Abstract
Background:
Screening for undiagnosed atrial fibrillation may lead to treatment with oral anticoagulation therapy, which can decrease the risk of ischemic stroke. The objective of this study was to conduct an economic evaluation of the Program for the Identification of 'Actionable' Atrial Fibrillation in the Pharmacy Setting (PIAAF-Pharmacy), which screened 1145 participants aged 65 years or more at 30 community pharmacies in Ontario and Alberta between October 2014 and April 2015.
Methods:
We used a 2-part decision model to evaluate the short- and long-term costs and quality-adjusted life-years (QALYs) of a pharmacy screening program for atrial fibrillation compared to no screening. Data from the PIAAF-Pharmacy study were used for the short-term model, and the relevant literature was used to extrapolate the benefits of the PIAAF-Pharmacy study in the long-term model. Costs and QALYs were calculated from a payer perspective over a lifetime horizon and were discounted at 1.5%/year.
Results:
Screening for atrial fibrillation in pharmacies was associated with higher costs ($26) and more QALYs (0.0035) compared to no screening, yielding an incremental cost per QALY gained of $7480. Univariate and probabilistic sensitivity analyses confirmed that screening for atrial fibrillation in a pharmacy setting was a cost-effective strategy.
Interpretation:
Our results support screening for atrial fibrillation in Canadian pharmacies. Given this finding, efforts should be made by provincial governments and pharmacies to implement such programs in Canada. The addition of atrial fibrillation screening alongside screening and management of other cardiovascular conditions may help to reduce the burden of stroke.
Atrial fibrillation is the most common abnormal rhythm disorder1 and the leading cause of stroke.2 Although stroke related to atrial fibrillation is preventable with oral anticoagulation therapy,3,4 the disorder is often unrecognized or is known but suboptimally treated (hereafter referred to as "actionable" atrial fibrillation).5 There are sparse data to suggest that atrial fibrillation screening strategies are cost-effective.6,7 In the Program for the Identification of 'Actionable' Atrial Fibrillation in the Pharmacy Setting (PIAAF-Pharmacy), which involved a pharmacist, a coordinator and volunteers in each pharmacy, people aged 65 years or more attending pharmacies in Alberta and Ontario were screened for atrial fibrillation with a hand-held single-lead electrocardiogram (ECG) device (HeartCheck, CardioComm Solutions).8 The study design and clinical results were recently published.8 Actionable atrial fibrillation in the PIAAF-Pharmacy study was defined as previously unrecognized atrial fibrillation or known atrial fibrillation that was not being treated with oral anticoagulant therapy. The disorder was newly diagnosed in 2.4% of the 1145 study participants. The PIAAF-Pharmacy was modelled after the Cardiovascular Health Awareness Program.9,10 The current analysis presents the economic evaluation of the PIAAF-Pharmacy study to better inform decision-makers about the value of screening for atrial fibrillation in Canadian pharmacies.
Methods
We used a decision analytical model to estimate the lifetime costs and effects of the PIAAF-Pharmacy program compared with no screening. The model comprised 2 parts. The first part of the model captured the short-term costs (i.e., cost of screening) and outcomes (e.g., new cases of atrial fibrillation detected) of the screening program itself based on data from the PIAAF-Pharmacy study.8 The second part of the model captured the long-term costs and benefits associated with stroke prevention resulting from the diagnosis of previously unrecognized atrial fibrillation based on relevant literature. In the absence of dominance (e.g., 1 strategy is more effective and less costly than the other), we calculated an incremental cost per quality-adjusted life-years (QALYs) gained to compare the 2 strategies (in-pharmacy atrial fibrillation screening v. no screening). We used a lifetime horizon in the analysis, with costs and outcomes occurring in the future discounted at an annual rate of 1.5%.11 The analysis was taken from a third-party public payer perspective. We conducted univariate and probabilistic sensitivity analyses to deal with uncertainty in model inputs.
Model structure
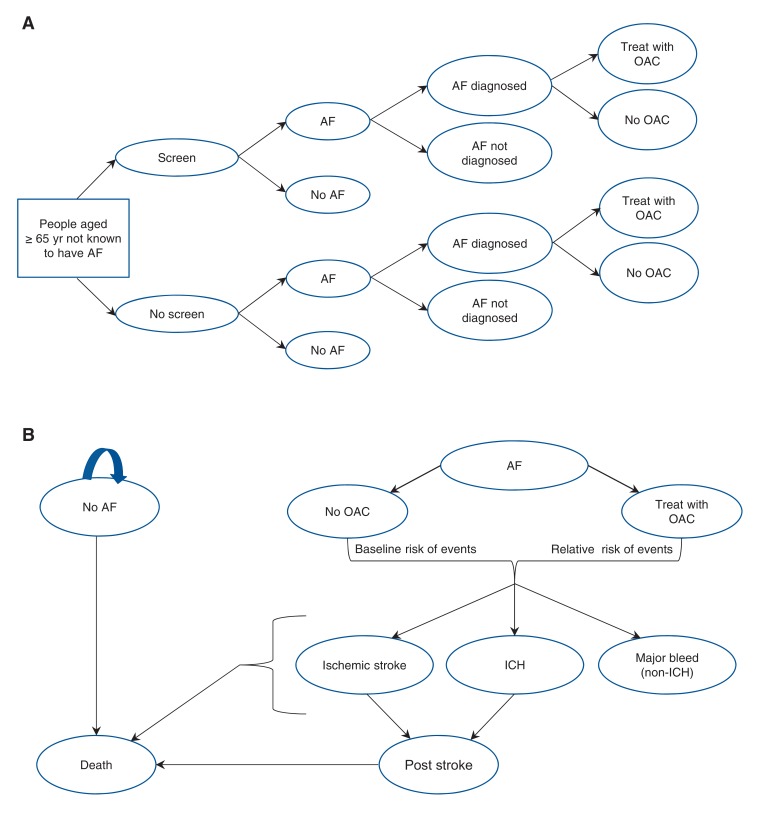
Figure 1, A, provides a graphical representation of the short-term decision model for atrial fibrillation screening, which is used as input for the long-term model. In the screening arm, atrial fibrillation is diagnosed based on positive findings of the single-lead ECG and its positive predictive value (PPV) to identify atrial fibrillation. A proportion of people with newly diagnosed atrial fibrillation would receive oral anticoagulant treatment for the prevention of stroke. For the no-screening arm, it is assumed that 3% of cases of undiagnosed atrial fibrillation would be detected every year without screening.12 Based on the short-term decision tree, people enter the long-term model (Figure 1, B) in 1 of 3 health states: 1) no atrial fibrillation, 2) atrial fibrillation being treated with oral anticoagulant therapy or 3) atrial fibrillation not being treated oral anticoagulant therapy. Those with atrial fibrillation are at risk for ischemic stroke, intracranial hemorrhage and nonintracranial major bleeding. Intracranial hemorrhage is further divided into hemorrhagic stroke and nonhemorrhagic stroke. People with atrial fibrillation who are receiving oral anticoagulant therapy are assumed to be at lower risk for ischemic stroke but at higher risk for intracranial hemorrhage and nonintracranial major bleeding compared to those not receiving oral anticoagulant therapy. Transitions between health states can occur every 3 months.
Figure 1.
Graphical representation of short-term (A) and long-term (B) atrial fibrillation (AF) screening model. People enter the long-term model in 1 of 3 health states: 1) no AF, 2) AF being treated with oral anticoagulant (OAC) therapy or 3) AF not being treated with OAC therapy. The curved blue arrow indicates that people with no AF are assumed to remain with no AF for the remainder of the model or until death. Note: ICH = intracranial hemorrhage.
Short-term model parameters
Based on the PIAAF-Pharmacy study results,8 we assumed that 2.4% of those in the screening group would have a positive result for atrial fibrillation for the first time. The PPV of the single-lead ECG used in that study, 65.4%, was based on unpublished data from a similar atrial fibrillation screening study conducted in physicians' offices (as opposed to pharmacies) in which all those with a positive result of single-lead ECG underwent 12-lead ECG and, if that gave a negative result, Holter monitor testing (Dr. Russell Quinn, Libin Cardiovascular Institute of Alberta, University of Calgary, Calgary, Alta.: personal communication, 2016). We applied the PPV to this percentage to calculate the proportion of screened people who have newly diagnosed atrial fibrillation (2.4% × 65.4% = 1.6%). We assumed that 71% of people with newly diagnosed atrial fibrillation would receive oral anticoagulant treatment for the prevention of stroke based on the fact that 5 of the 7 participants in the PIAAF-Pharmacy study in whom atrial fibrillation was newly diagnosed saw a physician within 6 weeks after screening and were prescribed oral anticoagulant therapy by the end of the 3-month study follow-up period. As in the economic evaluation of Aronsson and colleagues,6 we used a rate of discontinuation of oral anticoagulant therapy of 10% per year in the base-case analysis scenario according to the Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE) trial.13 We used cost data from the PIAAF-Pharmacy study to calculate the cost per screen by dividing the total cost of the screening sessions conducted in the study by the number of participants screened in the study. We estimated the total cost of the screening sessions by summing 3 cost categories: 1) training of personnel conducting the screening sessions, 2) in-pharmacy screening sessions, including transmission of results to family physicians, and 3) costs of single-lead ECG used in screening sessions and of confirmatory 12-lead ECG and Holter monitor testing.14
Long-term model assumptions
The key assumptions for the long-term model regarding stroke and bleeding risk, mortality, cost of events and utilities are presented in the following sections. A summary of the long-term model variables is also provided in Appendix 1 (available at www.cmajopen.ca/content/5/3/E653/suppl/DC1) along with other model inputs used in the short- and long-term models (e.g., cost and utility data).
Stroke and bleeding risk
We used the average CHA2DS2-VASc score15 for participants with newly diagnosed atrial fibrillation in the PIAAF-Pharmacy study, 3.3, in the model. The annual risk of stroke in the absence of oral anticoagulant therapy and the risk of intracranial hemorrhage and nonintracranial major bleeding for people with atrial fibrillation were based on findings from a Swedish cohort study involving 182 000 people in whom atrial fibrillation was diagnosed.16 We also used the average HAS-BLED score17 in that study, 2.18, for our model cohort because these scores were not captured in the PIAAF-Pharmacy study.
For people with atrial fibrillation who receive oral anticoagulant therapy, we applied the relative risk of ischemic stroke and major bleeding compared to those not receiving oral anticoagulant therapy separately for those treated with warfarin and for those treated with direct oral anticoagulant therapy. For people treated with warfarin, the relative risk of ischemic stroke and major bleeding was based on a meta-analysis by Lip and Edwards.18 For those who received direct oral anticoagulant therapy, we used data from a meta-analysis of ischemic stroke and major bleeding relative to warfarin.4 We estimated the relative risk of events associated with direct oral anticoagulant therapy compared to no treatment indirectly by multiplying the relative risk of events for direct oral anticoagulant therapy versus warfarin by the relative risk of events for warfarin compared to no treatment.
Mortality
For people without atrial fibrillation and for those with atrial fibrillation who do not experience an event (e.g., stroke), we applied age- and sex-specific mortality rates based on Canadian life tables.19,20 The 1-year mortality rate after ischemic stroke, 37.3%, was based on findings from McGrath and colleagues.21 The 1-year mortality rate following intracranial hemorrhage, 35.2%, was based on in-hospital mortality reported by Alonso and colleagues22 extrapolated to 1-year mortality following intracranial hemorrhage by applying the ratio of 30-day mortality to 1 year, as observed for ischemic stroke by McGrath and colleagues.21 We assumed mortality rates 1 year following stroke (ischemic or hemorrhagic) to be 2.3 times higher than for the general population based on data from Hardie and colleagues.23 Nonintracranial major bleeding was associated with a mortality rate of 7.4%.24
Cost of events
Based on Canadian registry data, we assumed that 52% of people receiving oral anticoagulants would receive warfarin and 48% would receive direct oral anticoagulant therapy.25 The cost of warfarin was based on a regimen of 5 mg per day. We also assigned monitoring costs to those receiving warfarin based on estimates used in a Canadian economic evaluation of atrial fibrillation treatments.26 Unit costs of orally administered anticoagulants were based on 2016 reimbursement prices from the Ontario Drug Benefit formulary.27 For people who had an ischemic stroke or an intracranial hemorrhage, we assigned separate costs for the first year and for subsequent years following the event based on Canadian data.28-31 All costs are expressed in 2016 Canadian dollars. When necessary, we used the health care component of the Canadian Consumer Price Index to adjust to 2016 Canadian dollars.32
Utilities
We assigned age- and sex-specific general population EQ-5D utility values to people (with or without atrial fibrillation) with no events.33 EQ-5D is a preference-based measure of health status that is widely used in clinical trials, observational studies and other health surveys. People with an ischemic stroke or intracranial hemorrhage (hemorrhagic or nonhemorrhagic stroke) were assigned a utility weight of 0.60 to reflect the decreased long-term quality of life after these events. We estimated this utility weight by combining the average utility for stroke according to the score on the modified Rankin Scale (a commonly used scale for measuring the degree of disability or dependence in activities of daily living of people who have had a stroke) (mRS 0-2, mRS 3-5)34 with the proportion of people in these modified Rankin Scale categories, as derived from data from the Atrial Fibrillation Clopidogrel Trial with Irbesartan for Prevention of Vascular Events (ACTIVE A) trial.35 We multiplied the stroke utility weight by the age- and sex-specific population utility value for the cohort of patients who have a stroke.
Analysis of uncertainty
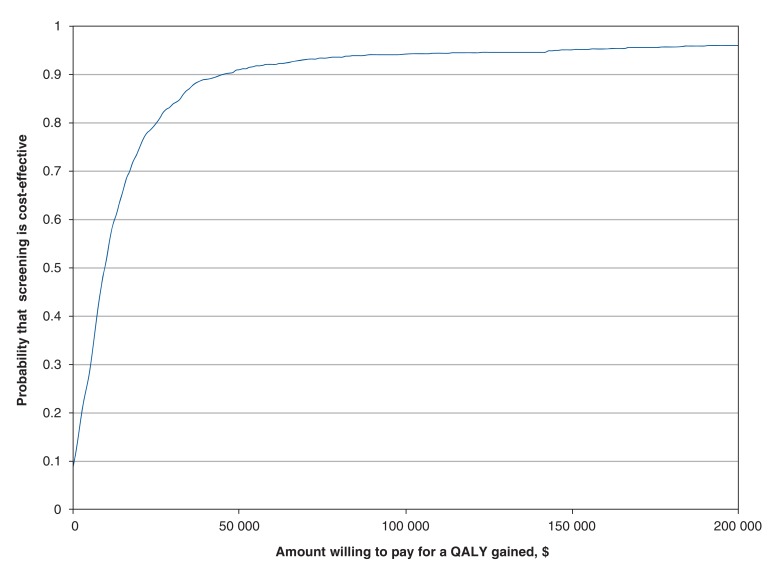
We first evaluated the uncertainty around the base-case cost-effectiveness results using probabilistic sensitivity analyses,36 in which we simulated the model results 1000 times, with values from model input variables being drawn from distributions specific to each model parameter (Appendix 1) by means of Monte Carlo techniques. We expressed parameter uncertainty around the base-case results using a cost-effectiveness acceptability curve, which shows the probability that atrial fibrillation screening is cost-effective across different willingness-to-pay thresholds.
In addition, we conducted deterministic sensitivity analyses in which we evaluated cost-effectiveness results while changing the value of a single model parameter at a time (cost per atrial fibrillation screen, proportion of people with atrial fibrillation receiving oral anticoagulant therapy, PPV, proportion of cases of undiagnosed atrial fibrillation that are diagnosed annually, time horizon, costs associated with stroke, proportion of orally administered anticoagulants that are direct and annual rate of discontinuation of oral anticoagulant therapy).
Ethics approval
The PIAAF-Pharmacy study was approved by the Human Research Ethics Board at the University of Alberta and the Hamilton Integrated Research Ethics Board.
Results
With a cost per person screened of $66 (Appendix 2, available at www.cmajopen.ca/content/5/3/E653/suppl/DC1), the model estimated that, compared to no screening, the PIAAF-Pharmacy screening intervention would result in higher expected costs ($26), more life-years (0.0032) and more QALYs (0.0035) over a lifelong time horizon, yielding an incremental cost per QALY gained of $7480 (Table 1). The increased per-person costs associated with the screening strategy ($66) and oral anticoagulant management ($29) are partially offset by the decreased costs associated with ischemic stroke (-$90) (Table 2).
Table 1: Base-case cost-effectiveness results.
| Intervention | Cost, $ | No. of life-years | No. of QALYs | Incremental $/life-year gained | Incremental $/QALY gained |
|---|---|---|---|---|---|
| PIAAF-Pharmacy screening | 443.99 | 9.027 | 6.880 | ||
| No screening | 417.93 | 9.023 | 6.876 | ||
| Incremental | 26.06 | 0.0032 | 0.0035 | 8213 | 7480 |
Note: PIAAF-Pharmacy = Program for the Identification of 'Actionable' Atrial Fibrillation in the Pharmacy Setting, QALY = quality-adjusted life-year.
Table 2: Expected costs by category.
| Intervention | Category; cost, $ | |||||
|---|---|---|---|---|---|---|
| Intervention | Oral anticoagulant therapy | Ischemic stroke | Intracranial hemorrhage | Major bleeding | Total | |
| PIAAF-Pharmacy screening | 66 | 35 | 269 | 55 | 20 | 443.98 |
| No screening | 0 | 5 | 358 | 41 | 13 | 417.93 |
| Incremental | 66 | 29 | -90 | 13 | 7 | 26.06 |
Note: PIAAF-Pharmacy = Program for the Identification of 'Actionable' Atrial Fibrillation in the Pharmacy Setting.
Probabilistic sensitivity analyses indicated that the probability that atrial fibrillation screening is cost-effective is 91% and 94% if the willingness to pay for a QALY gained is $50 000 and $100 000, respectively (Figure 2). The atrial fibrillation screening strategy is dominant or costs less than $50 000 per QALY in all deterministic sensitivity analyses except where 1) the proportion of people with confirmed atrial fibrillation who receive oral anticoagulant therapy is 20% or less (compared to 71% in the base-case analysis), 2) the PPV of single-lead ECG is 0.20 or lower (compared to 0.654 in the base-case analysis) or 3) the annual proportion of people with atrial fibrillation in the no-screening arm in whom the disorder is diagnosed symptomatically is 50% or higher (compared to 3% in the base-case analysis) (Table 3).
Figure 2.
Cost-effectiveness acceptability curve.
Table 3: One-way sensitivity analyses, PIAAF-Pharmacy screening versus no screening (base case: incremental cost per QALY gained = $1175).
| Variable | Incremental cost, $ | Incremental no. of QALYs | Incremental cost/QALY gained, $ |
|---|---|---|---|
| Cost of screening, $ (base case = $65) | |||
| 100 | 60 | 0.0035 | 17 195 |
| 90 | 50 | 0.0035 | 14 325 |
| 80 | 40 | 0.0035 | 11 455 |
| 70 | 30 | 0.0035 | 8585 |
| 60 | 20 | 0.0035 | 5715 |
| 50 | 10 | 0.0035 | 2845 |
| 40 | -0 | 0.0035 | Dominates |
| 30 | -10 | 0.0035 | Dominates |
| % of people with newly diagnosed atrial fibrillation who receive oral anticoagulant therapy (base case = 0.71) | |||
| 1.0 | 10 | 0.0049 | 2056 |
| 0.9 | 16 | 0.0044 | 3562 |
| 0.8 | 21 | 0.0039 | 5446 |
| 0.7 | 27 | 0.0034 | 7867 |
| 0.6 | 32 | 0.0029 | 11 096 |
| 0.5 | 38 | 0.0024 | 15 616 |
| 0.4 | 44 | 0.0020 | 22 397 |
| 0.3 | 49 | 0.0015 | 33 697 |
| 0.2 | 55 | 0.0010 | 56 298 |
| 0.1 | 61 | 0.0005 | 124 101 |
| Positive predictive value of single-lead electrocardiography (base case = 0.654) | |||
| 1.0 | 5 | 0.0053 | 911 |
| 0.9 | 11 | 0.0048 | 2291 |
| 0.8 | 17 | 0.0043 | 4015 |
| 0.7 | 23 | 0.0037 | 6232 |
| 0.6 | 29 | 0.0032 | 9189 |
| 0.5 | 36 | 0.0027 | 13 327 |
| 0.4 | 42 | 0.0021 | 19 535 |
| 0.3 | 48 | 0.0016 | 29 882 |
| 0.2 | 54 | 0.0011 | 50 575 |
| 0.1 | 60 | 0.0005 | 112 656 |
| % of people with undiagnosed atrial fibrillation in whom the disorder is diagnosed each year (base case = 0.03) | |||
| 0 | 20 | 0.0040 | 4951 |
| 0.05 | 30 | 0.0032 | 9215 |
| 0.1 | 36 | 0.0027 | 13 724 |
| 0.2 | 45 | 0.0019 | 23 499 |
| 0.3 | 50 | 0.0015 | 34 355 |
| 0.4 | 53 | 0.0011 | 46 475 |
| 0.5 | 56 | 0.0009 | 60 186 |
| Time horizon, yr (base case = lifetime) | |||
| 5 | 36 | 0.0010 | 37 226 |
| 10 | 25 | 0.0023 | 10 657 |
| 15 | 25 | 0.0031 | 7800 |
| 20 | 26 | 0.0034 | 7490 |
| 25 | 26 | 0.0035 | 7480 |
| Annual rate of discontinuation of oral anticoagulant therapy (base case = 10%) | |||
| 0 | 1 | 0.005 | 232 |
| 0.1 | 26 | 0.003 | 7480 |
| 0.2 | 38 | 0.002 | 15 480 |
| 0.3 | 45 | 0.002 | 24 333 |
| 0.4 | 50 | 0.001 | 34 208 |
| 0.5 | 53 | 0.001 | 45 382 |
| Alternative stroke costs | 46 | 0.003 | 13 277 |
| Warfarin represents 100% of orally administered anticoagulants* | 17 | 0.003 | 5985 |
| Direct oral anticoagulant therapy represents 100% of orally administered anticoagulants† | 36 | 0.004 | 8611 |
Note: PIAAF-Pharmacy = Program for the Identification of 'Actionable' Atrial Fibrillation in the Pharmacy Setting, QALY = quality-adjusted life-year.
*Base case: 52%.
†Base case: 48%.
Interpretation
The main findings of this economic evaluation of the PIAAF-Pharmacy study indicate that screening people aged 65 years or more for atrial fibrillation in Canadian pharmacies is highly cost-effective compared to no screening, yielding an incremental cost/QALY gained of $7480. The upfront costs associated with screening are partially offset by reductions in costs related to ischemic stroke owing to the initiation of oral anticoagulant treatment after atrial fibrillation is diagnosed. Except in unlikely situations (e.g., 20% of people with newly diagnosed atrial fibrillation would be prescribed oral anticoagulant therapy), the screening strategy was the dominant or a cost-effective strategy in all sensitivity analyses, which improves our confidence in the results. These results can be explained by the high costs associated with ischemic stroke and the associated value in preventing stroke comparing to the cost of screening and managing newly diagnosed cases of atrial fibrillation.
Our findings are fairly consistent with those of a cost-effectiveness analysis of an Australian in-pharmacy atrial fibrillation screening program among people aged 65 years or more, which yielded an incremental cost per QALY gained of A$5988 (Can$592837).7 In Sweden, the long-term cost-effectiveness of a nonpharmacy mass atrial fibrillation screening program was estimated to be €4313/QALY gained (Can$634137),6 and a similar study conducted in the Netherlands showed screening in primary care to be the dominant strategy.12
Limitations
In this economic evaluation, cost-effectiveness results were driven by predictions of ischemic stroke and other events related to atrial fibrillation or oral anticoagulant treatment that were not observed but were predicted based on short-term screening results. For example, in the absence of Canadian data, we used Swedish registry data16 for the estimates of stroke and major bleeding, although the Swedish study focused on atrial fibrillation diagnosed in the hospital as opposed to our community-based cohort. More patients in the Swedish cohort than in our cohort reported a history of stroke, valvular disease or heart failure. On the other hand, the proportions of people with diabetes and hypertension were higher in our cohort. These differences (e.g., the Swedish cohort may have been sicker) should not have affected our results, as we applied the risk of stroke and intracranial hemorrhage specific to the average CHADS2 score observed in our study. However, we had to rely on the Swedish registry data for the risk of major bleeding, because HAS-BLED scores were not collected in our study. In addition, the PIAAF-Pharmacy screening program is less likely to identify cases of intermittent atrial fibrillation than persistent or permanent atrial fibrillation. To deal with the uncertainty associated with key assumptions (e.g., cost per screen, proportion of people with atrial fibrillation receiving oral anticoagulant therapy, PPV) and associated parameter values, we conducted sensitivity analyses, which indicated that the results were robust except for extreme and unlikely situations. Our economic evaluation focused only on atrial fibrillation, and we did not integrate additional benefits associated with the PIAAF-Pharmacy study, such as the detection of other modifiable stroke risk factors (e.g., high blood pressure or risk of diabetes), which have already been shown to be clinically and economically advantageous.9,10 Inclusion of those additional factors would result in additional benefits associated with the program and would most likely result in overall cost-savings. As per the study design, the intervention was conducted by study coordinators and volunteers during scheduled screening sessions. As a result, some of their time in the pharmacy was spent waiting for eligible participants. It is reasonable to consider that an atrial fibrillation screening program could be better integrated into pharmacy workflows in collaboration with other pharmacy programs such as vaccinations, which would reduce waiting time and therefore the cost per person screened. Nonetheless, pharmacists will need to show adequate training in atrial fibrillation screening and sufficient resources and remuneration to perform this new service. Collaboration with physicians will also be key to ensure proper follow-up.
Conclusion
The results of this study have several policy implications. The PIAAF-Pharmacy study indicated that screening for atrial fibrillation and other modifiable risk factors in the pharmacy setting is feasible and is the dominant or cost-effective strategy compared to no screening, even at a cost of $66 per screen. Given this, efforts should be made by provincial governments and pharmacies to implement such programs in Canada. Adding atrial fibrillation screening in pharmacies should be considered along with other evidence-informed screening for cardiovascular disorders to identify those at high risk. Future research should focus on generating Canadian risk equations for stroke and major bleeding events.
Supplemental information
For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/5/3/E653/suppl/DC1
Supplementary Material
Acknowledgements
The authors acknowledge the pharmacists and managers from Rexall Pharmacy Group for their involvement in facilitating the pharmacy screening sessions.
Footnotes
Funding: The Program for the Identification of 'Actionable' Atrial Fibrillation in the Pharmacy Setting study was supported by the Canadian Stroke Prevention Intervention Network, Boehringer Ingelheim and in-kind support from CardioComm.
References
- 1.Miyasaka Y, Barnes ME, Gersh BJ, et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006;114:119–25. doi: 10.1161/CIRCULATIONAHA.105.595140. [DOI] [PubMed] [Google Scholar]
- 2.Marini C, De Santis F, Sacco S, et al. Contribution of atrial fibrillation to incidence and outcome of ischemic stroke: results from a population-based study. Stroke. 2005;36:1115–9. doi: 10.1161/01.STR.0000166053.83476.4a. [DOI] [PubMed] [Google Scholar]
- 3.Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007;146:857–67. doi: 10.7326/0003-4819-146-12-200706190-00007. [DOI] [PubMed] [Google Scholar]
- 4.Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383:955–62. doi: 10.1016/S0140-6736(13)62343-0. [DOI] [PubMed] [Google Scholar]
- 5.Gladstone DJ, Bui E, Fang J, et al. Potentially preventable strokes in high-risk patients with atrial fibrillation who are not adequately anticoagulated. Stroke. 2009;40:235–40. doi: 10.1161/STROKEAHA.108.516344. [DOI] [PubMed] [Google Scholar]
- 6.Aronsson M, Svennberg E, Rosenqvist M, et al. Cost-effectiveness of mass screening for untreated atrial fibrillation using intermittent ECG recording. Europace. 2015;17:1023–9. doi: 10.1093/europace/euv083. [DOI] [PubMed] [Google Scholar]
- 7.Lowres N, Neubeck L, Salkeld G, et al. Feasibility and cost-effectiveness of stroke prevention through community screening for atrial fibrillation using iPhone ECG in pharmacies. The SEARCH-AF study. Thromb Haemost. 2014;111:1167–76. doi: 10.1160/TH14-03-0231. [DOI] [PubMed] [Google Scholar]
- 8.Sandhu RK, Dolovich L, Deif B, et al. High prevalence of modifiable stroke risk factors identified in a pharmacy-based screening program. Open Heart. 2016;3:e000515. doi: 10.1136/openhrt-2016-000515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goeree R, von Keyserlingk C, Burke N, et al. Economic appraisal of a community-wide cardiovascular health awareness program. Value Health. 2013;16:39–45. doi: 10.1016/j.jval.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 10.Kaczorowski J, Chambers LW, Dolovich L, et al. Improving cardiovascular health at population level: 39 community cluster randomised trial of Cardiovascular Health Awareness Program (CHAP). BMJ. 2011;342:d442. doi: 10.1136/bmj.d442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guidelines for the economic evaluation of health technologies: Canada. 4th ed. Ottawa: Canadian Agency for Drugs and Technologies in Health. 2017. [Google Scholar]
- 12.Jacobs MS, Kaasenbrood F, Postma MJ, et al. Cost-effectiveness of screening for atrial fibrillation in primary care with a handheld, single-lead electrocardiogram device in the Netherlands. Europace. 2016 Oct. 12 doi: 10.1093/europace/euw285. [DOI] [PubMed] [Google Scholar]
- 13.Granger CB, Alexander JH, McMurray JJ, et al. ARISTOTLE Committees and Investigators. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981–92. doi: 10.1056/NEJMoa1107039. [DOI] [PubMed] [Google Scholar]
- 14.Ontario Ministry of Health and Long Term Care. Schedule of benefits: physician services under the health insurance act. Toronto: Queen's Printer for Ontario. 2002. (updated 2015). [Google Scholar]
- 15.Lip GYH, Nieuwlaat R, Pisters R, et al. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the Euro Heart Survey on Atrial Fibrillation. Chest . 2010;137:263–72. doi: 10.1378/chest.09-1584. [DOI] [PubMed] [Google Scholar]
- 16.Friberg L, Rosenqvist M, Lip GYH. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182 678 patients with atrial fibrillation: the Swedish Atrial Fibrillation cohort study. Eur Heart J. 2012;33:1500–10. doi: 10.1093/eurheartj/ehr488. [DOI] [PubMed] [Google Scholar]
- 17.Pisters R, Lane DA, Nieuwlaat R, et al. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138:1093–100. doi: 10.1378/chest.10-0134. [DOI] [PubMed] [Google Scholar]
- 18.Lip GY, Edwards SJ. Stroke prevention with aspirin, warfarin and ximelagatran in patients with non-valvular atrial fibrillation: a systematic review and meta-analysis. Thromb Res. 2006;118:321–33. doi: 10.1016/j.thromres.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 19.Table 1a. Complete life table, males, Canada, 2009 to 2011. Ottawa: Statistics Canada. 2015. [Google Scholar]
- 20.Table 1b. Complete life table, females, Canada, 2009 to 2011. Ottawa: Statistics Canada. 2015. [Google Scholar]
- 21.McGrath ER, Kapral MK, Fang J, et al. Investigators of the Ontario Stroke Registry. Association of atrial fibrillation with mortality and disability after ischemic stroke. Neurology. 2013;81:825–32. doi: 10.1212/WNL.0b013e3182a2cc15. [DOI] [PubMed] [Google Scholar]
- 22.Alonso A, Bengtson LGS, MacLehose RF, et al. Intracranial hemorrhage mortality in atrial fibrillation patients treated with dabigatran or warfarin. Stroke. 2014;45:286–91. doi: 10.1161/STROKEAHA.114.006016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hardie K, Hankey GJ, Jamrozik K, et al. Ten-year survival after first-ever stroke in the Perth Community Stroke Study. Stroke. 2003;34:1842–6. doi: 10.1161/01.STR.0000082382.42061.EE. [DOI] [PubMed] [Google Scholar]
- 24.Straube S, Tramèr MR, Moore RA, et al. Mortality with upper gastrointestinal bleeding and perforation: effects of time and NSAID use. BMC Gastroenterol. 2009;9:41. doi: 10.1186/1471-230X-9-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ha ACT, Singh N, Cox JL, et al. Oral anticoagulation for stroke prevention in Canadian practice: Stroke Prevention and Rhythm Interventions in Atrial Fibrillation (SPRINT-AF) Registry. Can J Cardiol. 2016;32:204–10. doi: 10.1016/j.cjca.2015.04.028. [DOI] [PubMed] [Google Scholar]
- 26.Coyle D, Coyle K, Cameron C, et al. Cost-effectiveness of new oral anticoagulants compared with warfarin in preventing stroke and other cardiovascular events in patients with atrial fibrillation. Value Health. 2013;16:498–506. doi: 10.1016/j.jval.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 27.Ontario Ministry of Health and Long-Term Care. Drugs funded by Ontario Drug Benefit (ODB) Program: e-formulary. Toronto: Queen's Printer for Ontario. 2009-2010. [updated 2016 Apr. 10, version 2.4]. [accessed 2016 Mar. 16]. Available https://www.formulary.health.gov.on.ca/formulary/
- 28.Blackhouse G, Assasi N, Xie F, et al. Cost-effectiveness of catheter ablation for rhythm control of atrial fibrillation. Int J Vasc Med. 2013;2013:262809. doi: 10.1155/2013/262809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goeree R, Blackhouse G, Petrovic R, et al. Cost of stroke in Canada: a 1-year prospective study. J Med Econ. 2005;8:147–67. [Google Scholar]
- 30.Mittmann N, Seung SJ, Hill MD, et al. Impact of disability status on ischemic stroke costs in Canada in the first year. Can J Neurol Sci. 2012;39:793–800. doi: 10.1017/s0317167100015638. [DOI] [PubMed] [Google Scholar]
- 31.Patient Cost Estimator. Ottawa: Canadian Institute for Health Information. 1996-2017. [accessed 2016 Oct. 26]. Available https://www.cihi.ca/en/patient-cost-estimator.
- 32.Consumer Price Index, health and personal care, by province (Canada) [table]. Ottawa: Statistics Canada. 2016. [accessed 2016 Apr. 15]. Available www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/econ161a-eng.htm.
- 33.Kind P, Hardman G, Macran S. UK population norms for EQ-5D. Discussion paper 172. York (UK): Centre for Health Economics, University of York. 1999. [Google Scholar]
- 34.Rivero-Arias O, Ouellet M, Gray A, et al. Mapping the modified Rankin Scale (mRS) measurement into the generic EuroQol (EQ-5D) health outcome. Med Decis Making. 2010;30:341–54. doi: 10.1177/0272989X09349961. [DOI] [PubMed] [Google Scholar]
- 35.ACTIVE Investigators. Connolly SJ, Pogue J, Hart RG, et al. Effect of clopidogrel added to aspirin in patients with atrial fibrillation. N Engl J Med. 2009;360:2066–78. doi: 10.1056/NEJMoa0901301. [DOI] [PubMed] [Google Scholar]
- 36.Briggs A, Sculpher M, Claxton K. Decision modelling for health economic evaluation. Oxford (UK): Oxford University Press. 2006. [Google Scholar]
- 37.Daily currency converter. Ottawa: Bank of Canada. 2016. [accessed 2016 Oct. 26]. Available www.bankofcanada.ca/rates/exchange/daily-converter/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.