Abstract
Os acromiale occur frequently in the population and can be a cause of significant shoulder dysfunction and rotator cuff impingement. When symptomatic os acromiale fail conservative management, surgical intervention may become necessary. The purpose of this article is to describe our preferred surgical technique for osteosynthesis of os acromiale using cannulated screws and tension-band wiring.
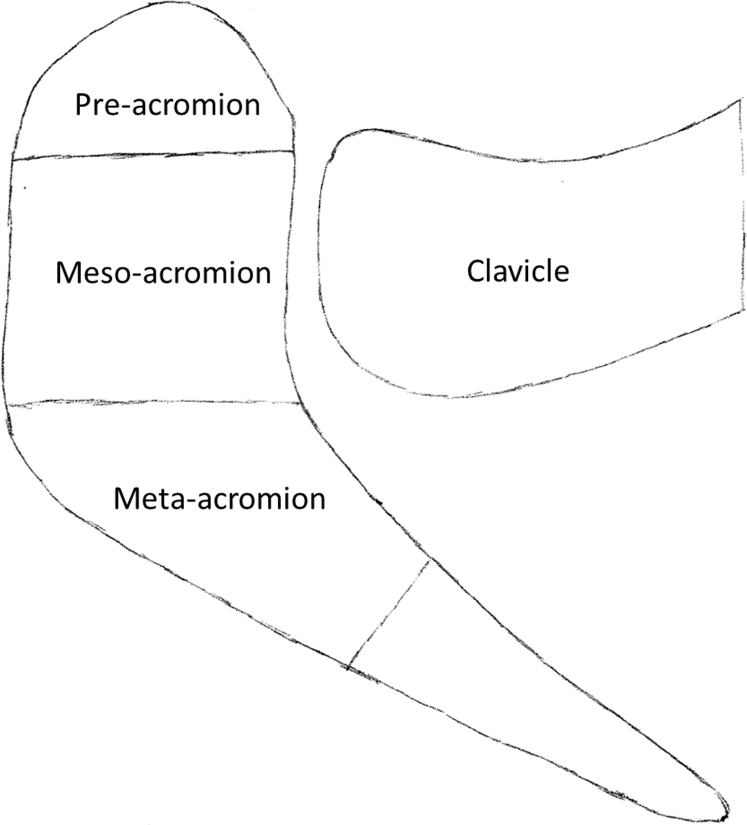
Os acromiale is defined as an unfused ossification center of the acromion and can be classified as one of 3 different types named for the unfused segment immediately anterior to the nonunion (Fig 1).1 Of the 3 types, the meso-type is the most common.2 Overall, os acromiale are widespread in the population, occurring in 8% of individuals.3 They can be asymptomatic and thus require no specific treatment4; however, for those that do cause symptoms, conservative therapy often fails, thereby leading to the need for surgical intervention.1, 5 Additionally, os acromiale have often been found to be associated with rotator cuff tears.1, 5, 6, 7 In the context of a rotator cuff tear, stabilization of the os acromiale may prevent further rotator cuff impingement and damage due to dynamic impingement.1 Historically, the choice of treatment for symptomatic os acromiale has chiefly depended on the size of the os acromiale.1 Excision, either arthroscopic or open, is reserved for pre-acromion–type os acromiale. Removal of larger fragments may result in deltoid dysfunction due to the deltoid muscle's origin at the acromion's lateral edge.5 For all other types, osteosynthesis is commonly recognized as the treatment of choice.1
Fig 1.
Illustration of left acromion and clavicle from a superior view. The ossification centers, pre-acromion, meso-acromion, and meta-acromion, are illustrated. In general, the type of os acromiale is defined by the unfused segment immediately anterior to the nonunion.
The purpose of this article and Video 1 is to describe our preferred technique of osteosynthesis for a symptomatic meso-type os acromiale after concomitant arthroscopic rotator cuff repair. Advantages and disadvantages for this technique are outlined in Table 1.
Table 1.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| The fixation construct with cannulated screws and tension bands has a high load-to-failure8 | Removal of hardware may be required |
| Transacromial approach results in an improved rate of bony union9 | |
| The wire-crossover technique of the tension-band construct resists the inferior bending moment of the deltoid and ensures that the loads are evenly distributed over the acromion |
Surgical Technique
Preoperative Planning
Os acromiale is a common finding; however, operative management is only indicated when the patient suffers from persistent symptoms like pain or functional deficits after a trial of conservative treatment. Moreover, a highly unstable os acromiale should be fixed to prevent its acting as a contributing factor to subacromial impingement and further rotator cuff damage. The clinical history and physical examination findings for os acromiale can be similar to the clinical presentation of an extra-articular shoulder impingement syndrome.1 Patients often report chronic symptoms including limited range of motion (ROM) in overhead activities and pain during the night while lying on the affected side. Palpation of the nonunion typically causes tenderness and discomfort. Clinical examination may reveal pain with impingement signs, painful ROM, and rotator cuff weakness. Gross motion of the anterior acromion is a unique clinical finding that suggests symptomatic os acromiale.
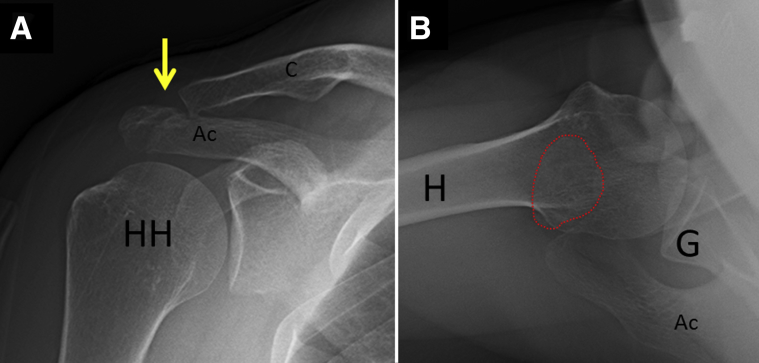
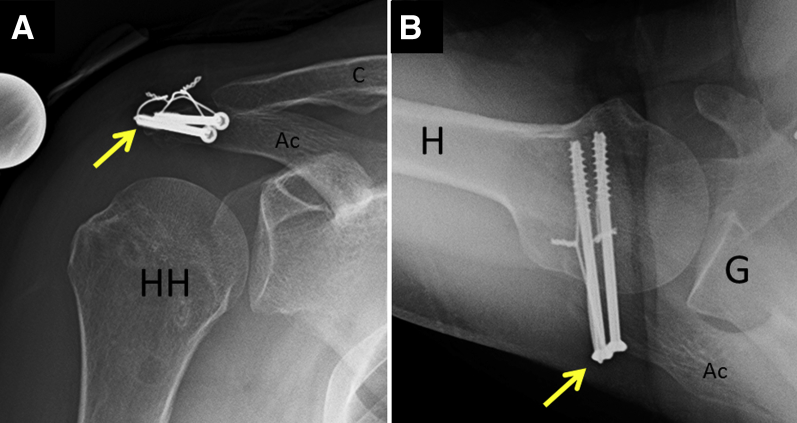
Imaging evaluation should always include anteroposterior, scapular Y, and axillary radiographs (Fig 2). Of these views, the axillary is the most helpful to identify the os acromiale and should be evaluated thoroughly. Magnetic resonance imaging (MRI) should additionally be performed to identify additional shoulder pathology, such as a concomitant rotator cuff tear.
Fig 2.
Preoperative radiographs of a right shoulder showing an os acromiale. (A) Anteroposterior view with the site of nonunion (arrow) somewhat visible. (B) Axillary view showing the best visualization of the os acromiale (red dotted line), in this case a meso-type. (Ac, acromion; C, clavicle; G, glenoid; H, humerus; HH, humeral head.)
A diagnostic injection with a local anesthetic into the site of nonunion may also help to determine whether the os acromiale is a pain generator. As such, comprehensive preoperative evaluation is advocated to determine whether the patient requires surgical management.
Anesthesia and Patient Positioning
After the induction of general anesthesia and placement of a regional interscalene block, the patient is placed in the beach-chair position, and the operative extremity is situated in a pneumatic arm holder (Tenet T-Max Beach Chair and Spider arm positioner; Smith & Nephew, Memphis, TN). The affected shoulder and axilla are prepared and draped using sterile techniques. The bony landmarks of the os acromiale and acromion, clavicle, acromioclavicular joint, and coracoid are palpated and marked with an indelible marker, along with the planned incision site.
Diagnostic Arthroscopy
The complete surgical technique is shown in Video 1. Diagnostic arthroscopy is first performed after establishing a posterior standard viewing portal. Next, an anterior standard working portal through the rotator interval is created, and a probe is inserted. In the glenohumeral joint, the rotator cuff, capsulolabral complex, articular cartilage, and long head of the biceps tendon are thoroughly evaluated. If synovectomy and lysis of adhesions are necessary, a 4.0-mm shaver (APS II; Arthrex, Naples, FL) and a 3.75-mm suction radiofrequency cautery device (Super TurboVac 90; ArthroCare, Austin, TX) are used. If tenosynovitis is present, a biceps tenotomy is performed from the origin of the biceps tendon anchor at the superior labrum for open subpectoral tenodesis at the end of the case. The arthroscope is then introduced in the subacromial space via the posterior standard portal. An additional anterolateral portal is established to perform bursectomy and subacromial spur removal. Dynamic evaluation of the os acromiale can be performed to assess for hypermobility of the unfused segment of bone. If a rotator cuff tear is present, an arthroscopic double-row knotless self-reinforcing repair is performed using the technique recently described by the senior author (P.J.M.).10 All arthroscopic instruments are then removed to prepare for osteosynthesis of the os acromiale.
Osteosynthesis
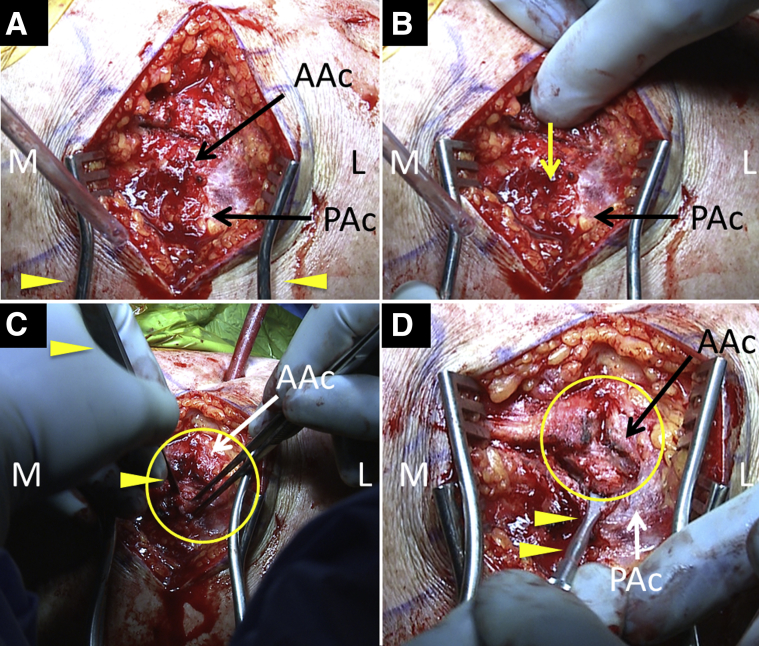
A transacromial incision of approximately 8 cm is made extending from the distal clavicle to the posterolateral border of the acromion. The incision is carried down through the skin and subcutaneous tissue to the periosteum overlying the acromion (Fig 3A).
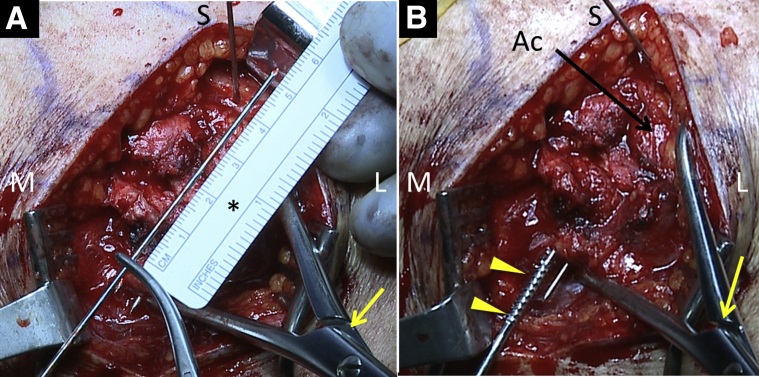
Fig 3.
Right shoulder from a posterior view. (A) An 8-cm incision is made over the lateral acromion in a posterolateral direction followed by soft tissue dissection down to the acromion with a retractor placed (arrowheads). (B) The senior surgeon (P.J.M.) locates the site of nonunion with vertical pressure inferiorly (yellow arrow), which causes gross movement of the distal fragment. (C) The periosteum is sharply dissected with a scalpel (arrowheads), thereby exposing and debriding the edges of the bone and nonunion site (circle). (D) An elevator (arrowheads) is used to lever the anterior part of the acromion into anatomic position. (AAc, anterior acromion; L, lateral; M, medial; PAc, posterior acromion.)
The os acromiale is identified by applying vertical pressure to the acromion at various positions along its length while examining for gross movement occurring at the edge of the os acromiale (Fig 3B). Once the site of the os acromiale is accurately identified, the periosteum is split along the length of the os and reflected anteriorly and posteriorly to expose the edges of the nonunion (Fig 3C). An elevator is then introduced between the os acromiale and the acromion to further improve exposure (Fig 3C). The margins of the nonunion are then burred down to a bleeding surface using a motorized rasp (PowerRasp, 5.5 mm × 13 cm; Arthrex), thereby removing any fibrous tissue and residual soft tissue.
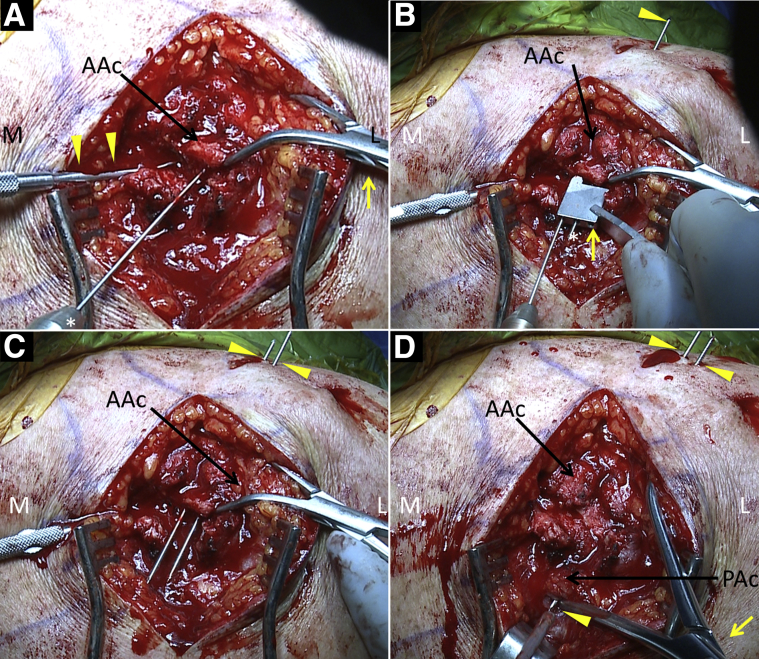
Once the nonunion is taken down and the margins of the os acromiale are exposed, fixation is performed. Initially, a double-ended Kirschner-wire (K-wire) that can fit through a 4.0-mm cannulated screw is drilled from the exposed posterior edge of the os acromiale out through the skin of the anterior shoulder (Fig 4A). Care is taken to ensure that the K-wire is drilled parallel to the thin acromial bone and that the wire does not inadvertently enter the subacromial space. A parallel drill guide is then placed over the posterior end of the first K-wire, and a second double-ended K-wire is drilled in a similar fashion from posterior to anterior through the os acromiale out the skin of the anterior shoulder. The parallel drill guide ensures that the second K-wire is positioned at a fixed distance from and parallel to the first (Fig 4 B and C). Both K-wires are then advanced further with the drill such that the posterior ends are flush with the edge of the os acromiale. The os acromiale is then reduced to its anatomic position and held provisionally with a large bone-holding clamp (Fig 4D).
Fig 4.
Right shoulder from a posterior view. (A) While the anterior acromion (AAc) is held in place by a reduction clamp (yellow arrow) and freer elevator (arrowheads), using a drill (*), a K-wire is advanced anteriorly through the posterior aspect of the anterior fragment of the acromion and (B) out the anterior skin (arrowhead); a drill guide (yellow arrow) is then placed over the first K-wire to allow the second K-wire (*) to be placed parallel to and at a fixed distance away from the first. (C) The K-wires (arrowheads) are advanced anteriorly. (D) The os acromiale is reduced into desired position with the reduction clamp (yellow arrow); the K-wires (arrowheads) are then drilled posteriorly into the posterior acromion, providing provisional fixation. (AAc, anterior acromion; L, lateral; M, medial; PAc, posterior acromion.)
Once the os acromiale is reduced and anatomic reduction is confirmed, the double-ended K-wires that had been previously drilled through the os acromiale posterior to anterior are then drilled anterior to posterior back through the os acromiale into the posterior acromion (Fig 4D).
When both K-wires have been passed into the posterior acromion, length of the screw needed to fix the os acromiale is determined indirectly by an additional K-wire superimposed over the acromion and a ruler (Fig 5A). A 2.7-mm cannulated drill is then used to overdrill the 2 K-wires. Two 4.0-mm cannulated partially threaded screws of appropriate length (Synthes, West Chester, PA) are advanced posteriorly to anteriorly (Fig 5B). Short partially threaded screws are used to achieve maximum compression of the os acromiale. When the bone quality is good and there is excellent screw purchase, screw fixation alone may be used. This is most typical in young patients with excellent-quality bone. In older patients with lower-density bone or those in whom screw purchase is not ideal, a tension-band construct is added. This has been shown biomechanically to strengthen the construct.8
Fig 5.
Right shoulder from a posterior view; the acromion is held in place with a reduction clamp (yellow arrows), and a spinal needle (S) marks the anterior end of the acromion. (A) A ruler (*) is used to measure the length of the screw needed to fix the os acromiale. (B) A 3.5-mm cannulated partially threaded screw (arrowheads) is advanced posteriorly to anteriorly, and the short threads of the screw are used to achieve maximum compression of the os acromiale. (Ac, acromion; L, lateral; M, medial.)
Tension-Band Wiring
Once the screws are placed, the double-ended K-wires are removed and two 18-gauge wires are threaded through the cannulated screws posteriorly to anteriorly. The anterior ends of the wires are retrieved anterior to the acromion at the anteriormost aspect of the incision (Fig 6A). The anterior end of the lateral 18-gauge wire and the posterior end of the medial 18-gauge wire are crossed and twisted in a tension-band fashion (Fig 6B). The same process is then repeated for the anterior end of the medial wire and posterior end of the lateral wire (Fig 6C). The excess K-wire is then cut at this point. Both remaining twisted wire stumps are bent down so as not to be prominent (Fig 6D). This tension-band fixation resists the inferior bending moment applied by the deltoid, and the crossover of wires during tensioning ensures the loads are distributed evenly across the acromion. The incision is then closed in standard fashion. Deep periosteal closure is performed with no. 0 Vicryl and then the subcutaneous tissue and skin is closed in a layered fashion. Radiographs of the final construct are presented in Figure 7. Pearls and pitfalls of the complete surgical technique are presented in Table 2.
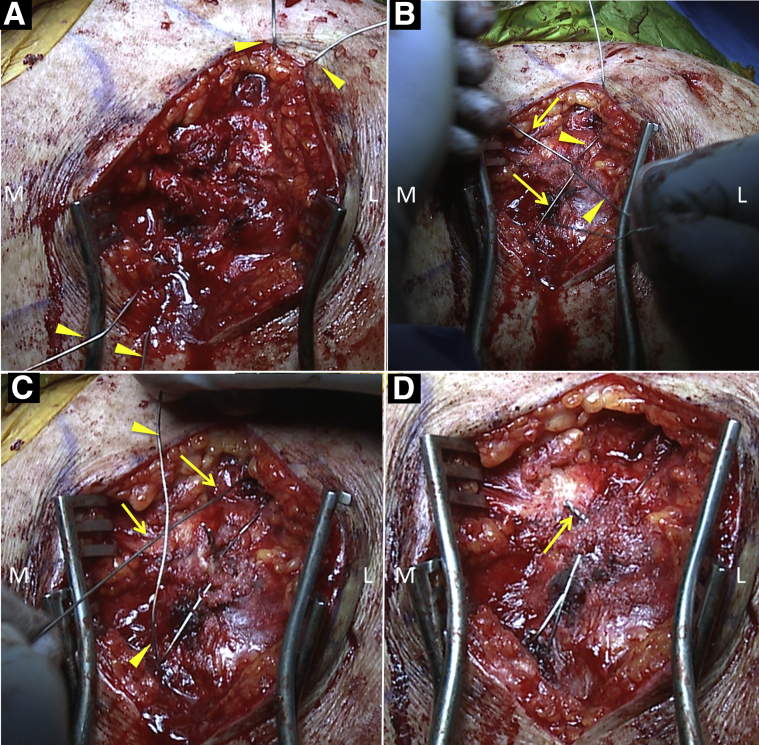
Fig 6.
Right shoulder from a posterior view. (A) View of closure of the deep tissue layer (*) just superior to the acromion; the 18-gauge wires (arrowheads) pass out through the incision but not the skin. (B) The anterior end of the lateral 18-gauge wire (arrowheads) and posterior end of the medial 18-gauge wire (arrows) are crossed and twisted in a tension-band fashion. (C) The anterior end of the medial wire (arrows) and posterior end of the lateral wire (arrowheads) are crossed and twisted in the same manner. (D) The final construct is viewed; the wires have been twisted, cut, and bent inferiorly (arrow) to minimize soft-tissue irritation. (L, lateral; M, medial.)
Fig 7.
Postoperative radiographs of a right shoulder showing an os acromiale fixed with 2 cannulated screws and a tension band (arrow). (A) Anteroposterior view of the final fixation construct. (B) Axillary view showing the best visualization; the os acromiale no longer appears to be present. (Ac, acromion; C, clavicle; G, glenoid; H, humerus; HH, humeral head.)
Table 2.
Pearls and Pitfalls
| Surgical Steps | Pitfalls | Pearls |
|---|---|---|
| Diagnostic arthroscopy | Missing concomitant lesions | Performing a thorough and standardized examination allows for identification of concomitant lesions. |
| Approach to the os acromiale | Difficulty locating the site of the nonunion | The surgeon should place inferior pressure on the anterior acromion to help identify the distal fragment of the nonunion. |
| Preparation of nonunion prior to osteosynthesis | Insufficient preparation resulting in postoperative nonunion | The margins of the nonunion can be burred down to a bleeding surface with a motorized rasp to remove fibrous tissue and residual soft tissue, and generate an environment that is enhances healing. |
| K-wire insertion | Improper drilling through the acromion resulting in penetrating the superior or inferior cortex | Ensure the K-wire is drilled parallel to the acromion. Drill first through the os acromiale and then into the acromion in a retrograde fashion. |
| Tension-band construct | Insufficient fixation | Crossover of the K-wires during tensioning ensures the loads are evenly distributed across the acromion. |
| Postoperative rehabilitation | Postoperative stiffness | Early passive range of motion for 4 weeks |
| Progression to full passive motion and start of active and active-assisted motion at 4 weeks postoperatively |
Postoperative Rehabilitation
The patient is placed in a sling postoperatively. Passive ROM is permitted for 4 weeks. At this point, gentle active ROM and activities of daily living are permitted. At 12 weeks postoperatively, full unassisted active ROM is permitted. If a biceps tenodesis is performed, resisted elbow flexion should be restricted for approximately 6 weeks.
Discussion
In general, clinical outcomes for fusion of os acromiale are positive; however, outcomes do vary depending on the surgical approach and fixation technique. Warner et al.5 reported osseous union at an average of 9 weeks in 6 of 7 shoulders (86%) that underwent open reduction, bone grafting, and internal fixation with tension-banding and cannulated screws.5 By contrast, osseous union was only achieved in 1 of 5 shoulders (20%) that underwent fixation with isolated tension banding.5 Comparable results were found by Peckett et al.,11 who reported bony union at an average 4 months in 25 of 26 patients (96%) treated with os acromiale fusion using tension banding and either K-wires or cannulated screws. In 15 shoulders undergoing os acromiale fusion with isolated tension banding, Hertel et al.9 compared an anterior deltoid-off approach versus a transacromial approach with preservation of the deltoid origin. At a mean follow-up of 44 months, the patients with transacromial approach had significantly higher rates of bony union compared to the anterior deltoid-off group (88% vs 43%).9 Boehm et al.6 found successful bony union in 15 of 22 patients (68%) who underwent os acromiale fusion with isolated tension banding at an average follow-up of 41 months. In that case series, Constant scores for patients with bony unions and nonunions did not significantly differ at 81% and 84%, respectively.6
Our preferred fixation technique was recently biomechanically evaluated by Spiegl et al.8 In that study, the authors tested different fixation techniques for meso-type os acromiale in a cadaver setup and found that ultimate load to failure was significantly higher with the use of tension banding and cannulated screws compared to cannulated screws alone.8 Overall, outcomes series and biomechanical studies have shown that osteosynthesis to achieve bony union is a safe, effective, and reliable technique for the treatment of large and unstable symptomatic os acromiale; however, high-level studies are still needed to compare outcomes between different techniques.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: E.M.F. is employed by the Steadman Philippon Research Institute where this article was written. Arthrex supports J.P.'s position in the Steadman Philippon Research Institute. P.J.M. receives consultant's fees and royalties from Arthrex, Medbridge, and Springer; is a partner of the Steadman Clinic; owns stock and stock options in GameReady and VuMedi; and receives financial support for a part of his research from Arthrex; the Steadman Philippon Research Institute receives funding from Smith & Nephew, Arthrex, Siemens, and Össur. The Steadman Philippon Research Institute receives funding from Smith & Nephew, Arthrex, Siemens, and Össur.
Supplementary Data
This instructional video presents a technique for open reduction and internal fixation of a symptomatic meso-type os acromiale using a construct of cannulated screws and tension bands. An additional rotator cuff repair is also performed. The technique is shown on a 55-year-old woman who presented with progressive pain and weakness of her right shoulder. Examination findings were significant for tenderness and gross motion of the acromion, and imaging revealed an os acromiale with associated supraspinatus tendon tear. After standard diagnostic arthroscopy, the full-thickness crescent-shaped supraspinatus tear is debrided, and a knotless double-row construct is used for repair. The medial row is addressed first, and an arthroscopic punch is used to create an anteromedial bone socket at the bone-cartilage margin. A vented 4.75-mm knotless suture anchor loaded with suture tape is placed in this socket. Next, using an arthroscopic grasper and suture passer, both limbs of the suture tape are passed through the tendon, at least 5 mm medial to the edge of the tear. The posteromedial anchor is placed in an identical fashion 10 mm posterior to the first anchor. For the lateral row, one limb of suture tape from each medial anchor is preloaded into the eyelet of an additional 4.75-mm suture anchor. Gentle tension is applied through the suture tapes to reduce and compress the cuff tissue on the footprint while placing the first lateral anchor. The process is repeated for the second lateral anchor; this completes the knotless repair of the rotator cuff. Attention is then turned to the os acromiale fusion. A transacromial approach of about 8 cm is made. The os acromiale is identified by applying vertical pressure to the acromion and examining for gross movement. The nonunion is exposed with sharp dissection of the fascia and the deltoid origin and levering of the distal segment using an elevator. The margins of the nonunion are burred down to a bleeding surface with a motorized rasp. The first K-wire is then drilled through the os acromiale and out the skin of the anterior shoulder. A drill guide for parallel drilling is placed over the first K-wire to guide the second K-wire. Both K-wires are advanced entirely into the anterior fragment. The os acromiale is then reduced to its final position, and the K-wires are drilled back into the posterior acromion providing provisional fixation. The length of screw is then measured with a spinal needle marking the anterior part of the acromion. After overdrilling the K-wires with a 3.5-mm drill, two 4.0-mm lag screws are inserted posteriorly to anteriorly. Both K-wires are then switched with 18-gauge wires, which will later be used as tension bands. Next the deltoid origin is reattached to the acromion and the fascia closed using Vicryl sutures. The 18-gauge wires are then twisted in a tension-band fashion, first by twisting together the anterolateral and posteromedial wires, then cutting them with a wire cutter. The process is repeated for the anteromedial and posteromedial wires. This construct resists the inferior bending moment applied by the deltoid, and the crossover of wires during tensioning ensure the loads are evenly distributed across the acromion. After tightening and cutting the wires, the stumps are bent down to minimize soft-tissue irritation. The integrity of the construct is then tested with vertical pressure to the anterior acromion. Postoperative radiographs show excellent reduction and fixation of the os acromiale. Postoperative rehabilitation is with sling immobilization for 4 weeks with immediate passive range of motion of the shoulder. After 4 weeks, gentle active range of motion with activities of daily living may be resumed. The patient may return to full, unassisted active range of motion at 12 weeks.
References
- 1.Kurtz C.A., Humble B.J., Rodosky M.W., Sekiya J.K. Symptomatic os acromiale. J Am Acad Orthop Surg. 2006;14:12–19. doi: 10.5435/00124635-200601000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Zlatkin M.B. Lippincott Williams & Wilkins; Philadelphia, PA: 2003. MRI of the shoulder. [Google Scholar]
- 3.Sammarco V.J. Os acromiale: Frequency, anatomy, and clinical implications. J Bone Joint Surg Am. 2000;82:394–400. doi: 10.2106/00004623-200003000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Kaplan P. WB Saunders; Philadelphia, PA: 2001. Musculoskeletal MRI. [Google Scholar]
- 5.Warner J.J., Beim G.M., Higgins L. The treatment of symptomatic os acromiale. J Bone Joint Surg Am. 1998;80:1320–1326. doi: 10.2106/00004623-199809000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Boehm T.D., Matzer M., Brazda D., Gohlke F.E. Os acromiale associated with tear of the rotator cuff treated operatively. Review of 33 patients. J Bone Joint Surg Br. 2003;85:545–549. doi: 10.1302/0301-620x.85b4.13634. [DOI] [PubMed] [Google Scholar]
- 7.Harris J.D., Griesser M.J., Jones G.L. Systematic review of the surgical treatment for symptomatic os acromiale. Int J Shoulder Surg. 2011;5:9–16. doi: 10.4103/0973-6042.80461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spiegl U.J., Smith S.D., Todd J.N., Wijdicks C.A., Millett P.J. Biomechanical evaluation of internal fixation techniques for unstable meso-type os acromiale. J Shoulder Elbow Surg. 2015;24:520–526. doi: 10.1016/j.jse.2014.09.040. [DOI] [PubMed] [Google Scholar]
- 9.Hertel R., Windisch W., Schuster A., Ballmer F.T. Transacromial approach to obtain fusion of unstable os acromiale. J Shoulder Elbow Surg. 1998;7:606–609. doi: 10.1016/s1058-2746(98)90008-8. [DOI] [PubMed] [Google Scholar]
- 10.Mook W.R., Greenspoon J.A., Millett P.J. Arthroscopic double-row transosseous equivalent rotator cuff repair with a knotless self-reinforcing technique. Open Orthop J. 2016;10:286–295. doi: 10.2174/1874325001610010286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peckett W.R., Gunther S.B., Harper G.D., Hughes J.S., Sonnabend D.H. Internal fixation of symptomatic os acromiale: A series of twenty-six cases. J Shoulder Elbow Surg. 2004;13:381–385. doi: 10.1016/j.jse.2004.01.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This instructional video presents a technique for open reduction and internal fixation of a symptomatic meso-type os acromiale using a construct of cannulated screws and tension bands. An additional rotator cuff repair is also performed. The technique is shown on a 55-year-old woman who presented with progressive pain and weakness of her right shoulder. Examination findings were significant for tenderness and gross motion of the acromion, and imaging revealed an os acromiale with associated supraspinatus tendon tear. After standard diagnostic arthroscopy, the full-thickness crescent-shaped supraspinatus tear is debrided, and a knotless double-row construct is used for repair. The medial row is addressed first, and an arthroscopic punch is used to create an anteromedial bone socket at the bone-cartilage margin. A vented 4.75-mm knotless suture anchor loaded with suture tape is placed in this socket. Next, using an arthroscopic grasper and suture passer, both limbs of the suture tape are passed through the tendon, at least 5 mm medial to the edge of the tear. The posteromedial anchor is placed in an identical fashion 10 mm posterior to the first anchor. For the lateral row, one limb of suture tape from each medial anchor is preloaded into the eyelet of an additional 4.75-mm suture anchor. Gentle tension is applied through the suture tapes to reduce and compress the cuff tissue on the footprint while placing the first lateral anchor. The process is repeated for the second lateral anchor; this completes the knotless repair of the rotator cuff. Attention is then turned to the os acromiale fusion. A transacromial approach of about 8 cm is made. The os acromiale is identified by applying vertical pressure to the acromion and examining for gross movement. The nonunion is exposed with sharp dissection of the fascia and the deltoid origin and levering of the distal segment using an elevator. The margins of the nonunion are burred down to a bleeding surface with a motorized rasp. The first K-wire is then drilled through the os acromiale and out the skin of the anterior shoulder. A drill guide for parallel drilling is placed over the first K-wire to guide the second K-wire. Both K-wires are advanced entirely into the anterior fragment. The os acromiale is then reduced to its final position, and the K-wires are drilled back into the posterior acromion providing provisional fixation. The length of screw is then measured with a spinal needle marking the anterior part of the acromion. After overdrilling the K-wires with a 3.5-mm drill, two 4.0-mm lag screws are inserted posteriorly to anteriorly. Both K-wires are then switched with 18-gauge wires, which will later be used as tension bands. Next the deltoid origin is reattached to the acromion and the fascia closed using Vicryl sutures. The 18-gauge wires are then twisted in a tension-band fashion, first by twisting together the anterolateral and posteromedial wires, then cutting them with a wire cutter. The process is repeated for the anteromedial and posteromedial wires. This construct resists the inferior bending moment applied by the deltoid, and the crossover of wires during tensioning ensure the loads are evenly distributed across the acromion. After tightening and cutting the wires, the stumps are bent down to minimize soft-tissue irritation. The integrity of the construct is then tested with vertical pressure to the anterior acromion. Postoperative radiographs show excellent reduction and fixation of the os acromiale. Postoperative rehabilitation is with sling immobilization for 4 weeks with immediate passive range of motion of the shoulder. After 4 weeks, gentle active range of motion with activities of daily living may be resumed. The patient may return to full, unassisted active range of motion at 12 weeks.