Abstract
An anterior cruciate ligament (ACL) tear is one of the most common orthopaedic injuries. Optimal results are not always achieved after surgical reconstruction after a surgical technical error, namely, tunnel malposition. Understanding of the anatomy is vital, and several anatomic landmarks can be used to aid in an optimal reconstruction technique. The purpose of this Technical Note is to describe our preferred technique for an arthroscopic single-bundle anteromedial ACL reconstruction, using a bone–patellar tendon–bone autograft fixed with interference screws.
An anterior cruciate ligament (ACL) tear is one of the most common orthopaedic injuries in the United States, with nearly 200,000 ACL reconstructions (ACLRs) performed annually.1 ACLR is performed to restore stability and kinematics of the knee joint. By improving knee stability with ACLR procedures, the risk of damaging chondral surfaces and menisci is minimized.2
There have been significant advances in ACLR surgical techniques, including a focus on the optimal reconstruction graft type. Graft selection for ACLR is primarily based on surgeon's experience and patient factors, such as gender, age, patient size and activity level. Both patella tendon and hamstring autografts for ACLR have been supported in the literature with good functional outcomes and low graft rupture rates.3 In a recent systematic review of 22 studies comparing ACL reconstruction grafts, patella tendon autografts had superior rotational stability, but a higher complication rate when compared with quadrupled hamstring autografts.4 Webster et al performed a randomized controlled study evaluating outcomes following hamstring autograft versus patella tendon autograft in ACLR. They reported no difference in graft failure rate; however, more patients who received patella autograft were able to return to bi-weekly sport.5
The purpose of this Technical Note is to describe our preferred technique for an arthroscopic single-bundle anatomic ACL reconstruction using a bone–patellar tendon–bone (BPTB) autograft fixed with biointerference screws. This Technical Note provides important pearls for performing a reproducible ACL reconstruction based on reliable anatomic and arthroscopically visualized landmarks.
Technique
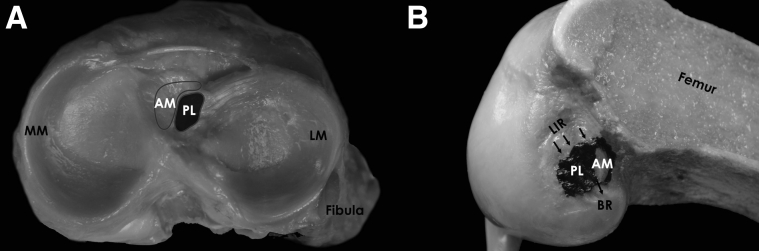
A comprehensive knowledge of the ACL footprint anatomy is crucial for successfully performing this procedure (Fig 1). The advantages and disadvantages of the bone-tendon-bone autograft are presented in Table 1, and a step-by-step approach with pearls for each part of the procedure are presented in Table 2. An ACL case example is demonstrated in Video 1.
Fig 1.
(A) An anatomic cadaveric dissection of the tibial plateau reveals the location of the ACL AM and PL bundles. Note that the anatomic footprint on the tibia is commonly identified arthroscopically as being approximately 9 mm posterior to the intermeniscal ligament and 7 mm anterior to the PCL. Note that the AM bundle is aligned with the anterior horn of the lateral meniscus attachment, and the PL bundle has fibrous attachments to the posterior aspect of the anterior horn of the lateral meniscus. (B) An anatomic cadaveric dissection of the lateral femoral condyle reveals the footprint locations of the AM and PL bundles. A knee flexion angle of 90° is needed to consistently identify the anatomic footprint of the ACL, as the attachment anatomy can appear to change as a function of knee flexion angle. The bifurcate ridge (BR) separates the AM and PL bundles, and the lateral intercondylar ridge (LIR), also known as resident's ridge, is more consistently identified arthroscopically and represents the anterior margin of the AM and PL femoral bundles. (ACL, anterior cruciate ligament; AM, anteromedial; PCL, posterior cruciate ligament; PL, posterolateral.)
Table 1.
Advantages and Disadvantages of Bone Tendon Bone Autograft
| Advantages | Disadvantages |
|---|---|
| Good bone to bone healing of the graft | Increased risk of patellar fracture |
| Good functional outcomes and return to sports | Increased risk of anterior knee pain and kneeling pain |
| Restores knee stability | Tendency toward increased risk of patellofemoral osteoarthritis |
| Does not weaken the hamstrings in the athletic population | Graft harvest may be technically challenging |
| Autograft readily available | |
| Easy to obtain optimal size of graft |
Table 2.
Step-by-Step Process
| Step | Pearls |
|---|---|
| Patient positioning | • The leg holder should be placed proximal enough to allow for femoral tunnel guide pin passage, exposure for an inside-out meniscal repair, or other concomitant open procedures. |
| • The leg holder should also be tilted slightly to allow for full knee flexion while reaming the ACL femoral tunnel. | |
| • It is important to remember to allow for the ability to flex and extend the knee at various stages of the surgical procedure, and therefore it should be checked before starting the procedure. | |
| Graft harvest | • Incise from the distal third of the patella up extending 2 cm distal to the tubercle. |
| • Carefully dissect the paratenon off both sides of the tendon. | |
| • Mark a 1-cm-wide tendon graft and make the cuts longitudinally in line with the fibers between the patella and the tibia. | |
| • A Bovie can be used to demarcate and expose the bony surface prior to the saw cut. | |
| • Start the lateral bony cuts with a saw from distal to proximal in an oblique fashion. Repeat for the transverse cut. | |
| • Use a straight osteotome just to release the bone plug. | |
| • Both bone plugs should be prepared so that they easily pass through a 10-mm sizer. The femoral plug should be approximately 20 mm in length, while leaving the tibial plug longer at 25 mm. | |
| Portal placement | • Portals should be placed along the medial and lateral aspects of the patellar tendon through the same incision. |
| • An accessory medial portal should be created before creating the femoral tunnel. | |
| Native ACL attachment identification | • The lateral intercondylar ridge, also known as resident's ridge, is more consistently identified arthroscopically, and this ridge represents the anterior margin of the AM and PL femoral bundles. A technical pearl for reconstituting native anatomy during reconstruction is to preserve some native ACL femoral footprint to help guide anatomic reconstruction. In general, the center of the ACL femoral attachment is 8.5 mm anterior to the posterior cartilage margin, 1.7 mm proximal to the bifurcate ridge, 14.7 mm proximal to the distal cartilage margin, and 6.1 mm posterior to the lateral intercondylar ridge. |
| • For the tibial attachment, the anterior horn of the lateral meniscus is the most consistent landmark. Placement of the tibial tunnel should be in line (7.5 mm medial) to this landmark. | |
| Femoral tunnel creation | • It has been reported that 90° of flexion is the optimal knee flexion to better identify the structures. |
| • A burr is used to mark the desired location. | |
| • When drilling, the knee should be flexed to 120° with a valgus stress to optimize the length of the tunnel and to avoid posterior wall blowout. | |
| • After reaming 2 to 3 mm, check the presence and thickness of the posterior wall of the tunnel. | |
| Tibial tunnel creation | • Remaining ACL fibers should be left intact to have a reliable landmark of the native ACL insertion site. |
| • For cases in which the ACL tibial stump is not visible, placing a tibial single-bundle tunnel medial at the midpoint of the anterior horn of the lateral meniscus attachment may be a useful arthroscopic landmark for single-bundle ACL reconstructions. | |
| • Careful attention must be paid to preserve the meniscal root insertions because iatrogenic anterior medial and lateral meniscus root and posterior lateral meniscus root avulsion can occur because of malposition of the tibial tunnel(s) during ACL reconstruction. | |
| Fixation | • The ACL graft is passed through the tibia into the femoral ACL tunnel and then fixed in the femur with a 7- × 20-mm titanium interference screw. The screw should be positioned superiorly on the tunnel to position the graft inferiorly. |
| • Cycle the knee several times while applying traction to remove any slack out of the graft and to ensure that no impingement is present. | |
| • Distal traction is then applied to the ACL graft, and the tibial ACL graft fixation is performed with a 9- × 20-mm titanium interference screw with the knee in full extension. |
ACL, anterior cruciate ligament; AM, anteromedial; PL, posterolateral.
Patient Positioning and Anesthesia
The patient is placed in the supine position on the operating table. After induction of general anesthesia, a bilateral knee examination is performed to evaluate for any concurrent ligamentous instability and to assess range of motion. A well-padded high-thigh tourniquet is subsequently placed on the operative leg, which is then placed into a leg holder (Mizuho OSI, Union City, CA) while the contralateral knee is placed into an abduction stirrup (Birkova Product, Gothenburg, NE). The leg holder should be placed proximal enough to allow for femoral tunnel guide pin passage, exposure for an inside-out meniscal repair or other concomitant open procedures. The foot of the operating table is then lowered, allowing the surgeon to freely manipulate the knee as needed.
Surgical Technique
Graft Harvest
With the knee flexed to 90°, an approximately 9-cm-long longitudinal incision is made over the anterior aspect of the knee from the inferior pole of the patella to approximately 2 cm distal to the tibial tubercle. Dissection is carried through the subcutaneous tissue to the patellar tendon paratenon layer sharply with a knife. Small subcutaneous flaps are then created medially and laterally to allow for adequate visualization of the medial and lateral borders of the patellar tendon. Creation of a larger distal medial flap will allow for easier ACL tibial tunnel drilling later in the procedure. The paratenon is then incised longitudinally centered on the patellar tendon, and this layer is carefully developed to aid in layered closure at the end of the case.
Next, a ruler is used to measure the width of the patellar tendon, which is typically 30 mm. The ruler is then used to mark the middle third of the tendon at a width of 10 mm. A scalpel is used to incise the tendon longitudinally from proximal to distal, keeping the knife blade moving smoothly in line with the fibers of the tendon until the tibia is reached. This step is then repeated on the other side of the tendon graft. Care should be taken not to narrow or widen the second incision relative to the initial incision or to incise into the underlying retropatellar fat pad. The distal pole of the patella and the tubercle are subsequently lightly marked with a sterile marking pen.
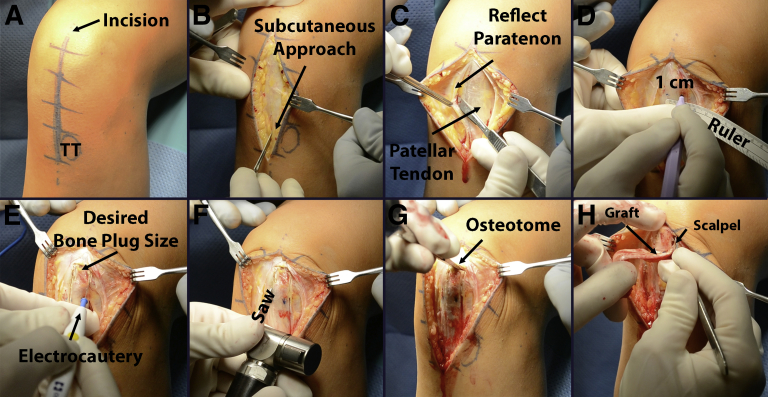
A Bovie electrocautery tip is then used to mark the periosteum for a 20-mm-long by 10-mm-wide bone plug from the patella and a 25-mm-long by 10-mm-wide bone plug from the tibial tubercle. Care is taken at this step to correctly identify the margin at which the patellar tendon is attached to bone; this can be accomplished by placing a freer elevator perpendicular to the insertion of the tendon on bone and measuring from that point. A small oscillating saw (Stryker, Kalamazoo, MI) with a 10-mm-wide blade is then used to cut the patellar bone plug. Care must be taken to angle the longitudinal cuts 30° toward the midline of the patella, thereby forming a trapezoidal bone plug while avoiding damage to the patellar chondral surface and avoiding a patellar fracture. Further, the length of the patellar bone plug should be confirmed before initiating cutting, because carrying this cut too close to the proximal patella may increase risk for iatrogenic patella fracture. The proximal horizontal cut is made by aiming the saw blade 45° obliquely toward either of the longitudinal cuts, to avoid cutting beyond the longitudinal cuts, thus reducing the risk of creating a potential stress riser in the patella (Fig 2). Thin ⅜- and ½-in. straight osteotomes are used to gently free the plug out from the patella. If adequate saw cuts have been made, the patellar plug should be able to be easily removable. Do not force the patellar plug out by levering it with the osteotomy because this can fracture the bone plug or the patella. If the bone plug is difficult to remove, it is recommended to reevaluate the cuts and perform recut where needed.
Fig 2.
Patellar tendon (bone-tendon-bone) harvest on the left knee. (A) The skin is initially marked from the patella to the tibial tubercle at the midline of the knee for a length of approximately 9 cm. (B) Sharp dissection is carried through skin and subcutaneous tissue to the paratenon layer using a scalpel. (C) The paratenon layer is separated from the underlying tendon in a thick flap, which is repaired during closure. (D) We use a surgical marker to delineate the middle one-third of the patellar tendon and mark a desired graft width of 10 mm in the center of the tendon. We then use a scalpel to mark a longitudinal incision, in line with the tendon fibers, in the center of the patellar tendon to the 10 mm desired width. (E) A Bovie electrocautery device is used to delineate the patellar and tibial bone plugs and clear soft tissue from the bone to facilitate the harvest. The patellar bone plug measures 10 mm wide by 20 mm long and the tibial bone plug measures 10 mm wide by 25 mm long from the tendinous insertion of the patellar tendon to the respective bones. (F) A sagittal saw is then used to harvest the plugs from the previously measured and established tracks created in panel E. The saw blade is angled 30° toward the midline of the patella for the lateral and medial cuts and 45° distally for the proximal cut. The saw blade is angled 20° toward midline in the tibia for the lateral and medial cuts and 45° proximally for the distal cut. (G) Thin ⅜- and ½-in. straight osteotomes are used to gently free the plug out from the patella. This process should be relatively easy if adequate saw cuts were previously made. Avoid excessive malleting and levering with the osteotomes to prevent cartilage damage and iatrogenic fracture. (H) The final step of harvest consists of sharply dissecting remaining soft tissue attachments from the graft during removal with a scalpel.
Next, the tibial bone plug is harvested. The oscillating saw is used to score the tibial cortex before penetrating the saw blade into the bone. Once the cortex has been scored, the saw blade is inserted to a depth of approximately 8 to 10 mm along each side of the plug. The saw blade should be angled slightly medially (approximately 20°) when on the lateral side of the tibial plug, and slightly laterally when on the medial side of the tibial plug (approximately 20°), to create an equilateral triangle–shaped tibial bone plug. The distal horizontal cut is made by aiming the saw 45° obliquely and proximally towards the longitudinal cuts to avoid cutting beyond the longitudinal cuts, thereby avoiding the creation of a potential stress riser. A thin osteotome is then used to gently lift the tibial plug out from the tibia. If adequate saw cuts have been made, the tibial plug should be easily removable. Careful dissection with a no. 15 blade scalpel is used to remove any remaining soft tissue attachments from the bone-tendon-bone graft; handling of the graft can be facilitated with a dry lap-sponge. The graft is then carefully removed from the knee and brought to the back table for preparation (Fig 2).
Graft Preparation
The BPTB graft can be prepared in a variety of ways. For the majority of patients, we aim to prepare both bone plugs so that they easily pass through a 10-mm sizer. We typically fashion the femoral plug to be approximately 20 mm in length, while leaving the tibial plug longer at 25 mm. The bone plugs are trimmed to the appropriate size using any combination of a saw, rongeur, and scissors. Excess bone should be saved for grafting into the bone plug harvest sites at the end of the case. A 1.6-mm K-wire is used to drill 2 holes approximately 5 mm apart in the tibial bone plug in the cancellous part of the plug, parallel to the cortical surface, followed by shuttling a no. 5 high-strength nonabsorbable FiberWire suture (Arthrex, Naples, FL) through each hole. The same procedure is repeated in the femoral bone plug. The bone-tendon junction of the femoral bone plug is marked with a sterile marking pen, as well as the most proximal aspect of the tibial plug, which will assist with graft orientation during graft passage and fixation.
Femoral Tunnel Preparation
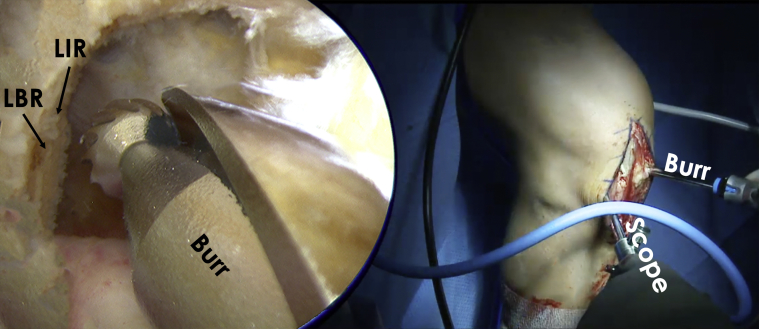
Standard anterolateral and anteromedial portals are created and a diagnostic arthroscopy is performed. Attention is then turned to the intercondylar notch, where a combination of arthroscopic 4.5-mm-full-radius shaver (Smith & Nephew, Andover, MA) and a radiofrequency cautery device (Smith & Nephew) are used to clear off the lateral aspect of the notch along the native ACL origin on the lateral femoral condyle. Specifically, the lateral intercondylar ridge is identified as a landmark for reconstruction. Occasionally, a notchplasty is required to reshape and resect excess bone or osteophytes in the intercondylar femoral notch using an arthroscopic 5.5-mm round arthroscopic burr (Smith & Nephew). At this point, an 18-gauge spinal needle is used to create an accessory medial portal. Through this portal, a bur (Smith and Nephew) is used to mark the center of the femoral tunnel. The camera is then placed in the accessory medial portal to directly visualize the proposed tunnel site. One must be critical of tunnel placement to ensure an anatomic reconstruction and to adjust the starting point accordingly (Fig 1).
An over-the-top drill guide (7 mm offset) is then placed through the accessory medial portal while visualizing arthroscopically from the anterolateral portal, and the knee is flexed as much as possible to help gain access to the anatomic femoral ACL footprint. An eyelet pin (Arthrex) is drilled through the guide, exiting the distal lateral femur. A 10-mm low-profile reamer (Arthrex) is placed over the eyelet pin and reamed to a depth of 5 mm through the accessory medial portal under arthroscopic visualization from the anterolateral portal. While doing so, an arthroscopic shaver placed through a standard anteromedial portal is used to clear bony debris. The reamer is pulled back by hand, and the surgeon carefully assesses tunnel trajectory and placement. There should be an approximately 1.5 to 2 mm of back wall present. Once tunnel placement is confirmed, the reamer is advanced to a depth of 25 mm. A passing suture is placed through the end of the eyelet pin, which is then pulled laterally through the knee, keeping the looped end of the passing suture exiting the accessory medial portal. The passing suture is then clamped to prevent inadvertent suture damage or removal. At this juncture, we typically address concomitant meniscal and/or chondral pathology (Fig 3).
Fig 3.
An arthroscope placed in the anterolateral portal on the patient's left knee is used to visualize the femoral footprint of the ACL. The anteromedial portal is used as a working portal to facilitate use of the various arthroscopic instruments including shavers, electrocautery, and burr. After soft tissue is cleared using an arthroscopic shaver and radiofrequency device, the LIR and the LBR can be identified. The LBR marks the separation between the anteromedial and posterolateral bundles of the ACL. The LIR, also known as resident's ridge, is more consistently identified arthroscopically, and this ridge represents the anterior margin of the AM and PL femoral bundles. An arthroscopic burr is used to perform a focal notchplasty to restore the anatomic shape of the intercondylar notch, which helps facilitate graft passage and prevents graft impingement, thereby ensuring full knee range of motion after reconstruction. (ACL, anterior cruciate ligament; AM, anteromedial; LBR, lateral bifurcate ridge; LIR, lateral intercondylar ridge; PL, posterolateral.)
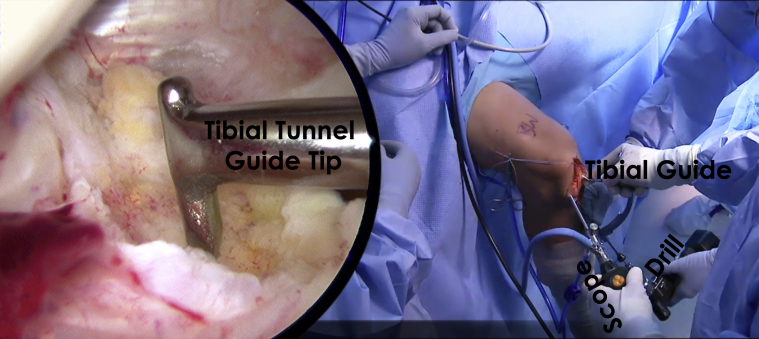
Tibial Tunnel Preparation
An arthroscopic coagulator (Smith & Nephew) device is used to mark the tibial tunnel placement. The anterior horn of the lateral meniscus is used to guide anatomic tunnel placement, and the tunnel should not exit the tibial plateau posterior to the anterior horn of the lateral meniscus. A tibial drill guide set at 65° (Arthrex) is placed through the anteromedial portal to the marked spot (Fig 4), and the drill guide is placed flush with the proximal tibia. The guide should engage the tibia approximately halfway down the tibial tubercle bone plug harvest site roughly 1.5 to 2 cm medial to the tubercle. The guide pin is then drilled, followed by a 10-mm acorn reamer (Arthrex). A small rongeur is used to carefully remove all soft tissue from the tunnel aperture, as this soft tissue can preclude easy graft passage. The passing suture previously placed through the femoral tunnel is unclamped, and the loop is pulled into the joint. An arthroscopic grasper is introduced into the joint through the tibial tunnel and used to pull the passing stitch distally through the tunnel.
Fig 4.
An arthroscope placed in the anterolateral portal of the patient's left knee is used to visualize the tibial footprint of the ACL. The standard anteromedial portal is used as a working portal and the tibial ACL guide set to 65° is placed through this portal to the anatomic center of the ACL. The anatomic footprint on the tibia is commonly identified arthroscopically as being approximately 9 mm posterior to the intermeniscal ligament, 7 mm anterior to the PCL, and should not exit the tibial plateau posterior to the anterior horn of the lateral meniscus. The guide should engage the tibia approximately halfway down the tibial tubercle bone plug harvest site roughly 1.5-2 cm medial to the tubercle. (ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.)
Graft Passage and Fixation
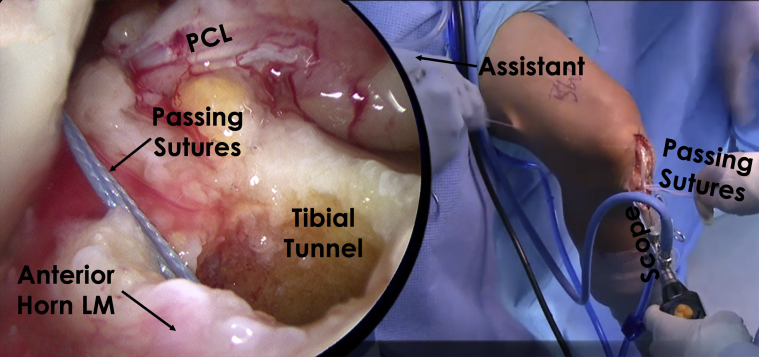
The femoral bone plug sutures are passed through the loop of the passing suture, which is then pulled up through the tunnels and out the lateral thigh. The 4 femoral bone plug suture ends are equally pulled with a clamp to advance the graft into the joint (Fig 5).
Fig 5.
Graft passage after creation of the femoral and tibial tunnels is facilitated by the previously placed “passing suture” by retrieving the looped end through the distal tibial tunnel. The graft passage process is visualized arthroscopically through the anterolateral portal on the patient's left knee. The 4 suture ends on the patellar bone plug end of the patellar tendon graft are placed through the loop and then pulled through the joint and out the lateral aspect of the femur and skin by an assistant. The graft is pulled and positioned into the femoral tunnel under arthroscopic visualization with the aid of a 90° hemostat placed through the anteromedial portal, ensuring the graft does not twist during passage. The graft is pulled until the bone plug abuts the lateral wall of the femoral tunnel.
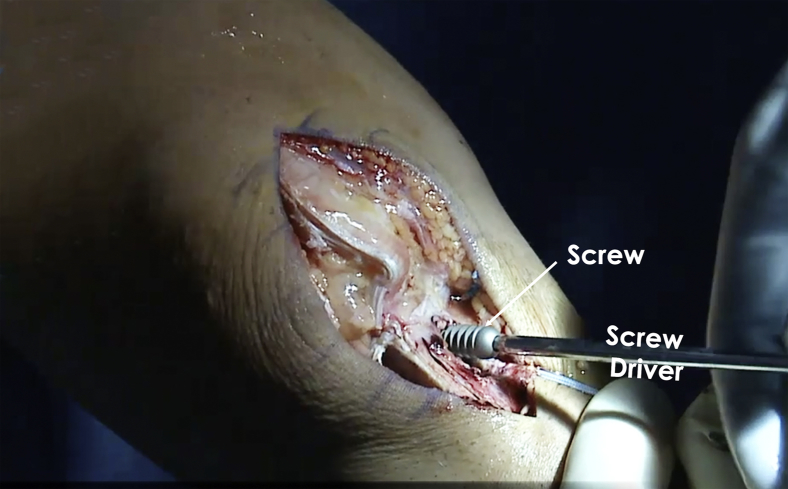
A 90° hemostat should be used to assist in graft passage and positioning within the femoral tunnel. If the graft is not advancing, care should be taken to check the tibial tunnel aperture. Next, the knee is maximally flexed and a blunt-tipped guide pin is passed through the accessory medial portal into the superior aspect of the femoral tunnel-bone plug junction. The ACL graft is then fixed in the femoral tunnel with a 7- × 20-mm cannulated titanium interference screw (Arthrex) (Fig 6).
Fig 6.
Femoral fixation of the ACL graft is performed with the patient's left knee in maximal flexion. A guide pin is inserted through the accessory medial portal with visualization from the anterolateral portal to the superior aspect of the graft and femoral tunnel junction. A 7- × 20-mm cannulated titanium interference screw is then placed under arthroscopic visualization, which is facilitated by a soft tissue, cannulated protector to prevent iatrogenic injury to the PCL and the ACL graft. The screw is placed while an assistant is pulling lateral tension on the passed graft. (ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.)
Next, the knee is cycled 20 times to remove slack from the ACL graft in the tibial tunnel. Thereafter, assess for graft impingement at the edge or roof of the intercondylar notch throughout a full passive range of motion. A blunt-tipped guide pin is then placed at the anterolateral aspect of the tibial tunnel–bone plug junction with the knee reduced in full extension. A 9- × 20-mm cannulated titanium interference screw (Arthrex) is used for tibial fixation (Fig 7). Any excess tibial bone plug can be removed with a small oscillating saw. Knee stability is then assessed clinically, and arthroscopic examination is performed to confirm that there is no impingement.
Fig 7.
Tibial fixation of the ACL graft is performed with the patient's left knee fully extended and the joint reduced. A guide pin is inserted to the superolateral aspect of the tunnel-graft interface. The assistant pulls the graft taut while a 9- × 20-mm cannulated titanium interference screw (Arthrex) is used for tibial fixation. Excess bone that may be present outside of the tibial tunnel can be removed with a rongeur or oscillating saw. (ACL, anterior cruciate ligament.)
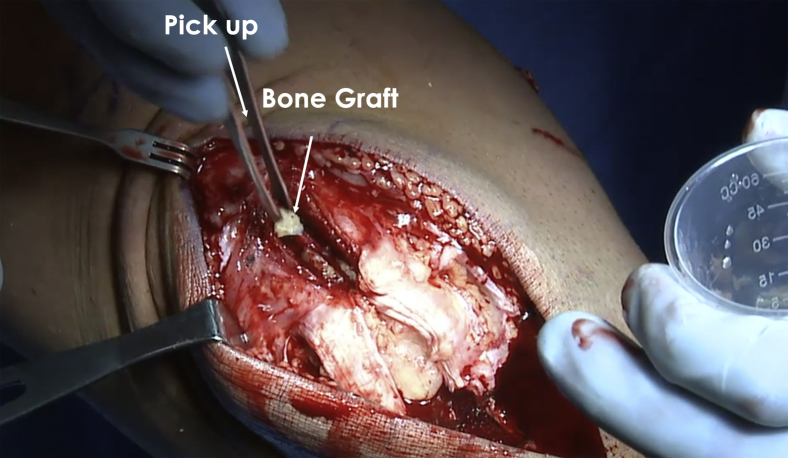
Closure
Excess bone from the harvested patellar tendon autograft that was saved during graft preparation is used to graft the patellar and tibial bone plug harvest sites, with priority given to the patellar site. The patellar tendon defect is then loosely reapproximated with no. 0 Vicryl interrupted sutures with the knee in flexion, taking care not to overtighten the tendon. Next, the paratenon layer is closed with a running or interrupted no. 0 Vicryl suture. The subcutaneous tissue and skin layer are closed in a standard fashion (Fig 8).
Fig 8.
Excess bone from the patellar tendon bone-tendon-bone autograft that was saved during graft preparation is used as bone graft at the patellar and tibial harvest sites. A priority is placed on bone graft being used to fill the patellar bone void created during harvest.
Discussion
Anatomic single-bundle ACL reconstruction is the gold standard treatment for ACL tears, especially in young, active individuals. Biomechanical studies have demonstrated that anatomic single-bundle ACL reconstructions restore knee kinematics to near native states, comparable to double-bundle ACL reconstruction.6 Clinical studies suggest that the BPTB autograft is superior to the hamstring tendon allograft in restoring stability, but functional outcomes are comparable.7 We recommend BPTB autograft in the athletic population because of the good healing potential of the bone plugs to the bone tunnels, the ability to restore knee kinematics after reconstruction, and lower risk of revision than hamstring tendon autograft. Patients who require good hamstring function such as sprinters, football wide receivers, and soccer players should be considered for BPTB autograft when performing ACL reconstruction.
Xie et al.4 reported that BPTB autografts might be superior in restoring rotational stability of the knee joint, and allowed patients to return to higher activity compared with 4-strand hamstring tendon autografts in a meta-analysis of 22 studies. Furthermore, Persson et al.8 reported a higher risk of revision in patients with hamstring autograft compared with BPTB autograft in a registry study evaluating 12,643 patients. Other registry studies have demonstrated a higher risk of failure with hamstring tendon autografts than patellar tendon autografts.9, 10 However, in a separate meta-analysis of 1,443 patients at minimum 5 years' follow-up, Xie et al.11 found no significant difference between BPTB and hamstring tendon autografts in International Knee Documentation Committee scores; KT-1000 assessment; Lachman test scores; and extension deficit, flexion deficit, and graft failure rates.
There have been some concerns raised against the use of BPTB autograft. There is a tendency toward increased complications with BPTB autograft, including patellar fractures, anterior knee pain, and kneeling pain.7, 11 A higher prevalence of radiographic osteoarthritis has been reported after BPTB autograft ACL reconstruction compared with hamstring autograft reconstruction in some studies.11 It is important when performing this procedure to be meticulous when harvesting the graft to avoid stress risers and thus the risk of patella fracture. The rehabilitation protocol should be tailored to allow graft incorporation and healing to avoid graft failure.
In a recent systematic review by Kurz et al.12 reporting on the credibility and quality of meta-analyses addressing graft choice in ACL reconstruction, the authors reported limited credibility of some of the included studies, with a trend toward earlier studies having limited methodological “rigor.” More high-quality studies are needed to evaluate graft choice in ACL reconstructions and improve surgical techniques, coupled with biological approaches to ultimately improve the return to activities of the patients.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: R.F.L. receives institutional support from Arthrex, Ossur, Siemens, and Smith & Nephew; consultancy fees from Arthrex, Smith & Nephew, and Ossur; grants from Health East, Norway, and the National Institutes of Health (R-13 grant for biologics); and has patents for Ossur and Smith & Nephew.
Supplementary Data
The patient is placed in the supine position on the operating table. Patellar tendon (bone-tendon-bone) harvest: The skin is initially marked from the patella to the tibial tubercle at the midline of the knee for a length of approximately 9 cm. Sharp dissection is carried through skin and subcutaneous tissue to the paratenon layer using a scalpel. The paratenon layer is separated from the underlying tendon in a thick flap, which is repaired during closure. We use a surgical marker to delineate the middle one-third of the patellar tendon and mark a desired graft width of 10 mm in the center of the tendon. We then use a scalpel to mark longitudinal incision, in line with the tendon fibers, in the center of the patellar tendon to the 10 mm desired width. A Bovie electrocautery device is used to delineate the patellar and tibial bone plugs and clear soft tissue from the bone to facilitate the harvest. The patellar bone plug measures 10 mm wide by 20 mm long, and the tibial bone plug measures 10 mm wide by 25 mm long from the tendinous insertion of the patellar tendon to the respective bones. A sagittal saw is then used to harvest the plugs from the previously measured and established tracks created before. The saw blade is angled 30° toward the midline in the patella for the lateral and medial cuts and 45° distally for the proximal cut. The saw blade is angled 20° toward midline in the tibia for the lateral and medial cuts and 45° proximally for the distal cut. Thin ⅜- and ½-in. straight osteotomes are used to gently free the plug out from the patella. This process should be relatively easy if adequate saw cuts were previously made. Avoid excessive malleting and levering with the osteotomes to prevent cartilage damage and iatrogenic fracture. The final step of harvest consists of sharply dissecting remaining soft tissue attachments from the graft during removal with a scalpel. We typically fashion the femoral plug to be approximately 20 mm in length, while leaving the tibial plug longer at 25 mm and to easily pass through a 10-mm sizer. Standard anterolateral and anteromedial portals are created, and a diagnostic arthroscopy is performed. The femoral tunnel is created first. An arthroscope placed in the anterolateral portal is used to visualize the femoral footprint of the ACL. After soft tissue is cleared using an arthroscopic shaver and radiofrequency device, the LIR and the LBR can be identified. The LBR marks the separation between the anteromedial and posterolateral bundles of the ACL. The LIR, also known as resident's ridge, is more consistently identified arthroscopically, and this ridge represents the anterior margin of the anteromedial and posterolateral femoral bundles. An arthroscopic burr is used to perform a focal notchplasty to restore the anatomic shape of the intercondylar notch, which helps facilitate graft passage and prevents graft impingement, thereby ensuring knee range of motion after reconstruction. Then attention is turned to the tibial ACL attachment. An arthroscope placed in the anterolateral portal is used to visualize the tibial footprint of the ACL. The standard anteromedial portal is used as a working portal, and the tibial ACL guide set to 65° is placed through this portal to the anatomic center of the ACL. The anatomic footprint on the tibia is commonly identified arthroscopically as being approximately 9 mm posterior to the intermeniscal ligament, 7 mm anterior to the PCL, and should not exit the tibial plateau posterior to the anterior horn of the lateral meniscus. The guide should engage the tibia approximately halfway down the tibial tubercle bone plug harvest site roughly 1.5 to 2 cm medial to the tubercle. Graft passage after creation of the femoral and tibial tunnels is facilitated by previously placed “passing sutures” by retrieving the looped end through the distal tibial tunnel. The graft passage process is visualized arthroscopically through the anterolateral portal. The 4 suture ends on the patellar bone-plug end of the patellar tendon graft are placed through the loop and then pulled through the joint and out the lateral aspect of the femur and skin by assistance. The graft is pulled and positioned into the femoral tunnel under arthroscopic visualization with the aid of a 90° hemostat placed through the anteromedial portal, ensuring the graft does not twist during passage. The graft is pulled until the lateral wall of the tunnel is met with the bone plug. Femoral fixation of the ACL graft is performed with the knee in maximal flexion. Then a guide pin is inserted through the accessory medial portal with visualization from the anterolateral portal to the superior aspect of the graft and femoral tunnel junction. A 7- × 20-mm cannulated titanium interference screw is then placed under arthroscopic visualization; this is facilitated with a soft tissue, cannulated protector to prevent iatrogenic injury to the PCL. The screw is placed while an assistant is pulling lateral tension on the passed graft. Tibial fixation of the ACL graft is performed with the knee fully extended and the joint reduced. A guide pin is inserted to the superior-lateral aspect of the tunnel-graft interface. The assistant pulls the graft taut while a 9- × 20-mm cannulated titanium interference screw is used for tibial fixation. Excess bone that may be present outside of the tibial tunnel can be removed with an oscillating saw. Excess bone from the bone–patellar tendon–bone autograft that was saved during graft preparation is used as bone graft at the patellar and tibial harvest sites. A priority is placed on bone graft being used to fill the patellar bone void created during harvest. (ACL, anterior cruciate ligament; LBR, lateral bifurcate ridge; LIR, lateral intercondylar ridge; PCL, anterior cruciate ligament.)
References
- 1.Centers for Disease Control and Prevention. National Center for Health Statistics . Centers for Disease Control and Prevention; Atlanta, GA: 1996. National Hospital Discharge Survey: Annual summary. [Google Scholar]
- 2.Chalmers P.N., Mall N.A., Moric M. Does ACL reconstruction alter natural history? A systematic literature review of long-term outcomes. J Bone Joint Surg Am. 2014;96:292–300. doi: 10.2106/JBJS.L.01713. [DOI] [PubMed] [Google Scholar]
- 3.Gabler C.M., Jacobs C.A., Howard J.S., Mattacola C.G., Johnson D.L. Comparison of graft failure rate between autografts placed via an anatomic anterior cruciate ligament reconstruction technique: A systematic review, meta-analysis, and meta-regression. Am J Sports Med. 2016;44:1069–1079. doi: 10.1177/0363546515584043. [DOI] [PubMed] [Google Scholar]
- 4.Xie X., Liu X., Chen Z., Yu Y., Peng S., Li Q. A meta-analysis of bone-patellar tendon-bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee. 2015;22:100–110. doi: 10.1016/j.knee.2014.11.014. [DOI] [PubMed] [Google Scholar]
- 5.Webster K.E., Feller J.A., Hartnett N., Leigh W.B., Richmond A.K. Comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction: A 15-year follow-up of a randomized controlled trial. Am J Sports Med. 2016;44:83–90. doi: 10.1177/0363546515611886. [DOI] [PubMed] [Google Scholar]
- 6.Goldsmith M.T., Jansson K.S., Smith S.D., Engebretsen L., LaPrade R.F., Wijdicks C.A. Biomechanical comparison of anatomic single- and double-bundle anterior cruciate ligament reconstructions: An in vitro study. Am J Sports Med. 2013;41:1595–1604. doi: 10.1177/0363546513487065. [DOI] [PubMed] [Google Scholar]
- 7.Li S., Chen Y., Lin Z., Cui W., Zhao J., Su W. A systematic review of randomized controlled clinical trials comparing hamstring autografts versus bone-patellar tendon-bone autografts for the reconstruction of the anterior cruciate ligament. Arch Orthop Trauma Surg. 2012;132:1287–1297. doi: 10.1007/s00402-012-1532-5. [DOI] [PubMed] [Google Scholar]
- 8.Persson A., Fjeldsgaard K., Gjertsen J.E. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: A study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004-2012. Am J Sports Med. 2014;42:285–291. doi: 10.1177/0363546513511419. [DOI] [PubMed] [Google Scholar]
- 9.Gifstad T., Foss O.A., Engebretsen L. Lower risk of revision with patellar tendon autografts compared with hamstring autografts: A registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med. 2014;42:2319–2328. doi: 10.1177/0363546514548164. [DOI] [PubMed] [Google Scholar]
- 10.Rahr-Wagner L., Thillemann T.M., Pedersen A.B., Lind M. Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: Results from the Danish Registry of Knee Ligament Reconstruction. Am J Sports Med. 2014;42:278–284. doi: 10.1177/0363546513509220. [DOI] [PubMed] [Google Scholar]
- 11.Xie X., Xiao Z., Li Q. Increased incidence of osteoarthritis of knee joint after ACL reconstruction with bone-patellar tendon-bone autografts than hamstring autografts: A meta-analysis of 1,443 patients at a minimum of 5 years. Eur J Orthop Surg Traumatol. 2015;25:149–159. doi: 10.1007/s00590-014-1459-3. [DOI] [PubMed] [Google Scholar]
- 12.Kurz A., Evaniew N., Yeung M., Samuelsson K., Peterson D., Ayeni O.R. Credibility and quality of meta-analyses addressing graft choice in anterior cruciate ligament reconstruction: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;25:538–551. doi: 10.1007/s00167-016-4282-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is placed in the supine position on the operating table. Patellar tendon (bone-tendon-bone) harvest: The skin is initially marked from the patella to the tibial tubercle at the midline of the knee for a length of approximately 9 cm. Sharp dissection is carried through skin and subcutaneous tissue to the paratenon layer using a scalpel. The paratenon layer is separated from the underlying tendon in a thick flap, which is repaired during closure. We use a surgical marker to delineate the middle one-third of the patellar tendon and mark a desired graft width of 10 mm in the center of the tendon. We then use a scalpel to mark longitudinal incision, in line with the tendon fibers, in the center of the patellar tendon to the 10 mm desired width. A Bovie electrocautery device is used to delineate the patellar and tibial bone plugs and clear soft tissue from the bone to facilitate the harvest. The patellar bone plug measures 10 mm wide by 20 mm long, and the tibial bone plug measures 10 mm wide by 25 mm long from the tendinous insertion of the patellar tendon to the respective bones. A sagittal saw is then used to harvest the plugs from the previously measured and established tracks created before. The saw blade is angled 30° toward the midline in the patella for the lateral and medial cuts and 45° distally for the proximal cut. The saw blade is angled 20° toward midline in the tibia for the lateral and medial cuts and 45° proximally for the distal cut. Thin ⅜- and ½-in. straight osteotomes are used to gently free the plug out from the patella. This process should be relatively easy if adequate saw cuts were previously made. Avoid excessive malleting and levering with the osteotomes to prevent cartilage damage and iatrogenic fracture. The final step of harvest consists of sharply dissecting remaining soft tissue attachments from the graft during removal with a scalpel. We typically fashion the femoral plug to be approximately 20 mm in length, while leaving the tibial plug longer at 25 mm and to easily pass through a 10-mm sizer. Standard anterolateral and anteromedial portals are created, and a diagnostic arthroscopy is performed. The femoral tunnel is created first. An arthroscope placed in the anterolateral portal is used to visualize the femoral footprint of the ACL. After soft tissue is cleared using an arthroscopic shaver and radiofrequency device, the LIR and the LBR can be identified. The LBR marks the separation between the anteromedial and posterolateral bundles of the ACL. The LIR, also known as resident's ridge, is more consistently identified arthroscopically, and this ridge represents the anterior margin of the anteromedial and posterolateral femoral bundles. An arthroscopic burr is used to perform a focal notchplasty to restore the anatomic shape of the intercondylar notch, which helps facilitate graft passage and prevents graft impingement, thereby ensuring knee range of motion after reconstruction. Then attention is turned to the tibial ACL attachment. An arthroscope placed in the anterolateral portal is used to visualize the tibial footprint of the ACL. The standard anteromedial portal is used as a working portal, and the tibial ACL guide set to 65° is placed through this portal to the anatomic center of the ACL. The anatomic footprint on the tibia is commonly identified arthroscopically as being approximately 9 mm posterior to the intermeniscal ligament, 7 mm anterior to the PCL, and should not exit the tibial plateau posterior to the anterior horn of the lateral meniscus. The guide should engage the tibia approximately halfway down the tibial tubercle bone plug harvest site roughly 1.5 to 2 cm medial to the tubercle. Graft passage after creation of the femoral and tibial tunnels is facilitated by previously placed “passing sutures” by retrieving the looped end through the distal tibial tunnel. The graft passage process is visualized arthroscopically through the anterolateral portal. The 4 suture ends on the patellar bone-plug end of the patellar tendon graft are placed through the loop and then pulled through the joint and out the lateral aspect of the femur and skin by assistance. The graft is pulled and positioned into the femoral tunnel under arthroscopic visualization with the aid of a 90° hemostat placed through the anteromedial portal, ensuring the graft does not twist during passage. The graft is pulled until the lateral wall of the tunnel is met with the bone plug. Femoral fixation of the ACL graft is performed with the knee in maximal flexion. Then a guide pin is inserted through the accessory medial portal with visualization from the anterolateral portal to the superior aspect of the graft and femoral tunnel junction. A 7- × 20-mm cannulated titanium interference screw is then placed under arthroscopic visualization; this is facilitated with a soft tissue, cannulated protector to prevent iatrogenic injury to the PCL. The screw is placed while an assistant is pulling lateral tension on the passed graft. Tibial fixation of the ACL graft is performed with the knee fully extended and the joint reduced. A guide pin is inserted to the superior-lateral aspect of the tunnel-graft interface. The assistant pulls the graft taut while a 9- × 20-mm cannulated titanium interference screw is used for tibial fixation. Excess bone that may be present outside of the tibial tunnel can be removed with an oscillating saw. Excess bone from the bone–patellar tendon–bone autograft that was saved during graft preparation is used as bone graft at the patellar and tibial harvest sites. A priority is placed on bone graft being used to fill the patellar bone void created during harvest. (ACL, anterior cruciate ligament; LBR, lateral bifurcate ridge; LIR, lateral intercondylar ridge; PCL, anterior cruciate ligament.)