Abstract
GIP-dependent Cushing’s syndrome is caused by ectopic expression of glucose-dependent insulinotropic polypeptide receptor (GIPR) in cortisol-producing adrenal adenomas or in bilateral macronodular adrenal hyperplasias. Molecular mechanisms leading to ectopic GIPR expression in adrenal tissue are not known. Here we performed molecular analyses on adrenocortical adenomas and bilateral macronodular adrenal hyperplasias obtained from 14 patients with GIP-dependent adrenal Cushing’s syndrome and one patient with GIP-dependent aldosteronism. GIPR expression in all adenoma and hyperplasia samples occurred through transcriptional activation of a single allele of the GIPR gene. While no abnormality was detected in proximal GIPR promoter methylation, we identified somatic duplications in chromosome region 19q13.32 containing the GIPR locus in the adrenocortical lesions derived from 3 patients. In 2 adenoma samples, the duplicated 19q13.32 region was rearranged with other chromosome regions, whereas a single tissue sample with hyperplasia had a 19q duplication only. We demonstrated that juxtaposition with cis-acting regulatory sequences such as glucocorticoid response elements in the newly identified genomic environment drives abnormal expression of the translocated GIPR allele in adenoma cells. Altogether, our results provide insight into the molecular pathogenesis of GIP-dependent Cushing’s syndrome, occurring through monoallelic transcriptional activation of GIPR driven in some adrenal lesions by structural variations.
Keywords: Endocrinology
Keywords: Molecular pathology
Ectopic GIPR expression in GIP-dependent Cushing’s syndrome occurs from a single GIPR gene allele through somatic 19q13 microduplications and chromosome rearrangements.
Introduction
Adrenal Cushing’s syndrome results from excessive pituitary adrenocorticotropin–independent (ACTH-independent) cortisol production by benign or malignant adrenocortical tumors or from bilateral adrenal hyperplasia. The recent identification of activating somatic mutations of the PRKACA gene in one-third of cortisol-secreting adrenal adenomas (1–3) and of germline and secondary somatic inactivating mutations of ARMC5 in approximately 50% of operated patients with apparently sporadic primary bilateral macronodular adrenal hyperplasias (4) has provided important new insights into the molecular pathogenesis of adrenal Cushing’s syndrome. Regulatory mechanisms of cortisol secretion in patients with bilateral macronodular hyperplasia, such as ectopic adrenal ACTH production, have also been recently discovered (5).
In a subset of patients with adrenal Cushing’s syndrome, the cortisol excess is driven by aberrant (ectopic or excessive) expression of certain G protein–coupled receptors in adrenal lesions (6, 7). Although the molecular pathogenesis of food-dependent Cushing’s syndrome is unknown, the condition is associated with ectopic glucose-dependent insulinotropic polypeptide receptor (GIPR) expression in adrenocortical adenomas or bilateral macronodular adrenal hyperplasia (8–10). Adrenal GIPR exposes the gland to inappropriate postprandial stimulation by glucose-dependent insulinotropic polypeptide (GIP). Activation of the ectopic receptor, functionally coupled to cAMP signaling, triggers adrenal cell proliferation and excessive hormone production (6). Here, we report molecular events leading to adrenal GIPR expression in a large international collection of adrenocortical adenomas and bilateral macronodular adrenal hyperplasias derived from patients with GIP-dependent adrenal Cushing’s syndrome or with GIP-dependent primary aldosteronism.
Results
Clinical presentation.
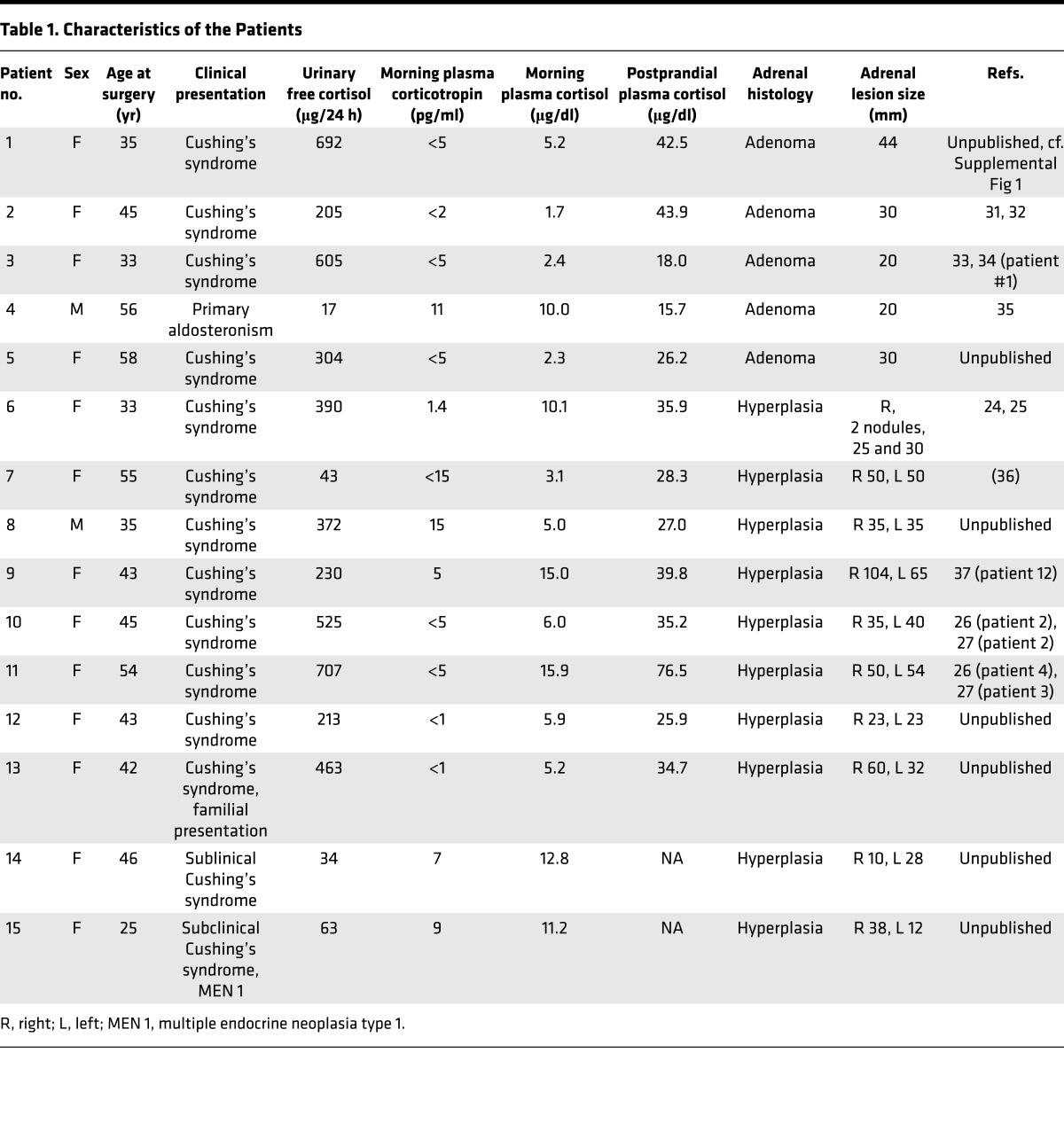
Detailed clinical phenotypes are described in Table 1 and Supplemental Figure 1; supplemental material available online with this article; https://doi.org/10.1172/jci.insight.92184DS1 Twelve patients had overt Cushing’s syndrome, two patients had subclinical Cushing’s syndrome and one patient had primary aldosteronism. One patient (#13) presented with familial nonsyndromic Cushing’s syndrome, and one patient (#15) presented with multiple endocrine neoplasia type 1 (MEN 1), caused by the frameshift 219–220delCG mutation in the MEN1 gene; other patients had nonsyndromic and nonfamilial presentations.
Table 1. Characteristics of the Patients.
Adrenal expression of GIPR occurs from a single allele of the GIPR gene.
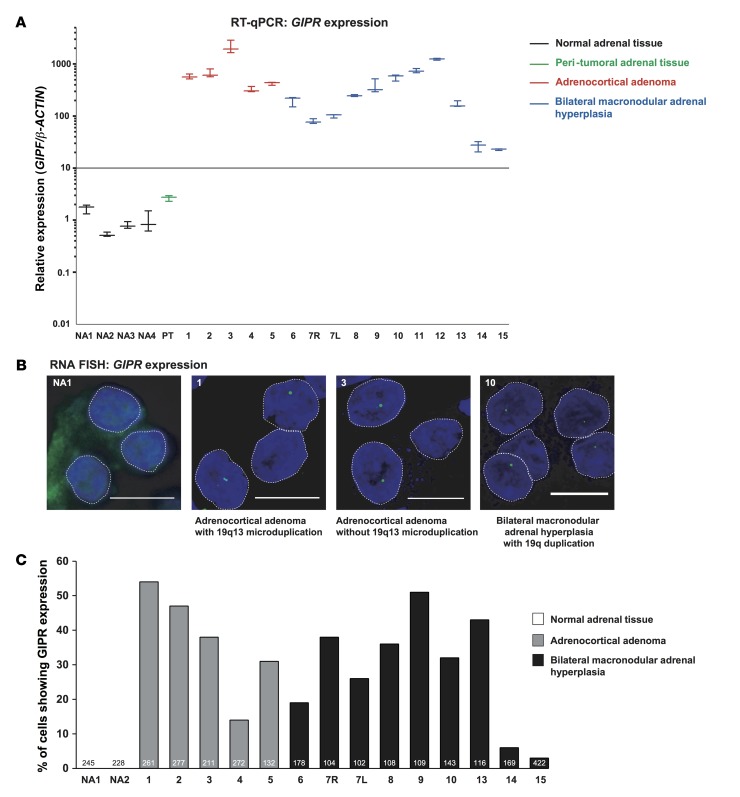
We detected a somatic CTNNB1 p.Ser45Cys mutation in the tumor DNA of patient #1. No abnormalities in other genes known to be associated with adrenocortical adenomas and bilateral macronodular adrenal hyperplasias were detected in the tumor DNA of all 15 patients. The GIPR expression profile in the adrenal samples is shown in the Figure 1A. The relative abundance of GIPR transcripts in the normal adrenal tissue samples was very low, estimated at 26 molecules/μg RNA. All 16 adrenal samples selected for the study showed abundant GIPR expression (more than 10-fold of the mean expression in the unaffected adrenal tissue samples). The relative abundance of GIPR transcripts was not different between the adenoma and hyperplasia samples. Peritumoral adrenal tissue from patient #1 did not express GIPR. Interestingly, as reported previously (11), concomitant aberrant expression of one or more G protein–coupled hormone receptors was detected in one adenoma (from patient #4) and in 3 hyperplasia samples (from patient #6, #10, and #11) in addition to GIPR (Supplemental Figure 2).
Figure 1. Adrenal glucose-dependent insulinotropic polypeptide receptor (GIPR) expression in patients with GIP-dependent Cushing’s syndrome or aldosteronoma.
(A) GIPR expression profile in adrenal tissue samples obtained on reverse transcription quantitative PCR (RT-qPCR) and normalized to the β-actin housekeeping gene. Similar results were obtained when GIPR expression was normalized to 18S. Four samples of normal adrenal tissue (NA1–NA4); non-tumorous adrenal tissue (PT) adjacent to adenoma of patient #1; 5 adrenocortical adenomas; and 10 bilateral adrenal hyperplasias from patients with aberrant adrenal sensitivity to GIP were studied. In one patient with bilateral adrenal hyperplasia (#7), samples from both adrenal lesions (R, right; L, left) were analyzed. Results are expressed as relative GIPR expression compared with mean expression level in the unaffected adrenal tissue samples, arbitrary set at 1, representing 1.60 × 10–4 ± 0.54 × 10–4 amol/amol of β-actin. The expression of GIPR in adrenal lesions of patients with GIP-dependent Cushing’s syndrome or aldosteronoma was increased (570 ± 159–fold, ranging from 23- to 2,152-fold) compared with the mean expression level in the unaffected adrenal tissue (P < 0.0001, Mann-Whitney U test). Experiments were performed twice; one representative experiment is shown here. Three independent determinations were done for each sample. The lines represent the median values; the whiskers represent the minimal and maximal values. (B) Representative examples of adrenal GIPR expression as assessed by RNA FISH in adrenal lesions with or without 19q13 duplication. Monoallelic (a maximum of one RNA FISH signal is visible per nucleus) GIPR expression in interphase nuclei is visible as one green pinpoint in adrenal lesions of patients with GIP-dependent Cushing’s syndrome or aldosteronoma. RNA FISH analysis was performed on all adrenal lesions with aberrant sensitivity to GIP, except for lesions of patient #11 and #12, due to the lack of good quality frozen tissue in these two samples. Normal adrenal tissue did not show any GIPR expression. (C) Percentage of nuclei with monoallelic GIPR expression determined by RNA FISH. At the bottom of the histogram, the number of analyzed nuclei is indicated. Scale bars: 5 μm.
To determine how many GIPR alleles are actively transcribed in patients’ adrenal cells, we applied nascent RNA FISH, allowing detection of nascent RNA molecules at their transcription sites. This method enables the study of GIPR expression at the single-cell level and takes into account the heterogeneity of the adrenal lesions. The method enables the quantification of the number of GIPR alleles transcribed in the patients’ adrenal cells. Consistent with quantitative PCR (RT-qPCR) results, normal adrenal tissue did not show GIPR expression. All adenoma and hyperplasia samples expressed GIPR from a single allele in a different proportion of nuclei (Figure 1B, representative samples showing monoallelic GIPR expression). Furthermore, samples showing the highest GIPR transcript levels measured by RT-qPCR (Figure 1A) also exhibited the highest proportion of nuclei expressing GIPR (Figure 1C).
Identification of 19q13.32 duplications.
We studied the molecular events leading to transcriptional activation of a single allele of the GIPR gene in the adrenal lesions. We performed pyrosequencing of the GIPR promoter region (chr19: 46,171,165–46,171,452), containing 10 CpG islands. Of note, 3 CpGs were located close to functional Sp1/Sp3 binding motifs as described previously (12). Pyrosequencing showed absence of methylation in the proximal GIPR promoter in normal adrenal tissue, adenoma, and hyperplasia samples (Supplemental Figure 3).
Alternatively, transcriptional activation of a single allele of GIPR could be related to structural chromosomal imbalances. Oligonucleotide-based array comparative genomic hybridization analysis (array-CGH) was used to map somatic DNA copy number alterations (CNAs) in all adenoma and hyperplasia samples. The global CGH array profile is presented in Supplemental Figure 4, and identified CNAs are described in detail in Supplemental Tables 1–3. Very few CNAs were detected in adenoma samples, suggesting that GIPR-expressing adenomas belong to the “CNA-negative” subgroup of adrenocortical tumors (2). In contrast, as previously shown (13), hyperplasia samples had a higher number of extensive chromosomal imbalances.
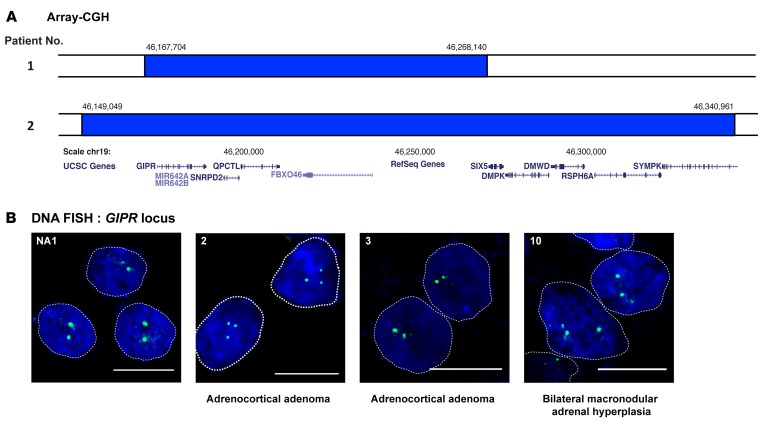
In 3 samples, we identified somatic duplication in 19q13.32. In patient #1, array-CGH revealed a microduplication of 19q13.32 encompassing a 100.4-kb region (hg19 assembly, chr19:46,167,704–46,268,140) in the adrenal adenoma (Figure 2A). The duplication was not found in adjacent non-tumorous adrenal tissue and in the germline DNA. In patient #2, array-CGH also revealed a microduplication of 19q13.32 encompassing a 191.9-kb region (hg19 chr19:46,149,049–46,340,961) in the adrenal adenoma (Figure 2A). In patient #10, the entire long arm of chromosome 19 was duplicated in hyperplasia tissue, with ratios suggesting mosaicism. Again, this duplication was absent in the germline DNA. No duplications in 19q13.32 were identified in 4 GIP nonresponsive adenoma samples and 11 GIP nonresponsive hyperplasia samples. The smallest regions of overlap (hg19 chr19: 46,167,704–46,268,140) encompassed 5 genes, namely GIPR, SNRPD2, QPCTL, FBXO46, and SIX5. RT-qPCR of RNA of these adrenal samples versus RNA from unaffected adrenal tissue showed that GIPR was the only overexpressed gene. Expression of the other 4 duplicated genes was not significantly different (Supplemental Figure 5).
Figure 2. Genomic 19q13 duplications in adrenal lesions of 3 patients with glucose-dependent insulinotropic polypeptide–dependent (GIP-dependent) Cushing’s syndrome.
(A) 19q13 microduplications, as seen on oligonucleotide-based array comparative genomic hybridization analysis (array-CGH), in the adenomas of patients #1 and #2. Duplicated genomic segments are shown in blue and adjacent nonduplicated segments in white. The genomic coordinates of the duplicated segments are shown above the blue boxes. The magnification scale of chromosome 19 and the genomic content in the duplicated regions are shown below the boxes (adapted from the UCSC Genome Browser, http://genome.ucsc.edu/). (B) Representative examples of GIP receptor (GIPR) loci visualized by DNA FISH analysis. Three GIPR loci (green) are visible in the majority of the interphase nuclei in the adrenal tissue of 3 patients with genomic 19q13 duplication on array-CGH (Supplemental Figure 4), represented here by samples of patients #2 and #10. DNA FISH analysis of the adrenal sample of patient #1 is shown in Figure 3C. Two GIPR loci are present in the interphase nuclei of the normal adrenal tissue and in adrenal lesions without 19q13 duplication on array-CGH, represented by adenoma of patient #3. Scale bars: 5 μm.
DNA FISH confirmed duplication of the GIPR locus in adenoma samples from patients #1 and #2 and a hyperplasia sample from patient #10. As expected, two GIPR loci were observed in normal adrenal tissue. Other adenoma and hyperplasia samples also had two detectable GIPR alleles as resolved by DNA FISH (Figure 2B).
Characterization of the chromosomal rearrangements.
To further characterize the molecular events leading to transcriptional activation of a single allele of GIPR, we performed mate-pair sequencing on DNA samples from 6 selected adrenal lesions. We analyzed DNA from the 3 adrenal lesions harboring the 19q13.32 duplication and from 3 lesions without CNAs on the GIPR locus. Sequencing of mate-pair libraries yielded 121,226,487 ± 18,679,783 mapped pairs with insert sizes of 3.4 ± 0.8 kb. This provided effective coverage of 68 ± 14× relative to the six billion base pair diploid genome in adrenal cells. BAM preprocessing with SVDetect yielded 12,752,546 ± 2,772,124 abnormally mapped pairs.
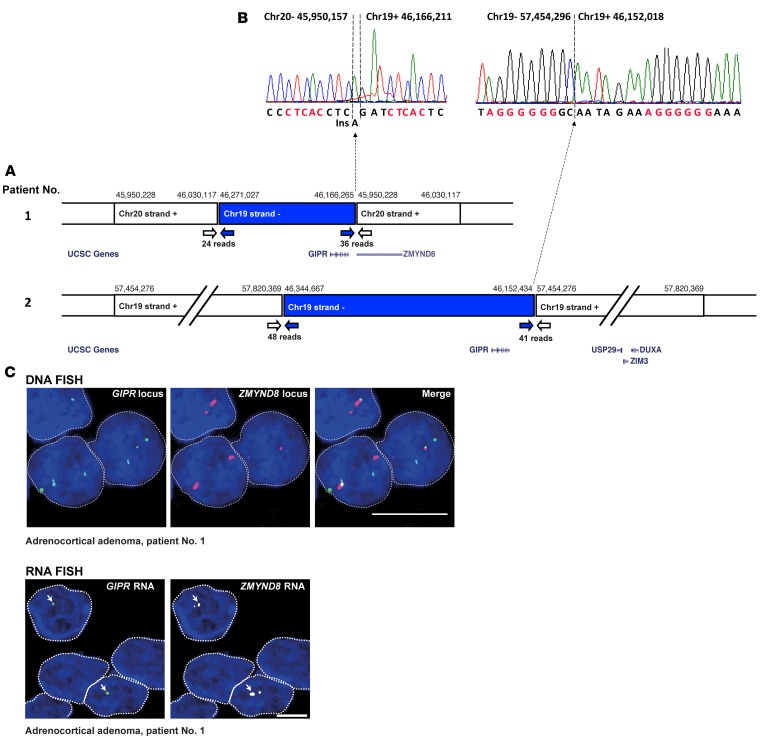
In the adenoma of patient #1, mate-pair SVDetect analysis identified an interchromosomal rearrangement between the duplicated segments 19q13.32 and 20q13.12. Abnormal pairs indicated two breakpoints (hg19 chr19:46,166,265–chr20:45,950,228 and chr19:46,271,027–chr20:46,030,117) compatible with duplication of one of these chromosome segments, separated by insertion of the other nonduplicated segment in inverted orientation. Similarly, in adenoma from patient #2, mate-pair analysis identified an intrachromosomal rearrangement between the duplicated segments 19q13.32 and 19q13.43. Abnormal pairs revealed two breakpoints (hg19 chr19:46,152,434–57,454,276 and chr19:46,344,667–57,820,369), indicating a similar configuration of the rearrangement (Figure 3A). In both adenoma samples, breakpoints close to the GIPR gene were characterized at base pair resolution by conventional Sanger sequencing of the PCR fragments (Figure 3B), showing a junction of canonical nonhomologous end-joining typical of chromosomal translocations in human cells (14). In the hyperplasia sample of patient #10 with 19q duplication, mate-pair analysis did not identify breakpoints at the pericentromeric region. In the other 4 samples, mate-pair SVDetect analysis did not reveal rearrangements, including at the GIPR locus.
Figure 3. Chromosome rearrangements in adrenocortical adenoma of two patients with glucose-dependent insulinotropic polypeptide–dependent (GIP-dependent) Cushing’s syndrome drive ectopic GIP receptor (GIPR) expression in adenoma cells.
(A) Genomic rearrangements in adenoma samples from patient #1 and #2, as revealed by mate-pair analysis. Next-generation sequencing (NGS) data identified abnormally mapped reads corresponding in tumor from patient #1 to interchromosomal rearrangement between chromosome segments 19q13.32 and 20q13.12, and in tumor from patient #2 to intrachromosomal rearrangement between chromosome segments 19q13.32 and 19q13.43. The genomic coordinates of the rearranged genomic segments are shown above the boxes. White and blue arrows indicate abnormal reads corresponding to break points. Selected genes in the rearranged chromosome segments are shown below the boxes (adapted from the UCSC Genome Browser). The break point at position hg19 chr20:45,950,228 in adenoma from patient #1 corresponds to the second intron of the zinc finger and the MYND (myeloid, Nervy, and DEAF-1) domain containing 8 (ZMYND8) gene, which is consequently truncated. In the adenoma of patient #2, the break point at position hg19 chr19:57,454,276 falls within a noncoding region of chromosome 19. (B) The breakpoints in the proximity of the GIPR gene at base-pair resolution, characterized by conventional Sanger sequencing of the PCR fragments, showing one base-pair insertion (Ins) typical of canonical nonhomologous end-joining. Microhomologies are indicated in red. (C) DNA (top) and RNA FISH (bottom) analyses in adenoma of patient #1. On DNA FISH, 3 GIPR loci (green) and two ZMYND8 loci (red) are visible in each interphase nucleus. Thus, DNA FISH confirms duplication of the 19q13.32 region and its insertion in close proximity to ZMYND8 in this sample. Representative examples of GIPR expression (green) and of ZMYND8 expression (white) in adenoma of patient #1, as analyzed by RNA FISH, are also shown. Arrows indicate GIPR expression from a single allele in each nucleus. The RNA FISH signal corresponds to the translocated GIPR allele fused with intron 2 of the ZMYND8 gene located in chromosome region 20q13.12. Scale bars: 5 μm.
The rearranged genomic environment drives aberrant monoallelic expression of GIPR.
To further explore the functional impact of the GIPR genomic rearrangements as identified in adenoma of the patient #1, we performed DNA and RNA FISH on this sample. We confirmed the insertion of the duplicated 19q13.32 region in close proximity to the ZMYND8 gene (zinc finger and MYND [myeloid, Nervy, and DEAF-1] domain containing 8) on chromosome 20. RNA FISH revealed that GIPR was only expressed from the allele translocated on chromosome 20, as indicated by ZMYND8 expression (Figure 3C).
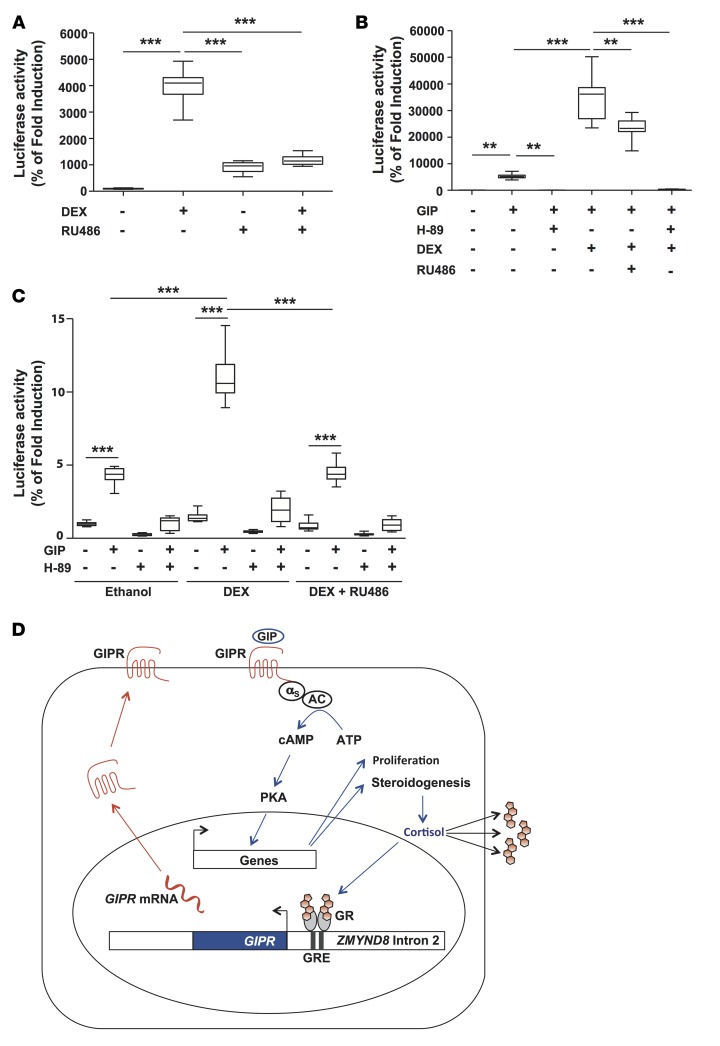
We investigated the functional impact of the newly observed genomic environment in the tumor of patient #1. In this tumor, the chromosome rearrangement juxtaposed the GIPR gene to the second intron of the ZMYND8 gene, which contains an alternative start site for RNA polymerase II and several cis-acting regulatory elements, including a glucocorticoid response element (GRE) (15) (Supplemental Figure 6A) and Sp1 binding motifs. Transient transfections of HEK 293T cells with a ZMYND8 intron 2-pGL4.26-luciferase vector showed transcriptional activation of ZMYND8 intron 2 by glucocorticoids, confirming the functional status of the GRE (Figure 4A). Expression of a chimeric ZMYND8 intron 2-pGL4.26-GIPR vector (Supplemental Figure 6B) in HEK 293T cells and in adrenocortical H295R cells resulted in increased cAMP signaling in the presence of 10–7 M GIP, which was abolished by the protein-kinase A inhibitor H-89. Co-treatment with dexamethasone resulted in a significant increase in cAMP production by HEK 293T cells (Figure 4B) and by H295R cells (Figure 4C). Thus, this GRE-containing fragment of intron 2 of ZMYND8 was sufficient to drive GIPR expression.
Figure 4. Functional analysis of zinc finger and MYND (myeloid, Nervy, and DEAF-1) domain containing 8 (ZMYND8) intron 2–glucose-dependent insulinotropic polypeptide receptor (GIPR) chromosome rearrangement.
(A) Transient transfection assays of HEK 293T cells with a ZMYND8 intron 2-pGL4.26-Luciferase vector (Supplemental Figure 5A). Transactivation of ZMYND8 intron 2 by dexamethasone (DEX), and its prevention by the glucocorticoid receptor antagonist RU486, confirms the functional status of the glucocorticoid response element (GRE) in ZMYND8 intron 2. Transient transfection assays of HEK 293T cells (B) and adrenocortical H295R cells (C) with a chimeric ZMYND8 intron 2–pGL4.26–GIPR plasmid (Supplemental Figure 5B) and a CRE-Luc reporter vector. Treatment with glucose-dependent insulinotropic polypeptide (GIP) resulted in increased cAMP signaling, as shown by transactivation of the cAMP response elements (CRE) in the CRE-Luc vector, indicating that transfected cells expressed functional GIPR. Co-treatment with dexamethasone resulted in a significant increase in GIP-induced cAMP production, demonstrating enhancement of GIPR expression by glucocorticoids. Data in A–C are presented as box-and-whisker plots. The bounds of the boxes represent the first and the third quartiles (bottom and top of the box); the lines within the boxes represent the median values; the whiskers depict the minimal and maximal values. Presented data are the means of 2 independent experiments, with n = 8 for each experiment. Statistical significance was evaluated by Kruskal-Wallis test followed by Dunn’s post-test. **P < 0.01, ***P < 0.001. (D) Schematic representation of the positive regulatory loop that maintains ectopic GIPR expression in the adenoma of patient #1.
Discussion
Since the initial description of GIP-dependent Cushing’s syndrome (9, 10), molecular mechanisms responsible for ectopic GIPR expression in adrenal tissue have remained elusive (6). Here, we describe the results of combined molecular analyses in the largest reported collection of adrenocortical adenomas and bilateral macronodular adrenal hyperplasias from patients with GIP-dependent Cushing’s syndrome or aldosteronism. GIPR expression analysis by RNA FISH consistently demonstrated GIPR expression from a single allele in all adenoma and hyperplasia samples with aberrant sensitivity to GIP, whereas GIPR was not expressed in normal adrenal cells. Monoallelic GIPR expression observed in all adrenal lesions suggested a common disease mechanism leading to transcriptional activation of a single allele of this gene. Either chromosome rearrangements and point mutations and/or epigenetic abnormal modifications of the GIPR regulatory region (promoter or enhancer) could underlie inappropriate adrenal lesion GIPR expression.
Indeed, molecular and cytogenetic assessments showed that 3 adrenal lesions harbored somatic duplications in chromosome region 19q13.32. The duplicated region that was common to all 3 samples contained 5 protein-encoding genes, of which only GIPR, located at the extremity of the duplicated region, was markedly overexpressed in these adrenocortical lesions. Recently, we described Xq26.3 microduplications in patients with early-onset acrogigantism (16), showing that genomic gains may promote inappropriate hormonal hypersecretion.
In two adenoma samples, the duplicated 19q13.32 region was rearranged with other chromosome regions, whereas in one hyperplasia sample, 19q duplication without chromosome rearrangements was detected. Examples of genomic rearrangements in endocrine tumors include gene fusion involving the RET oncogene in papillary thyroid carcinomas (17), a chimeric 11 β-hydroxylase/aldosterone synthase gene in glucocorticoid-remediable aldosteronism (18), and juxtaposition of the parathyroid hormone promoter with the cyclin D gene in some parathyroid adenomas (19). In the two tumors described here, chromosome rearrangements did not result in fusion of the coding sequences of two genes but placed GIPR in a chromatin environment favoring transcriptional activation in the vicinity of cis-acting regulatory regions. As shown by RNA FISH experiments, this genomic environment drove abnormal expression of the translocated GIPR allele in the cells in both adenomas.
In the adenoma of patient #1, GIPR was fused with an intronic regulatory region of the ZMYND8 gene located in chromosome region 20q13.12. ZMYND8 is ubiquitously expressed and plays a role in chromatin recognition of transcription-associated DNA damage (20, 21). We show that GIPR expression in this tumor was positively regulated by glucocorticoids via a functional GRE located in the second intron of ZMYND8 (15). Consequently, GIPR stimulation by GIP led to postprandial cortisol production, which maintained inappropriate GIPR expression, thus forming an intracrine and/or paracrine positive regulatory loop responsible for excess cortisol (Figure 4D). In the adenoma of patient #2, GIPR was placed in a vast intergenic region, with the closest protein-coding gene USP29 situated 176 kb from the break point. Recently, the Encyclopedia of DNA Elements (ENCODE) enabled us to assign biochemical functions for 80% of the genome, in particular outside of the well-studied protein-coding regions, pointing out the importance of such apparent “desert” intergenic regions in transcriptional regulation (15).
The observation of structural variations on the 19q13.32 locus does not apply to other adenoma and bilateral macronodular adrenal hyperplasia cases analyzed. Genetic or epigenetic alterations in the GIPR promoter region could be the cause of transcriptional activation of GIPR in these adrenal lesions without structural variations on the 19q13.32 locus. However, no changes in methylation of the proximal GIPR promoter were detected in this study (Supplemental Figure 3). Considering the possible link between chronic pituitary ACTH stimulation in Cushing’s disease and adrenal GIPR expression (22), in some cases of primary bilateral macronodular hyperplasia adrenal GIPR expression could be amplified by ectopic ACTH produced within the adrenocortical tissue (5).
Several adrenal lesions expressed more than one aberrant receptor (Supplemental Figure 2). No genomic duplications in the corresponding loci were detected by array-CGH analysis in these 4 patients. Of note, in patients #7 (left adrenal lesion) and #10, the entire long arm of the chromosome 1 was duplicated. Chromosome 1q contains the gene encoding vasopressin receptor type 1b receptor, AVPR1b, but AVPR1b was not expressed in these lesions. In contrast to microduplications with chromosome rearrangements, which create a novel genomic environment favorable for transcription, arm-level duplications alone are probably not sufficient to drive aberrant gene expression. How several receptors encoded on different chromosomes can be expressed in the same tissues remains enigmatic. Recently, a link between activating CTNNB1 p.Ser33Cys, p.Gly34Arg, and p.Ser45Phe mutations and overexpression of gonadotropin-releasing hormone receptor and luteinizing hormone/chorionic gonadotropin receptor in 3 aldosterone-producing adenomas has been suggested (23). We did not identify these CTNNB1 mutations, in particular in 3 bilateral macronodular adrenal hyperplasia samples (24–27) that also overexpressed luteinizing hormone/chorionic gonadotropin receptor (Supplemental Figure 2). As reported by others (28), the relation between these CTNNB1 mutations and gonadal receptor expression thus seems not to be a recurrent finding.
However, one GIPR-expressing adrenal adenoma harbored a somatic CTNNB1 p.Ser45Cys mutation, which could contribute to tumor development. By analogy, the MEN1 mutation in patient #15 may have presented a genetic hit leading to bilateral adrenal hyperplasia development. No mutations in genes known to be involved in adrenal tumorigenesis were identified in the remaining 14 adrenal lesions. In particular, consistent with previous reports (4, 29), no ARMC5 mutations were detected in any of the patients with GIP-dependent Cushing’s syndrome studied. Thus, ARMC5-related bilateral macronodular adrenal hyperplasia and GIPR-dependent adrenal proliferation seem to have different pathogeneses. Activation of the ectopic GIP receptor, functionally coupled to cAMP signaling, not only triggers excessive hormone production, but very likely contributes to adrenal cell proliferation and tumor development as demonstrated in mice (30).
In conclusion, we demonstrated that ectopic GIPR expression in adrenocortical adenomas and in bilateral macronodular adrenal hyperplasias of patients with GIP-dependent Cushing’s syndrome or GIP-dependent aldosteronism is consistently associated with transcriptional activation of a single allele of the GIPR gene. Three adrenal lesions harbored somatic duplications in 19q13.32 containing the GIPR; in two, genomic gain was associated with chromosomal rearrangements, creating a chromatin environment favoring GIPR transcription.
Methods
Patients.
We analyzed 16 adrenal samples derived from 15 patients who had undergone adrenalectomy for adrenocortical adenoma or ACTH-independent bilateral macronodular adrenal hyperplasia. In a patient with primary bilateral macronodular adrenal hyperplasia (#7, Table 1), samples from both adrenal lesions were available for analysis. Samples were collected at 8 endocrine centers in Europe, the USA, and Canada. All adrenal lesions with proven GIPR expression available in these participating centers were selected for the study. Fourteen specimens were obtained from 12 patients with overt GIP-dependent Cushing’s syndrome and from one patient with GIP-dependent aldosteronism. Eight of these cases were previously reported (24–27, 31–37). GIP-dependent Cushing’s syndrome was diagnosed according to standard criteria showing hypercortisolism (38) in combination with low morning (fasting) plasma cortisol and ACTH concentrations and an increase in plasma cortisol concentration in response to a meal or to other tests, such as GIP infusion. GIP-dependent aldosteronism was diagnosed in a patient presenting with classical clinical and biological criteria of hyperaldosteronism (39) and a significant postprandial and post–GIP infusion renin-independent increase in plasma aldosterone concentration. Two additional primary bilateral macronodular adrenal hyperplasia samples from patients with subclinical Cushing’s syndrome without presurgical biochemical demonstration of aberrant adrenal sensitivity to food were included (patients #14 and #15), based on GIPR expression screening among 78 adrenal lesion samples derived from patients with overt or subclinical Cushing’s syndrome collected at the NIH. We further included 4 samples of adrenocortical adenomas and 11 samples of bilateral adrenal hyperplasia with no GIPR expression as controls. Eleven of these control samples were obtained from patients with adrenal Cushing’s syndrome, two samples were from patients with primary hyperaldosteronism, and one sample was from a patient with nonfunctioning adrenal adenoma. We also studied samples of macroscopically and histologically unaffected adrenals obtained from 4 subjects who underwent total nephrectomy with adrenalectomy for renal cell carcinoma and peritumoral adrenal tissue from patient #1 (Table 1). We analyzed leukocyte DNA from patients #1 and #10.
Molecular analysis of the adrenal lesions and in vitro studies.
We sequenced the ARMC5, PRKACA, and PRKAR1A genes, exon 3 of the CTNNB1 gene, and exons 7–9 of the GNAS gene in DNA extracted from the adrenal lesions. We measured gene expression levels in adrenal samples using reverse transcription qPCR (RT-qPCR). We analyzed expression of ADRB1, AGTR1, AVPR1a, GIPR, GnRHR, HTR4, LHCGR, MC2R, QPCTL, SIX5, SNRPD2, FBOX46, and ZMYND8 (Supplemental Table 4). We applied DNA and RNA FISH to frozen samples. We performed array-CGH on DNA samples from the adrenal lesions. We performed mate-pair analyses on the tumor DNA of 6 patients. We transfected human HEK 293T cells and adrenocortical H295R cells with the ZMYND8 intron 2-pGL4.26-Luc and ZMYND8 intron 2-pGL4.26-GIPR plasmid constructs for in vitro studies. More details are provided in Supplemental Methods, available online with this article.
Study approval.
Patients with adrenocortical adenomas and bilateral macronodular adrenal hyperplasias expressing GIPR and patients from whom unaffected adrenal tissue was obtained gave written informed consent for genetic analyses; all studies were approved by the local ethics committee at Bicêtre hospital, Le Kremlin-Bicêtre, France.
Statistics.
Data are expressed as mean ± SEM. Differences between groups were analyzed by nonparametric Mann-Whitney U test or Kruskal-Wallis test, followed by Dunn’s post-test (Prism, GraphPad Software). P values less than 0.05 were considered statistically significant.
Author contributions
ALL, CAS, SV, RC, VD, NS, HL, EL, AL, PC, J. Bouligand, and PK contributed to the conception and design of the research; ALL, SV, RC, LT, VD, MH, PH, HGB, GT, VB, EC, EL, J. Bouligand, and PK conducted experiments ; ALL, CAS, SV, RC, LT, VD, AB, FRF, PH, HGB, SS, GT, AGM, JY, ML, and EL acquired data ; ALL, SV, RC, LT, VD, AGB, FRF, PH, EL, J. Bouligand, and PK analyzed data ; CAS, CA, IB, DM, AT, J. Bertherat, HL, WdH, and AL provided tissue samples; CAS, SV, RC, J. Bouligand, and PK wrote the manuscript.
Supplementary Material
Acknowledgments
This work was supported by grants from Inserm and Université Paris-Sud. ALL was the recipient of a “Poste d’Accueil Inserm” and a fellowship from the Association de Recherche contre le Cancer (ARC). VD was the recipient of a “Allocation Année-Recherche” from CHU de Brest. PK was the recipient of a “Contrat d’Interface Inserm.” This work was also supported in part by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the ERA-NET E-Rare-2-GOSAMPAC. The authors are indebted to Gaëlle Barrande, Sarah Cazenave, Olivier Chabre, Rachel Desailloud, Philippe Emy, Benoit Lambert, Aurore Mensah, Marie-Laure Nunes, Jean-Jacques Patard, and Yves Reznick for their help in collecting adrenal tissues; Sophie Brisset, Erika Brunet, Edith Heard, Agnès Linglart, and Florence Tenenbaum for helpful discussions; Sylvain Baulande, Bruno Francou, Patricia Legoix-Ne, Florian Nadal, and Thomas Rio Frio for their help with next-generation sequencing; and Bernard Thorens for the gift of the hGIPR plasmid. We are indebted to Andrew Demidowich (NICHD, NIH, Bethesda, MD, USA), Ricardo Correa (now at Endocrinology, Medicine, Brown University Medical School, Providence, RI, USA), and Paraskevi Salpea (now at the University of Brussels, Brussels, Belgium) for assisting with data and tissue collection from patients at the NICHD, NIH, Bethesda, MD, USA.
Version 1. 09/21/2017
Electronic publication
Funding Statement
Poste d’Accueil Inserm, Contrat d’Interface Inserm, Association de Recherche contre le Cancer
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Reference information: JCI Insight. 2017;2(18):e92184. https://doi.org/10.1172/jci.insight.92184.
Contributor Information
Anne-Lise Lecoq, Email: anne-lise.lecoq@u-psud.fr.
Say Viengchareun, Email: say.viengchareun@u-psud.fr.
Lucie Tosca, Email: lucie.tosca@abc.aphp.fr.
Vianney Deméocq, Email: vianney.demeocq@gmail.com.
Mirella Hage, Email: mirella.hage@u-psud.fr.
Annabel Berthon, Email: annabel.berthon@nih.gov.
Fabio R. Faucz, Email: fabio.faucz@nih.gov.
Patrick Hanna, Email: patrickhanna@live.com.
Nicolas Servant, Email: nicolas.servant@curie.fr.
Sylvie Salenave, Email: sylvie.salenave@bct.aphp.fr.
Clovis Adam, Email: clovis.adam@bct.aphp.fr.
Vanessa Benhamo, Email: vanessabenhamo@hotmail.fr.
Eric Clauser, Email: eric.clauser@inserm.fr.
Anne Guiochon-Mantel, Email: anne.mantel@aphp.fr.
Jacques Young, Email: jacques.young@aphp.fr.
Marc Lombès, Email: marc.lombes@u-psud.fr.
Isabelle Bourdeau, Email: isabelle.bourdeau@umontreal.ca.
Dominique Maiter, Email: dominique.maiter@uclouvain.be.
Antoine Tabarin, Email: antoine.tabarin@chu-bordeaux.fr.
Jérôme Bertherat, Email: jerome.bertherat@aphp.fr.
Hervé Lefebvre, Email: herve.lefebvre@chu-rouen.fr.
Wouter de Herder, Email: w.w.deherder@erasmusmc.nl.
Estelle Louiset, Email: Estelle.Louiset@univ-rouen.fr.
Philippe Chanson, Email: philippe.chanson@bct.aphp.fr.
References
- 1.Beuschlein F, et al. Constitutive activation of PKA catalytic subunit in adrenal Cushing’s syndrome. N Engl J Med. 2014;370(11):1019–1028. doi: 10.1056/NEJMoa1310359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goh G, et al. Recurrent activating mutation in PRKACA in cortisol-producing adrenal tumors. Nat Genet. 2014;46(6):613–617. doi: 10.1038/ng.2956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cao Y, et al. Activating hotspot L205R mutation in PRKACA and adrenal Cushing’s syndrome. Science. 2014;344(6186):913–917. doi: 10.1126/science.1249480. [DOI] [PubMed] [Google Scholar]
- 4.Assié G, et al. ARMC5 mutations in macronodular adrenal hyperplasia with Cushing’s syndrome. N Engl J Med. 2013;369(22):2105–2114. doi: 10.1056/NEJMoa1304603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Louiset E, et al. Intraadrenal corticotropin in bilateral macronodular adrenal hyperplasia. N Engl J Med. 2013;369(22):2115–2125. doi: 10.1056/NEJMoa1215245. [DOI] [PubMed] [Google Scholar]
- 6.Lacroix A, Ndiaye N, Tremblay J, Hamet P. Ectopic and abnormal hormone receptors in adrenal Cushing’s syndrome. Endocr Rev. 2001;22(1):75–110. doi: 10.1210/edrv.22.1.0420. [DOI] [PubMed] [Google Scholar]
- 7.Lacroix A. Heredity and cortisol regulation in bilateral macronodular adrenal hyperplasia. N Engl J Med. 2013;369(22):2147–2149. doi: 10.1056/NEJMe1312792. [DOI] [PubMed] [Google Scholar]
- 8.Hamet P, Larochelle P, Franks DJ, Cartier P, Bolte E. Cushing syndrome with food-dependent periodic hormonogenesis. Clin Invest Med. 1987;10(6):530–533. [PubMed] [Google Scholar]
- 9.Lacroix A, et al. Gastric inhibitory polypeptide-dependent cortisol hypersecretion — a new cause of Cushing’s syndrome. N Engl J Med. 1992;327(14):974–980. doi: 10.1056/NEJM199210013271402. [DOI] [PubMed] [Google Scholar]
- 10.Reznik Y, et al. Food-dependent Cushing’s syndrome mediated by aberrant adrenal sensitivity to gastric inhibitory polypeptide. N Engl J Med. 1992;327(14):981–986. doi: 10.1056/NEJM199210013271403. [DOI] [PubMed] [Google Scholar]
- 11.El Ghorayeb N, Bourdeau I, Lacroix A. Multiple aberrant hormone receptors in Cushing’s syndrome. Eur J Endocrinol. 2015;173(4):M45–M60. doi: 10.1530/EJE-15-0200. [DOI] [PubMed] [Google Scholar]
- 12.Boylan MO, Jepeal LI, Wolfe MM. Sp1/Sp3 binding is associated with cell-specific expression of the glucose-dependent insulinotropic polypeptide receptor gene. Am J Physiol Endocrinol Metab. 2006;290(6):E1287–E1295. doi: 10.1152/ajpendo.00535.2005. [DOI] [PubMed] [Google Scholar]
- 13.Almeida MQ, et al. Integrated genomic analysis of nodular tissue in macronodular adrenocortical hyperplasia: progression of tumorigenesis in a disorder associated with multiple benign lesions. J Clin Endocrinol Metab. 2011;96(4):E728–E738. doi: 10.1210/jc.2010-2420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ghezraoui H, et al. Chromosomal translocations in human cells are generated by canonical nonhomologous end-joining. Mol Cell. 2014;55(6):829–842. doi: 10.1016/j.molcel.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.ENCODE Project Consortium. An integrated encyclopedia of DNA elements in the human genome. Nature. 2012;489(7414):57–74. doi: 10.1038/nature11247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Trivellin G, et al. Gigantism and acromegaly due to Xq26 microduplications and GPR101 mutation. N Engl J Med. 2014;371(25):2363–2374. doi: 10.1056/NEJMoa1408028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grieco M, et al. PTC is a novel rearranged form of the ret proto-oncogene and is frequently detected in vivo in human thyroid papillary carcinomas. Cell. 1990;60(4):557–563. doi: 10.1016/0092-8674(90)90659-3. [DOI] [PubMed] [Google Scholar]
- 18.Lifton RP, et al. A chimaeric 11 beta-hydroxylase/aldosterone synthase gene causes glucocorticoid-remediable aldosteronism and human hypertension. Nature. 1992;355(6357):262–265. doi: 10.1038/355262a0. [DOI] [PubMed] [Google Scholar]
- 19.Motokura T, et al. A novel cyclin encoded by a bcl1-linked candidate oncogene. Nature. 1991;350(6318):512–515. doi: 10.1038/350512a0. [DOI] [PubMed] [Google Scholar]
- 20.Malovannaya A, et al. Analysis of the human endogenous coregulator complexome. Cell. 2011;145(5):787–799. doi: 10.1016/j.cell.2011.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gong F, et al. Screen identifies bromodomain protein ZMYND8 in chromatin recognition of transcription-associated DNA damage that promotes homologous recombination. Genes Dev. 2015;29(2):197–211. doi: 10.1101/gad.252189.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Swords FM, et al. The aberrant expression of the gastric inhibitory polypeptide (GIP) receptor in adrenal hyperplasia: does chronic adrenocorticotropin exposure stimulate up-regulation of GIP receptors in Cushing’s disease? J Clin Endocrinol Metab. 2005;90(5):3009–3016. doi: 10.1210/jc.2004-0946. [DOI] [PubMed] [Google Scholar]
- 23.Teo AE, et al. Pregnancy, primary aldosteronism, and adrenal CTNNB1 mutations. N Engl J Med. 2015;373(15):1429–1436. doi: 10.1056/NEJMoa1504869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.N’Diaye N, Hamet P, Tremblay J, Boutin JM, Gaboury L, Lacroix A. Asynchronous development of bilateral nodular adrenal hyperplasia in gastric inhibitory polypeptide-dependent cushing’s syndrome. J Clin Endocrinol Metab. 1999;84(8):2616–2622. doi: 10.1210/jcem.84.8.5930. [DOI] [PubMed] [Google Scholar]
- 25.Lampron A, Bourdeau I, Hamet P, Tremblay J, Lacroix A. Whole genome expression profiling of glucose-dependent insulinotropic peptide (GIP)- and adrenocorticotropin-dependent adrenal hyperplasias reveals novel targets for the study of GIP-dependent Cushing’s syndrome. J Clin Endocrinol Metab. 2006;91(9):3611–3618. doi: 10.1210/jc.2006-0221. [DOI] [PubMed] [Google Scholar]
- 26.Bertherat J, et al. In vivo and in vitro screening for illegitimate receptors in adrenocorticotropin-independent macronodular adrenal hyperplasia causing Cushing’s syndrome: identification of two cases of gonadotropin/gastric inhibitory polypeptide-dependent hypercortisolism. J Clin Endocrinol Metab. 2005;90(3):1302–1310. doi: 10.1210/jc.2004-1256. [DOI] [PubMed] [Google Scholar]
- 27.Louiset E, et al. Expression of serotonin7 receptor and coupling of ectopic receptors to protein kinase A and ionic currents in adrenocorticotropin-independent macronodular adrenal hyperplasia causing Cushing’s syndrome. J Clin Endocrinol Metab. 2006;91(11):4578–4586. doi: 10.1210/jc.2006-0538. [DOI] [PubMed] [Google Scholar]
- 28.Berthon A, Drelon C, Val P. Pregnancy, primary aldosteronism, and somatic CTNNB1 mutations. N Engl J Med. 2016;374(15):1493–1494. doi: 10.1056/NEJMc1514508. [DOI] [PubMed] [Google Scholar]
- 29.Espiard S, et al. ARMC5 mutations in a large cohort of primary macronodular adrenal hyperplasia: clinical and functional consequences. J Clin Endocrinol Metab. 2015;100(6):E926–E935. doi: 10.1210/jc.2014-4204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mazzuco TL, Chabre O, Sturm N, Feige JJ, Thomas M. Ectopic expression of the gastric inhibitory polypeptide receptor gene is a sufficient genetic event to induce benign adrenocortical tumor in a xenotransplantation model. Endocrinology. 2006;147(2):782–790. doi: 10.1210/en.2005-0921. [DOI] [PubMed] [Google Scholar]
- 31.de Herder WW, et al. Food-dependent Cushing’s syndrome resulting from abundant expression of gastric inhibitory polypeptide receptors in adrenal adenoma cells. J Clin Endocrinol Metab. 1996;81(9):3168–3172. doi: 10.1210/jcem.81.9.8784063. [DOI] [PubMed] [Google Scholar]
- 32.N’Diaye N, Tremblay J, Hamet P, De Herder WW, Lacroix A. Adrenocortical overexpression of gastric inhibitory polypeptide receptor underlies food-dependent Cushing’s syndrome. J Clin Endocrinol Metab. 1998;83(8):2781–2785. doi: 10.1210/jcem.83.8.5038. [DOI] [PubMed] [Google Scholar]
- 33.Luton JP, Bertherat J, Kuhn JM, Bertagna X. [Aberrant expression of the GIP (gastric inhibitory polypeptide) receptor in an adrenal cortical adenoma responsible for a case of food-dependent Cushing’s syndrome] Bull Acad Natl Med. 1998;182(9):1839–1849. [PubMed] [Google Scholar]
- 34.Groussin L, et al. The ectopic expression of the gastric inhibitory polypeptide receptor is frequent in adrenocorticotropin-independent bilateral macronodular adrenal hyperplasia, but rare in unilateral tumors. J Clin Endocrinol Metab. 2002;87(5):1980–1985. doi: 10.1210/jcem.87.5.8458. [DOI] [PubMed] [Google Scholar]
- 35.Lampron A, et al. Regulation of aldosterone secretion by several aberrant receptors including for glucose-dependent insulinotropic peptide in a patient with an aldosteronoma. J Clin Endocrinol Metab. 2009;94(3):750–756. doi: 10.1210/jc.2008-1340. [DOI] [PubMed] [Google Scholar]
- 36.Preumont V, Mermejo LM, Damoiseaux P, Lacroix A, Maiter D. Transient efficacy of octreotide and pasireotide (SOM230) treatment in GIP-dependent Cushing’s syndrome. Horm Metab Res. 2011;43(4):287–291. doi: 10.1055/s-0030-1270523. [DOI] [PubMed] [Google Scholar]
- 37.Doppman JL, Chrousos GP, Papanicolaou DA, Stratakis CA, Alexander HR, Nieman LK. Adrenocorticotropin-independent macronodular adrenal hyperplasia: an uncommon cause of primary adrenal hypercortisolism. Radiology. 2000;216(3):797–802. doi: 10.1148/radiology.216.3.r00au40797. [DOI] [PubMed] [Google Scholar]
- 38.Lacroix A, Feelders RA, Stratakis CA, Nieman LK. Cushing’s syndrome. Lancet. 2015;386(9996):913–927. doi: 10.1016/S0140-6736(14)61375-1. [DOI] [PubMed] [Google Scholar]
- 39.Funder JW, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an Endocrine Society Clinical practice guideline. J Clin Endocrinol Metab. 2016;101(5):1889–1916. doi: 10.1210/jc.2015-4061. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.