Abstract
Arthroscopic shoulder surgery can be performed in both the beach chair and lateral decubitus positions. The beach chair position is a reliable, safe, and effective position to perform nearly all types of shoulder arthroscopic procedures. The advantages of the beach chair position include the ease of setup, limited brachial plexus stress, increased glenohumeral and subacromial visualization, anesthesia flexibility, and the ability to easily convert to an open procedure. This position is most commonly used for rotator cuff repair, subacromial decompression, and superior labrum anterior-to-posterior repair procedures. To perform arthroscopy surgery in the beach chair position successfully, meticulous care during patient positioning and setup must be taken. In this Technical Note, we describe the necessary steps to safely and efficiently prepare patients in the beach chair position for arthroscopic shoulder surgery.
For the vast majority of all shoulder arthroscopic procedures, patients can be positioned in either the beach chair (BC) or the lateral decubitus (LD) position. The literature is controversial with regard to which position is superior for a given procedure, and certainly, there are many advantages and disadvantages when comparing both positions.1, 2, 3 Regardless of position, proper setup and positioning are of utmost importance to optimize surgical success and patient safety.1 Ultimately, it is a combination of the surgeon's training and experience along with the specific intended procedure that will dictate which position the patient is placed in for a given procedure. The BC position was described in the early 1980s as an alternative patient position to address the issue of brachial plexus traction injuries experienced by patients in the LD position.1, 4
The BC position creates a favorable teaching environment for experienced surgeons to teach and guide surgeons in training. The upright orientation of the patient helps trainees easily identify internal and external anatomic landmarks.1, 5 Another advantage of the BC position is the ability to easily manipulate and rotate the arm in order to access different areas of the shoulder during surgery, as opposed to needing to work around the nuances of the LD traction/weight setup. Such manipulation may allow for greater visualization of the anterior shoulder structures including the subscapularis, the posterosuperior rotator cuff, the subacromial space, and the glenohumeral joint itself. These advantages enhance a surgeon's ability to perform rotator cuff repairs, work in the subacromial space, and perform superior labrum anterior-to-posterior stabilization.4, 5 Further, as Skyhar et al.4 noted in their study, the ease of converting an arthroscopic procedure to an open procedure in the BC position is noteworthy and efficiently accomplished. Further, the upright position of the BC position gives the surgical and anesthesia team the freedom to choose between regional and general anesthesia for the surgery and allows for an easy transition to the supine position should airway complications arise.1, 2 In the subsequent section, we describe our technique for BC patient positioning for shoulder arthroscopy. A summary of key steps is provided in Table 1, and a summary of the technique is provided in Video 1.
Table 1.
Keys Steps to Beach Chair Patient Positioning
| Step | Notes |
|---|---|
| Position the patient properly in supine position | Position the patient to ensure the buttocks will be pressed against the back of the bed |
| Raise the back of the bed to 60° | |
| Shift the patient so the medial scapula is on the edge of the bed | Several folded surgical towels can be placed medially to the scapula to improve position |
| Confirm the buttocks' position against the back of the bed | No gap between the patient and the bed |
| Place a large pad or several pillows underneath the patient's legs | |
| Secure the nonoperative arm to the patient's abdomen or on an arm board | |
| Secure the head and airway accessibility | A variety of methods can be used, but maintenance of a neutral position is vital |
| Position the arm in the proper position using an arm-positioner | Be aware when applying traction to avoid neurologic damage |
| Secure the patient's position with a safety-belt and tape | |
| Rotate the bed 60° to 90° | To provide the surgical team the appropriate amount of space |
Technique
Shoulder arthroscopy in the BC position is performed in the supine position, and can be conducted under general or regional anesthesia. When performing arthroscopic surgery in the BC position, we prefer the use of regional anesthesia with an interscalene block with sedation or with general anesthesia. If general anesthesia is used, the eyes can be protected with a padded face-mask; tape placed over the eyes by the anesthesia team will also protect against corneal abrasions. Sequential compression devices are placed on both lower extremities for venous thromboembolism prophylaxis (Fig 1). After induction of anesthesia, and prior to positioning, an examination under anesthesia (EUA) should be carried out on the operative shoulder, assessing range of motion and stability in all directions.
Fig 1.
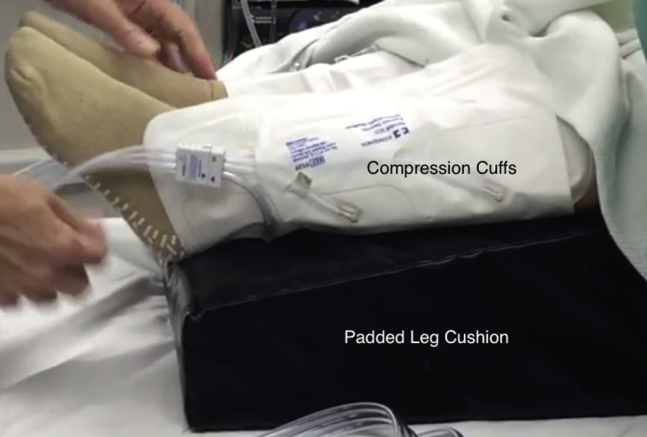
Intraoperative photograph demonstrating the use of sequential compression devices for venous thromboembolism prophylaxis during shoulder arthroscopy in the beach chair position.
Patient Positioning
After the patient has been transferred to the operating table and following the EUA, a team-based approach is used to ensure the patient is in the appropriate position prior to raising the back of the table up to the BC position. First, one should ensure that the patient is high enough on the table such that when the back of the table is raised, the patient's buttocks will be at the break of the bed; this will ensure the lumbar spine is in a favorable position during the procedure (Fig 2). At this point, the back of the bed is lifted to approximately 60° and the patient is shifted so the medial border of their scapula is just at the edge of the bed. Several folded surgical towels can be placed medial to the patient's scapula to improve the shoulder position. The patient's buttocks should be confirmed as being firmly against the operating table with no gap between the patient and the operating table. A large pad or several pillows can be placed underneath the patient's legs. The nonoperative arm can be tucked and secured to the patient's abdomen or placed on an arm board. Care should be taken to confirm that all bony prominences, particularly on the nonsurgical arm, are well padded.
Fig 2.

Intraoperative photograph demonstrating the patient's hips positioned near the break of the bed in order to prevent the patient from slipping down the bed as the head of the bed is raised into the beach chair position.
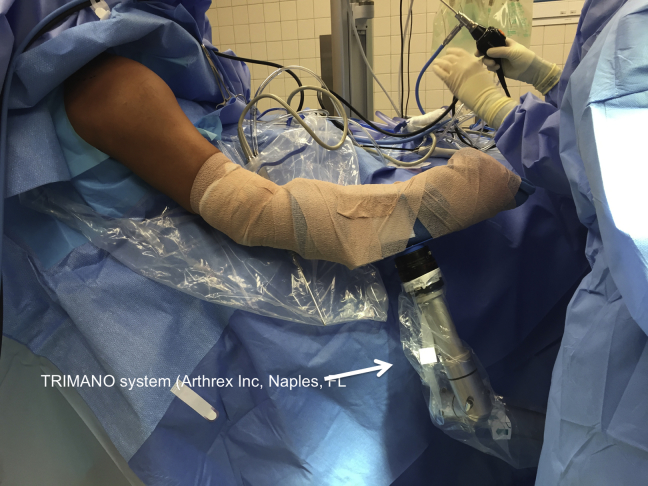
Next, the head is secured. There are several ways in which the head and neck can be secured in the BC position. Some surgeons use a specialized headrest with foam mask placed over the patient to secure the head and neck in a neutral position (Fig 3). Others use a foam pad (often ripping the bottom ipsilateral corner off of the pad to allow for more working room) under the patient's head with a surgical towel and tape used to secure the head and neck in a neutral position (Fig 4). The surgical arm is wrapped in a sterile stockinette; and self-adherent wrap (such as Coban; 3M Health Care, St. Paul, MN) can be secured in a commercial arm-holding device (such as the Trimano [Arthrex, Naples FL; Fig 5], or Spider [Smith & Nephew, Andover, MA; Fig 6]), as show in Video 1, or alternatively, can rest freely on a padded Mayo stand. If an arm-positioning device is used, care must be taken when applying traction to the arm in order to avoid neurologic damage.1, 5, 6 Regardless of the technique used, it is critical to use a team-based approach, with open communication with the anesthesia staff, while securing the patient's head and neck in a neutral position. This will ensure that the airway remains open and easily accessible, and that the ears and eyes are carefully protected. Once the patient is properly positioned, a safety-belt and tape are applied to secure the patient to the table (Fig 7). In addition, we secure the patient with thick tape both at the level of the thighs and the torso in an effort to maintain the body in a steady position for the duration of the surgical procedure. The operating table is then rotated 60° to 90° to give the surgical team a dedicated workspace, while maintaining appropriate access to the patient for the anesthesia team.
Fig 3.

Operative arm (right arm) of a patient placed in the beach chair position demonstrating securement of the head and neck with a foam mask (Spider Limb Positioner; Smith & Nephew).
Fig 4.
Intraoperative photograph demonstrating an alternative approach to securing the head and neck with a foam headrest and tape/towel construct.
Fig 5.
Intraoperative photograph demonstrating operative arm (right arm) of a patient placed in the beach chair position using the Trimano commercial arm holder (Arthrex).
Fig 6.
Intraoperative photograph demonstrating operative arm (right arm) of a patient placed in the beach chair position using the Spider Limb Positioner (Smith & Nephew).
Fig 7.
Intraoperative photograph demonstrating the use of a safety strap across a patient placed in the beach chair position for shoulder arthroscopy.
Portal Placement
After patient positioning is determined to be adequate, the patient is draped and prepped in standard fashion. Before proceeding further, the surgical team ensures that the proper perioperative arthroscopy fluid is readily available and in stock. The authors typically use an arthroscopy pump system with the pressure initially set to 40 mmHg, with normal saline with 1:1000 epinephrine (typically 1 mL for a 5 L bag of fluid). Next, anticipated portal sites and drawn out using bony landmarks, including the acromion, clavicle, acromio-clavicular joint (ACJ) and coracoid process (Fig 8). In the BC position, the standard posterior portal is typically placed 2 cm inferior and 1 cm medial to the posterolateral corner of the acromion. A standard anterior rotator-interval portal is often created next using needle localization with a spinal needle placed just lateral to the coracoid process under direct visualization. Additional portals may be created to effectively and efficiently complete the surgical procedure.7
Fig 8.
Operative arm (right arm) of a patient placed in the beach chair position (Spider Limb Positioner; Smith & Nephew) with anticipated portal sites marked using bony landmarks, including the acromion, clavicle, acromioclavicular joint, and coracoid process. (A, anterior; L, lateral; P, posterior.)
Discussion
In this Technical Note, we describe a safe, reliable, and reproducible technique for patient positioning in the BC position for shoulder arthroscopy. Shoulder arthroscopy can be performed in either the LD or BC position, with advantages and disadvantages to each position.5 Shoulder arthroscopy in the BC position has several advantages over performing similar procedures in the LD position. As mentioned previously, arthroscopy in the BC position provides an excellent teaching environment for surgical trainees, as the upright position of the patient provides an easily recognizable and familiar view of the glenohumeral joint.1, 2, 4, 5 As opposed to the LD position, this easily conceptualized patient position allows surgical trainees to focus on surgical technique and less on orientating and identifying anatomic landmarks. The ability to easily convert the BC position to the supine position has also been described as an advantage, should any airway complications arise during the procedure.1, 2 The BC position was initially created to reduce the number of brachial plexus injuries caused by traction in the LD position, with reported injuring rates ranging from 10% to 30%.2, 4 Rodeo et al. conducted a retrospective study analyzing the rates of neurologic complications following arthroscopy of various joints. Within the shoulder joint, reported rates were very low, between 0 and 30%; the authors also report no incidences of nerve palsy at their institution when placing the patients in the BC position.6 Advocates of the BC position argue that BC allows for superior visualization of the anterior aspect of the glenohumeral joint, rotator cuff, and subacromial space, all of which facilitate easier rotator cuff repair, subacromial decompression, and capsular release.4 The BC position also affords the surgical and anesthesia teams the flexibility of choosing either general or regional anesthesia. If necessary, a regionally anesthetized patient can be converted to general anesthesia very quickly given the ease of airway access and ease of converting from the BC to the supine position. The BC position gives a surgeon the flexibility to convert an arthroscopic procedure to an open procedure should the need arise,2, 3 which may be more challenging in the LD position.4, 5
When performing shoulder arthroscopic surgery, there are several risks and complications associated with the BC position that must be discussed. Although there is a reduced risk of traction-based neurologic injury in patients who are placed in the BC position compared with the LD position,2 patients may be at greater risk of cerebral hypoperfusion when in the BC position, though certainly, this complication is rare. Although the exact etiology of cerebral hypoperfusion is likely multifactorial, the effects of permissive hypotension, a strategy often employed to minimize blood loss and improve visualization, are compounded by the position of the patient's head relative to the body.8, 9, 10 Liguori et al.11 found that the administration of metoprolol is beneficial to the patient by reducing the number of hypotensive and bradycardic events. In order to address the issues of hypotension, the blood pressure cuff should be placed at the level of the heart and not on the calf; if this is not possible, it is critical for the anesthesiologist to interpret calf pressures relative to heart-level pressure in order to avoid iatrogenic cerebral hypoperfusion. Further, to maximize intraoperative visualization while also maintaining an acceptable blood pressure, the patient's perioperative blood pressure should be approximately 80% of the resting pressure.8 A summary of advantages and disadvantages of the BC position is provided in Table 2 and a summary of pearls and pitfalls is provided in Table 3.
Table 2.
Advantages and Disadvantages of Beach Chair Patient Positioning for Shoulder Arthroscopy
| Advantages | Disadvantages |
|---|---|
| Favorable teaching environment with upright anatomic position | Increased risk for cerebral hypoperfusion and hypotension |
| Reduced neurovascular complications | Reduced visualization of the complete glenohumeral joint for instability and superior labrum anterior-to-posterior (SLAP) repairs |
| Easier conversion to an open procedure or general anesthesia (if complications arise) | Limited access to the posterior and posterior-inferior aspects of the joint |
| Increased access to the anterior, superior glenohumeral joint and subacromial space |
Table 3.
Pearls and Pitfalls Associated with Beach Chair Patient Positioning for Shoulder Arthroscopy
| Pearls | Pitfalls |
|---|---|
| • Slowly raise the head of bed during patient positioning to avoid iatrogenic hypotension | • Hypoglossal nerve injury |
| • Be aware of potential for cerebral hypotension | • Cervical plexus injury |
| ○ Consider using a beta-blocker (per anesthesia team) | • Vasovagal episode |
| ○ Consider location of blood pressure cuff placement | • Visual loss |
| • Position buttocks up against bed to avoid pressure injury | • Cerebral ischemia |
| • Avoid excessive ER to prevent brachial plexus strain | • Hypotension |
| • Avoid contralateral elbow flexion beyond 90° → ulnar nerve | • Vertebral artery hypoperfusion |
| • Be careful with head position | • Difficult access to inferior glenoid |
| ○ Know how the head-holder functions | • Difficult low-anterior portal placement |
| ○ Place head/neck in neutral to decrease risk of hypovascular incidents | |
| • Ensure proper padding at the knees → peroneal nerve irritation |
In summary, the technique, advantages, disadvantages, and risks of the BC position have been described in this Technical Note to help physicians position their patients in the most advantageous position for shoulder arthroscopy.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.T.H. reports other from Novartis, other from NuVasive, outside the submitted work. M.T.P. reports other from AAOS; personal fees, nonfinancial support, and other from Arthrex; personal fees, nonfinancial support, and other from SLACK Incorporated; other from American Orthopaedic Society for Sports Medicine; other from American Shoulder and Elbow Surgeons; other from Arthroscopy; other from Arthroscopy Association of North America; other from International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine; personal fees from Joint Restoration Foundation (AlloSource); other from Knee; other from Orthopedics; other from San Diego Shoulder Institute; other from Society of Military Orthopaedic Surgeons, outside the submitted work. A.A.R. reports other from American Orthopaedic Society for Sports Medicine; personal fees, nonfinancial support, and other from Arthrex; personal fees and nonfinancial support from DJO Surgical; other from Orthopedics; other from Orthopedics Today; personal fees and nonfinancial support from Ossur; other from SAGE; personal fees, nonfinancial support, and other from Saunders/Mosby-Elsevier; personal fees, nonfinancial support, and other from Slack; personal fees and nonfinancial support from Smith & Nephew, from Wolters Kluwer Health–Lippincott Williams & Wilkins, and other from American Shoulder and Elbow Surgeons, outside the submitted work. N.N.V. reports personal fees and nonfinancial support from Arthrex; personal fees, nonfinancial support, and other from Arthroscopy; personal fees and nonfinancial support from Arthrosurface; other from Cymedica, personal fees and nonfinancial support from DJ Orthopaedics, personal fees and other from Minivasive; other from Omeros; personal fees and nonfinancial support from Orthospace; personal fees, nonfinancial support, and other from Smith & Nephew; personal fees and nonfinancial support from Athletico; personal fees and nonfinancial support from ConMed Linvatec; personal fees and nonfinancial support from Miomed; personal fees and nonfinancial support from Mitek; personal fees and other from Vindico Medical-Orthopedics Hyperguide; other from Arthroscopy Association Learning Center Committee; other from Slack; other from American Orthopaedic Society for Sports Medicine, other from American Shoulder and Elbow Surgeons; other from Journal of Knee Surgery; and nonfinancial support from Ossur, outside the submitted work.
Supplementary Data
Technique for beach chair patient position setup of the right arm of a patient including examination under anesthesia, arm-holder device setup (Spider Limb Positioner; Smith & Nephew), and marking of anticipated portal placement with narration of all critical steps.
References
- 1.Li X., Eichinger J.K., Hartshorn T., Zhou H., Matzkin E.G., Warner J.P. A comparison of the lateral decubitus and beach-chair positions for shoulder surgery: Advantages and complications. J Am Acad Orthop Surg. 2015;23:18–28. doi: 10.5435/JAAOS-23-01-18. [DOI] [PubMed] [Google Scholar]
- 2.Peruto C.M., Ciccotti M.G., Cohen S.B. Shoulder arthroscopy positioning: Lateral decubitus versus beach chair. Arthroscopy. 2009;25:891–896. doi: 10.1016/j.arthro.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Gelber P.E., Reina F., Caceres E., Monllau J.C. A comparison of risk between the lateral decubitus and the beach-chair position when establishing an anteroinferior shoulder portal: A cadaveric study. Arthroscopy. 2007;23:522–528. doi: 10.1016/j.arthro.2006.12.034. [DOI] [PubMed] [Google Scholar]
- 4.Skyhar M.J., Altchek D.W., Warren R.F., Wickiewicz T.L., O'Brien S.J. Shoulder arthroscopy with the patient in the beach-chair position. Arthroscopy. 1988;4:256–259. doi: 10.1016/s0749-8063(88)80040-9. [DOI] [PubMed] [Google Scholar]
- 5.Provencher M.T., Mcintire E.S., Gaston T.M., Frank R.M., Solomon D.J. Avoiding complications in shoulder arthroscopy: Pearls for lateral decubitus and beach chair positioning. Tech Shoulder Elbow Surg. 2010;11:1–3. [Google Scholar]
- 6.Rodeo S.A., Forster R.A., Weiland A.J. Neurological complications due to arthroscopy. J Bone Joint Surg Am. 1993;75:917–926. doi: 10.2106/00004623-199306000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Chalmers P.N., Sherman S.L. Patient positioning, portal placement, normal arthroscopic anatomy, and diagnostic arthroscopy. In: Cole B.J., Sekiya J.K., editors. Surgical techniques of the shoulder, elbow, and knee in sports medicine. Elsevier-Saunders; Philadelphia, PA: 2008. pp. 3–12. [Google Scholar]
- 8.Papadonikolakis A., Wiesler E.R., Olympio M.A., Poehling G.G. Avoiding catastrophic complications of stroke and death related to shoulder surgery in the sitting position. Arthroscopy. 2008;24:481–482. doi: 10.1016/j.arthro.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 9.Murphy G.S., Szokol J.W., Marymont J.H. Cerebral oxygen desaturation events assessed by near-infrared spectroscopy during shoulder arthroscopy in the beach chair and lateral decubitus positions. Anesth Analg. 2010;111:496–505. doi: 10.1213/ANE.0b013e3181e33bd9. [DOI] [PubMed] [Google Scholar]
- 10.Salazar D., Hazel A., Tauchen A.J., Sears B.W., Marra G. Neurocognitive deficits and cerebral desaturation during shoulder arthroscopy with patient in beach-chair position: A review of the current literature. Am J Orthop (Belle Mead NJ) 2016;45:E63–E68. [PubMed] [Google Scholar]
- 11.Liguori G.A., Kahn R.L., Gordon J., Gordon M.A., Urban M.K. The use of metoprolol and glycopyrrolate to prevent hypotensive/bradycardic events during shoulder arthroscopy in the sitting position under interscalene block. Anesth Analg. 1998;87:1320–1325. doi: 10.1097/00000539-199812000-00020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technique for beach chair patient position setup of the right arm of a patient including examination under anesthesia, arm-holder device setup (Spider Limb Positioner; Smith & Nephew), and marking of anticipated portal placement with narration of all critical steps.