google Scholar]
- 68.Allen EG, Sullivan AK, Marcus M, et al. Examination of reproductive aging milestones among women who carry the FMR1 premutation. Hum Reprod. 2007;22(8):2142–2152 [DOI] [PubMed] [Google Scholar]
- 69.Smith LE, Seltzer MM, Greenberg JS. Daily health symptoms of mothers of adolescents and adults with fragile x syndrome and mothers of adolescents and adults with autism spectrum disorder. J Autism Dev Disord. 2012;42(9):1836–1846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Seltzer MM, Baker MW, Hong J, Maenner M, Greenberg J, Mandel D. Prevalence of CGG expansions of the FMR1 gene in a US population-based sample. Am J Med Genet B Neuropsychiatr Genet. 2012;159B(5):589–597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Murray A. Premature ovarian failure and the FMR1 gene. Semin Reprod Med. 2000;18(1):59–66 [DOI] [PubMed] [Google Scholar]
- 72.Ennis S, Ward D, Murray A. Nonlinear association between CGG repeat number and age of menopause in FMR1 premutation carriers. Eur J Hum Genet. 2006;14(2):253–255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mailick MR, Hong J, Greenberg J, Smith L, Sherman S. Curvilinear association of CGG repeats and age at menopause in women with FMR1 premutation expansions. Am J Med Genet B Neuropsychiatr Genet. 2014;165B(8):705–711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tejada MI, García-Alegría E, Bilbao A, et al. Analysis of the molecular parameters that could predict the risk of manifesting premature ovarian failure in female premutation carriers of fragile X syndrome. Menopause. 2008;15(5):945–949 [DOI] [PubMed] [Google Scholar]
- 75.Bianchi ML. Osteoporosis in children and adolescents. Bone. 2007;41(4):486–495 [DOI] [PubMed] [Google Scholar]
- 76.De Caro JJ, Dominguez C, Sherman SL. Reproductive health of adolescent girls who carry the FMR1 premutation: expected phenotype based on current knowledge of fragile x-associated primary ovarian insufficiency. Ann N Y Acad Sci. 2008;1135:99–111 [DOI] [PubMed] [Google Scholar]
- 77.Tassone F, Berry-Kravis EM, eds. Fragile X-Associated Tremor Ataxia Syndrome (FXTAS). New York, NY: Springer; 2010:188 [Google Scholar]
- 78.Leehey MA, Berry-Kravis E, Goetz CG, et al. FMR1 CGG repeat length predicts motor dysfunction in premutation carriers. Neurology. 2008;70(16 Pt 2):1397–1402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tassone F, Greco CM, Hunsaker MR, et al. Neuropathological, clinical and molecular pathology in female fragile X premutation carriers with and without FXTAS. Genes Brain Behav. 2012;11(5):577–585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chonchaiya W, Nguyen DV, Au J, et al. Clinical involvement in daughters of men with fragile X-associated tremor ataxia syndrome. Clin Genet. 2010;78(1):38–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Coffey SM, Cook K, Tartaglia N, et al. Expanded clinical phenotype of women with the FMR1 premutation. Am J Med Genet A. 2008;146A(8):1009–1016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Winarni TI, Chonchaiya W, Sumekar TA, et al. Immune-mediated disorders among women carriers of fragile X premutation alleles. Am J Med Genet A. 2012;158A(10):2473–2481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Martorell L, Tondo M, Garcia-Fructuoso F, et al. Screening for the presence of FMR1 premutation alleles in a Spanish population with fibromyalgia. Clin Rheumatol. 2012;31(11):1611–1615 [DOI] [PubMed] [Google Scholar]
- 84.Rodriguez-Revenga L, Madrigal I, Blanch-Rubió J, et al. Screening for the presence of FMR1 premutation alleles in women with fibromyalgia. Gene. 2013;512(2):305–308 [DOI] [PubMed] [Google Scholar]
- 85.Au J, Akins RS, Berkowitz-Sutherland L, et al. Prevalence and risk of migraine headaches in adult fragile X premutation carriers. Clin Genet. 2013;84(6):546–551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hamlin AA, Sukharev D, Campos L, et al. Hypertension in FMR1 premutation males with and without fragile X-associated tremor/ataxia syndrome (FXTAS). Am J Med Genet A. 2012;158A(6):1304–1309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hamlin A, Liu Y, Nguyen DV, Tassone F, Zhang L, Hagerman RJ. Sleep apnea in fragile X premutation carriers with and without FXTAS. Am J Med Genet B Neuropsychiatr Genet. 2011;156B(8):923–928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Summers SM, Cogswell J, Goodrich JE, et al. Prevalence of restless legs syndrome and sleep quality in carriers of the fragile X premutation. Clin Genet. 2014;86(2):181–184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Berry-Kravis E, Goetz CG, Leehey MA, et al. Neuropathic features in fragile X premutation carriers. Am J Med Genet A. 2007;143A(1):19–26 [DOI] [PubMed] [Google Scholar]
- 90.Hagerman RJ, Leavitt BR, Farzin F, et al. Fragile-X-associated tremor/ataxia syndrome (FXTAS) in females with the FMR1 premutation. Am J Hum Genet. 2004;74(5):1051–1056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Soontarapornchai K, Maselli R, Fenton-Farrell G, et al. Abnormal nerve conduction features in fragile X premutation carriers. Arch Neurol. 2008;65(4):495–498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wheeler AC, Raspa M, Green A, et al. Health and reproductive experiences of women with an FMR1 premutation with and without fragile X premature ovarian insufficiency. Front Genet. 2014;5:300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Seltzer MM, Barker ET, Greenberg JS, Hong J, Coe C, Almeida D. Differential sensitivity to life stress in FMR1 premutation carrier mothers of children with fragile X syndrome. Health Psychol. 2012;31(5):612–622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.McConkie-Rosell A, Spiridigliozzi GA, Rounds K, et al. Parental attitudes regarding carrier testing in children at risk for fragile X syndrome. Am J Med Genet. 1999;82(3):206–211 [PubMed] [Google Scholar]
- 95.McConkie-Rosell A, Spiridigliozzi GA, Sullivan JA, Dawson DV, Lachiewicz AM. Carrier testing in fragile X syndrome: effect on self-concept. Am J Med Genet. 2000;92(5):336–342 [DOI] [PubMed] [Google Scholar]
- 96.McConkie-Rosell A, Spiridigliozzi GA, Sullivan JA, Dawson DV, Lachiewicz AM. Longitudinal study of the carrier testing process for fragile X syndrome: perceptions and coping. Am J Med Genet. 2001;98(1):37–45 [PubMed] [Google Scholar]
- 97.McConkie-Rosell A, Spiridigliozzi GA, Sullivan JA, Dawson DV, Lachiewicz AM. Carrier testing in fragile X syndrome: when to tell and test. Am J Med Genet. 2002;110(1):36–44 [DOI] [PubMed] [Google Scholar]
- 98.Wheeler A, Hatton D, Reichardt A, Bailey D. Correlates of maternal behaviours in mothers of children with fragile X syndrome. J Intellect Disabil Res. 2007;51(Pt 6):447–462 [DOI] [PubMed] [Google Scholar]
- 99.Bailey DB Jr, Raspa M, Bishop E, et al. Health and economic consequences of fragile X syndrome for caregivers. J Dev Behav Pediatr. 2012;33(9):705–712 [DOI] [PubMed] [Google Scholar]
- 100.Abbeduto L, Seltzer MM, Shattuck P, Krauss MW, Orsmond G, Murphy MM. Psychological well-being and coping in mothers of youths with autism, Down syndrome, or fragile X syndrome. Am J Ment Retard. 2004;109(3):237–254 [DOI] [PubMed] [Google Scholar]
- 101.Lanfranchi S, Vianello R. Stress, locus of control, and family cohesion and adaptability in parents of children with Down, Williams, Fragile X, and Prader-Willi syndromes. Am J Intellect Dev Disabil. 2012;117(3):207–224 [DOI] [PubMed] [Google Scholar]
- 102.Hall SS, Burns DD, Reiss AL. Modeling family dynamics in children with fragile x syndrome. J Abnorm Child Psychol. 2007;35(1):29–42 [DOI] [PubMed] [Google Scholar]
- 103.Johnston C, Hessl D, Blasey C, et al. Factors associated with parenting stress in mothers of children with fragile X syndrome. J Dev Behav Pediatr. 2003;24(4):267–275 [DOI] [PubMed] [Google Scholar]
- 104.Wheeler AC, Skinner DG, Bailey DB. Perceived quality of life in mothers of children with fragile X syndrome. Am J Ment Retard. 2008;113(3):159–177 [DOI] [PubMed] [Google Scholar]
- 105.Hartley SL, Seltzer MM, Hong J, et al. Cortisol response to behavior problems in FMR1 premutation mothers of adolescents and adults with fragile X syndrome: a diathesis-stress model. Int J Behav Dev. 2012;36(1):53–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Seltzer MM, Greenberg JS, Hong J, et al. Maternal cortisol levels and behavior problems in adolescents and adults with ASD. J Autism Dev Disord. 2010;40(4):457–469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Raspa M, Bailey DB Jr, Bann C, Bishop E. Modeling family adaptation to fragile X syndrome. Am J Intellect Dev Disabil. 2014;119(1):33–48 [DOI] [PubMed] [Google Scholar]
- 108.Sorensen PL, Gane LW, Yarborough M, Hagerman RJ, Tassone F. Newborn screening and cascade testing for FMR1 mutations. Am J Med Genet A. 2013;161A(1):59–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Visootsak J, Hipp H, Clark H, Berry-Kravis E, Anderson T, Laney D. Climbing the branches of a family tree: diagnosis of fragile X syndrome. J Pediatr. 2014;164(6):1292–1295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Raspberry KA, Skinner D. Negotiating desires and options: how mothers who carry the fragile X gene experience reproductive decisions. Soc Sci Med. 2011;72(6):992–998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Raspberry K, Skinner D. Enacting genetic responsibility: experiences of mothers who carry the fragile X gene. Sociol Health Illn. 2011;33(3):420–433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Polussa J, Schneider A, Hagerman R. Molecular advances leading to treatment implications for fragile X premutation carriers. Brain Disord Ther. 2014;3:1000119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Chen Y, Tassone F, Berman RF, et al. Murine hippocampal neurons expressing Fmr1 gene premutations show early developmental deficits and late degeneration. Hum Mol Genet. 2010;19(1):196–208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lozano R, Hagerman RJ, Duyzend M, Budimirovic DB, Eichler EE, Tassone F. Genomic studies in fragile X premutation carriers. J Neurodev Disord. 2014;6(1):27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Napoli E, Ross-Inta C, Wong S, et al. Mitochondrial dysfunction in Pten haplo-insufficient mice with social deficits and repetitive behavior: interplay between Pten and p53. PLoS One. 2012;7(8):e42504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ross-Inta C, Omanska-Klusek A, Wong S, et al. Evidence of mitochondrial dysfunction in fragile X-associated tremor/ataxia syndrome. Biochem J. 2010;429(3):545–552 [DOI] [PMC free article] [PubMed] [Google Scholar]